Abstract
To evaluate the association between body mass index (BMI: kg/m2) and mortality among Hispanic adults, we acquired 8 years (1997–2004) of National Health Interview Survey data linked to public-use mortality follow-up data through 2006. Using Cox proportional hazards regression, we fit separate models for two attained age strata (18 to <60 years, ≥60 years) adjusting for sex, smoking, and physical activity with over 38,000 analyzable respondents. We found that, among those aged ≥60 years, underweight (BMI ≤ 18.5) associated with elevated mortality (hazard ratio [HR] = 2.19; 95% confidence interval [CI], 1.38–3.46) while overweight (BMI of 25 to <30) and obesity grade 1 (BMI of 30 to <35) associated with reduced mortality (HR’s = 0.79; 95% CI, 0.65–0.95 and 0.71; 95% CI, 0.56–0.91), respectively. There were no significant associations between BMI and mortality among the 18 to <60 years attained age strata or among never smokers for either age strata. Overweight and obesity are not obviously associated with elevated mortality among Hispanic adults.
INTRODUCTION
The US Census Bureau estimates that the Hispanic population increased by 15.2 million between 2000 and 2010, accounting for more than half of the total US population increase of 27.3 million (1). Moreover, since the start of the 21st Century, the Hispanic population in the US has grown by 43%, which is four times the nation’s 9.7% growth rate and much more than the non-Hispanic white population, which grew a little over 1% over the same period (2). The US has the second largest Hispanic population in the world (2) and by 2050 Hispanic persons are projected to comprise 30% of the US population (3, 4).
The latest age-adjusted data from the National Health and Nutrition Examination Surveys (NHANES) estimates that 78.8% of Hispanic adults aged 20 years or older are overweight or obese compared to 66.7% among non-Hispanic persons (5). Similarly, male and female Hispanic children have higher odds of being overweight compared to their non-Hispanic counterparts (1.81 and 1.47, respectively) (6). The high prevalence of overweight and obesity among Hispanic persons is concerning not only because of obesity’s association with an array of adverse health conditions (e.g., heart disease, certain cancers), but also because Hispanic persons appear to be particularly vulnerable to developing metabolic syndrome, diabetes, asthma, and chronic obstructive pulmonary diseases (7–8).
Epidemiologic analyses show that obesity (i.e., body mass index [BMI: kg/m2] ≥30) associates with increased mortality in whites (e.g., 9, 10) and black women [11]. We [12] recently showed that, in a pooled analysis of multiple datasets comprising Hispanic adults, obesity did not associate with increased mortality. The present study was designed to estimate the association between BMI and all-cause mortality among Hispanic adults using nationally representative data from 8 consecutive years of the National Health Interview Survey (NHIS), comprising nearly 40,000 Hispanic adults residing in the US. Because the association of obesity with mortality may be confounded by the effects of smoking and levels of physical activity, we adjusted for these variables. We also conducted a sensitivity analysis restricted to never smokers.
METHODS AND PROCEDURES
The NHIS is an ongoing cross-sectional survey of the US civilian non-institutionalized population (13). Annually, NHIS collects data through self-report on about 100,000 individuals in 40,000 households. Typically, data is available only for a single-adult household member aged 18 years or older. Our analysis includes 8 years of combined NHIS data (1997–2004) of persons from one of seven Hispanic subgroups (i.e., Mexican, Mexican American, Central and South American, Puerto Rican, Other/Multiple Hispanic Subgroups, Cuban/Cuban American, and Dominican/Dominican American) (14). NHIS Linked Public-Use Mortality Files provide mortality follow-up data from the date of NHIS interview through December 31, 2006. Ascertainment of mortality is based primarily upon the results from a probabilistic match between NHIS and National Death Index death certificate records (15). We acquired the NHIS data through the Integrated Health and Interview Series, (16) which is funded by the National Institute of Child Health and Human Development to curate the NHIS data.
Study Variables
Predictor
BMI (kg/m2) was the predictor variable and was calculated from self-reported weight and height.
Outcome variables
Mortality information in terms of the age at death due to any cause, or the age at the last available follow-up.
