Abstract
Administrative data are commonly used to evaluate total joint arthroplasty, but analyses have historically been limited by the inability to capture which conditions were present-on-admission (POA). In 2007 Medicare began allowing hospitals to submit POA information. We used Medicare Part A data from 2008-2009 to examine POA coding for three common complications (pulmonary embolism [PE], hemorrhage/hematoma, and infection) for primary and revision total knee arthroplasty (TKA). POA information was complete for 60%-75% of complications. There was no evidence that higher TKA volume hospitals or major teaching hospitals were more likely to accurately code POA data. The percentage of complications coded as POA ranged from 6.4% (PE during index admission for primary TKA) to 68.8% (infection during index admission for revision TKA). Early experience suggests that POA coding can significantly enhance the value of Medicare data for evaluating TKA outcomes.
Introduction
Administrative data derived from physician and hospital insurance claims are now routinely used to evaluate hospital performance. The strengths and limitations of administrative data are well known.1,2 While clinical diagnosis-specific registries provide greater detail in most circumstances, evidence is accumulating that, when analyzed carefully, administrative data can provide accurate information that approximates what is found on medical record review.3,4 Since nationwide clinical registries in the United States (US) currently exist for only a few select diagnoses/procedures and are extremely costly and labor intensive to develop,5-8 administrative data continue to serve as the mainstay of hospital quality reporting and health services research. In the case of total knee arthroplasty (TKA) because multi-center clinical registries are not widely available, Medicare administrative data is commonly used to evaluate complications and readmission rates.9-11 It is highly likely that public reporting of hospital TKA outcomes in the US will be introduced by the Centers for Medicare and Medicaid Services (CMS) using Medicare administrative data in the near future.4
One of the major historical limitations in using administrative data to evaluate hospital TKA performance has been the inability to differentiate comorbid conditions from complications.12 For example, in the case of revision TKA it has been difficult (if not impossible) to accurately determine whether a post-operative infection was present-on-admission (POA) (i.e., the infection was the indication for the revision) or whether the infection represented a complication of the revision procedure.13 In an effort to improve the utility of Medicare administrative data for both research and hospital quality measurement, CMS introduced codes in October, 2007 to allow hospitals to report whether specific conditions were POA.14 Providing POA information to CMS offers hospitals an opportunity to substantially enhance the accuracy of complication-rate data collected by Medicare. At the same time, providing accurate POA data might require modest investments of time and effort on behalf of hospital staff and physicians engaged in coding and documentation. While POA data have been collected by CMS and coded in Medicare administrative data since 2007, to the best of our knowledge there are no studies that have examined how these codes are being used in orthopaedic surgery.
The overarching objective of our study was to evaluate early experience with POA coding for complications related to primary and revision TKA. In particular, we wanted to understand the proportion of hospitals using POA codes when reporting TKA complications to Medicare and whether there were differences between hospitals that were and were not reporting POA data to CMS. We hypothesized that higher volume hospitals and major teaching hospitals would be more likely to consistently report POA information to CMS, reflecting the fact that these hospitals would have the size, financial resources, and surgical volumes to justify the investment in collecting these codes. We also set out to explore how POA codes might impact three common complications (pulmonary embolism [PE], post-operative bleeding, and infection) that are of interest to hospitals, physician, and policy makers. We hypothesized that POA coding would be particularly important for infection related to revision TKA procedures where the POA codes would allow for differentiation between revision surgery performed for infection (i.e., infection was POA) versus infection developing as a true complication of the revision procedure (i.e., infection not POA, but developed post-operatively).
