Abstract
Background
Socioeconomic inequalities in mortality pose a serious impediment to enhance public health even in highly developed welfare states. This study aimed to improve the understanding of socioeconomic disparities in all-cause mortality by using a comprehensive approach including a range of behavioural, psychological, material and social determinants in the analysis.
Methods
Data from The North Denmark Region Health Survey 2007 among residents in Northern Jutland, Denmark, were linked with data from nationwide administrative registries to obtain information on death in a 5.8-year follow-up period (1stFebruary 2007- 31stDecember 2012). Socioeconomic position was assessed using educational status as a proxy. The study population was assigned to one of five groups according to highest achieved educational level. The sample size was 8,837 after participants with missing values or aged below 30 years were excluded. Cox regression models were used to assess the risk of death from all causes according to educational level, with a step-wise inclusion of explanatory covariates.
Results
Participants’ mean age at baseline was 54.1 years (SD 12.6); 3,999 were men (45.3%). In the follow-up period, 395 died (4.5%). With adjustment for age and gender, the risk of all-cause mortality was significantly higher in the two least-educated levels (HR = 1.5, 95%, CI = 1.2-1.8 and HR = 3.7, 95% CI = 2.4-5.9, respectively) compared to the middle educational level. After adjustment for the effect of subjective and objective health, similar results were obtained (HR = 1.4, 95% CI = 1.1-1.7 and HR = 3.5, 95% CI = 2.0-6.3, respectively). Further adjustment for the effect of behavioural, psychological, material and social determinants also failed to eliminate inequalities found among groups, the risk remaining significantly higher for the least educated levels (HR = 1.4, 95% CI = 1.1-1.9 and HR = 4.0, 95% CI = 2.3-6.8, respectively). In comparison with the middle level, the two highest educated levels remained statistically insignificant throughout the entire analysis.
Conclusion
Socioeconomic inequality influenced mortality substantially even when adjusted for a range of determinants that might explain the association. Further studies are needed to understand this important relationship.
Electronic supplementary material
The online version of this article (doi:10.1186/s12889-015-1813-3) contains supplementary material, which is available to authorized users.
Keywords: Educational inequality, Health status disparities, Educational status, Social class, Socioeconomic factors, Social determinants of health, Mortality, Proportional hazards models, Survival analysis
Background
Socioeconomic inequalities in mortality have been observed in several high-income countries [1-7]. This is revealed not only when comparing the most advantaged and the most disadvantaged social groups– a gradient can be observed across the entire socioeconomic hierarchy [1-3,6,8]. In Denmark, with its relatively low economic inequality, a high level of income protection and universally tax-financed healthcare, the past twenty years have seen increasing inequality in mortality [1]. This poses a serious challenge to public health [1-3,8], as reflected by the priority given by World Health Organization (WHO) to the social determinants of health in its draft for the 12th general work programme for 2014 – 2019 [9]. Providing for equality in health is a moral obligation, as both Mackenbach and Marmot have emphasized [8,10]. Despite a broad recognition of the importance of this subject the reasons for these disparities are still unknown [1-3,8,11,12]. It is crucial to obtain a comprehensive understanding of their underlying causes, as this is vital to prevent the persistence of the disparities [2,11,13]. Sociological theory explains health disparities by social stratification comprised of three components. Firstly, mobility mechanisms that place individuals into social strata causing differences in the personal characteristics of individuals between strata. Secondly, allocation rules causing differences in distribution of resources to social strata resulting in inequalities between social strata in access to material and immaterial resources. Thirdly, social processes that render some resources of greater value than others, i.e. resources that can be used to avoid health problems [8]. Additional theories can be related to the social stratification perspective. The theory of “fundamental causes” suggests that social forces underlying the social stratification induce health disparities as opposed to the proximal risk factors such as smoking, drinking and eating habits. Distal resources such as knowledge, money, power, prestige and beneficial social connections, that can be applied to enhance health, are distributed differently among social strata [8,14]. Health disparities may also arise from health-related selection during social mobility i.e. individuals are sorted into social classes based on health or psychosocial determinants as stipulated by the “social selection” theory [8,15]. The “Neo-materialist” theory propose that disparities in material recourses remain in welfare stats despite of relatively small income inequalities, and what remains is still substantial for health disparities, partly because material disadvantage is associated with lifestyle diseases resulting from poor health-related behaviours, such as lack of physical exercise and unhealthy diet etc [8,15]. Unequal distribution of psychosocial determinants such as psychosocial stress, lack of sense of control and social support may also be of importance in the explanation of health inequalities, as suggested by the “Psychosocial” theory [8,15]. Moreover the theory of “Diffusion of innovations” emphasizes that health disparities result from faster adaption of new healthy behaviours and earlier pick up of interventions among individuals with a higher socioeconomic status [8]. None of these theories are mutually exclusive, and they may be apparent simultaneously and reinforce each other [8,15]. Researchers have thus proposed various theories on the persistence of health inequalities in welfare states [8], from which potential pathways underlying the inequalities have been developed including behavioural, psychological, material and social mechanisms (Table 1) [11-13,16,17].
Table 1.
