Abstract
Surprisingly little is known about long-term spending patterns in the under-65 population. Such information could inform efforts to improve coverage and control costs. Using the MarketScan claims database, we characterize the persistence of healthcare spending in the privately-insured, under-65 population. Over a six-year period, 69.8% of enrollees never had annual spending in the top 10% of the distribution and the bottom 50% of spenders accounted for less than 10% of spending. Those in the top 10% in 2003 were almost as likely (34.4%) to be in the top 10% five years later as one year later (43.4%). Many comorbid conditions retained much of their predictive power even five years later. The persistence at both ends of the spending distribution indicates the potential for adverse selection and cream-skimming and supports the use of disease-management, particularly for those with the conditions that remained strong predictors of high spending throughout the follow-up period.
Keywords: Healthcare expenditures, health insurance, healthcare reform, comorbidities, economics
Introduction
Not surprisingly given the randomness of costly health events, many studies have shown that the spending distribution is highly skewed within a single year. However, surprisingly little is known about long-term spending patterns in the under-65 population that is the target of Affordable Care Act (ACA) coverage expansions. The extent to which health spending persists for multiple years has implications for insurers concerned about adverse selection, regulators attempting to detect and manage risk-selection by insurers, identification of cost-control measures most likely to be effective and the distributional impact of out-of-pocket spending under high deductible health plans.
Establishing the frequencies of different spending patterns and determining which individuals are at greater risk of specific spending patterns can inform the design of appropriate insurance products and public policies to ensure adequate coverage. If persistence is relatively low, high current expenditures will not strongly signal high future expenditures and vice versa. Therefore, currently healthy individuals may hesitate to opt out of ACA-mandated coverage and risk bearing an unexpected short-term spike in health care spending before their next open enrollment window. Similarly, Medicare buy-in programs for those under age 65 or Medicare Advantage may not face substantial risk selection. Conversely, if persistence is relatively high, risk selection is likely to be a substantial issue for health insurance exchanges (even with penalties for non-enrollment), and for Medicare buy-in programs and Medicare Advantage. With high persistence, premium insurance over time (insuring against the “risk of becoming a high risk”) would be a salient issue addressed by reforms such as limits on risk-rating [see Pauly, Kunreuther, and Hirth’s (1995) model of annual, but guaranteed renewable, insurance contracts when incurring an illness signals an increase in the probability of future illness].
Given the concentration of spending among a small percentage of patients, the success of cost control measures strongly depends on the ability to identify people likely to be (or become) perpetually high spenders and modify their care trajectories. This is consistent with the “hot spot” concept summarized by Atul Gawande (2011), where a number of private and Medicare demonstrations have reduced costs via outpatient care that targets the most complex, high need patients. While most demonstrations to date have not delivered savings, several of the more intensive efforts have (MedPAC, 2012; CBO, 2012). High persistence in health spending would suggest that longer-term disease management programs may be more effective than high-cost case management programs focusing on contemporaneous spending.
Understanding patterns of spending persistence is also important for analyzing the out-of-pocket burden for the steadily rising number of enrollees in Consumer Directed Health Plans (CDHPs) with tax-deductible Health Savings Accounts (HSAs) or Health Reimbursement Accounts (HRAs) (Kaiser Family Foundation/HRET, 2012) or other High Deductible Health Plans (HDHPs). CDHPs are expected to continue to play a significant role after implementation of the ACA as most CDHP designs qualify for meeting the insurance mandate. With a high deductible, the effective out-of-pocket price of care can change substantially from year-to-year, and with a savings plan that can be built up or drawn down over time (i.e., across years), understanding the likely time path of spending becomes even more salient to enrollees and policy-makers compared to those in traditional, single year plan designs. If spending patterns are persistent, then spending from year to year can be anticipated and patients and plan managers can reliably determine funding levels and manage year-to-year carryovers. Low-spenders could predictably accumulate substantial unused funds over time while high spenders deplete their accounts most years, yielding a very uneven long-term distribution of out-of-pocket spending across enrollees. Conversely, if there is substantial year-to-year mobility between spending levels, enrollees would need to make account contributions to fund an occasional high-spending year, but may also game the system by waiting until high-spending years to undergo discretionary treatments.
New Contribution
Surprisingly little is known about long-term spending patterns and the persistence of health spending in the under-65 population. Available data sets that are broadly representative, such as the Medical Expenditure Panel Survey (MEPS) have short follow up. Therefore, most research on longer-term spending patterns has relied on data from a single employer or insurer, or has involved the Medicare population. Finally, existing studies have been based mainly on data from the 1980s or 1990s. We use 6 recent years of claims (2003–2008) from the 2003–2008 Truven Health MarketScan Database to substantially improve on previous studies of the persistence of health spending the under-65 population in terms of timeliness, length of follow-up and sample sizes.
Key prior studies on persistence of health spending
Key studies using U.S. data are summarized in Table 1. Two prominent studies examined data for Medicare fee-for-service enrollees. Garber, MaCurdy, & McClellan (1998) found that among enrollees who were in the top 5% of the spending distribution in one year, 15.2% remained in the top 5% the following year and only 8.8% remained in that category two years later. Expenditure growth was concentrated among the highest spenders. More recently, Riley (2007) documented time trends in the persistence of spending among Medicare enrollees from 1975–2004, with persistence increasing until approximately the mid-1990s, and then decreasing somewhat thereafter.
Table 1.
Related Literature
| Study | Population Represented |
Outcome | Data Source | Years Covered |
Maximum Follow-Up Time |
|---|---|---|---|---|---|
| Garber et al. (1998) | Medicare enrollees | Total spending | Medicare claims for random sample of enrollees | 1987–1995 | 4 years |
| Riley (2007) | Medicare enrollees | Total spending | Continuous Medicare History Sample | 1975–2004 | 3 years |
| Eichner et al. (1997) | Privately insured (single employer) | Total spending | FFS claims for employees and dependents of 1 Fortune 500 company | 1989–1991 | 2 years |
| Chapman (1997) | Privately insured (single HMO) | Claims for 1 IPA model HMO | 1989–1993 | 3 years | |
| Monheit (2003) | US non-institutionalized population | Total spending | MEPS | 1996–97 | 1 year |
| Cohen and Yu (2012) | US non-institutionalized population | Total spending | MEPS | 2008–2009 | 1 year |
| Pauly and Zeng (2004) | Privately insured | Prescription drug spending | MarketScan | 1994–98 | 4 years |
The remaining studies focused on privately insured individuals or the general population. Eichner, McClellan, & Wise (1997) used three years of data (1989–1991) from a single employer and found that 19%–29% of persons with more than $5,000 in medical expenditures in 1989 continued to spend more than $5000 in 1990, and 12%–22% stayed at that level in 1991. Chapman (1997) used data from one Independent Practice Association (IPA) model Health Maintenance Organization (HMO) and found that of those in the top 5% of the 1989 spending distribution, 19% remained in the top 5% in 1990 and 14% remained in the top 5% in 1991. Similarly, of those in the 80th–94th percentiles of spending in 1989, 32% remained in the 80th–94th percentiles in 1990 and 10% moved into the top 5% of the 1990 distribution. Cohen and Yu (2012) used data on the non-institutionalized US population of all ages from the 2009–2010 Medical Expenditure Panel Study (MEPS) to analyze spending persistence over two years. They found that 40% of those in the top decile of spending in 2009 remained in the top decile in 2010, somewhat higher than the one-third estimated by Monheit (2003) in a similar analysis of MEPS data from 1996–1997. Pauly and Zeng (2004) used MarketScan data to examine implications of persistence in prescription drug spending for the market for drug coverage. Although they focused on drug coverage, they also reported some information on the persistence of total spending (probability of remaining in the top 20% of the spending distribution), finding 46% of those in the top quintile in 1994 were in the same spending quintile in 1998.
