Abstract
Aims
To estimate mortality rates among treated opioid-dependent individuals by cause and in relation to the general population, and to estimate the instantaneous effects of opioid detoxification and maintenance treatment (MMT) on the hazard of all-cause and cause-specific mortality.
Design
Population-based treatment cohort study.
Setting
Linked mortality data on all individuals first enrolled in publicly-funded pharmacological treatment for opioid dependence in California, USA from 2006 to 2010.
Participants
32,322 individuals, among whom there were 1,031 deaths (3.2%) over a median follow-up of 2.6 years (interquartile range: 1.4 - 3.7).
Measurements
The primary outcome was mortality, indicated by time to death, crude mortality rates (CMR), and standardized mortality ratios (SMR).
Findings
Individuals being treated for opioid dependence had a more than four-fold increase of mortality risk compared with the general population (SMR 4.5 95% CI: 4.2, 4.8). Mortality risk was higher (1) when individuals were out-of-treatment (SMR 6.1, 95% CI: 5.7, 6.5) than in-treatment (SMR 1.8, 95% CI: 1.6, 2.1) and (2) during detoxification (SMR 2.4, 95% CI 1.5, 3.8) than during MMT (SMR 1.8, 95% CI 1.5, 2.1), especially in the two weeks post-treatment entry (SMR 5.5, 95% CI 2.7, 9.8 versus SMR 2.5, 95% CI 1.7, 4.9). Detoxification and MMT both independently reduced the instantaneous hazard of all-cause and drug-related mortality. MMT preceded by detoxification was associated with lower all-cause and other-cause-specific mortality than MMT alone.
Conclusions
In people with opiate dependence, detoxification and methadone maintenance treatment both independently reduce the instantaneous hazard of all-cause and drug-related mortality.
Introduction
Opioid-dependent individuals suffer from mortality risks that are 6 to 20 times higher than the general population [1-3]. Overdose is the most common cause of death [4] however excess mortality also occurs due to suicide, injury, and drug-related chronic and infectious diseases [4]. Most of these deaths are premature and avoidable [4]. Treatment is a critical factor that can reduce mortality risk in opioid-dependent populations [2, 3, 5].
Methadone maintenance treatment (MMT) is the most effective and widely-used therapeutic intervention for heroin dependence [5-7]. MMT involves using methadone to block opioid receptors, thereby preventing effects and relieving withdrawal symptoms [8]. Mortality risk is highest within the 2 to 4 weeks following MMT initiation [9,10-12] and exit [9,10,12]. Continued MMT engagement is associated with sustained reductions in heroin use [3] and other benefits including decreases in HIV risk behaviors, lowered risk for hepatitis C (HCV) seroconversion, reductions in acquisitive crime and incarceration rates, and improvements in mental health and health-related quality of life [5,13,14]. In relation to mortality, treatment may be more effective if individuals remain in MMT [15], the average treatment duration is 12 or more months [9,16], and fewer treatment episodes are undertaken over time [13].
Opioid detoxification is a common but controversial therapy in the United States. Detoxification usually involves using medications (e.g., methadone, naltrexone) to rid the body of opioids while decreasing withdrawal-related discomfort [17]. The goal of detoxification is not treatment per se but rather controlled reduction of opioid dependence [18,19]. Detoxification (i.e., typically lasting 3-12 weeks) aims to taper methadone dosages, with the ultimate goal of opioid abstinence [6]. Given that opioid addiction is often a chronic relapsing condition [3,20,21] and treatment discontinuation typically results in relapse and elevated mortality risk [2,12], detoxification designed to achieve complete methadone taper may be a particularly harmful aspect of treatment [6].
In contrast, short-term detoxification followed by long-term MMT may be useful [6,19,22,23]. In practice, however, few detoxification patients transition to MMT [24]. Furthermore, repeated detoxification attempts among MMT-naïve patients have been associated with decreasing odds of successful treatment completion [24]. These recent findings, combined with the well-established high risk of opioid relapse following detoxification [17], suggest detoxification alone generally should not be considered adequate treatment [6]. A critical knowledge gap is to what degree mortality risk varies during and after MMT compared to detoxification.
Most mortality studies of mortality among opioid dependent patients have focused on the effects of a single treatment episode [2]. Addiction is now understood as a chronic condition [21] in which an individual may receive several treatments distributed over many years and from different providers [25-27]. Therefore, the effects of all treatments undertaken over time within a given treatment system may have more impact than that of a single treatment. Models that can capture the dynamic nature of treatment may be most appropriate but have been rarely applied [2].
Also poorly understood are variations in the relationship between treatment experiences and mortality according to whether all-cause versus cause-specific mortality is examined. Treatment is most likely to reduce illicit drug use in the short-term [5], which, in turn, may reduce immediate drug overdose risk. Over time, however, treatment-induced decreases in illicit drug use may reduce mortality risk due to infectious diseases (e.g., HIV, HCV) and also protect against death from cardiovascular disease [28], accidents, trauma, suicide [12,29], and other causes.
We aimed to calculate mortality rates among treated opioid-dependent individuals by cause and in relation to the general population, and to estimate the instantaneous effects of opioid detoxification and maintenance treatment on mortality– both all-cause and cause-specific.
Methods
Sample
We examined all individuals first admitted to publicly-funded agonist treatment for opioid dependence in California during the 5-year period covering January 1, 2006, to December 31, 2010. Treatment data was provided by the California Outcomes Monitoring System (CalOMS), a statewide information management system. Each state- or federally-funded opioid treatment program licensed to dispense methadone is required to submit CalOMS data monthly [30]. To focus on individuals being treated for the first time, we omitted from analysis individuals who had been admitted to treatment in the 20 years prior to January 1, 2006 as indicated by records available in CalOMS and its predecessor, CADDS. Patient data recorded in CalOMS by treatment staff at admission include demographics, alcohol and drug use, educational attainment and employment, and physical and psychological health. Discharge records are filed when appointments are missed without notification for ≥3 consecutive days for detoxification and for ≥14 days for MMT. Most individuals in our sample (86%) received treatment from only one treatment program during the study time-period.
Mortality data was obtained from the Centers for Disease Control and Prevention (CDC) National Death Index (NDI). NDI data linkage was performed by CDC staff using probabilistic record linkage methods that utilized patient Social Security Number (SSN), full name, birth date, and sex. Approximately 5% of CalOMS individuals had an invalid SSN and therefore were omitted from NDI linkage. In November 2012, NDI shared date and cause of death (International Classification of Diseases [ICD-10th revision]) for deaths that occurred as of December 31, 2010. Protocols were approved by the Institutional Review Boards at UCLA and the State of California.
