Abstract
Background
Enterobius vermicularis infection is a prevalent intestinal parasitic disease in children. In this study, we explored the epidemiological status and risk factors for E. vermicularis infection in children in southern China.
Methods
A cross-sectional survey was carried out in Gaozhou city, Guangdong province, China, in December 2011. Children aged 2–12 years from five schools participated in the study. The adhesive cellophane-tape perianal swab method was applied to detect E. vermicularis infection, while a questionnaire was sent to each child’s guardian(s) to collect demographic and socioeconomic data, as well as hygiene behaviors, pertaining to each child. Univariate and multivariate logistic regression analyses were performed to capture the potential risk factors.
Results
Out of the 802 children surveyed, 440 were infected with E. vermicularis, with an average prevalence of 54.86 %, and a range from 45.96 to 68.13 %. The age variable was found to be statistically significant, whereas the sex variable was not. It was found that a mother’s education level (low) and not washing hands before dinner were major risk factors in all children (802). After stratification by age, a father’s education level (primary or below) and biting pencils (or toys) were significant risk factors in the younger children (508), while not washing hands before dinner and playing on the ground were important risk factors in the older children (294).
Conclusion
This study demonstrates the prevalence of E. vermicularis infection in children in Gaozhou and reveals underlying risk factors. Most importantly, it reveals that risk factors differ among the different age groups, which indicates that different control measures targeted at particular age groups should be implemented.
Electronic supplementary material
The online version of this article (doi:10.1186/s40249-015-0058-9) contains supplementary material, which is available to authorized users.
Keywords: Enterobius vermicularis, Prevalence, Risk factor, Children, China
Multilingual abstracts
Please see Additional file 1 for translations of the abstract into the six official working languages of the United Nations.
Background
Enterobius vermicularis infection causes enterobiasis, which is among the most prevalent parasitic diseases in children. The infection is prevalent throughout the world, including in developed countries [1–7], and it is estimated that 4–28 % of children are infected globally [8]. However, less attention has been paid to E. vermicularis infection because the symptoms of enterobiasis are seemingly not very severe. It is usually endemic in overcrowded conditions, such as kindergartens and primary schools, due to the easy transmission from infected to uninfected children.
Some people with E. vermicularis infection are asymptomatic, while others, especially children, may present with perianal pruritus, restlessness, loss of appetite, insomnia, and irritability [9–11]. Particularly, mental development in infected children lags behind their peers due to prolonged and heavy infection [12]. It has also been reported that in some rare cases, E. vermicularis may penetrate into kidneys and fallopian tubes, which causes ectopic enterobiasis and leads to severe health disorders and even death [13, 14].
According to the 2004 national parasitic survey, an average prevalence of E. vermicularis infection in children reached 10.28 % in China, with the highest prevalence rates in Hainan (42.64 %), Gansu (33.27 %), and Guangdong (30.38 %) [15]. Due to the recent rapid economic development and improvements in hygiene in Guangdong, the prevalence of three species of soil-transmitted helminthiases (ascariasis, trichuriasis, and hookworm disease) have decreased to a low level, but the prevalence of E. vermicularis infection is still high [16, 17]. Although many studies have been done to explore the risk factors for E. vermicularis infection [11, 18], related research in China is rare. However, these risk factors need to be identified in order to improve control activities. We carried out a cross-sectional survey to understand the current situation and risk factors for E. vermicularis infection in Gaozhou city, Guangdong province, southern China.
Methods
Study design
This study was conducted in Gaozhou city, Guangdong province, southern China, which has a population of near 1.3 million. Five schools were willing to participate in the survey, with two schools located in urban and three in rural areas. Children born between 1999 and 2009 were enrolled. The adhesive cellophane-tape perianal swab method was applied to detect the eggs of E. vermicularis. A structured questionnaire was distributed to the guardian(s) of each child in order to explore the risk factors for E. vermicularis infection.
Detection of E. vermicularis infection
The sticky side of the transparent cellophane tape was stuck to the child’s anus between 08:00 and 09:00 in the morning. Then, the tape was removed and attached to a glass slide. Collected samples were transported to the Gaozhou Center for Disease Control and Prevention and examined under light microscopy. To increase the sensitivity, the same detection procedure was performed on three continuous days.