In addition to the studies of U.S. spending summarized in Table 1, an interesting recent study used an 18-year balanced panel of persons age 16 and over from the British Household Panel Survey to examine the persistence of healthcare utilization (Kohn & Liu, 2013). Key findings were that past use predicted future use even after controlling for health and other characteristics, that past utilization predicted future utilization more strongly at older ages and lower health status, and that first year utilization retained some predictive power throughout the follow-up.
Methods
Our primary data source is the 2003–2008 Truven Health MarketScan Database. The availability of 6 recent years of fully-adjudicated claims, representing the health care experience of millions of enrollees allows us to substantially improve on previous studies of the under-65 population in terms of timeliness, length of follow-up and sample sizes. This study received an IRB exemption through the University of Michigan IRB due to the use of secondary data.
MarketScan represents the healthcare experience of employees and dependents receiving health insurance coverage through over 100, mainly self-insured, medium and large employers. The number of individuals represented in MarketScan rose from 8 million in 2003 to 41 million in 2008, with enrollment distributed broadly across all four Census regions. Each region had at least 6.5 million covered lives in 2008, with the South being most heavily represented (38.8%). Data from all carve-outs (e.g., prescription drug, mental health) are included. Out-of-plan spending for items like over-the-counter drugs and patient-borne costs such as travel to appointments are not represented. If a deductible is imposed, claims satisfying the deductible and falling below the deductible threshold are included in the database. Spending has been adjusted to 2008 dollars using the medical cost Consumer Price Index (CPI). All models adjust standard errors for clustering at the MSA level. Given the very large sample size, these adjustments had little impact on the significance of the results. Firm identifiers were not available in the releasable data set, so clustering at the employer level was not possible.
The enrollment characteristics in the MarketScan Database are largely similar to nationally-representative data for individuals with employer-sponsored insurance (ESI) in the Medical Expenditure Panel Survey (MEPS), although a higher percentage of MarketScan enrollees reside in the South Census region. A comparison of the spending distribution of individuals in employer-sponsored plans in the 2005 MEPS survey to the 2005 MarketScan Database found the MarketScan expenditures were approximately 10% higher than MEPS. MarketScan provided a more complete capture of high cost spenders (e.g., institutionalized individuals or out of area utilization) and a more complete capture of spending across the spending distribution (Aizcorbe et al., 2012).
Over 2.5 million people can be followed for the entire 2003–2008 period. For these individuals enrollment is distributed across plan types in 2003 with 14% enrolled in Comprehensive plans, 28% in HMOs, 16% in point of service (POS) plans, 27% in PPOs and the remaining 5% in Other plan types (Table 2). By 2008 the mix of plan types changed (not shown) to 5% in Comprehensive plans, 28% in HMOs, 17% in POS plans, 46% in PPOs, 3% in CDHPs and 1% in Other or Unknown plan types. For firms with over 200 employees, the plan distribution from the Kaiser Family Foundation and Health Research & Educational Trust 2008 Annual Survey Employer Health Benefits was 1% Comprehensive, 20% HMO, 10% POS, 64% PPOs and 5% CDHP ((Kaiser Family Foundation/HRET, 2008). Not surprisingly given worker mobility, attrition is common. About 60 percent of commercially-insured, under age 65 individuals exit the sample within 5 years. Some attrition arises from benign reasons (in terms of the risk of biasing estimates of spending persistence in the broader population all persons under age 65 holding ESI at a point in time), such as censoring due to employers no longer providing data to MarketScan (i.e., the entire group exits rather than a self-selected subset of individuals), or exogenous exits such as children aging out of dependent status or workers aging into Medicare coverage. Other exits, such as death, retirement (without continued coverage), loss of employment or changing employers may be endogenous to health spending. Therefore, we describe the extent and correlates of attrition from our sample to gain some insight into the extent of selection in our continuous enrollment cohort.
Table 2.
2003 Sample characteristics by spending category
(1=Usually low, 2=Low/Moderate, 3=Sometimes high, 4=Often high, 5=Usually high)*
| 1 | 2 | 3 | 4 | 5 | All Sample |
|
|---|---|---|---|---|---|---|
| Age | 30.1 | 43.6 | 42.0 | 46.5 | 47.7 | 35.2 |
| Male | 0.52 | 0.41 | 0.40 | 0.37 | 0.35 | 0.47 |
| Charlson Comorbidity Index Score | 0.07 | 0.26 | 0.25 | 0.59 | 1.16 | 0.18 |
| Prescription Drug Spending | 255 | 1,482 | 1,172 | 2,856 | 7,522 | 890 |
| Medical Spending in 2003 | 932 | 3,349 | 5,647 | 11,980 | 24,477 | 3,376 |
| Trauma occurred | 0.010 | 0.010 | 0.013 | 0.015 | 0.018 | 0.011 |
| Median household income at zip code enrollee resided ($1,000's) | 49.8 | 49.9 | 48.4 | 47.6 | 47.7 | 49.3 |
| Urban Area | ||||||
| Urban | 0.80 | 0.79 | 0.76 | 0.75 | 0.77 | 0.79 |
| Rural | 0.19 | 0.21 | 0.23 | 0.25 | 0.23 | 0.20 |
| Unknown | 0.01 | 0.01 | 0.01 | 0.01 | 0.00 | 0.01 |
| Geographic Region of employee residence | ||||||
| Northeast | 0.09 | 0.10 | 0.08 | 0.08 | 0.08 | 0.09 |
| North Central | 0.27 | 0.32 | 0.30 | 0.33 | 0.34 | 0.29 |
| South | 0.32 | 0.36 | 0.38 | 0.40 | 0.39 | 0.34 |
| West | 0.30 | 0.21 | 0.23 | 0.19 | 0.19 | 0.27 |
| Unknown | 0.01 | 0.01 | 0.01 | 0.01 | 0.01 | 0.01 |
| Plan Type | ||||||
| Comprehensive | 0.12 | 0.17 | 0.15 | 0.19 | 0.22 | 0.14 |
| HMO | 0.32 | 0.22 | 0.24 | 0.18 | 0.16 | 0.28 |
| POS | 0.16 | 0.16 | 0.16 | 0.15 | 0.14 | 0.16 |
| PPO | 0.35 | 0.40 | 0.41 | 0.44 | 0.44 | 0.37 |
| Other | 0.05 | 0.05 | 0.05 | 0.04 | 0.04 | 0.05 |
| Relation to Employee | ||||||
| Employee | 0.42 | 0.58 | 0.59 | 0.59 | 0.54 | 0.48 |
| Spouse | 0.20 | 0.31 | 0.31 | 0.36 | 0.41 | 0.25 |
| Child/Other | 0.38 | 0.11 | 0.11 | 0.05 | 0.05 | 0.27 |
| Employee Classification | ||||||
| Non-union | 0.39 | 0.39 | 0.38 | 0.36 | 0.35 | 0.39 |
| Union | 0.17 | 0.24 | 0.21 | 0.27 | 0.29 | 0.19 |
| Unknown | 0.44 | 0.36 | 0.41 | 0.37 | 0.36 | 0.42 |
| Employment Status | ||||||
| Active Full Time | 0.91 | 0.82 | 0.84 | 0.76 | 0.70 | 0.87 |
| Active Part Time or Seasonal | 0.01 | 0.01 | 0.01 | 0.01 | 0.00 | 0.01 |
| Early Retiree | 0.05 | 0.13 | 0.11 | 0.17 | 0.20 | 0.08 |
| Medicare Eligible Retiree | 0.01 | 0.01 | 0.01 | 0.01 | 0.02 | 0.01 |
| Other/Unknown | 0.02 | 0.04 | 0.04 | 0.05 | 0.08 | 0.03 |
| Comorbidities | ||||||
| Myocardial Infarction | 0.000 | 0.002 | 0.004 | 0.012 | 0.018 | 0.002 |
| Congestive heart failure | 0.000 | 0.002 | 0.004 | 0.014 | 0.035 | 0.003 |
