Abstract
Opioid antagonists are pharmacological tools applied as an indirect measure to detect activation of the endogenous opioid system (EOS) in experimental pain models. The objective of this systematic review was to examine the effect of mu-opioid-receptor (MOR) antagonists in placebo-controlled, double-blind studies using ʻinhibitoryʼ or ʻsensitizingʼ, physiological test paradigms in healthy human subjects. The databases PubMed and Embase were searched according to predefined criteria. Out of a total of 2,142 records, 63 studies (1,477 subjects [male/female ratio = 1.5]) were considered relevant. Twenty-five studies utilized ʻinhibitoryʼ test paradigms (ITP) and 38 studies utilized ʻsensitizingʼ test paradigms (STP). The ITP-studies were characterized as conditioning modulation models (22 studies) and repetitive transcranial magnetic stimulation models (rTMS; 3 studies), and, the STP-studies as secondary hyperalgesia models (6 studies), ʻpainʼ models (25 studies), summation models (2 studies), nociceptive reflex models (3 studies) and miscellaneous models (2 studies). A consistent reversal of analgesia by a MOR-antagonist was demonstrated in 10 of the 25 ITP-studies, including stress-induced analgesia and rTMS. In the remaining 14 conditioning modulation studies either absence of effects or ambiguous effects by MOR-antagonists, were observed. In the STP-studies, no effect of the opioid-blockade could be demonstrated in 5 out of 6 secondary hyperalgesia studies. The direction of MOR-antagonist dependent effects upon pain ratings, threshold assessments and somatosensory evoked potentials (SSEP), did not appear consistent in 28 out of 32 ʻpainʼ model studies. In conclusion, only in 2 experimental human pain models, i.e., stress-induced analgesia and rTMS, administration of MOR-antagonist demonstrated a consistent effect, presumably mediated by an EOS-dependent mechanisms of analgesia and hyperalgesia.
Introduction
Human experimental pain models are essential in physiological and pharmacological research, testing hypothetical pain mechanisms, forward-translating observations from animal research or establishing evidence of analgesic drug efficacy. A number of receptor-specific agonists and antagonists are utilized as adjuncts investigating physiologic mechanisms behind pain inhibition and pain sensitization. Research has focused on various receptors, e.g., α2-receptors, 5-HT1A-receptors, NMDA-receptors and TRPV1-receptors, but above all, major interest has been dedicated to the endogenous mu-opioid-receptor (MOR). Selective MOR-antagonists have been used in a large number of human experimental [1–63] and clinical studies [64]. Early animal data demonstrated that MOR-antagonists increase nociceptive responding across various stimulation paradigms and species [61]. Subsequent studies in monkeys and humans showed that microinjections of morphine [65] or electrical stimulation [66] of the periaqueductal grey area (PAG) produced marked analgesia, which could effectively be antagonized by systemic administration of naloxone [67].
In human experimental pain models the research involving MOR-antagonists has primarily focused on pain thresholds and tolerance to pain stimuli, conceptualizing the idea that activity of the EOS hypothetically could be responsible for an attenuation of the responses to pain [43]. Consequently the administration of MOR-antagonist could indirectly substantiate or question the involvement of the EOS in acute experimental pain perception. Since results from the literature on the effect of MOR-antagonists on experimental pain seem ambiguous [57,61], the authors decided to undertake a systematic review separating the search data into studies utilizing ʻinhibitoryʼ test paradigms and ʻsensitizingʼ test paradigms. The main objective was to examine if certain physiological stimulation paradigms, techniques or methods could be modulated by naloxone or naltrexone, which is considered presumptive evidence of activation of the EOS. The primary outcomes were direct measures of experimental pain perception (pain ratings, pain thresholds, pain tolerance, hyperalgesia) or indirect measures of nociception (neuroimaging responses [BOLD (blood-oxygen-level dependent) contrast imaging, fMRI, PET], nociceptive reflexes [NRF], somatosensory evoked potentials [SSEP]). The secondary outcomes were autonomic measures of pain and nociception (autonomic, hemodynamic and neuroendocrine responses).
Materials and Methods
2.1 Registration and Search Strategy
The review was registered in the PROSPERO international database (CRD42014013102; http://www.crd.york.ac.uk/PROSPERO/DisplayPDF.php?ID=CRD42014013102). Only placebo-controlled, double-blind, experimental studies, including healthy human subjects, examining the effect of MOR-antagonists on pain inhibition and pain sensitization, were considered. It was required that the studies employed physiological stimuli, i.e., chemical, electrical, mechanical, pharmacological, thermal or a combination of stimuli. Psychological conditioning stimuli, often applied in placebo or behavioral studies, were not included in this review. Studies primarily concerning acupuncture, cardiovascular reactivity, clinical outcomes, endocrine functions, psychological or psychiatric outcomes and substance abuse, as well as, non-English studies, abstracts from scientific meetings and material from textbooks were not included. Studies with opioid-administration prior to administration of the MOR-antagonist were not included.
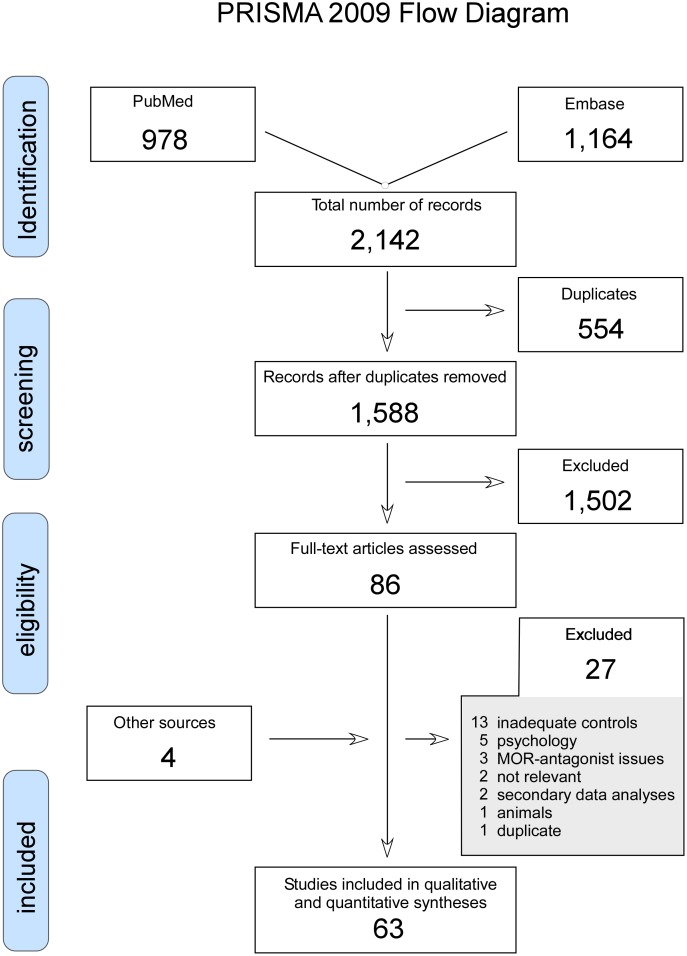
A literature search (LPHA, MPP, MUW) was performed in the databases PubMed and EMBASE (search completed August 8, 2014) using the following search terms: (pain OR pain measurement OR pain threshold OR pain perception OR pain sensitization OR pain inhibition OR pain summation OR pain conditioning OR pain habituation OR pain modulation OR secondary hyperalgesia OR hyperalgesia OR diffuse noxious inhibitory controls OR diffuse noxious inhibitory control OR DNIC) AND (levallorphan OR naloxone OR naltrexone OR methyl-naltrexone OR alvimopan OR diprenorphine OR meptazinol OR Receptors, Opioid, mu/antagonists and inhibitors OR mu-opioid receptor antagonist OR mu opiate receptor antagonist) AND (healthy OR subjects OR control group OR normal OR normals OR double-blind placebo controlled OR double-blind method). Reference-lists from retrieved studies were searched for additional relevant material (MUW). No contact with study authors to identify additional studies was made. In case of uncertainty concerning relevance of an article, the subject was discussed between the authors and a final decision was taken by the senior author (MUW). From the 2,142 records 86 full-text articles were assessed for eligibility. Sixty-three relevant studies were included in the review (Fig 1: PRISMA 2009 Flow Diagram). Assessing risk of bias was made by the Oxford quality scoring system [68] (MPP, MUW). Descriptive data and outcome data were extracted from these studies and accumulated in tables (MUW) and verified independently (MPP, LPHA). The PRISMA 2009 Checklist is in a supporting file (S1 PRISMA Checklist).
Fig 1. The search algorithm according to the PRISMA-requirements [126].
2.2 Definitions
Preliminary examination of the retrieved studies indicated that a classification of the studies into ʻinhibitoryʼ and ʻsensitizingʼ test paradigms would facilitate the presentation and interpretation of data.
2.2.1 ʻInhibitoryʼ Test Paradigms (ITP)
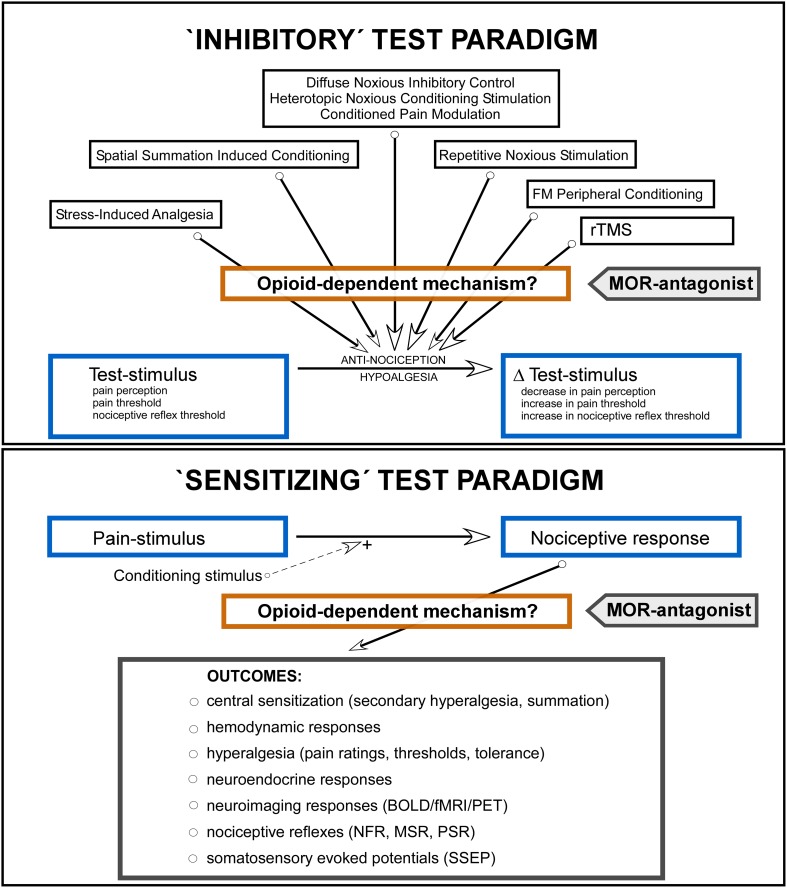
ITP-studies were characterized by implementation of a noxious or non-noxious inhibitory conditioning stimulus (Fig 2, upper panel; stress-induced analgesia [SIA], spatial summation induced conditioning, diffuse noxious inhibitory control [DNIC], heterotopic noxious conditioning stimulation, conditioned pain modulation [CPM], repetitive noxious stimulation, non-noxious frequency modulated peripheral conditioning and repetitive transcranial magnetic stimulation [rTMS]) [69]. The test-stimulus (Fig 2) was applied heterotopically, at a site different from the site of the conditioning stimulus, or homotopically, at the same site as the conditioning stimulus, where the test stimulus became an integrated part of the conditioning stimulus [19]. The response to the test-stimulus was evaluated by psychophysical measures, e.g., pain ratings, pain threshold and pain tolerance assessments, or physiological measures, e.g., the spinal nociceptive flexion reflex (RIII; Fig 2) [70]. The conditioning inhibitory effect was evaluated by the associated decrease in the response to the test-stimulus: △test-stimulus (Fig 2). MOR-antagonist was administered in order to indirectly uncover an EOS-dependent mechanism in the conditioning response: if the △test-stimulus was attenuated by the MOR-antagonist, a role of the EOS was presumed. In all the studies the outcomes were evaluated against baseline conditions and placebo-controls.
Fig 2. Schematic illustration of the ʻinhibitoryʼ test paradigms (ITP, upper panel) and the ʻsensitizingʼ test paradigms (STP, lower panel).
The ITP-studies employed an inhibitory conditioning stimulus with evaluation of the associated change in the applied test-stimulus (△test-stimulus). The objective of the ITP-studies was to examine the effect of mu-opioid-receptor (MOR) antagonist on the magnitude of the △test-stimulus, indicating an activation of the endogenous opioid system (EOS) responsible for the conditioning response leading to antinociception/hypoalgesia (the central rectangle [Opioid-dependent mechanism?] indicates a hypothetical augmentation of the conditioning response by the EOS). The STP-studies (lower panel) employed a pain stimulus leading to quantifiable ʻsensitizingʼ CNS-responses, e.g., changes in behavioral measures (hyperalgesia, pain ratings, thresholds, tolerance), nociceptive reflexes, neuroimaging or neuroendocrine variables. In a number of studies a sensitizing conditioning stimulus was applied, e.g., a burn injury [31] and application of capsaicin [35,36], enhancing the nociceptive responses. The objective of the STP-studies was to examine the effect of MOR-antagonist on the magnitude of elicited responses, indirectly either supporting or contradicting an effect mediated by the EOS (the central rectangle [Opioid-dependent mechanism?] indicates a hypothetical attenuation of the response by the EOS). FM Peripheral Conditioning = non-noxious Frequency Modulated Peripheral Conditioning; rTMS = repetitive Transcranial Magnetic Stimulation.
2.2.2 ʻSensitizingʼ Test Paradigms (STP)
STP-studies were characterized by implementation of a pain stimulus leading to quantifiable, ʻsensitizingʼ, nociceptive responses, i.e., changes in behavioral measures (hyperalgesia, pain ratings, thresholds, pain tolerance), thresholds of nociceptive reflexes, SSEP, or, miscellaneous neuroimaging or neuroendocrine variables (Fig 2, lower panel). In a number of the STP-studies an additional conditioning stimulus was applied, e.g., a burn injury [31] or capsaicin [35,36], enhancing the nociceptive response. MOR-antagonists were administered in order to indirectly uncover an EOS-dependent mechanism in the ʻsensitizingʼ nociceptive response: if the response was enhanced by the MOR-antagonist, an inhibitory role of the EOS was presumed. In all the studies the outcomes were evaluated against baseline conditions and placebo controls.
2.2.3 Habituation and Sensitization
The phenomenon by which repeated identical stimuli elicit progressively decrements in responses has been operationally defined as habituation [71]. The phenomenon by which repeated identical stimuli elicit progressively increments in responses is here defined as sensitization.
2.3 MOR-antagonists
The MOR-antagonists used in human research are alvimopan, diprenorphine, methylnaltrexone, naloxone and naltrexone. In addition, MOR-antagonists, or MOR-antagonists with partial κ-agonist effects, levallorphan, meptazinol and nalorphine, have been used in opioid blocking research. In the retrieved ITP- and STP-studies only naloxone and naltrexone were used.
Naloxone and naltrexone are non-specific opioid-antagonists with high affinity for the MOR [72]. Both drugs cross the blood-brain barrier and demonstrate central opioid-blocking effects, in contrast to the peripherally acting MOR-antagonists, e.g., alvimopan and methyl-naltrexone. Due to low systemic bioavailability of naloxone after oral administration, i.e., 2–3% [73], naloxone is given parenterally, when systemic opioid-blocking effects are required. In adults the distribution half-life (T½α) is 40 to 70 seconds [74], and the elimination (T½β) half-life is 54 to 64 min [74,75]. Naloxone, with a rapid onset and short duration of action, is suited for acute management of opioid-induced serious adverse effects [24] and is administered in IV doses of 0.04 mg to 0.4 mg [76]. Interestingly, naloxone expresses a dose-dependent, biphasic response with low doses producing analgesia and high doses producing hyperalgesia, both in animal inflammatory models [77] and in clinical models [78–80].
Naltrexone has a systemic bioavailability after oral administration of 5% to 60% [81] and since its main use clinically is treatment of substance dependence, the oral route is preferred. The elimination half-life of naltrexone and its active metabolite 6-beta-naltrexol, after oral administration is 4 to 10 hours [82]. Naltrexone is clinically given in daily doses of 50 to 100 mg.
Results
3.1 Literature Search
The search algorithm with the number of retrieved studies is presented in Fig 1. A total of 2,142 records were retrieved, and after subtracting 554 repeat entries, 1,588 records were considered for analysis. From these 1,502 records were not considered relevant for the review and therefore excluded. Eighty-six full text articles were assessed and of these 27 were excluded. Four additional studies were retrieved from reference lists and from consultation with experts in the field giving a total of 63 studies considered relevant for this review [1–63].
3.2 Research Areas
For the sake of clarity, data for ITP and STP are presented separately, each in a subsection.
3.2.1 ʻInhibitoryʼ Test Paradigms (25 studies)
The research areas were conditioning modulation models (22 studies) [1–22] and rTMS-models (3 studies) [23–25].
3.2.2 ʻSensitizingʼ Test Paradigms (38 studies)
The research areas were secondary hyperalgesia models (6 studies) [26–31], summation models (2 studies) [32,33], ʻpainʼ models (25 studies) [34–58], nociceptive reflex models (3 studies) [59–61] and miscellaneous (2 studies) [62,63].
3.3 Study Design
3.3.1 ʻInhibitoryʼ Test Paradigms
Study designs are presented in Table 1. All studies were double-blind and placebo-controlled, and, 17 of the 25 studies [1,2,6,8–10,12,14–17,20–25] were randomized. Four studies reported a counter-balanced design [6,9,20,21], while 19 studies reported use of a cross-over design [1,2,6,7,10–18,20–25]. Three studies, investigating rTMS-induced analgesia, used a sham-control [23–25]. One study used a control 25°C water-immersion test [21].