Questionnaire survey
The questionnaire included questions pertaining to the basic demography of the child and her/his parents, personal hygiene and clinical symptoms of the child, as well as the family’s socioeconomic status (see Additional file 2). The basic demography section asked such things as father’s education and vocation, mother’s education and vocation, annual income of household, parents’ knowledge about controlling parasitic diseases, and so on. The children’s personal hygiene habits section wanted to find out about certain behaviors, including washing hands before dinner, washing hands after toilet use, sucking fingers, biting pencils (toys), residual dirt in fingernails, playing on the ground, washing hands after games, and playing with soil. Information about taking anthelmintics in past six months was also collected. Four related symptoms of the E. vermicularis infection, namely bruxism, night terrors, enuresis, and scratching the anus, were documented.
Data analysis
Only when 90 % of each questionnaire was completed, could the data be included for analysis. Data were analyzed using the SPSS software (Version 20.0, IBM Corp., Armonk, New York). Firstly, a univariate logistic regression analysis was performed for each potential risk factor. Secondly, those variables with a p-value less than 0.1 were brought into the multivariate logistic regression model. Odds ratios (ORs) and 95 % confidence intervals (95 % CIs) were determined. Due to the significant difference of prevalence in ages, the children were divided into a younger age group (preschool children, under seven years of age) and an older age group (primary school children, aged seven years or above). Corresponding analyses were run again for each age group.
Ethical considerations
The study was approved by the Ethical Review Committee of the National Institute of Parasitic Diseases, Chinese Center for Disease Control and Prevention (reference no. 2011–006). The study’s purpose, procedure, and potential risks and benefits were explained to the director and teachers of each school. It was the teachers’ responsibility to explain the study to the children’s guardians, after which a written consent was obtained from the guardian of each child. After the survey, the results were fed back to the guardians.
Results
Epidemiological status
A total of 825 children participated in the survey, 23 of which were excluded because over 10 % of data pertaining to them was unfounded. The overall prevalence of E. vermicularis infection was 54.86 % (440/802, 95 % CI: 51.42–58.31 %). The prevalence ranged from 45.96 % (74/161, 95 % CI: 38.26–53.66 %) to 68.13 % (109/160, 95 % CI: 60.90–75.35 %) in the five schools (χ2 = 19.212, p = 0.001) (see Table 1).
Table 1.
The prevalence of Enterobius vermicularis infection in the study participants, by schools
| Schools | No. of examined | No. of infected | Prevalence (%) |
|---|---|---|---|
| Changpo | 172 | 96 | 55.81 |
| Caojiang | 158 | 88 | 55.70 |
| Shankou | 160 | 109 | 68.13 |
| Hongfen | 151 | 73 | 48.34 |
| Boyu | 161 | 74 | 45.96 |
| Total | 802 | 440 | 54.86 |
The prevalence in children from urban areas was 51.05 % (170/333, 95 % CI: 45.68–56.42 %), while it was 57.57 % (270/469, 95 % CI: 53.10–62.04 %) in children from rural areas. However, the difference was not statistically significant (χ2 = 3.341, p = 0.068).
Of the 802 children, 480 were boys and 322 were girls. The prevalence in boys and girls was 55.63 % (267/480, 95 % CI: 51.18–60.07 %) and 53.73 % (173/322, 95 % CI: 48.28–59.17 %), respectively, which points to no significant difference (χ2 = 0.280, p = 0.596). A significant difference was observed, however, among the different age groups, with prevalence peaking in children aged four (χ2 = 27.190, p = 0.002; see Fig. 1).
Fig. 1.