Covariates
Data on sex, smoking status (never smoked, former/current smoker), physical activity (no physical activity, regular physical activity) were included as covariates in the analysis. Regular physical activity was defined as 10+ minutes of vigorous physical activity for at least 3 times a week or 10+ minutes of moderate physical activity for at least 5 times a week. Missing data were handled using listwise deletion. Observations that lacked information concerning baseline age or any pertinent covariate were removed from the analysis. We also excluded pregnant women from our analyses.
Statistical Analysis
We calculated hazard ratios (HR) for the BMI-mortality association using Cox proportional hazard (PH) regression. We treated BMI as a categorical variable, based on the federal BMI-defined body weight classifications (18): underweight (BMI of 18.5 or less), normal weight, the reference category (BMI of 18.5 to less than 25), overweight (BMI of 25 to less than 30), obesity grade 1 (BMI of 30 to less than 35), and obesity grade 2 (BMI of 35 or greater). Similar to the approach used by Flegal and colleagues (17), we used age as the time scale and estimated separate models based upon two attained age strata (18 to <60 years and ≥60 years), where attained age refers to the sum of age at entry and the available follow-up time (The choice of these attained age strata was based on visual inspection of Kaplan-Meier estimates of the survival curves for each BMI category, which suggested crossing survival curves at approximately 60 years of age). We used the counting process formulation of the Cox model to account for left truncation due to variable age at baseline. Sex, smoking status, and physical activity were included as covariates in each model. The PH assumption for each covariate was examined by correlating the respective set of scaled Schoenfeld residuals with time (19). For the ≥60 years attained age stratum, we observed evidence for deviation from PH for the effects of sex and physical activity. We therefore fit a stratified PH model with separate baseline hazard functions for each combination of sex and physical activity level (20). However, since the results from the non-stratified and stratified model were similar, we report only the non-stratified results.