Table 1. ʻInhibitoryʼ Test Paradigms: Study Design.
| [Ref.] First Author | Year | Study Design | Primary Objective △ | Secondary Objective △ | Oxford Quality Score |
|---|---|---|---|---|---|
| ʻINHIBITORYʼ TEST PARADIGMS | |||||
| Conditioned Modulation Models | |||||
| [1] Willer JC | 1980 | DB, R, PC, 3-WX | Effect of Nx on stress-induced analgesia | NRR | 2 |
| [2] Willer JC | 1981 | DB, R, PC, 3-WX | Effect of Nx in stress-induced analgesia: pain reflexes | Effect of naloxone on development of hyperalgesia | 2 |
| [3] Pertovaara A | 1981 | DB, PC | Effect of Nx on dental pain threshold during non-painful high-frequency TENS | NRR | 1 |
| [4] Pertovaara A | 1982 | DB, PC | Effect of Nx on ischemia-induced pain reduction | Effect of naloxone on ischemia-induced changes in thermal sensitivity | 2 |
| [5] Willer JC | 1982 | DB, PC, | Effect on Nx on the depression on the nociceptive blink reflex induced by high frequency conditioning stimulation | NRR | 1 |
| [6] Pertovaara A | 1982 | DB, R, CB, PC, 2-WX | Effect of Nx on dental pain threshold during non-painful low-frequency TENS | NRR | 1 |
| [7] Buchsbaum MS | 1983 | DB, PC, 3-WX | Effect of Nx on pain sensitivity (assessed by EPs) before and after repeated electrical stimulation | NRR | 2 |
| [8] Jungkunz G | 1983 | DB, R, PC, 4-PG | Effect of Nx on cold pressor induced changes in electrical pain thresholds | Effect of naloxone on mentally stress induced changes in electrical pain thresholds | 3 |
| [9] Janal M | 1984 | DB, R, PC, CB | Effect of Nx on thermal and ischemic responses after exercise | NRR | 2 |
| [10] Willer JC | 1986 | DB, R, PC, 4-WX | Effect of Nx on stress-induced changes in nociceptive flexion reflex threshold | NRR | 2 |
| [11] Ernst M | 1986 | DB, PC, 2-WX | Effect of Nx on habituation to repeated noxious stimuli | NRR | 1 |
| [12] Willer JC | 1986 | DB, R, PC, 4-WX | Effect of Nx on habituation to repeated stress stimuli | Effect of naloxone on autonomic parameters during repeated stress stimuli | 2 |
| [13] Olausson B | 1986 | DB, PC, 2-WX, 4-SX | Effect of Nx on dental pain thresholds following low-frequency TNS | Effect of Nx on dental pain thresholds following muscular exercise | 2 |
| [14] Willer JC | 1990 | DB, R, PC, 2-WX | Effect of Nx on DNIC assessed by the nociceptive flexion reflex | NRR | 2 |
| [15] Poulsen L | 1996 | DB, R, PC, 2-WC, 4-SX | Effect of Nx on DNIC assessed by the nociceptive flexion reflex in extensive and poor metabolizers of sparteine (CYP2D6) | Effect of Nx on pain ratings during cold pressor test in extensive and poor metabolizers of sparteine (CYP2D6) | 2 |
| [16] Edwards RR | 2004 | DB, R, PC, 2-WX | Effect of Nx on DNIC | Effect of Nx on the relationship of cardiovascular reactivity and DNIC | 2 |
| [17] Julien N | 2006 | DB, R, PC, 4-WX | Effect of Nx on spatial summation induced activation of endogenous pain inhibitory system | NRR | 2 |
| [18] Robertson LJ | 2008 | DB, PC, 2-WX | Local effect of Nx on thermal hyperalgesia after a burn injury modified by repeated cold water immersions | NRR | 1 |
| [19] Rennefeld C | 2010 | DB, PC, 8-S | Effect of Nx on habituation to repeated pain stimuli | NRR | 1 |
| [20] Leonard G | 2010 | DB, R, PC, CB, 3-WX, 2-D | Effect of Nx on high-frequency TENS | NRR | 3 |
| [21] Sprenger C | 2011 | DB, R, PC, 2-WX, CB | Effect of Nx on HNCS ¤ induced by CWIT and evaluated by behavioral responses | Effect on Nx on HNCS ¤ induced by CWIT and evaluated by BOLD responses | 3 |
| [22] King CD | 2013 | DB, R, PC, 2-WX | Effect of NTx on CPM | NRR | 3 |
| Repetitive Transcranial Magnetic Stimulation Models | |||||
| [23] de Andrade DC | 2011 | DB, R, PC, SC, 2-WX, 3-PG | Effect of Nx on DLPFC/PMC- and M1-targeted repetitive transcranial magnetic stimulation induced analgesia | NRR | 3 |
| [24] Taylor JJ | 2012 | DB, R, PC, SC, 2x2-WX | Effect of Nx on LDPFC-targeted repetitive transcranial magnetic stimulation induced analgesia | NRR | 4 |
| [25] Taylor JJ | 2013 | DB, R, PC, SC, 2x2-WX | Effect of Nx on LDPFC-targeted repetitive transcranial magnetic stimulation induced analgesia | NRR | 5 |
△ Objectives related to the specific perspectives of the review.
¤ HNCS in man, DNIC in animals (the authors’ terminology [21]).
BI = first-degree burn injury; BOLD = blood-oxygen-level dependent contrast imaging; BTS = brief thermal sensitization; CB = counterbalanced; CPTT = cold pressor test; DB = double-blind; CYP2D6 = cytochrome P450 2D6 enzyme; CPM = conditioned pain modulation; DLPFC/PMC = right dorsolateral–prefrontal cortex premotor cortex (see LDPFC); DNIC = diffuse noxious inhibitory controls; EP = [somatosensory] evoked potentials; EPT = electrical pain threshold; EPIS = endogenous pain inhibitory system; fMRI = functional magnetic resonance imaging; HNCS = heterotopic noxious conditioning stimulations; IDES = intradermal electrical stimulation (rectangular, 0.5 ms duration, 2 Hz, high density); LDPFC = left dorsolateral prefrontal cortex; M1 = primary motor cortex; NFR = nociceptive flexion reflex; NRR = not relevant for the review; NTx = naltrexone; Nx = naloxone; OIH = opioid-induced hyperalgesia; R = randomized; PC = placebo-controlled; SB = single-blind; SBP = systolic blood pressure; SC = sham-controlled; SHA = secondary hyperalgesia area; SOWS = subjective opioid withdrawal scale; SSEP = EP; TCI = target-controlled infusion; TDES = transdermal electrical stimulation (low density); TENS = transcutaneous electrical nerve stimulation; X = cross-over (side to side); 2-D/3-D = two-/two-dose; 2-WX /3-WX/4-WC = two-/three-/four-way cross-over; 3-SX/4-SX/5-SX/6-SX = three-/four-/five-/six-session cross-over study; 8-S = eight session study; 2-PG/3-PG/4-PG/6-PG = two/three/four/six parallel-groups; 2x2-WX = 2 parallel groups each with a 2 way-cross over design.
3.3.2 ʻSensitizingʼ Test Paradigms
Study designs are presented in Table 2. All of the studies were placebo-controlled while 37 of the 38 studies were double-blind [26–37,39–63]. However, one study [37] mentions only blinding of the subjects, but the study is registered as a controlled clinical trial. Thirty of these studies were randomized [26–32,34–36,39–42,44–52,54–56,58,60,61,63], while 12 studies [35,37,38,41–43,48,50–53,57] used a counter-balanced design. Eight studies did not report a randomized design [33,37,38,43,53,57,59,62].
Table 2. ʻSensitizingʼ Test Paradigms: Study Design.
| [Ref.] First Author | Year | Study Design | Primary Objective △ | Secondary Objective △ | Oxford Quality Score |
|---|---|---|---|---|---|
| ʻSENSITIZINGʼ TEST PARADIGMS | |||||
| Secondary Hyperalgesia Models | |||||
| [26] Mikkelsen S | 1999 | DB, R, PC, 3-WX | Effect of pre-emptive Nx on ketamine-induced SHA | NRR | 5 |
| [27] Brennum J | 2001 | DB, R, PC, 3-WX, 2-D | Effect of Nx on SHA induced by BI | NRR | 3 |
| [28] Koppert W | 2003 | DB, R, PC, 4-WX | Effect of Nx on SHA/pain induced by IDES/TDES | NRR | 2 |
| [29] Koppert W | 2005 | DB, R, PC, † 4-SX, TCI | Effect of Nx on SHA/pain induced by IDES | NRR | 2 |
| [30] Chu FL | 2011 | DB, R, PC, 2-WX # | Effect of Nx on OIH induced by remifentanil | Effect of Nx on SHA/pain induced by IDES | 3 |
| [31] Pereira MP | 2013 | DB, R, PC, 2-WX | Effect of Nx on reinstatement of SHA induced by BI | Effect of Nx on SHA induced by BTS | 5 |
| Summation Models | |||||
| [32] Benedetti F | 1999 | DB, R, PC, 6-PG | Effect of Nx on spatially directed expectation of pain | NRR | 2 |
| [33] Price DD | 2002 | DB, PC, 4-PG | Effect of Nx on heat- and cold-induced temporal summation of second pain | Effect of Nx on first and second pain | 1 |
| ʻPainʼ Models | |||||
| Capsaicin: | |||||
| [34] Graven-Nielsen | 2002 | DB, R, PC, 2-WX | Effect of Nx on capsaicin-induced muscle pain | NRR | 2 |
| Capsaicin & heat: | |||||
| [35] Drummond PD | 2000 | CB, R, PC, 2-WX | Effect of iontophoretically applied Nx on capsaicin induced heat-sensitization | NRR | 1 |
| [36] Anderson WS | 2002 | DB, R, PC, 2-WX | Effect of Nx on capsaicin-induced pain kindled by heating | NRR | 3 |
| Comb. modalities, others: | |||||
| [37] Grevert P | 1978 | DB, CB, PC, 3-WX, 2-D, 2-PG | Effect of Nx on pain induced by ischemia and cold-water immersion | NRR | 1 |
| [38] McCubbin JA | 1994 | SB, CB, PC, 2-WX | Effect of Nx on pain rating for hand-grip challenge and cold pressor challenge | Effect of Nx on relationship between SBP and pain ratings. | 1 |
| [39] Stacher G | 1988 | DB, R, PC, 3-WX, 2-D | Effect of Nx on threshold and tolerance to electrically induced pain and threshold to heat-induced pain | NRR | 3 |
| [40] Younger JW | 2009 | DB, R, PC, 2-WX | Effect of NTx on changes in sensitivity to heat, cold, and mechanical pain | Effect of NTx on mood and opioid-withdrawal symptoms (SOWS) | 5 |
| [41] Bruehl S | 2012 | DB, R, PC, CB, 2-WX | Effect of Nx used as tool revealing endogenous opioid activity during ischemic and pressure pain tests | NRR | 2 |
| [42] Bruehl S | 2013 | DB, R, CB, PC, 3-SX | Effect of Nx used as tool revealing endogenous opioid activity during ischemic and heat pain tests | NRR | 3 |
| Electrical | |||||
| [43] El-Sobky A | 1976 | DB, CB, PC, 3-WX, 2-D | Effect of Nx on electrically induced pain threshold and tolerance | NRR | 1 |
| [44] Buchsbaum MS | 1977 | DB, R, PC, 2-WX | Effect of Nx on pain sensitivity after low to high intensity electrical stimulation | Effect of Nx on SSEP after low to high intensity electrical stimulation | 3 |
| [45] Bromm B | 1983 | DB, R, PC, 5-SX | Effect of Nx on pain sensitivity to phasic electrical stimuli | Effect of Nx on pain SSEP after single repeated electrical stimuli | 3 |
| Ischemia: | |||||
| [46] Grevert P | 1977 | DB, R, PC, 3-WX, 2-D | Effect of Nx on pain induced by the tourniquet test | NRR | 3 |
| [47] Grevert P | 1983 | DB, R, PC, 3-WX, 2-D | Effect of an 8 hr Nx-infusion on pain induced by the tourniquet test | Effect of 8 hr Nx-infusion on cortisol, β-endorhin and blood pressure | 2 |
| [48] Posner J | 1985 | DB, R, CB, PC, 6-SX | Effect of Nx on pain induced during the tourniquet test | NRR | 3 |
| Mechanical: | |||||
| [49] Schobel HP | 1998 | DB, R, PC, 2-WX | Effect of Nx on pain ratings to pinching stimuli | Effects of Nx on hemodynamic and sympathetic responses to pain | 2 |
| [50] Cook DB | 2000 | DB, R, CB, PC, 3-WX | Effect of NTx on pain induced by dynamic hand grip fatiguing exercise | Effect of NTx on sympathetic nerve activity during exercise | 3 |
| Thermal: | |||||
| [51] Lautenbacher S | 1990 | DB, R, CB, PC, 2-WX | Effect of Nx on pain induced by tonic and phasic heat stimuli | NRR | 2 |
| [52] Lautenbacher S | 1994 | DB, R, CB, PC, 2-WX | Effect of Nx on heat and cold pain thresholds, and vibratory thresholds | NRR | 2 |
| [53] Al’Absi M | 2004 | DB, CB, PC, 2-WX | Effect of NTx on pain induced by heat and CPTT | NRR | 2 |
| [54] Borras MC | 2004 | DB, R, PC, 2-WX | Effect of Nx on pain and CNS-responses (fMRI) to suprathreshold heat stimuli | 2 | |
| [55] Kern D | 2008 | DB, R, PC, 2x2-WX, | Effect of Nx on paradoxical pain induced by the “thermal grill” | Effect of Nx on thermal thresholds | 4 |
| [56] Kotlyar M | 2008 | DB, R, PC, 2-WX | Effect of NTx on pain induced by CPTT | Effect of NTx on sympathetic responses induced by CPTT | 3 |
| [57] Schoell ED | 2010 | DB, CB, PC, 2-WX | Effect of Nx on pain ratings and CNS-responses (BOLD) to suprathreshold heat stimuli | 2 | |
| [58] Pickering G | 2013 | DB, R, PC, 4-WX | Effect of Nx on pain induced by repeated heat stimuli | Effect of Nx on SSEP induced by heat | 5 |
| Nociceptive Reflex Models | |||||
| [59] Boreau F | 1978 | DB, PC | Effect of Nx on spinal reflexes | NRR | 1 |
| [60] France CR | 2005 | DB, R, PC, 2-WX | Effect of NTx on pain ratings, NFR thresholds and EPT assessments. | NRR | 3 |
| [61] France CR | 2007 | DB, R, PC, 2-WC | Effect of NTx on pain thresholds, pain tolerance and NFR recordings. | NRR | 3 |
| Miscellaneous Models | |||||
| [62] Eissenberg T | 2000 | DB, PC, 4-WX | Effect of NTx on reversal of oxycodone induced antihyperalgesia in UV-exposed skin | NRR | 2 |
| [63] Robertson LJ | 2007 | DB, R, PC, X | Local effect of Nx on opioid induced antihyperalgesia following a burn | NRR | 2 |
△ Objectives related to the specific perspectives of the review.
† ratio of placebo-treated vs. naloxone-treated was 0.5.
# study design is for remifentanil-placebo infusions.
For explanation of abbreviations, please refer to legend Table 1.
3.4 Quality Scoring
3.4.1 ʻInhibitoryʼ Test Paradigms
Evaluation was by the Oxford quality scoring system [68] (Table 1). The median (25–75% IQR) score was 2 (2 to 3). Seven out of 25 studies qualified for a score > 2 [8,20–25] and 6 studies for a score < 2 [3,5,6,11,18,19]. In 5 studies either the randomization [22,25] or the blinding procedure [7,13,24,25] was described, but in the remaining 20 studies no information on these procedures were presented. In 5 studies withdrawals and the reasons for withdrawing subjects were reported [8,13,21,24,25].
3.4.2 ʻSensitizingʼ Test Paradigms
Evaluation was by the Oxford quality scoring system (Table 2) [68]. The median (25–75% IQR) score was 2 (2 to 3). Eighteen of 38 studies qualified for a score > 2 [26,27,30,31,36,39,40,42,44–46,48,50,55,56,58,60,61] and 6 studies for a score < 2 [33,35,37,38,43,59]. In 6 [26,31,39,40,45,58] and 10 [26,31,40,42,46,48,50,55,56,58] studies, respectively, the randomization or the blinding procedure was described. In 26 studies no information on these procedures were presented [27–30,32–38,41,43,44,47,49,51–54,57,59–63]. However, 16 studies reported withdrawals and the reasons for withdrawing subjects [26,27,30,31,36–38,40,44,53,54,57,58,60–62].
3.5 Statistics
3.5.1 ʻInhibitoryʼ Test Paradigms
None of the 25 studies reported a priori sample size estimations. In 5 studies the confounding issue of limited sample size was discussed [15,16,18,20,22]. Effect size calculations with estimates of Cohen’s d and partial η2 (eta squared) [83] were reported in 2 studies [16,22]. In 3 studies corrections for multiple comparisons were made with the Bonferroni adjustment [24,25] and the Tukey-Kramer method [23], respectively. Association was estimated by the Pearson’s correlation coefficient (r) in 10 studies [1,2,4,6,11,14,16,18,21,22]. Analyses of variance (one-way/two-way/three-factor/repeated measures/mixed model ANOVAs) [7,9,12,14,16–19,22–25] or covariance [11] were performed in 13 out of the 25 studies.
3.5.2 ʻSensitizingʼ Test Paradigms
A priori sample size estimations were reported in 4 [27,31,40,50] of the 38 studies. Post-hoc sample size estimates [40] including analyses with Fisher’s post-hoc least significant difference (LSD) [49,55] were made in 3 studies. In 5 studies the issue of limited sample size was discussed [40,41,50,56,63]. Effect size calculations with estimates of Cohen’s d and partial η2 were reported in 2 studies [33,50] and with correlation coefficients in 1 study [41]. In 10 studies corrections for multiple comparisons were made with Bonferroni, Newman-Keul’s multiple range test, Scheffés post-hoc test, Tukey’s test or by applying a 1% significance level [26,28,29,31,32,34,35,48,62,63]. Analyses of variance (one-way/two-way/three-factor/repeated measures ANOVAs; multivariate ANOVA [MANOVA; WILKS test]; linear mixed models; Friedman test) [27–29,32–36,38–40,42,44–53,55–58,60,62,63] were performed in 29 out of 38 studies. Association was estimated by Pearson’s correlation coefficient (r) in 7 studies [28,42,44,45,50–52] and by logistic regression analyses in 1 study [41]. Multiple regression analyses with general linear models (GLM) were made in 2 studies [38,54]. Estimation of significance of indirect effects was made by the Sobel test and by bootstrap estimates [84] in 1 study [42]. Calculations compensating for extreme outliers by Winsorized blockade effect measures were made in 1 study [41].
3.6 Demographics
3.6.1 ʻInhibitoryʼ Test Paradigms
Demographics are presented in Table 3. The total number of subjects in the ITP-studies was 429, with a median (IQR) number of subjects in each study of 14.0 (8.0 to 24.0). Two studies did not report the gender of the subjects [8,25], but calculated from the remaining 23 studies, the gender ratio (males/females) was 1.9 (249/134). Interestingly, none of the studies rendered information concerning body weight, a detail of some importance, since 11 of the studies used weight-based infusion regimens [5,10,12,16,17,19–21,23–25].
