Abstract
Previous studies have demonstrated gender-related differences in early and late outcomes following type A dissection diagnosis. However, it is widely unknown whether gender affects early clinical outcomes and survival after repair of type A aortic dissection. The goal of this study was to compare the early and late clinical outcomes in women versus men after repair of acute type A aortic dissections.
Between January 2000 and October 2010 a total of 251 patients from four academic medical centers underwent repair of acute type A aortic dissection. Of those, 79 were women and 172 were men with median ages of 67 (range, 20–87 years) and 58 years (range, 19–83 years), respectively (p < 0.001). Major morbidity, operative mortality, and 10-year actuarial survival were compared between the groups.
Operative mortality was not significantly influenced by gender (19% for women vs. 17% for men, p = 0.695). There were similar rates of hemodynamic instability (12% for women vs. 13% men, p = 0.783) between the two groups. Actuarial 10-year survival rates were 58% for women versus 73% for men (p = 0.284).
Gender does not significantly impact early clinical outcomes and actuarial survival following repair of acute type A aortic dissection.
Keywords: aortic dissection, repair, dissection, cardiac surgery
Acute type A aortic dissections exist as a lethal cardiovascular emergency affecting women and men alike, however, gender as it relates to outcomes of surgical repair remains ill-defined. Within the general population, aortic dissections occur 2.6 to 3.5 times per 100,000 person-years.1 2 3 4 While a history of hypertension and advancing age increase the risk of its development, neither contraindicates surgical intervention owing in large part to the dismal survival rates following diagnosis.4 5 6 However, in the absence of surgery, true lethality subsists in the heightened risk of aortic rupture and malperfusion.1 7 8 9 10 11 12 13 14 15 16 17 The urgency to treat these potentially catastrophic vascular crises has led to heightened interest in understanding patient characteristics as they relate to outcomes—among them most important is gender.
Gender influences the incidence (men twice as common as women), the age at presentation, and the extent of dissected aorta,18 19 20 however, there is a paucity of data on gender-related clinical outcomes and survival following repair of type A dissection. The goal of our study was to answer the question: are early clinical outcomes and actuarial survival following acute type A dissection repair similar between women and men?
Methods
Patients
The Society of Thoracic Surgeons Databases at Beth Israel Deaconess, Carolinas Medical Center, Missouri Baptist Medical Center, and Meijer Heart and Vascular Institute were queried to identify all patients who underwent repair of aortic dissection between January 2000 and October 2010. A total of 251 patients, 172 men and 79 women, underwent repair for acute type A aortic dissections. Patients excluded were those that presented with a type A dissection who did not have surgery.
A preoperative diagnosis of aortic dissection was accomplished using computed tomography angiography (CTA) or transesophageal echocardiography (TEE). Most of the patients (84%) had a CTA. The diagnosis was later confirmed at the time of operation. A database was created for entry of demographic, procedural data, and preoperative outcomes. These were prospectively entered by dedicated data-coordinating personnel. Long-term survival data were obtained from the Social Security Death Index (available at: http://www.genealogybank.com/gbnk/ssdi/). Follow-up was 97% complete.
Study approval from the institutional review boards of each center was obtained before this analysis. Patient confidentiality was maintained at all times, consistent with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) regulations.
Definitions
Definitions for this study were obtained from the Society of Thoracic Surgeons' national cardiac surgery database (available at: http://www.sts.org). Acute type A dissection was defined as any dissection involving the ascending aorta with presentation within 2 weeks of symptoms. Cerebrovascular accident was defined as a history of central neurological deficit persisting for more than 24 hours. Diabetes was defined as a history of diabetes mellitus regardless of duration of disease or need for antidiabetic agents. Prolonged ventilation was defined as pulmonary insufficiency requiring ventilatory support. Hemodynamic instability was defined as hypotension (systolic blood pressure < 80 mm Hg) or the presence of cardiac tamponade, shock, acute congestive heart failure, myocardial ischemia, and/or infarction. Operative mortality includes all deaths occurring during the hospitalization in which the operation was performed (even if death occurred after 30 days from the operation), and those deaths occurring after discharge from the hospital, but within 30 days of the procedure.