Methods
Data
We used Medicare Provider Analysis and Review (MedPAR) Part A data files from 2007-2009 containing a 100% sample of hospitalizations for fee-for-service beneficiaries to identify all enrollees age 65 years and older who underwent primary or revision TKA. Patients were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD9-CM) procedure codes (81.54 for primary and 80.06, 81.55, 00.80, 00.81, 00.82, 00.83, 00.84 for revision TKA).3,15-17 The Part A files contain a range of data collected from discharge abstracts for all hospitalized fee-for-service Medicare enrollees including: patient demographics; ICD9-CM codes for primary and secondary diagnoses and procedures; admission source (e.g., emergency department or transfer from outside hospital); admission and discharge dates; each patient’s unique Medicare beneficiary number allowing for identification of patient readmissions; and each hospital’s unique six digit identification number. Comorbid illnesses present at the time of admission were identified using algorithms described by Elixhauser et al.18,19 which consider 30 specific conditions and exclude comorbid conditions that may represent complications of care or that are related to the primary reason for hospitalization. We also determined the number of comorbid conditions for each patient and then calculated the mean number of comorbid conditions across different groups. As these comorbidity algorithms were developed prior to the integration of POA codes into Medicare data, the Elixhauser coding schemes do not attempt to differentiate comorbidities that were or were not POA. Since 2008 Medicare Part A data collection has allowed for submission of POA fields for each primary and secondary diagnosis and procedure.14 For each diagnosis and procedure, POA codes can either be entered directly by the physician (or their delegate) into an electronic health record that also collects billing information or POA codes can be abstracted from the medical record and submitted separately by coding/billing staff. For each diagnosis and procedure, the POA indicator is assigned one of the following values:
| Y = Condition present at the time of inpatient admission. |
| N = Condition not present at the time of inpatient admission. |
| U = Documentation is insufficient to determine if condition was present on admission. |
| W = Provider is unable to clinically determine whether condition was present on admission or not. |
| 1 = Unreported/not used -- exempt from POA reporting -- this code is the equivalent code of a blank, however, it was determined that blanks were undesirable when submitting the data. |
| Z = Denotes the end of the POA indicators |
| X = Denotes the end of the POA indicators in special data processing situations that may be identified by CMS in the future. |
In order to generate appropriate analytical cohorts we applied several inclusion and exclusion criteria for our analyses (See Appendices A and B); criteria were different for the primary and revision TKA cohorts reflecting underlying differences in the indications for these procedures. First, we excluded Medicare HMO enrollees from both the primary and revision TKA cohorts as the MedPAR data is incomplete for enrollees in such plans. Second, we limited our cohort to the first primary (or revision) TKA performed on a given patient during any 1-year period using methods we have described previously to avoid including staged procedures performed in close temporal proximity; data from 2007 was needed to allow us to implement the 1-year “look back.”20 Third, as primary TKA is most often an elective procedure while revision TKA can be either an elective or more urgent procedure, we applied separate exclusion criteria to the primary and revision TKA populations in accordance with prior studies as described below. For primary TKA, we sequentially excluded patients admitted through the emergency department (N=2993), and patients admitted after transfer from another acute-care hospital (N=374); these exclusion criteria were developed to select a population of primary elective TKA patients. Our revision TKA population did not exclude these types of patients because revision TKA can be an emergent or unscheduled procedure and thus exclusion of these populations would not make sense. The MedPAR data was merged with hospital-level data obtained from the 2009 American Hospital Association Annual Survey for variables including hospital bed-size, for-profit/not-for-profit status, and hospital teaching status.
Statistical Analysis
Our overarching objective was to examine how hospitals are using POA codes and how POA coding is being used with respect to selected complications after primary and revision TKA. We focused on three complication rates that we and others have studied previously using administrative data and that are a focus for the US Medicare program4: 1) pulmonary embolism; 2) infection; and 3) hemorrhage/hematoma. Codes used to identify these complications were based upon prior analyses that we and others have used previously and are included in Appendix C.3,21,22 All analyses were conducted separately for the primary and revision TKA cohorts.
First, we compared the demographic characteristics and prevalence of selected comorbidities for patients who did and did not experience complications. We stratified the primary TKA cohort into three groups: 1) patients who experienced no complication; 2) patients who experienced one-or-more complications during the index hospital stay; and 3) patients who were discharged alive without complications during the index hospital stay, but subsequently experienced one-or-more complications during readmission within 90-days of surgery. We then compared demographics and comorbid illnesses among these three groups using analysis of variance for comparisons of continuous variables and the chi-squared test for categorical variables. Analogous analyses were conducted for the revision TKA population.
Second, we set out to examine whether there were differences in hospitals that did and did not regularly use POA codes. For purposes of these analyses we analyzed all primary and revision TKA cases performed in a given hospital in aggregate to maximize sample size. For each hospital we calculated the total number of TKA cases experiencing one-or-more complications during either the index admission or readmission occurring within 90-days of surgery. We calculated the percentage of cases experiencing complications at each hospital for which POA coding was complete. Since POA codes have only been recently introduced and there are few published papers defining how best to use these codes, we relied upon a common sense approach in our study; coding was deemed complete for a given patient if the POA fields for primary or secondary diagnoses were coded as Y, N, U or W. Conversely, POA fields that were coded as 1, Z or X were considered incomplete. Thus a hospital with 10 TKA complications of which five had completed POA coding, this hospital would have had a POA coding completeness of 50% (5-of-10 complications).
We reviewed the distribution of POA coding completeness across all hospitals and then stratified hospitals into three groups: 1) hospitals reporting valid POA codes for ≤25% of complication cases; 2) hospitals reporting valid POA codes for >75% of complication cases; and 3) all other hospitals (i.e., those reporting valid POA codes for 26%-75% of complication cases). We used bivariate methods to compare the characteristics of hospitals with low, intermediate, and high POA coding percentages. In particular, we examined hospital bed-size, teaching status, geographic region, governance status (for-profit, not-for-profit), and Medicare disproportionate share (DSH) payment on TKA cases; DSH payments reflect supplemental payments that CMS makes to hospitals that provide a particularly large proportion of care to lower income patients (i.e., Medicaid eligible patients). For Medicare DSH payment, we grouped hospitals into 1) zero DSH hospitals if a hospital did not receive any DSH payments, 2) low DSH hospitals if a hospital’s DSH payment was less than the median DSH payment of all hospitals receiving DSH payment, and 3) high DSH hospitals otherwise using a method that we have described previously.23
Third, we examined the impact of POA coding on our three selected complications (pulmonary embolism [PE]; hemorrhage; and infection). Analyses were conducted separately for primary and revision TKA. We began by stratifying complications into those that occurred during the index admission and those that occurred on readmission. Next, for each complication we examined the percentage of the total number of complications that were coded as present on admission (Y), not present on admission (N), other values (U, W) and for which data was missing (1, Z, X).