| Peripheral vascular disease | 0.000 | 0.003 | 0.004 | 0.011 | 0.019 | 0.002 |
| Cerebrovascular disease | 0.001 | 0.008 | 0.011 | 0.028 | 0.047 | 0.006 |
| Chronic pulmonary disease | 0.039 | 0.080 | 0.067 | 0.112 | 0.175 | 0.056 |
| Rheumatologic disease or connective tissue disease | 0.001 | 0.008 | 0.008 | 0.024 | 0.070 | 0.006 |
| Peptic Ulcer disease | 0.001 | 0.002 | 0.003 | 0.007 | 0.010 | 0.002 |
| Mild liver disease | 0.000 | 0.001 | 0.002 | 0.004 | 0.009 | 0.001 |
| Moderate or severe liver disease | 0.000 | 0.000 | 0.000 | 0.001 | 0.003 | 0.000 |
| Moderate or severe renal disease | 0.000 | 0.002 | 0.002 | 0.006 | 0.030 | 0.002 |
| Diabetes | 0.011 | 0.087 | 0.065 | 0.152 | 0.241 | 0.043 |
| Diabetes + complications | 0.000 | 0.006 | 0.005 | 0.018 | 0.048 | 0.004 |
| Any tumor (Other Malignancy) | 0.005 | 0.023 | 0.028 | 0.058 | 0.079 | 0.016 |
| Metastatic solid tumor | 0.000 | 0.001 | 0.002 | 0.006 | 0.012 | 0.001 |
| AIDS | 0.000 | 0.000 | 0.000 | 0.002 | 0.020 | 0.001 |
| Dementia | 0.001 | 0.002 | 0.001 | 0.002 | 0.003 | 0.001 |
| PDG Category | ||||||
| Major Depressions | 0.006 | 0.028 | 0.024 | 0.055 | 0.106 | 0.017 |
| Anxiety Disorders (NOS) | 0.010 | 0.032 | 0.026 | 0.044 | 0.061 | 0.019 |
| Organic Mental Disorders | 0.001 | 0.003 | 0.004 | 0.008 | 0.017 | 0.003 |
| Alcohol Use Disorders | 0.001 | 0.002 | 0.004 | 0.007 | 0.009 | 0.002 |
| Opioid and Other Substance Use Disorders | 0.003 | 0.006 | 0.010 | 0.017 | 0.023 | 0.006 |
| Schizophrenia Disorders | 0.000 | 0.001 | 0.001 | 0.002 | 0.005 | 0.001 |
| Other Psychotic Disorders (NEC, NOS) | 0.000 | 0.002 | 0.002 | 0.006 | 0.014 | 0.002 |
| Bipolar Disorders | 0.001 | 0.005 | 0.004 | 0.014 | 0.034 | 0.003 |
| Other Specific & Atypical Affective Disorders | 0.004 | 0.017 | 0.014 | 0.028 | 0.047 | 0.010 |
| Post Traumatic Stress Disorders | 0.001 | 0.002 | 0.002 | 0.004 | 0.007 | 0.001 |
| Personality Disorders | 0.000 | 0.001 | 0.001 | 0.001 | 0.003 | 0.000 |
| Impulse Control, Adjustment and other Mental Disorders | 0.030 | 0.069 | 0.054 | 0.082 | 0.109 | 0.044 |
| Sample Size | 1,562,478 | 222,210 | 581,917 | 120,326 | 69,498 | 2,556,429 |
Usually low – low spending at least four years, no years with high spending, Low/Moderate – low spending in three or fewer years, no years with high spending, Sometimes high – 1 or 2 years of high spending, Often high – 3 or 4 years of high spending, Usually high – 5 or 6 years of high spending. High spending is the top 10% and low spending is the bottom 70% of annual expenditures.
For employees and dependents remaining in MarketScan continuously from 2003–2008, healthcare spending is characterized several ways. To create manageable and interpretable groupings, we classified each individual’s annual spending as high, moderate or low. Due to the skewed distribution of expenditures and changes in average spending over time, rather than using tertiles or fixed dollar cutoffs, we defined high as the top 10 percent, moderate as the top 10%–30%, and low as the bottom 70% of the spending distribution for the year. In 2008, the cut points between categories were $3,362 (top 30 percent) and $10,535 (top 10 percent). Because there are 729 possible patterns of spending across categories over six years, we then developed a typology of patterns based on time spent in the three categories. To enhance interpretability, we created five ordered categories:
Usually low (low spending at least four years and no years with high spending)
Low/Moderate (low spending in three or fewer years but no years with high spending)
Sometimes high (one or two years of high spending)
Often high (three or four years of high spending)
Usually high (five or six years of high spending)
The extremes of the ordered categorization reflect the greatest persistence of spending. Clearly, these classifications mask some potentially interesting variation (e.g., is spending rising or falling over time?) that could be explored by using other classification schemes in further research. However, we believe that this classification scheme provides useful insights into the dynamics of health spending and yields meaningful and intuitive interpretations.
To describe the dynamics of high spending, we construct transition tables showing the probability that a person in the top 10% of the spending distribution in 2003 remains in the top 10% one through five years later. To determine how the concentration of spending that has often been calculated for a single year persists over multiple years, we calculate the percent of spending by different shares of the population over one, three and six years.
Logistic regression is used to model the dichotomous outcome (spending in the top 10% in year t+n, where n=1, 2, 3, 4 or 5, as a function of characteristics in year t). This determines the extent to which current characteristics predict future high spending in both the short- and long-term. Ordered logistic regressions are estimated to predict which of the five spending patterns occurred over the six-year study period.
Results
The characteristics of persons in different six-year spending categories are summarized in Table 2. 69.8% of the sample never had spending in the top 10% (that is, they were in the Usually low or Low/Moderate categories). Of the 30.2% who appeared in the top 10% at least once, about three quarters (75.4%) were in the Sometimes high category (that is, top 10% no more than twice during the six year period). Those in the Usually high group were on average 17.6 years older than those in the Usually low group, and this high spending group was predominantly female (65%). More individuals in the higher spending groups had PPO or Comprehensive insurance coverage in 2003 compared to the other types of insurance plan. As the categorizations included more time spent in years with higher annual medical expenditures, individuals were less likely to be children/other, and the relative mix of employees vs. spouses shifted towards spouses at the higher spending categories (e.g., employees outnumbered spouses by 42.1% vs. 19.8% in the Usually low category, but only by 53.7% to 41.1% in the Usually high category). The Charlson comorbidity index, a measure of morbidity based on the presence of pre-defined comorbid conditions, was 17.1 times higher for individuals classified as Usually high, compared to those in the Usually low group.
Table 3 shows the probability of top 10% spenders remaining in that category in subsequent years. Focusing on the top row, of those individuals who were in the top 10% of expenditures in 2003, the likelihood of being in the top 10% declined only gradually as the follow-up time rose. For example, 43.4% remained in the top 10% in 2004 and 34.4% (not necessarily the same individuals) were high spenders in 2008. Therefore, those who were in the top 10% in 2003 were 79.3% (34.4%/43.4%) as likely to be high spenders five years later as they were only one year later, indicating only a modest decline in the persistence of high spending over time.
Table 3.
