Abstract
The EGFR-targeted antibody cetuximab is effective against head and neck cancer (HNC), but in only 15 – 20% of patients, and the variability and extent of cetuximab-mediated cellular immunity is not fully understood. We hypothesized that regulatory T cells (Treg) may exert a functional and clinical impact on antitumor immunity in cetuximab-treated individuals. The frequency, immunosuppressive phenotype and activation status of Treg and NK cells were analyzed in the circulation and tumor microenvironment of cetuximab-treated HNC patients enrolled in a novel neoadjuvant, single-agent cetuximab clinical trial. Notably, cetuximab treatment increased the frequency of CD4+FOXP3+ intratumoral Treg expressing CTLA-4, CD39 and TGF-β. These Treg suppressed cetuximab-mediated ADCC and their presence correlated with poor clinical outcome in two prospective clinical trial cohorts. Cetuximab expanded CTLA-4+FOXP3+ Treg in vitro, in part by inducing DC maturation, in combination with TGF-β and TCR triggering. Importantly, cetuximab-activated NK cells selectively eliminated intratumoral Treg but preserved effector T cells. In ex vivo assays, ipilimumab targeted CTLA-4+ Treg and restored cytolytic functions of NK cells mediating ADCC. Taken together, our results argue that differences in Treg-mediated suppression contribute to the clinical response to cetuximab treatment, suggesting its improvement by adding ipilimumab or other strategies of Treg ablation to promote anti-tumor immunity.
Keywords: regulatory T cells, cetuximab, checkpoint receptors, tumor infiltrating lymphocytes
Introduction
Epidermal Growth Factor Receptor (EGFR)-specific therapy is moderately effective in the treatment of head and neck squamous cell cancer [HNC, refs.(1,2)]. EGFR-specific monoclonal antibodies (Ab) such as cetuximab enhance survival of HNC patients, while EGFR-specific tyrosine kinase inhibitors do not (3,4). However, the response rate for cetuximab therapy in HNC patients is low (15 ~ 20%). It has been proposed that cetuximab resistance is related to the activity of downstream EGFR-independent pathways (5), decreased EGFR internalization (6), genetic alterations of EGFR (7) or genotype of Fcγ receptor IIIa (CD16) on NK cells (8). This latter mechanism is based on accumulating evidence that cetuximab mediates Ab-dependent cellular cytotoxicity (ADCC) of NK cells (9), which can be augmented by cytokines (10–12). Furthermore, cetuximab can facilitate cross-talk between NK cells and dendritic cells (DC), which induces EGFR-specific cytotoxic T lymphocytes (CTL) (10,12) and/or activation of the complement system (13). Despite the various potential mechanisms of cetuximab activity, little is known about the effects of anti-EGFR mAb therapy on the cellular immune system in the tumor microenvironment (2). In addition, the cellular and molecular escape mechanisms negatively regulating ADCC or EGFR-specific CTL activity (12,14) have yet to be delineated.
The frequency of regulatory T cells (Treg) is increased at tumor sites and among the peripheral blood lymphocytes (PBL) of cancer patients (15–17), including those with HNC (18). The enrichment of Treg in tumor infiltrating lymphocytes (TIL) may promote cancer cell growth and the metastatic potential by suppressing antitumor immunity. Treg could also suppress NK cell responses through expression of suppressive cytokines and other tumor growth promoting effects (19). It is known that Treg can inhibit NKG2D expression, impairing NK cell cytotoxicity and DC maturation (20,21). However, whether Treg inhibit cetuximab-induced, NK cell-mediated ADCC or anti-tumor T cells in treated cancer patients is unknown, and the mechanism(s) and clinical implications of such Treg-mediated suppressive effects remain to be elucidated.
In this study, we investigated the effects of cetuximab therapy on the frequency of Treg in the peripheral circulation and in the tumor microenvironment of HNC patients, using freshly-isolated TIL from a prospective clinical trial of single-agent cetuximab-treated patients. We found that Treg suppress NK cell-mediated ADCC in a TGF-β1- dependent manner. The frequency of Treg was inversely associated with NK cell activation at the tumor sites and with the clinical course of the disease in cetuximab-treated patients. Interestingly, NK cells selectively eliminated intratumoral FOXP3+ Treg in the presence of ipilimumab ex vivo and thus decreased the Treg suppression of NK cells mediating cetuximab-driven ADCC. These results indicate that depletion of Treg by targeting CTLA-4 promotes antitumor immunity in the tumor microenvironment and enhances the efficacy of cetuximab therapy.
Materials and Methods
Patients and specimens
All patients were seen in the Outpatient Clinic of the Department of Otolaryngology at the University of Pittsburgh Medical Center, and all subjects signed an informed consent approved by the Institutional Review Board of the University of Pittsburgh (IRB #99-06). Peripheral venous blood samples were obtained from cetuximab-treated patients with previously untreated stage III/IV HNC, including 22 patients treated with cetuximab plus cisplatin/paclitaxel/radiotherapy followed by 6 months of maintenance single agent cetuximab (UPCI-05-003, NCT 00226239, ref. (22) and 18 patients receiving single-agent cetuximab on a separate prospective phase II clinical trial (UPCI #08-013, NCT 01218048, refs. (12,23), as described in Table 1. All analyses were conducted on protocol patients who were receiving single-agent cetuximab. Blood samples were obtained 1 – 7 days before cetuximab therapy and again after the conclusion of therapy (~1 month). The comparison (cetuximab-naïve) HNC cohorts were gender and age-matched, previously cetuximab-untreated patients with HNC. No patients were excluded as a result of prior treatments or performance status. Blood from cetuximab-naïve patients with HNC was drawn within the same period after completing therapy without cetuximab.
Table 1.
Demographics of the cetuximab-treated HNC patients in this study
| Regimen | No. of Patients | Tumor site (No. of patients) | Mean age | Male | Female |
|---|---|---|---|---|---|
| UPCI 08-013a | 18 | OC (8) OP (8) L (2) |
59.7 | 12 | 6 |
| UPCI 05-003b | 22 | OC (6) OP(7) L (3) HP (3) Other (3) |
60.0 | 13 | 9 |
Tumor site abbreviation: OC, oral cavity; OP, oropharynx; L, larynx; HP, hypopharynx
Cetuximab 250 mg/m2 weekly (after an initial dose of 400 mg/m2).
Cetuximab 250 mg/m2 days weekly (after an initial dose of 400 mg/m2), docetaxel 75 mg/m2 day 1, cisplatin 75 mg/m2 day 1, repeated every 21 days-3 cycles, then radiotherapy to 70 Gy (2 Gy/d) with concurrent cetuximab 250 mg/m2 weekly cisplatin 30 mg/m2, then maintenance cetuximab for 6 months. Blood was drawn during single-agent cetuximab maintenance.
Collection and processing of PBMC and TIL
Blood samples from cancer patients and healthy donors (40mL) were drawn into heparinized tubes and centrifuged on Ficoll-Hypaque gradients (GE Healthcare Bioscience). Peripheral blood lymphocytes (PBL) were recovered, washed in RPMI-1640 or AIM-V medium (Invitrogen) and immediately used for experiments. For TIL isolation, tumor tissues obtained from HNC patients undergoing surgery were collected, placed in sterile medium and delivered to the laboratory for processing. Tumor tissues were sliced into small pieces, which then were transferred to a cell strainer (70 μm nylon) and mechanically minced using a syringe plunger. No enzymes were used for TIL recovery. The cells which passed through the cell strainer were collected and subjected to Ficoll-Hypaque gradient centrifugation. Mononuclear cells were recovered and used for ADCC assays or were stored at −80 °C for l FACS analysis. For pre- and post-cetuximab treatment, PBMC and TIL were isolated from HNC patients before and after therapy, according to the protocol for the UPCI #08-013 trial.
Cell isolation
CD4+CD25+ T cells and CD3−CD56+ NK cells were isolated from freshly-obtained PBMC by immunomagnetic sorting (Miltenyi, Germany) or by using a human NK cell Enrichment Kit (STEM Cell Technology), respectively, following the manufacturers’ instructions. Cell separation was performed using an AutoMACS (for Treg isolation) and EasySep magnet (for NK cell isolation) according to the manufacturer’s protocol. Flow-bases cell sorting was used to isolate NK cells from TIL. Viability of separated cells was measured using trypan blue dye.
