Abstract
Background
Research has found some disparities between U.S. women with and without disabilities in receiving clinical preventive services. Substantial differences may also exist within the population of women with disabilities. The current study examined published research on Pap smears, mammography, and clinical breast examinations across disability severity levels among women with disabilities.
Methods:
Informed by an expert panel, we followed guidelines for systematic literature reviews and searched MEDLINE, PsycINFO, and Cinahl databases. We also reviewed in-depth four disability- or preventive service-relevant journals. Two reviewers independently extracted data from all selected articles.
Findings
Five of 74 reviewed publications of met all our inclusion criteria and all five reported data on Pap smears, mammography, and clinical breast examination. Articles classified disability severity groups by functional and/or activity levels. Associations between disability severity and Pap smear use were inconsistent across the publications. Mammography screening fell as disability level increased according to three of the five studies. Results demonstrated modestly lower screening, but also were inconsistent for clinical breast examinations across studies.
Conclusion
Evidence is inconsistent concerning disparities in these important cancer screening services with increasing disability levels. Published studies used differing methods and definitions, adding to concerns about the evidence for screening disparities rising along with increasing disability. More focused research is required to determine whether significant disparities exist in cancer screening among women with differing disability levels. This information is essential for national and local public health and health care organizations to target interventions to improve care for women with disabilities.
Introduction and Background
Research has established some disparities between women with and without disabilities in accessing clinical preventive services in the United States. A review of research published from 1990 through 2005 concluded that most studies were consistent in finding reduced routine breast and cervical cancer screening among women with disabilities than among those without (Wisdom et al., 2010). For example, Nosek and Gill (1998) reported that women with functional limitations were significantly less likely than others to have had a Pap test within the past 3 years. Among women age 40 years or older, those with functional limitations were significantly less likely to have had a mammogram within the past 2 years. Havercamp, Scandlin, and Roth (2004) found that women with developmental disabilities were significantly less likely than those with no disabilities to have ever received breast and cervical cancer screening. Notably, women with developmental disabilities were roughly five times more likely to have never received a Pap test (Havercamp et al., 2004). Wei, Findley, and Sambamoorthi (2006) demonstrated strikingly lower rates of breast and cervical cancer screening among women with disabilities compared with other women. More recently, Courtney-Long, Armour, Frammartino, and Miller (2011) noted that, compared with women without disabilities, women with disabilities were less likely to have received a mammogram within the past 2 years even when controlling for sociodemographic, social support, health status, and health care access variables.
This is not unexpected, given that the literature indicates that women with disabilities encounter a number of barriers to receiving clinical preventive services. These include barriers related to physical access, communication, professional support (Barr, Giannotti, Van Hoof, Mongoven, & Curry, 2008; Suzuki, Krahn, Small, & Peterson-Besse, in press), secondary or co-occurring medical conditions, and difficulty traveling to facilities (Suzuki et al., in press). Furthermore, women with multiple disabilities have reported more barriers to returning for regular mammograms than women with a single type of disability (Yankaskas et al., 2010). This latter finding highlights the fact that, in addition to differences between women with and without disabilities, there may be substantial differences within the population of women with disabilities. For example, given the complex barriers to clinical preventive services encountered by women with disabilities, it can be hypothesized that severity of the disability may impact the extent to which women with disabilities are able to obtain screenings. Understanding these differences would help to target efforts to improve screening utilization among those most likely to be missed by general population interventions.
Although some research has studied differences between subgroups of women with disabilities (Cheng et al., 2001; Chevarley, Thierry, Gill, Ryerson, & Nosek, 2006; Diab & Johnston, 2004; Iezzoni, McCarthy, Davis, & Siebens, 2000; Iezzoni, McCarthy, Davis, Harris-David, & O’Day, 2001), a systematic examination of research in this area has not previously been conducted. The purpose of the present study was to systematically review existing research about disparities in U.S. women’s cancer screenings within the group of women with disabilities, by level of disability severity. We describe and qualitatively synthesize the findings across available studies. Specifically, we examine utilization rates of cervical cancer screening (Pap smears), mammograms, and clinical breast examinations. Further, the paper examines the strength of evidence to describe trends where the findings are sufficiently robust and identify areas where data are particularly sparse.
We used the recommendations for clinical preventive services established and updated by the U.S. Preventive Services Task Force (USPSTF, 2010) as the benchmark for this review. There are not separate recommendations for women with disabilities; thus, all women with disabilities should theoretically be receiving screenings with similar frequency as the general population of women. USPSTF recommendations are graded from A through D or I (insufficient evidence) based on expert assessment of the available evidence to support the recom mendations and magnitude of net benefit. These recommenda tions are intended to influence health care professional practices. The USPSTF recommendations relevant for our systematic review were from their publication dates and inclusive data were from 2002: The USPSTF recommended screening mammography with or without clinical breast examination every 1 to 2 years for women aged 40 or older (B grade recommendation; USPSTF, 2002). This was updated in 2009 to biennial screening mammography for women aged 50 to 74 (B grade) with decisions about screenings before age 50 to be guided by individual circumstances. Much of the research reviewed for the present review would have occurred when the 2002 recommendations for screenings beginning at age 40 and conducted every 1 to 2 years would have been in effect. For cervical cancer, the recommendation in 2003 was to screen women who were sexually active and who had a cervix (A grade). See USPSTF for more information about more recent recommendations (USPSTF, 2009, 2012).
Methods
Conceptual Framework
This paper is derived from one of the foci of a larger study on disability disparities in health outcomes and preventive services funded by the National Institute on Disability and Rehabilitation Research. The larger study conducted a systematic scoping review of the literature to identify concentrations and gaps in the literature on within disability group disparities in utilization of clinical preventive services, using the following key question: What English language studies, conducted in the United States and presenting original analyses, have been published in the peer-reviewed literature from 2000 to 2009 that examine clinical preventive service use disparities among subgroups of people with disabilities ages 18 to 64? Because screening recommen-dations, healthcare delivery systems, and healthcare coverage vary remarkably across countries and age groups, our expert panel advised that we also limit our current review to studies about U.S. women between the ages of 18 and 64.
