OVERVIEW
In an environment rife with controversy about patient safety in hospitals, medical error rates, and nursing shortages, consumers need to know how good the care is at their local hospitals. Nursing’s best kept secret is the single most effective mechanism for providing that type of comparative information to consumers, a seal of approval for quality nursing care: designation of magnet hospital status by the American Nurses Credentialing Center (ANCC). Magnet designation, or recognition of the “best” hospitals, was conceived in the early 1980s when the American Academy of Nursing (AAN) conducted a study to identify which hospitals attracted and retained nurses and which organizational features were shared by these successful hospitals, referred to as magnet hospitals. In the 1990s, the American Nurses Association (ANA), through the ANCC, established a formal program to acknowledge excellence in nursing services: the Magnet Nursing Services Recognition Program. The purpose of the current study is to examine whether hospitals selected for recognition by the ANCC application process—ANCC-accredited hospitals—are as successful in creating environments in which excellent nursing care is provided as the original AAN magnet hospitals were. We found that at ANCC-recognized magnet hospitals nurses had lower burnout rates and higher levels of job satisfaction and gave the quality of care provided at their hospitals higher ratings than did nurses at the AAN magnet hospitals. Our findings validate the ability of the Magnet Nursing Services Recognition Program to successfully identify hospitals that provide high-quality nursing care.
In the 1980s, the American Academy of Nursing reported on hospitals that were able to recruit and retain highly qualified nurses in a competitive market. Subsequent research showed that ‘magnet hospitals’ have better outcomes than nonmagnet hospitals. This study compares the original magnet hospitals with ones that met criteria for accreditation as magnet hospitals by the American Nurses Credentialing Center. It provides the evidence nurses need to convince their hospitals to seek this accreditation.
The public is inundated with media coverage of changes in health care that could adversely affect their access to and the quality of health care services. Public opinion polls confirm that consumers’ trust in hospitals is eroding and interest in the quality of health care is increasing.1, 2 Consumer concerns are visibly evident in the ongoing congressional debates on the Patient Bill of Rights, federal and state legislation providing protection against premature hospital discharge of new mothers and infants, and legislation stipulating minimum nurse-to-patient ratios in California hospitals.
More than 80% of the public polled in a recent survey wanted to know how to evaluate the quality of hospital care.2 Various lists of the “best” hospitals, such as that in U.S. News and World Report (“America’s Best Hospitals”) have been published, generating consumer interest and creating marketing opportunities for hospitals.3 Likewise, the designation “accreditation with commendation” from the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) has been touted by hospitals as an indicator of high-quality hospital care. There is little hard evidence that “best” hospitals achieve better outcomes than other hospitals4, 5 or that JCAHO commendation translates into better patient care, but consumers appear to take note of these appraisals, perhaps because of a lack of alternatives.
For close to two decades, nursing has had a potential vehicle for informing consumers about the quality of hospital nursing care. In the early 1980s, 41 hospitals were awarded “magnet hospital” designation as a result of a national study conducted by the American Academy of Nursing. Two aims of the AAN initiative were to identify hospitals that were successful in attracting and retaining nurses and to determine the organizational features those hospitals had in common that might account for their success.6 The magnet hospitals had in common organizational features that promoted and sustained professional nursing practice, including flat organizational structures, unit-based decision-making processes, influential nurse executives, and investments in the education and expertise of nurses. Unlike other “best” hospitals, the AAN magnet hospitals (hereafter referred to as “original magnet hospitals”) have been the subject of considerable research; subsets of the magnet hospitals were reexamined in 1986,7 1989,8 and 1991,9 and the results documented that the distinguishing organizational features have endured.
The organizational attributes that attract nurses to magnet hospitals have also been found to be consistently and significantly associated with better patient outcomes than those of matched nonmagnet hospitals. Several recently published research synthesis papers reinforce the empirical evidence suggesting that magnet hospitals achieve better outcomes than comparable hospitals.10, 11We conducted two earlier studies that reaffirmed the magnitude of the superior outcomes in the magnet hospitals.
In the first study, we examined Medicare mortality rates using 1988 data for 39 of the 41 original magnet hospitals (one hospital had closed and one was a Veterans Administration hospital not included in the Medicare data) by using a multivariate matched sampling procedure that controlled for hospital characteristics that previous research had shown to be associated with mortality (such as ownership, teaching status, size, location, financial status, physician qualifications, technology index, and emergency admissions). The 39 magnet hospitals were matched with 195 comparison hospitals (five per magnet hospital) selected from all nonmagnet U.S. hospitals with more than 100 Medicare discharges. Medicare mortality rates in magnet and comparison hospitals were compared using variance components models, which pool information from each group of five matched hospitals and adjust for differences in patient composition, as measured by predicted mortality. After adjustment for differences in predicted mortality for Medicare patients, the magnet hospitals had a 4.6% lower mortality rate (p = 0.026), which translates to between 0.9 to 9.4 fewer deaths per 1,000 discharges (with 95% confidence).12
The second study of the magnet hospitals involved data from 1,205 consecutively admitted patients with AIDS and from 820 nurses on 40 units in a subset of 20 magnet hospitals.13 Patient outcomes were compared for patients with AIDS in magnet hospitals without dedicated AIDS units and in comparison hospitals with and without dedicated AIDS units. Patients with AIDS in scattered-bed units in magnet hospitals had lower odds of dying than did AIDS patients in any other setting—lower by 60%, for example, than patients in scattered-bed units in nonmagnet hospitals.9 Other analyses associated with this study showed that magnet hospitals had significantly higher levels of patient satisfaction,14 significantly lower rates of nurse burnout,15 and lower rates of needlestick injuries in nurses14 than did comparison hospitals. While magnet hospitals were found to have higher nurse-to-patient ratios than other hospitals, the cost of more nurses was more than offset by significantly shorter lengths of stay and lower utilization of ICU days. Overall, multiple studies point to significantly better outcomes in magnet hospitals, as compared with nonmagnet hospitals.