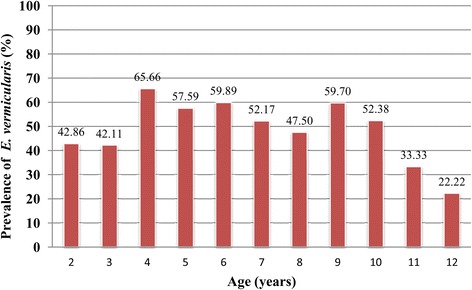
The prevalence of Enterobius vermicularis infection, by age groups
Risk factors for E. vermicularis infection
The results of the associations between each variable and E. vermicularis infection are shown in Table 2. Variables such as age, mother’s education, and washing hands before dinner were found to be significant risk factors. The younger children (two to six years of age) were more likely to be infected than older children (seven to twelve years of age) (OR = 1.63, 95 % CI: 1.20–2.20). Children who had mothers with low education levels had an OR of 1.50 times (95 % CI: 1.09–2.07) higher of being infected with E. vermicularis, while those who did not wash their hands before dinner had an OR of 1.52 (95 % CI: 1.02–2.28) higher.
Table 2.
Results of logistical regression analyses of risk factors and Enterobius vermicularis infection in the study participants
| Variables | No. of positive (%) | OR (95 %CI) a | OR (95 %CI) b | Variables | No. of positive (%) | OR (95 %CI) a | OR (95 %CI) b |
|---|---|---|---|---|---|---|---|
| Age group (years) | Washing hands before dinner | ||||||
| 7 to 12 (n = 294) | 145 (49.32) | 1.00 | 1.00 | Yes (n = 671) | 359 (53.50) | 1.00 | 1.00 |
| 2 to 6 (n = 508) | 295 (58.07) | 1.42 (1.07–1.90) c | 1.63 (1.20–2.20)* | No (n = 131) | 81 (61.83) | 1.41 (0.96–2.07) c | 1.52(1.02–2.28)* |
| Sex | Washing hands after toilet use | ||||||
| Boys (n = 480) | 267 (55.63) | 1.00 | – | Yes (n = 584) | 321 (54.97) | 1.00 | – |
| Girls (n = 322) | 173 (53.73) | 0.93 (0.70–1.23) | No (n = 214) | 115 (53.74) | 0.95 (0.70–1.30) | ||
| Father’s education | Sucking fingers | ||||||
| Middle school and above (n = 297) | 153 (51.52) | 1.00 | – | Yes (n = 145) | 79 (54.48) | 1.00 | – |
| Primary school and below (n = 505) | 287 (56.83) | 1.24 (0.93–1.65) | No (n = 656) | 361 (55.03) | 1.02 (0.71–1.47) | ||
| Father’s floating in and out of jobsd | Biting pencils (or toys) | ||||||
| No (n = 440) | 232 (52.73) | 1.00 | – | No (n = 640) | 343 (53.59) | 1.00 | – |
| Yes (n = 362) | 208 (57.46) | 1.21 (0.92–1.60) | Yes (n = 161) | 97 (60.25) | 1.31 (0.92–1.87) | ||
| Mother’s education | Residual dirt in fingernails | ||||||
| Middle school and above (n = 215) | 103 (47.91) | 1.00 | 1.00 | Yes (n = 347) | 194 (55.91) | 1.00 | – |
| Primary school and below (n = 587) | 337 (57.41) | 1.47 (1.07–2.01) c | 1.501 (1.09–2.07)* | No (n = 454) | 246 (54.19) | 0.93 (0.70–1.24) | |
| Mother’s floating in and out of jobsd | Playing on the ground | ||||||
| No (n = 545) | 288 (52.84) | 1.00 | – | No (n = 457) | 250 (54.70) | 1.00 | – |
| Yes (n = 257) | 152 (59.14) | 1.29 (0.96–1.74) c | Yes (n = 345) | 190 (55.07) | 1.02 (0.77–1.34) | ||
| Annual income of household | Washing hands after playing/games | ||||||
| >15,000 RMB (n = 237) | 131 (55.27) | 1.00 | – | Yes (n = 451) | 253 (56.10) | 1.00 | – |
| ≤15,000 RMB (n = 565) | 309 (54.69) | 0.98 (0.72–1.33) | No (n = 348) | 186 (53.45) | 0.90 (0.68–1.19) | ||
| Brought up by parents | Playing with/in soil | ||||||
| Yes (n = 406) | 215 (52.96) | 1.00 | - | Yes (n = 430) | 241 (56.05) | 1.00 | – |
| No (n = 396) | 225 (56.82) | 1.170 (0.89–1.54) | No (n = 372) | 199 (53.49) | 0.90 (0.68–1.19) | ||
| Parents‘ knowledge about controlling parasitic diseases | Taking anthelmintics in past six months | ||||||
| Yes (n = 535) | 296 (55.33) | 1.00 | - | Yes (n = 256) | 132 (51.56) | 1.00 | – |
| No (n = 262) | 141 (53.82) | 0.94 (0.70–1.27) | No (n = 534) | 300 (56.18) | 1.20 (0.89–1.62) | ||
OR odds ratio, 95 %CI 95 % confidence interval
* p < 0.05