Measures
The key independent variable is episodes of time in which an individual received detoxification, methadone maintenance treatment (MMT), or no-treatment. Following previous analyses [24], we used the earliest admission and latest discharge to consolidate records into treatment episodes. If records were unavailable for episode t, but a subsequent episode t+1 was initiated, discharge dates were imputed using a discharge date of (episode start date(t+1)–14) for episode t for MMT or (episode start date(t+1)–3 for detoxification. About 11% (5,749 of 52,769) of treatment episode discharge dates were imputed. We merged successive episodes when discharge and subsequent admission dates were within the 3-day (detoxification) and 14-day (MMT) discontinuation thresholds. Detoxification episodes directly preceding MMT episodes were not merged as transition from detoxification to MMT was of interest. Time periods in which an individual was not receiving either detoxification or MMT were coded as out-of-treatment periods.
The dependent variable is time to death, stratified by cause. Using previously-defined classifications [12], we coded cause of death into three categories: (1) drug-related (drug or alcohol poisoning, other drug-related); (2) HIV- and HCV-related; and (3) all other causes (Appendix 1 presents details). Following prior research [16,31,32], deaths occurring on or prior to discharge were allocated to “in-treatment” time-periods; deaths occurring anytime after discharge were attributed to “out-of-treatment” time-periods.
Finally, we considered several fixed and time-varying covariates. Fixed covariates (e.g., age, gender) were drawn from the first treatment admission. Time-varying measures were provided by repeated assessment at each admission and reflect patient demographics, drug-use severity, and co-morbidity (Table 4 shows complete list).
Table 4. Factors associated with mortality among individuals accessing pharmacological treatment for opioid dependence in California, 2006-2010.
(n=90,509 episodes as experienced by 32,222 individuals, of whom 1,031 died)
| All-cause (n=1,031) | Cause-specific | |||
|---|---|---|---|---|
| Drug-related (n=450) | HCV/HIV (n=57) | Other causes (n=524) | ||
| Model | 1a | 2ai | 2bi | 2ci |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Episode type (ref. out-of-treatment)ˆ | ||||
| Detoxification | 0.22 (0.13, 0.36) | 0.12 (0.05, 0.28) | 0.28 (0.04, 2.24) | 0.34 (0.18, 0.64) |
| Maintenance treatment | 0.27 (0.23, 0.32) | 0.24 (0.18, 0.33) | 0.19 (0.09, 0.40) | 0.30 (0.23, 0.37) |
| Primary drug (ref. daily heroin)ˆ | ||||
| Daily prescription opioids | 1.02 (0.86, 1.22) | 0.84 (0.65, 1.09) | 1.11 (0.48, 2.56) | 1.23 (0.96, 1.58) |
| Non-daily prescription opioids | 0.78 (0.62, 0.99) | 0.57 (0.39, 0.82) | na | 1.13 (0.82, 1.55) |
| Non-daily heroin | 1.14 (0.97, 1.35) | 0.95 (0.74, 1.22) | 1.28 (0.68, 2.39) | 1.34 (1.07, 1.67) |
| Model | 1b | 2aii | 2bii | 2cii |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Episode type (ref. out-of-treatment)ˆ | ||||
| Detoxification with no prior maintenance treatment | 0.21 (0.13, 0.35) | 0.11 (0.05, 0.27) | 0.28# (0.03, 2.22) | 0.33 (0.17, 0.65) |
| Detoxification with prior maintenance treatment | 0.63 (0.16, 2.53) | 0.62 (0.09, 4.45) | 0.69 (0.10, 4.91) | |
| Maintenance treatment with no prior detoxification | 0.30 (0.25, 0.37) | 0.26 (0.18, 0.36) | 0.17 (0.07, 0.41) | 0.34 (0.26, 0.44) |
| Maintenance treatment with prior detoxification | 0.20 (0.14, 0.28) | 0.21 (0.12, 0.35) | 0.25 (0.08, 0.82) | 0.19 (0.11, 0.31) |
| Primary drug (ref. daily heroin)ˆ | ||||
| Daily prescription opioids | 1.02 (0.86, 1.22) | 0.84 (0.65, 1.09) | 1.11 (0.48, 2.56) | 1.24 (0.96, 1.58) |
| Non-daily prescription opioids | 0.79 (0.62, 1.01) | 0.57 (0.39, 0.83) | na | 1.15 (0.84, 1.59) |
| Non-daily heroin | 1.15 (0.98, 1.35) | 0.95 (0.74, 1.23) | 1.28 (0.68, 2.38) | 1.34 (1.07, 1.68) |
time-varying variable. HR= Hazard Ratio; 95% CI = 95% confidence interval. Bolded values are statistically significant.
24 observations were deleted due to missingness.
Other variables included in each model and statistically significant but not shown above include: age, gender, race/ethnicity, has a disability,ˆ labor force status,ˆ Medi-Cal beneficiary,ˆ mentally ill,ˆ has hepatitis C,ˆ has tuberculosis,ˆ hospital stay in past 30 days,ˆ been tested for HIV.ˆ
Other variables included in each model but not statistically significant and not shown above include: educational attainment, years from 1st primary drug use to 1st treatment episode,ˆ criminal justice system involved,ˆ and secondary drug type.ˆ
Due to the relatively few HCV/HIV-related deaths, detoxification with and without prior MMT were collapsed into one category when treatment experiences were examined (Model 2bii).
Data analysis
Follow-up duration was determined using first treatment admission to death or last observation (ending on December 31, 2010). Crude mortality rates (CMRs) were calculated by summing person years and numbers of deaths by age and sex and calculating a rate per 1,000 person-years. Indirect standardized mortality ratios (SMR) were calculated by dividing observed deaths in the cohort by expected deaths based on US population mortality rates (as provided by the Centers for Disease Control and Prevention, National Vital Statistics System) by year, sex, and age group.
Cox proportional hazards models with time-varying covariates were fitted to the arranged in-treatment and out-of-treatment episodes to investigate the instantaneous effects of detoxification and MMT (defined as time-varying covariates) on all-cause and cause-specific mortality [33], controlling for covariates. For each model, we examined the effect of detoxification and maintenance (reference group: out-of-treatment) on mortality risk. We then considered the effect of four mutually exclusive states (reference group: out-of-treatment): MMT with prior detoxification, MMT-only, detoxification-only, and detoxification with prior MMT. We also conducted sensitivity analyses, using the Wei-Lin-Weissfeld method (robust standard error estimates), to evaluate how the patterns of treatment effects on all-cause and cause-specific mortality would be affected after accounting for the clustering of individuals within programs. All hypotheses were tested using a significance level of α=0.05. Analyses were conducted using SAS 9.3 [34] and R [35].
Results
Among 32,322 individuals, there were 1,031 deaths (3.2%) over the 5-year follow-up (76,657 person years, median observation 2.6 years [interquartile range: 1.4 - 3.7]). Compared to individuals who remained alive, those who died were older at first treatment (43.3 vs. 35.0 years), fewer were female (25.1% vs. 36.1%), fewer were working (21.2% vs. 30.7%), and more had co-occurring mental and physical health problems (Table 1). Additionally, more deceased individuals identified heroin as their primary drug problem (70.7% vs. 63.1%) and more used their primary drug for 10+ years before initiating treatment (64.4% vs. 45.2%).