Table 3. ʻInhibitoryʼ Test Paradigms: Demographics and Drugs.
| [Ref.] First Author | N | Male/Female | Age (yr) | Drug | Dose | Administration | Additional drugs § |
|---|---|---|---|---|---|---|---|
| ʻINHIBITORYʼ TEST PARADIGMS | |||||||
| Conditioned Modulation Models | |||||||
| [1] Willer JC | 6 | 4/2 | Range: 23–24 | Nx | B: 4 mg | i.v. | - |
| [2] Willer JC | 6 | 4/2 | Range: 22–35 | Nx | B: 5 mg | i.v. | - |
| [3] Pertovaara A | 6 | 6/0 | Range: 23–37 | Nx | B: 0.8 mg | i.v. | - |
| [4] Pertovaara A | 10 # | 10/0 | Range: 20–38 A | Nx | B: 2 mg | i.v. | - |
| [5] Willer JC | 15 | 10/5 | Range: 21–33 | Nx | B: 0.02 mg/kg | i.v. | - |
| [6] Pertovaara A | 7 | 6/1 | Range: 21–27 | Nx | B: 0.8 mg | i.v. | - |
| [7] Buchsbaum MS | 19 | 10/9 | NR | Nx | B: 8 mg | i.v. | |
| [8] Jungkunz G | 32 | NR | NR | Nx | B: 0.8 mg | i.v. | - |
| [9] Janal M | 12 | 12/0 | Mean: 39 ± 12 SD | Nx | B: 0.8 mg | i.v. | - |
| [10] Willer JC | 8 | 4/4 | Range: 26–38 | Nx | B: 0.06–0.07 mg/kg | i.v. | Diazepam |
| [11] Ernst M | 6 | 2/4 | NR | Nx | B: 1.2 mg | i.m. | - |
| [12] Willer JC | 8 | 4/4 | Range: 25–36 | Nx | B: 0.08 mg/kg | i.v. | Diazepam |
| [13] Olausson B | 11 | 8/3 | Range: 21–40 | Nx | B: 0.8 mg | i.v. | - |
| [14] Willer JC | 9 | 4/5 | Range: 23–36 | Nx | B: 0.4 mg | i.v. | - |
| [15] Poulsen L | 41 | 26/15 | NR | Nx | B: 0.8 mg | i.v. | - |
| [16] Edwards RR | 6 | 3/3 | Mean: 22 ± 4 SD | Nx | B: 6 mg/kg | i.m. | - |
| [17] Julien N | 20 | 10/10 | Female: 31 ± 8; Male: 28 ± 8 | Nx | B: 0.28 mg/kg | i.v. | - |
| [18] Robertson LJ | 32 | 17/15 | Median: 19; Range: 17–39 | Nx | B: 80 microg/0.2 ml (burn site) | s.c. | - |
| [19] Rennefeld C | 24 | 24/0 | 26 ± 5 | Nx | B: 0.15 mg/kg + I: 0.2 mg/kg/h | i.v. | - |
| [20] Leonard G | 21+3 ¤ | 12+1/9+2 | 25 ± 6 | Nx | B: 0.14 mg/kg x 2; B: 0.02 mg/kg x 2 | i.v. | - |
| [21] Sprenger C | 20 | 20/0 | Mean: 26 ± 1 SD | Nx | B: 0.15 mg/kg + I: 0.2 mg/kg/h | i.v. | - |
| [22] King CD | 33 | 16/16 | Mean: 24 ± 4 SD | NTx | 50 mg | p.o. | - |
| Repetitive Transcranial Magnetic Stimulation Models | |||||||
| [23] de Andrade DC | 36 | 24/12 | Mean: 29 ± 6 SD | Nx | B: 0.1 mg/kg + I: 0.1 mg/kg/h | i.v. | - |
| [24] Taylor JJ | 24 | 12/12 | Mean: 25 ± 3 SD | Nx | B: 0.1 mg/kg | i.v. | Capsaicin topical |
| [25] Taylor JJ | 14 | NR | Range: 18–45 | Nx | B: 0.1 mg/kg | i.v. | Capsaicin topical |
§ not interfering with the MOR-antagonist assessments (drugs without administration route stated are i.v.).
¤ 3 additional volunteers were included due to unintended ʻcarry-overʼ (sequence) effects.
# 12 volunteers total (2 volunteers did not participate in the naloxone parts of the study).
SD standard deviation.
A = age presented separately for each of the 6 groups of volunteers
B = bolus (up to 4 min administration time allowed); F = female; I = infusion; M = male; ITP = iontophoresis; N.R. = not reported; NTx = naltrexone; Nx = naloxone; SD = standard deviation; TCI = target-controlled infusion (total dose indicated).
3.6.2 ʻSensitizingʼ Test Paradigms
Demographics are presented in Table 4. The total number of subjects in the STP-studies was 1,048, with a median (IQR) number in each study of 14.5 (11.3 to 23.8) subjects. The second largest (n = 158) [60] and the third largest (n = 151) [61] study reported partially duplicate data [61]. One study [41] was a companion study to a previously published study [85]. Two studies did not report the gender of the subjects [43,48], but based on calculations from the remaining 36 studies, the gender ratio (males/females) was 1.4 (601/430). Only 8 studies rendered information concerning body weight [31,32,34,36,49,51,53] or BMI [56], a detail of some importance, since 9 of the studies used weight-based infusion regimens [28–32,36,49,55,57]. Eight of the studies included patients with fibromyalgia [33,40], chronic low back pain [41,42], borderline arterial hypertension [49], bulimia nervosa [51] or major depression [52], but these data are not presented in the present review.
Table 4. ʻSensitizingʼ Test Paradigms: Demographics and Drugs.
| [Ref.] First Author | N | Male/Female | Age (yr) | Drug | Dose | Administration | Additional drugs § |
|---|---|---|---|---|---|---|---|
| ʻSENSITIZINGʼ TEST PARADIGMS | |||||||
| Secondary Hyperalgesia Models | |||||||
| [26] Mikkelsen S | 23 | 23/0 | NR | Nx | B: 0.8 mg/15 min + 0.4 mg/h | i.v. | Ketamine |
| [27] Brennum J | 24 | 24/0 | 24; Range: 20–31 | Nx | B: 0.4 mg; B: 10 mg | i.v. | - |
| [28] Koppert W | 13 | 13/0 | 31 ± 5 | Nx | B: 10 microg/kg | i.v. | Remifentanil |
| [29] Koppert W | 15 | 12/3 | 29 ± 6 | Nx | B: 0.05, 0.5, and 5.0 microg/kg; TCI: 0.16, 1.6 and 16 microg/kg | i.v. | - |
| [30] Chu FL | 9 | 9/0 | 30 ± 9 | Nx | B: 0.1 mg/kg | i.v. | Remifentanil |
| [31] Pereira MP | 22 | 11/1 | F: 23 ± 1; M: 25 ± 2 | Nx | B: 21 microg/kg | i.v. | - |
| Summation Models | |||||||
| [32] Benedetti F | 173 | 90/83 | A | Nx | B: 0.14 mg/kg | i.v. | Capsaicin injection |
| [33] Price DD | 14 A | 0/14 | Mean: 46 | Nx | B: 0.8 mg | i.v. | Fentanyl |
| ʻPainʼ Models | |||||||
| Capsaicin: | |||||||
| [34] Graven-Nielsen | 15 | 15/0 | Mean: 24; Range: 21–31 | Nx | I: 0.8 mg /15 min + 0.5 mg /75 min | i.v. | Capsaicin injection |
| Capsaicin & heat: | |||||||
| [35] Drummond PD | 14 | 7/7 | Mean: 22 ± 6 SD | Nx | ITP: 0.5 mM | ITP | Capsaicin topical |
| [36] Anderson WS | 9 | 5/4 | Mean: 29 ± 5 SD | Nx | B: 0.1 mg/kg | i.v. | Capsaicin topical |
| Comb. modalities, others: | |||||||
| [37] Grevert P | 30 | 15/15 | NR | Nx | B: 1 mg/2 mg # ; B: 10 mg | i.v. | - |
| [38] McCubbin JA | 16 | 16/0 | Range: 18–24 | Nx | I: 8 mg | i.v. | - |
| [39] Stacher G | 24 | 12/12 | Range: 19–33 | Nx | I: 5 mg; I: 20 mg | i.v. | - |
| [40] Younger JW | 10 B | 0/10 | Mean: 55 ± 8 SD | NTx | 50 mg | p.o. | - |
| [41] Bruehl S | 39 C | 11/28 | Mean: 31 ± 8 SD | Nx | I: 8 mg | i.v. | - |
| [42] Bruehl S | 31 D | 13/18 | Mean: 34 ± 10 SD | Nx | I: 8 mg | i.v. | Morphine |
| Electrical: | |||||||
| [43] El-Sobky A | 5 | NR | NR | Nx | I: 0.4 mg; I: 0.8 mg | i.v. | - |
| [44] Buchsbaum MS | 21 | 10/11 | Mean: 20 | Nx | I: 2 mg | i.v. | - |
| [45] Bromm B | 15 | 15/0 | Range: 21–29 | Nx | 32 mg E | p.o. | Tilidine |
| Ischemia | |||||||
| [46] Grevert P | 12 | 6/6 | Median: 28 | Nx | B: 10 mg; B: 2 mg | i.v. | - |
| [47] Grevert P | 12 | 12/0 | Mean: 25 ± 3 SD | Nx | B: 10mg + I: 6 mg/h (8 hr); B: 2 mg + I: 1.2 mg/h (8 hr) | i.v. | - |
| [48] Posner J | 12 | NR | Range: 20–46 | Nx | I: 2 mg F | i.v. | Codeine p.o. |
| Mechanical: | |||||||
| [49] Schobel HP | 9 G | 9/0 | Mean: 25 ± 6 SD | Nx | I: 0.15 mg/kg | i.v. | - |
| [50] Cook DB | 12 | 12/0 | Mean: 24 ± 4 SD | NTx | 50 mg H | p.o. | Codeine p.o. |
| Thermal: | |||||||
| [51] Lautenbacher S | 11 I | 0/11 | Mean: 23 ± 3 SD | Nx | I: 5 mg | i.v. | - |
| [52] Lautenbacher S | 10 J | 12/8 | Mean: 36 ± 11 | Nx | I: 5 mg | i.v. | - |
| [53] Al’Absi M | 26 | 15/11 | Mean: 21 ± 9 | NTx | 50 mg | p.o. | |
| [54] Borras MC | 10 | 10/0 | Mean: 32 ± 7 | Nx | B: 4 mg | i.v. | - |
| [55] Kern D | 12 | 6/6 | Range: 21–38 | Nx | B: 0.1 mg/kg; I: 0.1 mg/kg/h (0.05 mg/kg) K | i.v. | Ketamine |
| [56] Kotlyar M | 19 | 9/10 | Mean: 26 ± 7 | NTx | 50 mg | p.o. | - |
| [57] Schoell ED | 16 L | 8/8 | Mean: 29 ± 5 | Nx | B: 0.15 mg/kg; I: 0.2 mg/kg/h | i.v. | - |
| [58] Pickering G | 10 M | 10/0 | Mean: 26 ± 2 SD | Nx | I: 8 mg N | i.v. | Paracetamol i.v. |
| Nociceptive Reflex Models | |||||||
| [59] Boreau F | 10 | 6/4 | Range: 22–33 | Nx | B: 0.8 mg | i.v. | - |
| [60] France CR | 158 | 85/73 | Mean: 19 ± 2 SD | NTx | B: 50 mg | p.o. | - |
| [61] France CR | 151 | 83/68 | Mean: 19 ± 2 SD | NTx | B: 50 mg | p.o. | - |
| Miscellaneous Models | |||||||
| [62] Eissenberg T | 12 | 8/4 | Mean: 22 ± 3 SD | NTx | B: 50 mg | p.o. | Oxycodone |
| [63] Robertson LJ | 24 | 9/15 | Median: 26; Range: 17–39 | Nx | B: 80 microg/0.2 ml (burn site) | s.c. | Fentanyl |
| Total all studies | 1,477 | ||||||
§ not interfering with the MOR-antagonist assessments (drugs without administration route stated are i.v.).
# 1mg: cold water challenge; 2mg: ischemic pain challenge.
A study includes fibromyalgia patients (n = 15, data not reported here).
B study includes fibromyalgia patients (n = 10, data not reported here).
C study included patients with chronic low back pain (n = 37; data not reported here) and 2 healthy subjects on antidepressant medication.
D study includes chronic low back pain patients (n = 45, data not reported here).
E study includes treatment arms of combinations of tilidine (100 mg) and naloxone (8–32 mg; data not reported here).
F study includes treatment arms with codeine (60 mg p.o.) and codeine/naloxone (2 mg i.v.; data not reported here).
G study includes subjects with borderline hypertension (n = 21, data not reported here).
H study includes treatment arm with codeine (60 mg p.o.; data not reported here).
I study includes patients with bulimia nervosa (n = 10) and anorexia nervosa (n = 10; data not reported here).
J study includes patients with major depression (n = 20; data not reported here).
K study includes placebo-controlled treatment arm with ketamine (0.4 mg/kg; data not reported here).
L the total number of subjects were 20 (4 were excluded).
M the total number of subjects were 12 (2 were excluded).
N study includes treatment arms with paracetamol (1g i.v.) and paracetamol/naloxone (8 mg i.v.; data not reported here).
SD standard deviation.
For explanation of abbreviations, please, refer to legend Table 3.
3.7 MOR-antagonists
3.7.1 ʻInhibitoryʼ Test Paradigms
Naloxone was used in 24 [1–21,23–25] studies and naltrexone in 1 study [22] (Table 3). Naloxone was administered IV in 21 studies [1–10,12–15,17,19–21,23–25], IM in 2 studies [11,16] and SC in 1 study [18]. In the naloxone studies, estimated from a mean body-weight of the subjects of 70 kg [31] (Table 3), the IV-doses ranged between 6 to 350 microg/kg [14,19] and the IM-doses between 17 to 6,000 microg/kg [11,16]. The estimated weighted mean dose of parenterally administered naloxone was 195 microg/kg. One study used two-doses of naloxone [20]. Naltrexone was administered PO in a dose of 0.71 mg/kg [22]. In all studies normal saline was used as placebo tested against MOR-antagonists.
3.7.2 ʻSensitizingʼ Test Paradigms
Naloxone was used in 31 studies [26–39,41–49,51,52,54,55,57–59,63] and naltrexone in 7 studies [40,50,53,56,60–62] (Table 4). Naloxone was administered IV in 28 studies [26–34,36–39,41–44,46–49,51,52,54,55,57–59], SC in 1 study [63], PO in 1 study [45] and by iontophoresis in 1 study [35]. In the naloxone studies, estimated from a mean body-weight of the subjects of 70 kg [31] (Table 4), the IV-doses ranged between 6 to 827 microg/kg [27,43,47] and the PO-dose was 457 microg/kg [45]. In one dose-response study target-controlled infusion of naloxone was used [29] in doses ranging from 0.21 to 21 microg/kg. The SC-dose, 1 microg/kg, was minute and only intended for a local effect. The estimated weighted mean dose of IV administered naloxone was 125 microg/kg. Two separate doses of naloxone were used in 6 studies [27,37,39,43,46,47]. One study used a 3-dosing target-controlled infusion regimen [29]. Naltrexone was exclusively administered PO in doses of 0.71 mg/kg [40,50,53,56,60–62]. In all studies normal saline was used as placebo tested across the MOR-antagonists.
3.8 Adjuvant Drugs
3.8.1 ʻInhibitoryʼ Test Paradigms
Adjuvant drugs were used in 4 studies either due to anxiolytic action (diazepam) [10,12] or to promote induction of pain (capsaicin [Table 3]) [24,25].
3.8.2 ʻSensitizingʼ Test Paradigms
Adjuvant drugs were used in 11 studies due to the anti-hyperalgesic actions (codeine, fentanyl, ketamine, morphine, paracetamol, oxycodone, remifentanil, tilidine) [26,28,33,42,45,48,50,55,58,62,63] in 4 studies due to the pain-induction ability (capsaicin) [32,34–36] and in 2 studies due to development of opioid-induced hyperalgesia (remifentanil [Table 4]) [28,30].
3.9 Primary Test Stimuli
3.9.1 Electrical Stimuli
ʻInhibitoryʼ Test Paradigms. Fourteen studies [1–8,10–15] used electrical stimuli as primary test stimuli (Table 5): 9 studies [1,2,5,7,8,10,12,14,15] used transcutaneous stimulation, while 4 studies [3,4,11,13] used non-invasive dental (pulpal) stimulation. Sural nerve-stimulation was used in 6 studies [1,2,10,12,14,15], tibial nerve-stimulation in 2 studies [1,12], alveolar nerve-stimulation in 4 studies [3,4,11,13] and supraorbital nerve-stimulation in 1 study [5]. In 6 studies [1,2,10,12,14,15] the nociceptive flexion reflex (NFR; also termed nociceptive polysynaptic reflex [NPR]) was elicited by sural nerve-stimulation and EMG-recordings of the RIII component from the biceps femoris muscle or the rectus femoris [15]. In 2 of these studies [1,12] the monosynaptic spinal reflex (MSR) was elicited by tibial nerve-stimulation and the EMG-recording of the H-component from the soleus muscle. A detailed description of the characteristics of the electrical stimuli is presented in Table 5.
Table 5. ʻInhibitoryʼ Test Paradigms: Testing Methods and Results.
| [Ref.] First Author | Primary Test Stimuli | Conditioning Stimuli | Outcome Variables △ | Main Findings |
|---|---|---|---|---|
| ʻINHIBITORYʼ TEST PARADIGMS | ||||
| Conditioned Modulation Models | ||||
| [1] Willer JC | MSR (Tibial-TNS + EMG H-S); NPR (Sural-TNSA + EMG RIII-BF) | NS: Sural noxious TNS; CAS: Warning announcement + randomized tactile /noxious stimuli | Reflex amplitudes (MSR [H]), reflex thresholds (NPR [RIII]), HR and RR | Nx facilitated the MSR (H-reflex), decreased the NPR (RIII) threshold and increased magnitude of autonomic variables, in response to noxious sural nerve conditioning stimulation |
| [2] Willer JC | NPR (Sural-TNSA + EMG RIII-BF) | NS: Sural noxious/tactile TNS; CAS: Warning announcement + randomized tactile /noxious stimuli | Reflex thresholds (NPR [RIII]), HR and RR | Nx reversed the increase in NPR (RIII) threshold responses to repetitive stress stimuli |
| [3] Pertovaara A | DEPTA | HF-TENSA | DEPT | Nx did not affect increases in DEPT induced by HF-TENS |
| [4] Pertovaara A | DEPTA; Thermal thresholds (TTA) | Arm ischemia (SETT) | VAS, heat thresholds, cold thresholds, electrical pain thresholds | Nx did not reverse ischemia induced elevation in dental electrical pain threshold but likely reduced the increase in heat thresholds (very low-powered study!) |
| [5] Willer JC | Blink reflex (BR-TNS) | HF-TNS | Nociceptive EMG- component of BR (R2) | Nx had no effect on the depression on the nociceptive blink reflex induced by high frequency non-noxious conditioning stimulation |
| [6] Pertovaara A | DEPTA | LF-TENS | EPT | Nx had no effect on the elevation of dental pain threshold due to non-noxious TENS. |
| [7] Buchsbaum MS | RESA | RES | CPS, EP | Nx increased pain sensitivity (enhanced amplitudes of EPs) after prolonged RES and attenuated RES-induced SIA |
| [8] Jungkunz G | FEPT | NS: FES; UCAS: Arithmetic stress (n = 15) or CWITA (0°C; n = 14) | EPT | Nx reversed the increases in electrical pain thresholds induced by CWIT. |
| [9] Janal M | HGSD50%, 20; CPTT180s; Radiant heat stimulation (RHSD) | Exercise (running 85% of MAC); Arm ischemia (SETT) | CPS, TTTo, WDL, HPR, psychometrics, endocrine response | Nx attenuated exercise induced ischemic but not thermal hypoalgesic effects. CPTT-data failed to demonstrate post-exercise hypoalgesia |
| [10] Willer JC | NFR (Sural-TNSA + EMG RIII-BF) | NS: Sural noxious/tactile TNS; CAS: Warning announcement + randomized tactile /noxious stimuli | VAS, reflex-thresholds (NFR [RIII]) | Nx reversed the analgesic response and the increase in nociceptive reflex thresholds to repetitive stress stimuli, an effect mitigated by diazepam |
| [11] Ernst M | DEPTB | RDEPTB | EPT; Electrical discomfort thresholds | Nx had no effect on increase in dental electrical pain or discomfort thresholds induced by repetitive stimulation. |
| [12] Willer JC | NFR (Sural-TNSA + EMG RIII-BF); MSR (Tibial-TNS + EMG H-S) | NS: Sural noxious/tactile TNS; CAS: Warning signal + randomized tactile/noxious stimuli | VAS, reflex-thresholds (NFR [RIII]), HR, RR | Nx reversed the analgesic response, the increase in reflex thresholds and the increase in magnitude of autonomic responses to repetitive stress stimuli |
| [13] Olausson B | DEPTC | LF-TNS | EPT | Nx paradoxically prolonged the LF-TNS induced increase in EPT. |
| [14] Willer JC | NFR (Sural-TNSA + EMG RIII-BF) | HWIT (46°C) | Reflex-thresholds (NFR [RIII]) | Nx completely blocked the inhibitory effect of DNIC on the nociceptive flexion reflex |
| [15] Poulsen L | NFR (Sural-TNSA + EMG RIII-RF) | CWIT (0.9°C) | NFR [RIII-RMS]), E-VAS | Nx near-significantly blocked the inhibitory effect of DNIC on the nociceptive flexion reflex and increased CPTT-induced pain, in extensive metabolizers of sparteine. |
| [16] Edwards RR | Thermal stimulations (TSHSA, HPT) | CWITA (1–3°C, repeated 4 times, duration not stated) ¤ | NRS, HPT, ABP, | Nx had no effect on DNIC-induced changes on heat pain perception, but seemed to increase cardiovascular reactivity to noxious cold |
| [17] Julien N | CWIT (12°C) | CWITC (12°C) | VAS | Nx inhibited the endogenous pain inhibitory systems activated by the spatial summation model |
| [18] Robertson LJ | HPT (RHSHG) | BIA + CWITA (2°C, repeated 6–10 times with 20 s interval) | HPT; VRS immersion | Locally administered Nx augmented sensitivity to cold water immersion tests (pain threshold, tolerance, rating). Locally administered Nx had modifying effects on heat sensitivity in non-burn skin after repeated cold water immersions |
| [19] Rennefeld C | HPT, HPR (TSHSB-stimuli); PDT (monofilaments 0.08–2,492 mN) | Repeated TSHSB (8 days) | HPT, HPR, PDT, VAS; (Day 1 + 8) | Nx had no effect on the magnitude of habituation for any of the stimulation sites (armstim, armnon-stim and leg). |
| [20] Leonard G | HSA | HF-TENSB | HPT, HPTo, HPR (COVAS) | High-dose Nx (0.28 mg/kg) blocked the analgesic effect of high-frequency TENS |
| [21] Sprenger C | HSB | CWITA (0°C; control 25°C) | EVAS, HPR, CPR, BOLD-responses | Nx compared to placebo:* increased pain ratings during CWIT; * did not alter pain ratings during phasic heat stimulation; * impaired the correlation between cold pain and endogenous analgesia; * reversed the coupling between ACC and DPCS |
| [22] King CD | HSC | CWITB (mean temperature 12.9°C) | EVAS, HPR, CPR; Psychometrics (CASE, PCS, SSE) | NTx abolished CPM induced decreases in HPR in subjects with low PCS-scores, but not in subjects with high PCS-scores |
| Repetitive Transcranial Magnetic Stimulation Models | ||||
| [23] de Andrade DC | CC | rTMS | CPT, CPRR | Nx attenuated the analgesic effect of M1-targeted repetitive transcranial magnetic stimulation (rTMS), but did not affect stimulation of DLPFC/PMC or sham controls. |
| [24] Taylor JJ | TTA, HSD | rTMS + Capsaicin (0.1%, topical, skin) | NRS, HPR; WDT, CDT, HPT, CPT, HPTo, CPTo; ± DLPFC-rTMS | Nx attenuated the analgesic effect of DLPFC-targeted repetitive transcranial magnetic stimulation |
| [25] Taylor JJ | TTA, HSD | rTMS + Capsaicin (0.1%, topical, skin) | NRS, HPR; HPTo; ± DLPFC-rTMS | Nx attenuated rTMS-induced analgesia, as well as rTMS-induced attenuation of BOLD signal response to heat-capsaicin stimuli throughout pain processing regions, including midbrain and medulla. |
△ Outcome variable related to specific objectives of the review.