In the early 1990s, the ANA, through the ANCC—the organization that certifies registered nurses in clinical specialties—established a formal magnet hospital program to recognize excellence in nursing services.16, 17 The Magnet Nursing Services Recognition Program is a voluntary form of external professional nurse peer review available to all hospitals (and more recently to nursing homes). ANCC magnet hospital designation is based on a hospital’s ability to meet 14 standards of nursing care evaluated in a multistage process of written documentation and on-site evaluation by nurse experts—a process similar to JCAHO accreditation. The ANCC magnet hospital recognition program is similar in objectives and design to the original AAN magnet hospital program, except that the ANCC program involves a voluntary application process and requires hospital recertification every four years. Because the ANCC magnet hospital recognition program is available to all hospitals, it’s a vehicle for providing information to consumers about the quality of nursing care in local hospitals.
The purpose of this study was to examine whether ANCC-recognized magnet hospitals had the same organizational attributes responsible for excellent nursing care as the original magnet hospitals did and whether they had high rates of nurse satisfaction and the same quality of care (as assessed by nurses) and thus offered evidence that the good outcomes shown to exist in the original magnet hospitals can be expected to exist in those selected through the newer ANCC Magnet Nursing Services Recognition Program.
METHODS
In the present study, seven ANCC magnet hospitals were compared with 13 original magnet hospitals (see More on Methods and Statistics, page 33). We do not contend that the two groups are matched groups of hospitals (as in our previous studies); they are simply two groups of magnet hospitals selected through different processes a decade apart. In fact, there are several differences between the two groups of hospitals. The ANCC magnet hospitals are larger, with an average of 457 beds, compared with 398 beds in the original magnet hospitals. Also, ANCC magnet hospitals are more likely to be teaching institutions; 71% of ANCC magnet hospitals are members of the Council of Teaching Hospitals, compared with 31% of the original hospitals.
More on Methods and Statistics.
This study used a comparative multisite observational design incorporating two subsamples of hospitals. Our objective was to compare contemporary ANCC-recognized magnet hospitals with the original magnet hospitals. The ANCC hospitals studied included all ANCC magnet hospitals that existed at the time the study began (n = 7). The original magnet hospital subsample was selected through use of a sampling frame developed by Marlene Kramer for her 1986 study of the original magnet hospitals.7 Kramer used a 40% sample—proportionate by regions of the country—of the 41 original magnet hospitals. Because part of our research focuses on changes in the clinical practice environment in magnet hospitals over time, we restudied the original magnet hospitals from Kramer’s sample to have data on magnet hospitals at two points in time. At the time of our study (1998), two of Kramer’s 16 hospitals had merged, leaving 15 hospitals. We attempted to recruit all 15 hospitals to our study, but three nurse executives declined to participate, leaving us with 12 hospitals and without an original magnet hospital in the West Coast region. We therefore recruited the remaining original magnet hospital located in that region for our study (a hospital not studied by Kramer), for a total of 13 original magnet hospitals. The three nurse executives who declined to participate noted that their hospitals no longer had the elements of professional nurse practice that had won them AAN magnet hospital designation in 1982. Thus, to the extent that the refusals bias the sample of original magnet hospitals, the bias would be toward having a stronger group of original magnet hospitals, since the weaker ones declined to participate and would thereby provide a stronger test of how the ANCC-recognized magnet hospitals measure up than might be the case if all the original magnet hospitals had been included.
This study, approved by all 20 hospitals’ institutional review boards, was conducted in the spring of 1998. The nurse survey component of the study included a census of all registered nurses on staff who worked at least 16 hours per week on any medical or surgical nursing unit in study hospitals, yielding roughly 3,600 eligible nurses. Study participation was voluntary and all participating nurses provided informed consent. A research nurse was appointed at each hospital to carry out the protocol, which involved distributing the questionnaire packets and sending reminder postcards at two weeks, follow-up questionnaires at four weeks, and final reminder postcards at six weeks.
The NWI-R is a modification of the Nursing Work Index,7 consisting of 49 items rated with a 4-point Likert-type scale that gauges staff nurse perceptions of selected organizational traits in their work setting (for example, “This factor is present in my current job situation”). Three of the NWI-R subscales—which measure the constructs of nurse autonomy, nurse control over the practice setting, and nurses’ relations with physicians—have been used in multiple studies and have consistently demonstrated acceptable internal consistency reliability (Cronbach’s alpha): autonomy, 0.78; control, 0.79; and nurse–physician relations, 0.73.18 Completed questionnaires were received from 2,045 nurses (56% response rate), of whom 1,064 nurse respondents were in ANCC magnet hospitals and 981 were in original magnet hospitals.
Although the results we report are bivariate and largely descriptive, we used significance tests (chi-square statistics with categorical variables and t-statistics with continuous ones, such as the years-of-experience and practice-environment subscales) to ensure that the differences we observed between the nurses in the two groups of hospitals were not the result of sampling fluctuations or chance.
Nurses on medical-surgical units at all institutions were invited to complete a 15-page self-administered survey that took approximately 30 minutes to complete. It included the following sections:
job characteristics, including hours worked, workload, supervisory responsibilities, non-nursing duties
job outlook, including job satisfaction, intent to leave, and perceptions of job security and job market
organizational attributes of the work setting as measured by the revised Nursing Work Index (NWI-R)18
job-related feelings as measured by the Maslach Burnout Inventory19
occupational exposures to blood14
demographic and educational characteristics20
The results presented below are from analyses of the nurse survey data alone and reflect our belief that by querying nurses much can be learned about hospitals—how they are organized and how their organization affects nurses and, ultimately, patients. All of the variables we report, except one—relations between nurses and physicians—differed significantly across the nurses’ surveys in the two groups we compared.
