Abstract
The best surgical technique for pilonidal sinus disease (PSD) is still disputed. The objective of this prospective randomized study is to compare the short and long-term results of modified Limberg flap and Karydakis flap surgeries that have been widely used in recent years. Ninety one patients were included in the study. The patients were divided into two groups: modified Limberg flap (MLF; n = 46) and Karydakis flap (KF; n = 45). Preoperative findings of the patients, their surgical findings, and short and long-term postoperative findings were recorded and statistically compared. While no significant difference was discovered between the groups in terms of postoperative analgesic need, hospital stay, postoperative infection rate, drain stay time, painless sitting time, painless toilet-sitting time, and painless walking time, return to work or school time was shorter in the MLF group compared with the KF group (20.61 ± 7.89 days, 23.29 ± 6.42, respectively; P < 0.05). Cosmetically, the visual analog scale (VAS) of the KF group was significantly higher than that of the MLF group (VAS score 7.12 ± 1.28, 5.45 ± 1.77, respectively; P < 0.05). Considering recurrence rates, no statistically significant difference was found between the groups. Our study found out that short and long-term results of the MLF and KF procedures are similar. We believe both methods can be safely used in surgical PSD treatment given that in the MLF procedure, shorter return-to-work time is achieved, while the procedure provides better cosmetic results.
Key words: Pilonidal sinus, Limberg flap, Karydakis flap, Surgical techniques
Pilonidal sinus disease (PSD) is a chronic inflammation and infection of the sacrococcygeal region. It often affects young adult males and produces clinic findings with abscess and discharge in sacrococcygeal region or painful sinus tract in the natal cleft.1,2 Its incidence rate is predicted to be minimum 26 and maximum 700 in 100,000, and its incidence rate among Turkish servicemen is reported to be 8.8% in a study.3,4
Discussion as to whether PSD is a congenital disease continued until a few decades ago, and many authors are now convinced that it is an acquired disease. Although theories of Karydakis and Bascom provide the best explanation about the pathogeny of the disease, there is no definite etiology and pathogenesis.5,6 Male sex, obesity, sedentary lifestyle, jobs that require sitting for long hours, family history, hirsute body habitus, trauma or irritation of the natal cleft, and poor hygienic conditions are among the listed risk factors.7,8
Several methods were defined in order to determine the ideal treatment of PSD. The expectations from an ideal treatment can be listed as simplicity and convenience, good postoperative patient comfort, low complication rate, early return-to-work time and low recurrence rate.9 Although several medical and surgical methods exist, ranging from phenol application to complex advancement flaps, no optimal treatment method has been defined yet due to high complication and recurrence rates.10,11 Recently, lateralization of the natal cleft has gained significance in surgical PSD treatment. The purpose with this method is to prevent recurrence on the midline by removing the cavity in the natal cleft. While this is achieved with the Karydakis flap (KF) by moving the suture laterally, it is achieved in the modified Limberg flap (MLF) operation by flattening the natal cleft with a full-thickness flap.6,12
Our objective is to compare short- and long-term results of Karydakis flap and Modified Limberg flap operations, which have been widely preferred in recent years in surgical treatment of PSD, by conducting a prospective randomized study.