¤ Sequence I-II: temporal heat summation (forearm); sequence III-IV: HPT (forearm); sequences separated by 2 min.
ABP = arterial blood pressure; ACC = subgenual anterior cortex cinguli; BIA = burn injury A (probe area 0.8 cm2, 48°C, 2 min, application force 1N, arms/hands); BDI = Beck Depression Inventory; BIB = burn injury B (12.5 cm2, 47°C, 7 min); BOLD = blood-oxygen-level dependent contrast imaging; BTS = brief thermal sensitization (45°C, 3 min); BR-TNS = nociceptive component of blink reflex (supraorbital transcutaneous nerve stimulation, 0.1 ms duration, 0.15 Hz, 9–12 mA) assessed by integrated and rectified m. orbicularis oculi EMG [25–45 ms gated = R2 response]); BS = brush stimulation (1 cm stroke, 1 Hz, duration 25s, ISI 30s); CAS = conditioned aversive stimuli; CASE = cognitive affective side effects; CC = contact cold (30 x 30 mm2/ 25 x 50 mm2; -0.5°C/s or NR); CDT = cool detection threshold; CEVAS = continuous (0.2 Hz) EVAS; CHA = contact heat (30 x 30 mm2, 0.5°C/s); CHB = contact heat (2 cm2, 0.5°C/s); CHC = contact heat (3 x 3 cm2, 1°C/s); CHEP = contact heat evoked potentials (SSEP); COVAS = computerized visual analog scale; CPR = cold pain rating; CPRR = cold pain ratings at 5, 10 and 15°C, applied in a random order for 2 seconds; CPS = categorical pain scale; CPT = cold pain threshold; CPTo = cold pain threshold; CPTT = cold pressor test (ice-water); CWIT = cold-water immersion test (max. duration 2 min, hand); CWITA = cold-water immersion test A (approx. 7 min duration, hand/foot/leg); CWITB = cold-water immersion test B (40s, repeated 5 times, intersession resting period 3 min, fixed temperature level [8–16°C] corresponding to a CPR [“mild-to-moderate pain”: EVAS mean 42 (0–100)], foot); CWITC = cold-water immersion test C (8 consecutive immersions, 2 min duration, inter-stimulus interval 5 min, fingertip to shoulder and vice versa); CWITD = cold-water immersion test D (immersion 5 min duration, 10°C, hand, n = 18)); DEPTA = dental electrical pain threshold A (10 ms stimuli, 5 Hz); DEPTB = dental electrical pain threshold B (100 pulses, single pulse duration 0.1 ms, 0.6 s train, 0–0.5 mA); DEPTC = dental electrical pain threshold C (duration 22 ms, 6.2 Hz, 0–0.1 mA); DLPFC = left dorsolateral prefrontal cortex; DPCS = descending pain control system; EDT = electrical detection threshold; EMG RII-BF = electromyographic reflex responses [RII, latency 50–70 ms] from biceps femoris muscle [BF]; EMG RIII-BF = electromyographic reflex responses [RIII, latency 90–150 ms] from biceps femoris muscle [BF]; EMG H-reflex = electromyographic reflex responses [H] from soleus muscle [S]; EP = [somatosensory] evoked potentials; EPT = electrical pain threshold; EPTo = electrical pain tolerance; EVAS = electronic VAS; FEPT = finger electrical pain threshold (100 Hz, pulse-trains of 100 ms, duration 1s, 0–1.9 mA); FES = finger electrical stimulation (see FEPT); fMRI = functional magnetic resonance imaging; FPP = finger pressure pain (2,000 g applied at dorsal surface of middle phalanx of index finger for 1 min); HF-TENSA = high-frequency transcutaneous nerve stimulation A (bi-phasic stimulus, duration 0.6 ms, 100 Hz, 45 mA, cheeks); HF-TENSB = high-frequency transcutaneous nerve stimulation B (duration 0.06 ms, 100 Hz, segmental, sural nerve); HF-TNS = high-frequency transcutaneous nerve stimulation (duration 0.2 ms, 100 Hz, 2 mA, segmental/heterosegmental cutaneous nerves); HGD80% max = handgrip dynamometer 80% maximum grip strength for 90s; HGSD = handgrip strength measured by dynamometry (isometric, repeated contractions; set to 50% maximum grip strength 20 contractions/ set to 50% maximum grip strength/30% of maximal voluntary contraction/12-kg load 20 times); HPR = heat pain ratings; HPT = heat pain threshold; HPTo = heat pain tolerance; HR = heart rate; HSA = tonic heat stimulus with contact thermode (1 cm2, fixed temperature level corresponding to HPR 50 [COVAS 0–100], duration 120 s); HSB = phasic heat stimulus with contact thermode (9 cm2, 47.5°C, duration 5 s, repeated 64 times, inter-stimulus interval 45 s); HSC = tonic heat stimulus with contact thermode (5.3 cm2, fixed temperature level [46–50°C] corresponding to a HPR [“mild-to-moderate pain”], duration 30 s repeated 5 times, intersession resting period 3 min); HSD = tonic heat stimulus with contact thermode (9 cm2, fixed temperature level corresponding to HPR 7 [NRS 0–10], duration 22 s); HSE = phasic and tonic heat stimuli with contact thermode (6 cm2; 0.7°C/s or 35 s at HPT); HSF = tonic heat stimuli with contact thermode (3 x 3 cm2, 4 stimuli, 46°C, 25s, ISI 30s); HSG = phasic heat stimuli with contact thermode (3 x 3 cm2, 4 randomized stimuli, 43–48°C, duration 5 s, ISI 62 s, 10°C/s, repeated 10 times); HSH = stimulation with short phasic contact stimuli (stimulus area 0.6 cm2, peak temperature 51.8°C, 6 stimuli, ISI 15 s); HSI = phasic heat stimulus with RHSHG-technique (45°C, 5 s); HWIT = hot water immersion test (2 min, hand); IDES = intradermal electrical stimulation (rectangular, 0.5 ms duration, 2 Hz, high density); ISI = interstimulus interval; IPT = ischemia pain threshold; IPTo = ischemia pain tolerance; ITC-SS = infra-threshold cold stimulation—single stimuli (2.5 cm2, 0.2°C, 0.7 s stimuli, forearm); ITC-TS = infra-threshold cold stimulation—temporal summation (2.5 cm,2 0.2°C, 0.7 s stimuli, train of 15 stimuli, 3 s inter-stimulus interval, hand); LDPFC = left dorsolateral prefrontal cortex; LF-TENS = transcutaneous electrical nerve stimulation (2.5 Hz, 0.2 ms duration, train of 5 impulses, 100 ms interval; stimulation areas 18.0 cm2); LF-TNS = low-frequency transcutaneous electrical nerve stimulation (duration 0.1 ms, 2 Hz, 9–45 V, 30 min stimulation hand/face [infraorbital nerve]); MAC = maximal aerobic capacity; MPQ = McGill Pain Questionnaire; MSNA = microneurographic recordings of sympathetic nerve activity to muscle; MSR = monosynaptic spinal reflex; NFR = nociceptive flexion reflex (same as NPR [RIII]); N.R. = not reported; NRS = pain ratings by numerical pain scale (0–10/100); NS = noxious stimuli; NPR = nociceptive polysynaptic reflex (same as NFR [RIII]); PAA = pressure algometry (1 cm2, 30 kPa/s); PAB = see PAA (1 cm2, 98 kPa/s); PANAS = Positive and Negative Affect Schedule; PCS = pain catastrophizing scale; PDT = pin-prick detection threshold; PMES = pain magnitude estimation scale; PPR = pin-prick pain rating; PPT = pin-prick pain threshold; PRPT = pressure pain thresholds; PSR = tactile polysynaptic reflexes (RII); RDEPTB = repetitive (1Hz, 3 min stimulation, inter-stimulus interval 7 min, 11 stimulation periods), DEPTB (see above); RESA = repetitive electrical skin stimulation (1–31 mA; other data NR); RESB = see RESA (1–31 mA, 1 mA increment, 93 stimuli, ISI 2.5 s); RESC = see RESA (200 Hz, duration 20 ms, ISI 20–40 s, repeated 40 times); rTMS = repetitive transcranial magnetic stimulation; RHS = radiant heat stimulation; RHSD = radiant heat stimulation by dolorimeter (0, 50, 340 and 390 mcal/s/cm2); RHSHG = radiant heat stimulation by halogen globe (95 mm2 [14] and [52]/ 28 mm2 [28] apertures, 0.5°C/s, maximum 45/48/49°C); RMS = root mean square; RPS = ratio proportional pain scale; RR = respiratory rate; SBP = systolic blood pressure; SHA = secondary hyperalgesia areas; SETT = modified submaximal effort tourniquet test; SIA = stress-induced analgesia; SOWS = subjective opioid withdrawal scale; SP = skin pinching (two opposed pegs, diameter 6 mm, force 18–25 N, stimulus duration 2 min, ISI 8 min, 5 anatomical sites); SSE = somatic side effects; SSEP = EP; STCR = supra-threshold cold stimulation pain ratings; STAI = State-trait Anxiety Inventory; STHR = supra-threshold heat stimulation pain ratings; STH-SS = supra-threshold heat stimulation—single stimulation (2.5 cm2, 52°C, duration 0.7 s/3.0 s, hand); STH-TS = supra-threshold heat stimulation—temporal summation (se STH-SS characteristics; train-of-ten); STPPR = suprathreshold pressure pain ratings (28 mm2, 700 kPa, 60 s); Sural noxious/tactile TNS = transdermal electrical sural nerve stimulation (randomized: 3 noxious stimuli [70–80 mA] or 2 tactile stimuli [4–8 mA]); Sural-TNSA = transdermal electrical sural nerve stimulation A (1 ms duration, train of 8–10, 20 ms train-duration [1]/1 ms duration, train-of-10, internal frequency 300 Hz, train-frequency 0.2 Hz, 10 mA [2]/ 1 ms duration, train-of-6, internal frequency 200 Hz, train-frequency 0.2 Hz, 10 mA [8]/ 1 ms duration, train-of-8, train-frequency 0.25 Hz, 0–30 mA [10]/ 1 ms duration, train-of-5, train-duration 20 ms, train-frequency 0.17 Hz [11]/ 1 ms duration, long lasting train (50–60 ms), internal frequency 300 Hz, 10 mA [48]; Sural-TNSB = transdermal electrical sural nerve stimulation B (300 Hz, 1 ms duration, long-lasting train, 5 mA); Sural-TNSC = transdermal electrical sural nerve stimulation C (volley of 5 stimuli, 1 ms duration, interstimulus interval 3 ms, 4–40 mA, 3 stimulation sessions spaced by 5 min); TAM = tibialis anterior muscle; TCS = thermal contact stimulators (3.1 cm2/0.8 cm2, 43/46/49°C, 2 x 6 stimuli, stimulus-duration max. 5 s, forearm); TDES = transdermal electrical stimulation (low density); TESA = transcutaneous electrical stimulation (duration 1 ms, 100 Hz, 0–6.4 mA, increments 0.05 mA, train-of-eight, randomized interval 15–25 s); TESB = see TESA (0.2 mA increments, ISI 1.2 s); TG = “thermal grill” is a device applied to the skin composed of six bars with alternating warm and cold temperatures (even- and odd-numbered) controlled by Peltier elements; Tibial-TNS = transdermal posterior tibial nerve stimulation (1 msec duration, 0.2 Hz); TSHSA = Temporal summation of heat stimuli A (49°C, stimulation area 9 cm2, stimulus duration 0.5 s, inter-stimulus interval 2.5 s, train of 10 stimuli, left forearm); TSHSB = Temporal summation of heat stimuli B (48°C, stimulation area 9 cm2, stimulus duration 6 s, inter-stimulus interval 4 s, train of 6 stimuli, 10 blocks separated by 40–60 s, left forearm); TTA = thermal thresholds (stimulation areas 1.8/9 cm2, lip/forearm); TTB = see TTA (6 cm2; 0.7°C/s, baseline either 32°C or 38°C); TTTo = tourniquet test tolerance; VT = vibratory threshold; UCAS = unconditioned aversive stimulus; UV-burn = ultraviolet “solar” stimulator (150W xenon lamp, UVA [400 nm] and UVB [290 nm], aperture 2 cm) skin exposure: 2.5 MED (“minimal erythemic dose”, arm); VAS = pain intensity and/or unpleasantness ratings by visual analog scale (0–100); VNS = visual numeric pain scale (0–100); VRS = verbal pain rating scale; VS = vibratory stimulation (0.8 cm2, 100 Hz, 0.5 s, displacement 1 mm); VT = vibratory threshold (stimulation area N.R., 3.7 N/cm2, 0.2 microm/s); WCT = warming by contact thermode (2 cm2, 37°C, > 80 min); WDL = withdrawal latency; WDT = warmth detection threshold.
ʻSensitizingʼ Test Paradigms. Eight studies [32,39,43–45,59–61] used electrical stimuli as primary test stimuli (Table 6) and all used transcutaneous stimulation. Sural nerve-stimulation was used in 3 studies [59–61], and additional tibial nerve-stimulation in 1 study [59]. In the former studies the nociceptive flexion reflex was elicited by sural nerve-stimulation and EMG-recordings of the RIII component from the biceps femoris muscle [59–61]. In one of the studies [59] the monosynaptic spinal reflex was elicited by tibial nerve-stimulation and the EMG-recording of the H-component from the soleus muscle. In this study [59] tactile polysynaptic reflexes (PSR) were additionally elicited from sural nerve-stimulation and EMG-recordings of the RII-component from the biceps femoris muscle. A detailed description of the characteristics of the electrical stimuli is presented in Table 6.
