Abstract
Objectives
This study aimed to evaluate the prevalence, severity, duration, and location of pain after transobturator midurethral sling.
Methods
We evaluated patients who underwent inside-out transobturator sling from March 2011 through February 2013. Presence of pelvic girdle pain, its severity, and location were documented preoperatively and at 2- and 6-week postoperative visits. Pain severity was measured on a scale of 1 to 10, with 10 being the “worst imaginable” pain.
Results
Of the 130 women analyzed, the median age was 50.0 years (interquartile range, 44.0–62.0). Thirty-nine percent of women reported preoperative pain, mostly mild with a median score of 1.0 (1.0–5.0). The most common sites of postoperative-onset pain were the lateral leg, medial leg, groin, and low back. Women reporting preoperative pain were not more likely to report postoperative-onset pain than women without preoperative pain (P = 0.42). Twelve percent of women at 2 weeks and 0.8% at 6 weeks reported severe postoperative-onset pain. Women reporting postoperative-onset pain were equally likely to be satisfied with the procedure as those without pain at 2 (P = 0.76) and 6 (P = 0.74) weeks.
Conclusions
Women undergoing transobturator sling commonly report preoperative pain. An expected postoperative increase in pain generally resolved by the sixth postoperative week. The lateral leg was the most common site of pain. Postoperative-onset pain was not associated with decreased patient satisfaction.
Keywords: lateral leg, pain, transobturator sling, TVT-O
Suburethral slings have become a first-line option in the treatment of stress urinary incontinence. The minimally invasive midurethral sling procedures offer the estimated 20% of women with stress urinary incontinence a high likelihood of surgical cure with relatively low associated morbidity. Differences between retropubic and transobturator approaches have been well studied, with evidence of fairly similar effectiveness but distinct risk profiles.1, 2 Among the recognized risks of the transobturator approach is the possibility of postoperative pain and neuropathy.3
The inside-out transobturator modification was first described by de Leval4 in 2003. Since that time, the prevalence and characterization of associated pain has gradually emerged in the literature, with multiple locations identified. In 2007, Meschia et al2 reported a 5% incidence of thigh pain among patients after the procedure. Neuman et al5 also localized pain to the thigh, but found 32% reported pain. Laurikainen et al1 randomized women to retropubic and transobturator procedures, and found a 16% incidence of groin pain among those patients who underwent transobturator sling. Giberti et al6 described pelvic pain after transobturator sling in 10% of their cohort, and 2.2% of subjects in a study by Kaelin-Gambirasio et al7 reported perineal pain. Although some of these described pain entities may overlap, the varied pattern suggests that pain after transobturator midurethral sling likely is caused by multiple physiologic processes. As we previously reported, patients and providers use a variety of terms to describe the location of pain after transobturator sling.8
Given the variability in pain location, the variation in pain duration is not surprising. Although limited evidence exists, cohort studies suggest that pain lasts only a few weeks, whereas case reports document a small number of patients with years of persistent pain.5, 9–11 Although these reports describe postoperative pain severe enough to warrant sling excision, we are unaware of published reports quantifying the typical severity and course of patient-reported discomfort associated with transobturator slings. Further, it is unclear what effect, if any, such pain has on the patient perception of sling effectiveness or overall satisfaction after a midurethral sling.
The primary objectives of our study were to characterize the prevalence, severity, duration, and location of pain in patients undergoing transobturator midurethral sling. Secondary objectives were to evaluate whether pain was associated with the perception of sling success or patient satisfaction with the procedure.