All p-values are 2-tailed, with p-values less 0.05 deemed statistically significant. All statistical analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC). This project was approved by the University of Iowa Institutional Review Board.
Results
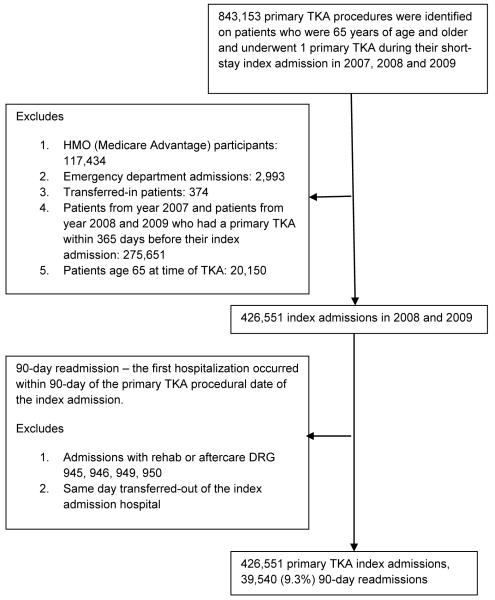
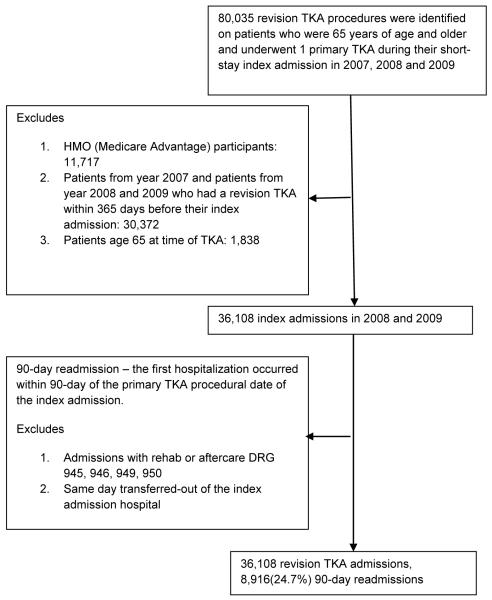
Our study cohort consisted of 426,551 Medicare enrollees who underwent primary TKA and 36,108 who underwent revision TKA in 2008-2009 (Appendix A and B). Among the primary TKA cohort, 6,202 patients (1.5%) had a code for one-or-more of our three conditions (PE, hemorrhage, or infection) during the index hospital stay and an additional 5,165 (1.2%) had such a code on a subsequent readmission within 90-days of surgery (Table 1). Among the revision TKA cohort, 8,955 patients (24.8%) had a code for one-or-more of our three conditions (PE, hemorrhage, or infection) during the index hospital stay and an additional 877 (2.4%) had such a code on a subsequent readmission within 90-days of surgery (Table 2). Primary TKA patients with complications (on either the index admission or readmission) tended to be slightly older, were less likely to be female, were less likely to be white and more likely to be black than patients who did not experience a complication (Table 1). Patients experiencing complications after primary TKA had a greater burden of comorbid illness as measured by the mean number of comorbid conditions (Table 1). Findings were generally similar with respect to demographics and comorbidity for the revision TKA patients (Table 2).
Table 1.
Characteristics of Primary TKA patients
| All Patients (N = 426551) |
No Complication (N = 415184) |
In-hospital Complication (N = 6202) |
90-day Readmission Complication (N = 5165) |
P-value* | |
|---|---|---|---|---|---|
| Age, mean (SD) | 74.5 (6.0) | 74.5 (6.0) | 74.9 (6.0) | 75.1 (6.1) | <0.0001 |
| Sex, women (%) | 274601 (64.4) | 267708(64.5) | 3840 (61.9) | 3053 (59.1) | 0.0001 |
| Race, number (%) | |||||
| White | 388113 (91.0) | 378027 (91.1) | 5493 (88.6) | 4593 (88.9) | <0.0001 |
| Black | 22471 (5.3) | 21678 (5.2) | 428 (6.9) | 365 (7.1) | <0.0001 |
| Other | 14818 (3.5) | 14355 (3.5) | 264 (4.3) | 199 (3.9) | 0.0010 |
| Missing | 1149 (0.3) | 1124 (0.3) | 17 (0.3) | 8 (0.2) | 0.2790 |
| Comorbidity, number (%) |
|||||
| Diabetes | 91400 (21.4) | 89003 (21.4) | 1245 (20.1) | 1152 (22.3) | 0.0104 |
| CHF | 16322 (3.8) | 15643 (3.8) | 379 (6.1) | 300 (5.8) | <0.0001 |
| Obesity | 47686 (11.2) | 46445 (11.2) | 565 (9.1) | 676 (13.1) | <0.0001 |
| Renal failure | 16509 (3.9) | 16030 (3.9) | 242 (3.9) | 237 (4.6) | 0.0263 |
| Number of comorbid conditions, mean (SD) |
2.1 (1.4) | 2.1 (1.4) | 2.6 (1.4) | 2.3 (1.5) | <0.0001 |
P-values compare differences among no-complication, in-hospital complication, and 90-day readmission complication groups
Patients who died in-hospital would not contribute to the 90-day readmission complication group numerator or denominator (575 patients died in-hospital)
Patients who experienced both an in-hospital and readmission complication were counted only in the in-hospital complication group.