Operative Technique
The surgical approach did not differ between genders. The diagnosis of type A aortic dissection was confirmed intraoperatively for all patients by TEE. Following a median sternotomy, total cardiopulmonary bypass was initiated with venous cannulation of the right atrium and arterial cannulation of the femoral or right axillary artery. In most cases, cold blood cardioplegia was administered antegrade via the ostia of the coronary arteries and/or retrograde through the coronary sinus to ensure myocardial protection. Otherwise, distal aortic clamping was applied without hypothermic circulatory arrest. A vent was then placed in the left ventricle via the right superior pulmonary vein. To restore the aortic root, the intimal tear was resected followed by replacement of the ascending aorta and resuspension or repair of the aortic valve. After reaching a mean cooling temperature range of 15 to 18°C, the aortic clamp was removed and the aortic arch was inspected. The distal anastomosis was then completed and antegrade aortic perfusion was established. In cases where the aortic root or valve was irreparable, patients underwent either a root replacement with a composite valve graft and coronary button reimplantation, or a valve replacement with mechanical or tissue prosthesis. A Bentall procedure was performed if the repair site extended from the aortic valve to the ascending aorta. Teflon (polytetrafluoroethylene) strips were used to reinforce both the proximal and distal suture lines. For some patients, biological glue (BioGlue surgical adhesive, Cryolife, Kennesaw, GA) was utilized to reapproximate the dissected layers.
Statistical Analysis
Univariate comparisons of preoperative, operative, and postoperative variables were performed between women (n = 79) and men (n = 172). Continuous variables were tested using the Student t-test for association, while categorical variables were assessed by the chi-square or Fisher exact test, based on the count of patients in the contingency tables.
Survival Analysis
Kaplan–Meier univariate unadjusted survival estimates were calculated and compared for men and women using a log-rank test. A p-value of < 0.05 was considered statistically significant. All analyses were conducted using SPSS Statistics Version 21 (IBM Corp., Armonk, NY).
Results
Preoperative Characteristics
Preoperative characteristics are summarized in Table 1. Women were older (p < 0.001), and had lower creatinine levels before surgery (p < 0.001). Women also tended to have lower rates of chronic renal failure, however, this difference was not statistically significantly (p = 0.054). Hemodynamic instability was not found to be significantly different between the two groups (p = 0.783).
Table 1. Preoperative patient characteristics.
| Variablea | Men (n = 172) | Women (n = 79) | p-Value |
|---|---|---|---|
| Age (y) | 58 (19–83) | 67 (20–87) | < 0.001 |
| Diabetes | 14 (8%) | 3 (4%) | 0.216 |
| Hypertension | 136 (80%) | 62 (79%) | 0.993 |
| Ejection fraction | 55 (20–70) | 55 (15–75) | 0.153 |
| COPD | 20 (12%) | 11 (14%) | 0.608 |
| Creatinine | 1.2 (0.5–12.5) | 0.9 (0.4–3.8) | < 0.001 |
| Hemodynamic instability | 21 (13%) | 9 (12%) | 0.783 |
| Arrhythmias | 19 (11%) | 13 (16%) | 0.233 |
| NYHA class | 0.604 | ||
| I | 11 (9%) | 9 (15%) | − |
| II | 8 (6%) | 4 (7%) | − |
| III | 25 (20%) | 10 (17%) | − |
| IV | 81 (65%) | 36 (61%) | − |
| History of cerebrovascular accident | 29 (18%) | 14 (19%) | 0.835 |
| Number of diseased vessels | 0.820 | ||
| 0 | 134 (84%) | 63 (85%) | − |
| 1 | 12 (8%) | 4 (5%) | − |
| 2 | 6 (4%) | 2 (3%) | − |
| 3 | 7 (4%) | 5 (7%) | − |
| EF < 40 | 10 (11%) | 4 (10%) | 1.000 |
Abbreviations: COPD, chronic obstructive pulmonary disease; EF, ejection fraction; NYHA, New York heart association.
