Abstract
Background
Previous research has shown that overweight Latino children underestimate their body size. Erroneous perception of body size may have important health and behavioral implications and serve as a significant barrier to weight control.
Objective
The aim of this study was to determine whether children’s perceptions of their body size became more accurate following a pediatric obesity intervention focused on increasing physical activity.
Design/Methods
This analysis includes 61 overweight (body mass index ≥85%) Latino children (aged 8–11 years) parent-child dyads who completed a pilot randomized control trial.
Results
After the intervention, 40.7% (11/27) of children in the intervention group rated their body size accurately compared to 21.2% (7/33) in the control group. The difference indicates a trend towards significance (P = .09).
Conclusions
Participating in monthly physical activity skill building sessions may increase children’s accuracy in body size perception. This may be an important first step towards behavior modification.
Keywords: Obesity, Body Mass Index, Physical Activity, Hispanic Americans, Randomized Controlled Trial
BACKGROUND
The prevalence of obesity has more than tripled for children aged 6 to 11 years over the past 3 decades.1 The National Health and Nutrition Survey found that nearly 21% of children ages 2 to 5 and 30% of children ages 6 to 19 are overweight or at risk for becoming overweight.2 The health risks of overweight and obesity in childhood are well-established and include the onset of type 2 diabetes, hypertension, hyperlipidemia, abnormal glucose tolerance, and psychosocial problems such as weight prejudice.3 Moreover, overweight children are significantly more likely to become overweight adults: 26% to 41% of adults who are overweight were obese in preschool and 42% to 63% were obese in elementary school.4 One study showed approximately 80% of children who were overweight at age 10 to 15 years were obese adults at age 25 years.5 In fact, some have argued that obesity in adulthood is perhaps the most serious consequence of childhood obesity, because it is linked with increased mortality and morbidity.6 The national “Healthy People 2010” initiative calls for a reduction of 50% or more in the numbers of overweight children and adolescents.7 With only 1 year until 2010, given the numbers of overweight children, the trajectory looks dire unless new promising approaches are identified.
Latinos of all ages are disproportionately affected by overweight, with up to 27% of Latino children have body mass indices (BMIs) ≥95th percentile.8 This difference could be attributable to differences in energy expenditure (physical activity) and energy intake (nutrition) among this ethnic group,9 but a cultural component likely affects the perception of obesity and its related health consequences. In several studies, Latino adults have been found to be inaccurate in their perceptions of their own overweight.10,11 In several studies, Latina mothers not only had difficulty recognizing overweight among their children but they did not see the links between health and weight.12,13 A recent study showed that whereas parents frequently did not see their children’s overweight, their children were even less likely to recognize their own body sizes correctly.11 In a study of low-income Latinas and their children aged 5 to 7 years, all of the women selected a relatively thin body image as the most desirable and healthy for themselves but preferred a plumper figure for their children.14 These findings indicate that Latina mothers may have a more favorable view of childhood obesity and may fail to perceive overweight in their children as problematic.
A number of studies have evaluated and supported the strong links between perceived body size and the attempt to regulate weight.15,16 A study in Britain found that among adolescents the impact of their own weight perception on perceived pressure to lose weight was nearly 5 times greater than measured BMI.17 Erroneous perception of body size may have important health and behavioral implications by posing a significant barrier for intended and actual behavioral changes toward weight control. Understanding this and other potential mechanisms that may influence the adoption and maintenance of positive health behaviors is necessary for the development and implementation of optimal obesity prevention and/or treatment interventions.
Using a community-engaged, culturally-relevant, family-centered approach as called for by the Institute of Medicine18 and the “Strategic Plan for NIH Obesity Research,”19 we developed and implemented a culturally-meaningful pediatric obesity intervention located at a community recreation center and designed for Latino families with overweight children aged 8 to 11 years. The intervention was not designed to address body size perception, but we were interested in examining whether the intervention had an effect on how accurately children saw their body size over time. In this study, we examined whether children’s perceptions of their body size became more accurate following the 6-month intervention focused on increasing physical activity.