RESULTS
Nurses’ education and experience
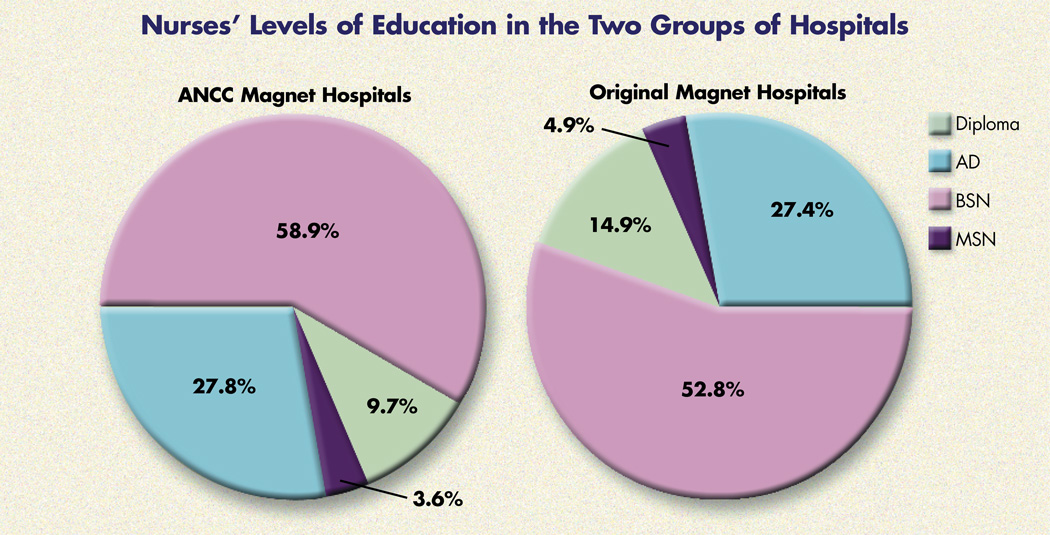
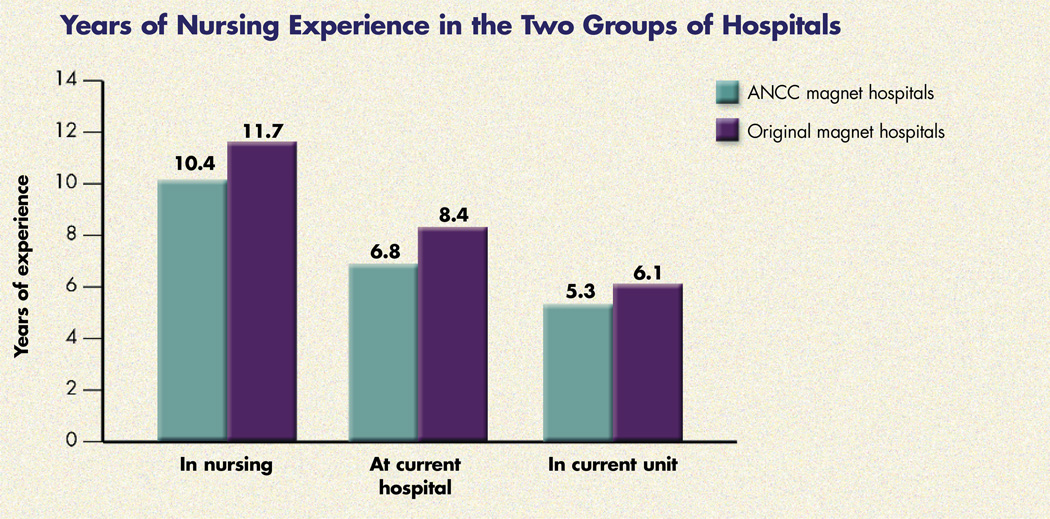
Generally, both groups of magnet hospitals had a registered nurse workforce with significantly higher educational preparation than nonmagnet hospitals had. Approximately 34% of nurses working in the nation’s hospitals have a baccalaureate degree as their highest level of education,21 whereas over 50% of nurses in both groups of magnet hospitals were prepared at the baccalaureate level. In comparing nurses’ education across the two groups of magnet hospitals, the percentage of nurses with baccalaureate degrees was significantly higher in ANCC magnet hospitals (see Nurses’ Levels of Education in the Two Groups of Hospitals, page 28). However, nurses practicing in ANCC magnet hospitals had significantly less nursing experience, fewer years of employment at their current institutions, and fewer years assigned in their current units than did nurses in the original magnet hospitals (see Years of Nursing Experience in the Two Groups of Hospitals, above). On average, nurses in ANCC magnet hospitals had worked in nursing and at their current hospitals for about one and a half years less than had nurses in the original magnet hospitals. Similarly, nurses in ANCC hospitals had worked on their current units for about one year less than had nurses in the original magnet hospitals.
Nurses’ Levels of Education in the Two Groups of Hospitals.
The chi-square value testing the independence of education across the two hospital settings is 16.5 with three degrees of freedom (p < 0.001).
Years of Nursing Experience in the Two Groups of Hospitals.
T-test statistics for mean differences were 3.0 (p + 0.002), 5.2 (p < 0.001), and 3.4 (p < 0.001) for years in nursing, at current hospital, and in current unit, respectively. Standard errors associated with estimated means are between 0.2 years and 0.3 years.