Continuous data are shown as median (range) and categoric data are shown as n (%).
Operative Characteristics
Operative patient characteristics of women and men who underwent repair for acute type A aortic dissection are presented in Table 2. BioGlue use was more prevalent in both men and women but there is a tendency to use felt strips more frequently in women and BioGlue more frequently in men (p = 0.032). There was no difference in proximal aortic root reconstruction techniques between women and men (p = 0.730). The most common aortic valve procedure was resuspension of the aortic valve.
Table 2. Operative patient characteristics.
| Variablea | Male (n = 172) | Female (n = 79) | p-Value |
|---|---|---|---|
| CPB time > 200 min | 70 (41%) | 30 (38%) | 0.631 |
| CPB time, min | 182 (5–411) | 167 (64–684) | 0.470 |
| Circulatory arrest time, min | 14 (0–90) | 17 (0–84) | 0.470 |
| Aortic valve procedure | 0.730 | ||
| Nothing | 35 (21%) | 20 (27%) | − |
| Replacement | 15 (9%) | 6 (8%) | − |
| Resuspension | 80 (47%) | 31 (41%) | − |
| Aortic root replacement | 39 (23%) | 18 (24%) | − |
| Distal anastomotic technique | |||
| Distal with cross-clamp | 47 (28%) | 28 (36%) | 0.159 |
| Open distal | 122 (72%) | 49 (64%) | 0.225 |
| Hemiarch technique | 84 (49%) | 41 (53%) | 0.548 |
| Total arch replacement | 18 (11%) | 7 (9%) | 0.728 |
| Arterial cannulation | 0.299 | ||
| Axillary | 71 (53%) | 27 (42%) | − |
| Femoral | 31 (23%) | 20 (31%) | − |
| Other | 32 (24%) | 18 (28%) | − |
| Retrograde cerebral perfusion | 17 (10%) | 12 (16%) | 0.201 |
| Antegrade cerebral perfusion | 45 (26%) | 18 (23%) | 0.605 |
| BioGlue/Felt strip | 0.032 | ||
| BioGlue | 88 (56%) | 36 (47%) | − |
| Felt strip | 28 (18%) | 25 (33%) | − |
| Both | 16 (10%) | 9 (12%) | − |
Abbreviation: CPB, cardiopulmonary bypass.
Continuous data are shown as median (range) and categoric data are shown as n (%).
Postoperative Characteristics
Postoperative outcomes are depicted in Table 3. No significant differences were documented in operative mortality or major morbidity between the two groups. Acute renal failure rates were lower for women than men, however, their difference was not statistically significant (p = 0.054). The median hospital length of stay was similar for both women and men (p = 0.863).
Table 3. Postoperative patient characteristics.
| Variablea | Men (n = 172) | Women (n = 79) | p-Value |
|---|---|---|---|
| Deep sternal wound infection | 3 (2%) | 0 | 0.554 |
| Prolonged ventilation | 74 (46%) | 41 (55%) | 0.165 |
| Acute renal failure | 40 (25%) | 10 (14%) | 0.054 |
| Hemodialysis | 16 (11%) | 5 (7%) | 0.434 |
| Hemorrhage related re-exploration | 34 (22%) | 9 (13%) | 0.109 |
| Cardiac arrest | 12 (7%) | 9 (12%) | 0.228 |
| Stroke | 14 (8%) | 4 (5%) | 0.415 |
| Atrial fibrillation | 40 (25%) | 19 (26%) | 0.851 |
| Hospital length of stay (d) | 11 (0–70) | 11 (0–99) | 0.863 |
| Operative mortality | 29 (17%) | 15 (19%) | 0.695 |
Continuous data are shown as median (range) and categoric data are shown as n (%).