METHODS
Participants
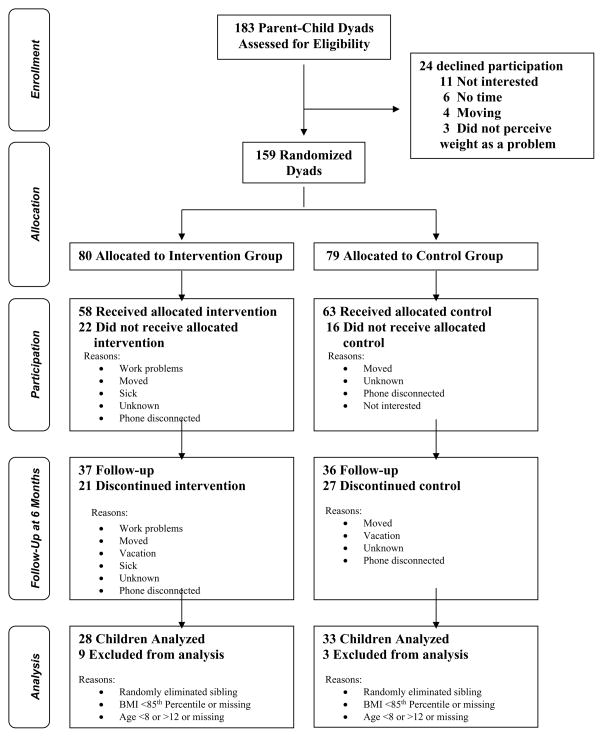
Latino children (defined as having a parent born in Latin America) 8 to 11 years of age with a BMI ≥85th percentile for age and gender were identified from community sources in Forsyth County, North Carolina including a primary care clinic, radio advertising, and local churches. Eligibility criteria required that participants read at a third grade level or greater and could be reached by telephone during the study. Each child needed to have at least one adult family member (>18 years) participate. The majority of participating families were migrant farm workers. Informed consent for adults and assent for children were obtained verbally. Figure 1 displays the participant flow through the study. This study was reviewed and approved by the Institutional Review Board of Wake Forest University Health Sciences.
Figure 1.
Flow of participants through the trial
Study Design
We conducted a randomized control trial in which the unit of randomization was the child-parent dyad.
Data Collection
Data were collected at 3 time points: baseline, 6 months, and 12 months. Here we report on the comparison of intervention and control group from baseline to 6 months (ie, see page 4, during the time of the active intervention). All baseline and control group data were collected at a community-based primary care clinic. The 6-month data for the intervention group were collected at a recreation center. Free transportation and childcare for other children were available to participating families.
Measures
Body size
Body Mass Index (BMI, defined as weight in kilograms divided by the square of height in meters3) served as the primary measure of adiposity. Standing height was measured using a portable direct-reading stadiometer and body weight was measured using a digital scale. Because the amount of body fat varies for children by age and between girls and boys, BMI percentile for age and gender was calculated using the CDC calculator20 and analyzed instead of raw BMI.