A systematic scoping review uses systematic review methods for study retrieval and review, but asks a broad key question and includes varied study designs with the intention of mapping the literature in an area of study (Arksey & O’Malley, 2005; Petticrew & Roberts, 2006). The current study was a subanalysis on a topic identified from the larger scoping review: Utilization of women’s health services among women with disabilities by level of disability severity.
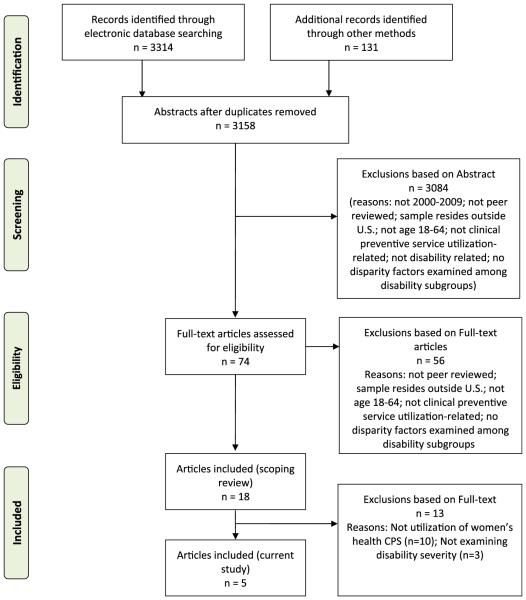
Disability was defined broadly, based on the conceptual domains of the International Classification of Disability, Functioning, and Health (ICF; World Health Organization, 2001). The ICF defines disability as an umbrella term for impairments, activity limitations, or participation restrictions. Further, the ICF emphasizes that environmental factors interact with all of these constructs. We therefore included any disability or functional limitation, falling into physical, sensory, cognitive, mental health, social, or activity limitation functional categories. Detailed methods for the scoping review are reported elsewhere (Peterson, Walsh, Drum, & The Expert Panel on Health and Health Care Disparities among Individuals with Disabilities, Submitted). A brief summary of those methods are as follows. Figure 1 displays the flowchart of our processes in more detail.
Figure 1.
Flowchart for review.
Data Sources and Eligibility Criteria
We used systematic review methods, informed by guidelines outlined by Petticrew and Roberts (2006), the Cochrane Collaboration (Higgins & Green, 2008), and the PRISMA statement on reporting systematic reviews (Moher, Liberati, Tetzlaff, & Altman, 2009). All decisions setting the key question and definitions of concepts relevant to the question were guided by the Disability Rehabilitation Research Project Expert Panel on Health Disparities. Our comprehensive search strategy consisted of electronic searches of MEDLINE, PsycINFO, and Cinahl data-bases. Details of the electronic search strategy, which combined terms for disability populations with terms for clinical preventive services, are available elsewhere (Peterson et al., submitted). For disability, we included a total of 30 individual search terms and a global combined term (details available from authors). Example terms included broad categories such as disabled persons, activities of daily living, developmental disabilities, and mobility limitation, as well as more specific conditions such as paraplegia and blindness. Terms used to search for clinical preventive services included preventive health services, mass screening, and guideline adherence. The search strategy also included table of contents reviews of four disability or preventive service-relevant journals (Disability & Health Journal, Journal of Disability Policy Studies, Archives of Physical Medicine & Rehabilitation, and American Journal of Preventive Medicine), reviewing the reference lists of all articles included for extraction for potentially relevant titles, and articles nominated by members of the Expert Panel. Inclusion criteria were: published in English-language peer-reviewed journals from 2000 to 2009; about adults aged 18 to 64 who have a disability and reside in the United States; examination of use of clinical preventive services. Articles included in the review could describe either observational or intervention research and were not limited by study design. Articles included in the review were required to present original analyses of data, and review articles were not included. Articles were included that presented relevant data, even if disparities in clinical preventive service use by people with disabilities was not a study focus. Review for inclusion was conducted at the abstract and full-text levels. Exclusion at the abstract level was conducted in a hierarchical sequential fashion. Once an article was excluded for one reason, the article was not subjected to review for additional sequential reasons. The sequential exclusion was as follows: 1) non-English language publications; 2) outside of 2000 to 2009 date range; 3) population located outside of the United States; 4) non-peer reviewed publications; 5) article did not include original data; 6) article was non-target age range; 7) article did not examine utilization of clinical preventive services; 8) non-disability target population; and 9) did not examine disparities. For example, among 3,084 articles reviewed at the abstract level, we excluded 546 because they were not about U.S.-based populations. However, had they been retained at that step, many would likely have failed to meet subsequent inclusion criteria. At the abstract level, there was a 10% overlap across reviewers to monitor inter-rater reliability and reviewer drift. Dual independent review was conducted of all articles at the full-text level. The inclusion and exclusion process for the parent review had acceptable agreement for inclusion among reviewers: 98.9% agreement for abstracts and 89.6% agreement for full-text reviews. All inclusion discrepancies were resolved by consensus.
Data Extraction
Data were extracted from each article using a form developed for this study. Two reviewers independently extracted data relevant to the review key questions from all included articles, with all data discrepancies resolved by consensus. We extracted all data that examined potential within-disability group differences in use of any clinical preventive services. A number of individual and system-level factors were extracted to examine for possible disparity evidence, including disability severity. For articles that the reviewers concluded were unclear for the relevant evidence, they asked for review by at least one member of the Expert Panel to address specific questions before finalizing the coded information.