MATERIALS AND METHODS
We conducted a prospective observational cohort study of patients undergoing the inside-out tension-free vaginal tape obturator (TVT-O; Ethicon, Inc, Somerville, NJ) procedure at our institution from March 2011 through February 2013. Study approval was obtained from the Mount Auburn Hospital Institutional Review Board. All women 18 years and older planning to undergo transobturator sling were eligible. Women were consented and enrolled at the preoperative visit. Residents and fellows participated in cases as appropriate for training. All participants underwent the sling procedure with cystoscopy in lithotomy position using padded Allens. Women undergoing only sling placement and cystoscopy typically were prescribed 30 ibuprofen 600-mg tablets with 3 refills and 10 tablets of a narcotic—either oxycodone with acetaminophen 5/325 mg or hydrocodone with acetaminophen 5/500 mg—with no refills. More might be given if appropriate for a concomitant procedure. The presence, severity, and location of pain were recorded preoperatively and at 2- and 6-week postoperative visits. If there was clinical need for a postoperative visit beyond 6 weeks, data collection was extended. The primary outcome was postoperative-onset pain in any lower body location. Postoperative-onset pain was defined as pain at any given site that was reported at either or both of the postoperative visits but was not reported at the preoperative visit. Clinicians conducting postoperative visits verbally asked participants to grade the severity of their pain at each site on a 0 to 10 scale, with 10 being the “worst imaginable” pain. Severe pain was defined as a pain score of 7 or greater. Clinicians indicated the location of the patient’s pain at each visit on a standardized diagram with views of a woman anteriorly, posteriorly, and in lithotomy. Any additional treatment or referrals to outside providers for the indication of pain were noted. Concomitant procedures were abstracted from the operative report.
Sling effectiveness was assessed using subjective criteria. Participants were asked to categorize their stress-related leakage episodes since the surgery as being “zero,” “one or more but fewer than preoperatively,” or “the same or more as preoperatively.” These categories were considered to be cured, improved, or failed, respectively. Finally, clinicians were prompted to indicate a participant’s satisfaction or lack thereof with the question “Is the patient satisfied with the outcome of the surgery?” and if not, to specify a reason.
All data analysis was performed using SAS 9.3 (SAS Institute Inc, Cary, NC). All tests were 2-sided, and P values of less than 0.05 were considered statistically significant. Data are presented as median and interquartile range or proportion. Comparisons were made using the appropriate tests for independent and paired data.
RESULTS
During the study period, 137 women were enrolled. Two participants did not undergo surgery, 3 had retropubic slings, and 2 had incomplete records; they were excluded from the analysis. The remaining 130 women had transobturator midurethral sling procedures performed by one of 4 fellowship-trained urogynecologists. The median age of participants at the time of surgery was 50.0 years (44.0–62.0 years). The median body mass index (BMI) was 27.2 kg/m2 (23.8–31.3 kg/m2). Nearly half (44.6%) of the participants reported postoperative-onset pain. Those participants who reported postoperative-onset pain at one or both postoperative visits had a BMI slightly higher than those who reported no postoperative-onset pain, but this difference did not meet statistical significance (P = 0.06). Data on age, BMI, and use of concomitant procedures are shown in Table 1.
TABLE 1.
Characteristics of Women Undergoing Transobturator Sling
| Characteristic | All Women, n = 130 | No Postoperative-Onset Pain, n = 72 | Postoperative-Onset Pain, n = 58 | P* |
|---|---|---|---|---|
| Age at surgery, y | 50.0 (44.0Y62.0) | 52.0 (45.0Y65.0) | 50.0 (42.0Y60.0) | 0.14 |
| BMI, kg/m2 | 27.2 (23.8Y31.3) | 26.1 (23.2Y30.9) | 28.8 (25.0Y31.6) | 0.06 |
| Concomitant surgery | 0.01 | |||
| Yes | 68 (52.3) | 45 (62.5) | 23 (39.7) | |
| No | 62 (47.7) | 27 (37.5) | 35 (60.3) |
Data are presented as median (interquartile range) or n (%).
P values are comparing women without new postoperative pain and women with new postoperative pain.