Persistence of high spending across years (N=2,556,429)
| Top 10% | High 1 year later |
High 2 years later |
High 3 years later |
High 4 years later |
High 5 years later |
|---|---|---|---|---|---|
| 2003 | 43.4% | 39.6% | 37.7% | 35.9% | 34.4% |
| 2004 | 44.0% | 40.2% | 37.9% | 36.3% | |
| 2005 | 44.3% | 40.3% | 38.2% | ||
| 2006 | 44.9% | 40.9% | |||
| 2007 | 45.4% |
High spending is in the top 10% of annual expenditures
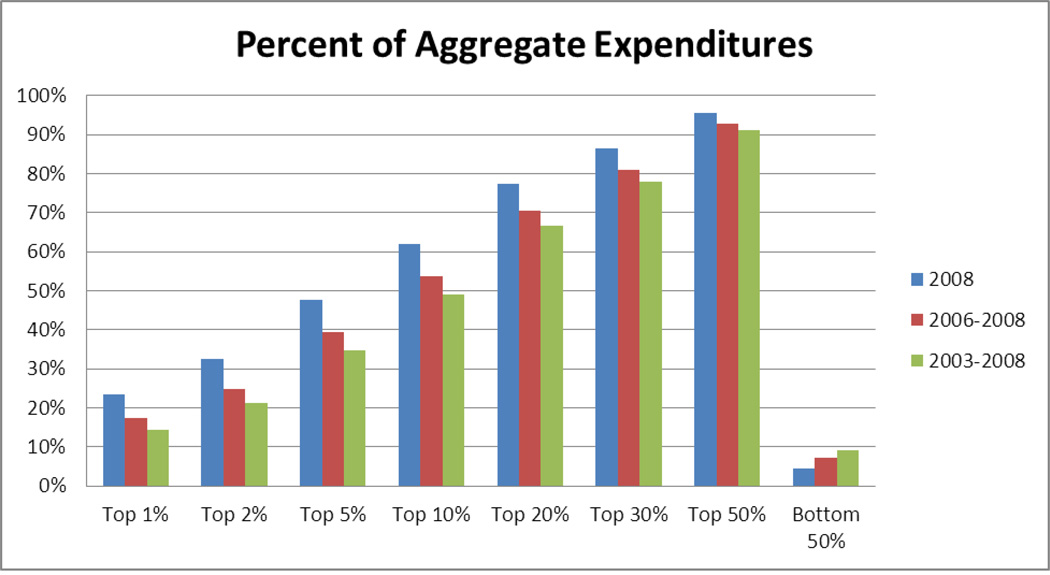
Figure 1 shows the percent of aggregate expenditures that different percentiles of enrollees account for in 2008, 2006–2008 and 2003–2008. The one year (2008) concentration statistics are quite similar to those often quoted. With longer time frames, concentration declines moderately at the high end (e.g., top 1% of 2008 spenders account for 24% of 2008 spending whereas the top 1% of 2003–2008 spenders account for 14% of all 2003–2008 spending). At the low end of the distribution, concentration changes only modestly when comparing one and six year measures (bottom 50% accounted for 5% of 2008 spending vs. 9% of 2003–2008 spending).
Figure 1. Concentration of health expenditures over 1, 3, and 6 years.
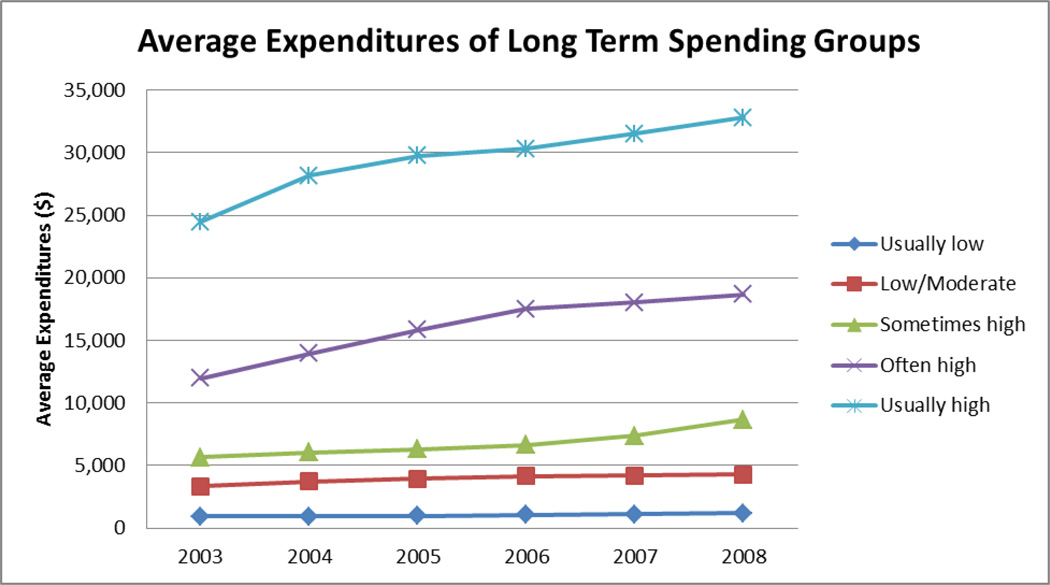
Figure 2 illustrates spending growth by category. For those classified as Usually low spenders, average annual expenditures increased from $932 to $1,207 (29.5% increase), while for the Low/Moderate group, the average annual medical expenditures went from $3,349 to $4,293 (28.2% increase). For individuals who were classified as Sometimes high, average annual medical expenditures jumped from $5,647 to $8,664 from 2003 to 2008 (53.4% increase). Similarly, those who were Often high (3–4 years of high spending) had an increase in their average annual expenditures from $11,980 to $18,661 (55.8% increase). Finally, those who were Usually High (5–6 years high) went from spending on average $24,477 in 2003, to $32,785 in 2008 (33.9% increase).
Figure 2. Long Term Spending Group Expenditures.
Usually low – low spending at least four years, no years with high spending, Low/Moderate – low spending in three or fewer years, no years with high spending, Sometimes high – 1 or 2 years of high spending, Often high – 3 or 4 years of high spending, Usually high – 5 or 6 years of high spending. High spending is the top 10% and low spending is the bottom 70% of annual expenditures.
An important consideration in a discussion of persistence in healthcare spending is how well individual characteristics predict future expenditures. If certain characteristics consistently predict higher medical spending, targeted case management could be implemented to defray these future costs. Table 4 shows the results of logistic regressions to determine which 2003 characteristics predicted spending in the top decile in subsequent years. Results are reported as mean marginal effects across all observations, indicating the average change in the predicted probability of high spending associated with each independent variable. Higher probability of being in the top ten percent was associated with several demographic and geographic characteristics including older age (positive linear and negative quadratic effect, but the net effect was positive throughout our sample’s age range), female gender, enrollment in a PPO in 2003, early retiree status, union membership, location in rural and higher income areas and certain census regions. Many of these factors had relatively small effects.
Table 4.