Nurse staffing
Two independent data sources show that the ANCC magnet hospitals had a significantly higher ratio of registered nurses to patients than did the original magnet hospitals. Data from the 1997 Annual Hospital Survey of the American Hospital Association (AHA) were analyzed and show that ANCC magnet hospitals employed 190 full-time equivalent registered nurses per 100 patients (average daily census), compared with 128 nurses per 100 patients in the original magnet hospitals. Analysis of the 1997 AHA data also reveal that the average nurse-to-patient ratio for community hospitals overall was lower still, at 109 registered nurses per 100 patients.22 The higher nurse-to-patient ratios obtained from analysis of AHA data are supported by reports from our survey of nurses practicing in both groups of magnet hospitals: nurses in ANCC magnet hospitals reported caring for, on average, one fewer patient per shift than did the nurses in the original magnet hospitals.
Clinical practice environment
In addition to differences in nurse staffing, nurses at ANCC and original magnet hospitals differed in their appraisals of other aspects of their practice environment.
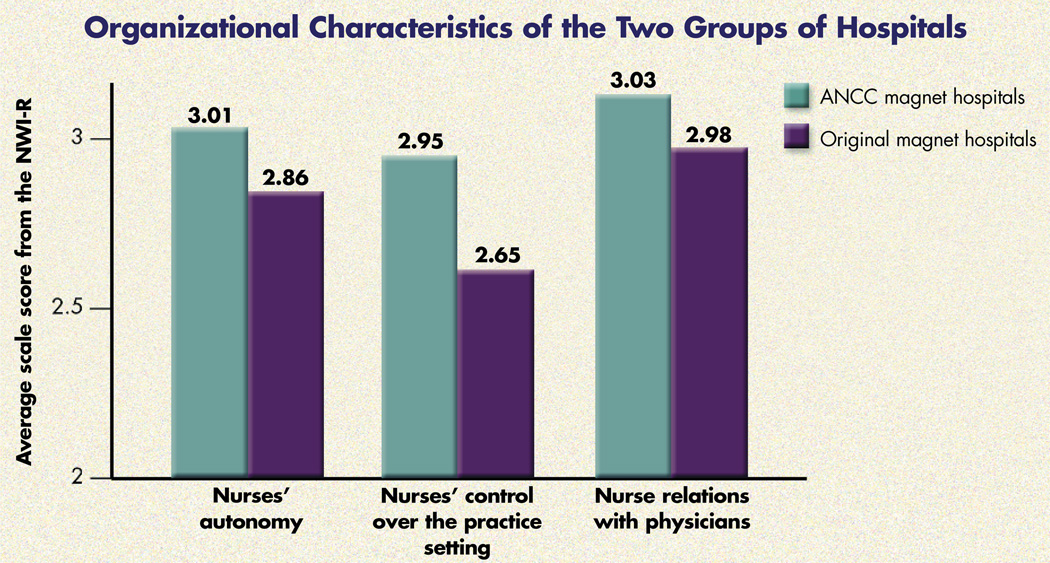
In our study, we found that some of the same types of differences in the questionnaire’s subscales exist between the ANCC magnet hospitals and the original magnet hospitals that, in earlier research, we found to exist between original magnet hospitals and nonmagnet hospitals. In previous studies, we characterized the practice environment of hospitals by creating three subscales using items from the NWI-R to measure the extent of nurse autonomy, nurses’ control over their practice environment, and the quality of nurses’ relations with physicians.18 Our previous research showed that nurses’ clinical work context in the original magnet hospitals was characterized by significantly greater autonomy, more control over the practice setting, and better relations with physicians when compared with nurses’ practice environment in nonmagnet hospitals.9, 12 In the current study, however, high levels of nurse autonomy and nurse control over the practice setting were more characteristic of ANCC magnet hospitals than of the original magnet hospitals, and these differences were statistically significant (see Organizational Characteristics of the Two Groups of Hospitals, above). By control over the practice setting, we mean that nurses had sufficient intraorganizational status to influence others and to deploy resources when necessary for good patient care. Nurses’ relationships with physicians were similar in the two groups of magnet hospitals.
Organizational Characteristics of the Two Groups of Hospitals.
T-tests for mean differences were 6.2 (p < 0.001), 12.3 (p < 0.001), and 1.6 (p = 0.10) for nurses’ autonomy, control over the practice setting, and relations with physicians, respectively. Standard errors associated with the estimated means are approximately 0.02 points.