Perceived body size
Children were shown pictures of child body sizes and asked to select the image that most looked like their own. The picture scale ranged from 1 to 7, where 1 and 2 were considered underweight, 3 and 4 were considered by health providers to be the ideal body size, 5 was considered to be overweight, and 6 and 7 were considered to be obese.21 This scale is significantly and highly correlated with measured percentage overweight (r=0.79).21
Intervention Group
Intervention parent-child dyads participated in 6 monthly sessions between baseline and 6-month follow-up. The first session occurred in a clinic and included (a) height and weight measurement with standardized instrumentation, (b) survey completion with adults completing self-administered surveys separately from their children in the language of their choice, (c) use of an activity van to “try out” activities (eg, hoola hoop, hackey sack), (d) completion of a pre-visit brief 1-page survey reporting on activity behaviors, (e) a group medical interview applying brief principles of motivational interviewing (with 2 families/interview), (f) completion of a reciprocal contract with clear activity goals set, and (g) a 45-minute session on healthy lifestyles. The remaining 5 clinics occurred at a local recreation center. These hour-long monthly sessions included (a) a 20-minute skills building teaching session (eg, how to recognize if you are exercising enough or too much during aerobic activity; how to warm-up and cool-down; how to avoid dehydration; how to utilize a recreation facility; how to avoid cramps); (b) a 30 minute group activity to practice the skills taught (eg, soccer, dance, volleyball, and outdoor games); and (c) and the completion of a reciprocal activity contract with clear goal setting. Discussion of body sizes was not part of the curriculum, nor did it arise in conversation throughout the sessions. The skills building topics and exercises incorporated into the sessions were informed by three focus groups with Latino parents and children. All sessions were led by the same bilingual Latina program manager to ensure treatment fidelity across sessions.
Control Group
Control parent-child dyads participated in a baseline and 6-month follow-up session. At each session, each dyad received standard of care counseling from physicians trained using American Academy of Pediatrics guidelines.22 This was followed by a 45-minute group health education session led by a trained bilingual Latina program manager who provided general information about healthy lifestyles.
ANALYSIS
To remove the presence of siblings from the data (and thus correlation between specific pairs of children), 1 child was randomly chosen from each of the 5 pairs of siblings present in the data to be included in the analysis. In turn, the subset of data used for the analysis consisted of the 61 children who met the inclusion/exclusion criteria and had both a baseline and 6-month visit. Each child’s “true” body size was determined by their measured BMI-for-age percentile at baseline - it was assumed a child’s BMI would not change drastically enough from baseline to 6 months to move them from one BMI-for-age percentile group to the other (≥85% to <95%, and ≥95%). A child with a BMI-for-age percentile ≥85% and <95% had a corresponding “true” body size of 5, whereas a child with a BMI-for-age percentile ≥95% has a “true” body size of 6 or 7. It was then determined whether each child’s perceived body image was accurate (ie, matched their true body size) at both baseline and 6 months.
Nonparametric Wilcoxon rank-sum and Pearson χ2 (without a continuity correction) tests were used to test for differences in the baseline demographics between the intervention and control groups. Both 2-sided and 1-sided tests of proportion were used to test for differences in the proportion of children with an accurate body image both within and between treatment groups. P values <.05 were considered statistically significant and no adjustments for multiple comparisons were made.
RESULTS
As mentioned, the reported results are based on the 61 children who met the inclusion/exclusion criteria and had both a baseline and 6-month visit. Most children (80%, 49/61) had ≥95% BMI with a mean age of 9.6 years (standard deviation [SD] = 1.1). Refer to Table 1 for child demographics. Mean adult BMI was 33.2 (SD= 7.6). Mean age was 33.0 years (SD=7.5). Of the participating adults, the majority were mothers (94%, 45/48), and from Mexico (76%, 35/46). The majority of participating adults (98%, 44/45) reported speaking predominately Spanish both at home and with friends suggesting they had a lower degree of acculturation.
Table 1.
Baseline Demographics of Completer Children (1 Child From Each Sibling Pair Randomly Removed).
| Control (N = 33) | Intervention (N = 28) | Combined (N = 61) | p-value | |
|---|---|---|---|---|
| Age in years (mean ± SD) | 9.7 ± 1.1 | 9.6 ± 1.1 | 9.6 ± 1.1 | .76a |
|
| ||||
| Gender | ||||
| Male | 64% (21/33) | 46% (13/28) | 56% (34/61) | .18b |
|
| ||||
| Female | 36% (12/33) | 54% (15/28) | 44% (27/61) | |
|
| ||||
| BMI in kg/m2 (mean ± SD) | 26.5 ± 5.4 | 25.5 ± 4.4 | 26.0 ± 5.0 | .66a |
|
| ||||
| BMI-for-age percentile (mean ± SD) | 96.9 ± 2.8 | 95.6 ± 4.0 | 96.3 ± 3.4 | .40a |
|
| ||||
| Dichotomized BMI-for-age percentile | ||||
| ≥ 85% and < 95% | 12% (4/33) | 29% (8/28) | 20% (12/61) | .11b |
|
| ||||
| ≥ 95% | 88% (29/33) | 71% (20/28) | 80% (49/61) | |
Wilcoxon rank-sum test
Pearson χ2 (without a continuity correction) test.