Materials and Methods
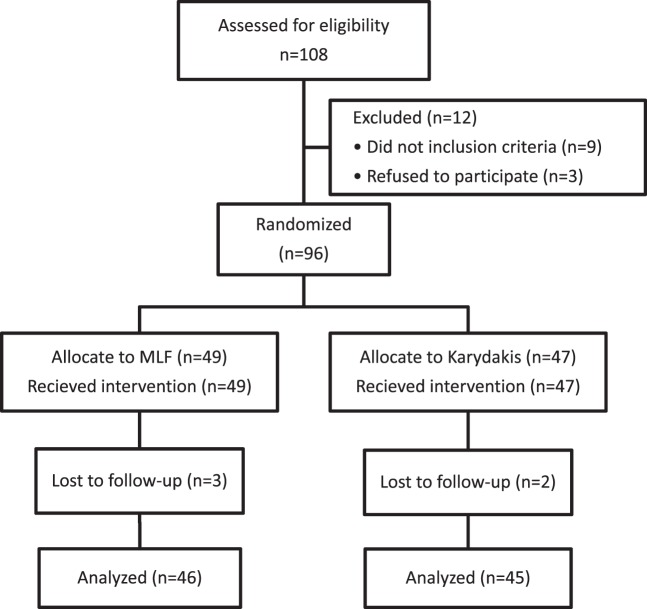
This prospective randomized study was carried out in General Surgery Clinic Etlik Specialization Training and Research Hospital. The study was also approved by Ethical Review Board of Medicine Faculty Yildirim Beyazit University. A total of 108 patients in the hospital diagnosed through a physical examination as having chronic PSD were evaluated. Patients with diabetes mellitus, immunodeficiency, neurological disorder, drug addiction, alcoholism, ASA 3–4, those who are under 17 and over 60, and those whose orifice was located away more than 3 cm were excluded. As 9 patients did not match the criteria of the study, and 3 refused to be included, they were excluded (Fig. 1). After the patients were advised about the clinical details of the surgical procedures and their written informed consent was obtained, they were referred to clinic for randomization. The patients were computer based randomized by an independent officer using patient admission numbers. Both surgical procedures were performed by the same surgeons.
Fig. 1.
Trial flow chart.
Fig. 2.
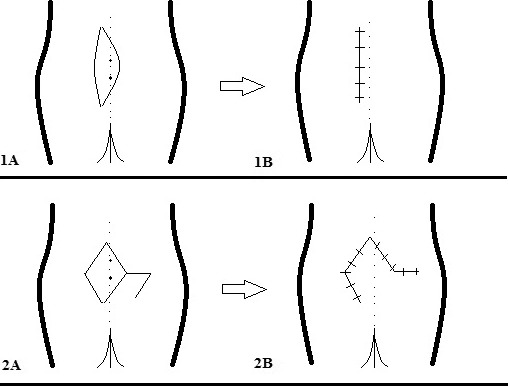
Preparation of the Karydakis (1A, 1B) and modified Limberg (2A, 2B) flap techniques.
Surgical Procedure
All patients were taken into the operation under spinal anesthesia in prone position. All of them were administered antibiotics prophylaxis with 1 g Cefazolin through intravenous method on the operating table. The patients were placed in the jackknife position allowing better sight of the operation area, and both buttocks were retracted to the lateral using sticky tapes. The operating site was cleaned with 10% povidone-iodine solution.
Operations were performed in the modified Limberg flap (MLF) group as defined by Mentes et al.13 Rhomboid excision was performed, the lower end being 2 cm lateral to the midline and covering the whole area where the sinus spread. Using electrocautery, hemostasis was provided. In order to ensure tension-free repair, the flap was released at the bottom including gluteal fascia, and then slid to medial in order to cover the defect. A suction drain was applied to the region in all patients. The subcutaneous tissue was closed with 2-fold 2/0 polyglactin suture (Ethicon US, LLC, Cincinnati, Ohio), and the skin was closed with 3/0 polypropylene (Ethicon US, LLC) mattress suture. When the drain amount fell below 20 mL/d, it was removed.
Operations were performed in the Karydakis flap (KF) group as defined by Karydakis.5 In this technique, an asymmetrical elliptic excision was done, lower and upper ends being located at approximately 2 cm lateral to the natal cleft, and all defective tissues were removed until reaching to the healthy borders. After that, the medical wound edge was mobilized, and the flap was slid by suturing to the fascia and skin suitable wound layers on the lateral wound edge corresponding to one another. The subcutaneous tissue was closed with 2-fold 2/0 polyglactin suture, and the skin was closed with 3/0 polypropylene mattress suture. In all patients, a suction drain was applied to the region. When the drain amount fell below 20 mL/d, it was removed.