Concomitant surgery included a vaginal procedure in 49 (37.7%) participants, a laparoscopic procedure in 28 (21.5%), a robotic in 10 (7.7%), and an abdominal in 2 (1.5%). Twenty-one (16.2%) women had multiple concomitant surgeries. Compared with patients undergoing both a sling and a concomitant procedure, patients undergoing sling alone were significantly more likely to report postoperative-onset pain during at least 1 postoperative visit (P = 0.01). Among women reporting postoperative-onset pain, there was no significant difference in severe pain between those who underwent concomitant procedures and those who did not (P = 0.07).
More than one third (39.2%) of the study population reported preoperative pain, mostly mild in severity with a median pain score of 1.0 (1.0–4.0). Among these women, the most commonly reported site was the hip (60.8%). The sites of pain by time of onset are shown in Table 2.
TABLE 2.
Location of Pain by Time of Onset
| Preoperative Pain |
Postoperative-Onset Pain, All Participants |
Postoperative-Onset Pain, No Concomitant Surgery |
|||
|---|---|---|---|---|---|
| n = 130 | 2-wk Visit, n = 117 | 6-wk Visit, n = 119 | 2-wk Visit, n = 55 | 6-wk Visit, n = 55 | |
| Any pain | 51 (39.2) | 53 (45.3) | 8 (6.7) | 32 (58.2) | 5 (9.1) |
| Low back | 6 (4.6) | 8 (6.8) | 0 (0.0) | 2 (3.6) | 0 (0.0) |
| Hip | 31 (23.8) | 5 (4.3) | 1 (0.8) | 3 (5.5) | 1 (1.8) |
| Leg | |||||
| Lateral | 7 (5.4) | 20 (17.1) | 0 (0.0) | 13 (23.6) | 0 (0.0) |
| Medial | 6 (4.6) | 14 (12.0) | 2 (1.9) | 12 (21.8) | 1 (1.8) |
| Anterior | 8 (6.2) | 3 (2.6) | 0 (0.0) | 2 (3.6) | 0 (0.0) |
| Posterior | 2 (1.5) | 3 (2.6) | 1 (1.0) | 1 (1.8) | 0 (0.0) |
| Groin | 9 (6.9) | 8 (6.8) | 1 (0.8) | 4 (7.3) | 1 (1.8) |
| Incision site | 0 (0.0) | 4 (3.4) | 1 (0.8) | 4 (7.3) | 0 (0.0) |
| Motor weakness | 0 (0.0) | 4 (3.4) | 0 (0.0) | 3 (5.5) | 0 (0.0) |
| Other | 10 (7.7) | 3 (2.6) | 4 (3.4) | 2 (3.6) | 3 (5.5) |
Data are reported as n (%).
Percentages do not add to 100%. Some women reported more than 1 site of pain and some women did not report site of pain.
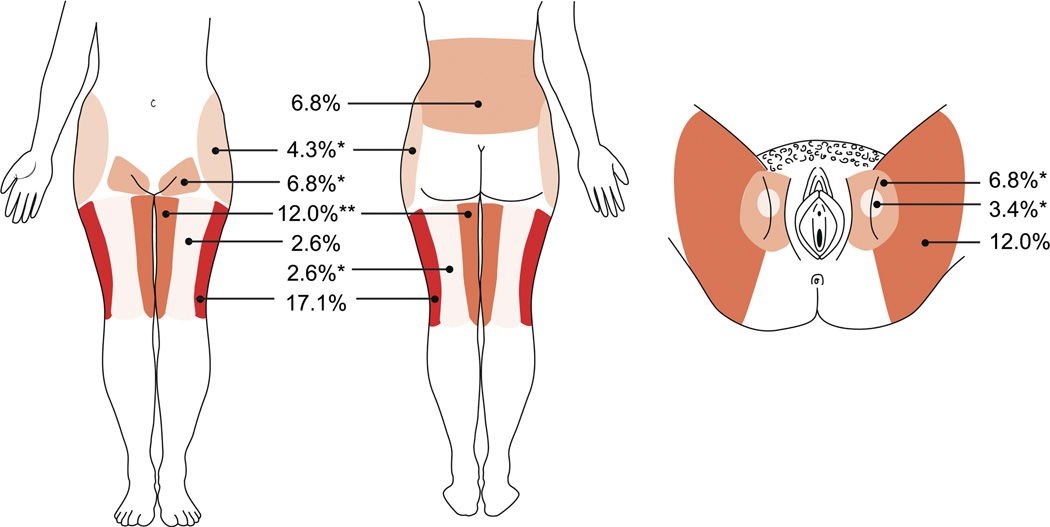