Potential mechanisms underlying socioeconomic inequalities in all-cause mortality
| Behavioural mechanisms | Psychological mechanisms |
|---|---|
| Differences in socioeconomic strata in terms of health-related behaviours and lifestyles, including smoking habits, alcohol consumption, exercise and dietary patterns as well as morbid obesity [8,15]. | Disparities in personality profile and psychological resources, such as cognitive ability, knowledge, cooping abilities, attitude, a sense of control and perceived social standing. The personality profile is believed to be a determining factor for the socioeconomic position, as educational and occupational achievements are dependent on personal talent and effort [8]. Furthermore, psychological stress is hypothesized to increase the risk of premature mortality by producing disruptions in the neuroendocrine system [8,15]. |
| Material mechanisms | Social mechanisms |
| Unequal distribution of material resources such as income, but also what income enables i.e., being able to afford healthy food, access to goods and services, favourable living and housing conditions, employment status, service provision such as schools and transport and welfare to population health [8,15]. | Stratified difference in social resources such as social relationships, social support, interpersonal trust, norms of reciprocity and mutual aid, power and prestige [8,15]. |
These mechanisms may, both independently and in combination, by reinforcing each other, influence the socioeconomic gradient in mortality [11,13,17]. It is crucial to focus on the identification of determinants that may explain the socioeconomic inequalities in mortality [1-3,8,11,13]. Studies have investigated the impact of behavioural determinants on the association between socioeconomic position and mortality. These found, that the association was substantially accounted for by adjustment for health-related behavioural determinants [16,18-23]. In addition, only few studies have combined the study of behaviours in combination with study of material or psychosocial determinants [11-13,17,24,25], possibly because data on the composition of social strata or on the distribution of immaterial determinants among social groups can be difficult to obtain [8]. This study linked data from The North Denmark Region Health Survey 2007 with individual-level data obtained from nationwide administrative registers. The self- administrated health survey obtained information on demographic characteristics, lifestyle factors, disease, quality of life, work characteristics, social support etc. [26].
Aim
The aim of our study was to explore whether behavioural, material, psychological and social determinants could explain the association between educational status and all-cause mortality. This was done by investigating the separate and mutual effect for each group of determinants.
Methods
Design and population
A register-based cohort study of inhabitants in the Danish Region of Northern Jutland was conducted with a follow-up period from the 1st February 2007 to 31st December 2012. The participants had previously answered a postal questionnaire, sent to a sample of 23,491 citizens in Northern Jutland, Denmark, aged 16-80 years drawn randomly from a population of 438,759 inhabitants in the Civil Registration System [26,27]. The sample was stratified by the region’s 11 municipalities. Two reminders were sent to citizens who had not returned the health survey [26]. For the current study only participants aged ≥30 years were included, as final educational status was considered to be acquired at this age. This excluded 1,266 participants aged 16-29 years, leaving a total of 10,231 participants. The response rate was 51.79% (49.90% men) among subjects aged ≥30 years. Information on educational status was missing for 125 (1.22%) participants, reducing the study population to 10,106 subjects. Only participants with no missing on all of the independent variables were included in the final sample, resulting in 8,837 subjects.
Socioeconomic status
A conceptual challenge exists in defining socioeconomic position on an individual level. Often used measurements include educational status, income or occupational class [25,28]. It has been demonstrated that these factors cannot be used interchangeably as they are related to different causal processes [28]. In this study, educational status served as a proxy for the participants’ socioeconomic position, as this is a fundamental determinant of both occupation and income [28]. Information on individuals’ highest completed course of education was obtained from the Population’s Education Register. The register only provides information on education authorised by the Danish Ministry of Education and of a duration of more than 80 hours [29]. Based on the International Standard Classification of Education (ISCED 2011) [30], we grouped participants according to their highest completed education, but deviated from the ISCED classification for the fourth level, i.e., post-secondary non-tertiary education, as no such programmes exist in Denmark [31]. Instead, programmes at ISCED level 3 were split into two, resulting in five groups (A-E):
-
A.
Early childhood education, primary education and lower secondary education (ISCED levels 0-2)
-
B.
General upper secondary education, high school programmes (ISCED level 3)
-
C.
Vocational upper secondary education, vocational training and education (ISCED level 3)
-
D.
Short or medium-length higher education, first-cycle programmes tertiary education, bachelor or equivalent (ISCED level 5-6)
-
E.
Long length higher education, second-cycle programmes, Master’s or equivalent, or Third-cycle programmes Doctoral, PhD programmes or equivalent (ISCED levels 7-8)
All-cause mortality
Information on all-cause mortality was obtained from the Civil Registration System [27]. Time to death was measured by days from the time of receiving questionnaire the 1st of February 2007 until death, emigration or end of follow-up, right censoring on December 31st 2012, resulting in a 5.8 year follow-up period.
Demographic information and health status
Demographic information on age and gender was gathered from Civil Registration System [27]. Based on information from the National Patient Registry co-morbidity was measured using the Charlson index [32]. The register holds information on all admissions and outpatients visits to Danish hospitals and specialty clinics. All admissions and visits were registered by a primary diagnosis and, if appropriate, one or more secondary diagnoses, according to the International Classification of Diseases, 10th Revision [33]. Objective health was assessed based on Charlson co-morbidity scores, a weighted index that takes into account the number and the seriousness of co-morbid diseases. Each condition was assigned a score of 1, 2, 3, or 6, depending on the associated risk of dying [32]. The objective health variable was formed based on the Charlson co-morbidity scores 0, 1, 2 and ≥3 (Additional file 1: Table S2a). Information on subjective self-reported health was obtained from the health survey by the global question “In general how do you assess your current health?” with five response options ranging from Very good to Very poor, and a Don’t know response [26] The subjective health variable was formed on the basis of the response options (Additional file 1: Table S2a).