Current Study and Analysis
From the results of the systematic scoping review (Peterson et al., submitted), we observed that utilization of women’s health services was the only area with sufficient data to warrant further analysis of evidence for subgroup disparity. During our initial scoping review, 18 articles met initial criteria (See Figure 1 [Allen, Wieland, Griffin, & Gozalo, 2009; Armour, Swanson, Waldman, & Perlman, 2008; Burns, 2009; Carney, Allen, & Doebbeling, 2002; Cheng et al., 2001; Chevarley et al., 2006; Coughlin, Long, & Kendall, 2002; Daumit, Crum, Guallar, & Ford, 2002; Diab & Johnston, 2004; Folsom et al., 2002; Havercamp et al., 2004; Iezzoni et al., 2000; Iezzoni et al., 2001; Kroll & Neri, 2004; Neri, Bradley, & Groce, 2007; Salsberry, Chipps, & Kennedy, 2005; Schenck et al., 2009; Wei et al., 2006]). We reviewed the set of articles that included women’s health topics (n = 10) for relevance and found that only one factor examining potential within-disability group differences—disability severity—had sufficient data to justify synthesis. For the present study, we included all articles coded as examining utilization of mammography, clinical breast examination, or cervical cancer screening and coded as examining differences in utilization by level of disability severity. For each publication included in our study, we report descriptive data (including definition of disability and of disability severity subgroups) and study findings (both prevalence and adjusted odds ratios [AOR], as available). In several cases, disability severity groups were compared with a common non-disability referent group, rather than to each other. In these cases, we indirectly compared disability groups to each other to determine whether these differences reflected disability severity trends.
Because studies were heterogeneous in objectives and outcomes, we did not systematically rate individual study quality. One of the authors (E.M.A.) reviewed each article further for assessment of the data source, services and classifications, and analyses (e.g., statistical adjustments). These written assessments were reviewed by all authors for consideration of the results. We drew conclusions based on qualitative synthesis of the findings by clinical preventive service topic.
Results
Characteristics of Studies
Results of the data abstraction process are summarized in Table 1. As noted, there were five studies that met our criteria for inclusion in this review, and all five reported data and analysis on receipt of Pap smears, mammography, and clinical breast examination (Cheng et al., 2001; Chevarley et al., 2006; Diab & Johnston, 2004; Iezzoni et al., 2000; Iezzoni et al., 2001). Three studies used data from the 1994-1995 National Health Interview Survey-Disability Supplement (NHIS-D; Chevarley et al., 2006; Iezzoni et al., 2000; Iezzoni et al., 2001), one used data from the Behavioral Risk Factor Surveillance System (BRFSS) analyzing data from 1998 (13 states) and 2000 (18 states) separately (Diab & Johnston, 2004), and one study used multiple sclerosis (MS) patient data from three U.S. health care systems (Cheng et al., 2001). Demographically, all studies included a large majority of White women.
Table 1.
Systematic Review of Disparities among Women with Disabilities for Cancer Clinical Preventive Screenings
| Study, Year | Participants, n, Demographics, Disability |
Data Source: Primary Data (Further Description; Year[s]) |
Definition Clinical Preventive Screening |
Disability Severity Subgroups | Results | ||
|---|---|---|---|---|---|---|---|
| Cervical cancer screening (Pap smear) | |||||||
| Cheng, 2001 | MS patients; N = 692; Adults (M = 47); 86% White |
Received outpatient care in 3 U.S. health care systems |
Past 3 years | Mobility level | % | AOR | |
| Ambulatory | 93 | 5.32 | |||||
| Ambulatory with help | 79 | 2.11 | |||||
| Not ambulatory | 68 | REF | |||||
| Chevarley, 2006 |
N = 77,762 includes women without disability; Age ≥ 18; 76% White |
NHIS-D (1994–1995) | Functional limitations (n) | % in levels† | |||
| 0, 1–2, ≥3 | 0 | 1–2 | ≥3 | ||||
| Within past year | 49.6 | 47.9 | 45.1 | ||||
| 1–3 years | 24.9 | 24.6 | 26.6 | ||||
| >3 years | 16.2 | 22.0 | 19.0 | ||||
| Never | 5.7 | 2.7 | 4.1 | ||||
| Unknown | 3.7 | 2.8 | 5.3 | ||||
| Diab, 2004 |
N = 24,289*; Age ≥ 18; 78% White |
BRFSS 1998; 13 states | Past 3 years | Activity limitation | % | AOR | |
| No limitation | 83.8 | REF | |||||
| Mild disability | 78.8 | 0.98 | |||||
| Moderate disability (IADL) | 72.7 | 0.99 | |||||
| Severe disability (ADL) | 72.9 | 0.94 | |||||
|
N = 35,341*; Age ≥ 18; 68% White |
BRFSS 2000; 18 states | Activity limitation | % | AOR | |||
| None | 84.5 | REF | |||||
| Mild disability | 80.7 | 1.00 | |||||
| Moderate disability (IADL) | 77.5 | 0.99 | |||||
| Severe disability (ADL) | 81.9 | 1.07 | |||||
| Iezzoni, 2000 | N = 77,437; Age 18–75 | NHIS-D (1994–1995) | Past 3 years | Mobility problems | % | AOR | |
| Major: Unable to walk, climb stairs, stand, wheelchair/ scooter |
63.3 | 0.6 | |||||
| Moderate: A lot of difficulty | 79.6 | 1.3 | |||||
| Minor: Some difficulty | 79.4 | 1.2 | |||||
| None: No difficulty | 81.4 | REF | |||||
| Iezzoni, 2001 |
N = 77,762 total; includes women without disability; Age 18–75 |