Among the 117 participants who returned for a 2-week visit, 53 (45.3%) reported postoperative-onset pain in at least 1 location; 41 (35.0%) reported pain in more than 1 site. At this visit, the incidence of pain was highest in the lateral leg (17.1%), medial leg (12.0%), groin (6.8%), and low back (6.8%). In the subgroup undergoing sling and cystoscopy alone, the most common sites were the lateral leg (23.6%), medial leg (21.8%), groin (7.3%), and incision sites (7.3%). By 6 weeks after the procedure, only 8 (6.7%) participants reported postoperative-onset pain. The incidence and distribution of pain is demonstrated in Figure 1. Although 5 patients underwent surgical reoperation, these were all cases of either urinary retention necessitating sling release or persistent stress incontinence necessitating repeat sling procedure. No study participants returned to the operating room for an indication of pain.
FIGURE 1.
Distribution of postoperative-onset pain after transobturator sling. Shaded regions map to locations of 2-week pain specified in Table 2. Darker shading is used for regions with increased prevalence of pain. Each * represents 1 participant with pain at a given location at 6 weeks.
At the 2-week visit, 14 (12.0%) participants reported severe pain. Of these, the most common site was the leg, where 11 patients endorsed severe pain: 6 laterally, 6 medially, 2 anteriorly, and 1 posteriorly, with some patients indicating multiple sites. Only 1 (0.8%) participant reported severe pain—of the hip and groin—at the 6-week visit. This individual had reported pain of lower severity in the same locations at 2 weeks which had intensified; she was referred to physical therapy.
Women who reported preoperative pain were equally as likely to report postoperative-onset pain (49.0%) as women who did not report preoperative pain (41.8%; P = 0.42). Women with preoperative pain were equally as likely as women not reporting preoperative pain to be satisfied with the procedure at both 2 weeks (P = 0.76) and 6 weeks (P = 74). Similarly, at both postoperative visits, women reporting postoperative-onset pain were equally as likely to be satisfied with the procedure as those without pain (P = 0.42 at 2 weeks; P = 0.52 at 6 weeks).
With respect to subjective success of the procedure at 6 weeks, 92 (77.3%) women were cured, 20 (16.8%) improved, and 5 (4.2%) failed. Table 3 indicates the incidence of sling success and patient satisfaction. Participants who had not yet resumed the activity that had provoked leakage were among those who were uncertain as to the success of the procedure or their satisfaction. At both 2 and 6 weeks postoperatively, women with pain were equally likely to be successfully treated for their stress urinary incontinence than those without pain (P = 0.07 at 2 weeks; P = 0.32 at 6 weeks).
TABLE 3.