Table 6. ʻSensitizingʼ Test Paradigms: Testing Methods and Results.
| [Ref.] First Author | Primary Test Stimuli | Conditioning Stimuli | Outcome Variables △ | Main Findings |
|---|---|---|---|---|
| ʻSENSITIZINGʼ TEST PARADIGMS | ||||
| Secondary Hyperalgesia Models | ||||
| [26] Mikkelsen S | Nylon monofilament (1,150mN) Brush | BIB | SHA, HPT | Nx no effect on SHA or HPT |
| [27] Brennum J | Nylon monofilament (1,150mN) Gauze swab | BIB | SHA, HPT, STHR, VS, STPPR, VAS | Nx no effect of on SHA or on other outcomes |
| [28] Koppert W | Nylon monofilament (450mN), Cotton-wool tip | IDES; TDES | SHA, NRS; Allodynic areas | Nx associated with trend in increase in SHA. Nx increased NRS during IDES. Nx no effect on allodynic areas |
| [29] Koppert W | Nylon monofilament (450mN), Cotton-wool tip | IDES | SHA; Allodynia areas; NRS | Nx (2 highest doses) increased SHA and NRS during IDES. Nx tended to revert the decrease of allodynic areas |
| [30] Chu FL | Non-flexible steel wire (160 mN) | IDES | SHA, VAS | Nx no effect on the SHA |
| [31] Pereira MP | Nylon monofilament (890mN) | BIB; BTS | SHA, HPT, WDT, PPT | Nx did not reinstate SHA after resolution of a burn injury. Nx no effect on SHA during BTS |
| Summation Models | ||||
| [32] Benedetti F | Capsaicin (10 microg, s.c.); TDES | Capsaicin (10 microg, s.c.) | Placebo response; NRS | Nx completely abolished the spatial-specific placebo response |
| [33] Price DD | STH-SS; ITC-TS | STH-TS; ITC-TS | VAS, EPT | Nx did not have an effect on the study variables compared to placebo. |
| ʻPainʼ Models | ||||
| Capsaicin | ||||
| [34] Graven-Nielsen | PAA, PPT (nylon monofilament, 1,237 mN) | Capsaicin (50 microg, i.m. in TAM) | EVAS, PRPT, PPT; (sensitivity at 6 sites on both legs) | Nx had no effect on pressure or pinprick pain thresholds during capsaicin-induced muscle pain. |
| Capsaicin & heat | ||||
| [35] Drummond PD | Radiant heat stimulation (RHSHG) | Capsaicin (0.6%, 400 microL skin) | HPT | Iontophoretically applied Nx and saline increased radiant heat sensitivity induced by capsaicin. After “body cooling” the Nx site was less sensitive to heat than the saline site |
| [36] Anderson WS | WCT | Capsaicin (10%, 35 mg, skin) | PMES | Nx significantly increased normalized pain ratings compared to placebo and baseline |
| Comb. modalities, others | ||||
| [37] Grevert P | HGSD12 x 20, CWITD | Arm ischemia (SETT) | NRS, psychometrics | Nx had no effect on pain induced by arm ischemia and cold-water immersion |
| [38] McCubbin JA | CPTT90s; HGD80% max. | - | Pain rating (method N.R.); SBP | Nx did not affect pain ratings for cold pressor or handgrip challenge. Nx did not affect relationship between SBP and pain ratings |
| [39] Stacher G | TESA; RHS (method N.R.) | - | EPT, EPTo, HPT | Nx did not affect EPT or EPTo. Nx was associated with a slight but statistically significant increase in HPT |
| [40] Younger JW | CHA, CC, PAB | - | HPT, HPTo, CPT, CPTo, PRPT, SOWS | NTx did not affect thermal pain sensitivity or SOWS. NTx was associated with a slight but statistically significant increase in PRPT |
| [41] Bruehl S | FPP, HGSD50%, 5 min | - | IPT, IPTo, VAS, NRS, psychometrics (BDI, STAI, PANAS, MPQ) | Nx and placebo used as tools in estimating individual measures of endogenous opioid (EO) function |
| [42] Bruehl S | CHB, HGSD50%, 8 min | Arm ischemia (SETT) | IPT, IPTo, HPT, HPTo, VAS, NRS | Nx, morphine and placebo used as tools in estimating individual measures of endogenous opioid (EO) function |
| Electrical | ||||
| [43] El-Sobky A | TESB | - | EDT, EPT, EPTo | Nx did not affect electrical thresholds |
| [44] Buchsbaum MS | RESB | - | EP, CPS | Nx increased pain perception in pain insensitive individuals indicating a modulatory effect of endogenous opioid system. Nx did not affect the EP amplitude |
| [45] Bromm B | RESC | - | SSEP, CPS | Nx had no effect on pain perception but marginally increased SSEP amplitudes compared to placebo |
| Ischemia | ||||
| [46] Grevert P | HGSD12 x 20 | Arm ischemia (SETT) | NRS, psychometrics | Nx had no effect on ischemic arm pain |
| [47] Grevert P | HGSD12 x 20 | Arm ischemia (SETT) | VAS, psychometrics | Nx had no effect on ischemic arm pain |
| [48] Posner J | HGSD50% | Arm ischemia (SETT) | EVAS | Nx did not produce hyperalgesia or inhibited placebo analgesia |
| Mechanical | ||||
| [49] Schobel HP | SP | - | NRS, MSNA | Nx increased pain ratings and increased MSNA responses to pain |
| [50] Cook DB | HGSD30% | - | pain ratings (RPS), MSNA, | NTx has no effect on forearm musclepain, or MSNA during high-intensity handgrip tofatigue |
| Thermal | ||||
| [51] Lautenbacher S | HSE | - | HPT | Nx did not affect pain thresholds following phasic or tonic heat stimuli |
| [52] Lautenbacher S | TTB, VT | - | WDT, CDT, HPT, VT | Nx did not affect thermal or vibratory thresholds |
| [53] Al’Absi M | CHB, CPTT | - | HPT, HPTo, HPR (VNS), CPTT-rating (VNS) | NTx did not affect heat perception but was associated with reduced pain ratings during the CPTT |
| [54] Borras MC | BS, HSF | - | CEVAS, fMRI | Nx increased the “late” pain response after single heat stimuli. Nx produced activation of several brain regions enhanced by heat pain perception |
| [55] Kern D | TG | - | HPT, CPT, paradoxical pain*, STHR, STCR | Nx did not affect pain perception using the “thermo-grill illusion effect” |
| [56] Kotlyar M | CPTT | - | CPTT-rating (MPQ) | NTx did not affect pain perception during the CPTT |
| [57] Schoell ED | CHC, HSG | - | VAS, BOLD-signals, | Nx increased the intensity ratings for non-noxious heat stimuli. Nx affected the BOLD-signals in the ACC |
| [58] Pickering G | HSH | - | CHEP | Nx did not affect SSEP |
| Nociceptive Reflex Models | ||||
| [59] Boreau F | MSR (Tibial-TNS + EMG H-S); PSR (Sural-TNSB + EMG RII-BF); NPR (Sural-TNSA + EMG RIII-BF) | This study is not a DNIC study but uses stimulation techniques normally used in DNIC research | Reflex amplitudes (MSR [H]) and reflex thresholds (PSR [RII], NPR [RIII]) | Nx facilitated the MSR (H-reflex), but did not affect the PSR (RII-reflex) or the NPR (RIII) |
| [60] France CR | NFR (Sural-TNSC + EMG RIII-BF); EPT (Sural-TNSC) | This study is not a DNIC study but uses stimulation techniques normally used in DNIC research | Reflex thresholds (NFR [RIII]), EPT, VRS | NTx did not affect the NFR threshold. NTx was associated with increased pain ratings during NRF-assessments in women. NTx was associated with increased EPT in men. |
| [61] France CR | NFR (Sural-TNSC + EMG RIII-BF); EPT (Sural-TNSC) | This study is not a DNIC study but uses stimulation techniques normally used in DNIC research | Reflex thresholds (NFR [RIII]), EPT, EPTo, VRS | NTx was associated with hypoalgesic responding in terms of decreased NFR-activity, lower EPT and EPTo. |
| Miscellaneous Models | ||||
| [62] Eissenberg T | TCS | UV-burn# | EVAS | NTRx reversed oxycodone induced antihyperalgesia in UV-exposed skin |
| [63] Robertson LJ | HSI (RHSHG); PPR (monofilament 121 mN) | BIA | EVAS; HPT, HPR, PPR | Locally administered Nx antagonizes local antihyperalgesic effects of fentanyl in a burn, in regard to HPT, HPR, PPR |
△ Outcome variable related to specific objectives of the review.
# short lasting erythema and heat hyperalgesia.
* pain produced by a combination of non-noxious warmth and cool.
For explanation of abbreviations, please refer to legend Table 5.
3.9.2 Mechanical Stimuli
ʻInhibitoryʼ Test Paradigms. One study used pin-prick stimulations by nylon filaments [19] with bending forces from 0.08 mN to 2,492 mN [19] for assessments of detection thresholds (Table 5). One study used isometric handgrip strength measured by dynamometry [9].
ʻSensitizingʼ Test Paradigms. Innocuous stimuli with brush [26], cotton-wool [28,29], or gauze swabs [27] were used for assessment of allodynia (Table 6). Pin-prick stimulations used in 8 studies, were by nylon filaments [26–29,31,34,63] with bending forces 121 mN to 1,237 mN [34,63], or a non-flexible steel wire [30], and, were used for assessments of secondary hyperalgesia areas [26–31], pain thresholds [31,34] and pain ratings [63]. Pressure algometry was used in 4 studies for assessments of pain thresholds [34,40] and suprathreshold pain ratings [27,41]. Handgrip strength was measured by dynamometry in 8 studies [37,38,41,42,46–48,50] and skin pinching in 1 study [49]. Vibratory stimulation was used in 1 study [27].
3.9.3 Thermal Stimuli
ʻInhibitoryʼ Test Paradigms. Contact thermodes were used in 9 studies [4,16,19–25] with contact areas ranging from 1.0 cm2 to 9.0 cm2 [20,23] (Table 5). In 2 studies [9,18] radiant heat by a halogen globe directed at the skin, was used. Thermal thresholds were assessed in 7 studies [4,16,18–20,23,24] and thermal pain ratings in ten studies [9,16,17,19–25]. Eight studies used either phasic [16,19–21,23,24] or tonic heat stimuli [9,22,24,25], with temperatures ranging from 46°C to 50°C [22], stimulus duration of 5 [21] to 30 s [22] and repeated heat stimuli from 5 [22] to 64 times [21]. In 2 studies [16,19] temporal summation of heat stimuli in trains was used. In one of these [19] identical heat stimuli were used both as test stimulus and conditioning stimulus, in single mode and repeated mode, respectively. In 4 studies [9,15–17] cold-water immersion tests were used. In 1 study an ascending and descending spatial summation paradigm [17] was used, and in 2 studies [16,17] the cold-water immersion tests was employed both as test stimulus and conditioning stimulus. Two studies [24,25] used a block-testing technique, assessing heat allodynia with 3 separate 22 s stimuli using a temperature of the contact thermode calibrated at baseline corresponding to a pain rating of 7 (NRS, 0–10).
ʻSensitizingʼ Test Paradigms. Contact thermodes were used in 15 studies [26,27,31,33,36,40,42,51–55,57,58,62] with the contact areas of the thermodes ranging from 2.0 cm2 to 12.5 cm2 [26,42] (Table 6). Three studies [35,39,63] used a source of radiant heat, in 2 of the studies by a halogen globe with apertures ranging from 94 mm2 to 1 cm2 [35,63]. Thermal thresholds were assessed in 12 studies [26,27,31,35,39,40,42,51–53,55,63] and thermal pain ratings in 7 studies [27,33,36,42,57,62,63]. Ten studies used phasic [33,39,42,51,53,57,62,63] and/or tonic [36,51,54] heat stimuli, with temperatures ranging from 43°C [57] to 51.8°C [58], stimulus duration of 0.7 s [33] to 35 s [51] and repeated up to 10 times [57]. In 1 study [33] identical heat and cold stimuli were used both as test stimulus and conditioning stimulus, in single mode and repeated mode, respectively. Cold-water immersion tests (0°C to 10°C) with pain ratings were used in 4 studies [37,38,53,56].
3.10 Conditioning Stimuli
3.10.1 Electrical Stimuli
ʻInhibitoryʼ Test Paradigms. Six studies [1,2,7,10–12] used noxious electrical conditioning stimuli and 5 studies [3,5,6,13,20] used non-noxious electrical stimuli (peripheral conditioning). The studies used transcutaneous sural nerve-stimulation [1,2,10,12,20], transcutaneous nerve-stimulation [3,6,7,13], high-frequency (100 Hz) stimulation [3,5,20], or, low-frequency stimulation [13], or repetitive (1 Hz) dental stimulation [11]. Detailed stimulation characteristics are presented in Table 5.
ʻSensitizingʼ Test Paradigms. Three studies used noxious electrical conditioning stimuli applied intradermally [28–30] or transdermally [28] (Table 6). Data from the 3 studies [59–61] using a classical electrical DNIC-paradigm are reported in paragraph 3.9.1, second subsection and Table 6.
3.10.2 Mechanical Stimuli
ʻInhibitoryʼ Test Paradigms. Two studies [4,9] used the modified, ischemic submaximal effort tourniquet test, with assessment of hand grip strength, as conditioning stimulation (Table 5). One of these studies in addition used exercise (6.3 mile [10 km] run) at 85% of maximal aerobic capacity as a physiological conditioning stressor [9]. Another study employed 20 min leg and arm conditioning exercises on ergometers [13].
ʻSensitizingʼ Test Paradigms. Six studies [37,41,42,46–48] used the modified, ischemic submaximal effort tourniquet test, with assessment of hand grip strength, as conditioning stimulation (Table 6).
3.10.3 Thermal Stimuli
ʻInhibitoryʼ Test Paradigms. Nine studies [8,14–19,21,22] used thermal stimuli as a conditioning stimulus (Table 5). Cold-water-immersion tests (0 to 12.9°C) [8,15–18,21,22] and hot-water-immersion test (46°C) [14] were used in 8 studies. Two studies used cold-water-immersion tests (1 to 3°C) repeated 4 to 10 times [16,18]. Repeated heating, using a temporal summation pattern was used in 1 study [19].
ʻSensitizingʼ Test Paradigms. Six studies [26,27,31,33,62,63] used thermal stimuli as a conditioning stimulus (Table 6). First degree burn injuries, leading to development of erythema and hyperalgesia, were induced by thermodes [26,27,31] (area 12.5 cm2, 47°C, 7 min), heat probes [63] (area 0.8 cm2, 48°C, 2 min) and UV-light [62] (150W xenon lamp, UVA [400 nm] and UVB [290 nm], aperture 2 cm), in 5 studies. Repeated suprathreshold heat stimuli and infrathreshold cold stimuli, respectively, attaining a temporal summation pattern, were employed in 1 study [33]. A brief conditioning sensitization heat stimulus (brief thermal sensitization) was used in 1 study [31].
3.10.4 Pharmacological Stimuli
ʻInhibitoryʼ Test Paradigms. Conditioning with capsaicin 0.1% cream applied 30 min prior to heating with a contact thermode was used in 2 studies [24,25] (Table 5).
ʻSensitizingʼ Test Paradigms. Conditioning procedures with capsaicin administered SC (10 microg) [32], IM (50 microg) [34], and, topically, in an aqueous solution (0.4 ml, 0.6%) [35] or cream (35 mg, 10%) [36], were used in 4 studies (Table 6). Two of these studies used heat to further sensitize the capsaicin treated areas [35,36].
3.10.5 Miscellaneous Stimuli
ʻInhibitoryʼ Test Paradigms. In 3 studies [23–25] rTMS was applied as a conditioning analgesic stimulus. In the 2 latter studies [24,25] rTMS was targeted at the left dorsolateral prefrontal cortex (DLPFC) while in the third study [23] the analgesic effects were targeted at the right motor cortex (M1) and right DLPFC (Table 5).
3.11 Primary Objective and Outcome
Objective and outcome are related to the perspectives of this review and does not necessarily imply that these also are the main objectives and outcomes of the reviewed studies.
3.11.1 ʻInhibitoryʼ Test Paradigms
Conditioning Modulation Models. The primary objectives of the conditioning modulation studies are schematically presented in Fig 2A (upper part) and summarized in Table 1. All studies used a paradigm where the reversal effect of MOR-antagonist across 5 apparently different conditioning models (as defined by the authors) was examined. The conditioning models included stress-induced analgesia (7 studies) [1,2,7–10,12], spatial summation induced conditioning (1 study) [17], diffuse noxious inhibitory control (DNIC; 4 studies) [4,14–16], heterotopic noxious conditioning stimulation (1 study) [21], conditioned pain modulation (CPM [heterotopic noxious conditioning stimulation and DNIC are by some authors16;38 included in the CPM-moiety; 1 study) [22], repetitive noxious stimuli (3 studies) [11,18,19] and non-noxious frequency modulated peripheral conditioning (5 studies) [3,5,6,13,20].
The outcome variables affected by the conditioning stimulation were pain perception [4,7,9,10,12,15–23,25], pain thresholds [3,4,6,8,11,13,16,18,19], nociceptive reflex thresholds (RIII) [1,2,10,12,14,15], autonomic parameters (heart rate, respiratory rate, arterial blood pressure) [1,2,12,16], sensory detection threshold [18], MRT (blood oxygen level dependent [BOLD])-responses [21], nociceptive component of blink-reflex (R2) [5], psychometrics [9,22] and SSEP [7]. The test stimuli were applied heterotopically [4–6,8,14–16,21], homotopically [1,2,7,10,11,17,18,20] or, both heterotopically and homotopically [3,9,12,13,19,22]. The outcomes of MOR-antagonist administration were reversal of the effects of the conditioning modulation (Fig 2), examining relative increases in pain perception, pain threshold, nociceptive reflex threshold or autonomic variables.
Repetitive Transcranial Magnetic Stimulation Models. The primary objective of the dorsolateral prefrontal cortex (DLPFC) targeted rTMS-studies was to examine the effect of a MOR-antagonist on stimulation-evoked analgesia [23–25] (Table 1). The test stimuli were applied homotopically, i.e., at the right side when rTMS was targeted at the left hemisphere and vice versa. The outcomes were changes in pain perception, pain threshold and pain tolerance (Table 5).
3.11.2 ʻSensitizingʼ Test Paradigms
Secondary Hyperalgesia Models. The objectives were to examine if administration of a MOR-antagonist was associated with an increase in secondary hyperalgesia areas induced by a thermal injury [26,27,31], thermal suprathreshold stimulation [31] or noxious electrical high-intensity stimulation [28–30] (Table 2). Three studies examined either the effect of naloxone on ketamine-induced secondary hyperalgesia area [26] or opioid-induced hyperalgesia following remifentanil [28,30]. In both of these studies only data pertaining naloxone vs. placebo administration were considered relevant for this review. Another study examined re-instatement of secondary hyperalgesia area 72 hours after the burn-injury [31]. Outcomes were changes in secondary hyperalgesia areas, i.e. allodynia- or hyperalgesia-areas, evaluated by tactile or pin-prick stimuli, respectively (Table 6).
Summation Models. The objectives of the 2 summation studies were to examine the effect of a MOR-antagonist in regard to spatially directed expectation of pain [32], or temporal summation of phasic heat- and cold-stimuli [33] (Table 2). In the former, largest study (n = 173) of the review [32], SC injections of capsaicin were administered, unilaterally in the hand or in the foot, and expectations of analgesia were induced by application of a placebo cream, told to contain a ʻpowerful local anesthetic substanceʼ. This paradigm induced a placebo response in the treated body part, but not in untreated body parts. The objective of the study was to examine reversal effects of a MOR-antagonist on the placebo-response. In the latter study [33], repeated heat and cold stimuli, induced central sensitization, and the objective was to study the differential effect of naloxone on the first (single thermal stimuli [A-delta]) and second pain (repetitive thermal stimuli [C-fiber]) in the temporal summation process. The outcome parameters were in both studies pain ratings (Table 6).
ʻPainʼ Models. The objectives of these 25 studies were to examine the effect of MOR-antagonists on pain induced by capsaicin [34], capsaicin kindled by heat [35,36], cold [40,52,55], cold pressor test [37,38,53,56], electricity [39,43–45], heat [39,40,42,51–55,57,58], ischemia [37,42,46–48], or mechanical stimuli [37,38,41,42,46,47,49,50] (Table 2). The outcomes of MOR-antagonist administration compared to placebo, were changes in sensory thresholds [52], pain ratings [34,36–38,41,42,44–50,53–57], pain thresholds [34,35,39,40,42,43,51–53,55], pain tolerance [40–43,53], psychometrics [37,41,46,47], neuroimaging techniques [54,57], SSEP [44,45,58] or autonomic variables [38,49,50] (Table 6).
Nociceptive Reflex Models. The common objective of these 3 studies [59–61] was to examine the effect of MOR-antagonists on the thresholds of nociceptive flexion reflexes (Table 2). In addition, the first study [59] investigated non-nociceptive spinal reflexes, while the 2 other studies [60,61] investigated pain thresholds and pain ratings. The outcome parameters were nociceptive sural nerve stimulation induced changes in the biceps femoris muscle EMG-RIII component (Table 6).
Miscellaneous. The objective in the 2 studies was to examine the effects of MOR-antagonist on opioid induced antihyperalgesia following a burn-injury [62,63]. In both studies the MOR-antagonist was administered prior to opioid. The outcomes were pain ratings [62,63] and pain thresholds [63].
3.12 Secondary Objectives. Secondary objectives related to the administration of MOR-antagonists are presented in Tables 1 and 2.