a Result in univariate logistic regression analysis. b Result in multivariate logistic regression analysis. c Variables entering the multivariate logistic regression analysis (p < 0.1 in univariate logistic regression analysis). d This signifies people who were previously employed in agriculture that leave their hometowns for another developed city and take a temporary job there to earn money
After stratification by age group, it was found that risk factors associated with E. vermicularis infection were different between younger and older children (see Table 3). In the younger group, children with fathers who had a primary level of education or below and who bit pencils (or toys) had a higher risk of E. vermicularis infection. Compared to the children whose fathers had higher education levels, children whose fathers had low education levels were 1.73 times (95 % CI: 1.20–2.50) more likely to be infected with E. vermicularis, and children who bit pencils (or toys) were 1.61 times (95 % CI: 1.01–2.58) more likely to be infected than children who did not. In the older age group, not washing hands before dinner and playing on the ground were the major risk factors. Compared to the children who washed their hands before dinner, children who didn’t had an OR of 1.97 (95 % CI: 1.16–3.35) times higher of being infected with E. vermicularis. If children played on the ground, the risk of contracting E. vermicularis infection increased by 1.65 (95 % CI: 1.02–2.66) times.
Table 3.
Results of multivariate logistic regression analysis of risk factors and Enterobius vermicularis infection, by age groups
| Age group | Variables | No. of examined | No. of positive (%) | OR (95 %CI) a |
|---|---|---|---|---|
| 2–6 years | Father’s education | |||
| Middle school and above | 216 | 109 (50.46) | 1.00 | |
| Primary school and below | 292 | 186 (63.70) | 1.73 (1.20–2.50)* | |
| Biting pencils (or toys) | ||||
| No | 405 | 227 (56.05) | 1.00 | |
| Yes | 102 | 68 (66.67) | 1.61 (1.01–2.58)* | |
| 7–12 years | Washing hands before dinner | |||
| Yes | 212 | 96 (45.28) | 1.00 | |
| No | 82 | 49 (59.76) | 1.97 (1.16–3.35)* | |
| Playing on the ground | ||||
| No | 126 | 55 (43.65) | 1.00 | |
| Yes | 168 | 90 (53.57) | 1.65 (1.02–2.66)* | |
OR odds ratio, 95 %CI 95 % confidence interval
*p < 0.05
a Result in multivariate logistic regression analysis
Clinical symptoms
Four related symptoms of the infection, namely bruxism, night terrors, enuresis, and scratching the anus, were found in the study participants. However, the symptoms were recorded both in children with and without E. vermicularis infection and no significant differences were observed.
Discussion
This study found that the prevalence of E. vermicularis infection in children was 54.86 % in Gaozhou, which is relatively high for China [19]. It is higher than the average level of E. vermicularis infection observed in Guangdong in 2004 [15] and it is also higher than the rate of soil-transmitted helminthiases in Gaozhou [16, 20]. Thus, it can be concluded that E. vermicularis infection is still an important parasitic disease in Gaozhou. Significant statistical difference was observed in the age variable, but not in the sex variable. The prevalence of infection was higher in the younger age group, which is consistent with the fact that younger children might be less self-aware and might not be able to self-manage. The prevalence was not significantly significant among the sexes, however, which is in line with the similarities in behavior in children of different sexes in the same environment.