Data regarding patient age, sex, BMI, preoperative complaint time, preoperative discharge history, preoperative abscess drainage history, preoperative antibiotics use, lateral orifice existence, operation type, operation duration, hospital stay time, drain stay time, preoperative infection, postoperative analgesic need, painless sitting time, painless toilet-sitting time, painless walking time, return-to-work or school time, cosmetic dissatisfaction, recurrence, and whether operation was recommended to others were recorded in this study. Data were collected by examining the patients during postoperative dressing in the clinic. We assessed patients' wounds daily as they needed dressing. Patients were assessed weekly for the first month and subsequently every 3 months for the first year. After the first year, we told patients to contact us if they had any problems. We called all the patients for final examination on October 2013.
In order to assess cosmetic condition, visual analogue scale (VAS) with items 1 to 10 was used.
Statistics
Statistical analyses were carried out using statistical software (SPSS 17.0; SPSS, Inc, IBM Corp., Armonk, New York). Mean and standard deviation values were used for calculating numeric parameters, while numeric and percentage values were used for categorical variables. The Kolmogorov-Smirnov test was employed for calculating distribution of all variable groups in comparisons. Student's t-test (independent sample t-test), as a parametrical test, and Mann-Whitney U test, as a nonparametrical test, were used. In comparing categorical variables, cross-table statistics were used (χ2-Fisher's exact test). Significance limit of statistics was set at P < 0.05.
Results
Three patients from the MLF group and 2 from the KF group could not be contacted during follow-up. Eventually, results were statistically analyzed for modified Limberg flap (46 patients) and Karydakis flap (45 patients).
Seventy nine (86.8%) and 12 (13.2%) of the patients included in the study were males and females, respectively. Average age was 28 (18–25 years). No statistically significant difference was found between the groups in terms of age, sex, and BMI (P > 0.05; Table 2). Average preoperative complaint period of the patients was 36 months, and there was no significant difference between the groups (P > 0.05). Thirteen patients in the MLF group (28.2%), and 13 patients in the KF group (28.8%) described having sacrococcygeal discharge at any preoperative time, and no significant difference was found between the groups (P > 0.05). There was no significant difference between the groups in terms of number of patients who had gone through pilonidal abscess drainage. Of the patients in both groups, 17.3% had lateral orifice apart from natal cleft, and there was no significant difference between the groups (P > 0.05; Table 3).
Table 2.
Demographics of the patients
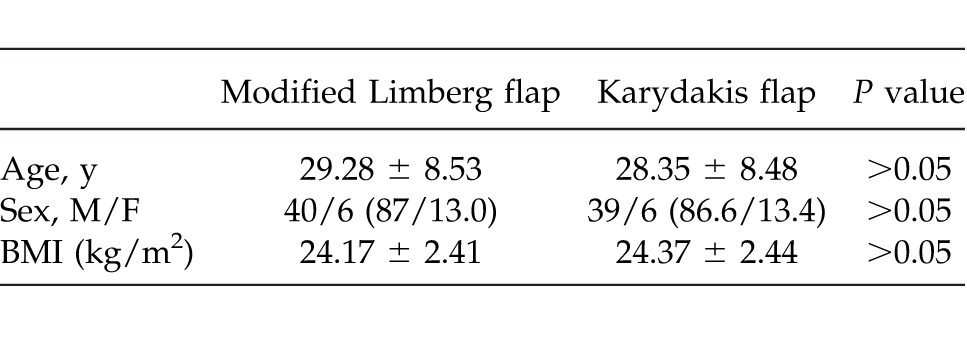
Table 3.