Logit Model (Mean Marginal Effects)
Dependent variable: indicator for being in the top decile of expenditures in each year, based on 2003 characteristics (All Sample)
| VARIABLES | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|
| Age | 0.00519*** (0.000132) |
0.00504*** (0.000147) |
0.00484*** (0.000145) |
0.00451*** (0.000132) |
0.00435*** (0.000163) |
| Age Squared | −3.57e-05*** (1.95e-06) |
−3.13e-05*** (2.10e-06) |
−2.77e-05*** (1.88e-06) |
−2.27e-05*** (1.68e-06) |
−1.92e-05*** (1.99e-06) |
| Gender (Male) | −0.0326*** (0.000945) |
−0.0299*** (0.000866) |
−0.0277*** (0.000742) |
−0.0244*** (0.00102) |
−0.0226*** (0.000794) |
| Region (base group West) | |||||
| Northeast | 0.00543 (0.00337) |
0.00592* (0.00318) |
0.00639** (0.00284) |
0.00640** (0.00307) |
0.00630* (0.00328) |
| North Central | 0.0117*** (0.00277) |
0.0111*** (0.00274) |
0.0111*** (0.00268) |
0.0103*** (0.00268) |
0.00801*** (0.00252) |
| South | 0.0215*** (0.00214) |
0.0174*** (0.00194) |
0.0166*** (0.00219) |
0.0155*** (0.00222) |
0.0150*** (0.00216) |
| Urban Area | −0.00853*** (0.00144) |
−0.00779*** (0.00152) |
−0.00705*** (0.00152) |
−0.00775*** (0.00135) |
−0.00713*** (0.00123) |
| Benefit Plan (base group PPO) | |||||
| HMO | −0.0236*** (0.00360) |
−0.0230*** (0.00397) |
−0.0193*** (0.00416) |
−0.0157*** (0.00345) |
−0.0127*** (0.00296) |
| POS | −0.0156*** (0.00250) |
−0.0113*** (0.00201) |
−0.00627*** (0.00191) |
−0.00343** (0.00168) |
−0.00181 (0.00190) |
| Other | −0.00815*** (0.00167) |
−0.00801*** (0.00175) |
−0.00535*** (0.00181) |
−0.00359** (0.00160) |
−0.00200 (0.00146) |
| Median HH income at zip code | 0.0868** (0.0423) |
0.101** (0.0424) |
0.0613 (0.0396) |
0.0463 (0.0397) |
0.0255 (0.0414) |
| Employee Classification: Union | 0.00759*** (0.00144) |
0.00745*** (0.00138) |
0.00707*** (0.00138) |
0.00546*** (0.00174) |
0.00550*** (0.00167) |
| Employment Status (base group: Active Full Time) | |||||
| Early Retiree | 0.0108*** (0.00107) |
0.00957*** (0.00126) |
0.00577*** (0.00101) |
0.00546*** (0.000899) |
0.00413*** (0.000874) |
| Other | 0.0145*** (0.00199) |
0.0143*** (0.00202) |
0.0152*** (0.00225) |
0.0126*** (0.00226) |
0.0126*** (0.00238) |
| Trauma occurred | 0.0389*** (0.00164) |
0.0344*** (0.00197) |
0.0345*** (0.00176) |
0.0309*** (0.00199) |
0.0341*** (0.00173) |
| Comorbidities | |||||
| Myocardial Infarction | 0.0896*** (0.00288) |
0.0716*** (0.00288) |
0.0651*** (0.00230) |
0.0598*** (0.00269) |
0.0529*** (0.00270) |
| Congestive heart failure | 0.0913*** (0.00393) |
0.0853*** (0.00333) |
0.0815*** (0.00296) |
0.0774*** (0.00326) |
0.0760*** (0.00296) |
| Peripheral vascular disease | 0.0773*** (0.00234) |
0.0645*** (0.00290) |
0.0636*** (0.00273) |
0.0597*** (0.00241) |
0.0590*** (0.00256) |
| Dementia | −0.0924*** (0.00914) |
−0.107*** (0.00852) |
−0.0913*** (0.00655) |
−0.0887*** (0.00669) |
−0.0799*** (0.00791) |
| Cerebrovascular disease | 0.0752*** (0.00239) |
0.0655*** (0.00216) |
0.0615*** (0.00168) |
0.0565*** (0.00209) |
0.0545*** (0.00209) |
| Chronic pulmonary disease | 0.0647*** (0.00151) |
0.0617*** (0.00148) |
0.0599*** (0.00139) |
0.0581*** (0.00150) |
0.0550*** (0.00144) |
| Rheumatologic disease or connective tissue disease | 0.127*** (0.00307) |
0.127*** (0.00293) |
0.122*** (0.00315) |
0.123*** (0.00310) |
0.121*** (0.00355) |
| Peptic Ulcer disease | 0.0693*** (0.00279) |
0.0671*** (0.00361) |
0.0602*** (0.00239) |
0.0562*** (0.00322) |
0.0563*** (0.00313) |
| Mild/Moderate/Severe liver disease | 0.0998*** (0.00427) |
0.0846*** (0.00420) |
0.0848*** (0.00353) |
0.0799*** (0.00418) |
0.0790*** (0.00390) |
| Moderate or severe renal disease | 0.138*** (0.00591) |
0.136*** (0.00538) |
0.141*** (0.00603) |
0.137*** (0.00687) |
0.135*** (0.00627) |
| Diabetes | 0.0789*** (0.00231) |
0.0788*** (0.00259) |
0.0790*** (0.00236) |
0.0781*** (0.00238) |
0.0767*** (0.00226) |
| Any tumor (Other Malignancy) | 0.0795*** (0.00277) |
0.0598*** (0.00222) |
0.0547*** (0.00193) |
0.0515*** (0.00176) |
0.0475*** (0.00179) |
| Metastatic solid tumor | 0.102*** (0.00303) |
0.0763*** (0.00369) |
0.0667*** (0.00476) |
0.0613*** (0.00406) |
0.0576*** (0.00299) |
| Diabetes + complications | 0.0759*** (0.00284) |
0.0709*** (0.00232) |
0.0749*** (0.00224) |
0.0725*** (0.00212) |
0.0679*** (0.00254) |
| AIDS | 0.287*** (0.0121) |
0.292*** (0.0110) |
0.291*** (0.0126) |
0.293*** (0.0132) |
0.297*** (0.0133) |
| PDG Category 1=Present | |||||
| Organic Mental Disorders / Other Psychotic Disorders (NEC, NOS) | 0.0795*** (0.00321) |
0.0745*** (0.00298) |
0.0670*** (0.00293) |
0.0645*** (0.00386) |
0.0592*** (0.00318) |
| Alcohol Use Disorders | 0.0161*** (0.00363) |
0.00582* (0.00340) |
0.00939** (0.00418) |
0.0150*** (0.00360) |
0.0175*** (0.00324) |
| Opioid and Other Substance Use Disorders | 0.0360*** (0.00208) |
0.0311*** (0.00232) |
0.0326*** (0.00210) |
0.0313*** (0.00145) |
0.0325*** (0.00145) |
| Schizophrenia Disorders | 0.0900*** (0.00749) |
0.0824*** (0.00644) |
0.0740*** (0.00673) |
0.0695*** (0.00696) |
0.0699*** (0.00736) |
| Bipolar Disorders | 0.0978*** (0.00311) |
0.0933*** (0.00316) |
0.0915*** (0.00300) |
0.0885*** (0.00239) |
0.0864*** (0.00255) |
| Major Depressions | 0.0761*** (0.00130) |
0.0694*** (0.00116) |
0.0651*** (0.00119) |
0.0627*** (0.00154) |
0.0597*** (0.00129) |
| Other Specific & Atypical Affective Disorders | 0.0505*** (0.00234) |
0.0458*** (0.00193) |
0.0455*** (0.00205) |
0.0428*** (0.00154) |
0.0380*** (0.00183) |
| Post Traumatic Stress Disorders | 0.0464*** (0.00353) |
0.0440*** (0.00357) |
0.0412*** (0.00415) |
0.0381*** (0.00365) |
0.0336*** (0.00400) |
| Anxiety Disorders (NOS) | 0.0403*** (0.00145) |
0.0370*** (0.00140) |
0.0344*** (0.00167) |
0.0324*** (0.00126) |
0.0325*** (0.00134) |
| Personality, Impulse Control, Adjustment, and Other Mental Disorders | 0.0465*** (0.000978) |
0.0423*** (0.00119) |
0.0413*** (0.000981) |
0.0393*** (0.00144) |
0.0385*** (0.00110) |
| Observations Pseudo R-squared |
2,465,152 0.132 |
2,465,152 0.122 |
2,465,152 0.117 |
2,465,152 0.111 |
2,465,152 0.107 |
Standard errors in parentheses
p<0.01,
p<0.05,
p<0.1
In terms of comorbid conditions, several notable patterns emerged. First, for most comorbidities measured in 2003, the mean marginal effect decayed monotonically and gradually as the prediction interval increased. Typically, the marginal effects for predictions of high spending five years later (in 2008) were 15–30% smaller than the marginal effects for predicting high spending one year later (in 2004). This suggests that although recent information is more predictive, considerable spending persistence is associated with most comorbidities. Second, for some comorbidities, the five year marginal effects remained nearly constant, indicating that longer-term persistence in spending associated with these conditions is as great as shorter-term persistence. These conditions, including rheumatologic conditions, renal disease, diabetes, and AIDS, tended to be chronic and often involve regular diagnostic testing and ongoing use of costly medications. Third, for another set of comorbidities (myocardial infarction, tumor, metastatic tumor), the marginal effects declined more substantially as the prediction interval lengthened. Because these conditions have high mortality rates, the declining marginal effects may simply reflect survivorship as only those patients doing relatively well remain in the sample long enough to observe spending five years later. Fourth, marginal effects for medical conditions tended to be larger than those for psychiatric conditions. AIDS has the highest marginal effects by far, and those psychiatric conditions that have relatively large marginal effects represent severe disorders (e.g., bipolar disorder, schizophrenia, major depression). Finally, the variable indicating trauma occurring in 2003 has a relatively small (compared to most medical comorbidities) marginal effect for predicting expenses one year later, as might be expected for what is arguably the clearest indicator of an acute condition in the model. However, that marginal effect decays only slightly as the prediction interval lengthens from one year to five years. This suggests that while trauma is only moderately predictive of being in the top ten percent one year later, there is an associated residual baseline cost that persists for at least five years after the initial event.
