Abstract
Objective
To test the feasibility and usability of mHealth TLC, an interactive, immersive 3-dimensional iPad health game that coaches lung cancer patients toward assertive communication strategies during first-person virtual clinics visits.
Method
We observed players and conducted semi-structured interviews. Research questions focused on scenario believability, the impact of technical issues, transparency of game goals, and potential of mHealth TLC to decrease lung cancer stigma (LCS) and improve patient–clinician communication.
Results
Eight users confirmed mHealth TLC to be: (1) believable, (2) clinic-appropriate, and (3) helpful in support of informed healthcare consumers. Concerns were expressed about emotionally charged content and plans to use mHealth TLC in clinic settings as opposed to at home.
Conclusions
Although the dialog and interactions addressed emotionally charged issues, players were able to engage, learn, and benefit from role-play in a virtual world. Health games have the potential to improve patient–clinician communication, and mHealth TLC specifically may decrease LCS, and promote optimal self-management.
Practice implications
Process reflection revealed the need for health games to be created by experienced game developers in collaboration with health care experts. To prepare for this best practice, research institutions and game developers interested in health games should proactively seek out networking and collaboration opportunities.
Keywords: Validation, Usability, Lung cancer, Stigma, Virtual worlds, Health games
1. Introduction
With the rise of technology in health care, the use of electronic games provides new possibilities for cost-effective and individually tailored health care interventions [1]. The advantages of virtual games include: (1) the ability to incorporate ethnic and cultural diversity [2] (e.g., allowing participants to select skin tones for their avatars), (2) increased patient access to information and support on demand [3] (e.g., access to online resources or preprogrammed education modules), (3) promotion of behavior change with positive feedback (e.g., points and awards) [4], and (4) the ability to provide information for personalized symptom management (e.g., integration of existing expert system diagnosis and recommendation software) [5].
Lung cancer patients report inadequate communication with physicians about important topics such as end of life care [6]. Stigma is one factor that contributes to poor patient–clinician communication and inappropriate medical referrals [7, 8]. Stigma is defined as blame or devaluation associated in this case with a diagnosis of lung cancer. Currently, there are no interventions that equip patients to manage experiences of lung cancer stigma (LCS) and improve patient–clinician communication. The Mobile Health Tool for Lung Cancer (mHealth TLC) is the first interactive, immersive 3-dimensional iPad health game that allows lung cancer patients to experience first person virtual visits with their clinicians. The aims of mHealth TLC are to decrease LCS, improve patient–clinician communication, and promote optimal self-management. mHealth TLC provides coached patient–provider communication techniques, opportunities for practiced stigma resistance, and patient-specific health information.
1.1. Theoretical framework: gaming, virtual reality and communication theories
Health games are conceptualized as motivational play for adults and can influence social skills, self-perception, empathy, psychosocial functioning (e.g., self-confidence and achievement motivation), and cognitive skills (e.g., attention, planning, and creativity) [9]. The theoretical basis for mHealth TLC draws from gaming, virtual reality, and communication research to create a safe environment where lung cancer patients can be informed and motivated, and can practice self-management with virtual providers.
Throughout the trajectory of the cancer experience, patients are exposed to both physical and psychological discomfort that can decrease motivation toward self-management [9]. Play promotes motivation through the incorporation of voluntary engagement and pleasure, independent of external rewards [10]. In addition, play is a means of stress management and has a key role in helping patients manage distasteful or shameful aspects of their illness [10]. Role-play fosters increased understanding of various social roles and encourages empathy.
Virtual environments are an ideal platform for the promotion of healthy behaviors [11, 12]. Immersion plus interaction constitute the basis for virtual reality. With immersion, players become motivated to proceed through the game’s obstacles and objectives [13]. Replacement of a normal text interface with an avatar – a visual “manifestation of self in a virtual world” (p.30) [14] creates more arousal, trust, and commitment and allows the user to practice interactions with a persona in a virtual world and “engage in… imaginary experiences that transcend the actual world in which they live” (p. 255) [15]. Advantages of virtual worlds include: the ability to carry out tasks that could be difficult in the real world, possibilities for continuing and growing social interactions, and adaptability to user needs [16]. Virtual reality interactions are effective approaches to behavior change for both cancer patients and older adults [17, 18].