Health-related behavioural, material, psychological and social determinants
Our study included a range of determinants in the explanation of the association between educational status and all-cause mortality. Based on the underlying mechanisms, the explanatory variables were divided into four groups: behavioural, material, psychological and social determinants, as shown in Table 1. Information on explanatory determinants was obtained from the health survey [26] and the Income Statistics Register [34]. The exact wording of the questions and the matching response options used in the self-reported questionnaire are shown in the (Additional file 1: Tables S2b-e).
Behavioural determinants
The behavioural determinants included smoking patterns, alcohol intake, Body Mass Index (BMI), dietary and exercise habit. Behavioural variables were formed on the basis of the response options (Additional file 1: Table S2b) with the exception of alcohol intake and BMI. Alcohol intake was estimated according to Danish Health and Medicines Authority recommendations on risk behaviours [35], which are based on the respondents’ weekly consumption of units (Additional file 1: Table S2b). Participants were categorized into three groups based on consumption and gender, i.e. (women/men) low-risk alcohol intake (<7/<14 units per week), moderate-risk alcohol intake (7-14/14-21 units per week), and high-risk alcohol intake (>14/>21 units per week) [35]. The participant’s BMI was calculated from information on weight and height (Additional file 1: Table S2b). A standard classification of BMI was used, <18.5 (underweight), 18.5 – 24.9 (normal weight), 25-29.9 (overweight), 30 -35 (obese I) and >35 (obese II) [36].
Psychological determinants
The psychological determinants included feeling stress, anxiety, nervousness, restlessness, hopelessness, unhappiness, feeling depressed and having too many worries. Psychological variables were formed on the basis of the response options (Additional file 1: Table S2c).
Material determinants
The material determinants included profession, income, residential area, type of residence, residential ownership, difficulty paying bills and use of neighbourhood facilities. With the exception of information on income, the material variables were formed on the basis of the response options (Additional file 1: Table S2d). Income information was obtained from the Income Statistics Register, which includes information on all tax return forms, thus covering all economically active citizens [34]. To obtain stable measures for household incomes and individual incomes, an average of income in three successive years (2004, 2005 and 2006) was calculated. Three groups were formed for both household and individual incomes; low, average and high income.
Social determinants
The social determinants included time spent with family or friends, being able to count on others for help, loneliness, trust and reciprocity, marital status, use of cultural facilities, social involvement in the local community and association activities. Social variables were formed on the basis of the response options (Additional file 1: Table S2e).
Ethics
The study was approved by the Danish Data Protection Agency (Ref.GEH-2014-014). All data were linked and stored in computers held by Statistics Denmark and made available with de-identified personal information to ensure that individuals could not be identified. In accordance with the Act on Processing of Personal Data only aggregated statistical analyses and results are published [37,38]. Retrospective anonymized register-based studies do not require obtained written informed consent and ethical approval [37,38].
Statistical analyses
For descriptive statistics, continuous variables were compared with Analysis of Variance (ANOVA) tests and discrete variables with Chi-square (Chi2) tests to test for difference between groups. Comparison of survival was performed with Proportional Hazards Cox Regression models. Time-on-study was used as the timescale. Hazard ratios (HR) and the corresponding 95% confidence intervals (95% CI) were determined. Educational level C, vocational upper secondary education was chosen as the reference group on the basis of size, as this group was the largest of the five educational levels. Analyses were performed in three preselected steps; initially, a calculation using a model adjusted for age and gender was performed (Model 1), followed by a calculations allowing for further adjustment for objective and subjective health (Model 2). A third model allowed additional adjustment for selected behavioural, psychological, material and social determinants (Model 3), with a step-wise inclusion of variables. Subjects were censored at the end of the follow-up period (31st December 2012). Analyses were conducted applying a design weight to correct for sample selection bias, as respondents in the different municipalities did not have equal chances of receiving the questionnaire. The proportional hazards assumption and the linearity assumption of the proportional hazards Cox regression model were tested and found to be valid. Schoenfeld’s residuals were used to test the proportional hazards assumption. We examined possible interactions between gender and educational status, and potential interactions between age and educational status. No statistically significant interactions were detected. The level of statistical significance was set at a p-value <0.05 for all statistical analyses. To detect whether excluding subjects with missing values on any of the independent variables would bias the results we performed a sensitivity analysis conducting the multivariable analyses on the full sample (n = 10,106), i.e. using all available data in the different models, (Additional file 2: Figure S3a, Additional file 3: Figure S3b). All data management were performed using SAS software, version 9.4 (SAS Institute Inc., Cary, North Carolina, USA) and all analyses were executed using R Studio software, version 0.97.551 (R Studio, Inc. ©2009-2012, part of the R statistical software package, version 3.0.2, Development Core Team).