We also conducted sensitivity analyses, using the approach described above, among individuals who reported being never smokers (N = 25,803) with sex and physical activity included as covariates. We excluded the underweight category from the sensitivity analysis of the never smokers of the 18 to <60 years attained age stratum since there were no deaths reported in that stratum. Data were analyzed using R statistical computing environment (version 2.13) (21), using the survey package for R (version 3.25) (22) to account for the complex sampling design of the NHIS. Statistical significance was evaluated at the 0.05 level.
RESULTS
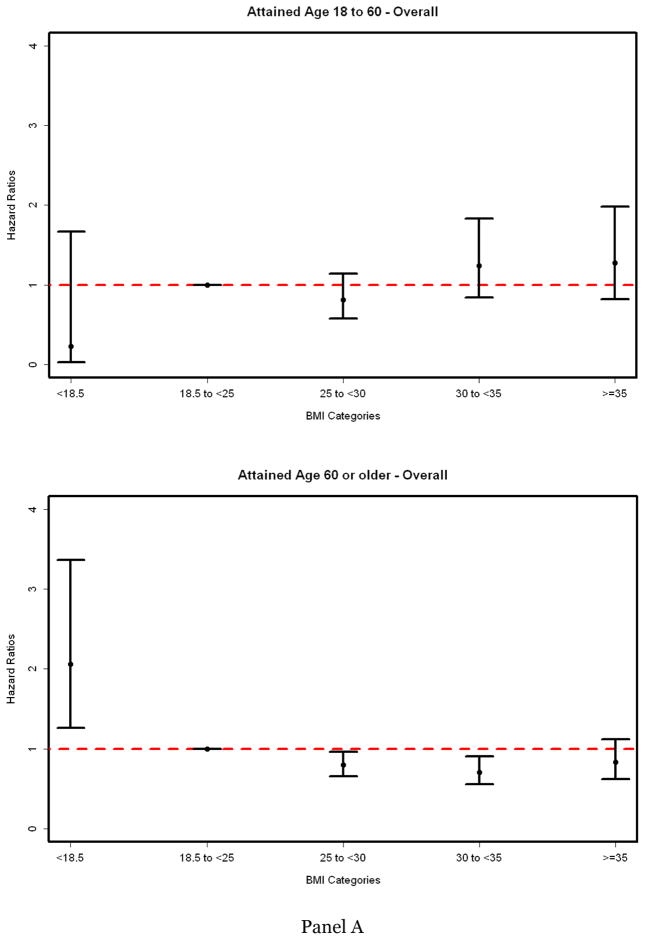
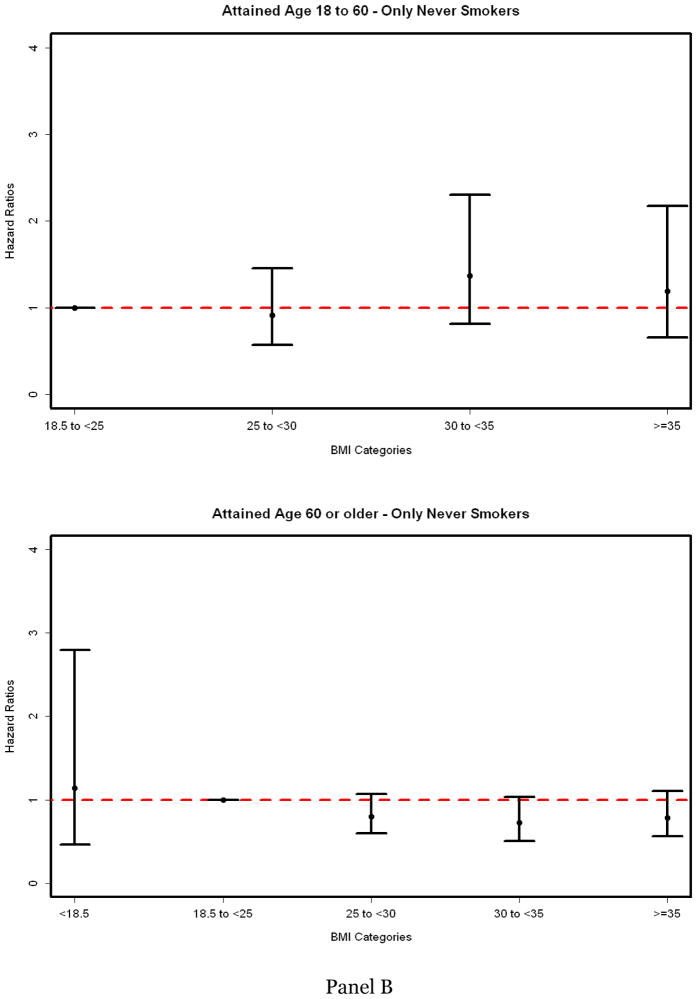
A description of the NHIS data for Hispanic respondents is shown in Table 1. Nearly 60% self-identified as Mexican or Mexican-American. There were 1,461 identified deaths through 2006 (403 in the 18 to <60 years attained age stratum and 1,058 in the ≥60 years attained age stratum). Estimated HRs by BMI category for the two attained age strata is shown in Figure 1 for the entire sample (Panel A) and for never smokers (Panel B).
Table 1.
Description of 1997–2004 National Health Interview Survey (NHIS) data for Hispanic Respondents
| CHARACTERISTIC | NHIS (1997–2004) |
|---|---|
| Sample size | 38,810 |
| Female, N (%) | 21,461 (55.3%) |
| Age, yrs | 40.9 ± 16 |
| Hispanic subgroups, N (%) | |
| Mexican | 13,032(33.6%) |
| Mexican American | 9,852 (25.4%) |
| Central/South American | 4,046 (10.4%) |
| Puerto Rican | 3,978 (10.3%) |
| Cuban/Cuban American | 2,352 (6%) |
| Dominican/Dominican American | 832 (2.1%) |
| Other/Multiple Hispanic Subgroups | 4,718 (12.2%) |
| Mean follow-up, yrs | 5.4 ± 2.3 |
| Deaths, N (%) | 1,461 (3.8%) |
| Prevalence of BMI level, % & Deaths (N) | |
| Underweight: <18.5 | 1.2% (37) |
| Normal weight: 18.5 to <25 | 33% (511) |
| Overweight: 25 to <30 | 38% (535) |
| Obesity Grade 1: 30 to <35 | 16.2% (211) |
| Obesity Grade 2: ≥35 | 11.6% (167) |
| Regular physical activity, N (%) | 10,132(26.1%) |
| Never smoker, N (%) | 25,803 (66.5%) |
Figure 1.