Similar to gaming’s focus on motivation, communication scholars have noted that interventions to improve communication should address motivation, knowledge, and action [19, 20]. Communication competence theory purports that success as a communicator requires both capacity (i.e., knowledge of communication skills) and adaptability (i.e., the ability to be a nimble participant, a quality gained through the action of practice) [21]. The link between cognition (i.e., knowing what to do) and behavior (i.e., doing) is facilitated through practice and vicarious learning. Patient interventions that use modeling and rehearsal as pedagogical strategies to transmit knowledge and encourage action through practice tend to be the most effective; health games promote success through modeling and rehearsal [22].
1.2. Health games and older adults
The process of aging changes interactions between cognitive and sensory motor aspects of behavior. Older adults may adapt to these changes by focusing cognitive resources serially, for instance by stopping conversation while putting on shoes [23]. This strategy of approaching tasks serially may preclude older adults from getting the information that they need in a clinic setting when they are being asked to perform sensory motor tasks, e.g., “follow me”, or “take a deep breath”. An additional layer of psycho-cognitive difficulty is introduced with stigma.
Within this context of serial cognitive resource allocation, gaming provides older adults with opportunities to practice parallel processing of everyday tasks. Interactive games that improve psychological health and cognitive functioning of older adults have demonstrated a positive impact on self-management and behavior change [24, 25]. The Center for Technology and Aging reports that for older adults, health game interventions reduce hospitalizations and costs, increase patient satisfaction, and improve self-management and coordination between patients and clinicians [26].
A few interventions have been evaluated with positive results, most with a focus on physical activity and cognition. Physical, interactive fitness games, “exergames,” have demonstrated benefits for older adults. Pre-post assessments of a Window’s-based Kinect TM exergame intervention with 24 older adults (71+) showed leg muscle and joint improvement, but no improvement in functional balance [27]. An RCT assessment of another exergame, the Nintendo Wii Fit, demonstrated that compared to usual exercise provided at retirement homes, the Wii Fit group obtained better balance (left single leg), flexibility (lateral reach), and gait speed [28]. From a cognitive perspective, an RCT of Lumosity showed that participants experienced significant improvements in reaction time, attention, visual memory, and wellbeing. However, neither working memory nor executive control was shifted by the intervention [29].
A recent study of technology adoption behavior by elderly users found that if older adults perceive enough personal utility, they are eager to participate in new digital technology [30]. As of 2014, more than half of older adults go online (59%), and over three quarters of older adults use cell phones (77%) [31]. However, health game usability issues related to sight or disability [31] can be a major concern for this demographic [24], and errors arising as a result of poor usability can hamper efficient learning [32].
Evidence exists that health game interventions help cancer patients access health information and facilitate informed decision making [33]. Time After Time, a health game for older men with localized prostate cancer [24], was found to be feasible and acceptable as an aid for older patients. Although targeted to adolescent cancer patients, Re-Mission, a health videogame, is associated with improved treatment adherence, self-efficacy, and health knowledge [34, 35]. Studies have documented the association between neural positive reward mechanisms activated by playing Re-Mission and positive attitudes toward chemotherapy [36].
1.3. Lung cancer, lung cancer stigma and stigma resistance
Lung cancer kills more men and women, and is associated with greater levels of psychological distress, than any other cancer [37–39]. Lung cancer stigma is a perceived health-related stigma, defined by experiences of exclusion, rejection, blame or devaluation resulting from anticipation of a negative judgment related to a lung cancer diagnosis [40]. The judgment inherent in any health-related stigma is medically unwarranted and may adversely affect health status [41].
Lung cancer stigma is a factor in the psychological and physical health of lung cancer patients [42–44]. LCS negatively impacts patient outcomes such as quality of life [43] and symptom severity [43, 44]. Clinician–patient communication has been found to be inadequate, especially for issues related to prognosis, symptom management, mental health, and end of life care [6]. Studies have shown that physicians believe type of cancer is not a factor in referral decisions, however, compared to breast cancer, lung cancer patients are less likely to receive appropriate referrals [8]. In addition, our previous work suggests that medical interactions may trigger LCS through activation of patient feelings of inferiority and loss of control [45].