Monoclonal antibodies and flow cytometry
The mAb used to stain human cells included CD39-FITC/PC7, FOXP3-FITC, FOXP3 PerCP-Cy5.5(clone PCH101, eBioscience, San Diego, CA), LAP-PE, PD-1-APC (eBioscience, San Diego, CA), CD14-ECD, CD4-PC5 (all Beckman Coulter, CA), CD73-PE, CTLA-4-PE, TIM-3-Brillian violet 421, CD107a-PE, CD137-Percp cy5.5, CD25-PE-Cy7, Granzyme B-FITC, Perforin-APC, CD39-APC, CD16-PE-Cy7 (Biolegend, San Diego, CA), CD25-PE (Miltenyi, Auburn, CA), LAG-3-ATTO647N conjugate (Enzo Life Sciences), CD56-PE-Texas Red, CD3-Alexa Fluor 405 conjugate (Invitrogen, Grand Island, NY) and CD4-AF700 (BD Biosciences, San Diego, CA) and their respective isotype controls. All mAb preparations were pre-titrated using activated as well as non-activated PBMC to determine the optimal staining dilution for each. Intracellular staining for Foxp3, granzyme B, and perforin was performed as follows: PBMC or TIL were stained with mAb for surface markers and subsequently fixed and permeabilized (eBioscience). After washing, cells were subjected to intracellular staining for Foxp3, granzyme B, and perforin. Flow cytometry was performed using an EPICS XL-MCL flow cytometer equipped with Expo32 software, a CyAn flow cytometer (Dako, Ft. Collins, CO) or Fortesa (Becton Dickinson) machine; data were analyzed using Summit V4.3 software or the flowJo software (TreeStar, Inc.). The acquisition and analysis gates were restricted to the lymphocyte gate based on characteristic properties of the cells in the forward and side scatter. At least 1 × 105 events were acquired for analysis and, where applicable, gates were restricted to CD3+CD4+ for Treg analysis. Ipilimumab was obtained from Bristol Myers Squibb (Redwood City, CA).
Transwell culture
A HNSCC cell line (JHU029) and NK cells (1:1 ratio, 0.2 ×106 cells/well for each cell type) were co-cultured in the presence of cetuximab (10 μg/ml) or human IgG1 in a the upper chamber of a transwell plate (0.4 μm polyester membrane, 6.5 mm insert, 24 well plate, Costar, New York, NY USA). In the lower chamber, purified monocytes and CD4+ T cells (1:2 ratio, 0.2 ×106 cells/well for monocytes and 0.4 ×106 cells/well for CD4+ T cells labeled with CFSE) were incubated in the presence or absence of TGF-β1 (2.5 ng/ml) and/or anti-CD3 antibody (5μg/ml). These conditions were previously established by us as optimal for Treg generation (18). Four days later, CD4+ T cells in the lower chamber were harvested for analysis of expansion of CTLA-4+Foxp3+ Treg, and their proliferation assessed by CFSE dilution using flow cytometry. Four days after incubation, the frequency of CTLA-4+Foxp3+ Treg was assessed by flow cytometry using the PerCP-Cy5.5 dye. To confirm DC maturation, tumor cells, NK cell and cetuximab in the upper chamber were incubated with monocytes alone in the lower chamber for 48 hr. Monocytes were harvested for analysis of their status by flow cytometry.
ADCC assay
Cetuximab-mediated NK cell cytotoxicity (ADCC) was measured as previously described (23) with the following modifications. Briefly, K562 or PCI-13 target cells were incubated with 2uM carboxy fluorescein succinimidyl ester (CFSE, Invitrogen) for 10 min at 37 °C in the dark. Staining with CFSE was quenched with RPMI complete medium, and after two washes the CFSE-labeled target cells were incubated with PBMC or NK in the absence or presence of Treg at various NK cell to target ratios ranging from 1:1 to 10:1 for 3 h or 18 h at 37°C in a 5% CO2 atmosphere. The ratio of NK cells to Treg was 2:1 in this system. After incubation, 7-amino-actinomycin D (7-AAD, Invitrogen) (1 ug/ml) was used to measure cell death, and cells were acquired on a Beckman Coulter XL or Fortesa (Becton Dickinson) cytometer. Target cell death was determined by measuring percentage of 7-AAD+ cells by gating only on CFSE-positive target cells. Target cells in the absence of PBMC or NK cells were used as a negative control, and target cells were incubated for 10 min at 56°C as a positive control for cell death. To measure accurate cytotoxicity on a per cell basis, lytic units (LU) were defined as the number of NK cells required to kill 20% of 5 × 104 target cells and then the reciprocal number of this value per 105 NK cells was calculated. The percentage of cytotoxic activity was calculated using the following formula: % specific lysis = (7-AAD+ targets - spontaneous 7-AAD+ targets)/(Maximum lysis - spontaneous 7-AAD+ targets) X 100.
Statistical analysis
Averages were calculated as means. For non-parametric distribution of samples, p-values were calculated by Kruskal-Wallis and two-tailed exact Wilcoxon-Mann-Whitney tests or nonparametric paired test (Wilcoxon matched paired test). Disease specific survival of HNC patients was defined as the time elapsed from the first treatment with cetuximab until death from HNC. Patients were censored if they were alive at last follow-up or had died but were cancer-free at the time of death. For prognostic correlations, we utilized the Treg frequency of 6 %, which was the mean frequency previously found in untreated HNSCC patients (24), and analyzed the prognosis of those patients with Treg frequencies above or below this level. Treg subclasses were tested for association with disease free survival with the log rank test. p values < 0.05 were considered to be significant.
Results
Cetuximab-induced increase in circulating Treg correlates with clinical outcome in cetuximab-treated HNC patients
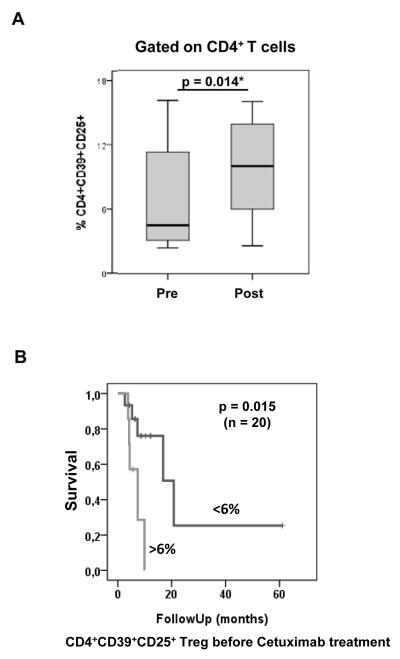
To investigate the effects of treatment with cetuximab on Treg in the circulation of HNC patients, the frequency of CD4+CD39+CD25hi Treg in PBL was analyzed before and after cetuximab therapy. Treg measurements were performed in previously untreated, stage III/IV HNC patients prior to receiving cetuximab-based chemoradiotherapy (CRT, UPCI #05-003), and compared with post-treatment Treg frequencies measured during single agent cetuximab maintenance therapy. As shown in Figure 1A, the frequency of CD4+CD39+CD25hiFoxp3+ Treg was found to be increased after cetuximab therapy (p=0.01). For prognostic correlations, we utilized Treg frequency of 6%, which was the mean frequency previously found in untreated HNSCC patients (24), and analyzed the prognosis of those patients with Treg frequencies above or below this level.
Figure 1. Cetuximab-based therapy increases CD4+CD25hi Treg in HNC patients’ peripheral blood.
(A) In 22 patients with HNC, the frequency of CD4+CD39+CD25+ Treg in peripheral blood (PBL) was compared before and after treatment (n=22). (B) Correlation of peripheral blood Treg frequencies in HNC patients (n=20) with clinical outcome. For prognostic correlations, we utilized the Treg frequency of 6 %, which was the mean frequency previously found in untreated HNSCC patients (24), and analyzed the prognosis of those patients with Treg frequencies above or below this level. The patients were divided into two groups (10 patients per group), one containing patients who had the Treg frequency < 6% and the other with the Treg frequency > 6%. The survival rate of these two groups were compared (median follow up=36 mo).