3.13 Main Findings
3.13.1 ʻInhibitoryʼ Test Paradigms
Conditioned Modulation Models. In the 7 SIA-studies [1,2,7–10,12], naloxone reversed the antinociceptive or analgesic effects of the conditioning stimuli, substantiated by decreases in threshold of the nociceptive flexion reflex (RIII) [1,2,10,12], threshold of the monosynaptic spinal reflex [1,12], electrical pain thresholds [8], and, increases in SSEP [7] and pain ratings (Table 5) [7,10,12]. One study demonstrated complete reversal of post-exercise ischemic hypoalgesia [9], although no response of naloxone to post-exercise thermal hypoalgesia was seen.
In the spatial summation induced conditioning study [17] naloxone reversed the spatial summation induced activation of the endogenous pain inhibitory system.
In 2 [14,16] of the 4 DNIC-studies [4,14–16], a naloxone-dependent complete reversal of the DNIC-induced increase in nociceptive flexion reflex [14] and an increased cardiovascular reactivity to tonic noxious cold stimulus [16] were demonstrated. However, in the latter study [16] no effect of naloxone on the heat pain perception (DNIC-efficiency [86]), compared to placebo, was observed. In the two remaining studies the findings were ambiguous [4,15]. In one of these studies [4] a significant naloxone-dependent effects were not demonstrated, though a likely reversal effect of naloxone on the conditioning-induced increase in heat pain thresholds was seen. In the other study [15] a trend (P = 0.07) towards a naloxone-dependent blocking effect of DNIC was observed and the authors attributed this to a type II error. The sample size in this cross-over study was 20 subjects (subgroup of extensive metabolizers of sparteine) indicating that the naloxone-dependent effect in this study, probably was rather weak.
In the heterotopic noxious conditioning stimulation study [21], naloxone generally did not affect pain ratings to phasic heat test stimuli during the cold-water immersion test (CWIT), however increased pain ratings to the tonic CWIT-conditioning stimulus were observed, compared with placebo treatment. The study also demonstrated an impaired correlation between the CWIT-pain ratings and the measure of endogenous analgesia (assessed by the phasic heat stimuli) in the naloxone-sessions compared to the placebo-sessions.
In the single CPM-study [22] (Table 5), it was demonstrated that naltrexone abolished a CPM-induced decrease in heat pain ratings, but only in subjects with low ratings on the pain catastrophizing scale (PCS).
The 3 studies [11,18,19] employing repetitive noxious stimulation, utilized very different methodological designs and reached different conclusions. One study observed that local administration of naloxone was associated with augmented sensitivity during repeated CWIT [18], while the other studies [11,19] were unable to demonstrate any naloxone-dependent effects on electrical pain thresholds [11] or on the magnitude of habituation in a complex model of repeated heat stimuli [19].
In 3 out of 5 studies [3,5,6,13,20] utilizing a non-noxious frequency modulated peripheral condition stimulation model, no effect of naloxone on the nociceptive component of the blink reflex [5] or dental electrical pain thresholds [3,6] was seen. In one study a paradoxically prolonged increase in the electrical dental pain threshold was observed after naloxone administration [13], indicating a hypoalgesic effect. A study using high-frequency transcutaneous electrical nerve stimulation induced thermal hypoalgesia was not affected by placebo or low-dose naloxone (0.04 mg/kg), but was blocked with high-dose naloxone (0.28 mg/kg) [20].
In summary, 8 studies [1,2,7–10,12,17], demonstrated consistently for SIA and for spatial summation induced conditioning, that conditioning effects were reversed by naloxone, corroborating a role of the endogenous opioid system in these testing models. For the remaining models [3–6,11,13–16,18–22] ambiguous findings on the MOR-antagonist efficacy in reversing the conditioning effects were reported.
Repetitive Transcranial Magnetic Stimulation Models. In these interesting sham-controlled studies with rTMS targeted at the dorsolateral prefrontal cortex (DLPFC) [23–25] and the motor cortex (M1) [23], pre-treatment with naloxone attenuated the analgesic effect indicating an endogenous opioid-dependent mechanism of rTMS (Table 6). Two of the studies [24,25] observed significant attenuating effects of naloxone on DLPFC-targeted rTMS, while the third study [23] only observed this for M1-targeted rTMS, but not for DLPFC-targeted rTMS.
3.13.2 ʻSensitizingʼ Test Paradigms
Secondary Hyperalgesia Models. One study [29] demonstrated a dose-dependent naloxone response, with increasing magnitudes of secondary hyperalgesia areas induced by high intensity intradermal electrical stimulation. Interestingly, in 2 [28,29] of 3 studies [28–30] with intradermal electrical stimulation increased pain ratings, indicating heightened pain sensitivity, were observed following naloxone administration. However, in 5 [26–28,30,31] of the 6 secondary hyperalgesia area studies [26–31] no signs of naloxone-dependent increases in secondary hyperalgesia areas were observed (Table 6). However, one of the studies examined the late reinstatement of secondary hyperalgesia areas, 72 hrs after a mild burn-injury [31].
Summation Models. In the large placebo study [32] naloxone completely abolished the placebo response indicating that endogenous opioids, spatially modulate specific placebo responses. In the temporal summation study [33] using repeated phasic heat and cold stimuli, no effect of naloxone, compared to placebo, on thermal wind-up, “first” pain or “second” pain, was observed (Table 6).
ʻPainʼ Models. In the 18 studies [34,36–38,41,42,44–50,53–57] using pain ratings as primary outcomes, 6 studies [36,44,49,53,54,57] observed an MOR-antagonist dependent effect, while 10 studies did not observe any significant effect [34,37,38,45–48,50,55,56] (Table 6). Five studies, examining the response to MOR-antagonists, reported increases in ratings to electrical stimuli (only in pain-insensitive individuals) [44], non-noxious heat [57], noxious heat [36,54], and skin pinch [49], while 1 study reported paradoxically decreased pain ratings during the cold pressor test [53]. Thirteen studies did not report any MOR-antagonist dependent changes in pain ratings in regard to the cold pressor test [37,38,56], dynamometric tests [37,38,46,47,50], electrical stimuli [45], ischemia [41,42,48], phasic thermal stimuli [42,53,55], or, pressure and pinprick stimuli [34].
In regard to thermal thresholds 2 studies, assessing heat pain thresholds,[35,38] observed an increase in thresholds, following either local, iontophoretic [35] or systemic [38] administration of MOR-antagonist, indicating a hypoalgesic mechanism of action. However, 6 studies [40,42,51–53,55] could not substantiate any change in heat pain thresholds associated with administration of MOR-antagonist. Three of these studies [40,52,55], additionally, could not show any effects on cool detection, cold pain or cold tolerance thresholds. Two studies [39,43] examining electrical thresholds and 1 study examining vibratory thresholds [52] could not show any effect related to the systemic opioid-blockade. Three studies measured SSEP [44,45,58], but only in 1 study [45] MOR-antagonist dependent changes in SSEP were observed. In one [49] of 2 studies [49,50] using microneurographic recordings of sympathetic nerve activity (MSNA), an increase in activity related to the opioid-blockade was seen.
Interestingly, 2 neuroimaging studies [54,57], using fMRI [54] and the BOLD-contrast imaging technique [54,57] could substantiate functional changes, i.e., increases in activity of several brain regions [54] or blocked deactivation of the pregenual ACC (anterior cortex cinguli) [57], correlating with perceptual responses to noxious and non-noxious heat exposure, following administration of MOR-antagonist (Table 6).
Summarizing the results from the 25 studies, the direction of MOR-antagonist dependent effect on pain ratings, threshold assessments and SSEP appear quite ambiguous and inconsistent [42]. Any evidence for stimulation modality specific changes in response to MOR-antagonists is lacking. However, the results on heat stimuli from the 2 neuroimaging studies seem consistent and promising [54,57].
Nociceptive Reflex Models. In the first study [59] naloxone facilitated, i.e. increased the amplitude, of the monosynaptic spinal reflex, but did not affect the tactile polysynaptic reflex (RII). In 2 [59,60] of the 3 threshold studies [59–61] no effect of naloxone on the threshold of nociceptive flexion reflex (Table 6) could be demonstrated. In the third study [61] the results were somewhat at odds with previous findings, indicating lowered nociceptive flexion reflex activity (defined as the rectified biceps femoris EMG measured at the 90–150 ms post-stimulation interval) after administration of naltrexone: a hypoalgesic effect corroborated by the naltrexone-associated findings of significantly decreased pain ratings at electrical pain and tolerance thresholds. However, both in the second [60] and third study [61] administration of naltrexone during noxious sural nerve-stimulation was associated with increased pain in female subjects, while in male subjects naloxone administration was associated with an increase in electrical pain thresholds.
Miscellaneous Models. In the 2 burn-injury studies [62,63] a naloxone-dependent reversal of opioid-induced anti-hyperalgesia was demonstrated primarily by an increase in heat sensitivity (Table 6).
3.14 Adverse Effects, Withdrawals and Outliers
3.14.1 ʻInhibitoryʼ Test Paradigms
Seven of the 24 studies described either drug-related adverse effects [1,22], withdrawals not related to administration of MOR-antagonist [13,21,24,25] or the occurrence of outliers [8]. In one study [22] adverse effects, termed “mild side effects”, like mental dulling, confusion, sedation and poor balance were reported. Unfortunately this study only described mean values of the adverse effects based on the group, while the absolute number of subjects experiencing the adverse effects was not given. In the study with the highest naloxone dosis, i.e. 6,000 microg/kg, the subjects were unable to tell the correct order (with a likelihood higher than chance) of active drug vs. placebo and no adverse effects were reported [16].
3.14.2 ʻSensitizingʼ Test Paradigms
Thirteen of the 38 studies described either occurrence of drug-related adverse effects [26,27,38,39,42,51,62], withdrawals not related to administration of MOR-antagonist [30,36,38,53,57,58] or the occurrence of outliers [55]. Six subjects were reported to experience adverse effects: 1 subject had psychotropic effects due to ketamine [26], 1 subject developed a second degree burn injury [26] and 4 subjects experienced sensation of warmth, palpitations, drowsiness, nausea and vomiting [27,62]: in 3 of the subjects very likely related to administration of MOR-antagonist. In one study [39] the responses in the side effect questionnaires showed that tiredness, lightheadedness, nausea, abdominal “grumbling”, and mood changes were reported slightly more often after naloxone than after placebo. In another study [51] a "drowsiness" scale demonstrated higher values for naloxone than for placebo.
Discussion
4.1 Main Results
The principal findings of this review on opioid-antagonism in experimental pain models, are first, that naloxone, in 10 out of 25 studies, utilizing an ʻinhibitoryʼ test paradigm, consistently reversed analgesic and anti-nociceptive effects of SIA [1,2,7–10,12] and repetitive transcranial magnetic stimulation [23–25], thus implicating a role of the endogenous opioid system. Second, in the remaining 15 out of 21 conditioned modulation studies, the effects of opioid-antagonism were negative (5 studies) [3,5,6,11,19], positive (5 studies) [13,14,17,18,20] or ambiguous (5 studies) [4,15,16,21,22]. Third, among the 38 studies utilizing a ʻsensitizingʼ test paradigm, in 5 [26–28,30,31] out of 6 studies examining secondary hyperalgesia models, an effect of MOR-antagonists could not be demonstrated. Fourth, only in 4 out of the 32 remaining ʻsensitizingʼ test paradigm studies, consistent effects of opioid-antagonism were demonstrated, i.e., in 2 neuroimaging studies [54,57] and 2 burn-injury studies assessing local hyperalgesic effect of the MOR-antagonist [62,63]. Fifth, and probably the most important finding, the plethora of stimulation modalities, conditioning methods, assessment methods and extent of opioid-blockade, preclude any attempt at quantitative evaluation of the retrieved studies.
4.2 Potential Clinical Implications
4.2.1 ʻInhibitoryʼ Test Paradigm
The descending conditioned pain modulation system (DNIC or CPM; cf. 4.4.2) is considered an important factor regulating pain sensitivity in humans [87–89] and it has been suggested that pathological changes in the CPM-system are important for the development of chronic pain in chronic tension headache, fibromyalgia and persistent postoperative pain [33,88,90–94]. The CPM system is in part modulated by exogenous opioids: a sub-therapeutic dose of morphine may uncouple the conditioning system, deregulating the balance between pain sensitization and inhibition [14,95]. Impairment of the descending inhibitory systems, e.g., the EOS and CPM, may contribute to the trajectory from acute to chronic pain. Research in blockade of the opioid system may improve our understanding of the underlying pathophysiological mechanisms and may lead to a reformulation of strategies for the prevention and management of chronic pain.
4.2.2 ʻSensitizingʼ Test Paradigm
Obviously, a number of scientific issues are common for the complementary test paradigms, ITP and STP, however, injury or disease related nociceptive input to the CNS may trigger a sustained excitability and increased synaptic efficiency in central neurons [93], i.e., central sensitization (CS), a stimulus-response enhancing mode which may contribute to the development and maintenance of a chronic pain state [93,96]. Animal data suggest that CS outlasts overt signs of hyperalgesia, in a silent form termed ʻlatent sensitizationʼ (LS). The LS far outlasts the conventional duration of the injury assessed by behavioral measures, but can be unmasked by administration of a centrally acting MOR-antagonist leading to “rekindling” or reinstatement of hyperalgesia [92,93,97]. Thus, post-injury pain remission is maintained in part by the EOS that masks the pro-nociceptive components of LS. ʻLatent sensitizationʼ could prime central nociceptive circuitry such that, when inhibitory systems fail, as upon exposure to excessive stress, a pain episode ensues [93,97]. The latent predisposition to relapse, may explain the episodic nature and vulnerability to stressors that accompany chronic pain states in humans [93,97].
4.3 Dose-issue
First, while the orally administered naltrexone dose was rather uniform 50 mg [22,40,50,53,56,60–62], the parenterally administered naloxone doses, ranged from 0.21 to 6,000 microg/kg [16,29]: a 29,000 fold difference in doses across studies (Tables 3 and 4)! This difference may obviously bias the study results, particularly considering the biphasic response pattern induced by MOR-antagonists (cf. 2.3). The dose-response issue, was examined by 8 studies [20,27,29,37,39,43,46,47], but only 2 studies recognized a dose-response pattern [20,29]. The ITP-study [20] comparing naloxone 0.04 mg/kg and 0.28 mg/kg, demonstrated a significant effect of the highest dose on blockade of the analgesic effect of high-frequency transcutaneous electrical nerve stimulation. However, there are some methodological objections to this study. The authors observed highly significant sequence effects: subjects randomized to receive placebo at their first session (naloxone administered at the second and third sessions) demonstrated a higher difference in pain scores compared to the naloxone sessions, than when placebo was administered at the third session (naloxone administered at the at the first and second sessions). This effect most likely was attributed to habituation generated by the conditioning electrical stimuli (cf. 4.4.1). Since only data from first sessions with placebo administration could be used, the authors in order to compensate for the unintended reduction in statistical power, in a post-hoc manner included 3 more subjects, most likely violating the study protocol. The STP-study [29] used successively, increasing naloxone doses of 0.21, 2.1 and 21.0 microg/kg, administered as target-controlled infusions. Significant dose-dependent increases in secondary hyperalgesia areas were demonstrated (in 2 out of 3 test sessions), and this study is the only, in a statistically correct way, to confirm a dose-response relationship for naloxone in the present review.
Second, the systemic bioavailability of orally administered naltrexone and naloxone are 5% to 60% [81] and, 2% to 3% [73], respectively. Thus, in studies using oral administration [22,40,45,50,53,56,60–62] a variable and low systemic bioavailability across subjects and studies may have influenced the results.
Third, the weighted mean dose of parenterally administered naloxone, was 158 microg/kg (11.0 mg for 70 kg BW). Human data, data based on a PET-study, demonstrated complete inhibition of [11C]-carfentanil binding to opioid-receptors following 100 microg/kg naloxone [98]. The authors are not aware of additional binding-studies and though the effective naloxone blocking dose may be lower, it is interesting that only in 19 out of 53 studies in the present review, with parenterally administered naloxone, a dose of ≥ 6 mg (86 microg/kg per 70 kg BW) was used. Considering the short half-life of naloxone it seems important to maintain steady effect compartment concentrations by target-controlled infusions.
4.4 ʻInhibitoryʼ Test Paradigms
4.4.1 Stress-induced Analgesia
In the SIA-models two stimuli are required: an aversive stressor-stimulus and a noxious test-stimulus [99]. The aversive stimuli in the present SIA-studies [1,2,7,8,10,12], were intense, noxious electrical conditioning stimulation [1,2,7,10,12], (in 4 of the studies even termed ʻinescapableʼ shocks [1,2,10,12]), the cold pressor test [8], an arithmetic stressing test or a 6.3 mile run at 85% of maximal aerobic capacity [9] (Table 5). In the electrical studies an alternating procedure was used, randomizing sequences of high-intensity noxious and low-intensity tactile stimuli, in order to facilitate apprehension and discomfort, adding psychological factors to the test paradigm. Electrical noxious test-stimuli evaluating the conditioning effects were employed in all studies.
Transcutaneous electrical stimulation is a ubiquitous method used in pain research, due to its ease of use, flexibility, and in particular, due to its versatility, regarding stimulation rates, intensity adjustments and generation of sequence-patterns. The method elicits pain and hyperalgesia by direct axonal stimulation, bypassing the sensory nerve endings [100]. Electrical stimuli are thus probably more suitable for examination of central pain components, than ʻphysiologicalʼ thermal and mechanical stimuli, reflecting both peripheral and central components of the pain response [101]. High-intensity, noxious electrical stimulation (for stimulation characteristics cf. Table 5) is associated with activation of the EOS and an apparent stimulation-dependent decrease in pain ratings [28,29,102]. The degree of habituation, assessed as decrements in pain ratings, following 45–180 min continuous noxious electrical stimulation, is between 20–60%, using constant stimulation intensity [28,29,100,102,103]. Using a test paradigm, adjusting the current strength to a constant level of pain perception, the increase in stimulation intensity during 45 min of continuous stimulation, is 260% [103]! Thus, in the SIA-studies the decrements in pain ratings [7,10,12], increases in threshold of the nociceptive flexion reflex (RIII) [1,2,10,12], thresholds of the monosynaptic spinal reflex [1,12], electrical pain thresholds [8], and, decreases in SSEP [7], observed in controls, could in part be explained by habituation [7] (Table 5).
Prolonged and intense, noxious electrical conditioning stimulation activates a naloxone-sensitive (indicating recruitment of the EOS) and a naloxone-insensitive inhibitory system [29]. Interestingly, these findings are not modality specific, but also apply to noxious contact heat [104,105], laser stimuli [106] and capsaicin application [36].
In heat-models it has been shown, that habituation involves the descending antinociceptive system and in addition comprises a naloxone-insensitive component [19]. The fMRI-based studies demonstrated that part of the antinociceptive system, the rostral and subgenual anterior cingulate cortex (rACC/sgACC)) and the periaqueductal grey area, were involved in habituation, indicating a contribution of central pathways to the phenomenon of habituation [104,106].
Experimental factors that potentially may influence habituation and its central correlates are the stimulation modality, stimulation rate, the timeline of the stimulation, i.e. short-term or long-term habituation, and, the use of phasic or tonic stimulation patterns [19,103,104].
4.4.2 Diffuse Noxious Inhibitory Control and Conditioned Pain Modulation
DNIC and CPM are synonymous terms, and it has recently been recommended that DNIC should be reserved for animal and CPM for human research [88]. In the present review the terms were used explicitly as stated in the studies.