NHIS-D (1994–1995) | Past 3 years | 1. Lower extremity mobility | % | AOR‡ | |
| Major/significant difficulty | 67.7 | 0.6 | |||||
| Some difficulty | 80.3 | 1.2 | |||||
| 2. Upper extremity mobility | % | AOR‡ | |||||
| Major/significant difficulty | 72.0 | 0.9 | |||||
| Some difficulty | 70.4 | 1.1 | |||||
| 3. Using hands | % | AOR‡ | |||||
| Major/significant difficulty | 72.5 | 0.9 | |||||
| Some difficulty | 70.8 | 0.7 | |||||
| Mammography | |||||||
| Cheng, 2001 | MS N = 245; Age ≥ 50; 86% White of total N |
Received outpatient care in 3 U.S. health care systems |
Past 2 years | Mobility level | % | AOR | |
| Ambulatory | 89 | 3.24 | |||||
| Ambulatory with help | 90 | 3.37 | |||||
| Not ambulatory | 71 | REF | |||||
| Chevarley, 2006 |
N = 77,762 total includes women without disability and younger ages; Age ≥ 30; 76% White in total N |
NHIS-D (1994–1995) | Functional limitations (n) | % in levels† | |||
| 0 | 1–2 | ≥3 | |||||
| Within the past | 0, 1–2, ≥3 | 29.6 | 32.3 | 28.2 | |||
| year | |||||||
| 1–2 years | 16.1 | 12.6 | 15.9 | ||||
| >2 years | 14.8 | 16.6 | 16.3 | ||||
| Never | 35.9 | 35.2 | 36.5 | ||||
| Unknown | 3.5 | 3.2 | 3.1 | ||||
| Diab, 2004 |
N = 10,356*; Age ≥ 50; 78% White of total sample N |
BRFSS 1998; 13 states | Past 2 years | Activity limitation | % | AOR | |
| None | 77.7 | REF | |||||
| Mild disability | 77.2 | 1.03 | |||||
| Moderate disability (IADL) | 71.6 | 0.99 | |||||
| Severe disability (ADL) | 68.4 | 0.84 | |||||
|
N = 14,522*; age ≥ 50; 68% White of total sample N |
BRFSS 2000; 18 states | Activity limitation | % | AOR | |||
| None | 82.2 | REF | |||||
| Mild disability | 80.0 | 1.00 | |||||
| Moderate disability (IADL) | 78.4 | 0.97 | |||||
| Severe disability (ADL) | 81.7 | 1.11 | |||||
| Iezzoni, 2000 |
N = 77,437 includes women without disability and younger ages; age ≥ 50 |
NHIS-D (1994–1995) | Past 2 years | Mobility problems | % | AOR | |
| Major: Unable to walk, climb stairs, stand, wheelchair/ scooter |
45.3 | 0.7 | |||||
| Moderate: A lot of difficulty | 51.5 | 0.9 | |||||
| Minor: Some difficulty | 58.3 | 1.0 | |||||
| None: No difficulty | 63.5 | REF | |||||
| Iezzoni, 2001 |
N = 77,762; includes women without disability and younger ages; age ≥ 50 |
NHIS-D (1994–1995) | Past 2 years | 1. Lower extremity mobility | % | AOR‡ | |
| Major/significant difficulty | 49.9 | 0.7 | |||||
| Some difficulty | 55.8 | 1.0 | |||||
| 2. Upper extremity mobility | % | AOR‡ | |||||
| Major/significant difficulty | 48.8 | 0.8 | |||||
| Some difficulty | 56.4 | 1.1 | |||||
| 3. Using hands | % | AOR‡ | |||||
| Major/significant difficulty | 41.7 | 0.6 | |||||
| Some difficulty | 52.6 | 0.8 | |||||
| Clinical breast examination | |||||||
| Cheng, 2001 | MS N = 245; age ≥ 50; 86% White of total N |
Received outpatient care in 3 U.S. health care systems |
Past year | Mobility level | % | AOR | |
| Ambulatory | 86 | 3.62 | |||||
| Ambulatory with help | 79 | 1.83 | |||||
| Not ambulatory | 69 | REF | |||||
| Chevarley, 2006 |
N = 77,762 total includes women without disability and younger ages; age ≥ 30; 76% White in total N |
NHIS-D (1994–1995) | Functional limitations (n) | % in levels† | |||
| 0 | 1–2 | ≥3 | |||||
| Within the past | 0, 1–2, >3 | 53.7 | 51.7 | 54.4 | |||
| year | |||||||
| 1–2 years | 18.7 | 17.9 | 16.4 | ||||
| >2 years | 18.5 | 20.3 | 20.3 | ||||
| Never | 5.0 | 7.4 | 5.1 | ||||
| Unknown | 4.1 | 2.7 | 3.8 | ||||
| Diab, 2004 |
N = 10,466*; age ≥ 50; 78% White in total sample N |
BRFSS 1998; 13 states | Past year | Activity limitation | % | AOR | |
| None | 67.4 | REF | |||||
| Mild disability | 64.2 | 0.98 | |||||
| Moderate disability (IADL) | 60.6 | 0.96 | |||||
| Severe disability (ADL) | 59.3 | 0.96 | |||||
|
N = 14,636*; age ≥ 50; 68% White in total sample N |
BRFSS 2000; 18 states | Activity limitation | % | AOR | |||
| None | 67.9 | REF | |||||
| Mild disability | 63.0 | 0.93 | |||||
| Moderate disability (IADL) | 63.6 | 0.96 | |||||
| Severe disability (ADL) | 60.1 | 1.05 | |||||
| Iezzoni, 2000 |
N = 77,437; includes women without disability and younger ages; age ≥ 50 |
NHIS-D (1994–1995) | Past 2 years | Mobility problems | % (no AOR) | ||
| Major: Unable to walk, climb stairs, stand, wheelchair/ scooter |
63.9 | ||||||
| Moderate: A lot of difficulty | 65.4 | ||||||
| Minor: Some difficulty | 71.7 | ||||||
| None: No difficulty | 75.7 | ||||||
| Iezzoni, 2001 |
N = 77,762; includes women without disability and younger ages; age ≥ 50 |
NHIS-D (1994–1995) | Past 2 years | 1. Lower extremity mobility | % | AOR‡ | |
| Major/significant difficulty | 67.4 | 0.6 | |||||
| Some difficulty | 69.2 | 1.2 | |||||
| 2. Upper extremity mobility | % | AOR‡ | |||||
| Major/significant difficulty | 69.3 | 0.9 | |||||
| Some difficulty | 67.0 | 1.1 | |||||
| 3. Using hands | % | AOR‡ | |||||
| Major/significant difficulty | 69.3 | 0.9 | |||||
| Some difficulty | 64.8 | 0.7 | |||||
Abbreviations: ADL, activities of daily living; AOR, adjusted odds ratio; BRFSS, Behavioral Risk Factor Surveillance System; CI, confidence interval; FL, functional limitation; IADL, Instrumental ADL; M, mean; MS, multiple sclerosis; NHIS-D, National Health Interview Survey-Disability supplement; REF, referent group; RR, relative risk.