Given that Treg suppress NK-mediated ADCC, we hypothesized that the Treg frequency might predict clinical response to cetuximab therapy. Indeed, in a cohort of HNC patients (n=22) treated with cetuximab, significantly longer survival was observed in patients with lower Treg frequencies. We have previously established a mean ± SD value of 5.3 ± 3.2% for Treg in untreated patients with HNSCC and have now used the value of 6% to separate the patients into two groups. Patients with a Treg frequency lower than 6% fared significantly better than those with the Treg frequency higher than 6% (p=0.015, Figure 1B). Those cetuximab-treated patients with the elevated Treg frequency after cetuximab therapy appeared to have worse outcome. This result strongly supports our finding that the frequency of CD4+CD39+CD25hi Treg is a critical factor modulating the efficacy of cetuximab treatment in HNC cancer patients. Although these patients received CRT in conjunction with cetuximab, Treg measurements were performed at baseline (untreated) and during single agent cetuximab treatment, suggesting that the effect was cetuximab-specific, a finding which was validated in a separate patient cohort below.
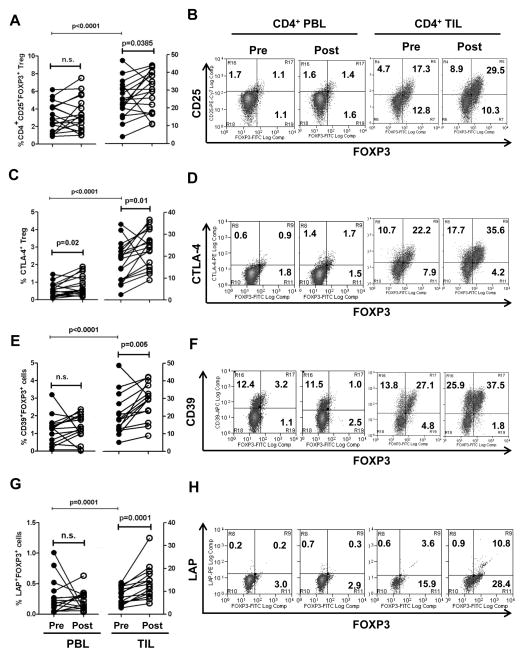
Frequency of intratumoral Treg and expression levels of CTLA-4, CD39, and TGF-β are increased after cetuximab monotherapy in HNC patients
To further document the cetuximab-specific effects on Treg, a second cohort of patients (n=18), who received only single agent neoadjuvant cetuximab in a second prospective phase II clinical trial (UPCI #08-013), was examined. As shown in Figure 2A, a highly significant and consistent enrichment of CD4+CD25hiFoxp3+ Treg was observed in TIL (p<0.0001) compared to PBL. The treatment of HNC patients with single-agent cetuximab for 4 weeks significantly increased the number of CD4+CD25hiFoxp3+ intratumoral Treg in these HNC patients as compared to baseline (pre-cetuximab) Treg levels. This result suggests that cetuximab monotherapy promotes Treg expansion in the tumor microenvironment, potentially contributing to immune suppression and impairing cetuximab-induced immunity (14).
Figure 2. Cetuximab monotherapy increases CD25+, CTLA-4+, CD39+, and LAP+ (membrane bound TGF-β+) cells mainly on intratumoral Foxp3+ Treg isolated from 18 HNC patients.
Flow cytometry analysis of circulating and intratumoral CD4+CD25hiFoxp3+ Treg isolated from a representative HNC patient treated with single-agent cetuximab therapy on a prospective phase II clinical trial (UPCI #08-013). PBL and TIL were respectively isolated from blood and tumors of HNC patients pre- and post-single-agent cetuximab therapy. Percentages of CD25+ (A), CTLA-4+ (C), CD39+(E), and LAP+ cells (G) in CD4+Foxp3+ Treg were compared pre- and post-single agent cetuximab therapy for a series of HNC patients. Representative flow cytometry analysis of CD25 (B), CTLA-4 (D), CD39 (F), and LAP (H) on Foxp3+ Treg of CD4+ PBL and TIL isolated from a HNC patient (pre- and post-cetuximab treatment). The numbers represent the percentages of CD25+, CTLA-4+, CD39+, and LAP+, and Foxp3+ cells in CD4+ T cells.
In order to characterize the immunosuppressive phenotype of Treg induced during cetuximab therapy, we analyzed expression of immunosuppressive molecules, including the immune checkpoint receptor, CTLA-4, as well as LAP (membrane bound TGF-β) and CD39 (an ectonucleotidase), present on the Treg surface. Effects of cetuximab monotherapy on expression of CTLA-4, TGF-β, and CD39 were assessed on paired PBL and TIL isolated prospectively from 18 HNC patients treated before and after 4 weeks of single-agent cetuximab therapy. As shown in Figure 2, cetuximab monotherapy significantly increased the frequency of CD4+Foxp3+ intratumoral Treg expressing CTLA-4, CD39, and TGF-β (p=0.002, p=0.005, and p=0.0001 respectively, Figure 2C, E, and H). Interestingly, a significant increase was only observed in circulating Treg expressing CTLA-4 (p=0.02, Figure 2C). We also observed that cetuximab monotherapy significantly increased the frequency of intratumoral CD4+Foxp3+ Treg expressing TIM-3 (p=0.0015). However, the frequency of CD4+Foxp3+ intratumoral Treg expressing PD-1 was not enhanced by cetuximab monotherapy. Although TIM-3+, PD-1+, and CD39+cells were also increased in Foxp3−CD4+ TIL by cetuximab monotherapy, CTLA-4+/CD39+ cells were significantly increased among the large fraction of CD4+Foxp3+ Treg from patients after cetuximab treatment, indicating that CTLA-4 and CD39 define a distinct subset of CD4+CD25hiFoxp3+ Treg enriched in the tumor microenvironment of cetuximab-treated patients.
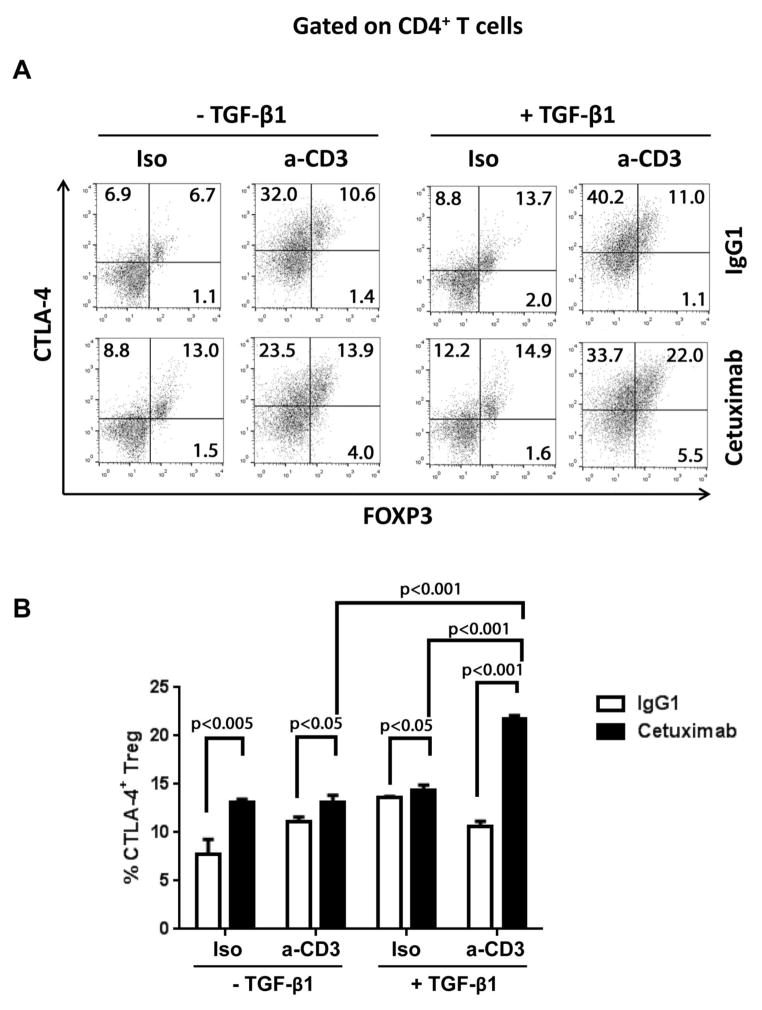
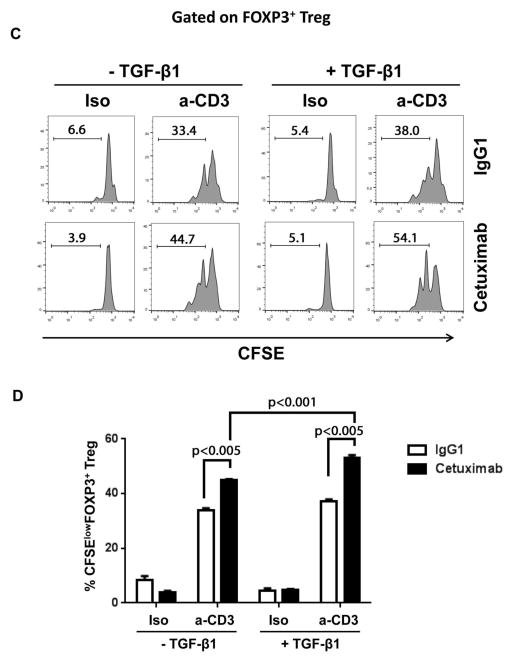
Cetuximab-induced DC maturation contributes to expansion of CTLA-4+ Treg in combination with TCR triggering
Several studies showed that in addition to cytokines such as TGF-β,. signaling mediated by TCR triggering and co-stimulation may be critical events that expand Treg in the tumor microenvironment (25–27). Based on these observations, and the previously reported capacity of cetuximab to promote DC maturation and CD8(+) T-cell priming through “NK-DC cross-talk” (12), we examined whether cetuximab therapy affects the TCR triggering and costimulation by analyzing the expression levels of HLA-DR, CD80 and CD86 on both intratumoral and peripheral blood HLA-DR+CD11c+ cells from these HNC patients. Indeed, DC activation/maturation markers were significantly upregulated on intratumoral HLA-DR+CD11c+ cells after cetuximab (not shown). Given that cetuximab-activated NK cells promote DC maturation (12), and that TGF-β is highly expressed in the tumor microenvironment, cetuximab therapy may promote the expansion of intratumoral Treg.