At baseline, 39.3% (24/61) of the children underestimated their body size compared to the judgments health providers would have made given their BMI percentile for age and gender. Also at baseline, children in the intervention and control groups were similar in how accurately they perceived their own body size, (intervention) 32.1% (9/28) vs (control) 27.3% (9/33), P = .89. Refer to Table 2 for the distribution of the perceived body sizes within each treatment group at baseline and follow-up.
Table 2.
Perceived Body Size Within Each Treatment Group at Both Time Pointsa
| Body type that looks most like me | Baseline Control (N=33) | 6 Month Control (N=33) | Baseline Intervention (N=28) | 6 Month Intervention (N=28) |
|---|---|---|---|---|
| 1. Underweight | 0 (0/33) | 0 (0/33) | 4 (1/28) | 0 (0/27) |
| 2. Underweight | 3 (1/33) | 0 (0/33) | 0 (0/28) | 4 (1/27) |
| 3. Healthy | 6 (2/33) | 0 (0/33) | 0 (0/28) | 4 (1/27) |
| 4. Healthy | 33 (11/33) | 33 (11/33) | 32 (9/28) | 26 (7/27) |
| 5. ≥ 85% and < 95% overweight | 33 (11/33) | 45 (15/33) | 40 (10/28) | 33 (9/27) |
| 6. ≥ 95% obese | 12 (4/33) | 21 (7/33) | 20 (7/28) | 26 (7/27) |
| 7. ≥ 95% obese | 12 (4/33) | 0 (0/33) | 4 (1/28) | 7 (2/27) |
Values are given as percentage. The values in parentheses indicate number of participants/total number of participants in the group.
At 6 months, 40.7% (11/27) in the intervention group rated their body size accurately compared to 21.2% (7/33) in the control group. In this pilot study, the difference indicates a trend towards significance (P = .09). The raw proportions support a trend in children in the intervention group having more accurate perceptions of their own body size after the 6-month culturally-tailored intervention promoting physical activity whereas the control group is shifted in the opposite direction (Refer to Table 3).
Table 3.
Accuracy of Perceived Body Image Within Each Treatment Group at Both Time Points
| Treatment group | Percentage (n) | |||
|---|---|---|---|---|
| Visit | Accurate | Inaccurate | Total | |
| Control | Baseline | 27.3% (9) | 72.7% (24) | 33 |
| 6 months | 21.2% (7) | 78.8% (26) | 33 | |
| Intervention | Baseline | 32.1% (9) | 67.9% (19) | 28 |
| 6 months | 40.7% (11) | 59.3% (16) | 27 | |
We looked for differences by gender but did not find any.
DISCUSSION
This exploratory study offers insights regarding an obesity intervention seeking to increase physical activity in an understudied population: Latino children. To date, there are very few pediatric obesity programs that successfully decrease obesity23–25 and almost no information on what works in Latino children. This study suggests that a skills-based monthly intervention over the course of six months, focused on physical activity, led children to reevaluate their body size and perceive their weight more accurately.