The 4 DNIC-studies [4,14–16] presented similar findings in regard to the ʻclassicalʼ DNIC-paradigm: a high intensity noxious stimulus decreased the response or increased the threshold to a heterotopically applied pain-stimulus [87]. However, naloxone-induced reversal of the DNIC-effect was only unambiguously demonstrated in one of the studies [14], an effect that would have been anticipated since previous studies have indicated opioid-sensitive components of DNIC [14,87,107]. Among the 3 DNIC-studies [4,15,16] with ambiguous findings, two of the studies were low-powered [4,16] and the authors of one of the studies stated that the negative findings could likely be attributed to a lack of statistical power (n = 6) [16]. Interestingly, one of the studies [15], seemingly adequately powered, indicated a weak naloxone-dependent effect (cf. 3.13.1).
Although the CPM-study [22] partially demonstrated a naltrexone-dependent abolishment of the conditioning induced decrease in pain response (Table 5), the general ambiguous findings in the 5 studies [4,14–16,22] seem difficult to reconcile.
4.4.3 Non-noxious Frequency Modulated Peripheral Condition Stimulation
The 5 studies on non-noxious frequency modulated peripheral conditioning did not show any consistent sign of involvement of the EOS [3,5,6,13,20].
4.4.4 Repetitive Transcranial Magnetic Stimulation
The methodological qualities of these studies were among the highest in the present review. An advantage was that the studies used sham-controlled and placebo-controlled procedures. Two of the studies [24,25] observed significant attenuating effects of naloxone on DLPFC-targeted rTMS, while the third study [23] only observed this for M1-targeted rTMS. The studies utilized thermal test paradigms, although they differed in regard to pretreatment with capsaicin that was used in two of the studies [24,25], i.e., application of capsaicin may lead to more intense pain perception [108]. The studies also differed in regard to left [24,25] and right [23] hemisphere targeted stimulation.
4.5 ʻSensitizingʼ Test Paradigms
4.5.1 Secondary Hyperalgesia Models
One study [29] demonstrated a dose-dependent naloxone response, with increasing magnitudes of secondary hyperalgesia areas induced by noxious, high intensity, intradermal electrical stimulation. Interestingly, in a preceding study by the same research group [28], using a nearly identical set-up, naloxone-infusion 10 microg/kg, was associated with a highly significant increase in secondary hyperalgesia area (140%) compared to pre-infusion values (P < 0.01). However, since the baseline values successively increased during the 30 min infusion period, the increase in secondary hyperalgesia areas compared to controls, did not reach significance (P = 0.16; deviations in baseline assessments in noxious electrical stimulation, cf. 4.4.1). The study abstract correctly indicated that naloxone resulted in increased pain ratings (ʻantianalgesiaʼ; P < 0.001), but, erroneously indicated that naloxone resulted in ʻmechanical hyperalgesia (P < 0.01)ʼ [28]. The third secondary hyperalgesia study using high intensity intradermal electrical stimulation, on remifentanil-induced opioid hyperalgesia (OIH) [30] was not able to demonstrate any effect of naloxone on secondary hyperalgesia. Though the study generally had a double-blind, controlled and randomized design, the naloxone part of the investigation did not include a placebo arm per se, but naloxone was administered blinded to the remifentanil and the placebo groups.
Consequently, in 5 of 6 secondary hyperalgesia studies obvious signs of EOS involvement could not be demonstrated, however, naloxone-dependent hyperalgesic responses during high intensity noxious electricity stimulation cannot be excluded. Recent data, examining latent sensitization [109] using a burn injury model [31] indicated that administration of a high dose of naloxone 2 mg/kg, 1 week after the injury, in 4 out of 12 subjects seem to be associated with late re-instatement of secondary hyperalgesia areas (submitted: Pereira MP et al. ʻEndogenous opioid-masked latent pain sensitization: studies from mouse to human.ʼ).
4.6 Study Bias
4.6.1 General Issues
The bibliographic age and the exploratory nature of the studies should be taken into consideration when discussing study bias, i.e., the risk that the true intervention effect will be overestimated or underestimated (http://handbook.cochrane.org/ [accessed 07.24.2014]). The present review using the simple Oxford quality scoring system from 1996 [68] demonstrated a high likelihood of bias, due to inaccurate reporting of randomization and blinding procedures. The Oxford quality scoring system was chosen in respect of the bibliographic age of the studies since it presents a more lenient evaluation paradigm than more sophisticated methods like the Cochrane Collaboration’s tool for assessing risk of bias. Approximately 25% and 50% of the studies were published before 1984 and before 2000, respectively, while the early report on the Consolidated Standards of Reporting Trials (CONSORT) was published in 1996 [110], with revised versions 2001 [111] and 2010 [112]. Compliance to these standards has been a requirement for randomized controlled trials (RCTs) in a number of clinical journals for more than 17 years [110]. The CONSORT statement thus contains guidelines applicable to clinical RCTs, but is it relevant for experimental RCTs?
The editorial accompanying the first CONSORT publication stated: “It seems reasonable to hope that, in addition to improved reporting, the wide adoption of this new publication standard will improve the conduct of future research by increasing awareness of the requirements for a good trial. Such success might lead to similar initiatives for other types of research”[110]. Requirements for clinical RCTs as outlined in CONSORT and SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) [113], could also be considered essential for experimental research in order to heighten validity, reliability and reproducibility of data, facilitating accurate reporting, evaluation and interpretation of study-data. Guidelines for reporting animal research data, ARRIVE (Animals in Research: Reporting In Vivo Experiments) [114], based on the CONSORT criteria, have been published and even extrapolated for use in a review including human experimental research [115].
4.6.2 Statistical Issues
The heterogeneity of the statistical methods used was considerable. Various ANOVA-methods, some rather advanced [24,42], were used in 41/63 studies, while a priori and post-hoc sample size estimations were only employed in 4/63 and 3/63 studies, respectively. Furthermore, in 49/63 studies, statistical methods aimed at reducing the risk of type I error (α [false positive]) associated with multiple comparisons, were not applied. It can readily be calculated that the likelihood by chance of achieving one or more false positive results, presenting as significant values (P < 0.05), during 5 and 10 uncorrected pair-wise comparisons, which was a normal procedure in the studies, are 23% and 40%, respectively, giving a high likelihood for falsely rejecting the null hypothesis [116,117]. A simple measure to attenuate the risk is to decrease the significance level to 1% which would give corresponding likelihoods of less than 4.9% and 9.6%, respectively. Conversely, the risk of committing a type II error (β [false negative]), i.e., indicating the power of the study, was generally not reported in the studies, although the limited sample size was discussed in 10/63 studies.
However, it could be argued that all the reviewed studies are experimental, and as such exploratory and hypothesis-generating in nature. In studies of healthy individuals, inferences from qualitative aspects, within-subject variances and fixed-effect models are often more important than inferences from quantitative aspects, between-subject variances and random-effect models, the latter being preferred in clinical research examining groups of patients [118]. The number of subjects needed is obviously much smaller for experimental research compared to clinical studies, mainly due to a much larger inherent biological variance in patients compared to healthy subjects. However, the exploratory nature of an experimental study is sometimes used as a an excuse for not adhering strictly to common statistical requirements [117]. For all research, decisions on the null hypothesis, primary and secondary outcomes, and, estimations of outcome variability (from pilot-data if not available from literature), minimal relevant differences, sample size and effect size calculations should be stated even in studies of exploratory nature. Otherwise, there is an obvious risk of wasting valuable research time and efforts, leading to ethical, economical or scientific dilemmas, which might impede future research [116,117,119].
4.6.3 Methodological Issues
Lack of standardization across the studies and the stimulation methods are evident (Tables 5 and 6). Guidelines for sensory testing procedures have been presented [120–123], but standardized protocols, like the German Research Network on Neuropathic Pain (DFNS) [122–124] were not used in any of the studies. Aspects of data reproducibility and validity were only discussed in few studies [29,31,125].
Conclusion
ʻThe consistent failure to find an effect of naloxone on experimental pain in humans suggests that endorphin release did not occur during these proceduresʼ [37].
This systematic review on endogenous opioid antagonism in physiological experimental pain models concludes that naloxone appears to have a demonstrable and relatively reliable effect in stress-induced analgesia (in all 7 studies) and repetitive transcranial magnetic stimulation (in all 3 studies). In all other pain models, both naloxone and naltrexone demonstrate a variable and unreliable effect.
Supporting Information
(PDF)
Data Availability
All relevant data are included within the paper.
Funding Statement
The authors have no support or funding to report.
References
- 1. Willer JC, Albe-Fessard D. Electrophysiological evidence for a release of endogenous opiates in stress-induced 'analgesia' in man. Brain Res. 1980; 198: 419–426. [DOI] [PubMed] [Google Scholar]
- 2. Willer JC, Dehen H, Cambier J. Stress-induced analgesia in humans: endogenous opioids and naloxone-reversible depression of pain reflexes. Science. 1981; 212: 689–691. [DOI] [PubMed] [Google Scholar]
- 3. Pertovaara A, Kemppainen P. The influence of naloxone on dental pain threshold elevation produced by peripheral conditioning stimulation at high frequency. Brain Res. 1981; 215: 426–429. [DOI] [PubMed] [Google Scholar]
- 4. Pertovaara A, Kemppainen P, Johansson G, Karonen SL. Ischemic pain nonsegmentally produces a predominant reduction of pain and thermal sensitivity in man: a selective role for endogenous opioids. Brain Res. 1982; 251: 83–92. [DOI] [PubMed] [Google Scholar]
- 5. Willer JC, Roby A, Boulu P, Albe-Fessard D. Depressive effect of high frequency peripheral conditioning stimulation upon the nociceptive component of the human blink reflex. Lack of naloxone effect. Brain Res. 1982; 239: 322–326. [DOI] [PubMed] [Google Scholar]
- 6. Pertovaara A, Kemppainen P, Johansson G, Karonen SL. Dental analgesia produced by non-painful low-frequency stimulation is not influenced by stress or reversed by naloxone. Pain. 1982; 13: 379–384. [DOI] [PubMed] [Google Scholar]
- 7. Buchsbaum MS, Davis GC, Naber D, Pickar D. Pain enhances naloxone-induced hyperalgesia in humans as assessed by somatosensory evoked potentials. Psychopharmacology (Berl). 1983; 79: 99–103. [DOI] [PubMed] [Google Scholar]
- 8. Jungkunz G, Engel RR, King UG, Kuss HJ. Endogenous opiates increase pain tolerance after stress in humans. Psychiatry Res. 1983; 8: 13–18. [DOI] [PubMed] [Google Scholar]
- 9. Janal MN, Colt EW, Clark WC, Glusman M. Pain sensitivity, mood and plasma endocrine levels in man following long-distance running: effects of naloxone. Pain. 1984; 19: 13–25. [DOI] [PubMed] [Google Scholar]
- 10. Willer JC, Ernst M. Diazepam reduces stress-induced analgesia in humans. Brain Res. 1986; 362: 398–402. [DOI] [PubMed] [Google Scholar]
- 11. Ernst M, Lee MH, Dworkin B, Zaretsky HH. Pain perception decrement produced through repeated stimulation. Pain. 1986; 26: 221–231. [DOI] [PubMed] [Google Scholar]
- 12. Willer JC, Ernst M. Somatovegetative changes in stress-induced analgesia in man: an electrophysiological and pharmacological study. Ann N Y Acad Sci. 1986; 467: 256–272. [DOI] [PubMed] [Google Scholar]
- 13. Olausson B, Eriksson E, Ellmarker L, Rydenhag B, Shyu BC, Andersson SA. Effects of naloxone on dental pain threshold following muscle exercise and low frequency transcutaneous nerve stimulation: a comparative study in man. Acta Physiol Scand. 1986; 126: 299–305. [DOI] [PubMed] [Google Scholar]
- 14. Willer JC, Le Bars D, De Broucker T. Diffuse noxious inhibitory controls in man: involvement of an opioidergic link. Eur J Pharmacol. 1990; 182: 347–355. [DOI] [PubMed] [Google Scholar]
- 15. Poulsen L, Arendt-Nielsen L, Brøsen K, Gram LF, Sindrup SH. Different effect of naloxone on pain perception in extensive and poor metabolizers of sparteine? Analgesia. 1996; 2: 255–258. [Google Scholar]
- 16. Edwards RR, Ness TJ, Fillingim RB. Endogenous opioids, blood pressure, and diffuse noxious inhibitory controls: a preliminary study. Percept Mot Skills. 2004; 99: 679–687. [DOI] [PubMed] [Google Scholar]
- 17. Julien N, Marchand S. Endogenous pain inhibitory systems activated by spatial summation are opioid-mediated. Neurosci Lett. 2006; 401: 256–260. [DOI] [PubMed] [Google Scholar]
- 18. Robertson LJ, Hammond GR, Drummond PD. The effect of subcutaneous naloxone on experimentally induced pain. J Pain. 2008; 9: 79–87. [DOI] [PubMed] [Google Scholar]
- 19. Rennefeld C, Wiech K, Schoell ED, Lorenz J, Bingel U. Habituation to pain: further support for a central component. Pain. 2010; 148: 503–508. 10.1016/j.pain.2009.12.014 [DOI] [PubMed] [Google Scholar]
- 20. Leonard G, Goffaux P, Marchand S. Deciphering the role of endogenous opioids in high-frequency TENS using low and high doses of naloxone. Pain. 2010; 151: 215–219. 10.1016/j.pain.2010.07.012 [DOI] [PubMed] [Google Scholar]
- 21. Sprenger C, Bingel U, Buchel C. Treating pain with pain: supraspinal mechanisms of endogenous analgesia elicited by heterotopic noxious conditioning stimulation. Pain. 2011; 152: 428–439. 10.1016/j.pain.2010.11.018 [DOI] [PubMed] [Google Scholar]
- 22. King CD, Goodin B, Kindler LL, Caudle RM, Edwards RR, Gravenstein N et al. Reduction of conditioned pain modulation in humans by naltrexone: an exploratory study of the effects of pain catastrophizing. J Behav Med. 2013; 36: 315–327. 10.1007/s10865-012-9424-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. de Andrade DC, Mhalla A, Adam F, Texeira MJ, Bouhassira D. Neuropharmacological basis of rTMS-induced analgesia: the role of endogenous opioids. Pain. 2011; 152: 320–326. 10.1016/j.pain.2010.10.032 [DOI] [PubMed] [Google Scholar]
- 24. Taylor JJ, Borckardt JJ, George MS. Endogenous opioids mediate left dorsolateral prefrontal cortex rTMS-induced analgesia. Pain. 2012; 153: 1219–1225. 10.1016/j.pain.2012.02.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Taylor JJ, Borckardt JJ, Canterberry M, Li X, Hanlon CA, Brown TR, George MS. Naloxone-reversible modulation of pain circuitry by left prefrontal rTMS. Neuropsychopharmacology. 2013; 38: 1189–1197. 10.1038/npp.2013.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mikkelsen S, Ilkjaer S, Brennum J, Borgbjerg FM, Dahl JB. The effect of naloxone on ketamine-induced effects on hyperalgesia and ketamine-induced side effects in humans. Anesthesiology. 1999; 90: 1539–1545. [DOI] [PubMed] [Google Scholar]
- 27. Brennum J, Kaiser F, Dahl JB. Effect of naloxone on primary and secondary hyperalgesia induced by the human burn injury model. Acta Anaesthesiol Scand. 2001; 45: 954–960. [DOI] [PubMed] [Google Scholar]
- 28. Koppert W, Angst M, Alsheimer M, Sittl R, Albrecht S, Schuttler J et al. Naloxone provokes similar pain facilitation as observed after short-term infusion of remifentanil in humans. Pain. 2003; 106: 91–99. [DOI] [PubMed] [Google Scholar]
- 29. Koppert W, Filitz J, Troster A, Ihmsen H, Angst M, Flor H et al. Activation of naloxone-sensitive and-insensitive inhibitory systems in a human pain model. J Pain. 2005; 6: 757–764. [DOI] [PubMed] [Google Scholar]
- 30. Chu LF, Dairmont J, Zamora AK, Young CA, Angst MS. The endogenous opioid system is not involved in modulation of opioid-induced hyperalgesia. J Pain. 2011; 12: 108–115. 10.1016/j.jpain.2010.05.006 [DOI] [PubMed] [Google Scholar]
- 31. Pereira MP, Werner MU, Ringsted TK, Rowbotham MC, Taylor BK, Dahl JB (2013) Does naloxone reinstate secondary hyperalgesia in humans after resolution of a burn injury? A placebo-controlled, double-blind, randomized, cross-over study. PLoS One. 2013; 8: e64608 10.1371/journal.pone.0064608 PONE-D-13-08611 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Benedetti F, Arduino C, Amanzio M. Somatotopic activation of opioid systems by target-directed expectations of analgesia. J Neurosci. 1999; 19: 3639–3648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Price DD, Staud R, Robinson ME, Mauderli AP, Cannon R, Vierck CJ. Enhanced temporal summation of second pain and its central modulation in fibromyalgia patients. Pain. 2002; 99: 49–59. [DOI] [PubMed] [Google Scholar]
- 34. Graven-Nielsen T, Gibson SJ, Laursen RJ, Svensson P, Arendt-Nielsen L. Opioid-insensitive hypoalgesia to mechanical stimuli at sites ipsilateral and contralateral to experimental muscle pain in human volunteers. Exp Brain Res. 2002; 146: 213–222. [DOI] [PubMed] [Google Scholar]
- 35. Drummond PD. The effect of peripheral opioid block and body cooling on sensitivity to heat in capsaicin-treated skin. Anesth Analg. 2000; 90: 923–927. [DOI] [PubMed] [Google Scholar]
- 36. Anderson WS, Sheth RN, Bencherif B, Frost JJ, Campbell JN. Naloxone increases pain induced by topical capsaicin in healthy human volunteers. Pain. 2002; 99: 207–216. [DOI] [PubMed] [Google Scholar]
- 37. Grevert P, Goldstein A. Endorphins: naloxone fails to alter experimental pain or mood in humans. Science. 1978: 199: 1093–1095. [DOI] [PubMed] [Google Scholar]
- 38. McCubbin JA, Bruehl S. Do endogenous opioids mediate the relationship between blood pressure and pain sensitivity in normotensives? Pain. 1994; 57: 63–67. [DOI] [PubMed] [Google Scholar]