To recapitulate the intratumoral Treg expansion observed in cetuximab-treated patients, we investigated whether the presence of cetuximab increased the frequency of CTLA-4+ Treg using a transwell plate-based ex vivo system. As shown in Figure 3 A and B, the frequency of CTLA-4+ Treg was increased in the setting of TCR stimulation using agonistic, plate-bound anti-CD3 mAb, compared to isotype control control mAb (p<0.05, p<0.005, and p<0.001 respectively) in the presence or absence of TGF-β. This result was only observed in the presence of cetuximab but not human IgG1 mAb. Under anti-CD3 stimulatory condition, cetuximab treatment significantly increase the frequency of CTLA-4+ Treg in the presence of TGF-β, compared to the absence of it (p<0.001). Taken together, these results indicate that the treatment with cetuximab can significantly increase the frequency of CTLA-4+ Treg, which is further expanded in the presence of TCR triggering.
Figure 3. Treatment with cetuximab combined with TCR triggering induces CTLA-4+ Treg expansion.
JHU029 cell line and NK cells (1:1 ratio) were co-cultured in the presence of cetuximab or human IgG1 at the upper chamber of transwell plate while at the lower chamber, purified monocytes and CFSE-labeled CD4+ T cells (1:2 ratio) were cultured with TGF-β1 in the presence or absence of anti-CD3 antibody. Similar results were seen of lower magnitude when TGF-β1 was omitted from the cultures. Four days after incubation, the frequency (A and B) and proliferation (C and D) of CTLA-4+Foxp3+ Treg was assessed by flow cytometry using the PerCP-Cy5.5 dye. Representative flow cytometry analysis of CTLA-4+Foxp3+ Treg (A) and their proliferation by CFSE dilution (C) are shown for each condition and their frequency was statistically compared, respectively (B and D).
We also investigated whether incubation with cetuximab induce proliferation of Foxp3+ Treg in the presence of TGF-β1 and/or anti-CD3 antibody by using a CFSE dilution-based assay and flow cytometry to measure the frequency of CTLA-4+FOXP3+ Treg. The presence of cetuximab significantly enhanced proliferation of Foxp3+ Treg under anti-CD3 Ab stimulatory conditions, compared to human IgG1 control mAb in the presence and absence of TGF-β (Figure 3 C and D, p<0.005). Under stimulation with anti-CD3 Ab, cetuximab treatment significantly expanded Foxp3+ Treg by TGF-β, compared to absence of it (p<0.001). This result is consistent with our previous report showing that cetuximab-activated NK cells induce DC maturation (12), which may provide antigen stimulation and co-stimulatory signals to preferentially expand Treg in the tumor microenvironment, where other suppressive signals exist (i.e., TGF-β1).
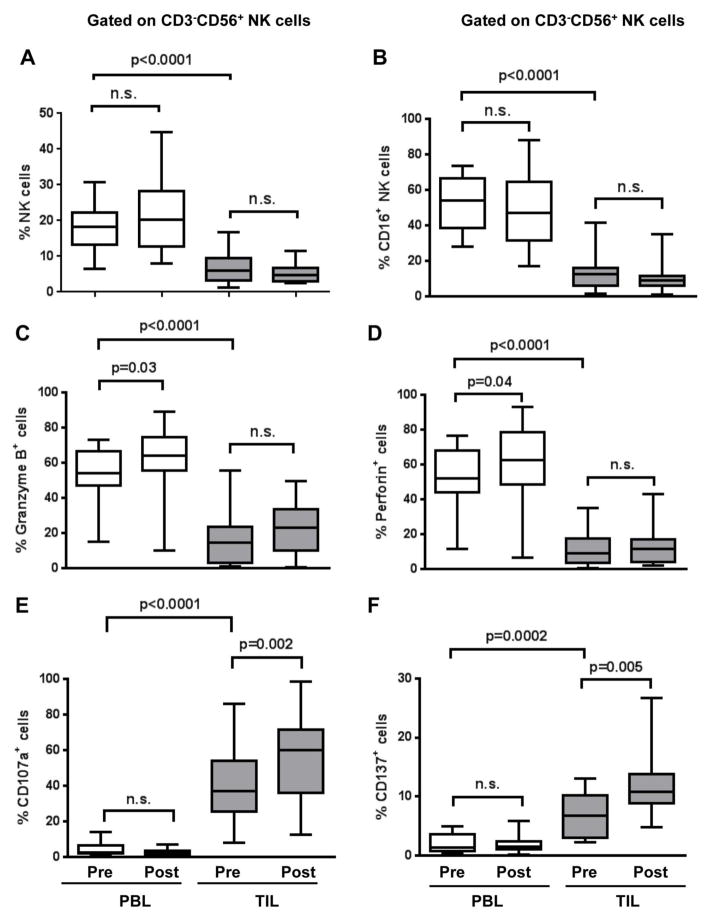
Cetuximab monotherapy differentially activates both circulating and intratumoral NK cells in HNC patients and their functional phenotypes are associated with the frequency of Treg
Previously we showed that cetuximab-mediated ADCC activity of NK cells was dependent on CD16 (FcγRIIIa) (8). However, this in vitro result has not yet been validated real-time in vivo in cetuximab-treated HNC patients, particularly in TIL freshly isolated from single-agent cetuximab treated patients. In order to examine whether cetuximab therapy activated NK cells in these patients, we examined granzyme B and perforin expression reflecting cytotoxic activity, and CD107a, CD137, and CD16 expression as measures of activation status, in both circulating and intratumoral NK cells. As shown in Figure 4 A, although the frequency of NK cells did not change in the PBL or TIL compartment during the therapy, the frequency of circulating NK cells was significantly higher than that of intratumoral NK cells. Similarly, the frequency of CD16+ NK cells also did not change during the cetuximab therapy on either circulating or intratumoral NK cells, albeit the frequency of circulating NK cells was notably higher than that of intratumoral NK cells (Figure 4B, p<0.0001). Interestingly, cetuximab therapy significantly upregulated granzyme B+ and perforin+ cells in circulating NK cells (p=0.03 and p=0.04 respectively, Figure 4C and D) while notably upregulating CD107a+ and CD137+ cells on intratumoral NK cells (p=0.002 and p=0.005, respectively, Figure 4E and F). The frequency of CD107a and CD137 positivity was substantially higher on intratumoral NK cells compared with those of circulating NK cells (p<0.0001, p=0.0002 respectively). The frequency of granzyme B+/perforin+ NK cells was significantly higher in PBL compared to tumor infiltrating NK cells p<0.0001), suggesting that a suppressive mechanism may inhibit full cetuximab-mediated NK cell activation in the tumor microenvironment.