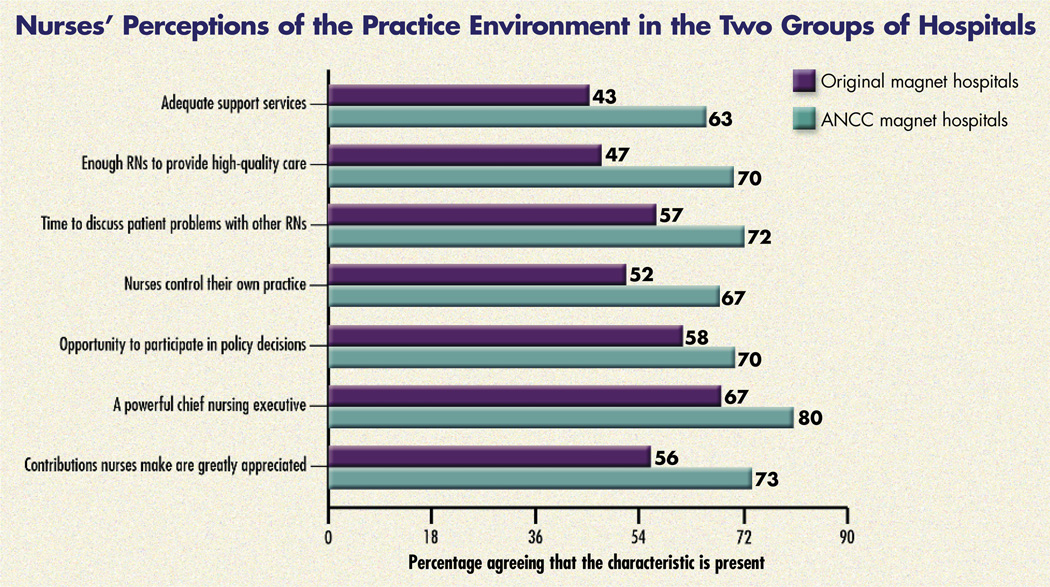
The positive conditions for nursing practice in ANCC magnet hospitals were further apparent when we considered a few of the items from the NWI-R. Nurses’ Perceptions of the Practice Environment in the Two Groups of Hospitals (page 31) shows the percentage of nurses agreeing that certain positive characteristics listed in our survey exist in their institutions (for example, having a powerful chief nursing executive). Nurses in ANCC magnet hospitals were substantially and significantly more likely than nurses in the original magnet hospitals to report that their units have adequate support services and enough RNs to provide high-quality care. They also reported having adequate time to discuss patient problems with other nurses. These findings are consistent with the higher reported nurse-to-patient ratios in ANCC magnet hospitals. Nurses in ANCC magnet hospitals also reported (in greater relative numbers) that they control their own practice, participate in policy decisions, have a powerful chief nursing executive, and that the contributions they make are greatly appreciated. In responding to these survey items and a majority of the full set of items on the NWI-R, the nurses in ANCC magnet hospitals rated their practice environments more highly than did nurses in the original magnet hospitals. Here again, we note that our previous research documented that nurses in the original magnet hospitals rated their practice environments significantly more favorably than did nurses in nonmagnet hospitals.
Nurses’ Perceptions of the Practice Environment in the Two Groups of Hospitals.
Chi-square values (with one degree of freedom) associated with the tests of independence of the seven variables across the two hospital settings are 84.4, 117.4, 49.3, 41.7, 28.0, 28.3, and 45.6 for the variables as listed above (from top to bottom), respectively. All have p values of less than 0.001. Standard errors associated with the percentages shown are between 1% and 2%.
Burnout and job satisfaction
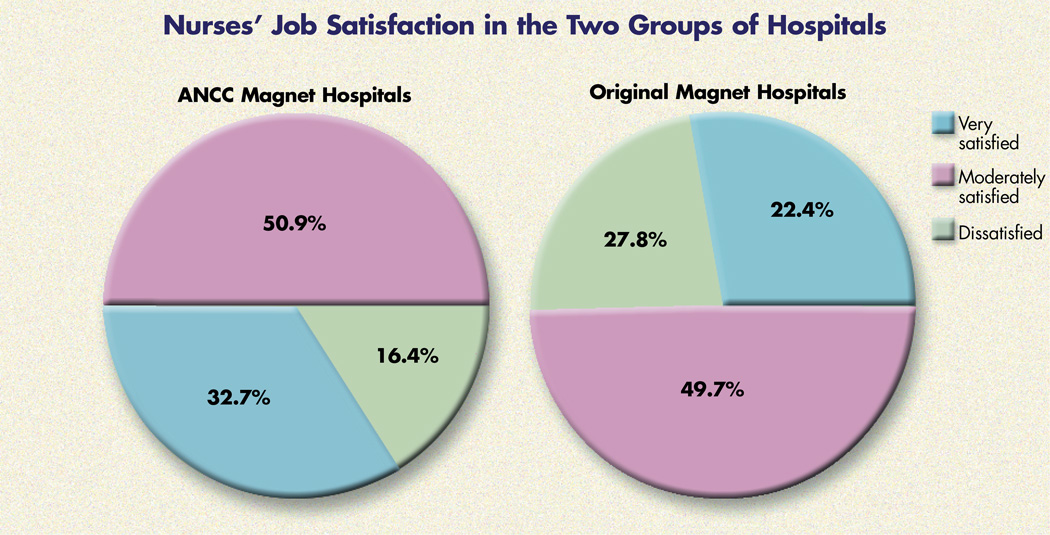
Differences in staffing and practice environments were associated with differences in nurse outcomes in the two groups. Nurses in ANCC magnet hospitals were significantly less likely than nurses in the original magnet hospitals to report feeling burned out, emotionally drained, or frustrated by their work (see Nurse Burnout in the Two Groups of Hospitals, page 31). Moreover, when nurses were asked how satisfied they were with their present job, those in ANCC magnet hospitals answered decidedly differently from those in the original magnet hospitals. Although half the nurses in both settings reported being moderately satisfied, nurses in the ANCC magnet hospitals were considerably less likely than those in original magnet hospitals to report being dissatisfied (16% vs. 28%, respectively) and were more likely to report being very satisfied (33 % vs. 22%, respectively) (see Nurses’ Job Satisfaction in the Two Groups of Hospitals, page 32).
Nurse Burnout in the Two Groups of Hospitals.
| Nurses who reported frequently feeling | ANCC Magnet Hospitals | Original Magnet Hospitals |
|---|---|---|
| • burned out from their work | 20.4% | 29.9% |
| • emotionally drained from their work | 42.2% | 51.6% |
| • frustrated by their job | 32.0% | 44.9% |
Chi-square values (with one degree of freedom) associated with the tests of independence of the three variables across the two types of hospitals are 14.6, 13.3, and 23.1 for burnout, emotional exhaustion, and frustration, respectively. All have p values of less than 0.001. Standard errors associated with the percentages shown in the table are between 1% and 2%.