Table 1. Patient characteristics at first treatment admission.
| Died (n=1,031) | Did not die (n=31,291) | Total (n=32,322) | |
|---|---|---|---|
|
| |||
| Mean (SD) / % | Mean (SD) / % | Mean (SD) / % | |
| Age in years at admission*** | 43.3 (12.9) | 35.0 (12.3) | 35.3 (12.4) |
| Female*** | 25.1 | 36.1 | 35.8 |
| Race/ethnicity: Hispanic | 23.5 | 24.3 | 24.2 |
| White | 60.8 | 61.1 | 61.1 |
| African American* | 9.6 | 7.8 | 7.8 |
| Other | 6.1 | 6.9 | 6.9 |
| Education: < High School | 31.1 | 29.9 | 30.0 |
| > High School/equivalent | 68.9 | 70.1 | 70.1 |
| Labor force participation*** | 21.2 | 30.7 | 30.4 |
| Legal status | 14.8 | 14.6 | 14.6 |
| Age at first use: <16*** | 16.1 | 15.7 | 15.7 |
| 16-21 | 35.3 | 40.6 | 40.5 |
| 21-30 | 22.9 | 26.5 | 26.3 |
| >30 | 25.6 | 17.3 | 17.5 |
| Injection drug user*** | 67.1 | 54.8 | 55.2 |
| Primary drug type: Heroin*** | 70.7 | 63.1 | 63.4 |
| Other drugs | 29.3 | 36.9 | 36.7 |
| Primary drug use frequency: < Daily | 21.9 | 22.1 | 22.1 |
| Daily | 78.1 | 77.9 | 77.9 |
| Secondary drug type: Heroin*** | 2.1 | 2.0 | 2.0 |
| Prescription opioids | 12.1 | 14.8 | 14.8 |
| Methamphetamine/cocaine | 18.5 | 15.2 | 15.3 |
| Marijuana | 4.4 | 6.6 | 6.6 |
| Alcohol | 7.2 | 4.6 | 4.6 |
| None | 55.7 | 56.8 | 56.8 |
| Years from 1st primary drug use to 1st treatment episode is <5 years*** | 21.3 | 33.9 | 33.5 |
| >= 5 and <10 years | 14.4 | 20.9 | 20.7 |
| >=10 years | 64.4 | 45.2 | 45.8 |
| Mental illness*** | 30.3 | 22.8 | 23.1 |
| Medical problems, past 30 days*** | 28.0 | 18.7 | 19.0 |
| Has a disability*** | 30.4 | 15.3 | 15.8 |
| Diagnosed with HCV*** | 24.5 | 12.2 | 12.6 |
| Diagnosed with tuberculosis*** | 4.1 | 2.1 | 2.1 |
| Tested for HIV*** | 73.1 | 65.1 | 65.4 |
| Medi-Cal Beneficiary*** | 36.1 | 26.8 | 27.1 |
Note: There were missing responses on years from first primary drug use to first treatment episode (N=11) and age at first use (N=11); figures indicate known status.
p <0.05;
p <0.01;
p <0.001
The single leading cause of death was drug- or alcohol-related (43.6%) (Figure 1 and Appendix 2). HCV and HIV-related illness accounted for 4.2% and 1.4% of deaths, respectively. Among the 50.8% that died of “other” causes, cardiovascular disease (14.3%) accounted for a significant proportion, as did trauma (suicide, unintentional injury, homicide) (10.1%), and other causes (26.5%), primarily cancer (7.8%), respiratory disease (5.2%), and liver disease (4.8%).
Figure 1. Crude mortality rates by cause of death according to in-treatment and out-of-treatment periods.
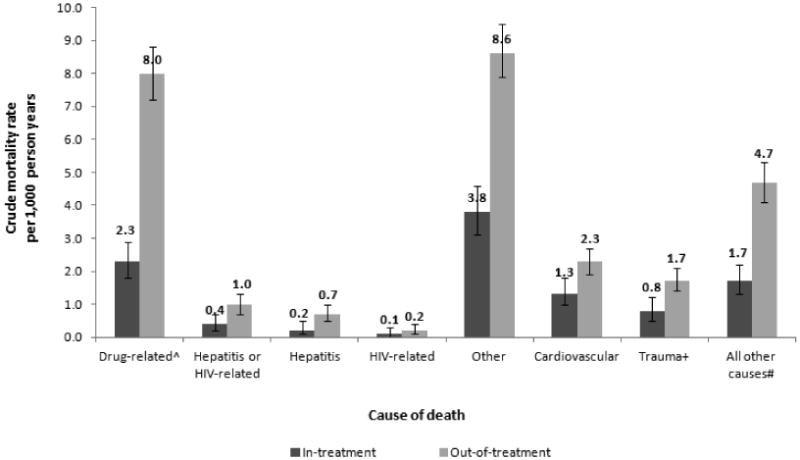
ˆ overdose (accidental poisoning by alcohol or other drugs), other drug-related (harmful alcohol or drug use or dependence)
+ suicide (intentional self-harm or self-poisoning), homicide, injury (accidental injury, traffic accidents)
# cancer, respiratory disease, liver disease, diabetes, infections/parasites, endometriosis, digestive disease, renal disease, central nervous system, other, and unknown
See Appendix 1 for ICD-10 codes incldued in each category of mortality.
Approximately 17.7% of deaths occurred while the patient was in-treatment; 10.4% within 14 days post-admission. About 82.3% of deaths occurred out-of-treatment; 14.7% within 14 days post- exit. Being in-treatment was associated with lower CMRs due to drug-related death (CMR 2.3, [95% CI 1.8, 2.9] vs. 8.0 [7.2, 8.8]) and other causes (CMR 3.8, 95% CI 3.1, 4.6 vs. 8.6, 7.9, 9.5) (Figure 1). HIV was an infrequent cause of death, whether in- or out-of-treatment.
Over 5 years, 32,322 individuals accounted for 90,509 episodes of detoxification (N=24,601; 27.2%), MMT (N=28,168; 31.1%), and no-treatment (N=37,740; 41.7%). For both the alive and deceased groups, more time was spent in MMT (36%) than in detoxification (∼7%) (Table 2). Deceased individuals accumulated fewer treatment days (237.0 vs. 325.3 mean days) prior to death, despite having had the same number of treatment episodes (1.6). About two-thirds of individuals in both groups had only one treatment episode and most of follow-up was spent out-of-treatment (56% and 57% of the time, respectively). Most treatment sequences were “detoxification-only” (25%), followed by “MMT-only” (19%) and “MMT preceded by detoxification” (11%); few were “detoxification preceded by MMT” (2%).