Figure 4. Cetuximab monotherapy differentially activates circulating and intratumoral NK cells.
PBL and TIL were isolated from HNC patients before and after single-agent cetuximab therapy to analyze CD3−CD56+ NK cells for their cytolytic activity-related molecules (granzyme B, perforin, and CD16), degranulation marker (CD107a), and activation molecule (CD137). Percentages of CD3−CD56+ NK cells (A), CD16+(B), granzyme B+(C), perforin+(D), CD107a+(E), CD137+ cells (F) of circulating and intratumoral CD3−CD56+ NK cells were compared in pre- and post-single-agent cetuximab therapy for HNC patients (n=17).
To determine whether Treg inhibit cetuximab-induced, NK cell-mediated ADCC in vivo, potentially facilitating tumor progression, we correlated the frequency of Treg with functional and phenotypic markers of activated NK cells in the tumor microenvironment. Indeed, CD4+CD25hiFoxp3+ Treg were 7.4 times more enriched in TIL than in PBL. In the presence of these enriched Treg, intratumoral NK cells manifested significantly impaired expression of ADCC-related functional molecules, including granzyme B, perforin, and CD16 compared to those of circulating NK cells. Indeed, significantly lower expression of granzyme B, perforin, and CD16 on intratumoral NK cells was observed. In contrast, in PBL, which had a low frequency of Treg, NK cells maintained intact expression of these cytolytic molecules (not shown). Thus, a strong inverse correlation exists between the frequency of Treg and functional impairment of NK cells in the tumor microenvironment.
Based on the association of a high Treg frequency with the impaired NK cell functional phenotype, we tested whether HNC patient Treg could directly suppress cetuximab-mediated, NK cell-induced ADCC. To this end, we investigated the effect of CD4+CD25hiFoxp3+ Treg on cetuximab-mediated ADCC ex vivo, finding that, indeed, Treg significantly suppressed cetuximab-mediated cytotoxicity (p=0.002). This effect was mainly mediated by Treg-derived TGF-β1, since the suppression was significantly abrogated using a neutralizing Ab specific for TGF-β1 (p=0.01). IL-10 appeared to play a minor role, as little inhibition of cetuximab-mediated ADCC mediated by Treg was observed after blockade of IL-10 alone (28). Taken together, this result indicates that Treg inhibit cetuximab-induced TIL NK cell-mediated cytotoxicity through TGF-β1 secretion.
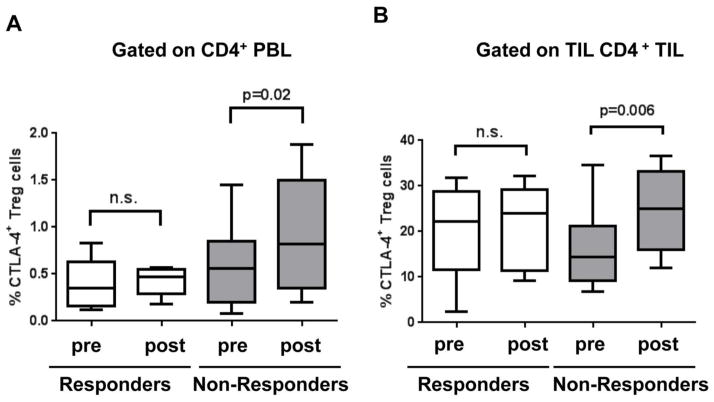
Treg are associated with clinical response to monotherapy with cetuximab
To further assess the clinical impact of Treg in predicting response in an independent clinical trial of patients after cetuximab therapy, we compared the extent of Treg induction in objective clinical responders (using post-treatment CT scan) with clinical non-responders. During cetuximab therapy, we found that clinical responders maintain stable levels of circulating and intratumoral CTLA-4+ Treg (Figure 5). On the contrary, the frequency of CTLA-4+ Treg were significantly increased among the non-responder patients’ PBL (p=0.02) and TIL (p=0.006), indicating that the induction of Tregs negatively impacts on the efficacy of cetuximab therapy, and that selected targets such as CTLA-4 which deplete Treg would potentially provide additional therapeutic benefit.
Figure 5. Cetuximab monotherapy increases the frequency of CTLA-4+ Treg only in non-responder group.
The frequency of CTLA-4+ Treg in CD4+ PBL (A) and TIL (B) was measured using flow cytometry, and compared in pre- and post-single-agent cetuximab monotherapy for 5 responders and 13 non-responders respectively.
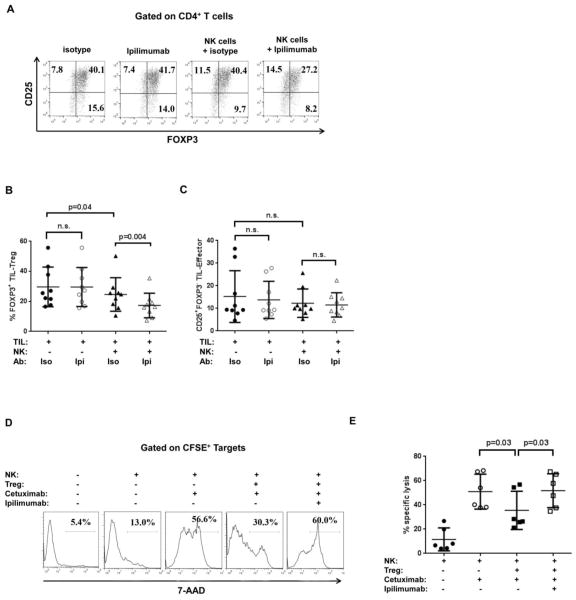
Treatment with ipilimumab enhances cetuximab-mediated ADCC by eliminating intratumoral Treg
We postulated that selective elimination of CTLA-4+ Treg, particularly at the tumor site, might improve the antitumor immunity followed by cetuximab therapy. Recent preclinical studies also showed that anti-CTLA-4 mAb induced rapid elimination of intratumoral Treg in murine tumor models, which improve anti-tumor immunity (29,30). However, similar results have not been reported using ipilimumab (anti-CTLA-4 mAb) in humans. Because ipilimumab is a human IgG1 isotype mAb, which like cetuximab has been shown to induce NK cell-mediated ADCC (8,31), we investigated whether ipilimumab could eliminate intratumoral CTLA-4+ Treg in the presence of NK cells. To test this possibility, we freshly isolated TIL containing Treg from a series of HNC tumors (n=6) and incubated them with ipilimumab in the absence or presence of NK cells. After 72 hr incubation, the frequency of Foxp3+ intratumoral Treg in CD4+ TIL was evaluated using a flow cytometry-based cytotoxicity assay. As shown in Figure 6A-B, the addition of ipilimumab together with exogenous NK cells significantly reduced (~40%) the proportion of Foxp3+ Treg in CD4+ TIL. Exogenous NK cells slightly reduced the frequency of TIL Treg even in the absence of ipilimumab compared to TIL control conditions without NK cells, indicating that circulating NK cells can also deplete TIL Treg in an ipilimumab-independent manner (p=0.04, Figure 6B). However, NK cells plus ipilimumab did not deplete effector CD4+TIL (CD25+Foxp3− cells) in the presence or absence of ipilimumab, confirming that NK cells selectively deplete Foxp3+ TIL Treg while they preserve effector T cells in TIL (Figure 6C). We also tested whether myeloid cells can eliminate intratumoral Treg in the presence of ipilimumab. In contrast to NK cells, however, myeloid cells did not deplete either intratumoral Treg either effector cells (not shown), indicating that the presence of myeloid cells may be dispensable for Treg elimination mediated by ipilimumab.
Figure 6. Treatment with ipilimumab enhances cetuximab-mediated ADCC by eliminating Treg.