Stigma resistance is a protective factor in other health-related stigmas (e.g., inflammatory bowel disease [46], HIV/AIDS [47–49], and schizophrenia [50]), but is unexplored in lung cancer. External interpersonal support (such as that received from support groups and supportive family [49], and empathetic care) contributes to stigma resistance [50]. A meta-analysis of mental illness stigma interventions has shown measurable reductions in public stigma, but did not change perceptions of stigma on the part of patients [51]. Considering this, there is room for patient-centered interventions that attempt stigma mitigation.
1.4. mHealth TLC scenario
mHealth Tool for Lung Cancer (mHealth TLC) is a technology-based stigma reduction intervention. Lung cancer patient “players” arrive ata bus stop outside a cancer center, where they are met by a guide or “coach”. The coach presents himself as a knowledgable friend (neither patient nor provider) who offers explanation and support and who may be called upon for advice or clarification throughout the experience. Many games start in the form of narrative to draw players into the game world [52]; narrative increases motivation and immersion [9, 13]. The coach in mHealth TLC provides the narrative (i.e., story of a lung cancer patient who previously visited this virtual clinic and achieved optimal health literacy and self-management). To continue the immersion, players are given choices about their physical and verbal responses to stimuli throughout the game, and encouraged to return for more practice over the course of four “visits”.
The goal for players is to choose the more assertive responses to help acquire the most information in order to manage their lung cancer and advance through the clinic landscape. Players experience successful navigation of a clinic visit through increasingly complex situations, giving them practice addressing issues and asking questions, which thereby develops skills they can use in their real world clinic visits.
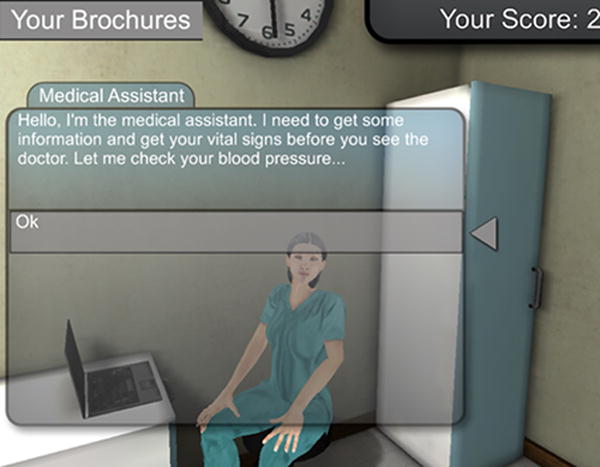
After initial interactions with the coach, players know that during the game they will: (1) interact with three oncology staff (i.e., the receptionist, medical assistant, and provider); (Fig. 1) (2) navigate through the clinic and acquire all of the information they need to manage their lung cancer care; (3) access the coach for help, as needed; (4) be provided opportunities to select from a range of verbal responses (e.g., aggressive, assertive, and passive), and thus tailor their communication strategy iteratively during play.
Fig. 1.
In order to create realistic dialog for players, coach, and non-playing characters, we used qualitative data from our previous studies with lung cancer patients [45]. Patients’ stories of experiences of stigmatization and attempts at self-management informed both narrative and dialog. Stigma, blame, and self-blame are addressed in the interactions, and information about the role of addiction, social/cultural factors, and tobacco industry influence on smoking behaviors are highlighted.
The goal of usability testing was to identify functional and conceptual problems, observe user performance, and determine user satisfaction. The research questions were: (1) Were game scenarios believable and potentially valuable to end-users? (2) What were the impacts of technical issues on player acceptance and tolerance of the game? (3) Were game goals transparent to participants and, if not, what were the perceived game goals? and (4) Did participants think that mHealth TLC could provide intended game outcomes to future players (i.e., better communication between patients and providers)?
The development team determined that this game version was too incomplete to test with patients. Usability testing was performed to determine whether the project should be developed in this platform, or continue in a different virtual environment. The development team worried that lung cancer patients might be further distressed by the emotional material contained in the game. For these reasons, we chose a small sample of locally recruited usability testers to gain insights that might direct further development.