Table 2.
Characteristics of Revision TKA patients
| All Patients (N = 36108) |
No Complication (N = 26276) |
In-hospital Complication (N = 8955) |
90-day Readmission Complication (N = 877) |
P-value* | |
|---|---|---|---|---|---|
| Age, mean (SD) | 75.3 (6.4) | 75.3 (6.4) | 75.5 (6.5) | 75.6 (6.6) | 0.0118 |
| Sex, women (%) | 21644 (59.9) | 16565 (63.0) | 4605 (51.4) | 474 (54.1) | <0.0001 |
| Race, number (%) | |||||
| White | 32334 (89.6) | 23524 (89.5) | 8030 (89.7) | 780 (88.9) | 0.7774 |
| Black | 2650 (7.3) | 1976 (7.5) | 602 (6.7) | 72 (8.2) | 0.0266 |
| Other | 1022 (2.8) | 699 (2.7) | 301 (3.4) | 22 (2.5) | 0.0022 |
| Missing | 102 (0.3) | 77 (0.3) | 22 (0.3) | 3 (0.3) | 0.7242 |
| Comorbidity, number (%) |
|||||
| Diabetes | 8434 (23.4) | 6018 (22.9) | 2199 (24.6) | 217 (24.7) | 0.0038 |
| CHF | 2492 (6.9) | 1455 (5.5) | 970 (10.8) | 67 (7.6) | <0.0001 |
| Obesity | 3677 (10.2) | 2784 (10.6) | 795 (8.9) | 98 (11.2) | <0.0001 |
| Renal failure | 1791 (5.0) | 1122 (4.3) | 624 (7.0) | 45 (5.1) | <0.0001 |
| Number of comorbid conditions, mean (SD) |
2.2 (1.4) | 2.2 (1.4) | 2.4 (1.4) | 2.3 (1.4) | <0.0001 |
P-values compare differences among no-complication, in-hospital complication, and 90-day readmission complication groups
Patients who died in-hospital would not contribute to the 90-day readmission complication group numerator or denominator (172 patients died in-hospital)
Patients who experienced both an in-hospital and readmission complication were counted only in the in-hospital complication group.
Hospitals that consistently submitted POA information to CMS (>75% of cases) did not appear to differ in substantive ways from hospitals that did not submit POA information (≤25% of cases)(Table 3). In particular, hospitals TKA volume, teaching status, for-profit/not-for-profit status, and poverty socioeconomic status of the patient population served (DSH payments) did not appear to be associated with more consistent or less consistent submission of valid POA codes to Medicare. We examined the characteristics of hospitals that provided valid POA codes for all (i.e., 100%) of their cases with complications. We found that the mean bed size of these hospitals was 89.9, 3.7% were major teaching hospitals, 24.0% were for-profit (59.4% not-for-profit, 16.6% government owned), and mean TKA volume was 70.6.
Table 3.