Results
Participants’ characteristics
Subjects’ mean age was 54.1 years (SD 12.6); 45.3% were men (n = 3,999). Additional file 1: Table S2 gives in condensed form information on baseline characteristics of the study population by educational status. The total distribution of demographic and all explanatory variables according to educational level can be found as Additional file 1: Tables S2a-e, (in the additional files).
Educational level A
Participants, whose highest education was primary school, were at baseline characterized by a high average age (59.6 years (±12.0)), a high proportion of death (7.4% (n = 207)), co-morbidity (3.8% (n = 107)), poor self-rated health (43.2% (n = 1,213)) obesity (15.3% (n = 429)) and were smokers (28.9%(n = 813)). Many had low income (51.1% (n = 1,434)), were tenants (17.4% (n = 489)) and flat-dwellers (9.4% (n = 265)) and were pensioners or on early retirement (49.9% (n = 1,507)). Use of community house or centre (9.7% (n = 272)) and clubs for older people (14.3% (n = 401)) were also prevalent in this group.
Educational level B
Respondents, with general upper secondary education, were characterized by lower average age (45.9 (±10.4)), a high prevalence of co-morbidity (2.1% (n = 5)), stress (64.5% (n = 151)) and difficulties with paying bills (4.3% (n = 10)).
Educational level C and D
Respondents, with vocational upper secondary education and short-to-medium higher education, respectively, were non-diverse in terms of baseline characteristics compared to the other educational levels.
Educational level E
Among respondents with a long higher education, high incomes were prevalent (77.1% (n = 273)), as was the use of neighbourhood facilities such as parks (49.4% (n = 175)), cinemas and theatres (17.8% (n = 63)). This group participated in association activities (46.3% (n = 164)) and spent less time with family (44.6% (n = 158)). Many were non-smokers (84.5% (n = 299)); alcohol consumption was high (20.3% (n = 72)) and self-rated health was good (81.4% (n = 288)).
Unadjusted and adjusted risk of all-cause mortality
In the 5.8-year follow-up period, 395 (4.5%) deaths occurred. All-cause mortality was unevenly distributed across educational levels; significantly more deaths occurred in the least educated groups (p < 0.001). Using multivariable Cox regression models with adjustment for confounding by age and gender, we found that the risk of mortality was significantly higher among respondents on levels A and B (Figure 1, model 1), (HR = 1.49, 95%CI = 1.20-1,84 and HR = 3.71, 95% CI = 2.35-5.87, respectively). The midmost level C, was chosen as reference group. In comparison with level C, no statistically significant difference was observed between the highest educational levels, D and E, (HR = 1.23, 95% CI = 0.79-1.92 and HR = 1.10, 95% CI = 0.59-2.04, respectively). Further adjustment for the effect of objective and subjective health (Figure 1, Model 2) resulted in comparable patterns for levels D and E, (HR = 1.26, 95% CI = 0.83-1.91 and HR = 1.10, 95% CI = 0.56-2.17, respectively). The higher risk of mortality also remained statistically significant for the respondents with shortest schooling, levels A and B (HR = 1.35, 95% CI = 1.08-1.68, and HR = 3.52, 95% CI = 1.97-6.29, respectively). The inequality among groups failed to disappear when adjustment was made for the effect of behavioural, psychological, material and social determinants (Figure 1, Model 3). The risk of mortality thus remained significantly higher among levels A and B (HR = 1.42, 95% CI = 1.08-1.86 and HR = 3.98, 95% CI = 2.33-6.78, respectively). Statistical differences remained statistically insignificant when comparing levels D and E with level C, (HR = 1.55, 95% CI = 0.93-2.58 and HR = 1.55, 95% CI = 0.75-3.18, respectively).
Figure 1.
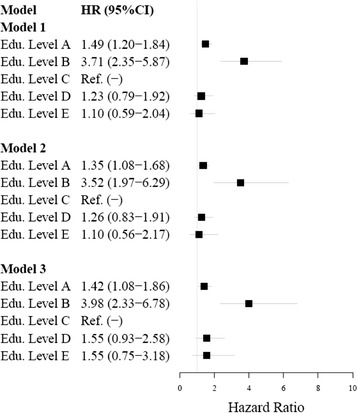
Hazard ratios and 95% confidence intervals for educational status calculated by Cox regression models on complete cases.
The effects of each group of determinants are shown in an additional file, (Additional file 2: Figure S2). Model 4 of this figure corresponds to a basic model with adjustment for the confounding effect of age and gender along with objective and subjective health. Further adjustment for the effect of behavioural determinants (Additional file 4: Figure S2, Model 5), the risk of mortality remained significantly higher on levels A and B, (HR = 1.35, 95% CI = 1.08-1.68, and HR = 3.56, 95% CI = 1.85-6.83, respectively). Similar results were found after additionally adjustment for the effect of psychological determinants (Additional file 4: Figure S2, Model 6). The mortality risk remained significantly higher on levels A and B (HR = 1.36, 95% CI = 1.09-1.71, and HR = 3.56, 95% CI = 1.92-6.61, respectively). After further adjustment for the effect of material determinants (Additional file 4: Figure S2, Model 7), the risk of mortality remained significantly higher on levels A and B (HR = 1.39, 95% CI = 1.10-1.75, and HR = 4.62, 95% CI = 2.29-9.36, respectively), when comparing with level C. The mortality risk did not show significant changes for levels D and E, although increased risk was noted (HR = 1.62, 95% CI = 0.91-2.87 and HR = 1.46, 95% CI = 0.56-3.78, respectively). Neither did additional adjustment for the effect of social determinants (Additional file 4: Figure S2, Model 8) affect the risk of mortality, which remained significantly higher on levels A and B, (HR = 1.42, 95% CI = 1.08-1.86, and HR = 3.98, 95% CI = 2.33-6.78, respectively).