2. Methods
Structured interviews for mHealth TLC usability testing incorporated “think-aloud” and verbal probing techniques which have previously been used in the assessment of computer-based and online information processing of websites [53, 54].
From October 10–18th, 2012, eight users were recruited from the University of California, San Francisco and participated in the usability testing. Users were health professionals (not students) between the ages of 20 and 50, and most were connected to lung cancer through experience with patients as nurses, doctors, or researchers. Most described themselves as “experienced” or “accomplished” computer users. Seven users were female, and only one was male. Only the male user and one female had experience with gaming or virtual reality simulations. Two users described some programming or scripting background. Users were interviewed by author1 and author2 as they tested the prototype, and audio was recorded. The one hour interview included: a brief introduction to mHealth TLC, playing mHealth TLC and providing think-aloud narration about their thoughts, choices made in the game, and answers to questions about game specifics and overall game impressions (see Appendix A for the interview protocol).
3. Results
3.1. Believability and value
The game was found to be believable, regardless of major technical task failures (e.g., the “ask the coach” function did not work, some avatars walked through walls, etc.) and some potentially unbelievable (because of the emotional content) narrative choices. Users likened the game to a “Choose your own adventure” story. Users reacted strongly when confronted with “angry” or “unhelpful” clinic staff – evidence of the game’s ability to emotionally engage players. Reactions to emotionally charged interactions included the following: users read the dialog out loud from the closed caption (despite the dialog already having been delivered by audio), users giggled before they responded (interpreted as a sign of discomfort), and users broke out of the game framework to make verbal comments to the researcher about how “it’s best to ignore” these types of responses.
Some users did not understand several of the basic “game” features (e.g., reward system, information brochures, and on-call coach support). Reward systems were not identified as valuable to users. Seven out of eight users were unable to collect the information in the brochures; the multi-step process of this task hindered comprehension and achievement. In addition, although users were able to “call the coach” outside of the ongoing narrative as was promised in the game introduction, none of the users were able to elicit any meaningful feedback about how to proceed from the on-call coach. By contrast, coach feedback scripted into the narrative throughout the game was appreciated and provided the users with information about their progression through the game.
In post-play interviews, all users responded positively to the idea of the acquisition of information through in-world brochures (although they were underused), and no one articulated a reason for choosing one brochure over another.
3.2. Technical issues
Users were not generally hindered by technical issues, which were numerous and observable in all aspects of the prototype. For example, a clipboard and headset cut through the bodies of clinic staff, which were sometimes missing limbs. In the medical assistant module, two of the closed caption dialog bubbles and their subsequent response choices were visible but blank, requiring researchers to instruct users to click unmarked dialog options. Auditory issues provoked the most responses; these included unequalized volume and repetitive background coughing. During orientation to the usability test, users were introduced to the possibility of technical issues with this script: “this is a prototype and you may experience issues.” Auditory issues were not explicitly mentioned, potentially encouraging higher expectations for auditory information. Additionally, the irregularity of the volume may have been more noticeable because it was one of the first bugs encountered; the coach was extremely loud in one dialog and then much fainter in the next.
Some “distractions” that users identified during the experience included voice/closed-caption mismatches (e.g., “participant” from the recorded audio instead of the written closed-caption “patient”). Odd camera angles also prompted comments suggesting at least momentary lapses in experience immersion.
Suggestions for improvement included providing more instruction at the beginning of the game and additional time to practice navigation basics. More consistent language was desired; for example “folder” and “notes” were used interchangeably as a mechanism to store information. The appearance of the coach was problematic. In his introduction, he was loud and perceived as “unlikeable,” but as users progressed and received positive feedback on their responses most agreed with the user who noted: “I didn’t like him at first … but by the end I felt he was my friend.”
3.3. Transparent goals
Users found the goals transparent, and despite not having the goals outlined at the beginning, they were able to verbalize them. Users perceived goals to be: (1) the ability to manage emotions and stay calm in an adverse office setting, (2) better communication with providers because of the ability to ask more questions and obtain necessary information, even when it is not offered, and (3) better navigation of clinic space and procedures. In short, users saw the goal of the game as preparation for “me [a player] to be an informed consumer of healthcare.”