Nurses’ Job Satisfaction in the Two Groups of Hospitals.
The chi-square value testing the independence of job satisfaction across the two hospital settings is 50.0 with two degrees of freedom (p < 0.001).
Quality of care
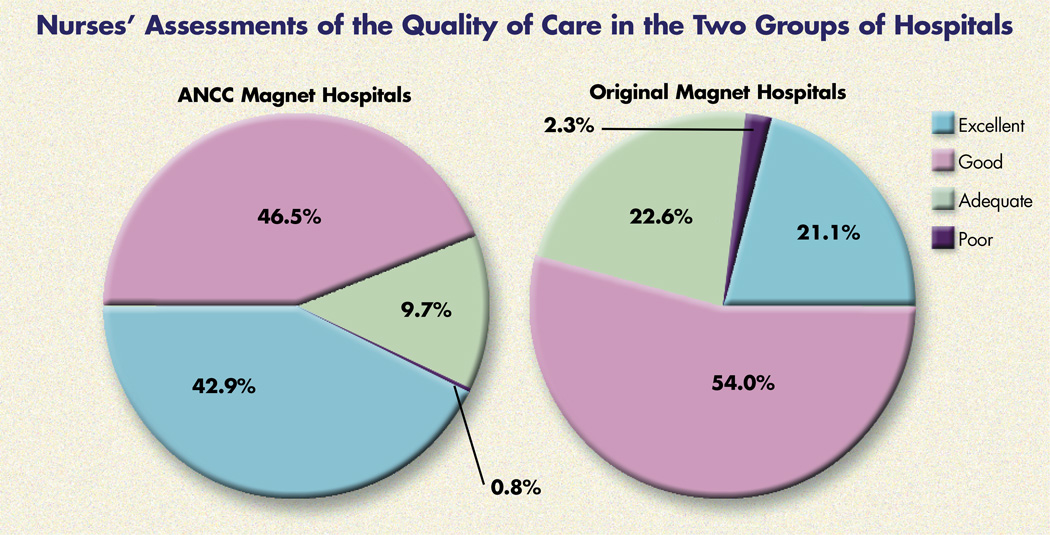
In previous research, we documented an association between attributes of the clinical practice environment and patient outcomes. For example, the greater control nurses reported having in the practice setting, the higher patients rated satisfaction with care.9, 13 In this study, we did not interview patients, but we used nurses to judge the quality of care in their hospitals; 43% of those in ANCC magnet hospitals, versus only 21% of nurses in the original magnet hospitals, indicated that the quality of care delivered to their patients was excellent (see Nurses’ Assessments of the Quality of Care in the Two Groups of Hospitals, page 32). Only one in 10 nurses in ANCC hospitals described the quality of care delivered to patients as either adequate or poor, whereas almost 25% of the nurses in the original magnet hospitals did so. However, nurses in both groups ranked care in their hospitals substantially higher than did a national convenience sample of nurses polled in a recent AJN study, in which only 10% of nurses rated care in their hospitals as excellent.23
Nurses’ Assessments of the Quality of Care in the Two Groups of Hospitals.
The chi-square value testing the independence of assessed quality of care across the two hospital settings is 137.9 with three degrees of freedom (p < 0.001).
DISCUSSION
The purpose of this study was to investigate whether the ANCC’s application-based process for designating magnet hospitals identifies institutions that nurses evaluate as favorably as the hospitals originally selected by the AAN for magnet designation (based on their reputations as good places to practice professional nursing). The original magnet hospitals have been shown to have substantially improved patient outcomes and greater respect for nurses than for those in nonmagnet hospitals. A finding that the ANCC magnet hospital designation identified hospitals with nurse practice environments that are comparable to those of the original magnet hospitals would provide strong evidence for consumers and nurses of the usefulness of ANCC recognition in identifying hospitals with good nursing care.
Our findings provide this evidence. The ANCC’s magnet hospital designation process successfully identified hospitals that provided practice environments that were as good as or better than those at the original magnet hospitals in terms of professional nursing practice and the quality of nursing care. In our study, nurses in ANCC magnet hospitals had significantly higher educational preparation than did nurses in the original magnet hospitals. We view education of the nurse workforce in a given institution as an organizational attribute, because decisions made by hospital management influence the selection and retention of more highly educated nurses. Likewise, managerial decisions determine nurse-to-patient ratios, and ANCC magnet hospitals had higher nurse-to-patient ratios than did the original magnet hospitals. These higher nurse-staffing levels were associated with other favorable practice conditions and outcomes for nurses and patients. We found that ANCC magnet hospitals had the same organizational traits that distinguished the original magnet hospitals in the 1980s and that are associated with better patient outcomes. Nurses in ANCC magnet hospitals were more satisfied with their jobs and were less likely to suffer from job-related burnout. And—perhaps of greatest importance—nurse-appraised quality of care is significantly higher in ANCC magnet hospitals.
Although this study did not systematically compare either type of magnet hospital to a representative group of nonmagnet hospitals—a topic for future research when data from a current study of all Pennsylvania hospitals become available—we provide evidence from other studies suggesting that both groups of magnet hospitals are more highly appraised by the nurses practicing in them than is the case in nonmagnet hospitals. The original magnet hospitals are not immune to changes in the nation’s health care system, and some have been adversely affected, including one of the original 41 that recently lost its accreditation because of poor quality of care. However, despite vast organizational change, many of the original magnet hospitals continue to foster elements of professional nursing practice that distinguish them from nonmagnet hospitals.24 Thus, our use of the original magnet hospitals as a comparison group likely underestimates, perhaps to a significant extent, the differences between ANCC magnet hospitals and nonmagnet hospitals. We are currently working to pool information from the nurses’ surveys with additional data from the participating hospitals—such as discharge data on patients with AIDS—and hospital-level data from the American Hospital Association and mortality statistics from Medicare. This pooled data set will allow us to determine whether (and to what extent) mortality differences between the ANCC magnet hospitals and the original magnet hospitals are due to differences in how nursing care is organized across the hospitals.