Sample n’s for this study are for the prevalence figures. Adjusted models had fewer subjects.
Prevalence figures for this study are age adjusted.
Reference group for comparisons in this study are all women without the specific disability in that cell.
Study classifications of disability severity groups were generally functional and/or activities based as defined by the ICF; however, no two studies used the same definitions. Cheng and colleagues (2001) compared women with MS across three ambulatory mobility levels. Chevarley and colleagues (2006) categorized women from the NHIS-D using a broad array of physical functional limitations and analyzed women with none (women without disability), one or two, and three or more limitations. Diab & Johnston (2004) used three questions from the BRFSS starting with “any limitations” and then asked women with limitations whether they needed assistance with routine or personal care tasks. Responses about assistance needs were used to classify women as having indicators of problems with instrumental activities of daily living and activities of daily living. Both BRFSS samples of women were then classified as having no limitation, mild disability (limitation only), moderate disability (limitation and instrumental activities of daily living), or severe disability (limitation and activities of daily living). Iezzoni and colleagues (2000) classified women by levels of mobility problems, from no difficulty (women without disability), through three levels of difficulty (minor, moderate, major) based on walking, stair climbing, or use of a wheelchair or scooter. Iezzoni and colleagues (2001) also examined disability severity among subgroups of physical functional problems. Functional groups included women with lower extremity mobility problems, upper extremity mobility problems, and problems using hands. Each group was further categorized by two levels (some difficulties vs. major/significant difficulties) and compared with a reference group of all other women without that specific disability.
Study Results
Pap smear
Across all five studies, there were inconsistent findings for the effect of disability severity on Pap smear use. The strongest results suggesting disparity were from among women with MS. Cheng and colleagues (2001) demonstrated a strong gradient (disability severity trend). Both unadjusted percentages and AOR results demonstrated greater proportions of women screened in the last 3 years with decreasing disability severity, comparing women who were not ambulatory (68% screened, reference category) with women who were ambulatory with help (79%; AOR, 2.11) and fully ambulatory (93%; AOR, 5.32). In a similar vein, Chevarley and colleagues (2006) demonstrated that age adjusted prevalence of recent Pap smear (within the last year) declined across functional groups (0 limitations, 49.6% screened; 1 2 limitations, 47.9%; 3 or more limitations, 45.1%). However, there were no clear trends representing a severity gradient or a “threshold” for some level of limitation across increasingly longer periods for Pap smears (e.g., within 1 3 years, longer than 3 years, never). The results also were not subjected to a multivariate comparison adjusting for possible confounders other than age. Data from the BRFSS surveys (Diab & Johnston, 2004) also examined Pap smears within the last 3 years. Although the unadjusted results showed some evidence of disparity for women with disability compared with women without disability, there was not a clear disability severity gradient. In addition, between the 2 years of data that the study analyzed separately, adjusted results suggested that for the 18 states included in the later BRFSS 2000 analysis, women with the highest level of disability severity were more likely to have received a Pap smear compared with other women with less severe disability and also compared with women without disability (the AOR for women with severe disability was 1.07 compared with women without disability; Table 1). Both studies conducted by Iezzoni and colleagues (Iezzoni et al., 2000; Iezzoni et al., 2001) demonstrate some indirect evidence of a “threshold” effect, where the most severe disability level was associated with lower Pap smear rates for women with mobility problems. However, the effect was absent, perhaps even reversed, for women whose disability was limited to their hands.
Mammography
Mammography was reduced for women with increasing levels of disability severity for three of the five studies. However, data from the NHIS-D using functional limitations (Chevarley et al., 2006) did not demonstrate any pattern of disparity across disability severity or increasing durations since last mammogram. Similarly, BRFSS data analysis from 2000 (Diab & Johnston, 2004) showed no effect of disability or disability severity for mammography within the last 2 years. Cheng and colleagues (2001) demonstrated a strong severity threshold effect for women who were not ambulatory (highest level of severity) compared with other women with MS. Data from the 1998 BRFSS demonstrated both unadjusted and adjusted comparisons showing decreasing mammography with increasing severity of disability (Diab & Johnston, 2004). Using different definitions of disability severity in the NHIS-D data, Iezzoni and co-workers (Iezzoni et al., 2000; Iezzoni et al., 2001) demonstrated an effect of increasing severity and decreasing mammography in the past 2 years in both analyses of the NHIS-D.