With previous research indicating that there is a strong association between self-perceived weight status and weight control behavior, often independent of objective weight status, self-perceived weight may be an important point of focus for the design and implementation of pediatric obesity interventions. It is noteworthy that the intervention never addressed body image, neither in the curriculum nor in the discussions that developed, and thus a curriculum that explicitly address body image may have a stronger effect. For Latino children to choose to actively participate in early obesity intervention efforts or to modify their daily physical activity and nutritional intake outside of a formal program, they must first be aware of their own overweight. In one of the few studies examining associations between weight perceptions and adaptive weight loss efforts, rather than maladaptive efforts, perceiving oneself to be overweight was a strong correlate for weight loss attempts by both men and women.26 It is still unknown what the effect of self-perceived weight has on weight loss behaviors of children.
Limitations
Given the prevalence of pediatric obesity, especially among Latino children, study participants might have considered their weight as just right because they are surrounded by obese children in their daily lives. BMI is only a proxy for body composition. It does not distinguish between the ratios of muscle versus fat mass, which children may be taking into consideration when evaluation the appropriateness of their own body size. Thus future work should address perceptions of degree of adiposity as well as body shape.
New Contribution to the Literature
In Latino preadolescents, inaccurate body size perception can be modified to be more accurate without explicit reference to body image through participation in monthly classes focused on developing physical activity skills. This may be a useful method to correct misperceptions.
Directions for Future Research
Further research is needed to determine the utility of targeting accuracy of self-perceived weight status as a motivator for weight loss among children in pediatric obesity interventions and prevention interventions. Future studies should also attempt to delineate the meaning and implications of body size and adiposity perceptions, which are likely to be multifactorial and have repercussions for health through behavior.
Acknowledgments
This study was funded by a research grant from the National Institutes of Health (NICHD Grant No. R21 HD050990-02, SLB Principal Investigator) and The Collaborative to Strengthen Families and Neighborhoods, funded in part by The Duke Endowment.
The authors thank Angelica Guzman, Irma Richardson, Erica Reynolds, and Valentina Intagliata for project management and data collection; Winston-Salem YMCA collaborators Florence Corpening, Robin Ervin, and Teresa Mason for their support throughout study implementation; and the Downtown Health Plaza, Winston-Salem, NC, for their support during study recruitment.
Contributor Information
Sabina B. Gesell, Division of General Pediatrics, Vanderbilt University School of Medicine.
Theresa A. Scott, Department of Biostatistics, Vanderbilt University School of Medicine.
Shari L. Barkin, Division of General Pediatrics, Vanderbilt University School of Medicine.
References
- 1.Institute of Medicine. Preventing Childhood Obesity: Health in the Balance. Washington, DC: National Academies Press; 2004. Committee on Prevention of Obesity in Children and Youth. [Google Scholar]
- 2.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288:1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 3.Dietz WH, Robinson TN. Use of the body mass index (BMI) as a measure of overweight in children and adolescents. J Pediatr. 1998;132:191–193. doi: 10.1016/s0022-3476(98)70426-3. [DOI] [PubMed] [Google Scholar]
- 4.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22:167–177. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 5.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 6.National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health risk. Arch Intern Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services. Healthy People 2010. Washington, DC: US Department of Health and Human Services; 2000. pp. 225–247. [Google Scholar]