Table 5 shows mean marginal effects from an ordered logistic regression determining how predictive individual characteristics in 2003 were of spending categories. Most results are consistent with those in Table 4. These marginal effects represent percentage point changes, and for interpretation it is useful to compare them to the absolute percentage of the sample appearing in the category. For example, diabetes strongly predicted consistently high spending, as the marginal effect for being in the Usually low category is −24.5% (relative to 61.1% of the entire sample in that category) and the marginal effect for being in the Usually high category is +3.0% (relative to 2.7% of the entire sample in that category). AIDS is the most powerful predictor of consistently high spending, as the marginal effect of being in the Usually low category is −91.5%, while the effect for being in the Usually high group is +11.3%. Other illnesses with large marginal effects on being in the Usually high category include moderate or severe renal disease, rheumatologic and connective diseases, congestive heart failure, myocardial infarction, liver disease and metastatic solid tumors.
Table 5.
Ordered Logit Model (Mean Marginal Effects)
(1=Usually low, 2=Low/Moderate, 3=sometimes high, 4=Often high, 5=Usually high) All Sample
| VARIABLES | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Age | −0.0121*** (0.000270) |
0.00129*** (3.60e-05) |
0.00706*** (0.000183) |
0.00227*** (6.51e-05) |
0.00149*** (2.64e-05) |
| Age Squared | 6.23e-05*** (3.98e-06) |
−6.64e-06*** (3.60e-07) |
−3.63e-05*** (2.46e-06) |
−1.17e-05*** (7.97e-07) |
−7.67e-06*** (4.27e-07) |
| Gender (Male) | 0.0866*** (0.00154) |
−0.00922*** (0.000371) |
−0.0505*** (0.000797) |
−0.0163*** (0.000282) |
−0.0107*** (0.000315) |
| Region (base group West) | |||||
| Northeast | −0.0324*** (0.00759) |
0.00345*** (0.000834) |
0.0189*** (0.00440) |
0.00609*** (0.00141) |
0.00399*** (0.000951) |
| North Central | −0.0436*** (0.00593) |
0.00464*** (0.000565) |
0.0254*** (0.00350) |
0.00819*** (0.00114) |
0.00537*** (0.000737) |
| South | −0.0629*** (0.00516) |
0.00670*** (0.000597) |
0.0366*** (0.00297) |
0.0118*** (0.000975) |
0.00774*** (0.000680) |
| Urban Area | 0.0243*** (0.00336) |
−0.00259*** (0.000388) |
−0.0142*** (0.00198) |
−0.00456*** (0.000624) |
−0.00299*** (0.000383) |
| Benefit Plan (base group PPO) | |||||
| HMO | 0.0577*** (0.00941) |
−0.00614*** (0.00101) |
−0.0336*** (0.00550) |
−0.0108*** (0.00171) |
−0.00709*** (0.00121) |
| POS | 0.0254*** (0.00474) |
−0.00271*** (0.000471) |
−0.0148*** (0.00281) |
−0.00478*** (0.000910) |
−0.00313*** (0.000554) |
| Other | 0.0227*** (0.00392) |
−0.00242*** (0.000446) |
−0.0132*** (0.00226) |
−0.00426*** (0.000717) |
−0.00279*** (0.000502) |
| Median HH income at zip code | −0.339*** (0.0968) |
0.0361*** (0.00998) |
0.197*** (0.0567) |
0.0636*** (0.0183) |
0.0417*** (0.0119) |
| Employee Classification: Union | −0.0155*** (0.00366) |
0.00165*** (0.000416) |
0.00902*** (0.00211) |
0.00291*** (0.000676) |
0.00190*** (0.000461) |
| Employment Status (base group: Active Full Time) | |||||
| Early Retiree | −0.0160*** (0.00259) |
0.00170*** (0.000248) |
0.00931*** (0.00154) |
0.00300*** (0.000501) |
0.00197*** (0.000308) |
| Other | −0.0195*** (0.00654) |
0.00208*** (0.000668) |
0.0114*** (0.00385) |
0.00367*** (0.00124) |
0.00240*** (0.000792) |
| Trauma occurred | −0.129*** (0.00372) |
0.0138*** (0.000373) |
0.0753*** (0.00244) |
0.0243*** (0.000764) |
0.0159*** (0.000490) |
| Comorbidities | |||||
| Myocardial Infarction | −0.309*** (0.00470) |
0.0329*** (0.00116) |
0.180*** (0.00273) |
0.0581*** (0.000912) |
0.0380*** (0.00100) |
| Congestive heart failure | −0.290*** (0.00980) |
0.0309*** (0.000905) |
0.169*** (0.00629) |
0.0545*** (0.00207) |
0.0357*** (0.00120) |
| Peripheral vascular disease | −0.230*** (0.00654) |
0.0245*** (0.000579) |
0.134*** (0.00429) |
0.0433*** (0.00145) |
0.0284*** (0.000832) |
| Dementia | 0.280*** (0.0158) |
−0.0298***(0.00194) | −0.163*** (0.00919) |
−0.0526*** (0.00284) |
−0.0344*** (0.00223) |
| Cerebrovascular disease | −0.242*** (0.00551) |
0.0257*** (0.000552) |
0.141*** (0.00370) |
0.0454*** (0.00125) |
0.0297*** (0.000822) |
| Chronic pulmonary disease | −0.183*** (0.00299) |
0.0195*** (0.000477) |
0.106*** (0.00201) |
0.0343*** (0.000839) |
0.0225*** (0.000456) |
| Rheumatologic disease or connective tissue disease | −0.362*** (0.00883) |
0.0385*** (0.000920) |
0.211*** (0.00576) |
0.0680*** (0.00197) |
0.0445*** (0.00133) |
| Peptic Ulcer disease | −0.231*** (0.00629) |
0.0246*** (0.000649) |
0.135*** (0.00404) |
0.0434*** (0.00148) |
0.0284*** (0.000768) |
| Mild/Moderate/Severe liver disease | −0.290*** (0.00844) |
0.0309*** (0.00101) |
0.169*** (0.00517) |
0.0545*** (0.00170) |
0.0357*** (0.00134) |
| Moderate or severe renal disease | −0.407*** (0.0160) |
0.0434*** (0.00178) |
0.237*** (0.00957) |
0.0765*** (0.00301) |
0.0501*** (0.00241) |
| Diabetes | −0.245*** (0.00640) |
0.0261*** (0.000617) |
0.143*** (0.00406) |
0.0461*** (0.00149) |
0.0302*** (0.000950) |
| Any tumor (Other Malignancy) | −0.219*** (0.00599) |
0.0234*** (0.000556) |
0.128*** (0.00392) |
0.0412*** (0.00123) |
0.0270*** (0.000896) |
| Metastatic solid tumor | −0.253*** (0.00859) |
0.0269*** (0.000995) |
0.147*** (0.00520) |
0.0475*** (0.00170) |
0.0311*** (0.00128) |
| Diabetes + complications | −0.230*** (0.00649) |
0.0245*** (0.00111) |
0.134*** (0.00390) |
0.0432*** (0.00125) |
0.0283*** (0.000777) |
| AIDS | −0.915*** (0.0332) |
0.0974*** (0.00387) |
0.533*** (0.0201) |
0.172*** (0.00613) |
0.113*** (0.00507) |
| PDG Category 1=Present | |||||
| Organic Mental Disorders / Other Psychotic Disorders (NEC, NOS) | −0.227*** (0.00763) |
0.0241*** (0.00117) |
0.132*** (0.00435) |
0.0425*** (0.00127) |
0.0279*** (0.00126) |
| Alcohol Use Disorders | −0.0792*** (0.00641) |
0.00843*** (0.000734) |
0.0461*** (0.00370) |
0.0149*** (0.00119) |
0.00974*** (0.000862) |
| Opioid and Other Substance Use Disorders | −0.145*** (0.00674) |
0.0154*** (0.000630) |
0.0844*** (0.00417) |
0.0272*** (0.00147) |
0.0178*** (0.000681) |
| Schizophrenia Disorders | −0.252*** (0.0144) |
0.0268*** (0.00180) |
0.147*** (0.00837) |
0.0473*** (0.00253) |
0.0310*** (0.00205) |
| Bipolar Disorders | −0.285*** (0.00715) |
0.0303*** (0.00111) |
0.166*** (0.00430) |
0.0535*** (0.00129) |
0.0351*** (0.00125) |
| Major Depressions | −0.201*** (0.00259) |
0.0214*** (0.000742) |
0.117*** (0.00134) |
0.0377*** (0.000663) |
0.0247*** (0.000592) |
| Other Specific & Atypical Affective Disorders | −0.141*** (0.00387) |