Clinical breast examination
Evidence for an effect of disability severity for clinical breast examination was evident in the study of women with MS. Cheng and colleagues (2001) examined clinical breast examination within the last year, and showed striking crude and adjusted disparities for women with increasing mobility problems. Women who were ambulatory were most likely to have received a clinical breast examination (86%), followed by women who were ambulatory with help (79%) and women who were not ambulatory (69%). Demographic and comorbidity-adjusted analyses also demonstrated this severity gradient pattern. Analyses based on the BRFSS demonstrated an effect of disparity in clinical breast examination in the past year across disability severity in both sets of unadjusted analyses (1998 and 2000 BRFSS states), but very weak or absent patterns in adjusted analyses (Diab & Johnston, 2004). In analysis of the NHIS D for mobility severity levels, Iezzoni and colleagues (2000) demon strated decreasing clinical breast examinations with increasing disability severity; however, the study did not include adjusted results. Using categories of mobility disability, Iezzoni and colleagues (2001) also demonstrated a modest effect of reduced clinical breast examination for more severe disability in both lower extremity and upper extremity mobility disability groups. However, the analysis of women with hand disability showed a modest reversed effect: women with major disability were more like the comparison group than women with some disability (AOR, 0.7 for the latter; 0.90 for the former).
Discussion
The five studies included in this review each contributed results relevant to our question about whether severity of disability is a risk factor for reduced clinical preventive services for women. However, each of the studies was designed for its own scientific question using their own disability definition. Overall, the five articles stated purposes and used methods that were not a direct match with our systematic review key question. There were varied definitions of disability and severity, and even differences in indicators of screening guidelines. In one case (Chevarley et al., 2006), mammography and clinical breast examination screening were examined for women aged 30 and older. Although guidelines from different sources have differed by age (age 40, 50, stopping at older ages) and by frequency, no recommendations suggest that mammography begin at age 30. Each study used a different method to define severity or level of disability, although they shared some common ground based on some form of physical function (e.g., mobility levels) or activity (e.g., self-care). The fact that three studies (Chevarley et al., 2006; Iezzoni et al., 2000; Iezzoni et al., 2001) all analyzed one data set (NHIS-D) but arrived at slightly differing findings demonstrates the importance of how disability severity is defined. These differences in definitions, as well as other differences between samples, produced problems and complexity in interpreting evidence patterns for our question about disability severity. For example, one study was based on a relatively small patient sample with healthcare coverage (Cheng et al., 2001; U.S. Department of Health and Human Services, 2000) and the other four were based on larger, community-dwelling, pop ulation-based samples. An additional barrier to reaching a clear conclusion was that only the crude (or minimally age-adjusted) prevalence figures provided direct evidence in some studies because the referent category for most adjusted analyses was women without disabilities. However, our focus was on comparisons among women with disabilities, looking at effects of disability severity.
In addition to the heterogeneity of study methodologies, there were differences in results for our question about disparity by disability severity. There was some evidence for disparity by disability severity for all three preventive services. However, the evidence varied by preventive service and whether the evidence supported a trend with disability severity across categories, or if there was evidence only for women with the highest level of impairment. Because national and local public health and healthcare organizations need to understand whether and where disparities exist, there is a considerable need for more (and more focused) research about cancer screening disparity among women with disability.
Implications for Policy
As noted, our review was hampered by having few articles that focused on and reported data on subgroups of women with disabilities. Whereas federal funding agencies support and request reporting data by subgroups (e.g., by gender or race/ ethnicity), there have been no previous policies that require or strongly support data on disability status (or subgroups) as a group with disparities. Without these policies, and/or funding initiatives that specifically request such analysis, there may continue to be sparse attention to disparities in women’s health within disability.
Differences in definition of disability created a significant obstacle to collating data and making comparisons across studies. Healthy People 2010 (U.S. Department of Health and Human Services, 2000) and again Healthy People 2020 (U.S. Department of Health and Human Services, 2010) had as one of their objectives to include a standard definition of disability in all surveillance. The Affordable Care Act (U.S. Department of Health and Human Services, n.d.a) provides promise to address this problem in two sections. First, Section 4302, “Under-standing Health Disparities” calls for routine inclusion of six disability identifier questions in federally funded or supported public health programs, activities and surveys (Madans, Loeb, & Altman, 2011). This led to standards for disability identification being established by the U.S. Department of Health and Human Services (U.S. Department of Health and Human Services, Office of Minority Health, 2011) that should standardize data collection for disability, and increase ability to distinguish among type (if not severity) of functional limitations in the future. Researchers are encouraged to add questions that would assess severity of disability (e.g., difficulty with complex activities entailed in performance of social roles; Altman & Bernstein, 2008). Further, Section 4203 of the Affordable Care Act requires establishing standards for accessible medical equipment like radiology equipment, examination tables, and weight scales. This requirement is anticipated to increase access of women, particularly with mobility limitations, to routine clinical procedures (U.S. Department of Health and Human Services, n.d.b). To monitor and evaluate these changes, and to continue to promote screening access for women, we will need population-level data. Although our report highlights the methods and data sources, and Affordable Care Act-driven changes promise to improve data and access, there may still need to be a funder incentive to generate interest in examining data for disability status, type, and severity.
Social factors are increasingly recognized as important contributors to health. Social determinants refer to the social circumstances in which people live their lives (World Health Organization, 2013) and are often measured in terms of education, income, urban/rural residence, health care access, transportation, and environmental safety factors. These social factors are as relevant for people with disabilities as the general population, and environmental access is especially important for people with disabilities, who can be excluded from participation through physical, attitudinal, or policy barriers. Our review sought to examine disparities related to social determinants in addition to disability severity, but these factors were not included in many of the studies we reviewed. Even where these factors were included (e.g., age, education), they were used as covariates in analyses, and the effects of social determinants were not examined for their contribution to health service utilization. Future research should begin to examine the contribution of these social factors to a range of health outcomes, including use of clinical preventive services.