Comparison of preoperative findings about disease
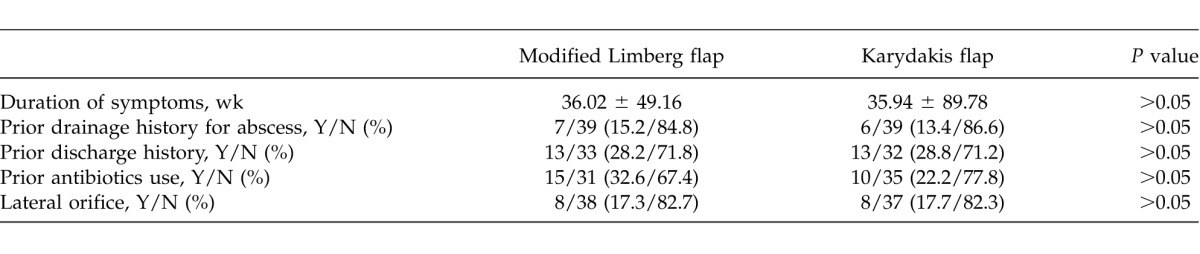
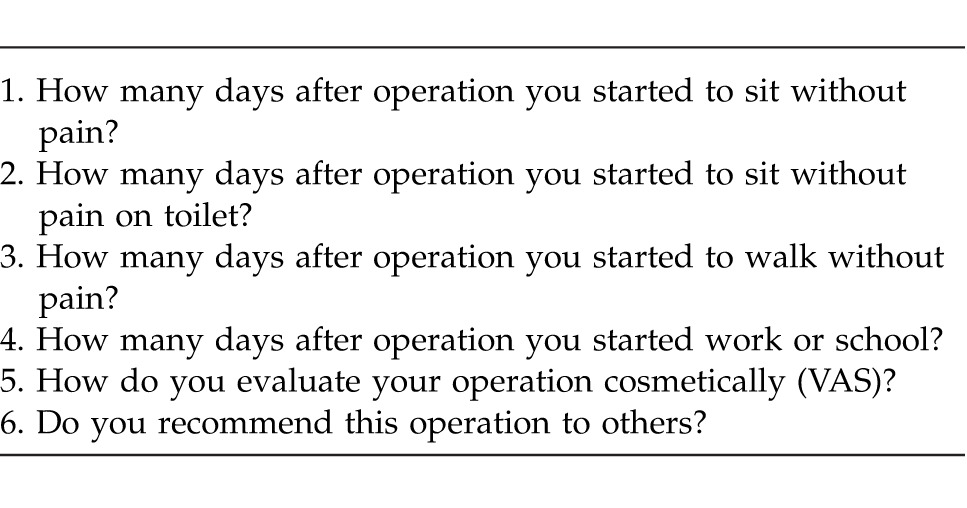
Table 1.
Question form used in patients interviews at the third month postoperatively
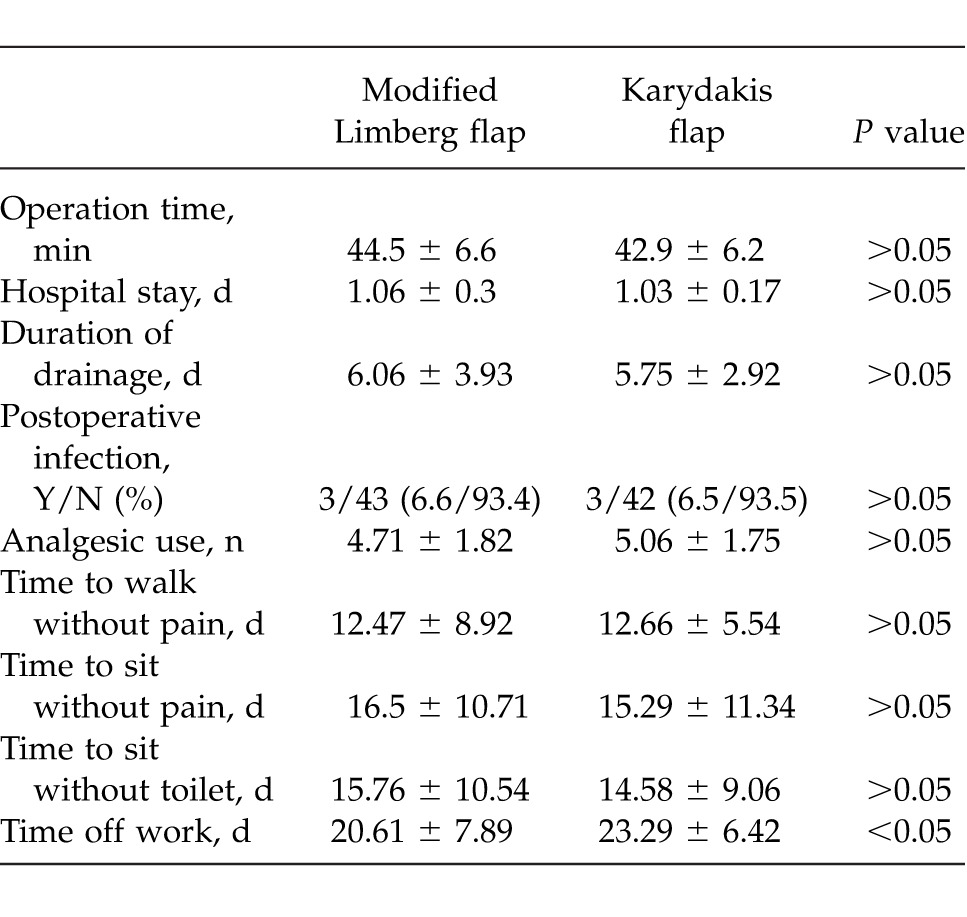
Average postoperative follow-up period was 26 months (range, 16–28 months). No significant difference was discovered between the groups in terms of operation duration (MLF: 44.57 ± 6.65 minutes, KF: 42.98 ± 6.28 minutes; P > 0.05). There was no significant difference between the groups regarding average hospital stay period and postoperative analgesic need. Three patients in the MLF group (6.6%) and 3 in the KF (6.5%) had postoperative wound infection; there was no significant difference between the groups (P > 0.05). No