In this study, several risk factors were found to be associated with a high prevalence of E. vermicularis infection. It was observed that E. vermicularis infection in children is related to not washing hands before dinner; children who washed their hands before dinner were at a significantly lower risk of contracting E. vermicularis infection than those who did not. This was similar to a finding in a previous report [6]. Furthermore, parents’ education levels also played an important role. Children whose mothers had low education levels had a higher risk of infection and only about a quarter of the children had mothers who had higher education levels. A study in Korea showed that parents’ knowledge about enterobiasis is correlated with the incidence of the disease in their children [11]. Combined with our findings, it can be suggested that children’s education at home needs to be strengthened in order to control enterobiasis. In addition, many children’s parents leave their hometowns to work and earn money in bigger cities (see data in Table 2: father/mother’s floating in and out of jobs), and thus some children are taken care of by their grandparents or others. Although no significant difference was found for this factor, it should be kept in mind and studied further.
It is interesting but not inconceivable that risk factors for E. vermicularis infection are different among the different age groups. For example, our study found that biting pencils (or toys) contributed to a higher risk factor in the younger age group, and not washing hands before dinner and playing on the ground contributed to a higher risk factor among the older age group. Taking into consideration children’s behavior at different ages, this makes sense. Biting things is more prevalent in younger children, who wouldn’t necessarily be allowed to play on the ground by themselves and whose hands would frequently be cleaned by their guardians. In contrast, older children would be allowed to play independently and thus come into contact with contaminated environments more frequently. As well as that, their parents and teachers are not as likely to help them clean their hands. We can assume that the risk of infection increases due to obvious behaviors in children, but these are easily overlooked. Thus, intervention measures should be targeted specifically to the different age groups in order to control enterobiasis. For example, parents and teachers should not only ask older children to adhere to personal hygiene practices, but also strengthen and increase supervision. For younger children, guardians should pay closer attention to cleaning pencils and toys, and prohibit their children to bite things.
Although our study has found some new and important risk factors, these alone don’t completely contribute to the high prevalence of E. vermicularis infection in Gaozhou. It is well known that anthelmintic therapy is the most effective approach to control E. vermicularis infection [21–23]. The ideal therapeutic strategy is massive chemotherapy and repeated medication [24, 25]. However, this study found that no mass-scale chemotherapy has been carried out in any school in the past year (data were collected from the director of each school). Approximately two-thirds of the children have never taken drugs for E. vermicularis infection in the past six months. It is therefore reasonable to conclude that this high prevalence is partially attributable to this factor. Re-infection is another important contributor. The lifecycle of E. vermicularis is very simple and it only takes two to four weeks for the eggs to develop into an adult worm [10]. The eggs of E. vermicularis can contaminate school materials, toys, door handles, desks, chairs, and even dust [26]. Children are susceptible to E. vermicularis infection through intimate contact with the contaminated environment and infected children [25, 27]. Thus, a high prevalence still presents in those taking anthelmintics because of rapid re-infection.
This study had some limitations and it is recommended that these are avoided in future studies. Firstly, as a cross-sectional survey, the actual relationship between cause and effect could not be ascertained [28], although the observed risk factors highlight risk of exposure, which benefits the control. Secondly, as E. vermicularis infection is an important parasitic disease, family aggregation should be explored, which was not done so in this study. Exploring this in future studies can further guide control measures.
Conclusion
Enterobius vermicularis infection is still an important health problem in children in Gaozhou and targeted interventions are imminently needed. These interventions should integrate different measures. Firstly, massive or selective chemotherapy is important in order to decrease high prevalence rates and control the infection source. Secondly, health education should be carried out targeting children, parents, other guardians, and teachers. The difference in risk factors among different age groups urges the adoption of interventions targeted at specific age groups. Taking into consideration the high re-infection rates in collective environments such as kindergartens and primary schools, environmental hygiene should also be emphasized.
Additional files
Multilingual abstracts in the six official working languages of the United Nations.
Content and options of the questionnaire.
Acknowledgements
We thank the technical staff at the Guangdong and Gaozhou Centers for Disease Control and Prevention for their assistance in our fieldwork. This study was supported by the fund of GlaxoSmithKline (Tianjin) R&D Co., Ltd, Tianjin, China.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
HML, CHZ, TJZ, LQX, and YDC contributed to the design of the study. HML, CHZ, ZSL ZHD, CWR, and QMZ implemented the fieldwork. HML and CHZ collected the data and wrote the paper. All authors read and approved the final paper.