Survival Analysis
Unadjusted Kaplan–Meier survival estimates are presented in Fig. 1. There was no difference in the follow-up time between the groups (p = 0.195). Women had a median follow-up time of 2,014 days (range, 1–4,203 days) and men median follow-up time of 2,180 days (range, 1–4,796 days). Actuarial 10-year survival was 58% for women versus 73% for men (log-rank p = 0.284).
Fig. 1.
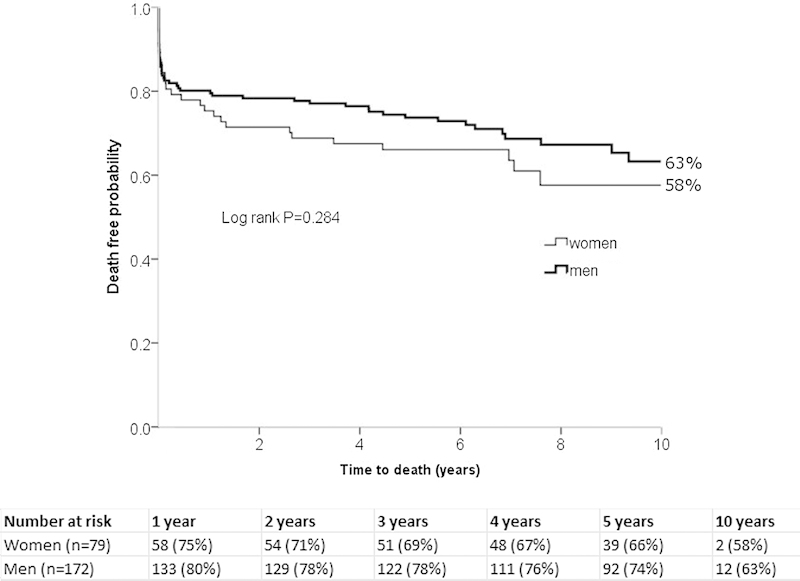
Actuarial unadjusted 10-year survival curves for women versus men (Kaplan–Meier plot is presented with the study originating at the day of operation).
Discussion
Our study is among the first to compare early and late postoperative outcomes between women and men following acute type A aortic dissection repair. Our patients had comparable early outcomes and actuarial survival, irrespective of gender. These results refute the notion that women fare worse than men after surgical repair for acute type A dissection.19
Principal Findings
Operative Mortality
Operative mortality rates were similar between women and men. Previous studies documented worse survival for women compared with men. Specifically, a recent study from the Kaiser Permanente-Registry of Aortic Dissections found the 12-month mortality following diagnosis of aortic dissection to be higher in women than men (33% for women vs. 19% for men, p < 0.01).18
Nienaber et al in a study using the international registry of aortic dissections found a higher operative mortality for women compared with men (31.9 vs. 21.9% for women and men, respectively, p = 0.013).19 However, this difference was only noted in one age group category (ages of 66- and 75-year-old), while there was no difference in mortality between women and men in other age groups. Furthermore, despite the imbalances in the preoperative characteristics (women had a higher rate of congestive heart failure and coma/altered mental status upon presentation), the authors did not use a risk-adjusted methodology (such as propensity score matching) to account for these preoperative imbalances. Moreover, Nienaber et al also included a heterogenous group of patients (either Stanford type A or B aortic dissections, patients treated either medically or surgically). Further, in the surgical cohort, postoperative cardiac tamponade, and hypotension was higher in women versus men and may have influenced the operative mortality. In contrast, our study included a homogenous patient population who underwent repair of type A dissection, excluding patients treated medically or those diagnosed with type B aortic dissection.
It is likely that the improvement in our results when compared with previous studies was affected by temporal factors. Patients in the Nienaber et al study were enrolled between 1996 and 2001 while our patients were enrolled from 2000 to 2010. Advances in diagnostic methods, earlier referral for surgery, and improved surgical experience and intraoperative management have contributed to better operative outcomes of this lethal aortic disease over the last decade. Because of this, it is not surprising that our outcomes were superior to those found in prior studies.