Hazard Ratios for Mortality (HRs) for Hispanic Respondents in the NHIS (1997–2004) by Age Group, Body Mass Index, and Among Never Smokers
In the attained age stratum of 18 to <60 years, there were no significant associations between any of the BMI categories and mortality. For the ≥60 years attained age stratum, underweight (BMI < 18.5) associated with an elevated mortality (HR = 2.19; 95% Confidence Interval [CI], 1.38–3.46), while overweight (BMI 25 to <30) and obesity grade 1 (BMI 30 to <35) associated with a reduced mortality (HR’s = 0.79; 95%CI, 0.65–0.95 and 0.71; 95%CI, 0.56–0.91), respectively. In analyses restricted to never smokers, we found no significant BMI-mortality associations in either of the attained age strata.
DISCUSSION
Using combined data on Hispanic adults from 8 consecutive years of the NHIS, we found that overweight and obesity were not associated with an increased mortality. Indeed, after adjusting for sex, smoking status, and physical activity, we found that overweight and obesity grade 1 were associated with decreased mortality among those in the ≥60 years attained age stratum. By contrast, underweight was associated with increased mortality among this age group. Among the 18 to <60 attained age stratum, underweight, overweight, and obesity did not associate with mortality. When we restricted the analysis to never smokers, we found no statistically significant associations between BMI and mortality in either of the attained age strata. However, it is important to note that, in the ≥60 years attained age stratum, both the point and interval estimates for overweight and grade 1 obese in never smokers overlapped with that of the overall sample. The lack of statistical significance in the analysis of never smokers could be due to reduced statistical power.
Similar findings (i.e., underweight associated with increased mortality and overweight and obesity associated with decreased mortality) have been obtained by other investigators studying older populations (e.g., 23). The association between underweight and mortality is also consistent with a vast number of BMI-mortality studies (e.g., 9–11, 24, 25). While a potential for confounding due to occult disease is possible, we chose not to omit early deaths or individuals with recent weight loss or pre-existing health conditions from our analyses. Several methodological papers, presenting evidence based on mathematical proof, computer simulation, and meta-analysis (e.g., 25–27), as well as large and well-conducted analyses (e.g., 28) have consistently shown that such measures, as well as adjusting for pre-existing health conditions, do not account for the elevated BMI-mortality association observed among the underweight (and invariably lead to a reduction in statistical power). The absence of associations between underweight and obesity with mortality among the younger age groups, however, is a finding that appears to be unique to Hispanic adults.
The pattern of results obtained among Hispanic adults is at odds with those typically found in non-Hispanic white and African American samples (e.g., 9–11). Specifically, white and African-American samples generally produce a J or U-shaped BMI-mortality association with elevated mortality in the lower and upper tails of the BMI distribution, with the lowest mortality in BMIs of 20 to about 25. However, at least one recent analysis, derived from data on over 1 million Asian adults (28), found, consistent with our current findings among Hispanic adults, no elevated mortality with higher BMIs among Indians and Bangladeshis.
Although seemingly paradoxical, our results may relate to the findings of numerous studies (e.g., 29) which show a Hispanic mortality advantage. This has been referred to as the “Hispanic Paradox” and methodological factors such as racial and ethnic misclassification on death certificates or migration and cultural effects are unable to account for the findings (e.g., 30). A recent study (31) suggests that a lower prevalence of smoking may help to explain Hispanic persons’ longevity advantage. While our results do not refute the role smoking may play in explaining the Hispanic paradox, it appears that other factors render obesity less deleterious, with respect to its association to mortality, than is commonly observed among white samples.