Characteristics of hospitals stratified by their use of POA indicator
| All TKA Hospitals (N = 2617) |
Hospitals with Valid POA Indicator for ≤ 25% TKA Cases with Complications (N = 709) |
Hospitals with Valid POA Indicator for 26%-75% of TKA Cases with Complications (N = 1254) |
Hospitals with Valid POA Indicator for > 75% TKA Cases with Complications (N = 654) |
P-value** | |
|---|---|---|---|---|---|
| TKA Volume, mean (SD) |
175.6 (200.2) | 122.9 (136.5) | 252.5 (215.8) | 80.1 (163.7) | <0.0001 |
| Complication Volume, mean (SD) |
9.0 (10.3) | 5.6 (6.5) | 14.0 (11.4) | 3.1 (5.9) | <0.0001 |
| Beds, mean (SD) | 137.7 (114.3) | 109.6 (87.9) | 174.2 (129.9) | 91.0 (70.3) | <0.0001 |
| Teaching Status, number (%) |
|||||
| Major | 252 (9.6) | 52 (7.3) | 174 (13.9) | 26 (4.0) | <0.0001 |
| Minor | 440 (16.8) | 84 (11.9) | 285 (22.7) | 71 (10.9) | |
| Non-Teaching | 1925 (73.6) | 573 (80.8) | 795 (63.4) | 557 (85.2) | |
| Geographic Region, number (%) |
|||||
| Midwest | 639 (25.1) | 161 (23.4) | 337 (27.1) | 141 (22.8) | 0.0002 |
| Northeast | 427 (16.7) | 105 (15.3) | 203 (16.3) | 119 (19.2) | |
| South | 997 (39.1) | 312 (45.4) | 468 (37.6) | 217 (35.1) | |
| West | 488 (19.1) | 109 (15.9) | 237 (19.0) | 142 (22.9) | |
| Governance, number (%) |
|||||
| For profit | 500 (19.1) | 153 (21.6) | 191 (15.2) | 156 (23.9) | <0.0001 |
| Government, non-federal |
378 (14.4) | 122 (17.2) | 148 (11.8) | 108 (16.5) | |
| Not for profit | 1739 (66.5) | 434 (61.2) | 915 (73.0) | 390 (59.6) | |
| DSH Status (%) | |||||
| High DSH | 1097 (41.9) | 310 (43.7) | 518 (41.3) | 269 (41.1) | 0.1971 |
| Low DSH | 970 (37.1) | 237 (33.4) | 485 (38.7) | 248 (37.9) | |
| Zero DSH | 550 (21.0) | 162 (22.9) | 251 (20.0) | 137 (21.0) | |
For primary TKA the coding of POA during the index admission was incomplete for approximately 33% of complications (Table 4A). For primary TKA we found that 46.9% of surgical site infections during the index admission were coded as POA, while not surprisingly the percentage of PEs and surgical site bleeding that were POA were much lower (6.4% and 9.4% respectively). Viewed from an alternative perspective, 57.8% of PEs, 52.6% of surgical site bleeding, and 19.1% of surgical site infections were coded as not POA; these would like represent true in-hospital complications. Looking at primary TKA complications identified during readmission within 90-days of surgery (Table 4B), our findings suggest that a much higher percentage of complications were POA when compared to complications identified on the index admission.
Table 4A.
Coding of Present-on-Admission (POA) indicator for primary TKA complications during index admission
| Total Patients at the Index Admission (N = 426551) | |||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Number of patients experiencing complication |
POA= Yes | POA= No | POA= Other | POA=Missing | |
| PE, number (%) | 2252 (0.5) | 144 (6.4) | 1302 (57.8) | 7 (0.3) | 799 (35.5) |
| Hemorrhage/Hematoma, number (%) |
3787 (0.9) | 356 (9.4) | 1993 (52.6) | 9 (0.2) | 1429 (37.7) |
| Infection, number (%) | 241 (0.1) | 113 (46.9) | 46 (19.1) | 0 | 82 (34.0) |
Table 4B.
Coding of Present-on-Admission (POA) indicator for primary TKA complications at readmission
| Total Patients eligible for 90-day Readmission (N = 425976) | |||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Number of patients experiencing complication |
POA= Yes | POA= No | POA= Other | POA=Missing | |
| PE, number (%) | 1848 (00.4) | 1183 (64.0) | 55 (3.0) | 3 (0.2) | 607 (32.9) |
| Hemorrhage/Hematoma, number (%) |
1630 (00.4) | 715 (43.9) | 126 (7.7) | 0 | 789 (48.4) |
| Infection, number (%) | 2163 (00.5) | 1442 (66.7) | 19 (0.9) | 3 (0.1) | 699 (32.3) |
Note:
The denominator used to calculate percentage in column A was N
The denominator used to calculate percentage in column B, C, D and E was the number found in column A in the same row.
The difference in the number of patients (“N”) between Table 4A and 4B reflect in-487 hospital deaths (575) that occurred during index admission.
Looking at complications identified on the index admission for revision TKA (Table 5A), our results looked somewhat different. In particular, we found that 23.1% of revision TKA cases were coded as having infection and 68.8% of these infections were POA. Viewed from a different perspective, only 2.0% of revision TKA surgical site infections identified at the index hospital admission were definitively coded as not POA; this suggests that the vast majority of revision TKA infections are POA and likely not “hospital acquired.” Interestingly, approximately 17% of both PEs and surgical site bleeding episodes were coded as POA for the index hospital admission which is somewhat higher than might be envisioned based upon clinical experience (Table 5A). Results focusing on readmissions after revision TKA found higher percentages of all three complications to be POA, particularly for PE and bleeding (Table 5B).
Table 5A.
Coding of Present-on-Admission (POA) indicator for revision TKA complications during index admission
| Total Patients at the Index Admission (N = 36108) | |||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Number of patients experiencing complication |
POA= Yes | POA= No | POA= Other | POA=Missing | |
| PE, number (%) | 163 (0.5) | 28 (17.2) | 85 (52.2) | 0 | 50 (30.7) |
| Hemorrhage/Hematoma, number (%) |
764 (2.1) | 136 (17.8) | 289 (37.8) | 0 | 339 (44.4) |
| Infection, number (%) | 8377 (23.2) | 5763 (68.8) |
165 (2.0) | 4 (0.1) | 2445 (29.2) |
Table 5B.