Presentation and Hemodynamics
Hemodynamic instability presentation was similar between women and men in our study. Women were older and had lower creatinine upon presentation, as compared with men. Previous studies have showed that creatinine is physiologically lower for women compared with men.21 22 Lower creatinine levels in female patients may be secondary to their shorter height and lower weight. Also consistent with previous studies, women were older compared with men in our study.18 19 20 However, these preoperative differences between women and men did not affect the operative mortality.
Postoperative Outcomes and Actuarial Survival
Early postoperative outcomes such as atrial fibrillation and stroke rates were comparable between women and men. However, acute renal failure was lower for women compared with men, albeit not significantly (p = 0.054), possibly secondary to a higher preoperative creatinine levels for men. Actuarial 10-year survival was similar between women and men (Fig. 1).
Clinical Implications
We conducted a four-institution observational study to assess the impact of gender on early- and long-term outcomes following repair of acute type A dissection. In this study, we examined an unselected cohort of patients from four academic institutions. This study is among the first to compare early clinical outcomes and actuarial survival between women and men following repair of acute type A aortic dissections. In our study, gender affected incidence (more women compared with men) and age at presentation (women were older compared with men); however, it did not have an impact on early clinical outcomes or survival, following repair of acute type A aortic dissection.
Study Limitations
The inherent limitations of a retrospective multi-institution analysis necessarily affected our study. The small study sample is another limitation which did not allow for multivariate analysis between the two groups. The study may also have introduced potential bias by the fact that nine different surgeons from four different institutions operated on the patients. Further investigation regarding the causes of late mortality, reoperations on the remaining dissected aorta, and the fate of the false lumen were beyond the scope of our study. Because of the retrospective nature of the study a complete list of antihypertensive medications was not available for the study. Further, information on the size of the ascending aorta, root or sinuses or presence of bicuspid aortic valve was not available for the study. These should be the focus of future reports evaluating the long-term outcomes of acute type A aortic dissection patients.
Conclusions
With the improvement of surgical technique and postoperative management, as well as earlier referral of patients, gender has minimal impact on the clinical characteristics, postoperative outcomes, and survival in patients presenting with acute type A aortic dissection. Early recognition and careful management of aortic dissections remain a top priority for optimizing patient outcomes.
References
- 1.Ramanath V S, Oh J K, Sundt T M III, Eagle K A. Acute aortic syndromes and thoracic aortic aneurysm. Mayo Clin Proc. 2009;84(5):465–481. doi: 10.1016/S0025-6196(11)60566-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clouse W D, Hallett J W Jr, Schaff H V. et al. Acute aortic dissection: population-based incidence compared with degenerative aortic aneurysm rupture. Mayo Clin Proc. 2004;79(2):176–180. doi: 10.4065/79.2.176. [DOI] [PubMed] [Google Scholar]
- 3.Cohen R, Mena D, Carbajal-Mendoza R, Arole O, Mejia J O. A case report on asymptomatic ascending aortic dissection. Int J Angiol. 2008;17(3):155–161. doi: 10.1055/s-0031-1278301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mészáros I, Mórocz J, Szlávi J. et al. Epidemiology and clinicopathology of aortic dissection. Chest. 2000;117(5):1271–1278. doi: 10.1378/chest.117.5.1271. [DOI] [PubMed] [Google Scholar]