Sensitivity analysis
The analysis on the full analytical sample (n = 10,106) using all available data in the different models produced results similar to those of the main analysis on complete cases (n = 8,837), (Additional file 3: Figure S3a and Additional file 4: Figure S3b in the additional files).
Discussion
Our study examined whether behavioural, psychological, material and social determinants could explain the association between socioeconomic status and all-cause mortality. The risk of mortality was found to vary across educational levels and to be significantly higher for respondents from the lower socioeconomic strata. Adjustment for behavioural, psychological, material and social determinants failed to eliminate the effect of the inequalities, as the risk remained significantly higher for the two groups with lowest educational levels (A, primary education and B, General upper secondary education) when compared with the midmost educational level (C, vocational upper secondary education). Surprisingly, no clear gradient in socioeconomic inequality as measured by educational achievement could be detected, as we found no statistically significant difference between the second-highest and the highest educational levels, when compared with the midmost educational level.
Strengths and limitations
Our study derives part of its strength from our comprehensive approach apparent from the inclusion of health-related behavioural, psychological and material as well as social determinants. Furthermore, the use of educational status as a proxy for socioeconomic position offered the double advantage of relative stability over a lifespan, and the ease of retrieval and recording. The risk of selection bias was minimized by the choice of educational status, which introduces less reverse causation than its alternative, occupational class and income, as mobility of individuals with poor health into certain strata is less likely to be effected by differences in educational level. Selection bias is more likely to influence health differences by occupational class and income, as occupation and income tends to decrease when an individual become chronically ill [28]. The independent effects of occupation and income were moreover taken into account by making separate adjustments for the effect of each dimension [28]. The use of all-cause mortality as the outcome measure had several advantages as this endpoint requires no further ascertainment than the time of death, thus preventing bias stemming from the classification of cause of death.
The criterion for selection of registers was content validity weighed against the quantity and relevance of the data. The accessibility, location and time covered by the register data were also considered [37]. Overall, the data obtained from registers was considered to be of high-quality information [27,29,33,34,37]. Among the limitations of the study are some unexpected irregularities in educational data. These occurred as a consequence of several changes in the educational system over the years; hence, data from before 1974 and for immigrants with no Danish schooling are self-reported, which increases the likelihood of misclassification [29]. Furthermore, income data may be biased by the impact of undeclared work, etc. [34]. Data obtained from the regional health survey may be biased as to selection, because of the non-response rate (48.2%), exactness of information obtained as well as missing values. Analysis on the full sample size, using all available data in the different models, did however not change the study results. As the outcome measure of all-cause mortality involves all causes of death, an uneven distribution across the groups cannot be ruled out. As the outcome measure all-cause mortality has the disadvantage of being a concept including many possible causes of death, which may be distributed differently across socioeconomic strata. The measure furthermore represents a combination of the effect of disease incidence, access to treatment, and survival. Hence, the observed inequalities may at least partially be due to disparities in survival after disease incidence or in the distribution of more lethal diseases. Thus, caution should be exercised when interpreting the results, as determinants of prolonged survival might not be the same as for disease incidence and treatment access. Data obtained on the explanatory determinants was self-reported and several variables were proxies. Objective measures and more detailed questions may have yielded a more accurate estimation of the contribution of the various determinants. Other explanatory determinants may have been needed in order to explain the association. Furthermore, exploring the association between educational level and all-cause mortality has methodological shortcomings. This approach does not allow for a causal interpretation of the observed changes in hazard ratios and can lead to an underestimation of the effect of the determinants and an overestimation of the effect of educational status on the association [39]. Additionally, we obtained information on many possible confounders such as age, gender and co-morbidity, but despite adjustment for the most relevant ones residual effects may be present as the design does not eliminate unmeasured confounders that could possibly affect the results. The response rate was less than 52% and the rate was particularly low among young men. Low response rates in some subgroups of the study population pose problems in the representativeness of the study population with the background population. Previous studies have shown a tendency to higher response rates among higher educated subjects [40] and lower mortality rates among participants than non-participants [41,42]. Hence it is possible that the contrast in educational level and health-related determinants observed in the study population were underrated in proportion to the general population. For these reasons caution should be taken when generalizing the results to the general population. Caution in interpretation is also warranted because of the limited number of deaths occurring in a study population and follow-up time of this magnitude.