Procedure Satisfaction and Success
| All | No Postoperative Pain | Postoperative Pain | P* | |
|---|---|---|---|---|
| 2-wk visit | n = 117 | n = 64 | n = 53 | |
| Satisfied | 0.42 | |||
| Yes | 100 (85.5) | 52 (81.3) | 48 (90.6) | |
| No | 11 (9.4) | 7 (10.9) | 4 (7.5) | |
| Patient uncertain | 3 (2.6) | 2 (3.1) | 1 (1.9) | |
| Missing | 3 (2.6) | 3 (4.7) | 0 (0.0) | |
| Success | 0.07 | |||
| Cured | 79 (67.5) | 48 (75.0) | 31 (58.5) | |
| Improved | 26 (22.2) | 11 (17.2) | 15 (28.3) | |
| Failure | 6 (5.1) | 4 (6.3) | 2 (3.8) | |
| Patient uncertain | 2 (1.7) | 1 (1.6) | 1 (1.9) | |
| Missing | 4 (3.4) | 0 (0.0) | 4 (7.5) | |
| 6-wk visit | n = 119 | n = 111 | n = 8 | |
| Satisfied | 0.52 | |||
| Yes | 109 (91.6) | 102 (91.9) | 7 (87.5) | |
| No | 10 (8.4) | 9 (8.1) | 1 (12.5) | |
| Success | 0.32 | |||
| Cured | 92 (77.3) | 87 (78.4) | 5 (62.5) | |
| Improved | 20 (16.8) | 18 (16.2) | 2 (25.0) | |
| Failure | 5 (4.2) | 4 (3.6) | 1 (12.5) | |
| Missing | 2 (1.7) | 2 (1.8) | 0 (0.0) |
Data are presented as n (%).
P value comparison is between the categories of “No Postoperative Pain” and “Postoperative Pain.”
Success of the procedure was highly associated with patient satisfaction. At 2 weeks, women who reported a failed procedure were less likely to be satisfied (0.0%) than women who were cured (96.2%) or improved (88.0%; P < 0.0001). A similar pattern was seen at 6 weeks (P < 0.0001).
DISCUSSION
Our findings demonstrate that many women have pain that may be overlooked before undergoing midurethral sling placement. When patients were asked specifically about pain before surgery, we found that nearly 40% reported pain. Our finding that postoperative onset pain is highly prevalent (45.3%) at 2 weeks but decreased dramatically to 6.7% at 6 weeks is consistent with wide range of pain prevalence reported by other authors.
The finding that pain was less common and less severe at the 6-week postoperative visit than at baseline was unanticipated. Given that stress urinary incontinence is not a painful condition and slings are not used in the treatment of pain, it is difficult to conceive of a mechanism by which our surgical intervention is directly improving preoperative pain. Rather, other explanations may account for these findings. Although it is possible that patients may continue to take pain medications after resolution of their surgical pain, we feel this is unlikely based on the limited amount of prescription medication we typically give to our patients. One alternative is that participants may have restricted their activity level such that they refrained from movements that provoked baseline pain. More likely is the explanation that patients, aware of their role as study participants, are filtering out pain unrelated to surgery and not reporting it at the 6-week visit.
The study’s prospective nature and assessment of baseline pain were study strengths. Additionally, the use of standardized pain scales and diagrams to establish severity and location were advantages of our study. There was no variation among participants with respect to the sling device as all received an inside-out transobturator sling, although caution is needed if these findings are to be generalized to other brands of transobturator sling. Our findings also are strengthened by the small (<10%) proportion of patients lost to follow-up at each postoperative visit.
Use of a diagram allowed us to determine that the lateral leg was the most implicated pain site in our patient population. Although a smaller proportion of participants reported groin pain, our results do not support the idea that the groin and site of the adductor longus are primary sites of pain after an inside-out transobturator sling. Although there is no clear mechanism to explain pain localized to the lateral leg, possibilities include intraoperative positioning and referred pain. Presumably, this would mean that shorter operating times would lower a patient’s risk for positioning-related pain, whereas we actually found patients who underwent sling alone, and thus shorter operating times, had a higher prevalence of pain. Potentially, this could be due to greater abduction during sling procedures alone.
Knowledge that pain from transobturator sling procedures is common but usually transient is informative for patient counseling and expectations. Evidence showing that preoperative pain is not associated with postoperative satisfaction may prevent us as clinicians from developing an unfounded belief that surgical candidates with pain will “not do well.” In fact, patient satisfaction with the procedure seems largely unrelated to preoperative or postoperative pain. Not surprisingly, sling efficacy was strongly associated with satisfaction.