All eight users understood and were able to articulate the goal “to practice dealing with this stuff.” In addition, all users understood the logic of the game (waiting room, exam room, and finally consultation room for a discussion with the care provider) and all users felt that they had done well or had “completed” the experience. They also noted that the experience helped clarify “what was possible” in a clinic visit.
3.4. Game outcomes
Users were divided about whether the game was clinic-appropriate. One user connected pre-office-visit play to potential efficacy: “This would be fresh in my mind right before a clinic visit. I would know to ask questions and lots of them and to take advantage of brochures [and other information]. That silence in this case is not golden.” Two older users found the material emotionally taxing and expressed interest in having more time to process the information prior to a real oncology visit. Some suggested timing game play for the evening before an actual clinic visit.
Users found effective the game instructions for eliciting patient-relevant information during an oncology office visit. They anticipated that the game would create informed healthcare consumers, patients who, as a result of their play, would ask in-depth questions of their providers and be active creators of their treatment plans. Users wanted to extend the reach of the game outside of the virtual world, and they noted that having the symptom information to review “offline,” “at home,” or with real clinicians would be valuable. As in previous user feedback sessions, several users mentioned the connection between the virtual game and the actual clinic. Users suggested that brochures collected in the game should be provided in paper at clinic visits.
4. Discussion and conclusion
4.1. Discussion
Usability testing of the virtual environment and narrative structure of the mHealth TLC concept suggests that it will be useful for lung cancer patients. Users found the avatar and office environment visuals believable within the context of the game and fully engaged with the narrative regardless of technical problems. The interactions experienced, though sometimes highly emotionally charged, were rated high on believability. These scenarios successfully elicited the cognitive and emotional experience of perceived stigma, and players experienced the opportunity to practice stigma resistance.
Some critical components of the game did not perform well with users. Auditory content distracted players, highlighting the need for investment in high-quality voice and sound recording. Although important, the oncall coaching function had minimal utilization and poor performance. The change in attitude toward the coach as he offered feedback suggested an opportunity to explore how the figure of the coach might be best optimized. Users valued opportunities to learn and practice stigma resistance and to become self-advocates when interacting.
An effective reward system is an important feature in a health game; however, it was not understood by users in the mHealth TLC prototype. Being able to actively make choices and engage in a participatory fashion may provide some positive reward [36], but an active reward system is an essential part of engagement for health games. A top priority in the next stage of development is to devise a creative and engaging reward system.
Providing mHealth TLC to lung cancer patients in waiting rooms or online at home is our ultimate goal, one that requires future development and testing. Usability results validated that mHealth TLC is clinic-appropriate. Both this test and prior participatory design sessions indicated the potential of this intervention as an in-clinic experience. Participants wanted and expected activities in the virtual world (e.g., indicating symptoms and taking brochures) to have “real world” parallels in a clinic setting. A minority of users (two) voiced concern that the emotional content of mHealth TLC would be too taxing just before an oncology office visit. Lung cancer patients have reported feeling “shellshocked” at their initial oncology office visits, and that these emotions interfered with comprehension and retention of information and patient–provider communication [45]. With this in mind, emotional overload remains a concern. Timing of the intervention, mental health support, and factors specific to the game and the situated experience of play need to be considered.
Users validated the potential for mHealth TLC to make a positive impact on the lung cancer patient care experience. Improvement in clinician–patient communication and self-management through active engagement in care and treatment decisions comprise this positive impact. Next steps in development include beta testing in a new platform, feasibility testing with patients on mobile tablets in waiting-room environments, and eventual factorial design trials for outcomes testing.
4.2. Limitations
This study is limited in that there were few testers, testers were not lung cancer patients, and we were testing a prototype instead of a finished product. The next round of feasibility tests will include patients with a more robust product. In keeping with an iterative development model, our team wanted to gather feedback throughout the development process prior to sharing the product with lung cancer patients.
4.3. Conclusion
mHealth TLC is an interactive, immersive 3-dimensional iPad health game that allows individuals to experience first person virtual visits with their clinicians. mHealth TLC has the potential to improve patient–clinician communication, decrease LCS, and promote optimal self-management. Positive usability results for the mHealth TLC include believable game narrative, minimal game experience interference due to task failures, participant generation of game and intervention goals, and indications that mHealth TLC may positively influence lung cancer patient outcomes. Theoretical and conceptual underpinnings of the game and narrative realism were validated. Although the dialog and interactions addressed emotionally charged issues, players were able to engage, learn, and benefit from role-play in a virtual world.