Contributor Information
Hong-Mei Li, Email: angela0736@hotmail.com.
Chang-Hai Zhou, Email: zhouchanghai2005@126.com.
Zhi-Shi Li, Email: gzcdcwww@163.com.
Zhuo-Hui Deng, Email: tracydzh@163.com.
Cai-Wen Ruan, Email: 1355874775@qq.com.
Qi-Ming Zhang, Email: 798234076@qq.com.
Ting-Jun Zhu, Email: ztjren@163.com.
Long-Qi Xu, Email: xlongqi@yahoo.com.cn.
Ying-Dan Chen, Email: cyingdan@126.com.
References
- 1.Chang TK, Liao CW, Huang YC, Chang CC, Chou CM, Tsay HC, et al. Prevalence of Enterobius vermicularis Infection among preschool children in kindergartens of Taipei City, Taiwan in 2008. Korean J Parasitol. 2009;47:185–7. doi: 10.3347/kjp.2009.47.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Remm M, Remm K. Effectiveness of repeated examination to diagnose enterobiasis in nursery school groups. Korean J Parasitol. 2009;47:235–41. doi: 10.3347/kjp.2009.47.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matthys B, Bobieva M, Karimova G, Mengliboeva Z, Jean-Richard V, Hoimnazarova M, et al. Prevalence and risk factors of helminths and intestinal protozoa infections among children from primary schools in western Tajikistan. Parasit Vectors. 2011;4:195. doi: 10.1186/1756-3305-4-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neghina R, Dumitrascu V, Neghina AM, Vlad DC, Petrica L, Vermesan D, et al. Epidemiology of ascariasis, enterobiasis and giardiasis in a Romanian western county (Timis), 1993–2006. Acta Trop. 2013;125:98–101. [DOI] [PubMed]
- 5.Dutto M, Montu D, Raineri G. Enterobiasis in pediatric subjects in north-western Italy: a study of home remedies. Ann Ig. 2012;24:81–4. [PubMed] [Google Scholar]
- 6.Remm M. Distribution of enterobiasis among nursery school children in SE Estonia and of other helminthiases in Estonia. Parasitol Res. 2006;99:729–36. doi: 10.1007/s00436-006-0220-1. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Moreno O, Domingo L, Teixidor J, Gracenea M. Prevalence and associated factors of intestinal parasitisation: a cross-sectional study among outpatients with gastrointestinal symptoms in Catalonia, Spain. Parasitol Res. 2011;108:87–93. doi: 10.1007/s00436-010-2044-2. [DOI] [PubMed] [Google Scholar]
- 8.Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, et al. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet. 2006;367:1521–32. doi: 10.1016/S0140-6736(06)68653-4. [DOI] [PubMed] [Google Scholar]
- 9.Song HJ, Cho CH, Kim JS, Choi MH, Hong ST. Prevalence and risk factors for enterobiasis among preschool children in a metropolitan city in Korea. Parasitol Res. 2003;91:46–50. doi: 10.1007/s00436-003-0836-3. [DOI] [PubMed] [Google Scholar]
- 10.Li YL. Human parasitology. Beijing: People's Medical Publishing House; 2008. [Google Scholar]
- 11.Kim DH, Son HM, Kim JY, Cho MK, Park MK, Kang SY, et al. Parents' knowledge about enterobiasis might be one of the most important risk factors for enterobiasis in children. Korean J Parasitol. 2010;48:121–6. doi: 10.3347/kjp.2010.48.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao YE, Zhang H, Chang Y, Xun M, Wu XH. The relationship between the infection of pinworn and personal-social factors and its influence on the children's growth. Chin J Parasit Dis Con. 2001;14:268–71. [Google Scholar]
- 13.Serpytis M, Seinin D. Fatal case of ectopic enterobiasis: Enterobius vermicularis in the kidneys. Scand J Urol Nephrol. 2012;46:70–2. doi: 10.3109/00365599.2011.609834. [DOI] [PubMed] [Google Scholar]
- 14.Pampiglione S, Rivasi F. Enterobiasis in ectopic locations mimicking tumor-like lesions. Int J Microbiol. 2009;2009:642481. doi: 10.1155/2009/642481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu LQ, Chen YD, Sun FH, Cai N, Fang YY, Wang LP, et al. A National Survey on Current Status of the Important Parasitic Diseases in Human Population. Chin J Parasitol Parasit Dis. 2005;23:332–9. [PubMed] [Google Scholar]
- 16.Zhang XC, Zhang QM, Pei FQ, Wang JL, Lin RX, Ruan CW. Survey on the infection situations of soil-borne nematodes in 5 surveillance sites at Guangdong Province in 2008–2009. J Trop Med. 2010;10:990–2. [Google Scholar]
- 17.Zhang QM, Zhang XC, Deng ZH, Lin RX, Wang JL, Ruan CW. Surveillance situations and analysis of soil-borne nematodiasis surveillance sites of Guangdong province in 2008. J Trop Med. 2011;11:703–5.