Interpretation
The study gave evidence of substantial inequality in all-cause mortality among the citizens of Northern Jutland, Denmark, as significantly more subjects from the lower socioeconomic strata died in the study period. Our results are similar to those found in comparable studies investigating the distribution of all-cause mortality among socioeconomic strata [1-7]. The risk of mortality was significantly higher on the second lowest educational level, where the average age was lower, thus the cause of death may have been different from those on the other educational levels [43]. Different causes such as the use of health benefits, or coping skills may therefore have been involved. The mortality risk remained significantly higher for respondents on lowest socioeconomic levels, which could possibly be explained by greater exposure to a wide range of risk factors for poor health over the life course. They may moreover have become more homogeneous regarding personal characteristics of significance to health, such as cognition, knowledge, material means, social support and health-related behaviours, as these disparities over time may lead to differences in risk factor profiles and vulnerability to such risk factors across socioeconomic strata [17]. A better understanding of the association between socioeconomic status and all-cause mortality is necessary to reduce the socioeconomic inequalities in mortality, which we were unable to explain by adjusting for behavioural, psychological, material and social determinants. While our results support comparable work [12,16,25], other studies have concluded that the gradient in all-cause mortality is explainable after adjustment for material determinants, either on their own or in combination with behavioural and psychosocial determinants [11,13,17]. In our study, adjustment for the effect of material determinants did increase the mortality risk on the lowest socioeconomic levels, but we found no indication of a strong effect of material determinants on all-cause mortality. However, unequal access to material resources may lead to differences in life circumstances in youth, ultimately resulting in lasting disparities in health. A life- course perspective focusing on fundamental causes, distal factors and habitus [14,44,45], therefore seems required to explain socioeconomic inequalities in all-cause mortality. Our study and previous studies are based on a causation theory, explaining inequalities in mortality by stratified differences in health determinants, thus an overlap of potential mechanisms should be considered in explaining the socioeconomic inequalities. None of these mechanisms are mutually exclusive; the different mechanisms could thus be interrelated, thereby challenging our ability to account for the effect on the socioeconomic gradient in all-cause mortality [11,13,17]. These reverse causalities can be categorized as measurement errors leading to possible bias in estimates [12]. Our simplified study models cannot account for the multiple pathways underlying the inequality, i.e. the methods applied were unable to account for the possible multiple mechanisms underlying the inequalities, as only the association between educational level and all-cause mortality was assessed. To prevent a development towards stronger disparity, further exploration into these complex issues is needed. We need to understand why an underprivileged socioeconomic position places people at higher risk of death than their better-off compatriots. Further exploration of the possibility that the underprivileged groups form a homogenous group is needed, as our data may have given an insufficient description. A life-course perspective to explain the persistent inequalities in all-cause mortality seems necessary for progress, as we believe this perspective is crucial to allow for the multiple mechanisms and pathways and to account for the inequality in all-cause mortality.
Conclusion
This study has demonstrated the existence of substantial inequality in all-cause mortality among citizens of Northern Jutland, Denmark. Despite the comprehensive approach, with incremental adjustment for the effect of a range of determinants, we were unable to account for the inequality revealed by the data. Uncovering the multiple underlying pathways may require less simplified models. We recommend that future research takes a life-course perspective that includes distal factors while simultaneously accounting for the complexity of the underlying multiple mechanisms and pathways to explain the association between socioeconomic status and all-cause mortality.
Acknowledgements
The authors wish to express their gratitude for the assistance and support received from the Public Health and Epidemiology Group at the Department of Health Science and Technology at Aalborg University. The North Denmark Region Health Survey 2007 was founded by The North Denmark Region.
Additional files
Table S2a. Baseline demographic characteristics, by educational level. Table S2b. Baseline behavioural characteristics, by educational level. Table S2c. Baseline psychological characteristics, by educational level. Table S2d. Baseline material characteristics, by educational level. Table S2e. Baseline social characteristics, by educational level.
Hazard ratios and 95% confidence intervals for educational status estimated by Cox regression models on complete cases (n = 8,837).
Hazard ratios and 95% confidence intervals for educational status estimated by Cox regression models on the full study sample - using all available data in the different models.
Hazard ratios and 95% confidence intervals for educational status estimated by Cox regression models on the full study sample - using all available data in the different models.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CO, CTP and LRBUC conceived the concept for the study and are responsible for its design. LRBUC carried out the data management process and statistical analyses with help and advice from CTP, RNM and LEJ. LRBUC drafted the manuscript. CTP, CO, HVN, KF, HB, RNM, LEJ, SRJK and SMH contributed to interpretation of data. All authors have critically revised the text for important intellectual content and have read and approved the final manuscript and are accountable for all aspects of the work.
Contributor Information
Line R Ullits, Email: lchris@hst.aau.dk.
Linda Ejlskov, Email: lej@hst.aau.dk.
Rikke N Mortensen, Email: rnm@hst.aau.dk.
Steen M Hansen, Email: sh@hst.aau.dk.
Stella R J Kræmer, Email: srjk@hst.aau.dk.
Henrik Vardinghus-Nielsen, Email: hvn@hst.aau.dk.
Kirsten Fonager, Email: kfo@hst.aau.dk.
Henrik Bøggild, Email: boggild@hst.aau.dk.
Christian Torp-Pedersen, Email: ctp@hst.aau.dk.
Charlotte Overgaard, Email: co@hst.aau.dk.