Much work remains to be done in determining how nurse staffing and skill interact with other organizational features to affect patient outcomes. A cross-national study currently under way on the impact of hospital organization and staffing on patient outcomes will soon provide definitive information on this important issue and offer a large representative sample of hospitals against which the ANCC magnet hospitals can be compared.25 Based on the excellent showing of ANCC magnet hospitals compared with a group of the original magnet hospitals in the present study, we anticipate that the ANCC hospitals will fare even better when compared with a more representative group of hospitals in the United States. That study will also provide the first firm estimate of the proportion of all hospitals in the United States that might qualify for ANCC magnet hospital recognition based on their nursing practice environments and patient outcomes. There is no way of knowing what percentage of hospitals now meets the ANA standards for professional nursing practice (which constitute the core criteria for ANCC magnet recognition).
The slow rate of ANCC magnet hospital recognition is problematic. This potentially useful quality indicator must be propelled into the public domain. At the time of this writing, almost a decade after the launching of the ANCC magnet hospital application and designation program, only 16 magnet hospitals have been identified. Moreover, almost 20 years after the designation of the original AAN magnet hospitals as centers of excellence in nursing care and despite substantial amounts of research literature documenting excellent patient outcomes and nursing practice conditions in these hospitals, the term “magnet hospital” receives little recognition, either among nurses or among other health care providers and consumers.
Our purpose in publishing this paper is to bring to nurses’ attention the potential for magnet hospital designation to provide consumers with a way to help them judge the quality of care in hospitals. More knowledgeable consumers would certainly support the kinds of safeguards that nurses have been proposing for hospitals. A vehicle such as ANCC magnet hospital designation could offer consumers a practical way to “vote with their feet” and to advocate change in their local hospitals.
As a Philadelphia Inquirer editorial noted, “Why hasn’t any area hospital asked the American Nurses Association to evaluate its patient care? There’s been no rallying call, to be sure, from the local hospitals’ trade group—whose representative was mighty quick to suggest that nurses might not be the most impartial people to assess nursing care, [but] when it comes to reassuring patients at the bedside, who wouldn’t prefer a nurse to a hospital manager?”26 Staff nurses and their leaders must embrace the idea of magnet hospital status; they must become champions for seeking ANCC recognition to create the critical mass of hospitals necessary to elevate the visibility of this nursing seal of approval to the level of JCAHO evaluation or other lists of the “best” hospitals. Our research documents that ANCC magnet hospital designation is a valid marker of good nursing care. Consumers are seeking information about quality, and they trust nurses’ appraisals. It is now up to the nation’s nurses to make something of this opportunity— for themselves and for their patients.
How UC Davis Medical Center ‘Won the Gold’.
Imagine working in an institution that fosters excellence in nursing service and offers holistic, family-centered patient care. Imagine a place where nurses institute change and the administration offers nurses career development guidance, educational opportunities, and support services for complex patient needs. That’s what it’s like to work at my institution, the University of California Davis Medical Center (UCDMC), which is recognized by the American Nurses Credentialing Center (ANCC) as a magnet hospital for nursing services.
When UCDMC was designated a magnet hospital in 1997, I felt as if I had won a gold medal at the nursing Olympics. The title gave our nurses the satisfaction of receiving recognition for a job well done.
Months earlier, while reviewing the ANCC standards for designation as a magnet hospital, our application committee happily discovered that our nursing department already met most of the standards. We only needed to show the ANCC what we did.
First, we compiled the demographic data that the ANCC requested; then, we divided among our committee members the task of gathering evidence demonstrating fulfillment of standards.
We gathered copies of our nursing structure standards, nursing and hospital policies and procedures, nursing committee mission statements and meeting minutes, data from our performance improvement programs, outlines and objectives from classes and competency programs, and sample nursing documentation. We discovered that some evidence of ANCC standards—for example, a hospital event for the staff and the community—wasn’t associated with a formal policy. For this we submitted a copy of a flyer advertising the event or a copy of a newspaper article reporting on it.
We devoted a section of the application to each standard, including a title page restating the ANCC standard to be demonstrated, a one- to four-paragraph essay describing how we met that standard, and copies of pertinent documents. Before submission, the application was reviewed and edited to avoid redundancy and to identify gaps.
After assessing our application, the ANCC sent two appraisers to our hospital for an on-site evaluation. During that phase, I realized how much magnet hospital designation meant to our nurses. To my delight, our nurses greeted appraisers at each unit and enthusiastically led the visitors on unit tours, eagerly sharing what was special about the unit. Later, at several discussion groups, nurses were invited to answer questions from the appraisers. I joyfully listened to accounts of what our nurses did to implement special programs, improve patient care, and increase staff satisfaction. I wished that every UCDMC nurse could have heard what I did. Until then I hadn’t known about the many ways our nurses made their units better places.