4.4. Practice implications
Results from this usability study of mHealth TLC demonstrated that the fundamentals of virtual games (i.e., motivation, play, and stories) can supersede serious technical difficulties, and support the use of early usability testing as a way to gather important data for improved intervention development. Glitches that we thought might rob players of motivation were not much of a problem to our test group. This observation suggests that a population of largely novice game players may not require high gaming production levels to benefit from health games.
Finally, health games, though they may be driven by research or practitioner initiatives, need to be created by experienced game developers in collaboration with health care experts. Looking forward, both health research institutions and game developers interested in health games should seek out opportunities for networking and collaboration in order to ensure that the best possible product reaches end users.
Supplementary Material
Acknowledgments
This research was supported in part by National Cancer Institute Grant CA-113710. This research was supported in part by a grant from the California Tobacco Related Disease Research Program TRDRP #21XT-0063.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.pec.2014.12.006.
Footnotes
Conflict of interest
We have no conflicts of interest with this work.
References
- 1.Kharrazi H, Lu AS, Gharghabi F, Coleman W. A scoping review of health game research: past, present, and future. Games Health: Res Dev Clin Appl. 2012;1:153–64. doi: 10.1089/g4h.2012.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dietrich DR. Avatars of whiteness: racial expression in video game characters. Sociol Inq. 2013;83:82–105. [Google Scholar]
- 3.Atkinson NL, Gold RS. The promise and challenge of eHealth interventions. Am J Health Behav. 2002;26:494–503. doi: 10.5993/ajhb.26.6.10. [DOI] [PubMed] [Google Scholar]
- 4.Read JL, Shortell SM. Interactive games to promote behavior change in prevention and treatment. J Am Med Assoc. 2011;305:1704–5. doi: 10.1001/jama.2011.408. [DOI] [PubMed] [Google Scholar]
- 5.Baggott C, Gibson F, Coll B, Kletter R, Zeltzer P, Miaskowski C. Initial evaluation of an electronic symptom diary for adolescents with cancer. JMIR Res Protoc. 2012;1:e23. doi: 10.2196/resprot.2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nelson JE, Gay EB, Berman AR, Powell CA, Salazar-Schicchi J, Wisnivesky JP. Patients rate physician communication about lung cancer. Cancer. 2011;117:5212–20. doi: 10.1002/cncr.26152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones L, Watson BM. Developments in health communication in the 21st century. J Lang Soc Psychol. 2012;31:415–36. [Google Scholar]
- 8.Wassenaar TR, Eickhoff JC, Jarzemsky DR, Smith SS, Larson ML, Schiller JH. Differences in primary care clinicians’ approach to non-small cell lung cancer patients compared with breast cancer. J Thorac Oncol. 2007;2:722–8. doi: 10.1097/JTO.0b013e3180cc2599. [DOI] [PubMed] [Google Scholar]
- 9.Kato PM. Video games in health care: closing the gap. Rev Gen Psychol. 2010;14:113. [Google Scholar]
- 10.Rieber LP. Seriously considering play: designing interactive learning environments based on the blending of microworlds, simulations, and games. Educ Technol Res Dev. 1996;44:43–58. [Google Scholar]
- 11.Neuendorf P, Simpson C. Designing effective teaching and learning scenarios for Health Education in Virtual Worlds. World Conference on Educational Multimedia, Hypermedia and Telecommunications. 2010:2478–82. [Google Scholar]
- 12.Falloon G. Using avatars and virtual environments in learning: what do they have to offer. Br J Educ Technol. 2010;41:108–22. [Google Scholar]
- 13.Annetta LA. The I’s have it: a framework for serious educational game design. Rev Gen Psychol. 2010;14:105. [Google Scholar]
- 14.Peterson M. Learning interaction in an avatar-based virtual environment: a preliminary study. PacCALL J. 2005;1:29–40. [Google Scholar]
- 15.Deuchar S, Nodder C. The impact of avatars and 3D virtual world creation on learning. 16th Annual NACCQ Conference. 2003 [Google Scholar]