References
- 1.Diderichsen F, Andersen I, Manuel C, Andersen AN, Bach E, Baadsgaard M, et al. Health Inequality - determinants and policies. Scand J Public Health. 2012;40:12–105. doi: 10.1177/1403494812457734. [DOI] [PubMed] [Google Scholar]
- 2.Gallo V, Mackenbach JP, Ezzati M, Menvielle G, Kunst AE, Rohrmann S, et al. Social Inequalities and Mortality in Europe - Results from a Large Multi-National Cohort. PLoS One. 2012;7(7):e39013. doi: 10.1371/journal.pone.0039013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mackenbach JP, Stirbu I, Roskam AR, Schaap MM, Menvielle G, Leinsalu M, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358(23):2468–81. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 4.Kunst AE, Mackenbach JP. The size of mortality differences associated with educational-level in 9 industrialized countries. Am J Public Health. 1994;84(6):932–7. doi: 10.2105/AJPH.84.6.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fawcett J, Blakely T, Kunst A. Are mortality differences and trends by education any better or worse in New Zealand? A comparison study with Norway, Denmark and Finland, 1980-1990s. Eur J Epidemiol. 2005;20(8):683–91. doi: 10.1007/s10654-005-7923-y. [DOI] [PubMed] [Google Scholar]
- 6.Mackenbach JP, Bos V, Andersen O, Cardano M, Costa G, Harding S, et al. Widening socioeconomic inequalities in mortality in six Western European countries. Int J Epidemiol. 2003;32(5):830–7. doi: 10.1093/ije/dyg209. [DOI] [PubMed] [Google Scholar]
- 7.Rehkopf DH, Berkman LF, Coull B, Krieger N. The non-linear risk of mortality by income level in a healthy population: US National Health and Nutrition Examination Survey mortality follow-up cohort, 1988-2001. BMC Public Health. 2008;8:383. doi: 10.1186/1471-2458-8-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mackenbach JP. The persistence of health inequalities in modern welfare states: the explanation of a paradox. Soc Sci Med. 2012;75(4):761–9. doi: 10.1016/j.socscimed.2012.02.031. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization (WHO) Twelfth General Programme of Work 2014–2019: not merely the absence of disease. 2014. [Google Scholar]
- 10.Marmot M. Why should the rich care about the health of the poor? CMAJ. 2012;184(11):1231–2. doi: 10.1503/cmaj.121088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Oort FVA, van Lenthe FJ, Mackenbach JP. Material, psychosocial, and behavioural factors in the explanation of educational inequalities in mortality in the Netherlands. J Epidemiol Community Health. 2005;59(3):214–220. doi: 10.1136/jech.2003.016493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muennig P, Kuebler M, Kim J, Todorovic D, Rosen Z. Gender differences in material, psychological, and social domains of the income gradient in mortality: implications for policy. PLoS One. 2013;8(3):e59191. doi: 10.1371/journal.pone.0059191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Skalicka V, van Lenthe F, Bambra C, Krokstad S, Mackenbach J. Material, psychosocial, behavioural and biomedical factors in the explanation of relative socio-economic inequalities in mortality: evidence from the HUNT study. Int J Epidemiol. 2009;38(5):1272–84. doi: 10.1093/ije/dyp262. [DOI] [PubMed] [Google Scholar]
- 14.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;35:80–94. doi: 10.2307/2626958. [DOI] [PubMed] [Google Scholar]
- 15.Bartley M. Health inequality: an introduction to theories, concepts and methods. Cambridge: Polity Press; 2004. [Google Scholar]
- 16.Stringhini S, Sabia S, Shipley M, Brunner E, Nabi H, Kivimaki M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159–66. doi: 10.1001/jama.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schrijvers CTM, Stronks K, van de Mheen HD, Mackenbach JP. Explaining educational differences in mortality: the role of behavioral and material factors. J Public Health. 1999;89(4):535–40. doi: 10.2105/AJPH.89.4.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nandi A, Glymour MM, Subramanian SV. Association among socioeconomic status, health behaviors, and all-cause mortality in the United States. J Epidemiol. 2014;25(2):170-170-7. doi: 10.1097/EDE.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 19.Nordahl H, Lange T, Osler M, Diderichsen F, Andersen I, Prescott E, et al. Education and cause-specific mortality: the mediating role of differential exposure and vulnerability to behavioral risk factors. J Epidemiol. 2014;25(3):389-389-96. doi: 10.1097/EDE.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 20.McFadden E, Luben R, Wareham N, Bingham S, Khaw K. Occupational social class, educational level, smoking and body mass index, and cause-specific mortality in men and women: a prospective study in the European Prospective Investigation of Cancer and Nutrition in Norfolk (EPIC-Norfolk) cohort. Eur J Epidemiol. 2008;23(8):511-511-22. doi: 10.1007/s10654-008-9267-x. [DOI] [PubMed] [Google Scholar]
- 21.Stringhini S, Dugravot A, Shipley M, Goldberg M, Zins M, Kivimäki M, et al. Health behaviours, socioeconomic status, and mortality: further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLoS Med. 2011;8(2):e1000419-e1000419. doi: 10.1371/journal.pmed.1000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laaksonen M, Talala K, Martelin T, Rahkonen O, Roos E, Helakorpi S, et al. Health behaviours as explanations for educational level differences in cardiovascular and all-cause mortality: a follow-up of 60 000 men and women over 23 years. Eur J Public Health. 2008;18(1):38-38-43. doi: 10.1093/eurpub/ckm051. [DOI] [PubMed] [Google Scholar]