significant difference was found between the groups with respect to start time of painless sitting, painless walking time, and painless toilet-sitting time (P > 0.05). The modified Limberg flap group had shorter return-to-work or school time compared with the KF group (20.61 ± 7.89 day, 23.29 ± 6.42, respectively; P < 0.05; Table 4).
Table 4.
Short-term results after the three procedures
Considering cosmetic results, patients in the KF group had a higher VAS score compared with those in MLF (VAS score: MLF: 5.45 ± 1.77, KF: 7.12 ± 1.28; P < 0.05). Regarding recurrence rates, no significant difference was found between the groups (Table 5).
Table 5.
Long-term results after the three procedures
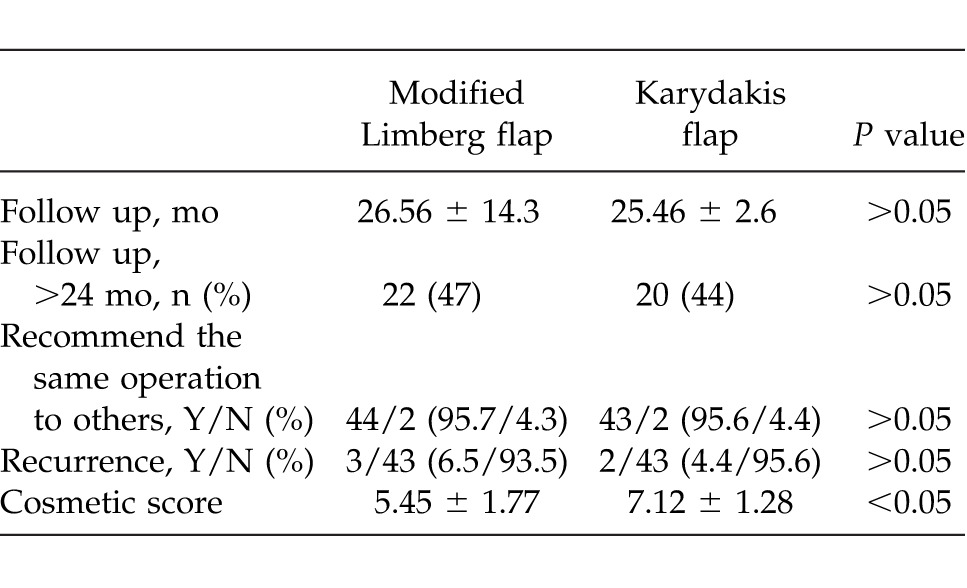
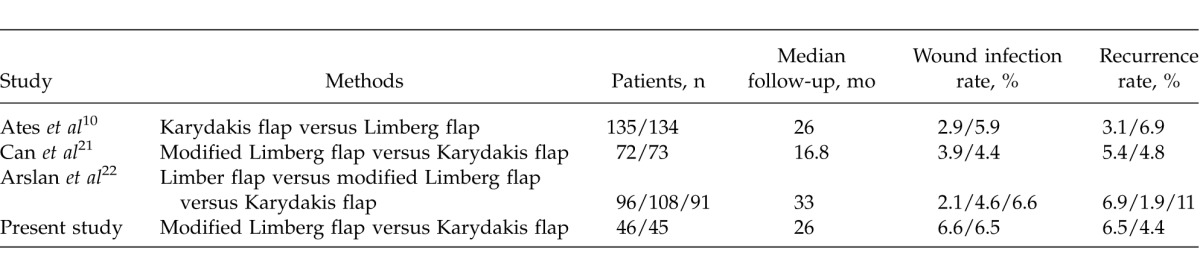
Table 6.