In conclusion, there is modest evidence for disparity in all three cancer clinical preventive screenings with increasing disability severity or among women with the most severe disability (threshold effect). The evidence from these five studies is far from conclusive. Heterogeneity of samples, definitions of disability severity, and choice of comparison groups adds to our caution in concluding there is a pattern of evidence for decreased screening with increased disability severity.
The field requires much more targeted analysis and consistent definitions to generate stronger evidence. All of the available studies and most future research will be observational in design. The descriptive epidemiologic research needs to develop to the level that there is some consistency of the scientific story, one of the core concepts of concluding causal inference in observational (versus interventional) research (Rothman, Greenland, & Lash, 2008). There are at least two avenues that can contribute to this development of evidence. One is for published research to provide sufficient detail on subgroups of people with disabilities that there are, at a minimum, crude estimates of the patterns of use of preventive services. Because disability is not often the sole focus of such studies, the samples that meet some classification of disability may be small and therefore not included in descriptive tables. Second, because descriptive results in observational studies are very likely to be confounded by other social determinant factors that are associated with disparities (e.g., education), there need to be publications that focus specifically on women with disabilities and thoroughly analyze the results to address disparities among subgroups. The majority of this work may be from existing research (secondary analyses of clinical research, healthcare administrative data, etc), and targeted analyses of large federal data with sufficient numbers of women with disabilities (e.g., NHIS, BRFSS, the Medical Expenditure Panel Study). All of these samples have special problems in addressing the question we raised in this article (samples, classifications, etc.). However, given that the goal is to understand whether there is consistency of the evidence, these differences might build the picture precisely because an emerging pattern would suggest a fairly consistent pattern among heterogeneous studies. In addition, a careful examination of the variations could explain why some analyses (outliers) do not fit the scientific picture. The essential first step is to have sufficient published research, with consistent definitions and outcomes, to begin to combine evidence.
Acknowledgments
Supported by grant #H133A080031 from National Institute on Disability and Rehabilitation Research/DOE. However, those contents do not necessarily represent the policy of the Department of Education, and you should not assume endorsement by the Federal Government.
References
- Allen SM, Wieland S, Griffin J, Gozalo P. Continuity in provider and site of care and preventive services receipt in an adult Medicaid population with physical disabilities. Disability and Health Journal. 2009;2(4):180–187. doi: 10.1016/j.dhjo.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman B, Bernstein A. Disability and health in the United States, 2001–2005. DHHS publication no. (PHS) 2008–1035) National Center for Health Statistics; Hyattsville, MD: 2008. [Google Scholar]
- Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. [Google Scholar]
- Armour BS, Swanson M, Waldman HB, Perlman SP. A profile of state-level differences in the oral health of people with and without disabilities, in the U.S., in 2004. Public Health Reports. 2008;123(1):67–75. doi: 10.1177/003335490812300110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr JK, Giannotti TE, Van Hoof TJ, Mongoven J, Curry M. Understanding barriers to participation in mammography by women with disabilities. American Journal of Health Promotion. 2008;22(6):381–385. doi: 10.4278/ajhp.22.6.381. [DOI] [PubMed] [Google Scholar]
- Burns ME. Medicaid managed care and health care access for adult beneficiaries with disabilities. Health Services Research. 2009;44(5):1521–1541. doi: 10.1111/j.1475-6773.2009.00991.x. Pt 1. Retrieved from. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&NEWS=N&PAGE=fulltext&D=medl&AN=19555397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney CP, Allen J, Doebbeling BN. Receipt of clinical preventive medical services among psychiatric patients. Psychiatric Services. 2002;53(8):1028–1030. doi: 10.1176/appi.ps.53.8.1028. [DOI] [PubMed] [Google Scholar]
- Cheng E, Myers L, Wolf S, Shatin D, Cui XP, Ellison G, et al. Mobility impairments and use of preventive services in women with multiple sclerosis: Observational study. BMJ. 2001;323(7319):968–969. doi: 10.1136/bmj.323.7319.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevarley FM, Thierry JM, Gill CJ, Ryerson AB, Nosek MA. Health, preventive health care, and health care access among women with disabilities in the 1994-1995 National Health Interview Survey, Supplement on Disability. Womens Health Issues. 2006;16(6):297–312. doi: 10.1016/j.whi.2006.10.002. [DOI] [PubMed] [Google Scholar]
- Coughlin TA, Long SK, Kendall S. Health care access, use, and satisfaction among disabled Medicaid beneficiaries. Health Care Financing Review. 2002;24(2):115–136. [PMC free article] [PubMed] [Google Scholar]
- Courtney-Long E, Armour B, Frammartino B, Miller J. Factors associated with self-reported mammography use for women with and women without a disability. Journal of Women’s Health. 2011;20(9):1279–1286. doi: 10.1089/jwh.2010.2609. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Crum RM, Guallar E, Ford DE. Receipt of preventive medical services at psychiatric visits by patients with severe mental illness. Psychiatric Services. 2002;53(7):884–887. doi: 10.1176/appi.ps.53.7.884. [DOI] [PubMed] [Google Scholar]
- Diab ME, Johnston MV. Relationships between level of disability and receipt of preventive health services. Archives of Physical Medicine and Rehabilitation. 2004;85(5):749–757. doi: 10.1016/j.apmr.2003.06.028. [DOI] [PubMed] [Google Scholar]
- Folsom DP, McCahill M, Bartels SJ, Lindamer LA, Ganiats TG, Jeste DV. Medical comorbidity and receipt of medical care by older homeless people with schizophrenia or depression. Psychiatric Services. 2002;53(11):1456–1460. doi: 10.1176/appi.ps.53.11.1456. [DOI] [PubMed] [Google Scholar]