- 5.Stamou S C, Kouchoukos N T, Hagberg R C. et al. Differences in clinical characteristics, management, and outcomes of intraoperative versus spontaneous acute type A aortic dissection. Ann Thorac Surg. 2013;95(1):41–45. doi: 10.1016/j.athoracsur.2012.08.050. [DOI] [PubMed] [Google Scholar]
- 6.Stamou S C, Hagberg R C, Khabbaz K R. et al. Is advanced age a contraindication for emergent repair of acute type A aortic dissection? Interact Cardiovasc Thorac Surg. 2010;10(4):539–544. doi: 10.1510/icvts.2009.222984. [DOI] [PubMed] [Google Scholar]
- 7.Svensson L G, Crawford E S. Philadelphia: W. B. Saunders Co.; 1997. Cardiovascular and Vascular Disease of the Aorta; pp. 1–6. [Google Scholar]
- 8.Hirst A E Jr, Johns V J Jr, Kime S W Jr. Dissecting aneurysm of the aorta: a review of 505 cases. Medicine (Baltimore) 1958;37(3):217–279. doi: 10.1097/00005792-195809000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Kouchoukos N T, Dougenis D. Surgery of the thoracic aorta. N Engl J Med. 1997;336(26):1876–1888. doi: 10.1056/NEJM199706263362606. [DOI] [PubMed] [Google Scholar]
- 10.Khandheria B K. Aortic dissection. The last frontier. Circulation. 1993;87(5):1765–1768. doi: 10.1161/01.cir.87.5.1765. [DOI] [PubMed] [Google Scholar]
- 11.Eagle K A, DeSanctis R W. Aortic dissection. Curr Probl Cardiol. 1989;14(5):225–278. doi: 10.1016/s0146-2806(89)80010-6. [DOI] [PubMed] [Google Scholar]
- 12.Goossens D, Schepens M, Hamerlijnck R. et al. Predictors of hospital mortality in type A aortic dissections: a retrospective analysis of 148 consecutive surgical patients. Cardiovasc Surg. 1998;6(1):76–80. doi: 10.1016/s0967-2109(97)00086-0. [DOI] [PubMed] [Google Scholar]
- 13.Nienaber C A, von Kodolitsch Y, Petersen B. et al. Intramural hemorrhage of the thoracic aorta. Diagnostic and therapeutic implications. Circulation. 1995;92(6):1465–1472. doi: 10.1161/01.cir.92.6.1465. [DOI] [PubMed] [Google Scholar]
- 14.Hagan P G, Nienaber C A, Isselbacher E M. et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897–903. doi: 10.1001/jama.283.7.897. [DOI] [PubMed] [Google Scholar]
- 15.Lui R C, Menkis A H, McKenzie F N. Aortic dissection without intimal rupture: diagnosis and management. Ann Thorac Surg. 1992;53(5):886–888. doi: 10.1016/0003-4975(92)91460-q. [DOI] [PubMed] [Google Scholar]
- 16.Bavaria J E Pochettino A Brinster D R et al. New paradigms and improved results for the surgical treatment of acute type A dissection Ann Surg 20012343336–342., discussion 342–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bavaria J E Brinster D R Gorman R C Woo Y J Gleason T Pochettino A Advances in the treatment of acute type A dissection: an integrated approach Ann Thorac Surg 2002745S1848–S1852., discussion S1857–S1863 [DOI] [PubMed] [Google Scholar]
- 18.Brar S, Schwartz J, Izquierdo K. et al. Gender Differences in Mortality in Aortic Dissection - Results from the Kaiser Permanente Registry of Aortic Dissections. J Am Coll Cardiol. 2012;59(13s1):E2079. [Google Scholar]
- 19.Nienaber C A, Fattori R, Mehta R H. et al. Gender-related differences in acute aortic dissection. Circulation. 2004;109(24):3014–3021. doi: 10.1161/01.CIR.0000130644.78677.2C. [DOI] [PubMed] [Google Scholar]
- 20.Holmes K W, Maslen C L, Kindem M. et al. GenTAC registry report: gender differences among individuals with genetically triggered thoracic aortic aneurysm and dissection. Am J Med Genet A. 2013;161A(4):779–786. doi: 10.1002/ajmg.a.35836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stevens L A, Levey A S. Measurement of kidney function. Med Clin North Am. 2005;89(3):457–473. doi: 10.1016/j.mcna.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Stevens L A, Coresh J, Greene T, Levey A S. Assessing kidney function—measured and estimated glomerular filtration rate. N Engl J Med. 2006;354(23):2473–2483. doi: 10.1056/NEJMra054415. [DOI] [PubMed] [Google Scholar]