Ipilimumab was added into TIL cultures in the absence or presence of NK cells (The ratio of NK to TIL was 2:1). 3 days after incubation, gates were set to include CD4+ TIL to analyze the frequency of Foxp3+ Treg. (A) Representative FACS dot plot for the frequency of Foxp3+ Treg in CD4+ TIL. The frequency of Foxp3+ TIL Treg (B) or CD25+Foxp3− TIL effector (C) in each condition was compared by analyzing CD4+ TIL of 9 HNC patients. Ipi and Iso represent ipilimumab and isotype respectively. (D) Representative flow cytometry analysis assessing the effect of ipilimumab on cetuximab-mediated ADCC in the presence of intratumoral Treg. Target HNC cells (JHU029) labeled with CFSE were incubated with peipheral NK cells in the absence or presence of intratumoral Treg (NK: JHU029 target:Treg ratio is 10:1:5). Cetuximab and/or ipilimumab were added into the co-culture as indicated. After 18 hrs, gates were set to include only CFSE-labeled target cells to analyze cell death assessed by 7-AAD staining. (E) The effect of ipilimumab on cetuximab-/NK cell-mediated ADCC were tested in the presence of intratumoral Treg isolated from HNC patients (n=6). Specific lysis was calculated as described in the Methods section.
Next, we postulated that Treg depletion using ipilimumab-mediated NK cell cytotoxicity could overcome the suppressive activity of Treg against NK cell-mediated HNC cell lysis induced by cetuximab. To test this hypothesis, we added ipilimumab or irrelevant isotype control mAb to the cetuximab-mediated ADCC assay system, with co-cultured NK and Treg (as described in Figure 5). As shown in Figure 6D and E, the cytolytic activity of NK cells previously suppressed by intratumoral Treg was recovered after incubation with ipilimumab (p=0.03). This result indicates that ipilimumab could reverse the suppressive activity and eliminate intratumoral CTLA-4+ Treg in the presence of NK cells, thus potentially enhancing cetuximab-mediated ADCC activity.
Discussion
In this report, we describe the unexpected finding that cetuximab-based therapy is associated with an increase in CTLA-4+Foxp3+ Treg in the circulation and in the microenvironment in treated HNC patients from two independent clinical trial cohorts. Indeed, higher levels of Treg correlated with worse prognosis in cetuximab treated HNC patients, as recently seen in lung cancer after neoadjuvant chemotherapy (32). For the first time, we also show that intratumoral NK cell activation and cytotoxicity occurs during cetuximab therapy, which is primarily inhibited by Treg-derived TGF-β1, providing a mechanism for their suppressive effect and impact on clinical course of the disease. Furthermore, we demonstrated that NK cells can selectively eliminate intratumoral Treg in the presence of ipilimumab, which induces recovery of cetuximab-ADCC activity from Treg suppression. Importantly, the suppressive effect of these Treg could be substantially abrogated by ipilimumab-mediated NK cell elimination of Treg, a strategy which has the potential to enhance cetuximab treated patient outcomes.
Although Treg are known to be enriched in the tumor microenvironment compared to peripheral blood, the mechanism underlying Treg enrichment at the tumor site has not been well elucidated. A recent study showed that a few dominant Treg clones recruited into tumor sites were dramatically expanded through T cell receptor (TCR) responses in the microenvironment (33). However, little information is available regarding their biological and clinical impact on mAb-induced immunity and tolerance in TME after mAb therapy. We previously proposed that cetuximab induces not only ADCC of NK cells (8,31) but also cross-talk between NK cells and DC, leading to generation of tumor antigen (TA)-specific T cells responses (14). Recently, we reported that cetuximab stimulated IFN-γ production from NK cells in vitro and subsequently induced DC maturation and enhanced the generation of TA-specific CD8+ T cells (12). Because TGF-β1, a critical factor for Treg generation, is abundant in the TME, this unique environment in conjunction with TCR triggering for Treg expansion could be promoted by cetuximab therapy in cancer patients’ tumor sites.
Treg are reported to express immune checkpoint receptors and suppressive molecules, which are involved in generation and function of Treg. In this study, we demonstrated that single-agent cetuximab therapy significantly increased not only the frequency of intratumoral Foxp3+CD25hi Treg but also their expression of CTLA-4, TIM-3, CD39, and TGF-β/LAP. Of particular interest is the expression of CTLA-4 and CD39 that are detected on the majority of intratumoral Treg, which is further upregulated by cetuximab treatment. Many studies define CTLA-4 as an effector receptor in mediating Treg suppressive functions (34). For example, Foxp3+ Treg-specific loss of CTLA-4 is sufficient to induce fatal lymphoproliferative disease, which is reminiscent of findings observed in CTLA-4-deficient mice (35). It has been reported that Treg can induce indoleamine 2,3-dioxygenase (IDO) activity in APCs through CTLA-4 and CD80/CD86 interaction. IDO catabolizes tryptophan, which locally depletes tryptophan and subsequently inhibits proliferation of T lymphocytes. In addition, IDO is involved in inhibiting NK cell function by inhibiting activating receptors and cytolytic activity (36). Similarly, it has been suggested that antibody-triggering of CTLA-4 can induce the release of TGFβ1 from Treg (37). However, the link between CTLA-4 and IDO/TGFβ1 currently remains controversial, albeit their critical roles in Treg-mediated immune suppressive activities (34). Based on the observation showing that CD39 specific blocking mAb attenuated immunosuppressive function of Treg and subsequently restored CD4 and CD8 T cells (38), it was proposed that blockade of CD39 could also restore NK cell-mediated antitumor immunity (39). Taken together, these results suggest that blockade of CTLA-4 or CD39 enzymatic activity is an attractive target to inhibit immunosuppressive functions of Treg in the tumor microenvironment, thus enhancing the efficacy of cetuximab immunotherapy against HNC. Treg from HNC patients potently suppress cetuximab-mediated ADCC in vitro, and correlate directly with phenotypic and functional impairment in tumor infiltrating NK cells from cetuximab treated patients, pointing to infiltrating Treg as the primary suppressive culprit responsible for impairment of cetuximab-mediated NK cell activation and tumor cell lysis. This finding was consistently reported from non-small cell lung cancer (NSCLC) patients showing that Treg potently inhibit NK-mediated and cetuximab-induced ADCC in vitro. (32). TGF-β1 is a critical factor not only to induce Treg but also to suppress NK cell functions, such as ADCC and cytokine production by downregulating FcγRIIIa, CD16. It has been well established that cetuximab induces ADCC against different cancer cell lines including HNC (9,41,42). In addition, several lines of evidence have consistently shown that intratumoral NK cells possess more severe dysfunctional phenotypes than circulating NK cells; this difference may be mediated via several mechanisms (43–45). Another study showed that TGF-β1 impaired CD16-mediated human NK cell ADCC by inhibiting granzyme A and B expression and IFN-g production via SMAD3 (46). Furthermore, it has been reported that TGF-β1 downregulated CD16 expression on peripheral blood NK cells (47), which parallels the impairment of cetuximab-mediated ADCC in the patients with esophageal squamous cell carcinoma (ESCC) (48). CD107a and CD137 on intratumoral NK cells were significantly upregulated compared to those on circulating NK cells, indicating that NK cells were actively stimulated, presumably due to the presence of the targets at the tumor sites. The low level of granzyme B and perforin in intratumoral NK cells may also reflect on theses NK cell phenotypes following their activation at the tumor site. In particular, CD107a and CD137 on intratumoral NK cells were further upregulated during cetuximab therapy, strongly suggesting that cetuximab-mediated ADCC take place at the tumor site. These results collectively support our observation showing that Treg suppress cetuximab-mediated ADCC of NK cells through TGF-β1 and might serve as a potential novel biomarker to predict the efficacy of cetuximab therapy in treating head and neck cancer patients.
Recently, two preclinical studies using mouse models showed that anti-CTLA-4 mAb eliminated intratumoral Treg in a FcγR- dependent manner (29,30). Despite the existence of NK cells, macrophages, and DC in TIL, addition of ipilimumab alone into the TIL culture did not reduce the frequency of intratumoral Treg. This result indicates that these intratumoral NK cells are not sufficiently numerous or functionally capable of eliminating TIL-Treg in the presence of ipilimumab, which may be due to their impaired cytolytic molecules such as granzyme B, perforin and/or CD16 expression. Based on our observation that peripheral NK cells are relatively more cytolytic than intratumoral NK cells and able to eliminate TIL-Treg in the presence of ipilimumab, their directed migration into tumor sites may be essential to eliminate intratumoral Treg, thus enhancing the efficacy of cetuximab in the treatment of HNC patients.
Acknowledgments
Grant Support
This work was supported by National Institute of Health grants R01 DE19727, P50 CA097190, CA110249, and University of Pittsburgh Cancer Institute grant P30CA047904.
We acknowledge excellent technical assistance from Clayton Mathis, Michael Meyer, and Bratislav Janjic, University of Pittsburgh Cancer Institute. We thank Ferris lab members for helpful suggestions.