0.0150*** (0.000737) |
0.0821*** (0.00204) |
0.0265*** (0.000696) |
0.0173*** (0.000650) |
| Post Traumatic Stress Disorders | −0.132*** (0.00769) |
0.0141*** (0.000956) |
0.0772*** (0.00445) |
0.0249*** (0.00153) |
0.0163*** (0.000941) |
| Anxiety Disorders (NOS) | −0.123*** (0.00348) |
0.0131*** (0.000675) |
0.0715*** (0.00175) |
0.0230*** (0.000651) |
0.0151*** (0.000589) |
| Personality, Impulse Control, Adjustment,and Other Mental Disorders | −0.140*** (0.00262) |
0.0149*** (0.000636) |
0.0815*** (0.00123) |
0.0263*** (0.000525) |
0.0172*** (0.000528) |
| Observations Pseudo R-squared |
2,465,152 0.120 |
2,465,152 0.120 |
2,465,152 0.120 |
2,465,152 0.120 |
2,465,152 0.120 |
Standard errors in parentheses
p<0.01,
p<0.05,
p<0.1
1. Usually low – low spending at least four years, no years with high spending, Low/Moderate – low spending in three or fewer years, no years with high spending, Sometimes high – 1 or 2 years of high spending, Often high – 3 or 4 years of high spending, Usually high – 5 or 6 years of high spending. High spending is the top 10% and low spending is the bottom 70% of annual expenditures.
Sample Attrition
Several factors predicted attrition from MarketScan prior to the end of the six-year period. First, average annual attrition rates for employees without dependents were 2.4 percentage points higher (15.1%) than those with dependents (12.7%). Second, there were offsetting trends with respect to health spending. Employees with higher spending were more likely to leave the sample, consistent with the expectation that their health conditions impair their ability to maintain employment. Employees in the highest quartile of spending were approximately 2.5 percentage points per year more likely to leave than those in the lowest quartile of spending. Conversely, as dependent spending rose, employees were less likely to leave the sample annually. Employees with dependents in the highest quartile of spending were 2 percentage points less likely to leave the sample than employees with dependents in the lowest quartile of spending. This is consistent with retention of coverage being more important for employees whose dependents are high care users. The extent to which attrition by health status affects our findings depends on the net effect of these offsetting forces. The fact that these attrition trends are of similar magnitude and opposite sign provides some assurance that inferences drawn about spending persistence in the working age population as a whole may not differ drastically from those based on a continuously enrolled population. To further test the extent to which prior health spending influences attrition, we estimated a logistic regression model predicting attrition as a function of prior spending, controlling for employee characteristics, plan type and region. Prior spending only modestly predicted attrition (adjusted odds ratio 1.008 per $1000 higher spending, suggesting that our estimates of persistence based on continuous enrollees may not differ substantially from estimates for an employer-based sample that could track spending after separation from the initial employer. Nonetheless, the findings reported here apply directly only to under-age 65 persons with stable ESI, and generalizations to broader populations such all persons with ESI at a point in time or the entire under 65 population may still be subject to selection biases.
Discussion
By using recent data for a large, under-65 population with a six year observation period, this study adds considerably to our knowledge of long-term health spending patterns at exactly the time when the country is implementing various health reforms. In terms of the broad question of how persistent health spending is over time, different observers may interpret our findings in different ways. Nonetheless, we believe that several conclusions can be drawn. Although individuals’ positions within the spending distribution vary over time, considerable persistence exists. This is particularly clear at the lower end of the spending distribution. Over the six-year period, 69.8% of enrollees never appeared in the top 10% of the annual spending distribution, and even over this long time frame, the bottom 50% of spenders accounted for less than 10% of total spending.
Persistence at the top of the distribution is also considerable. Of those in the top 10% in 2003, 43.4% remained in the top 10% one year later. This probability declined gradually in subsequent years, but even five years later, 34.4% of the top spenders in 2003 were still in the top 10%. The concentration of spending over the six-year period among the very highest spenders (top 1%) remains high (14% of spending), though notably lower than the one year concentration (24% of spending in 2008). Many enrollee characteristics and clinical conditions retained much of their predictive power for spending five years in the future (relative to their predictive power for spending the next year). Nonetheless, it is also clear that there exists quite a bit of mobility in who enters the top 10% of the spending distribution in any given year. Consistent with earlier research using the 2-year MEPS panels (Monheit, 2003; Cohen and Yu, 2012), mobility is evident in the short-term as more than half of those in the top 10% of the distribution in one year are not in the top 10% the following year. This study demonstrates mobility over the longer-term, with three quarters of those who ever appear in the top 10% of annual spending do so only once or twice over six years.
The CDHP plan structure increases the salience of information about spending persistence relative to traditional plan designs which do not roll over unused funds or generate incentives to move care across plan years based on year-to-date and anticipated spending relative to a high deductible. Understanding the degree of persistence in spending overall and as a function of demographics and comorbid conditions, allows the individual to anticipate spending over the coming years based on previous spending patterns and respond by adjusting contributions to their HSA, HRA or other savings. Individuals with low spending can anticipate a low likelihood of large expenses over the subsequent five years. In the rare high spending year they may take advantage of low cost-sharing rates in excess of the deductible, and may opt to undertake discretionary spending. In most years these low spending individuals may not need to make large contributions to an HSA or HRA.