Table 2. Patient experiences with treatment over the 5-year follow-up period.
| Died (n=1,031 people, 2,924 episodes) | Did not die (n=31,291 people, 87,585 episodes) | Total (n=32,322 people, 90,509 episodes) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean / % | SD | Mean / % | SD | Mean / % | SD | |
| Total number of days in treatment*** | 237.0 | 316.1 | 325.3 | 414.4 | 322.5 | 411.9 |
| Days in detoxification*** | 24.4 | 60.6 | 37.2 | 106.5 | 36.8 | 105.3 |
| Days in maintenance*** | 212.6 | 315.4 | 288.1 | 409.9 | 285.6 | 407.4 |
| Total number of in-treatment episodes | 1.6 | 1.1 | 1.6 | 1.1 | 1.6 | 1.1 |
| Detoxification episodes | 0.7 | 1.0 | 0.8 | 1.0 | 0.8 | 1.0 |
| Maintenance episodes | 0.8 | 0.8 | 0.9 | 0.8 | 0.9 | 0.8 |
| Number of in-treatment episodes is… | ||||||
| 1 | 64.5 | 61.3 | 61.4 | |||
| 2 | 23.5 | 25.1 | 25.0 | |||
| 3 | 8.0 | 8.1 | 8.1 | |||
| 4+ | 4.0 | 5.5 | 5.5 | |||
| Total proportion of time in treatment | 0.44 | 0.39 | 0.43 | 0.40 | 0.43 | 0.40 |
| Proportion of time in detoxification | 0.08 | 0.18 | 0.07 | 0.17 | 0.07 | 0.17 |
| Proportion of time in maintenance | 0.36 | 0.40 | 0.36 | 0.40 | 0.36 | 0.40 |
| Proportion of episodes in which patient received | ||||||
| Detoxification with no prior maintenance treatment (“detoxification only”) | 22.9 | 25.0 | 25.0 | |||
| Maintenance treatment with no prior detoxification (“maintenance only”) | 19.9 | 19.8 | 19.8 | |||
| Maintenance treatment with prior detoxification (recommended treatment sequence) | 10.0 | 11.4 | 11.3 | |||
| Detoxification with prior maintenance treatment | 2.4 | 2.3 | 2.3 | |||
p<0.001
There was a more than four-fold increase of mortality risk among opioid-dependent individuals compared to the general population (SMR 4.5, 95% CI 4.2, 4.8) (Table 3). The overall in-treament SMR was 1.8 (95% CI 1.6, 2.1), compared with the overall out-of-treatment SMR of 6.1 (95% CI 5.7, 6.5); thus the relative risk of death out-of-treatment was 3.3 (95% CI: 2.8, 3.9). The highest mortality risk occurred during the two weeks post-treatment exit -- individuals incurred about 30 times the number of deaths during this time-period than is expected in the general population (SMR 31.5, 95% CI 26.2, 37.5). Mortality risk dropped sharply during the subsequent weeks, however 28 or more days post-exit the rate was still more than 5 times higher than in the general population (SMR 5.3, 95% CI 4.9, 5.7). As for time-periods following treatment entry, mortality risk was highest during the two weeks post-admission (SMR 3.6, 95% CI 2.2, 5.7), then decreased and remained relatively low thereafter. When patterns were examined by treatment type - risk was higher while individuals were in detoxification (SMR 2.4, 95% CI 1.5, 3.8) than in MMT (SMR 1.8, 95% CI 1.5, 2.1), and this difference in risk was most apparent during the two weeks post-treatment entry (SMR 5.5, 95% CI: 2.7, 9.8 versus SMR 2.5, 95% CI:1.7, 4.9).
Table 3. Crude mortality rates and standardized mortality ratios by key strata.
| Variable | Freq. | No. deaths | PY follow-up | CMR | 95% CI | SMR | 95% CI | ||
|---|---|---|---|---|---|---|---|---|---|
| Gender | |||||||||
| Male | 20758 | 772 | 49324 | 15.7 | 14.6 | 16.8 | 4.3 | 4.0 | 4.6 |
| Female | 11564 | 259 | 27332 | 9.5 | 8.4 | 10.7 | 5.1 | 4.5 | 5.7 |
|
| |||||||||
| Age | |||||||||
| <18-30 | 13625 | 209 | 30484 | 6.9 | 6.0 | 7.9 | 6.5 | 5.6 | 7.4 |
| 30-40 | 7106 | 170 | 17074 | 10.0 | 8.6 | 11.6 | 6.5 | 5.6 | 7.6 |
| 40-50 | 6419 | 270 | 16655 | 16.2 | 14.4 | 18.3 | 5.1 | 4.5 | 5.8 |
| >50 | 5172 | 382 | 12444 | 30.7 | 27.8 | 33.9 | 3.2 | 2.9 | 3.5 |
|
| |||||||||
| Race/ethnicity | |||||||||
| White | 19744 | 627 | 45658 | 13.7 | 12.7 | 14.9 | 5.4 | 5.0 | 5.8 |
| Hispanic | 7832 | 242 | 19371 | 12.5 | 11.0 | 14.2 | 4.0 | 3.5 | 4.5 |
| African American | 2528 | 99 | 6149 | 16.1 | 13.2 | 19.6 | 3.1 | 2.5 | 3.7 |
| Other | 2218 | 63 | 5478 | 11.5 | 9.0 | 14.7 | 2.9 | 2.2 | 3.6 |
|
| |||||||||
| Unemployed | |||||||||
| No | 9812 | 219 | 25252 | 8.7 | 7.6 | 9.9 | 3.7 | 3.2 | 4.2 |
| Yes | 22510 | 812 | 51405 | 15.8 | 14.7 | 16.9 | 4.7 | 4.4 | 5.1 |
|
| |||||||||
| IV drug user | |||||||||
| No | 14495 | 339 | 33237 | 10.2 | 9.2 | 11.3 | 3.7 | 3.3 | 4.1 |
| Yes | 17827 | 692 | 43420 | 15.9 | 14.8 | 17.2 | 5.0 | 4.6 | 5.4 |
|
| |||||||||
| Medi-Cal beneficiary | |||||||||
| No | 23579 | 659 | 56456 | 11.7 | 10.8 | 12.6 | 4.5 | 4.2 | 4.8 |
| Yes | 8743 | 372 | 20201 | 18.4 | 16.6 | 20.4 | 4.4 | 4.0 | 4.9 |
|
| |||||||||
| Has mental illness | |||||||||
| No | 25805 | 766 | 61797 | 12.4 | 11.5 | 13.3 | 4.0 | 3.7 | 4.3 |
| Yes | 6517 | 265 | 14860 | 17.8 | 15.8 | 20.1 | 6.4 | 5.7 | 7.3 |
|
| |||||||||
| Died in treatment - overall | 183 | 28535 | 6.4 | 5.5 | 7.4 | 1.8 | 1.6 | 2.1 | |
| 1 to 14 days after admit | 19 | 1790 | 10.6 | 6.8 | 16.6 | 3.6 | 2.2 | 5.7 | |
| 15 to 28 days after admit | 8 | 1300 | 6.2 | 3.1 | 12.3 | 2.1 | 0.9 | 4.1 | |
| >28 days after admit | 156 | 25445 | 6.1 | 5.2 | 7.2 | 1.7 | 1.5 | 2.0 | |
|
| |||||||||
| Died in detoxification - overall | 20 | 3258 | 6.1 | 4.0 | 9.5 | 2.4 | 1.5 | 3.8 | |
| 1 to 14 days after admit | 11 | 767 | 14.4 | 7.9 | 25.9 | 5.5 | 2.7 | 9.8 | |
| 15 to 28 days after admit | 1 | 373 | 2.7 | 0.4 | 19.0 | 1.1 | 0.0 | 6.0 | |