Coding of Present-on-Admission (POA) indicator for revision TKA complications during 90-day readmission
| Total Patients eligible for 90-day Readmission (N = 35936) | |||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Number of patients experiencing complication |
POA= Yes | POA= No | POA= Other |
POA=Missing | |
| PE, number (%) | 157 (00.4) | 102 (65.0) | 11 (7.0) | 0 | 44 (28.0) |
| Hemorrhage/Hematoma, number (%) |
397 (11.1) | 150 (37.8) | 65 (16.4) | 0 | 182 (45.8) |
| Infection, number (%) | 2592 (77.2) | 1760 (67.9) |
26 (1.0) | 2 (0.1) | 804 (31.0) |
Note:
The denominator used to calculate percentage in column A was N
The denominator used to calculate percentage in column B, C, D and E was the number found in column A in the same row.
The difference in the number of patients (“N”) between Table 4A and 4B reflect in-502 hospital deaths (172) that occurred during index admission.
Discussion
In an analysis of Medicare administrative data we explored early experience with POA coding for select complications (PE, bleeding, infection) after primary and revision TKA. We found a number of important findings. First, in contrast to our expectation, we found no evidence that specific groups of hospitals (e.g., high volume TKA programs, major teaching hospitals) were more likely to submit valid POA information; this is important since submission of POA codes is likely to require investment of time and energy on behalf of hospitals. Second, we found that during the first two-years after POA introduction approximately 30%-50% of complications lacked valid POA codes suggesting that at an individual patient-level, hospitals are missing opportunities to provide important information to CMS that can help in accurately evaluating quality. Third, we found that the POA indicators appeared to add significant information particularly for surgical site infections for both primary and revision TKA. In sum, this analysis provides important information about how POA indicators are being used and opportunities for improvement.
Several of our findings warrant discussion. First, our finding that the use of POA codes did not appear to vary across different groups of hospitals is important and reassuring. There has long been concern that certain groups of hospitals including safety net hospitals or smaller hospitals could be at a disadvantage when it comes to quality improvement or data reporting.24,25 In particular, there have been concerns that hospital under greatest financial pressure might lack the resources or staff expertise to improve quality or train staff in reporting complex coding to Medicare. Our results provide a modicum of reassurance since we found no evidence that any single group of hospitals was consistently better (or worse) at reporting POA data.
Second, we found that many patients experiencing complications associated with TKA did not have POA data coded during the early year after these codes were introduced. We found that anywhere from 30%-45% of complications lacked useful POA data. POA coding seemed to be missing more often for bleeding complications than for either PE or surgical site infections which raises interesting questions about why POA coding seemed to vary between the various types of complications. It is possible that missing POA codes might reflect a lack of awareness of the importance and availability of POA codes among physicians, administrators, or coders; it also seems possible that submission of new codes could be delayed while electronic bill submission software is adapted and updated. As our analysis focused on the first two years after POA introduction, it will be important to examine whether submission of POA data increases over time. Irrespective of the underlying cause for not coding, it would generally behoove hospitals to provide this information in most cases. One potentially troubling possibility would be that hospitals would intentionally omit reporting POA information to avoid having to report that a specific complication (e.g., PE) was not POA but instead a true surgical complication.
It is also important to discuss our project in the context of prior studies evaluating POA indicators in administrative data. A number of prior studies have examined the potential impact of POA coding on hospital complication rates.12,26-30 In an important study Glance et al. used administrative data from California to examine the impact of POA coding for 13 common diagnoses. The investigators found that POA coding could significantly alter a given hospital’s quality ranking, but they did not specifically evaluate variation in POA coding across hospitals or for specific complications (e.g., PE, infection). Khanna and White performed an important analysis comparing the agreement between POA coding for venous thromboembolism (VTE) in hospital administrative (billing) data with the gold standard of clinical chart review in a sample of hospitalized medical patients.27 The investigators found that the predictive value of a POA code of “POA=No” was ~75% and concluded that addition of POA codes measurably improved the accuracy of administrative data for identification of VTE. Our work builds on prior studies by specifically evaluating POA coding as it relates to complications after TKA. Our results are timely and important given the high likelihood that CMS will soon implement public reporting of hospital outcomes for TJA and suggest that POA indicators could significantly improve the accuracy of such data.4
Third, while surgical site infections during the index hospitalization for primary TKA were rare (occurring in 0.1% of primary TKA cases) we found that 46.9% of the surgical site infections that did occur during the index admission for primary TKA were POA; this means that nearly 50% of primary TKA infections identified during the index hospital stay might not be actual surgical complications, but constitute patients with septic arthritis at the time of admission. This finding has important information for both researchers and government agencies who use Medicare data to evaluate hospital complication rates surrounding specific diagnoses or procedures. In contrast, we found that very few PEs and surgical site bleeds were POA at the time of the index admission. It is also important to note that when looking at primary TKA readmissions within 90-days of surgery we found that nearly 66% of PEs and surgical site infections were coded as POA which makes intuitive sense from a clinical standpoint (with an additional ~30% lacking completed POA codes).