- 16.Antonacci DM, Modaress N. Envisioning the educational possibilities of user-created virtual worlds. AACE J. 2008;16:115–26. [Google Scholar]
- 17.Morganti F, Marrakchi S, Urban PP, Iannoccari GA, Riva G. A virtual reality based tool for the assessment of survey to route spatial organization ability in elderly population: preliminary data. Cogn Process. 2009;10:257–9. doi: 10.1007/s10339-009-0284-9. [DOI] [PubMed] [Google Scholar]
- 18.Optale G, Urgesi C, Busato V, Marin S, Piron L, Priftis K, Gamberini L, Capodieci S, Bordin A. Controlling memory impairment in elderly adults using virtual reality memory training: a randomized control pilot study. J Neurol Rehabil. 2009;24:348. doi: 10.1177/1545968309353328. [DOI] [PubMed] [Google Scholar]
- 19.Spitzburgh B, Cupach W. Interpersonal communication competence. Beverly Hills, CA: Sage; 1984. [Google Scholar]
- 20.Street R. Interpersonal communication skills in health care contexts. Mahwah, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- 21.Epstein R, Street R. Patient-centered communication in cancer care: promoting healing and reducing suffering. Bethesda, MD: National Cancer Institute; 2007. (NIH Publication No. 07-6225). [Google Scholar]
- 22.Cegala DJ, Street RL, Jr, Clinch CR. The impact of patient participation on physicians’ information provision during a primary care medical interview. Health Commun. 2007;21:177–85. doi: 10.1080/10410230701307824. [DOI] [PubMed] [Google Scholar]
- 23.Schäfer S, Huxhold O, Lindenberger U. Healthy mind in healthy body? A review of sensorimotor–cognitive interdependencies in old age. Eur Rev Aging Phys Act. 2006;3:45–54. [Google Scholar]
- 24.Reichlin L, Mani N, McArthur K, Harris AM, Rajan N, Dacso CC. Assessing the acceptability and usability of an interactive serious game in aiding treatment decisions for patients with localized prostate cancer. J Med Internet Res. 2011;13:e4. doi: 10.2196/jmir.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murray E. Web-based interventions for behavior change and self-management: potential, pitfalls, and progress. Medicine 20. 2012;1:e3. doi: 10.2196/med20.1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Center for Technology and Aging. mHealth technologies: applications to benefit older adults. Draft position paper. 2011 [Google Scholar]
- 27.Sato K, Kuroki K, Saiki S, Nagatomi R. The effects of exercise intervention using Kinect TM on healthy elderly individuals: a quasi-experimental study. Open J Ther Rehabil. 2014;2014 [Google Scholar]
- 28.Nicholson VP, McKean M, Lowe J, Fawcett C, Burkett B. Six weeks of unsupervised Nintendo Wii fit gaming is effective at improving balance in independent older adults. J Aging Phys Act. 2014 doi: 10.1123/japa.2013-0148. [DOI] [PubMed] [Google Scholar]
- 29.Ballesteros S, Prieto A, Mayes J, Toril P, Pita C, Ponce de León L, Reales J, Waterworth J. Brain training with non-action video games enhances aspects of cognition in older adults: a randomized controlled trial. Front Aging Neurosci. 2014 doi: 10.3389/fnagi.2014.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melenhorst A. Adopting communication technology in later life: the decisive role of benefits [Unpublished doctoral dissertation] The Netherlands: Technical University of Eindhoven; 2002. [Google Scholar]
- 31.Pew Research Center. Older adults and technology use. 2014. [Google Scholar]
- 32.Beale IL. Video games for health: principles and strategies for design and evaluation. New York: Nova Science Publishers; 2010. [Google Scholar]
- 33.Harris L, Dresser C, Kreps GL. E-Health as dialogue: communication and quality of cancer care. Dialogue Syst Health Commun. 2006 [Google Scholar]
- 34.Beale IL, Kato PM, Marin-Bowling VM, Guthrie N, Cole SW. Improvement in cancer-related knowledge following use of a psychoeducational video game for adolescents and young adults with cancer. J Adolesc Health. 2007;41:263–70. doi: 10.1016/j.jadohealth.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 35.Kato PM, Cole SW, Bradlyn AS, Pollock BH. A video game improves behavioral outcomes in adolescents and young adults with cancer: a randomized trial. Pediatrics. 2008;122:e305–17. doi: 10.1542/peds.2007-3134. [DOI] [PubMed] [Google Scholar]