This study has several strengths including: the use of multiple years of NHIS data which contained large numbers of Hispanic respondents, the use of attained age and stratification to account for confounding and for effect modification by age, adjustment for sex, smoking status, and physical activity, and a supplementary analysis restricted to never smokers. The primary limitation of the study is that BMI was derived from self-reported weight and height. It has been shown that self-reported BMI can introduce bias which may account for discrepancies when compared to estimates derived from measured BMI (32). Nonetheless, the present results are consistent with those obtained using BMI calculated from measured weight and height (12). Another limitation is the relatively short duration of mortality follow-up (mean of 5.4 years). However, the results obtained herein are consistent with those previously published by our group (12) where the mean duration of follow-up was nearly 13 years. This suggests that the relatively short follow-up duration may not have markedly influenced the observed associations. Of course an additional limitation of this and all observational studies is that they show associations (or lack thereof) which may not necessarily indicate causation (or lack of causation).
In sum, our analyses suggest that there was no evidence that overweight and obesity associates with elevated mortality among Hispanic adults. This is an intriguing finding given that Hispanic persons have higher rates of obesity and diabetes compared to non-Hispanic whites. It appears, therefore, that, in contrast to samples of whites and African-American persons, overweight and obesity may impose a lesser, if any, morality burden upon Hispanic persons. The reasons for this are unclear and merit further investigation. In particular, given the high rates of conditions such as metabolic syndrome and pulmonary disease seen in Hispanic adults, it may be worthwhile to assess whether BMI associates with specific causes of death. To do so, however, would require a large, well-characterized prospective cohort of Hispanic adults to provide adequate statistical power to conduct cause-specific mortality analyses.
Acknowledgments
This project was supported in part by NIH grants: R21DK077959, P30DK056336, and T32HL072757.
Footnotes
DISCLOSURE
TM has no potential conflicts to disclose. RM has no potential conflicts to disclose. NMP has no potential conflicts to disclose. SWK has no potential conflicts to disclose. DBA has, anticipates, or has had financial interests with the Frontiers Foundation; Vivus, Inc; Kraft Foods; University of Wisconsin; University of Arizona; Paul, Weiss, Wharton & Garrison LLP; and Sage Publications. CJC has no potential conflicts to disclose. KRF has no potential conflicts to disclose.
References
- 1.Ennis SR, Rios-Vargas M, Albert NG. The Hispanic Population: 2010. U.S. Census Bureau; May 26, 2011. [Accessed August 18, 2011]. Web page. http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf. [Google Scholar]
- 2.Humes KR, Jones NA, Ramirez RR. [Accessed August 18, 2011.];Overview of Race and Hispanic Origin 2010: US Census Bureau. 2011 Mar 23; Web page. http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf.
- 3.Arias E. United States life tables by Hispanic origin. National Center for Health Statistics. Vital Health Stat. 2010;2:152. [PubMed] [Google Scholar]
- 4.Population division, US Census Bureau. Annual estimates of the population by sex, race and Hispanic or Latino origin for the United States: April 1, 2000 – July 1, 2004 (NC-EST2004-03) 2005. [Google Scholar]
- 5.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93 (11 Suppl 1):S9–30. doi: 10.1210/jc.2008-1595. [DOI] [PubMed] [Google Scholar]
- 8.CDC. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2003. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2004. Rev. [Google Scholar]
- 9.Berrington de Gonzalez AB, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1. 46 million white adults. N Eng J Med. 2010;363:2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900,000 adults: collaborative analysis of 57 prospective studies. Lancet. 2009;373:362–369. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boggs DA, Rosenberg L, Cozier YC, Wise LA, Coogan PF, Ruiz-Narvaez EA, Palmer JR. General and abdominal obesity and risk of death among black women. N Engl J Med. 2011;365:901–908. doi: 10.1056/NEJMoa1104119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fontaine KR, McCubrey R, Mehta T, Pajewski NM, Keith SW, Bangalore SS, Crespo CJ, Allison DB. Body Mass Index and Mortality Rate among Hispanic Adults: A Pooled Analysis of Multiple Epidemiologic Datasets. Int J Obes (Lond) 2011 doi: 10.1038/ijo.2011.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kovar MG, Poe GS National Health Interview Survey. National Health Interview Survey Design, 1973–84, and Procedures, 1975–83. 1985. Aug, p. 135. (PHS) 85-1320. PB87-148094. PC A07 MF A02. [PubMed] [Google Scholar]