- 18.Nithikathkul C, Akarachantachote N, Wannapinyosheep S, Pumdonming W, Brodsky M, Sukthana Y. Impact of health educational programmes on the prevalence of enterobiasis in schoolchildren in Thailand. J Helminthol. 2005;79:61–5. doi: 10.1079/JOH2004272. [DOI] [PubMed] [Google Scholar]
- 19.Chen YD, Wang JJ, Zhu HH, Zhu TJ, Zang W, Qian MB, et al. Enterobius vermicularis Infection Status among Children in 9 Provinces/Autonomous Regions/Municipalities of China. Chin J Parasitol Parasit Dis. 2013;31:251–5. [PubMed] [Google Scholar]
- 20.Zhang QM, Fang YY, Zhang XC, Ruan CW, Su GH, Liu T. Analysis on the surveillance situations of the national soil transmitted nematodiasis surveillance site in Gaozhou city in 2007. J Trop Med. 2008;8:1176–7. [Google Scholar]
- 21.Yang YS, Kim SW, Jung SH, Huh S, Lee JH. Chemotherapeutic trial to control enterobiasis in school children. Korean J Parasitol. 1997;35:265–9. doi: 10.3347/kjp.1997.35.4.265. [DOI] [PubMed] [Google Scholar]
- 22.Coulaud JP, Rossignol JF. Albendazole: a new single dose anthelmintic. Study in 1455 patients. Acta Trop. 1984;41:87–90. [PubMed] [Google Scholar]
- 23.St Georgiev V. Chemotherapy of enterobiasis (oxyuriasis) Expert Opin Pharmacother. 2001;2:267–75. doi: 10.1517/14656566.2.2.267. [DOI] [PubMed] [Google Scholar]
- 24.Kang IS, Kim DH, An HG, Son HM, Cho MK, Park MK, et al. Impact of health education on the prevalence of enterobiasis in Korean preschool students. Acta Trop. 2012;122:59–63. doi: 10.1016/j.actatropica.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 25.Otu-Bassey IB, Useh MF, Alaribe AA. The post-treatment effects of enterobiasis on the occurrence of enuresis among children in Calabar, Nigeria. Asian Pac J Trop Med. 2011;4:315–9. doi: 10.1016/S1995-7645(11)60093-X. [DOI] [PubMed] [Google Scholar]
- 26.Kim DH, Cho MK, Park MK, Kang SA, Kim BY, Park SK, et al. Environmental factors related to enterobiasis in a southeast region of Korea. Korean J Parasitol. 2013;51:139–42. doi: 10.3347/kjp.2013.51.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hong SH, Jeong YI, Lee JH, Cho SH, Lee WJ, Lee SE. Prevalence of Enterobius vermicularis among preschool children in Muan-gun, Jeollanam-do, Korea. Korean J Parasitol. 2012;50:259–62. doi: 10.3347/kjp.2012.50.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salim N, Schindler T, Abdul U, Rothen J, Genton B, Lweno O, et al. Enterobiasis and strongyloidiasis and associated co-infections and morbidity markers in infants, preschool- and school-aged children from rural coastal Tanzania: a cross-sectional study. BMC Infect Dis. 2014;14:644. doi: 10.1186/s12879-014-0644-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multilingual abstracts in the six official working languages of the United Nations.
Content and options of the questionnaire.