References
- 1.Argiris A, Heron DE, Smith RP, Kim S, Gibson MK, Lai SY, et al. Induction docetaxel, cisplatin, and cetuximab followed by concurrent radiotherapy, cisplatin, and cetuximab and maintenance cetuximab in patients with locally advanced head and neck cancer. J Clin Oncol. 2010;28(36):5294–300. doi: 10.1200/JCO.2010.30.6423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferris RL, Jaffee EM, Ferrone S. Tumor antigen-targeted, monoclonal antibody-based immunotherapy: clinical response, cellular immunity, and immunoescape. J Clin Oncol. 2010;28(28):4390–9. doi: 10.1200/JCO.2009.27.6360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB, et al. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med. 2006;354(6):567–78. doi: 10.1056/NEJMoa053422. [DOI] [PubMed] [Google Scholar]
- 4.Stewart JS, Cohen EE, Licitra L, Van Herpen CM, Khorprasert C, Soulieres D, et al. Phase III study of gefitinib compared with intravenous methotrexate for recurrent squamous cell carcinoma of the head and neck [corrected] J Clin Oncol. 2009;27(11):1864–71. doi: 10.1200/JCO.2008.17.0530. [DOI] [PubMed] [Google Scholar]
- 5.Bardelli A, Siena S. Molecular mechanisms of resistance to cetuximab and panitumumab in colorectal cancer. J Clin Oncol. 2010;28(7):1254–61. doi: 10.1200/JCO.2009.24.6116. [DOI] [PubMed] [Google Scholar]
- 6.Wheeler DL, Huang S, Kruser TJ, Nechrebecki MM, Armstrong EA, Benavente S, et al. Mechanisms of acquired resistance to cetuximab: role of HER (ErbB) family members. Oncogene. 2008;27(28):3944–56. doi: 10.1038/onc.2008.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bardelli A, Janne PA. The road to resistance: EGFR mutation and cetuximab. Nature medicine. 2012;18(2):199–200. doi: 10.1038/nm.2646. [DOI] [PubMed] [Google Scholar]
- 8.Lopez-Albaitero A, Lee SC, Morgan S, Grandis JR, Gooding WE, Ferrone S, et al. Role of polymorphic Fc gamma receptor IIIa and EGFR expression level in cetuximab mediated, NK cell dependent in vitro cytotoxicity of head and neck squamous cell carcinoma cells. Cancer immunology, immunotherapy: CII. 2009;58(11):1853–64. doi: 10.1007/s00262-009-0697-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pahl JH, Ruslan SE, Buddingh EP, Santos SJ, Szuhai K, Serra M, et al. Anti-EGFR antibody cetuximab enhances the cytolytic activity of natural killer cells toward osteosarcoma. Clinical cancer research: an official journal of the American Association for Cancer Research. 2012;18(2):432–41. doi: 10.1158/1078-0432.CCR-11-2277. [DOI] [PubMed] [Google Scholar]
- 10.Lee J, Moon C. Current status of experimental therapeutics for head and neck cancer. Experimental biology and medicine. 2011;236(4):375–89. doi: 10.1258/ebm.2010.010354. [DOI] [PubMed] [Google Scholar]
- 11.Roberti MP, Barrio MM, Bravo AI, Rocca YS, Arriaga JM, Bianchini M, et al. IL-15 and IL-2 increase Cetuximab-mediated cellular cytotoxicity against triple negative breast cancer cell lines expressing EGFR. Breast cancer research and treatment. 2011;130(2):465–75. doi: 10.1007/s10549-011-1360-2. [DOI] [PubMed] [Google Scholar]
- 12.Srivastava RM, Lee SC, Andrade Filho PA, Lord CA, Jie HB, Davidson HC, et al. Cetuximab-activated natural killer and dendritic cells collaborate to trigger tumor antigen-specific T-cell immunity in head and neck cancer patients. Clinical cancer research: an official journal of the American Association for Cancer Research. 2013;19(7):1858–72. doi: 10.1158/1078-0432.CCR-12-2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hsu YF, Ajona D, Corrales L, Lopez-Picazo JM, Gurpide A, Montuenga LM, et al. Complement activation mediates cetuximab inhibition of non-small cell lung cancer tumor growth in vivo. Molecular cancer. 2010;9:139. doi: 10.1186/1476-4598-9-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SC, Srivastava RM, Lopez-Albaitero A, Ferrone S, Ferris RL. Natural killer (NK): dendritic cell (DC) cross talk induced by therapeutic monoclonal antibody triggers tumor antigen-specific T cell immunity. Immunologic research. 2011;50(2–3):248–54. doi: 10.1007/s12026-011-8231-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hiraoka N, Onozato K, Kosuge T, Hirohashi S. Prevalence of FOXP3+ regulatory T cells increases during the progression of pancreatic ductal adenocarcinoma and its premalignant lesions. Clinical cancer research: an official journal of the American Association for Cancer Research. 2006;12(18):5423–34. doi: 10.1158/1078-0432.CCR-06-0369. [DOI] [PubMed] [Google Scholar]
- 16.Ichihara F, Kono K, Takahashi A, Kawaida H, Sugai H, Fujii H. Increased populations of regulatory T cells in peripheral blood and tumor-infiltrating lymphocytes in patients with gastric and esophageal cancers. Clinical cancer research: an official journal of the American Association for Cancer Research. 2003;9(12):4404–8. [PubMed] [Google Scholar]
- 17.Schaefer C, Kim GG, Albers A, Hoermann K, Myers EN, Whiteside TL. Characteristics of CD4+CD25+ regulatory T cells in the peripheral circulation of patients with head and neck cancer. British journal of cancer. 2005;92(5):913–20. doi: 10.1038/sj.bjc.6602407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jie HB, Gildener-Leapman N, Li J, Srivastava RM, Gibson SP, Whiteside TL, et al. Intratumoral regulatory T cells upregulate immunosuppressive molecules in head and neck cancer patients. British journal of cancer. 2013;109(10):2629–35. doi: 10.1038/bjc.2013.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghiringhelli F, Menard C, Terme M, Flament C, Taieb J, Chaput N, et al. CD4+CD25+ regulatory T cells inhibit natural killer cell functions in a transforming growth factor-beta-dependent manner. The Journal of experimental medicine. 2005;202(8):1075–85. doi: 10.1084/jem.20051511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smyth MJ, Teng MW, Swann J, Kyparissoudis K, Godfrey DI, Hayakawa Y. CD4+CD25+ T regulatory cells suppress NK cell-mediated immunotherapy of cancer. Journal of immunology. 2006;176(3):1582–7. doi: 10.4049/jimmunol.176.3.1582. [DOI] [PubMed] [Google Scholar]
- 21.Terme M, Chaput N, Combadiere B, Ma A, Ohteki T, Zitvogel L. Regulatory T cells control dendritic cell/NK cell cross-talk in lymph nodes at the steady state by inhibiting CD4+ self-reactive T cells. Journal of immunology. 2008;180(7):4679–86. doi: 10.4049/jimmunol.180.7.4679. [DOI] [PubMed] [Google Scholar]
- 22.Argiris A, Heron DE, Smith RP, Kim S, Gibson MK, Lai SY, et al. Induction docetaxel, cisplatin, and cetuximab followed by concurrent radiotherapy, cisplatin, and cetuximab and maintenance cetuximab in patients with locally advanced head and neck cancer. J Clin Oncol. 2010;28(36):5294–300. doi: 10.1200/JCO.2010.30.6423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim GG, Donnenberg VS, Donnenberg AD, Gooding W, Whiteside TL. A novel multiparametric flow cytometry-based cytotoxicity assay simultaneously immunophenotypes effector cells: comparisons to a 4 h 51Cr-release assay. Journal of immunological methods. 2007;325(1–2):51–66. doi: 10.1016/j.jim.2007.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schuler PJ, Harasymczuk M, Schilling B, Saze Z, Strauss L, Lang S, et al. Effects of adjuvant chemoradiotherapy on the frequency and function of regulatory T cells in patients with head and neck cancer. Clinical cancer research: an official journal of the American Association for Cancer Research. 2013;19(23):6585–96. doi: 10.1158/1078-0432.CCR-13-0900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karumuthil-Melethil S, Perez N, Li R, Prabhakar BS, Holterman MJ, Vasu C. Dendritic cell-directed CTLA-4 engagement during pancreatic beta cell antigen presentation delays type 1 diabetes. Journal of immunology. 2010;184(12):6695–708. doi: 10.4049/jimmunol.0903130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li R, Perez N, Karumuthil-Melethil S, Prabhakar BS, Holterman MJ, Vasu C. Enhanced engagement of CTLA-4 induces antigen-specific CD4+CD25+Foxp3+ and CD4+CD25- TGF-beta 1+ adaptive regulatory T cells. Journal of immunology. 2007;179(8):5191–203. doi: 10.4049/jimmunol.179.8.5191. [DOI] [PubMed] [Google Scholar]