- 39. Stacher G, Abatzi TA, Schulte F, Schneider C, Stacher-Janotta G, Gaupmann G et al. Naloxone does not alter the perception of pain induced by electrical and thermal stimulation of the skin in healthy humans. Pain. 1988; 34: 271–276. [DOI] [PubMed] [Google Scholar]
- 40. Younger JW, Zautra AJ, Cummins ET. Effects of naltrexone on pain sensitivity and mood in fibromyalgia: no evidence for endogenous opioid pathophysiology. PLoS One. 2009; 4: e5180 10.1371/journal.pone.0005180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bruehl S, Burns JW, Chung OY, Chont M. What do plasma beta-endorphin levels reveal about endogenous opioid analgesic function? Eur J Pain. 2012; 16: 370–380. 10.1002/j.1532-2149.2011.00021.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bruehl S, Burns JW, Gupta R, Buvanendran A, Chont M, Kinner E et al. Endogenous opioid function mediates the association between laboratory-evoked pain sensitivity and morphine analgesic responses. Pain. 2013; 154: 1856–1864. 10.1016/j.pain.2013.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. El-Sobky A, Dostrovsky JO, Wall PD. Lack of effect of naloxone on pain perception in humans. Nature. 1976; 263: 783–784. [DOI] [PubMed] [Google Scholar]
- 44. Buchsbaum MS, Davis GC, Bunney WE Jr. Naloxone alters pain perception and somatosensory evoked potentials in normal subjects. Nature. 1977; 270: 620–622. [DOI] [PubMed] [Google Scholar]
- 45. Bromm B, Meier W, Scharein E. Antagonism between tilidine and naloxone on cerebral potentials and pain ratings in man. Eur J Pharmacol. 1983; 87: 431–439. [DOI] [PubMed] [Google Scholar]
- 46. Grevert P, Goldstein A. Effects of naloxone on experimentally induced ischemic pain and on mood in human subjects. Proc Natl Acad Sci U S A. 1977; 74: 1291–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Grevert P, Albert LH, Inturrisi CE, Goldstein A Effects of eight-hour naloxone infusions on human subjects. Biol Psychiatry. 1983; 18: 1375–1392. [PubMed] [Google Scholar]
- 48. Posner J, Burke CA. The effects of naloxone on opiate and placebo analgesia in healthy volunteers. Psychopharmacology (Berl). 1985; 87: 468–472. [DOI] [PubMed] [Google Scholar]
- 49. Schobel HP, Handwerker HO, Schmieder RE, Heusser K, Dominiak P, Luft FC. Effects of naloxone on hemodynamic and sympathetic nerve responses to pain in normotensive vs. borderline hypertensive men. J Auton Nerv Syst. 1998. 69: 49–55. [DOI] [PubMed] [Google Scholar]
- 50. Cook DB, O'Connor PJ, Ray CA. Muscle pain perception and sympathetic nerve activity to exercise during opioid modulation. Am J Physiol Regul Integr Comp Physiol. 2000; 279: R1565–R1573. [DOI] [PubMed] [Google Scholar]
- 51. Lautenbacher S, Pauls AM, Strian F, Pirke KM, Krieg JC. Pain perception in patients with eating disorders. Psychosom Med. 1990; 52: 673–682. [DOI] [PubMed] [Google Scholar]
- 52. Lautenbacher S, Roscher S, Strian D, Fassbender K, Krumrey K, Krieg JC. Pain perception in depression: relationships to symptomatology and naloxone-sensitive mechanisms. Psychosom Med. 1994; 56: 345–352. [DOI] [PubMed] [Google Scholar]
- 53. al'Absi M, Wittmers LE, Ellestad D, Nordehn G, Kim SW, Kirschbaum C et al. Sex differences in pain and hypothalamic-pituitary-adrenocortical responses to opioid blockade. Psychosom Med. 2004; 66: 198–206. [DOI] [PubMed] [Google Scholar]
- 54. Borras MC, Becerra L, Ploghaus A, Gostic JM, DaSilva A, Gonzalez RG et al. fMRI measurement of CNS responses to naloxone infusion and subsequent mild noxious thermal stimuli in healthy volunteers. J Neurophysiol. 2004; 91: 2723–2733. [DOI] [PubMed] [Google Scholar]
- 55. Kern D, Pelle-Lancien E, Luce V, Bouhassira D. Pharmacological dissection of the paradoxical pain induced by a thermal grill. Pain. 2008; 135: 291–299. 10.1016/j.pain.2007.12.001 [DOI] [PubMed] [Google Scholar]
- 56. Kotlyar M, al'Absi M, Brauer LH, Grant JE, Fong E, Kim SW. Naltrexone effect on physiological and subjective response to a cold pressor task. Biol Psychol. 2008; 77: 233–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Schoell ED, Bingel U, Eippert F, Yacubian J, Christiansen K, Andresen H et al. The effect of opioid receptor blockade on the neural processing of thermal stimuli. PLoS One. 2010; 5: e12344 10.1371/journal.pone.0012344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Pickering G, Moustafa F, Desbrandes S, Cardot JM, Roux D, Dubray C. Paracetamol and opioid pathways: a pilot randomized clinical trial. Fundam Clin Pharmacol. 2013; 27: 339–345. 10.1111/j.1472-8206.2011.01010.x [DOI] [PubMed] [Google Scholar]
- 59. Boureau F, Willer JC, Dauthier C. Study of naloxone in normal awake man: effects on spinal reflexes. Neuropharmacology. 1978; 17: 565–568. [DOI] [PubMed] [Google Scholar]
- 60. France CR, al'Absi M, Ring C, France JL, Brose J, Spaeth D et al. Assessment of opiate modulation of pain and nociceptive responding in young adults with a parental history of hypertension. Biol Psychol. 2005; 70: 168–174. [DOI] [PubMed] [Google Scholar]
- 61. France CR, al'Absi M, Ring C, France JL, Harju A, Wittmers LE. Nociceptive flexion reflex and pain rating responses during endogenous opiate blockade with naltrexone in healthy young adults. Biol Psychol. 2007; 75: 95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Eissenberg T, Riggins EC III, Harkins SW, Weaver MF. A clinical laboratory model for direct assessment of medication-induced antihyperalgesia and subjective effects: initial validation study. Exp Clin Psychopharmacol. 2000; 8: 47–60. [DOI] [PubMed] [Google Scholar]
- 63. Robertson LJ, Drummond PD, Hammond GR. Naloxone antagonizes the local antihyperalgesic effect of fentanyl in burnt skin of healthy humans. J Pain. 2007; 8: 489–493. [DOI] [PubMed] [Google Scholar]
- 64. Taylor R Jr., Pergolizzi JV Jr., Porreca F, Raffa RB. Opioid antagonists for pain. Expert Opin Investig Drugs. 2013; 22: 517–525. 10.1517/13543784.2013.778973 [DOI] [PubMed] [Google Scholar]
- 65. Pert A, Yaksh T. Sites of morphine induced analgesia in the primate brain: relation to pain pathways. Brain Res. 1974; 80: 135–140. [DOI] [PubMed] [Google Scholar]
- 66. Richardson DE. Brain stimulation for pain control. IEEE Trans Biomed Eng. 1976; 23: 304–306. [DOI] [PubMed] [Google Scholar]
- 67. Adams JE. Naloxone reversal of analgesia produced by brain stimulation in the human. Pain. 1976; 2: 161–166. [PubMed] [Google Scholar]
- 68. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996; 17: 1–12. [DOI] [PubMed] [Google Scholar]
- 69. Yarnitsky D, Arendt-Nielsen L, Bouhassira D, Edwards RR, Fillingim RB, Granot M et al. Recommendations on terminology and practice of psychophysical DNIC testing. Eur J Pain. 2010; 14: 339 10.1016/j.ejpain.2010.02.004 [DOI] [PubMed] [Google Scholar]
- 70. Gracely RH. Studies of pain in human subjects In: MacMahon SB, Koltzenburg M, Tracey I, Turk DC, editors. Wall and Melzack's Textbook of Pain. Philadelphia, PA: Elsevier Saunders; 2013; pp. 283–300. [Google Scholar]
- 71. Glaser EM, Whittaker GC. Evidence for a non-specific mechanism of habituation. J Physiol. 1953; 122: 43–4P. [PubMed] [Google Scholar]
- 72. Rang HP, Dale MM, Ritter JM, Flower RJ. Analgesic drugs In: Rang HP, Dale MM, Ritter JM, Flower RJ, editors. Rang and Dale´s pharmacology. Churchill Livingstone; 2007; pp. 588–609. [Google Scholar]
- 73. Smith K, Hopp M, Mundin G, Bond S, Bailey P, Woodward J, Bell D. Low absolute bioavailability of oral naloxone in healthy subjects. Int J Clin Pharmacol Ther. 2012; 50: 360–367. [DOI] [PubMed] [Google Scholar]
- 74. Glass PS, Jhaveri RM, Smith LR. Comparison of potency and duration of action of nalmefene and naloxone. Anesth Analg. 1994; 78: 536–541. [DOI] [PubMed] [Google Scholar]
- 75. Chamberlain JM, Klein BL. A comprehensive review of naloxone for the emergency physician. Am J Emerg Med. 1994; 12: 650–660. [DOI] [PubMed] [Google Scholar]
- 76. Watson M, Lucas C, Hoy A, Back I. Principles of drug use in palliative medicine In: Watson M, Lucas C, Hoy A, Back I, editors. Oxford handbook of palliative care. Oxford University Press; 2005; pp. 35–79. [Google Scholar]
- 77. Calabrese EJ. Pain and u-shaped dose responses: occurrence, mechanisms, and clinical implications. Crit Rev Toxicol. 2008. 38: 579–590. 10.1080/10408440802026281 [DOI] [PubMed] [Google Scholar]
- 78. Levine JD, Gordon NC, Fields HL. Naloxone dose dependently produces analgesia and hyperalgesia in postoperative pain. Nature. 1979; 278: 740–741. [DOI] [PubMed] [Google Scholar]
- 79. Levine JD, Gordon NC. Influence of the method of drug administration on analgesic response. Nature. 1984; 312: 755–756. [DOI] [PubMed] [Google Scholar]
- 80. Levine JD, Gordon NC. Method of administration determines the effect of naloxone on pain. Brain Res. 1986; 365: 377–378. [DOI] [PubMed] [Google Scholar]
- 81. Gonzalez JP, Brogden RN. Naltrexone. A review of its pharmacodynamic and pharmacokinetic properties and therapeutic efficacy in the management of opioid dependence. Drugs. 1988; 35: 192–213. [DOI] [PubMed] [Google Scholar]
- 82. Crabtree BL. Review of naltrexone, a long-acting opiate antagonist. Clin Pharm. 1984; 3: 273–280. [PubMed] [Google Scholar]
- 83. Cohen J. A power primer. Psychol Bull. 1992; 112: 155–159. [DOI] [PubMed] [Google Scholar]
- 84. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004; 36: 717–731. [DOI] [PubMed] [Google Scholar]
- 85. Bruehl S, Burns JW, Chung OY, Chont M. Interacting effects of trait anger and acute anger arousal on pain: the role of endogenous opioids. Psychosom Med. 2011; 73: 612–619. 10.1097/PSY.0b013e318227cb88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Pud D, Granovsky Y, Yarnitsky D. The methodology of experimentally induced diffuse noxious inhibitory control (DNIC)-like effect in humans. Pain. 2009; 144: 16–19. 10.1016/j.pain.2009.02.015 [DOI] [PubMed] [Google Scholar]
- 87. van WG, Veldhuijzen DS. Perspective on diffuse noxious inhibitory controls as a model of endogenous pain modulation in clinical pain syndromes. J Pain. 2010; 11: 408–419. 10.1016/j.jpain.2009.10.009 [DOI] [PubMed] [Google Scholar]
- 88. Yarnitsky D. Conditioned pain modulation (the diffuse noxious inhibitory control-like effect): its relevance for acute and chronic pain states. Curr Opin Anaesthesiol. 2010; 23: 611–615. 10.1097/ACO.0b013e32833c348b [DOI] [PubMed] [Google Scholar]
- 89. Brock C, Olesen SS, Valeriani M, Arendt-Nielsen L, Drewes AM. Brain activity in rectosigmoid pain: unravelling conditioning pain modulatory pathways. Clin Neurophysiol. 2012; 123: 829–837. 10.1016/j.clinph.2011.07.047 [DOI] [PubMed] [Google Scholar]
- 90. Yarnitsky D, Crispel Y, Eisenberg E, Granovsky Y, Ben-Nun B, Best LA et al. Prediction of chronic post-operative pain: pre-operative DNIC testing identifies patients at risk. Pain. 2008; 138: 22–28. [DOI] [PubMed] [Google Scholar]
- 91. Pielsticker A, Haag G, Zaudig M, Lautenbacher S. Impairment of pain inhibition in chronic tension-type headache. Pain. 2005; 118: 215–223. [DOI] [PubMed] [Google Scholar]
- 92. Staud R, Weyl EE, Price DD, Robinson ME. Mechanical and heat hyperalgesia highly predict clinical pain intensity in patients with chronic musculoskeletal pain syndromes. J Pain. 2012; 13: 725–735. 10.1016/j.jpain.2012.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011; 152: S2–15. 10.1016/j.pain.2010.09.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. van Wilgen CP, Keizer D. The sensitization model to explain how chronic pain exists without tissue damage. Pain Manag Nurs. 2012; 13: 60–65. 10.1016/j.pmn.2010.03.001 [DOI] [PubMed] [Google Scholar]
- 95. Le Bars D, Villanueva L, Bouhassira D, Willer JC. Diffuse noxious inhibitory controls (DNIC) in animals and in man. Patol Fiziol Eksp Ter. 1992; 55–65. . [PubMed] [Google Scholar]
- 96. Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009; 10: 895–926. 10.1016/j.jpain.2009.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Schweinhardt P, Sauro KM, Bushnell MC. Fibromyalgia: a disorder of the brain? Neuroscientist. 2008; 14: 415–421. 10.1177/1073858407312521 [DOI] [PubMed] [Google Scholar]
- 98. Frost JJ, Douglass KH, Mayberg HS, Dannals RF, Links JM, Wilson AA et al. Multicompartmental analysis of [11C]-carfentanil binding to opiate receptors in humans measured by positron emission tomography. J Cereb Blood Flow Metab. 1989; 9: 398–409. [DOI] [PubMed] [Google Scholar]
- 99. Butler RK, Finn DP. Stress-induced analgesia. Prog Neurobiol. 2009; 88: 184–202. 10.1016/j.pneurobio.2009.04.003 [DOI] [PubMed] [Google Scholar]
- 100. Troster A, Ihmsen H, Singler B, Filitz J, Koppert W. Interaction of fentanyl and buprenorphine in an experimental model of pain and central sensitization in human volunteers. Clin J Pain. 2012; 28: 705–711. 10.1097/AJP.0b013e318241d948 [DOI] [PubMed] [Google Scholar]
- 101. Ravn P, Secher EL, Skram U, Therkildsen T, Christrup LL, Werner MU. Morphine- and buprenorphine-induced analgesia and antihyperalgesia in a human inflammatory pain model: a double-blind, randomized, placebo-controlled, five-arm crossover study. J Pain Res. 2013; 6: 23–38. 10.2147/JPR.S36827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Koppert W, Ihmsen H, Korber N, Wehrfritz A, Sittl R, Schmelz M et al. Different profiles of buprenorphine-induced analgesia and antihyperalgesia in a human pain model. Pain. 2005; 118: 15–22. [DOI] [PubMed] [Google Scholar]
- 103. Nickel FT, Ott S, Mohringer S, Saake M, Dorfler A, Seifert F et al. Brain correlates of short-term habituation to repetitive electrical noxious stimulation. Eur J Pain. 2014; 18: 56–66. 10.1002/j.1532-2149.2013.00339.x [DOI] [PubMed] [Google Scholar]
- 104. Bingel U, Schoell E, Herken W, Buchel C, May A. Habituation to painful stimulation involves the antinociceptive system. Pain. 2007. 131: 21–30. [DOI] [PubMed] [Google Scholar]
- 105. Bingel U, Herken W, Teutsch S, May A. Habituation to painful stimulation involves the antinociceptive system—a 1-year follow-up of 10 participants. Pain. 2008; 140: 393–394. 10.1016/j.pain.2008.09.030 [DOI] [PubMed] [Google Scholar]
- 106. Mobascher A, Brinkmeyer J, Warbrick T, Musso F, Schlemper V, Wittsack HJ et al. Brain activation patterns underlying fast habituation to painful laser stimuli. Int J Psychophysiol. 2010; 75: 16–24. 10.1016/j.ijpsycho.2009.10.008 [DOI] [PubMed] [Google Scholar]
- 107. Le Bars D, Willer JC, De Broucker T. Morphine blocks descending pain inhibitory controls in humans. Pain. 1992; 48: 13–20. [DOI] [PubMed] [Google Scholar]
- 108. Petersen KL, Rowbotham MC. A new human experimental pain model: the heat/capsaicin sensitization model. Neuroreport. 1999; 10: 1511–1516. [DOI] [PubMed] [Google Scholar]
- 109. Corder G, Doolen S, Donahue RR, Winter MK, Jutras BL, He Y et al. Constitutive mu-opioid receptor activity leads to long-term endogenous analgesia and dependence. Science. 2013; 341: 1394–1399. 10.1126/science.1239403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Altman DG. Better reporting of randomised controlled trials: the CONSORT statement. BMJ. 1996; 313: 570–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Ann Intern Med. 2001; 134: 657–662. [DOI] [PubMed] [Google Scholar]
- 112. Schulz KF, Moher D, Altman DG. CONSORT 2010 comments. Lancet. 2010: 376: 1222–1223. 10.1016/S0140-6736(10)61879-X [DOI] [PubMed] [Google Scholar]
- 113. Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gotzsche PC, Krleza-Jeric K et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013; 158: 200–207. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Kilkenny C, Browne W, Cuthill IC, Emerson M, Altman DG. Animal research: reporting in vivo experiments—the ARRIVE guidelines. J Cereb Blood Flow Metab. 2011; 31: 991–993. 10.1038/jcbfm.2010.220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Vignoletti F, Abrahamsson I. Quality of reporting of experimental research in implant dentistry. Critical aspects in design, outcome assessment and model validation. J Clin Periodontol. 2012; 39 Suppl 12: 6–27. 10.1111/j.1600-051X.2011.01830.x [DOI] [PubMed] [Google Scholar]
- 116. Noordzij M, Dekker FW, Zoccali C, Jager KJ. Sample size calculations. Nephron Clin Pract. 2011; 118: c319–c323. 10.1159/000322830 [DOI] [PubMed] [Google Scholar]
- 117. Werner MU. Sample size and effect size calculations are necessary in clinical studies in order to avoid false positive and false negative conclusions. Scand J Pain. 2013; 4: 163–164. [DOI] [PubMed] [Google Scholar]
- 118. Friston KJ, Holmes AP, Worsley KJ. How many subjects constitute a study? Neuroimage. 1999; 10: 1–5. [DOI] [PubMed] [Google Scholar]
- 119. Ioannidis JP. Why most published research findings are false. PLoS Med. 2005; 2: e124 04-PLME-E-0321R2 [pii]; 10.1371/journal.pmed.0020124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Walk D, Sehgal N, Moeller-Bertram T, Edwards RR, Wasan A, Wallace M et al. Quantitative sensory testing and mapping: a review of nonautomated quantitative methods for examination of the patient with neuropathic pain. Clin J Pain. 2009; 25: 632–640. 10.1097/AJP.0b013e3181a68c64 [DOI] [PubMed] [Google Scholar]
- 121. Backonja MM, Walk D, Edwards RR, Sehgal N, Moeller-Bertram T, Wasan A et al. Quantitative sensory testing in measurement of neuropathic pain phenomena and other sensory abnormalities. Clin J Pain. 2009; 25: 641–647. 10.1097/AJP.0b013e3181a68c7e [DOI] [PubMed] [Google Scholar]
- 122. Rolke R, Baron R, Maier C, Tolle TR, Treede RD, Beyer A et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain. 2006; 123: 231–243. [DOI] [PubMed] [Google Scholar]
- 123. Geber C, Klein T, Azad S, Birklein F, Gierthmuhlen J, Huge V et al. Test-retest and interobserver reliability of quantitative sensory testing according to the protocol of the German Research Network on Neuropathic Pain (DFNS): a multi-centre study. Pain. 2011; 152: 548–556. 10.1016/j.pain.2010.11.013 [DOI] [PubMed] [Google Scholar]
- 124. Maier C, Baron R, Tolle TR, Binder A, Birbaumer N, Birklein F et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): somatosensory abnormalities in 1236 patients with different neuropathic pain syndromes. Pain. 2010; 150: 439–450. 10.1016/j.pain.2010.05.002 [DOI] [PubMed] [Google Scholar]
- 125. Werner MU, Petersen MA, Bischoff JM Test-retest studies in quantitative sensory testing: a critical review. Acta Anaesthesiol Scand. 2013; 57: 957–963. 10.1111/aas.12150 [DOI] [PubMed] [Google Scholar]
- 126. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6: e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
All relevant data are included within the paper.