Focusing instead on revision TKA, our analysis provides a number of important pieces of information. We found that approximately 20%-25% of revision TKA procedures appeared to have a site infection POA. Viewed from an alternative perspective, only 2% of revision TKA patients with infection on the index admission were reported definitely not to have infection POA (POA= No), again providing useful information to researchers, surgeons, and policy makers interested in evaluating arthroplasty quality. Our results also provide useful information related to PE and surgical site bleeding; for example, for revision TKA 52% of PEs occurring during the index hospital stay and 38% of the surgical site bleeds were clearly coded as not present-on-admission (POA) suggesting that these were clear cases of in-hospital complications.
Our study has a number of limitations that warrant brief mention. First, our study was limited to fee-for-service Medicare beneficiaries and thus extrapolation to other populations should be done with caution. Second, we evaluated POA coding reported in Medicare administrative data. We did not have access to patient medical records and thus are unable to validate the accuracy of these codes; while POA codes have been validated in other circumstances and found to agree approximately 75% of the time with data found in the medical record,27,30 validation of Medicare POA codes specific to the complications most common in total joint arthroplasty will be critical.
In conclusion, POa data appear to add important information that enhances our understanding of surgical outcomes and quality. Researchers and policy makers seeking to evaluate TKA outcomes should take advantage of POA data to optimize the accuracy of statistical models and hospital performance reports. Surgeons and hospitals should make efforts to submit complete POA information to insure that data and resulting performance reports are accurate.
Acknowledgments
Grant Support: PC is supported by a K24 award from NIAMS (AR062133). This work is also funded in-part by R01 AG033035 from NIA at the NIH.
Appendix A. Primary TKA patient cohort creation flow chart
Appendix B. Revision TKA patient cohort creation flow chart
Appendix C. ICD-9-CM codes used to identify pulmonary embolism, surgical site bleeding and surgical site infection
| ICD-9-CM codes | |
|---|---|
| Pulmonary Embolism | Any diagnoses = (4151, 41511, 41519) |
| Hemorrhage/Hematoma | Any diagnoses = (99812, 99811) |
| Infection | Any diagnoses = (71100, 71105, 71106, 71160, 71165, 71166, 71190, 71195, 71196, 7300, 73000, 73005, 73006, 7301, 73010, 73015, 73016, 73020, 73025, 73026, 73090, 73095, 73096, 99660, 99666, 99667) |
Footnotes
Conflict of Interest: Dr. Cram, Li, and Ms. Lu have no conflicts to disclose.
References
- 1.Iezzoni LI. Using administrative diagnostic data to assess the quality of hospital care. Pitfalls and potential of ICD-9-CM. 1990;6(2):272–281. doi: 10.1017/s0266462300000799. 1990/// [DOI] [PubMed] [Google Scholar]
- 2.Iezzoni LI. Data Source and implications: Administrative databases. In: Iezzoni LI, editor. Risk adjustment of measuring health care outcomes. Health Administration Press; Ann Arbor, MI: 1997. pp. 169–242. [Google Scholar]
- 3.Katz JN, Losina E, Barrett J, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population.[see comment] Journal of Bone & Joint Surgery - American Volume. 2001 Nov;83-A(11):1622–1629. doi: 10.2106/00004623-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Grosso LM, Curtis JP, Lin Z, et al. Hospital-level risk-standardized complication rate following ellective primary total hip arthroplasty (THA) and/or total knee arthroplasty (TKA): measure methdology report. Yale New Haven Center for Outcomes Research and Evaluation (CORE); 2012. [Google Scholar]
- 5.Shroyer AL, Coombs LP, Peterson ED, et al. The Society of Thoracic Surgeons: 30-day operative mortality and morbidity risk models. Ann Thorac Surg. 2003 Jun;75(6):1856–1864. doi: 10.1016/s0003-4975(03)00179-6. discussion 1864-1855. [DOI] [PubMed] [Google Scholar]
- 6.Brindis RG, Fitzgerald S, Anderson HV, Shaw RE, Weintraub WS, Williams JF. The American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR): building a national clinical data repository. Journal of the American College of Cardiology. 2001 Jun 15;37(8):2240–2245. doi: 10.1016/s0735-1097(01)01372-9. [DOI] [PubMed] [Google Scholar]
- 7.Lonner JH. National joint replacement registry. Am J Orthop (Belle Mead NJ) 2009 Oct;38(10):497–498. [PubMed] [Google Scholar]