- 36.Cole SW, Yoo DJ, Knutson B. Interactivity and reward-related neural activation during a serious videogame. PLoS ONE. 2012;7:e33909. doi: 10.1371/journal.pone.0033909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 38.Else-Quest NM, LoConte NK, Schiller JH, Hyde JS. Perceived stigma, self-blame, and adjustment among lung, breast and prostate cancer patients. Psychol Health. 2009;24:949–64. doi: 10.1080/08870440802074664. [DOI] [PubMed] [Google Scholar]
- 39.Lynch J, Goodhart F, Saunders Y, O’Connor SJ. Screening for psychological distress in patients with lung cancer: results of a clinical audit evaluating the use of the patient Distress Thermometer. Support Care Cancer. 2010;19:193–202. doi: 10.1007/s00520-009-0799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cataldo JK, Slaughter R, Jahan TM, Pongquan VL, Hwang WJ. Measuring stigma in people with lung cancer: psychometric testing of the cataldo lung cancer stigma scale. Oncol Nurs Forum. 2011;38:E46–54. doi: 10.1188/11.ONF.E46-E54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weiss MG, Ramakrishna J. Stigma interventions and research for international health. Lancet. 2006;367:536–8. doi: 10.1016/S0140-6736(06)68189-0. [DOI] [PubMed] [Google Scholar]
- 42.Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: qualitative study. Br Med J. 2004;328:1470–3. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cataldo JK, Jahan TM, Pongquan VL. Lung cancer stigma, depression, and quality of life among ever and never smokers. Eur J Oncol Nurs. 2012;16:264–9. doi: 10.1016/j.ejon.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cataldo JK, Brodsky JL. Lung cancer stigma, anxiety, depression and symptom severity. Oncology. 2013;85:33–40. doi: 10.1159/000350834. (1423–0232) [DOI] [PubMed] [Google Scholar]
- 45.Brown C, Cataldo J. Explorations of lung cancer stigma for female long-term survivors. Nurs Inq. 2013 doi: 10.1111/nin.12024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Taft T, Ballou S, Keefer L. A preliminary evaluation of internalized stigma and stigma resistance in inflammatory bowel disease. J Health Psychol. 2012 doi: 10.1177/1359105312446768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Poindexter CC, Shippy RA. HIV diagnosis disclosure: stigma management and stigma resistance. J Gerontol Soc Work. 2010;53:366–81. doi: 10.1080/01634371003715841. [DOI] [PubMed] [Google Scholar]
- 48.Goudge J, Ngoma B, Manderson L, Schneider H. Stigma, identity and resistance among people living with HIV in South Africa. SAHARA J. 2009;6:94–104. doi: 10.1080/17290376.2009.9724937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Buseh AG, Stevens PE. Constrained but not determined by stigma: resistance by African American women living with HIV. Women Health. 2007;44:1–18. doi: 10.1300/J013v44n03_01. [DOI] [PubMed] [Google Scholar]
- 50.Sibitz I, Unger A, Woppmann A, Zidek T, Amering M. Stigma resistance in patients with schizophrenia. Schizophr Bull. 2011;37:316–23. doi: 10.1093/schbul/sbp048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Griffiths KM, Carron-Arthur B, Parsons A, Reid R. Effectiveness of programs for reducing the stigma associated with mental disorders. A meta-analysis of randomized controlled trials. World Psychiatry. 2014;13:161–75. doi: 10.1002/wps.20129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lu AS. Using Health Games: Spotlight on Story Narrative in Health Games: an interview with Amy Shirong Lu. 2012. [Google Scholar]
- 53.Eveland WP, Dunwoody S. Examining information processing on the World Wide Web using think aloud protocols. 2000. pp. 219–44. [Google Scholar]
- 54.Donker A, Markopoulos P. A comparison of think-aloud, questionnaires and interviews for testing usability with children. People and computers XVI-memorable yet invisible. Springer; 2002:305–16. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