There are several limitations to this study. As discussed previously, use of pain medication was not assessed. This information would have provided a more nuanced understanding of participants’ pain profiles. In addition, the relatively small sample size limits our ability to perform meaningful subgroup analyses and limits the study’s power to detect small, but potentially clinically meaningful, differences. Finally, although pain usually resolved by 6 weeks, the short follow-up interval gives no further information regarding the outcomes of those patients with persistent pain. Further study is needed to determine this subgroup’s natural history and the best treatment.
This study further characterizes the nature of pain after transobturator midurethral sling procedures. Understanding postoperative pain is not only necessary for thorough patient counseling, but also an important part of providing compassionate surgical care.
ACKNOWLEDGMENT
The authors thank Jane N. Hayward for the help in preparation of Figure 1.
This work was conducted with support from Harvard Catalyst/The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award 8UL1TR000170-05 and financial contributions from Harvard University and its affiliated academic health care centers).
Footnotes
The authors have declared they have no conflicts of interest.
REFERENCES
- 1.Laurikainen E, Valpas A, Kivela A, et al. Retropubic compared with transobturator tape placement in treatment of urinary incontinence: a randomized controlled trial. Obstet Gynecol. 2007;109(1):4–11. doi: 10.1097/01.AOG.0000249607.82768.a1. [DOI] [PubMed] [Google Scholar]
- 2.Meschia M, Bertozzi R, Pifarotti P, et al. Peri-operative morbidity and early results of a randomised trial comparing TVT and TVT-O. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(11):1257–1261. doi: 10.1007/s00192-007-0334-8. [DOI] [PubMed] [Google Scholar]
- 3.Boyles SH, Edwards R, Gregory W, et al. Complications associated with transobturator sling procedures. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(1):19–22. doi: 10.1007/s00192-006-0091-0. [DOI] [PubMed] [Google Scholar]
- 4.de Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol. 2003;44(6):724–730. doi: 10.1016/j.eururo.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Neuman M, Sosnovski V, Goralnik S, et al. Comparison of two inside-out transobturator suburethral sling techniques for stress incontinence: early postoperative thigh pain and 3-year outcomes. Int J Urol. 2012;19(12):1103–1107. doi: 10.1111/j.1442-2042.2012.03117.x. [DOI] [PubMed] [Google Scholar]
- 6.Giberti C, Gallo F, Cortese P, et al. Transobturator tape for treatment of female stress urinary incontinence: objective and subjective results after a mean follow-up of two years. Urology. 2007;69(4):703–707. doi: 10.1016/j.urology.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 7.Kaelin-Gambirasio I, Jacob S, Boulvain M, et al. Complications associated with transobturator sling procedures: analysis of 233 consecutive cases with a 27 months follow-up. BMC Womens Health. 2009;9:28. doi: 10.1186/1472-6874-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cadish LA, Hacker MR, Dodge LE, et al. Association of body mass index with hip and thigh pain following transobturator midurethral sling placement. Am J Obstet Gynecol. 2010;203(5):508. doi: 10.1016/j.ajog.2010.07.023. e501-e505. [DOI] [PubMed] [Google Scholar]
- 9.Masata J, Hubka P, Martan A. Pudendal neuralgia following transobturator inside-out tape procedure (TVT-O)—case report and anatomical study. Int Urogynecol J. 2012;23(4):505–507. doi: 10.1007/s00192-011-1555-4. [DOI] [PubMed] [Google Scholar]
- 10.Trivedi P, D’Costa S, Shirkande P, et al. A comparative evaluation of suburethral and transobturator sling in 209 cases with stress urinary incontinence in 8 years. J Gynecol Endosc Surg. 2009;1(2):105–112. doi: 10.4103/0974-1216.71615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolter CE, Starkman JS, Scarpero HM, et al. Removal of transobturator midurethral sling for refractory thigh pain. Urology. 2008;72(2):461. doi: 10.1016/j.urology.2007.12.052. e461-e463. [DOI] [PubMed] [Google Scholar]