| >28 days after admit | 8 | 2118 | 3.8 | 1.9 | 7.6 | 1.5 | 0.7 | 3.0 | |
|
| |||||||||
| Died in maintenance - overall | 163 | 25277 | 6.4 | 5.5 | 7.5 | 1.8 | 1.5 | 2.1 | |
| 1 to 14 days after admit | 8 | 1024 | 7.8 | 3.9 | 15.6 | 2.5 | 1.1 | 4.9 | |
| 15 to 28 days after admit | 7 | 926 | 7.6 | 3.6 | 15.8 | 2.4 | 1.0 | 4.9 | |
| >28 days after admit | 148 | 23327 | 6.3 | 5.4 | 7.5 | 1.7 | 1.5 | 2.0 | |
|
| |||||||||
| Died out of treatment –overall | 848 | 48122 | 17.6 | 16.5 | 18.8 | 6.1 | 5.7 | 6.5 | |
| 1 to 14 days after exit | 125 | 1398 | 89.4 | 75.0 | 106.5 | 31.5 | 26.2 | 37.5 | |
| 15 to 28 days after exit | 29 | 1474 | 22.8 | 15.8 | 32.7 | 8.0 | 5.4 | 11.5 | |
| >28 days after exit | 694 | 45449 | 15.3 | 14.2 | 16.4 | 5.3 | 4.9 | 5.7 | |
|
| |||||||||
| Total | 32322 | 1031 | 76657 | 13.4 | 12.7 | 14.3 | 4.5 | 4.2 | 4.8 |
PY: person-years; CMR: Crude Mortality Rate; SMR: Standardized Mortality Ratio; 95% CI: 95% confidence interval. The Poisson exact method was used to calculate 95% confidence intervals for SMRs.
Table 4 presents information on factors associated with mortality risk as identified by an all-cause model (Model 1a,b) and a cause-specific model stratified by drug-related causes (Model 2a), HCV/HIV-related causes (Model 2b), and all other causes (Model 2c).
In the all-cause model (Model 1a), exposure to detoxification (HR 0.22, 95% CI 0.13, 0.36) and MMT (HR 0.27, 95% CI 0.23, 0.32) was associated with a significant reduction in the hazard of mortality, compared to out-of-treatment periods. The comparative instantaneous effects of detoxification and MMT were not statistically different (p=0.42). When episodes were categorized to account for experiences with different treatments (Model 1b), detoxification-only (HR 0.21, 95% CI 0.13, 0.35) and MMT with prior detoxification (HR 0.20, 95% CI 0.14, 0.28) were each associated with a greater reduction in mortality risk than MMT-only (HR 0.30, 95% CI 0.25, 0.37). However, only the reduction effect of MMT with prior detoxification was statistically significantly greater than that of MMT-only (p=0.03).
In cause-specific models, a reduction in mortality risk due to drug-related causes (Model 2ai) was associated with exposure to detoxification (HR 0.12, 95% CI 0.05, 0.28) and MMT (HR 0.24, 95% CI 0.18, 0.33) (vs. no-treatment), with detoxification demonstrating a more protective but not statistically significant effect than MMT (p=0.12). In the alternative categorization of treatment, the greatest reduction in risk was associated with detoxification-only (HR 0.11, 95% CI 0.05, 0.27), followed by MMT with prior detoxification (HR 0.21, 95% CI 0.12, 0.35), and MMT-only (HR 0.26, 95% CI 0.18, 0.36) (Model 2aii). The reduction effects of detoxification-only and MMT with prior detoxification were not statistically significantly different from that of MMT-only (p=0.06 and 0.45, respectively). In addition, compared with daily heroin use, non-daily prescription opioid use was associated with a significantly reduced risk of drug-related death (HR 0.57, 95% CI 0.39, 0.82).
A significant decrease in risk of HCV/HIV-related death (Model 2bi) was associated with MMT exposure (vs. no-treatment) (HR 0.19, 95% CI 0.09, 0.40). The greatest reduction in risk was associated with MMT-only (HR 0.17, 95% CI 0.07, 0.41) and then MMT with prior detoxification (HR 0.25, 95% CI 0.08, 0.82) (Model 2bii). These two effects were not statistically significantly different (p=0.58).
As for death by “other” causes (Model 2ci), exposure to detoxification (HR 0.34, 95% CI 0.18, 0.64) and MMT (vs. no-treatment) (HR 0.30, 95% CI 0.23, 0.37) was associated with a reduction in risk, with detoxification demonstrating a less protective but not statistically significant effect than MMT (p=0.68). The greatest reduction in risk was associated with MMT with prior detoxification (HR 0.19, 95% CI 0.11, 0.31), followed by detoxification-only (HR 0.33, 95% CI 0.17, 0.65) and MMT-only (HR 0.34, 95% CI 0.26, 0.44) (Model 2cii). Only MMT with prior detoxification had a statistically significantly greater effect than MMT-only (p=0.03).
Finally, our sensitivity analyses indicated that the significance pattern of most treatment effects described above remained the same after the clustering of individuals within treatment programs was considered. As the single exception, for drug-related mortality, detoxification-only was associated with a significantly greater reduction in risk than MMT-only (p=0.04).
Discussion
We examined over 32,000 opioid treatment entrants across a statewide public treatment system for whom admissions and exits were tracked over time. Exposure to detoxification and maintenance treatment (versus being out-of-treatment) was associated with a lower all-cause and cause-specific mortality risk. While the instantaneous effects of detoxification and maintenance treatment were not statistically significantly different, extended exposure to treatment in a non-time-limited treatment program can reduce mortality substantially, and should be prioritized. Additionally, most deaths occurred during out-of-treatment time-periods, and mortality risk was greatest immediately following treatment entry and exit.