- 8.Paxton EW, Inacio MC, Khatod M, Yue EJ, Namba RS. Kaiser Permanente National Total Joint Replacement Registry: Aligning Operations With Information Technology. Clin Orthop Relat Res. 2010 Oct;468(10):2646–2663. doi: 10.1007/s11999-010-1463-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cram P, Cai X, Lu X, Vaughan-Sarrazin MS, Miller BJ. Total knee arthroplasty outcomes in top-ranked and non-top-ranked orthopedic hospitals: an analysis of medicare administrative data. Mayo Clin Proc. 2012 Apr;87(4):341–348. doi: 10.1016/j.mayocp.2011.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012 Sep 26;308(12):1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manley M, Ong K, Lau E, Kurtz SM. Total knee arthroplasty survivorship in the United States Medicare population: effect of hospital and surgeon procedure volume. Journal of Arthroplasty. 2009 Oct;24(7):1061–1067. doi: 10.1016/j.arth.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 12.Glance LG, Osler TM, Mukamel DB, Dick AW. Impact of the present-on-admission indicator on hospital quality measurement: experience with the Agency for Healthcare Research and Quality (AHRQ) Inpatient Quality Indicators. Medical Care. 2008 Feb;46(2):112–119. doi: 10.1097/MLR.0b013e318158aed6. [DOI] [PubMed] [Google Scholar]
- 13.Cram P, Ibrahim SA, Lu X, Wolf BR. Impact of alternative coding schemes on incidence rates of key complications after total hip arthroplasty: a risk-adjusted analysis of a national data set. Geriatr Orthop Surg Rehabil. 2012 Mar;3(1):17–26. doi: 10.1177/2151458511435723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Medicare and Medicaid Services . Hospital-acquired conditions present-on-admission: examination of spillover effects and unintended consequences. RTI International; Research Triangle Park, NC: 2012. Contract # HHSM 500-2005-000291. [Google Scholar]
- 15.Mitchell JB, Bubolz T, Paul JE, et al. Using Medicare claims for outcomes research. Medical Care. 1994 Jul;32(7 Suppl):JS38–51. [PubMed] [Google Scholar]
- 16.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. Journal of Bone & Joint Surgery - American Volume. 2004 Sep;86-a;(9):1909–1916. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Losina E, Barrett J, Mahomed NN, Baron JA, Katz JN. Early failures of total hip replacement: effect of surgeon volume. Arthritis & Rheumatism. 2004 Apr;50(4):1338–1343. doi: 10.1002/art.20148. [DOI] [PubMed] [Google Scholar]
- 18.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical Care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005 Nov;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 20.Cram P, Lu X, Callaghan JJ, Vaughan-Sarrazin MS, Cai X, Li Y. Long-Term Trends in Hip Arthroplasty Use and Volume. J Arthroplasty. 2011 Jul 11; doi: 10.1016/j.arth.2011.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012 Jul 18;94(14):e1038. doi: 10.2106/JBJS.K.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. Journal of Bone and Joint Surgery. 2005 Jun;87(6):1222–1228. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 23.Li Y, Lu X, Wolf BR, Callaghan JJ, Cram P. Variation of Medicare Payments for Total Knee Arthroplasty. J Arthroplasty. 2013 Jul 8; doi: 10.1016/j.arth.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chatterjee P, Joynt KE, Orav EJ, Jha AK. Patient Experience in Safety-Net Hospitals: Implications for Improving Care and Value-Based Purchasing. Arch Intern Med. 2012 Jul 16;:1–7. doi: 10.1001/archinternmed.2012.3158. [DOI] [PubMed] [Google Scholar]
- 25.Ross JS, Cha SS, Epstein AJ, et al. Quality of care for acute myocardial infarction at urban safety-net hospitals. Health Aff (Millwood) 2007 Jan-Feb;26(1):238–248. doi: 10.1377/hlthaff.26.1.238. [DOI] [PubMed] [Google Scholar]
- 26.Dalton JE, Glance LG, Mascha EJ, Ehrlinger J, Chamoun N, Sessler DI. Impact of present-on-admission indicators on risk-adjusted hospital mortality measurement. Anesthesiology. 2013 Jun;118(6):1298–1306. doi: 10.1097/ALN.0b013e31828e12b3. [DOI] [PubMed] [Google Scholar]
- 27.Khanna RR, Kim SB, Jenkins I, et al. Predictive Value of the Present-On-Admission Indicator for Hospital-acquired Venous Thromboembolism. Med Care. 2013 Apr 1; doi: 10.1097/MLR.0b013e318286e34f. [DOI] [PubMed] [Google Scholar]
- 28.Needleman J, Buerhaus PI, Vanderboom C, Harris M. Using Present-On-Admission Coding to Improve Exclusion Rules for Quality Metrics: The Case of Failure-to-Rescue. Med Care. 2013 Aug;51(8):722–730. doi: 10.1097/MLR.0b013e31829808de. [DOI] [PubMed] [Google Scholar]
- 29.Kim H, Capezuti E, Kovner C, Zhao Z, Boockvar K. Prevalence and predictors of adverse events in older surgical patients: impact of the present on admission indicator. Gerontologist. 2010 Dec;50(6):810–820. doi: 10.1093/geront/gnq045. [DOI] [PubMed] [Google Scholar]
- 30.Goldman LE, Chu PW, Osmond D, Bindman A. The accuracy of present-on-admission reporting in administrative data. Health Serv Res. 2011 Dec;46(6pt1):1946–1962. doi: 10.1111/j.1475-6773.2011.01300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]