- 27.Perez N, Karumuthil-Melethil S, Li R, Prabhakar BS, Holterman MJ, Vasu C. Preferential costimulation by CD80 results in IL-10-dependent TGF-beta1(+) -adaptive regulatory T cell generation. Journal of immunology. 2008;180(10):6566–76. doi: 10.4049/jimmunol.180.10.6566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strauss L, Bergmann C, Szczepanski M, Gooding W, Johnson JT, Whiteside TL. A unique subset of CD4+CD25highFoxp3+ T cells secreting interleukin-10 and transforming growth factor-beta1 mediates suppression in the tumor microenvironment. Clinical cancer research: an official journal of the American Association for Cancer Research. 2007;13(15 Pt 1):4345–54. doi: 10.1158/1078-0432.CCR-07-0472. [DOI] [PubMed] [Google Scholar]
- 29.Bulliard Y, Jolicoeur R, Windman M, Rue SM, Ettenberg S, Knee DA, et al. Activating Fc gamma receptors contribute to the antitumor activities of immunoregulatory receptor-targeting antibodies. The Journal of experimental medicine. 2013;210(9):1685–93. doi: 10.1084/jem.20130573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simpson TR, Li F, Montalvo-Ortiz W, Sepulveda MA, Bergerhoff K, Arce F, et al. Fc-dependent depletion of tumor-infiltrating regulatory T cells co-defines the efficacy of anti-CTLA-4 therapy against melanoma. The Journal of experimental medicine. 2013;210(9):1695–710. doi: 10.1084/jem.20130579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lopez-Albaitero A, Ferris RL. Immune activation by epidermal growth factor receptor specific monoclonal antibody therapy for head and neck cancer. Archives of otolaryngology--head & neck surgery. 2007;133(12):1277–81. doi: 10.1001/archotol.133.12.1277. [DOI] [PubMed] [Google Scholar]
- 32.Pircher A, Gamerith G, Amann A, Reinold S, Popper H, Gachter A, et al. Neoadjuvant chemo-immunotherapy modifies CD4(+)CD25(+) regulatory T cells (Treg) in non-small cell lung cancer (NSCLC) patients. Lung cancer. 2014;85(1):81–7. doi: 10.1016/j.lungcan.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Sainz-Perez A, Lim A, Lemercier B, Leclerc C. The T-cell receptor repertoire of tumor-infiltrating regulatory T lymphocytes is skewed toward public sequences. Cancer research. 2012;72(14):3557–69. doi: 10.1158/0008-5472.CAN-12-0277. [DOI] [PubMed] [Google Scholar]
- 34.Walker LS, Sansom DM. The emerging role of CTLA4 as a cell-extrinsic regulator of T cell responses. Nature reviews Immunology. 2011;11(12):852–63. doi: 10.1038/nri3108. [DOI] [PubMed] [Google Scholar]
- 35.Wing K, Onishi Y, Prieto-Martin P, Yamaguchi T, Miyara M, Fehervari Z, et al. CTLA-4 control over Foxp3+ regulatory T cell function. Science. 2008;322(5899):271–5. doi: 10.1126/science.1160062. [DOI] [PubMed] [Google Scholar]
- 36.Pietra G, Manzini C, Rivara S, Vitale M, Cantoni C, Petretto A, et al. Melanoma cells inhibit natural killer cell function by modulating the expression of activating receptors and cytolytic activity. Cancer research. 2012;72(6):1407–15. doi: 10.1158/0008-5472.CAN-11-2544. [DOI] [PubMed] [Google Scholar]
- 37.Oida T, Xu L, Weiner HL, Kitani A, Strober W. TGF-beta-mediated suppression by CD4+CD25+ T cells is facilitated by CTLA-4 signaling. Journal of immunology. 2006;177(4):2331–9. doi: 10.4049/jimmunol.177.4.2331. [DOI] [PubMed] [Google Scholar]
- 38.Nikolova M, Carriere M, Jenabian MA, Limou S, Younas M, Kok A, et al. CD39/adenosine pathway is involved in AIDS progression. PLoS pathogens. 2011;7(7):e1002110. doi: 10.1371/journal.ppat.1002110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bastid J, Cottalorda-Regairaz A, Alberici G, Bonnefoy N, Eliaou JF, Bensussan A. ENTPD1/CD39 is a promising therapeutic target in oncology. Oncogene. 2013;32(14):1743–51. doi: 10.1038/onc.2012.269. [DOI] [PubMed] [Google Scholar]
- 40.Bedi A, Chang X, Noonan K, Pham V, Bedi R, Fertig EJ, et al. Inhibition of TGF-beta enhances the in vivo antitumor efficacy of EGF receptor-targeted therapy. Molecular cancer therapeutics. 2012;11(11):2429–39. doi: 10.1158/1535-7163.MCT-12-0101-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Botta C, Bestoso E, Apollinari S, Cusi MG, Pastina P, Abbruzzese A, et al. Immune-modulating effects of the newest cetuximab-based chemoimmunotherapy regimen in advanced colorectal cancer patients. Journal of immunotherapy. 2012;35(5):440–7. doi: 10.1097/CJI.0b013e31825943aa. [DOI] [PubMed] [Google Scholar]
- 42.Kurai J, Chikumi H, Hashimoto K, Yamaguchi K, Yamasaki A, Sako T, et al. Antibody-dependent cellular cytotoxicity mediated by cetuximab against lung cancer cell lines. Clinical cancer research: an official journal of the American Association for Cancer Research. 2007;13(5):1552–61. doi: 10.1158/1078-0432.CCR-06-1726. [DOI] [PubMed] [Google Scholar]
- 43.Balsamo M, Scordamaglia F, Pietra G, Manzini C, Cantoni C, Boitano M, et al. Melanoma-associated fibroblasts modulate NK cell phenotype and antitumor cytotoxicity. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(49):20847–52. doi: 10.1073/pnas.0906481106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Izawa S, Kono K, Mimura K, Kawaguchi Y, Watanabe M, Maruyama T, et al. H(2)O(2) production within tumor microenvironment inversely correlated with infiltration of CD56(dim) NK cells in gastric and esophageal cancer: possible mechanisms of NK cell dysfunction. Cancer immunology, immunotherapy: CII. 2011;60(12):1801–10. doi: 10.1007/s00262-011-1082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mamessier E, Sylvain A, Thibult ML, Houvenaeghel G, Jacquemier J, Castellano R, et al. Human breast cancer cells enhance self tolerance by promoting evasion from NK cell antitumor immunity. The Journal of clinical investigation. 2011;121(9):3609–22. doi: 10.1172/JCI45816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Trotta R, Dal Col J, Yu J, Ciarlariello D, Thomas B, Zhang X, et al. TGF-beta utilizes SMAD3 to inhibit CD16-mediated IFN-gamma production and antibody-dependent cellular cytotoxicity in human NK cells. Journal of immunology. 2008;181(6):3784–92. doi: 10.4049/jimmunol.181.6.3784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Keskin DB, Allan DS, Rybalov B, Andzelm MM, Stern JN, Kopcow HD, et al. TGFbeta promotes conversion of CD16+ peripheral blood NK cells into CD16- NK cells with similarities to decidual NK cells. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(9):3378–83. doi: 10.1073/pnas.0611098104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Watanabe M, Kono K, Kawaguchi Y, Mizukami Y, Mimura K, Maruyama T, et al. NK cell dysfunction with down-regulated CD16 and up-regulated CD56 molecules in patients with esophageal squamous cell carcinoma. Diseases of the esophagus: official journal of the International Society for Diseases of the Esophagus/ISDE. 2010;23(8):675–81. doi: 10.1111/j.1442-2050.2010.01073.x. [DOI] [PubMed] [Google Scholar]