Results of different studies treatment techniques for PSD
Discussion
Pilonidal sinus is a widespread disease usually found with young population. It often occurs in the sacrococcygeal region. Its etiology has not been clearly explained yet. Harlak et al compared 587 pilonidal sinus patients with 2780 healthy individuals, and discovered that the time spent sitting during the day, hair density, and bathing frequency are risk factors for pilonidal sinus. It is observed in this present study that 72% of the patients with pilonidal sinus have all of these 3 risk factors.8
Although several surgical methods have been defined for PSD treatment, no golden standard method is available yet. Complications that may occur as a result of surgical treatment may sometimes appear with more morbidity than the disease itself. There is still a search for optimal treatment method due to labor loss and high recurrence rate, as it affects young adult males. Extensive surgical excision is a commonly used technique in PSD treatment. The real controversy comes in about the next stage.14
Marsupialization has been used in surgical pilonidal sinus treatment for many years. Marsupializing the edges of the wound is done to ensure reduction in wound size and shorten healing time. Nevertheless, it is noteworthy to mention that healing time of the patients who received marsupialization lasts up to 4 to 5 weeks, and a significant number of wound dressings is required as a result.15 The disadvantage led the surgeons to quit the practice of leaving the wound open, and adopt operations such as excision + primary repair. These operations are known to ensure shorter return-to-work time and quick-healing compared with marsupialization, yet it is reported that they have high complication rates (wound disintegration, infection, pain).16,17 Although a high wound infection rate is often linked in literature to the fact that suture line is located at the midline,18 it could also be linked to the application of numerous subcutaneous sutures, placed in order to avoid possible separations in the suture line, and the tissue perfusion that decreases due to tension. This led the surgeons to flap operations that would flatten the natal cleft, keep the suture line away from the natal cleft, and reduce the tension. In this study, we compared MLF and KF operations that are often used in recent times in order to avoid problems related with natal cleft.
Following PSD surgical treatment, early postoperative morbidity and comfort is an important concern. The most notable early postoperative problem is wound infection. Samer et al carried out a study on 120 patients where they found that the modified Karydakis flap (MKF) group (n = 60) had 2% wound infection, while the MLF group (n = 60) had 3%; and no significant difference was found between the groups.19 The study carried out by Can et al on 145 patients did not discover significant differences between the two groups (MLF group, n = 72; KF group, n = 73) in terms of wound infection, collection, wound disintegration, and total surgical area complications considering early postop findings.20 The study by Aslan et al carried out on 295 patients (LF group, n = 96; MLF group, n = 108; KF group, n = 91) reported that seroma, partial wound disintegration, and maceration rate were significantly higher than the other 2 groups (seroma: 5.2, 7.4, 19.8%; partial wound dehiscence: 2.1, 3.7, 15.4%; maceration: 1, 3.7, 11%, respectively). Same study found no significant difference between the groups in terms of wound infection.21 The present study did not discover any significant difference between the groups in terms of wound infection, which is in line with the literature.