We celebrated our magnet hospital designation with a gala for all of the nurses, and now we hold annual festivities to recognize achievements. Our nurse recruitment department uses our magnet hospital designation to attract new nurses, and physicians report that the designation influenced their decision to join UCDMC. Earning magnet hospital designation was like winning at the Olympics, but unlike the Olympics—where only a few can win—being a magnet hospital lets us all win.—Susan L. Vomund, BSN, RN,C, is a clinical resource nurse specializing in perinatal and women’s health services at the University of California Davis Medical Center, Sacramento, CA
Acknowledgments
This research was funded in part by the National Institute of Nursing Research, the National Institutes of Health, the Baxter Allegiance Foundation, and the Claire M. Fagin Leadership Chair in Nursing, University of Pennsylvania School of Nursing. The authors are grateful to the staff nurses and chief nurse officers of the 20 participating magnet hospitals for making this study possible, to Dr. Marlene Kramer for making available her 1986 magnet hospital nurse survey data, and to Drs. Eileen Lake and Julie Sochalski for their contributions to the study.
REFERENCES
- 1.Hensley S. VHA readies ad campaign. Proposed plan would play up local hospitals’ strengths [news] Mod Healthc. 1998;28(4):2–3. [PubMed] [Google Scholar]
- 2.National Coalition on Health Care. How Americans perceive the health care system: a report on a national survey. J Health Care Finance. 1997;23(4):12–20. [PubMed] [Google Scholar]
- 3.Morrissey J. All benchmarked out. Even the top 100 hospitals can’t find many more ways to be more productive. Mod Healthc. 1998;28(49):38–40. 2–4, 6. [PubMed] [Google Scholar]
- 4.Chen J, et al. Do “America’s Best Hospitals” perform better for acute myocardial infarction? N Engl J Med. 1999;340(4):286–292. doi: 10.1056/NEJM199901283400407. [see comments]. [DOI] [PubMed] [Google Scholar]
- 5.Hill CA, et al. “Best hospitals”: a description of the methodology for the Index of Hospital Quality. Inquiry. 1997;34(1):80–90. [PubMed] [Google Scholar]
- 6.McClure ML, et al. American Academy of Nursing. Magnet hospitals: attraction and retention of professional nurses. Kansas City, Mo.: American Nurses Association; 1983. Task Force on Nursing Practice in Hospitals. [PubMed] [Google Scholar]
- 7.Kramer M, Hafner LP. Shared values: impact on staff nurse job satisfaction and perceived productivity. Nurs Res. 1989;38(3):172–177. [PubMed] [Google Scholar]
- 8.Kramer M. The magnet hospitals. Excellence revisited. J Nurs Adm. 1990;20(9):35–44. [PubMed] [Google Scholar]
- 9.Aiken LH, et al. Organization and outcomes of inpatient AIDS care. Med Care. 1999;37(8):760–772. doi: 10.1097/00005650-199908000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Scott JG, et al. Review of magnet hospital research: findings and implications for professional nursing practice. J Nurs Adm. 1999;29(1):9–19. doi: 10.1097/00005110-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Havens DS, Aiken LH. Shaping systems to promote desired outcomes. The magnet hospital model. J Nurs Adm. 1999;29(2):14–20. doi: 10.1097/00005110-199902000-00006. [published erratum appears in J Nurs Adm 1999;29(4):5]. [DOI] [PubMed] [Google Scholar]
- 12.Aiken LH, et al. Lower Medicare mortality among a set of hospitals known for good nursing care. Med Care. 1994;32(8):771–787. doi: 10.1097/00005650-199408000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Aiken LH, et al. Satisfaction with inpatient AIDS care. Med Care. 1997;35(9):948–962. doi: 10.1097/00005650-199709000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Aiken LH, et al. Hospital nurses’ occupational exposure to blood: prospective, retrospective, and institutional reports. Am J Public Health. 1997;87(1):103–107. doi: 10.2105/ajph.87.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aiken LH, Sloane D. Effects of organizational innovations in AIDS care on burnout among urban hospital nurses. Work and Occupation. 1997;24(4):453–477. [Google Scholar]
- 16.Lewis CK, Matthews JH. Magnet program designates exceptional nursing services. Am J Nurs. 1998;98(12):51–52. [PubMed] [Google Scholar]
- 17.American Nurses Credentialing Center. Magnet nursing recognition program for excellence in nursing service—acute care. Washington, DC: American Nurses Credentialing Center; 1999. [Google Scholar]
- 18.Aiken LH, Patrician PA. Measuring organizational traits of hospitals: the revised nursing work index. Nursing Research. 2000 May-Jun; doi: 10.1097/00006199-200005000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Maslach C, Jackson SE. Maslach burnout inventory: manual. 2nd ed. Palo Alto, Calif.: Consulting Psychologists Press; 1986. [Google Scholar]
- 20.Aiken LH, et al. Design of an outcomes study of the organization of hospital AIDS care. Research in the Sociology of Health Care. 1997;14:3–26. [Google Scholar]
- 21.Moses E. Registered Nurse Population: Findings from the National Sample Survey. Rockville, MD: Department of Health and Human Services; 1997. [Google Scholar]
- 22.American Hospital Association. Annual survey database. The Association; 1997. [Google Scholar]
- 23.Shindul-Rothschild J, et al. 10 keys to quality care. Am J Nurs. 1997;97(11):35–43. [PubMed] [Google Scholar]
- 24.Buchan J. Still attractive after all these years? Magnet hospitals in a changing health care environment. J Adv Nurs. 1999;30(1):100–108. doi: 10.1046/j.1365-2648.1999.01054.x. [DOI] [PubMed] [Google Scholar]
- 25.Sochalski J, Aiken LH. Accounting for variation in hospital outcomes: a cross-national study. Health Aff (Millwood) 1999;18(3):256–259. doi: 10.1377/hlthaff.18.3.256. [DOI] [PubMed] [Google Scholar]
- 26.Why hasn’t any area hospital asked the American Nursing Association to evaluate its patient care? Philadelphia Inquirer. 1997 Dec.:A20. 1997. [Google Scholar]