Taken together, findings indicate that to optimize the life-saving effects of pharmacological treatment for opioid dependence, it should be offered without time constraints to maximize its protective effects against mortality; and supplemented by interventions that target risk factors for mortality occurring immediately following treatment entry and exit. These might include proactive efforts to support individuals during vulnerable periods [36], such as checking-up on the well-being of individuals and re-engaging them in treatment when needed.
In addition, the large sample size and the era in which data were collected enabled examination of overall and cause-specific mortality in relation to certain patient characteristics that are of particular salience given recent changes in the nature of opioid addiction. Compared with daily heroin use, non-daily prescription opioid use was associated with a reduced risk of drug-related death. Findings are most likely explained by differences in addiction severity, with non-daily prescription opioid use posing a less severe threat to health than daily heroin use. It may also be the case that treated prescription opioid patients have curtailed behaviors that increase overdose risk, such as use of certain prescription drugs; multiple prescriptions, providers, and pharmacies; and high daily doses [37].
Finally, most individuals (∼45%) initiated treatment 10 or more years after first heroin use. Other studies report few individuals with addiction receive any treatment in their first decade of use [25,38,39], even though treatment can facilitate abstinence [25,38,39] particularly if it is received soon after drug use onset [25]. In the present study, longer time from first use to first treatment was not associated with mortality risk. However, given that prolonged opioid use careers increase exposure to injection drug use and other risky health behaviors, more concerted efforts are needed to encourage individuals to initiate treatment for opioid dependence sooner after first use.
Limitations
Our analysis had several limitations. First, some misclassification is inherent in using administrative databases for research purposes. We implemented several rules and used previously-implemented algorithms to minimize linkage and data management errors [24]. Second, factors that have been associated with longer MMT durations including medication dosage and other treatment aspects (e.g., counseling services) were unobserved. Also, we only captured treatment provided at publicly-funded facilities in California. Therefore, we did not measure the effects of treatment provided in other settings (e.g., office-based buprenorphine treatment, Veterans Health Administration-based opioid treatment programs). Also, selection into detoxification or maintenance treatment may have been influenced by unmeasured factors. We expect that MMT individuals had greater addiction severity and co-morbidity; if measured incompletely and effects are as hypothesized, instantaneous MMT effects were likely understated. Finally, the median observation time was 2.6 years and instantaneous effects during treatment were measured. Three or more treatments distributed over many years before sustaining abstinence is typical [26,27], heroin abstinence for 5 or more years substantially increases the likelihood of continued abstinence [26], and individuals receive MMT much longer than detoxification. Therefore, if observed over a longer time horizon the cumulative protective effect of MMT on mortality may be greater than demonstrated by the present study. Study strengths include the large and ethnically diverse sample, inclusion of all public opioid treatment programs statewide, a comprehensive set of patient- and treatment-related risk and protective factors, and measurement of several variables as time-dynamic, thereby permitting more accurate measurement.
Prior research has examined the extent to which the addiction treatment career impacts abstinence and criminal activity [3,25,26,38]. Whether and how opioid treatment careers affect mortality risk is less understood. Findings extend knowledge of the extent to which maintenance and detoxification treatments impact mortality risk among opioid users, particularly within the current changing environment of opioid addiction in the United States.
Acknowledgments
Supported by: NIDA grant number R01DA031727 (PI: Nosyk) & P30DA016383 (PI: Hser).
Appendix 1. Causes of Mortality, by ICD-10 Codes
| Raw category | ICD-10 Codes | Coded category | N | % of total |
|---|---|---|---|---|
| Poisoning by drugs or alcohol-accidental and intent not determined | X40, X41, X42, X44, x45, Y11, Y12, Y14 | Drug-related | 394 | 38% |
| Drug-related | F10.1, F10.2, F11.1, F11.2, F11.9, F14.1, F15.1, F19.1, F19.2, F19.9, X61, X62, X64, | Drug-related | 56 | 5% |
| Viral hepatitis | B16.9, B18.1, B18.2, B94.2 | Hepatitis | 43 | 4% |
| HIV-related | B20.1, B20.3, B20.6, B20.7, B20.8, B21.0, B21.2, B21.3, B22.2, B22.7, B24 | HIV-related | 14 | 1% |
| Cardiovascular | I10, I11.0, I11.9, I12.0, I13.1, I21.9, I25.0, I25.1, I25.5, I25.8, I25.9, I26.9, I28.1, I33.0, I35.0, I35.1, I35.9, I38, I42.0, I42.2, I42.9, I49.0, I49.9, I50.0, I51.4, I51.6, I51.7, I51.8, I51.9, I60.8, I61.9, I62.9, I64, I67.7, I69.8, I71.0, I73.9, I80.2, Q23.1 | Other | 147 | 14% |
| Suicide | X67, X70, X72, X73, X74, X78, X81, X83 | Other | 39 | 4% |
| Unintentional injury | V03.0, V03.1, V04.1, V05.9, V09.2, V13.4, V27.4, V43.5, V44.6, V47.5, V48.5, V57.5, V87.7, V89.2, V89.9, V94.3, W10, W18, W19, W65, W70, W80, X00, Y30, Y350, Y86 | Other-trauma | 47 | 5% |
| Homicide | X93, X94, X95, X99, Y08, Y09 | Other-trauma | 18 | 2% |
| Cancer | C02.9, C10.9, C16.9, C18.9, C21.0, C22.0, C22.1, C22.9, C25.9, C34.9, C43.9, C44.6, C50.9, C53.9, C55, C56, C61, C62.9, C64, C67.9, C71.9, C76.0, C78.6, C79.8, C85.1, C85.9, C91.1, C92.0 | Other-trauma | 80 | 8% |
| Respiratory | J15.4, J18.0, J18.1, J18.9, J43.9, J44.0, J44.9, J45.9, J46, J69.0, J82, J84.1, J84.9 | Other | 54 | 5% |
| Liver-related | K70.0, K70.1, K70.3, K70.4, K70.9, K72.1, K72.9, K74.6, K75.9, K76.6, K76.9 | Other | 49 | 5% |
| Other | D57.0, D68.9, D84.9, F01.1, F32.9, F54, L02.4, L89, M19.9, M32.1, M80.9, R56.8, R99, X47, X59.9 | Other | 28 | 3% |
| Diabetes | E10.1, E11.2, E11.9, E14.1, E14.5, E14.9 | Other | 13 | 1% |
| Infection & parasitic | A16.9, A19.9, A40.0, A41.9, A86, B94.8, B99 | Other | 12 | 1% |
| Endocrine, nutritional & metabolic | E03.9, E46, E66.8, E66.9, E78.5, E87.2 | Other | 10 | 1% |
| Digestive | K22.9, K55.9, K56.5, K59.0, K65.0, K81.0, K92.9 | Other | 7 | 1% |
| Renal | N03.9, N17.9, N18.0, N18.9, N39.0 | Other | 7 | 1% |
| Central nervous system | G00.2, G12.2, G35, G40.9, G47.3, G93.1, G96.9 | Other | 7 | 1% |
| Not found in ICD-10 codebook | K85.9, M72.6 | Other | 6 | 1% |
| Total | 1031 | 100% |