Many studies in the literature analyzed early postop results of surgical PSD treatment. Karaca et al carried out a prospective randomized study on 81 patients (MLF, n = 46; MKF, n = 35) where they found that MLF operations are superior to MKF operations in terms of postoperative pain, time of painless sitting on chair and time of painless sitting on armchair. The same study further found no significant difference between the groups in terms of full healing time.22 In their prospective randomized study, Ertan et al found that Limberg flap is advantageous compared with primary repair in terms of painless walking and return-to-work time; whereas they did not find any significant difference between the groups in terms of painless toilet-sitting time and hospital stay.18 In their prospective randomized study on 269 patients, Ates et al found that Limberg flap is superior to Karydakis flap in terms of operation time and hospital stay time; on the other hand they did not find any significant difference between the groups in terms of time of return to normal activity, and postop pain.10 Muzi et al discovered in their study that tension-free primary repair shortened hospital stay time, while it was not different from Limberg flap in terms of return-to-work time. The same study found tension-free primary repair to be more favorable in terms of postoperative pain and cost.23 Our study found that return-to-work or -school time was shorter among the MLF group, while it showed no significant difference between the groups in terms of patient comfort in the early postoperative period.
As PSD operations may cause extensive tissue defects, cosmetic condition gains significance for the patient while considering the effectiveness of the operations. The fact that in Limberg flap operations, extensive tissue excision and suture lines extending to the lateral from medial are involved may be regarded disadvantageous in terms of cosmetic appearance. Ates et al compared Limberg flap and Karydakis flap operations in their 269-case prospective randomized study in terms of cosmetics using VAS score. This study found VAS score to be 7.08 ± 1.75 in the Karydakis group, and to be 3.16 ± 1.40 in the Limberg group.10 Our study found the MLF operation to be cosmetically superior to KF (VAS score: 5.45 ± 1.77 and 7.12 ± 1.28, respectively).
Recurrence after pilonidal sinus surgery is not a rare case, and many patients may need multiple operations. These recurrences often appear in the first 3 years.24 If a recurrence appears in the first year, this is called early recurrence, and usually results from postoperative wound infections or incomplete excision. In their study, Arslan et al reported that the appearance of seroma, hematoma, or wound infection in the early period increases the risk of recurrence of the disease.21 The same study found recurrence rates in the KF flap group to be significantly higher than those in the MLF and LF groups (11, 1.9, 6.3%, respectively). Studies that involve similar surgeries did not report significant difference among groups with regard to recurrence rates.10,19,20 Our study did not find any significant difference between the groups with respect to recurrence.
Conclusion
In this prospective randomized study, where we compare two widely used surgical methods in recent times, no significant difference was found between the surgical techniques used in terms of early period patient comfort and recurrence risk. We believe that both methods can be safely used in PSD treatment, although MLF procedure achieves shorter return-to-work time, while KF procedure provides better cosmetic results.
Acknowledgments
This study has not been funded. Authors declared no conflicts of interests.