- Havercamp SM, Scandlin D, Roth M. Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in North Carolina. Public Health Reports. 2004;119(4):418–426. doi: 10.1016/j.phr.2004.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, Ltd; West Sussex, England: 2008. [Google Scholar]
- Iezzoni LI, McCarthy EP, Davis RB, Harris-David L, O’Day B. Use of screening and preventive services among women with disabilities. American Journal of Medical Quality. 2001;16(4):135–144. doi: 10.1177/106286060101600405. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, McCarthy EP, Davis RB, Siebens H. Mobility impairments and use of screening and preventive services. American Journal of Public Health. 2000;90(6):955–961. doi: 10.2105/ajph.90.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroll T, Neri MT. Use of primary prevention services among male adults with cerebral palsy, multiple sclerosis, or spinal cord injury in managed care and fee-for-service. Managed Care Quarterly. 2004;12(3):6–10. [PubMed] [Google Scholar]
- Madans J, Loeb M, Altman B. Measuring disability and monitoring the UN convention on the rights of persons with disabilities: The work of the Washington Group on Disability Statistics. BMC Public Health. 2011;11(Suppl. 4):S4. doi: 10.1186/1471-2458-11-S4-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine. 2009;6(7):1–6. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neri SV, Bradley EH, Groce NE. Frequency of HIV testing among persons with disabilities: Results from the national health interview survey, 2002. AIDS Education and Prevention. 2007;19(6):545–554. doi: 10.1521/aeap.2007.19.6.545. [DOI] [PubMed] [Google Scholar]
- Nosek MA, Gill CJ. Use of cervical and breast cancer screening among women with and without functional limitations: United States, 1994-1995. MMWR - Morbidity & Mortality Weekly Report. 1998;47(40):853–856. [PubMed] [Google Scholar]
- Peterson JJ, Walsh ES, Drum CE. The Expert Panel on Health and Health Care Disparities among Individuals with Disabilities. (Submitted). Disparities in the utilization of clinical preventive services among subgroups of the population with disabilities: A systematic scoping review. American Journal of Preventive Medicine [Google Scholar]
- Petticrew M, Roberts H. Systematic reviews in the social sciences: A practical guide. Blackwell; Malden, MA: 2006. [Google Scholar]
- Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd Lippincott Williams & Wilkins; Philadelphia: 2008. [Google Scholar]
- Salsberry PJ, Chipps E, Kennedy C. Use of general medical services among Medicaid patients with severe and persistent mental illness. Psychiatric Services. 2005;56(4):458–462. doi: 10.1176/appi.ps.56.4.458. [DOI] [PubMed] [Google Scholar]
- Schenck AP, Peacock SC, Klabunde CN, Lapin P, Coan JF, Brown ML. Trends in colorectal cancer test use in the Medicare population, 1998-2005. American Journal of Preventive Medicine. 2009;37(1):1–7. doi: 10.1016/j.amepre.2009.03.009. [DOI] [PubMed] [Google Scholar]
- Suzuki R, Krahn G, Small E, Peterson-Besse J. Multi-level barriers to obtaining mammograms for women with mobility limitations: post workshop evaluation. American Journal of Health Behavior. 2013;37(5):711–718. doi: 10.5993/AJHB.37.5.15. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . Healthy people 2010. U.S. Government Printing Office; Washington, DC: 2000. [Google Scholar]
- U.S. Department of Health and Human Services. (n.d.a) Affordable Care Act for Americans With Disabilities. Retrieved August 15, 2012, from http://www.hhs.gov/od/affordable_care_act.html.
- U.S. Department of Health and Human Services. (n.d.b) People With Disabilities and the Affordable Care Act: Fact sheets. Retrieved August 15, 2012, from http://www.healthcare.gov/news/factsheets/2011/08/people-with-disabilities.html.
- U.S. Department of Health and Human Services . Healthy people 2020. ODPHP Publication No. B0132. U.S. Department of Health and Human Services; Rockville, MD: 2010. [Google Scholar]
- U.S. Department of Health and Human Services, Office of Minority Health Final data collection standards for race, ethnicity, primary language, sex, and disability status required by section 4302 of the affordable care act. 2011 Retrieved September 5, 2012, from http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlid=208.
- U.S. Preventative Services Task Force Screening for breast cancer: Recommendations and rationale. Ann Intern Med. 2002;137(5):344–346. doi: 10.7326/0003-4819-137-5_part_1-200209030-00011. Part 1. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force (USPSTF) The guide to clinical preventive services. Agency for Healthcare Research and Quality; Rockville, MD: 2009. [Google Scholar]
- U.S. Preventive Services Task Force (USPSTF) Recommendations. 2010 doi: 10.7326/0003-4819-153-12-201012210-00007. Retrieved May 21, 2012, from http://www.uspreventiveservicestaskforce.org/recommendations.htm. [DOI] [PubMed]
- U.S. Preventive Services Task Force (USPSTF) Screening for cervical cancer: U.S. preventive services task force recommendation statement. 2012 Retrieved September 11, 2012, from http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm.
- Wei W, Findley PA, Sambamoorthi U. Disability and receipt of clinical preventive services among women. Womens Health Issues. 2006;16(6):286–296. doi: 10.1016/j.whi.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisdom JP, McGee MG, Horner-Johnson W, Michael YL, Adams E, Berlin M. Health disparities between women with and without disabilities: A review of the research. Social Work in Public Health. 2010;25(3):368–386. doi: 10.1080/19371910903240969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . International classification of functioning, disability and health. Author; Geneva: 2001. [Google Scholar]
- World Health Organization Social determinants of health. 2013 Retrieved February 8, 2013, from http://www.who.int/social_determinants/en/
- Yankaskas BC, Dickens P, Bowling JM, Jarman MP, Luken K, Salisbury K, et al. Barriers to adherence to screening mammography among women with disabilities. American Journal of Public Health. 2010;100(5):947–953. doi: 10.2105/AJPH.2008.150318. [DOI] [PMC free article] [PubMed] [Google Scholar]