Appendix 2. Mortality, by cause according to episode type
| Total | Death occurred during time-period when patient was… | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||||||
| In-treatment | Out-of-treatment | ||||||||||||||
|
| |||||||||||||||
| n | % | CMR | 95% CI | n | % | CMR | 95% CI | n | % | CMR | 95% CI | ||||
| Drug-relatedˆ | 450 | 43.6 | 5.9 | 5.4 | 6.4 | 65 | 35.5 | 2.3 | 1.8 | 2.9 | 385 | 45.4 | 8.0 | 7.2 | 8.8 |
| Hepatitis or HIV-related | 57 | 5.5 | 0.7 | 0.6 | 1.0 | 10 | 5.5 | 0.4 | 0.2 | 0.7 | 47 | 5.5 | 1.0 | 0.7 | 1.3 |
| Hepatitis | 43 | 4.2 | 0.6 | 0.4 | 0.8 | 7 | 3.8 | 0.2 | 0.1 | 0.5 | 36 | 4.2 | 0.7 | 0.5 | 1.0 |
| HIV-related | 14 | 1.4 | 0.2 | 0.1 | 0.3 | 3 | 1.6 | 0.1 | 0.0 | 0.3 | 11 | 1.3 | 0.2 | 0.1 | 0.4 |
| Other | 524 | 50.8 | 6.8 | 6.3 | 7.4 | 108 | 59.0 | 3.8 | 3.1 | 4.6 | 416 | 49.1 | 8.6 | 7.9 | 9.5 |
| Cardiovascular | 147 | 14.3 | 1.9 | 1.6 | 2.3 | 38 | 20.8 | 1.3 | 1.0 | 1.8 | 109 | 12.9 | 2.3 | 1.9 | 2.7 |
| Trauma+ | 104 | 10.1 | 1.4 | 1.1 | 1.6 | 22 | 12.0 | 0.8 | 0.5 | 1.2 | 82 | 9.7 | 1.7 | 1.4 | 2.1 |
| All other causes# | 273 | 26.5 | 3.6 | 3.2 | 4.0 | 48 | 26.2 | 1.7 | 1.3 | 2.2 | 225 | 26.5 | 4.7 | 4.1 | 5.3 |
|
| |||||||||||||||
| Total | 1,031 | -- | 13.4 | 12.7 | 14.3 | 183 | 17.7 | 6.4 | 5.5 | 7.4 | 848 | 82.3 | 17.6 | 16.5 | 18.8 |
overdose (accidental poisoning by alcohol or other drugs), other drug-related (harmful alcohol or drug use or dependence)
suicide (intentional self-harm or self-poisoning), homicide, injury (accidental injury, traffic accidents)
cancer, respiratory disease, liver disease, diabetes, infections/parasites, endometriosis, digestive disease, renal disease, central nervous system, other, and unknown
See Appendix 1 for ICD-10 codes included in each category of mortality
References
- 1.Darke S, Mills KL, Ross J, Teesson M. Rates and correlates of mortality amongst heroin users: Findings from the Australian Treatment Outcome Study (ATOS), 2001–2009. Drug & Alcohol Dependence. 2011;15:190–195. doi: 10.1016/j.drugalcdep.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 2.Degenhardt L, Bucello C, Mathers B, Briegleb C, Ali H, Hickman M, McLaren J. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction. 2011;106:32–51. doi: 10.1111/j.1360-0443.2010.03140.x. [DOI] [PubMed] [Google Scholar]
- 3.Hser YI, Evans E, Grella C, Ling W, Anglin D. Long-term course of opioid addiction. Harvard Review of Psychiatry. doi: 10.1097/HRP.0000000000000052. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 4.Degenhardt L, Larney S, Randall D, Burns L, Hall W. Causes of death in a cohort treated for opioid dependence between 1985 and 2005. Addiction. 2014;109:90–99. doi: 10.1111/add.12337. [DOI] [PubMed] [Google Scholar]
- 5.Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: Available evidence to inform clinical practice and research. Journal of Substance Abuse Treatment. 2005;28:321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 6.Nosyk B, Anglin MD, Brissette S, Kerr T, Marsh D, Schackman BR, Wood E, Montaner JSG. A call for evidence-based medicine for the treatment of opioid dependence in North America. Health Aff (Millwood) 2013;32:1462–1469. doi: 10.1377/hlthaff.2012.0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Substance Abuse and Mental Health Services Administration. Medication-Assisted Treatment for Opioid Addiction: 2010 State Profiles, Substance Abuse and Mental Health Services Administration. [accessed 6 August 2014];2011 http://www.dpt.samhsa.gov/pdf/MedicationAssistedTreatmentForOpioidAddiction_2010StateProfiles03.pdf. Archived at http://www.webcitation.org/6S06Y5MNk on 21 August 2014.
- 8.NIH Consensus Statement. Effective medical treatment of opiate addiction. National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. JAMA. 1998;280:1936–43. [PubMed] [Google Scholar]
- 9.Cornish R, Macleod J, Strang J, Vickerman P, Hickman M. Risk of death during and after opiate substitution treatment in primary care: prospective observational study in UK General Practice Research Database. BMJ. 2010;341:c5475. doi: 10.1136/bmj.c5475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cousins G, Teljeur C, Motterlini N, McCowan C, Dimitrov BD, Fahey T. Risk of drug-related mortality during periods of transition in methadone maintenance treatment: a cohort study. J Subst Abuse Treat. 2011;41:252–60. doi: 10.1016/j.jsat.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Davoli M, Bargagli AM, Perucci CA, Schifano P, Belleudi V, Hickman M, et al. Risk of fatal overdose during and after specialist drug treatment: the VEdeTTE study, a national multi-site prospective cohort study. Addiction. 2007;102:1954–1959. doi: 10.1111/j.1360-0443.2007.02025.x. [DOI] [PubMed] [Google Scholar]
- 12.Degenhardt L, Randall D, Hall W, Law M, Butler T, Burns L. Mortality among clients of a state-wide opioid pharmacotherapy program over 20 years: Risk factors and lives saved. Drug Alcohol Depend. 2009;105:9–15. doi: 10.1016/j.drugalcdep.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 13.Teesson M, Ross J, Darke S, Lynskey M, Ali R, Ritter A, Cooke R. One year outcomes for heroin dependence: findings from the Australian Treatment Outcome Study (ATOS) Drug Alcohol Depend. 2006;83:174–80. doi: 10.1016/j.drugalcdep.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Werb D, Kerr T, Marsh D, Li K, Montaner J, Wood E. Effect of methadone treatment on incarceration rates among injection drug users. Eur Addict Res. 2008;14:143–9. doi: 10.1159/000130418. [DOI] [PubMed] [Google Scholar]
- 15.Gibson A, Degenhardt L, Mattick RP, Ali R, White J, O'Brien S. Exposure to opioid maintenance treatment reduces long-term mortality. Addiction. 2008;103:462–8. doi: 10.1111/j.1360-0443.2007.02090.x. [DOI] [PubMed] [Google Scholar]
- 16.Peles E, Schreiber S, Adelson M. 15-Year survival and retention of patients in a general hospital-affiliated methadone maintenance treatment (MMT) center in Israel. Drug Alcohol Depend. 2010;107:141–8. doi: 10.1016/j.drugalcdep.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 17.O'Connor PG. Methods of detoxification and their role in treating patients with opioid dependence. JAMA. 2005;294:961–963. doi: 10.1001/jama.294.8.961. [DOI] [PubMed] [Google Scholar]
- 18.Amato L, Minozzi S, Davoli M, Vecchi S, Ferri M, Mayet S. Psychosocial and pharmacological treatments versus pharmacological treatments for opioid detoxification. Cochrane Database Syst Rev. 2004;3:CD005031. doi: 10.1002/14651858.CD005031. [DOI] [PubMed] [Google Scholar]
- 19.Substance Abuse and Mental Health Services Administration. Detoxification and substance abuse treatment: A treatment improvement protocol TIP 45. [accessed 19 June 2013];2006 http://store.samhsa.gov/product/TIP-45-Detoxification-and-Substance-Abuse-Treatment/SMA12-4131. Archived at http://www.webcitation.org/6S06n8hGd on 21 August 2014.