- 23.Lantz PM, Golberstein E, House JS, Morenoff J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of US adults. Soc Sci Med. 2010;70(10):1558–66. doi: 10.1016/j.socscimed.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Regidor E, Kunst AE, Rodriguez-Artalejo F, Mackenbach JP. Small socio-economic differences in mortality in Spanish older people. Eur J Public Health. 2012;22(1):80–5. doi: 10.1093/eurpub/ckr051. [DOI] [PubMed] [Google Scholar]
- 25.Khang Y, Lynch JW, Yang S, Harper S, Yun S, Jung-Choi K, et al. The contribution of material, psychosocial, and behavioral factors in explaining educational and occupational mortality inequalities in a nationally representative sample of South Koreans: Relative and absolute perspectives. Soc Sci Med. 2009;68(5):858–66. doi: 10.1016/j.socscimed.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 26.The North Denmark region and The National Institute of Public Health, University of Southern Denmark, Rasmussen NK, Pedersen J, Hayes VS, Hesse U, Biering-Sørensen S. Sådan står det til med sundheden i Nordjylland : Sundhedsprofil for Region Nordjylland og 11 nordjyske kommuner. 2007 [http://www.rn.dk/Sundhed/Til-sundhedsfaglige-og-samarbejdspartnere/Sundhedsfremme-og-forebyggelse/Sundhedsprofil/Sundhedsprofil-2007/Resultater/~/media/Rn_dk/Sundhed/Til%20sundhedsfaglige%20og%20samarbejdspartnere/Sundhedsfremme%20og%20forebyggelse/Sundhedsprofil/2007/Sundhedsprofil2007.ashx]
- 27.Pedersen CB. The Danish civil registration system. Scand J Public Health. 2011;39:2225. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 28.Geyer S, Hemströem O, Peter R, Vågerö D. Education, income, and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. J Epidemiol Community Health. 2006;60(9):804–810. doi: 10.1136/jech.2005.041319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jensen VM, Rasmussen AW. Danish education registers. Scand J Public Health. 2011;39:91–4. doi: 10.1177/1403494810394715. [DOI] [PubMed] [Google Scholar]
- 30.United nation educational scientific and cultural organisation (UNESCO) United nation educational scientific and cultural organisation (UNESCO), Institute for Statistics . International Standard Classification of Education (ISCED) 2011. Canada: ISBN; 2012. [Google Scholar]
- 31.European commission Eurydice, © European Union, 1995-2015, European Encyclopedia on National Education Systems. Structure of the national education system 2013/14: [https://webgate.ec.europa.eu/fpfis/mwikis/eurydice/index.php/Denmark:Overview]
- 32.Charlson ME, Pompei P, Ales KL, Mackenzie CR. A New method of classifying prognostic Co-morbidity in longitudinal-studies - development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 33.Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health. 2011;39:30–3. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 34.Baadsgaard M, Quitzau J. Danish registers on personal income and transfer payments. Scand J Public Health. 2011;39:103–5. doi: 10.1177/1403494811405098. [DOI] [PubMed] [Google Scholar]
- 35.Danish Health and Medicines Authority, Sundhedsstyrelsen . Alcohol - Stop before 5 units - it can make a difference, Our 7 recommendations about alcohol. 2014. [Google Scholar]
- 36.World Health Organization . Obesity: preventing and managing the global epidemic. Report of a WHO Consultation (WHO Technical Report Series 894) Geneva, Switzerland: ISBN; 2000. [PubMed] [Google Scholar]
- 37.Thygesen LC, Daasnes C, Thaulow I, Bronnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: Structure, access, legislation, and archiving. Scand J Public Health. 2011;39:12–6. doi: 10.1177/1403494811399956. [DOI] [PubMed] [Google Scholar]
- 38.The Danish Data Protection Agency, Datatilsynet . Compiled version of the Act on Processing of Personal Data. 2014. [Google Scholar]
- 39.Lange T, Hansen JV. Direct and indirect effects in a survival context. J Epidemiol. 2011;22(4):575-575-81. doi: 10.1097/EDE.0b013e31821c680c. [DOI] [PubMed] [Google Scholar]
- 40.Tjønneland A, Olsen A, Boll K, Stripp C, Christensen J, Engholm G, et al. Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health. 2007;35(4):432-432-41. doi: 10.1080/14034940601047986. [DOI] [PubMed] [Google Scholar]
- 41.Andersen LB, Vestbo J, Juel K, Bjerg AM, Keiding N, Jensen G, et al. A comparison of mortality rates in three prospective studies from Copenhagen with mortality rates in the central part of the city, and the entire country. Copenhagen Center for Prospective Population Studies. Eur J Epidemiol. 1998;14(6):579-579-85. doi: 10.1023/A:1007485116788. [DOI] [PubMed] [Google Scholar]
- 42.Osler M, Linneberg A, Glümer C, Jørgensen T. The cohorts at the research centre for prevention and health, formerly ‘The glostrup population Studies’. Int J Epidemiol. 2011;40(3):602-602-10. doi: 10.1093/ije/dyq041. [DOI] [PubMed] [Google Scholar]
- 43.Eurostat Statistics Explained . Causes of death statistics. 2015. [Google Scholar]
- 44.Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. J Epidemiol Community Health. 2003;57(10):778–83. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Marmot M, Wilkinson R. Social Determinants of Health. 2. Oxford: Oxford University Press; 2006. The life course, the social gradient, and health. [Google Scholar]