- 14.Botman SL, Jack SS. Combining National Health Interview Survey Datasets: Issues and Approaches. Stat Med. 1995;14:669–77. doi: 10.1002/sim.4780140523. [DOI] [PubMed] [Google Scholar]
- 15.Ingram DD, Lochner KA, Cox CS. Mortality experience of the 1986–2000 National Health Interview Survey linked mortality files participants. National Center for Health Statistics. Vital Health Stat. 2008;2:147. [PubMed] [Google Scholar]
- 16.Johnson PJ, Blewett LA, Ruggles S, Davern ME, King ML. Four decades of population health data: the integrated health interview series as an epidemiologic resource. Epidemiol. 2008;19:872–875. doi: 10.1097/EDE.0b013e318187a7c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flegal K, Graubard B, Williamson D, Gail M. Impact of smoking and preexisting illness on estimates of the fractions of deaths associated with underweight, overweight, and obesity in the US population. Am J Epidemiol. 2007;166:975–982. doi: 10.1093/aje/kwm152. [DOI] [PubMed] [Google Scholar]
- 18.National Heart, Lung, and Blood Institute. [Accessed August 25, 2010.];Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults Web page. http://www.nhlbi.nih.gov/guidelines/obesity.
- 19.Grambsch P, Therneau T. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. [Google Scholar]
- 20.Klein P, Moeschberger ML. Survival analysis: techniques for censored and truncated data. 2. New York, NY: Springer; p. 309. [Google Scholar]
- 21.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2010. http://R-project.org. [Google Scholar]
- 22.Lumley T. Analysis of complex survey samples. J Stat Software. 2004;9:1–19. [Google Scholar]
- 23.Chapman IM. Obesity paradox during aging. Interdiscip Top Gerontol. 2010;37:20–36. doi: 10.1159/000319992. [DOI] [PubMed] [Google Scholar]
- 24.Calle EE, Teras LR, Thun MJ. Obesity and mortality. NEJM. 2005;353:2197–2199. doi: 10.1056/NEJM200511173532020. [DOI] [PubMed] [Google Scholar]
- 25.Allison DB, Faith MS, Heo M, et al. Hypothesis concerning the U-shaped relation between body mass index and mortality. Am J Epidemiol. 1997;146:339–349. doi: 10.1093/oxfordjournals.aje.a009275. [DOI] [PubMed] [Google Scholar]
- 26.Allison DB, Heo M, Flanders DW, Faith MS, Williamson DF. Examination of “early mortality exclusion” as an approach to control for confounding by occult disease in epidemiologic studies of mortality risk factors. Am J Epidemiol. 1997;146:672–680. doi: 10.1093/oxfordjournals.aje.a009334. [DOI] [PubMed] [Google Scholar]
- 27.Allison DB, Faith MS, Heo M, Townsend-Butterworth D, Williamson DF. Meta-analysis of the effect of excluding early deaths on the estimated relationship between body mass index and mortality. Obes Res. 1999;4:342–54. doi: 10.1002/j.1550-8528.1999.tb00417.x. [DOI] [PubMed] [Google Scholar]
- 28.Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K. Association between Body-mass index and risk of death in over one million Asians. N Engl J Med. 2011;364:719–729. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Turra CM, Elo IT. The impact of salmon bias on the Hispanic mortality advantage: New evidence from social security data. Popul Res Policy Rev. 2008;27:515–530. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arias E, Eschbach K, Schauman WS, Backlund EL, Sorlie PD. The Hispanic mortality advantage and ethnic misclassification on US death certificates. Am J Public Health. 2010;100:S171–177. doi: 10.2105/AJPH.2008.135863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blue L, Fenelon A. Explaining low mortality among US immigrants relative to native-born Americans: the role of smoking. Int J Epidemiol. 2011;40:786–793. doi: 10.1093/ije/dyr011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keith SW, Fontaine KR, Pajewski NM, Mehta T, Allison DB. Use of self-reported height and weight biases the body mass index-mortality association. Int J Obese. 2011;35:401–408. doi: 10.1038/ijo.2010.148. [DOI] [PMC free article] [PubMed] [Google Scholar]