- 20.Hser Y, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch Gen Psychiatry. 2001;58:503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- 21.McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 22.Stein MD, Friedmann PD. Optimizing opioid detoxification: rearranging deck chairs on the Titanic. J Addict Dis. 2007;26:1–2. doi: 10.1300/J069v26n02_01. [DOI] [PubMed] [Google Scholar]
- 23.Stephenson DK California Society of Addiction Medicine. Guideline for physicians working in California Opioid Treatment Programs. [accessed 08 August 2014];CSAM Committee on Treatment of Opioid Dependence: 2008. http://www.csam-asam.org/sites/default/files/csam_otpguideline_oct08.pdf. Archived at http://www.webcitation.org/6S06ugHhR on 21 August 2014.
- 24.Nosyk B, Li L, Evans E, Urada D, Huang D, Wood E, Rawson R, Hser YI. Utilization and outcomes of detoxification and maintenance treatment for opioid dependence in publicly-funded facilities in California, US: 1991-2012. Drug and Alcohol Dep. 2014;143:149–57. doi: 10.1016/j.drugalcdep.2014.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evans E, Li L, Grella C, Brecht ML, Hser YI. Developmental timing of first drug treatment and 10-year patterns of drug use. J Subst Abuse Treat. 2013;44:271–9. doi: 10.1016/j.jsat.2012.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hser YI. Predicting long-term stable recovery from heroin addiction: findings from a 33-year follow-up study. J Addict Dis. 2007;26:51–60. doi: 10.1300/J069v26n01_07. [DOI] [PubMed] [Google Scholar]
- 27.Scott CK, Foss MA, Dennis ML. Pathways in the relapse--treatment—recovery cycle over 3 years. J Subst Abuse Treat. 2005;28:S63–72. doi: 10.1016/j.jsat.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 28.Herning RI, Better WE, Tate K, Umbricht A, Preston KL, Cadet JL. Methadone treatment induces attenuation of cerebrovascular deficits associated with the prolonged abuse of cocaine and heroin. Neuropsychopharmacology. 2003;28:562–8. doi: 10.1038/sj.npp.1300073. [DOI] [PubMed] [Google Scholar]
- 29.Caplehorn JR, Dalton MS, Haldar F, Petrenas AM, Nisbet JG. Methadone maintenance and addicts' risk of fatal heroin overdose. Subst Use Misuse. 1996;31:177–196. doi: 10.3109/10826089609045806. [DOI] [PubMed] [Google Scholar]
- 30.California Alcohol and Drug Programs. California Outcomes Measurement Systems (CalOMS) Treatment Data Compliance Standards. [accessed 15 July 2013];2005 http://www.dhcs.ca.gov/provgovpart/Documents/FMAB/Contract_Information/Doc_3T-4/3S_CalOMS_Data_Compliance.pdf. Archived at http://www.webcitation.org/6S07RwyOZ on 21 August 2014.
- 31.Clausen T, Anchersen K, Waal H. Mortality prior to, during and after opioid maintenance treatment (OMT): a national prospective cross-registry study. Drug Alcohol Depend. 2007;94:151–7. doi: 10.1016/j.drugalcdep.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 32.Gibson A, Degenhardt L, Mattick RP, Ali R, White J, O'Brien S. Exposure to opioid maintenance treatment reduces long-term mortality. Addiction. 2008;103:462–8. doi: 10.1111/j.1360-0443.2007.02090.x. [DOI] [PubMed] [Google Scholar]
- 33.Lau B, Cole SR, Gange SJ. Competing risk regression models for epidemiologic data. Am J Epidemiol. 2009;170:244–56. doi: 10.1093/aje/kwp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.SAS Institute Inc. SAS 9.3. [accessed 18 August 2014];2013 http://www.sas.com/en_us/home.html. Archived at http://www.webcitation.org/6S05KcmrH on 21 August 2014.
- 35.R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2014. [accessed 21 August 2014]. http://www.R-project.org. Archived at http://www.webcitation.org/6S04eoAYm on 21 August 2014. [Google Scholar]
- 36.Clausen T. Mortality is reduced while on opiate maintenance treatment, but there is a temporary increase in mortality immediately after starting and stopping treatment, a finding that may vary by setting. Evidence Based Medicine. 2011;16(3):94–95. doi: 10.1136/ebm1184. [DOI] [PubMed] [Google Scholar]
- 37.Paulozzi LJ, Kilbourne EM, Shah NG, Nolte KB, Desai HA, Landen MG, et al. A history of being prescribed controlled substances and risk of drug overdose death. Pain Med. 2012;13:87–95. doi: 10.1111/j.1526-4637.2011.01260.x. [DOI] [PubMed] [Google Scholar]
- 38.Brecht ML, Huang D, Evans E, Hser YI. Polydrug use and implications for longitudinal research: ten-year trajectories for heroin, cocaine, and methamphetamine users. Drug Alcohol Depend. 2008;96:193–201. doi: 10.1016/j.drugalcdep.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hser YI, Evans E, Huang D, Brecht ML, Li L. Comparing the dynamic course of heroin, cocaine, and methamphetamine use over 10 years. Addict Behav. 2008;33:1581–1589. doi: 10.1016/j.addbeh.2008.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]