The concentration of long-term medical spending documented in this study supports the use of disease-management, particularly for those with the conditions that remained strong predictors of high spending throughout the five year follow-up period. Many characteristics measured in 2003 retained long-term predictive power with regard to future spending, including age, gender, and a variety of medical conditions. These data provide a way to further delineate individuals who may benefit from disease-management. The PPACA also addresses this issue with the development of Accountable Care Organizations (ACOs), giving physicians incentives and a foundation upon which to coordinate care across providers. Further, the medical home model provides another way to coordinate care for individuals with illnesses that predispose them to recurring medical expenditures. Focusing these efforts to address the relatively small set of individuals with consistently high costs (e.g., the 10 percent of the population that accounts for half of all spending over a six-year horizon) could lead to substantial reductions in overall medical expenditures in both the short- and the long-term.
Our categorizations of six-year spending ranged from Usually low to Usually high, based on the number of years spent in either the high (top 10%) or low (bottom 70%) ends of the spending distribution. Comparing the characteristics most prevalent among those in each category allows us to paint a better picture of the makeup of individuals who were consistently high spenders. Those in the top 10% for at least five of the six years were more likely to be from the North Central or South regions, female and older. This regional variation may be indicative of regional differences in care delivery and how people approach medical utilization, or overall health status. Insurance plan types also seem to play a role in costs incurred, as PPOs were more prevalent in the higher spending groups. This may be indicative of either increased moral hazard in less managed plans, or individuals selecting such plans knowing that they will frequently use the medical system. The greater degree of persistence at both ends of the spending distribution decreases the utility gained from insurance for these populations and undermines the function of insurance markets through the increased potential for adverse selection and cream-skimming (Breyer, Bundorf, & Pauly, 2011). This raises concerns regarding the participation of low-cost individuals in insurance exchanges. Therefore, the sorts of case-mix adjustment or reinsurance mechanisms contained in the PPACA may be necessary to ensure that health plans offered on the exchanges compete primarily on the basis of value and quality rather than risk avoidance. However, the high persistence seen at the low end of the spending distribution may be a greater concern given the legislation’s limits on premium adjustments for age and other factors and the relatively modest initial penalties for failing to satisfy the individual coverage mandate. The fraction of these low cost consumers who opt out of the system will be a key determinant of premiums charged to those with high cost conditions.
This work has several limitations. First, MarketScan only includes employees and dependents of the large firms that are clients of TruvenHealth. Although the MarketScan database is the same one used by CMS to calibrate its risk-adjustment model for the health exchanges (Patient Protection and Affordable Care Act, 2014), these data should not be interpreted as representative of the entire under-65 US population or of the previously uninsured who are seeking coverage through the ACA’s health exchanges. Second, our simple categorization of spending patterns abstracts away from some potentially interesting features of the data (e.g., is a person’s spending rising or falling, are their high cost years adjacent or scattered?) that could be explored in further research. Third, the models predicting future high spending at the individual level had limited predictive power, reflecting the high degree of unpredictable variation inherent to healthcare spending data. Fourth, requiring six years of continuous enrollment creates attrition bias to the extent that attrition is affected by health, an issue largely ignored by prior studies of longer-term spending persistence. No compelling instrumental variable or exclusion restriction is available to allow us to generalize directly to the broader population of all workers holding ESI at a point in time or all persons under age 65. Therefore, our results should be interpreted as reflective of spending patterns among a population that maintains ESI over a six year timeframe. However, attrition due to mortality is less important in the under-65 population than in the Medicare population. Further, in our sample, high spending employees were more likely to exit before six years but high spending dependents were more likely to stay. On net, spending only modestly predicted attrition. Likewise, better understanding of cost-patterns among long-term employees is significant in its own right. Many of the interventions that might influence cost trajectories (e.g., workplace wellness programs, disease management, value-based insurance design incentives for care of chronic conditions) are likely to have larger returns over a longer time horizon. Therefore, from an employer perspective such interventions would be most valuable in the segment of the employee population that remains enrolled over the longer-term.
References
- Aizcorbe A, Liebman E, Pack S, Cutler DM, Chernew ME, Rosen AB. Measuring health care costs of individuals with employer-sponsored health insurance in the U.S.: A comparison of survey and claims data. Statistical Journal of the IAOS. 2012;28:43–51. doi: 10.3233/SJI-2012-0743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breyer F, Bundorf MK, Pauly MV. Health care spending risk, health insurance, and payment to health plans. In: Pauly MV, Mcguire TG, Barros PP, editors. Handbook of Health Economics, Vol 2. Elsevier; 2011. pp. 691–762. [Google Scholar]
- Chapman JD. Biased Enrollment and Risk Adjustment for Health Plans (Doctoral dissertation) Cambridge: Harvard University; 1997. [Google Scholar]
- Cohen SB, Yu W. The concentration and persistence in the level of health expenditures over time: Estimates for the U.S. population, 2009–2010. Agency for Health Care Research and Quality Statistical Brief #392. 2012 downloaded on June 4, 2013 from http://meps.ahrq.gov/mepsweb/data_files/publications/st392/stat392.pdf.
- Congressional Budget Office (CBO) Lessons from Medicare’s demonstration projects on disease management, care coordination, and value-based payment. Washington, DC: Congressional Budget Office; 2012. [Google Scholar]
- Eichner MJ, McClellan MB, Wise DA. Health expenditure persistence and the feasibility of medical savings accounts. In: Poterba JM, editor. Tax Policy and the Economy, Volume 11. Cambridge, MA: MIT Press; 1997. pp. 91–128. [Google Scholar]
- Garber AM, MaCurdy TE, McClellan MB. Persistence of Medicare expenditures among elderly Medicare beneficiaries. In: Garber AM, editor. In Frontiers in Health Policy Research. Cambridge MA: MIT Press; 1998. pp. 154–178. [Google Scholar]
- Gawande A. The hot spotters: Can we lower medical costs by giving the neediest patients better care? New Yorker. 2011 Jan 24;:41–51. [PubMed] [Google Scholar]
- Kaiser Family Foundation, Health Research and Educational Trust (HRET) Employer Health Benefits: 2008 Annual Survey. Menlo Park, CA: KFF; 2008. Retrieved from http://kaiserfamilyfoundation.files.wordpress.com/2013/04/7790.pdf. [Google Scholar]
- Kaiser Family Foundation, Health Research and Educational Trust (HRET) Employer Health Benefits: 2012 Annual Survey. Menlo Park, CA: KFF; 2012. Retrieved from http://kff.org/private-insurance/report/employer-health-benefits-2012-annual-survey/ [Google Scholar]
- Kohn JL, Liu JS. The dynamics of medical care use in the British Household Panel Survey. Health Economics. 2013;22:687–710. doi: 10.1002/hec.2845. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Medicare and the Health Care Delivery System. 2012 [Google Scholar]
- Monheit AC. Persistence in health expenditures in the short run: Prevalence and consequences. Medical Care. 2003;41(7) Suppl:III-53–III-64. doi: 10.1097/01.MLR.0000076046.46152.EF. [DOI] [PubMed] [Google Scholar]
- Patient Protection and Affordable Care Act. HHS Notice of Benefit and Payment Parameters for 2015, 79(47) Federal Register. 2014 Mar 11; Retrieved from http://www.gpo.gov/fdsys/pkg/FR-2014-03-11/pdf/2014-05052.pdf. [PubMed]
- Pauly MV, Kunreuther H, Hirth R. Guaranteed renewability in insurance. Journal of Risk and Uncertainty. 1995;10:143–156. [Google Scholar]
- Pauly MV, Zeng Y. Forum for Health Economics and Policy. Vol. 7. Berkeley, CA: Berkeley Electronic Press; 2004. Adverse selection and the challenges to Stand-Alone Prescription Drug Insurance. [DOI] [PubMed] [Google Scholar]
- Riley GF. Long-term trends in the concentration of Medicare spending. Health Affairs. 2007;26(3):808–816. doi: 10.1377/hlthaff.26.3.808. [DOI] [PubMed] [Google Scholar]