- 8.Suminski RR, Poston WS, Jackson AS, Foreyt JP. Early identification of Mexican American children who are at risk for becoming obese. Int J Obes Relat Metab Disord. 1999;23:823–829. doi: 10.1038/sj.ijo.0800933. [DOI] [PubMed] [Google Scholar]
- 9.Fitzgibbon ML, Stolley MR, Dyer AR, VanHorn L, KauferChristoffel K. A community-based obesity prevention program for minority children: rationale and study design for Hip-Hop to Health Jr. Prev Med. 2002;34:289–297. doi: 10.1006/pmed.2001.0977. [DOI] [PubMed] [Google Scholar]
- 10.Yancey AK, Simon PA, McCarthy WJ, Lightstone AS, Fielding JE. Ethnic and sex variations in overweight self-perception: Relationship to sedentariness. Obesity. 2006;14:980–988. doi: 10.1038/oby.2006.112. [DOI] [PubMed] [Google Scholar]
- 11.Intagliata V, Ip EH, Gesell SB, Barkin SL. Accuracy of self- and parental perception of overweight among Latino preadolescents. N C Med J. 2008;69:88–91. [PMC free article] [PubMed] [Google Scholar]
- 12.Crawford PB, Gosliner W, Anderson C, et al. Counseling Latina mothers of preschool children about weight issues: suggestions for a new framework. J Am Diet Assoc. 2004;104:387–394. doi: 10.1016/j.jada.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Ariza AJ, Chen EH, Binns HJ, Christoffel KK. Risk factors for overweight in five- to six-year-old Hispanic-American children: a pilot study. J Urban Health. 2004;81:150–161. doi: 10.1093/jurban/jth091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Contento IR, Basch C, Zybert P. Body image, weight, and food choices of Latina women and their young children. J Nutr Educ Behav. 2003;35:236–248. doi: 10.1016/s1499-4046(06)60054-7. [DOI] [PubMed] [Google Scholar]
- 15.McCabe MP, Ricciardelli LA. Body image and strategies to lose weight and increase muscle among boys and girls. Health Psychol. 2003;22:39–46. [PubMed] [Google Scholar]
- 16.Ricciardelli LA, McCabe MP. Children’s body image concerns and eating disturbance: a review of the literature. Clin Psychol Rev. 2001;21:325–344. doi: 10.1016/s0272-7358(99)00051-3. [DOI] [PubMed] [Google Scholar]
- 17.Gillison F, Standage M, Skevington S. Relationships among adolescents’ weight perceptions, exercise goals, exercise motivation, quality of life and leisure-time exercise behavior: a self-determination theory approach. Health Education Research. 2006;21:836–847. doi: 10.1093/her/cyl139. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine. Progress in Preventing Childhood Obesity: How do we measure up? Washington, DC: The National Academies Press; 2006. Committee on Progress in Preventing Childhood Obesity. [Google Scholar]
- 19.US Department of Health and Human Services. Strategic Plan for NIH Obesity Research: A Report of the NIH Obesity Research Task Force. Rockville, MD: National Institutes of Health; 2004. [Google Scholar]
- 20.Centers for Disease Control and Prevention. [Accessed December 6, 2007];BMI calculator for child and teen: English version. http://apps.nccd.cdc.gov/dnpabmi/Calculator.aspx.
- 21.Bulik CM, Wade TD, Heath AC, Martin NG, Stunkard AJ, Eaves LJ. Relating body mass index to figural stimuli: population-based normative data for Caucasians. Int J Obes Relat Metab Disord. 2001;25:1517–1524. doi: 10.1038/sj.ijo.0801742. [DOI] [PubMed] [Google Scholar]
- 22.Barlow SE, Dietz WH. Obesity evaluation and treatment: Expert Committee recommendations. The Maternal and Child Health Bureau, Health Resources and Services Administration and the Department of Health and Human Services. Pediatrics. 1998 Sep;102(3):E29. doi: 10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 23.Summerbell CD, Ashton V, Campbell KJ, Edmunds L, Kelly S, Waters E. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2003;(3):CD001872. doi: 10.1002/14651858.DC001872. [DOI] [PubMed] [Google Scholar]
- 24.Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database of Syst Rev. 2005;(3):CD001871. doi: 10.1002/14651858.DC001871. [DOI] [PubMed] [Google Scholar]
- 25.Thomas H. Obesity prevention programs for children and youth: why are their results so modest? Health Educ Res. 2006;21:783–795. doi: 10.1093/her/cyl143. [DOI] [PubMed] [Google Scholar]
- 26.Lemon SC, Rosal MC, Zapka J, Borg A, Anderson V. Contributions of weight perceptinos to weight loss attempts: differences by body mass index and gender. Body Image. 2008;6:90–96. doi: 10.1016/j.bodyim.2008.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]