References
- 1.Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K. Primary closure techniques in chronic pilonidal sinus: a survey of the result of different surgical approaches. Dis Colon Rectum. 2002;45(11):1458–1462. doi: 10.1007/s10350-004-6451-2. [DOI] [PubMed] [Google Scholar]
- 2.Mayo OH. Observations on Injuries and Diseases of the Rectum. London, England: Burgess and Hill;; 1833. pp. 45–46. [Google Scholar]
- 3.Al-Khamis A, McCallum I, King PM, Bruce J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev. 2010;(1):CD006213 doi: 10.1002/14651858.CD006213.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akinci OF, Bozer M, Uzunköy A, Düzgün SA, Coşkun A. Incidence and etiological factors in pilonidal sinus among Turkish soldiers. Eur J Surg. 1999;165(4):339–342. doi: 10.1080/110241599750006875. [DOI] [PubMed] [Google Scholar]
- 5.Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. ANZ J Surg. 1992;62(5):385–389. doi: 10.1111/j.1445-2197.1992.tb07208.x. [DOI] [PubMed] [Google Scholar]
- 6.Bascom J. Pilonidal disease: origin from follicles of hairs and results of follicle removal as treatment. Surgery. 1980;87(5):567–572. [PubMed] [Google Scholar]
- 7.Humphries AE, Duncan JE. Evaluation and management of pilonidal disease. Surg Clin North Am. 2010;90(1):113–124. doi: 10.1016/j.suc.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Harlak A, Mentes O, Kilic S, Coskun K, Duman K, Yilmaz F. Sacrococcygeal pilonidal disease: analysis of previously proposed risk factors. Clinics. 2010;65(2):125–131. doi: 10.1590/S1807-59322010000200002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aldemir M, Kara IH, Erten G, Taçyildiz I. Effectiveness of collagenase in the treatment of sacrococcygeal pilonidal sinus disease. Surg Today. 2003;33(2):106–109. doi: 10.1007/s005950300022. [DOI] [PubMed] [Google Scholar]
- 10.Ates M, Dirican A, Sarac M, Aslan A, Colak C. Short and long-term results of the Karydakis flap versus the Limberg flap for treating pilonidal sinus disease: a prospective randomized study. Am J Surg. 2011;202(5):568–573. doi: 10.1016/j.amjsurg.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 11.Gurer A, Gomceli I, Ozdogan M, Ozlem N, Sozen S, Aydin R. Is routine cavity drainage necessary in Karydakis flap operation? A prospective, randomized trial. Dis Colon Rectum. 2005;48(9):1797–1799. doi: 10.1007/s10350-005-0108-7. [DOI] [PubMed] [Google Scholar]
- 12.Ersoy E, Devay AO, Aktimur R, Doganay B, Ozdoğan M, Gündoğdu RH. Comparison of the short-term results after Limberg and Karydakis procedures for pilonidal disease: randomized prospective analysis of 100 patients. Colorectal Dis. 2009;11(7):705–710. doi: 10.1111/j.1463-1318.2008.01646.x. [DOI] [PubMed] [Google Scholar]
- 13.Mentes BB, Leventoglu S, Cihan A, Tatlicioglu E, Akin M, Oguz M. Modified Limberg transposition flap for sacrococcygeal pilonidal sinus. Surg Today. 2004;34(5):419–423. doi: 10.1007/s00595-003-2725-x. [DOI] [PubMed] [Google Scholar]
- 14.Corman ML. Colon and Rectal Surgery. 2nd ed. Philadelphia, PA: Lippincott;; 1989. pp. 297–304. [Google Scholar]
- 15.Mentes O, Bagci M, Bilgin T, Coskun I, Ozgul O, Ozdemir M. Management of pilonidal sinus disease with oblique excision and primary closure: Result of 493 patients. Dis Colon Rectum. 2005;49(1):104–108. doi: 10.1007/s10350-005-0226-2. [DOI] [PubMed] [Google Scholar]
- 16.Schoeller T, Wechselberger G, Otto A, Papp C. Definite surgical treatment of complicated recurrent pilonidal disease with a modified fasciocutaneous V-Y advancement flap. Surgery. 1997;121(3):258–263. doi: 10.1016/s0039-6060(97)90354-8. [DOI] [PubMed] [Google Scholar]
- 17.Ertan T, Koc M, Gocmen E, Aslar K, Keksek M, Kilic M. Does technique alter quality of life after pilonidal sinus surgery? Am J Surg. 2005;190(3):388–392. doi: 10.1016/j.amjsurg.2004.08.068. [DOI] [PubMed] [Google Scholar]
- 18.Akin M, Leventoglu S, Mentes BB, Bostanci H, Gokbayir H, Kilic K, et al. Comparison of the classic Limberg flap and modified Limberg flap in the treatment of pilonidal sinus disease: a retrospective analysis of 416 patients. Surg Today. 2010;40(8):757–762. doi: 10.1007/s00595-008-4098-7. [DOI] [PubMed] [Google Scholar]
- 19.Bessa SS. Comparison of short-term results between the modified Karydakis flap and the modified Limberg flap in the management of pilonidal sinus disease: a randomized controlled study. Dis Colon Rectum. 2013;56(4):491–498. doi: 10.1097/DCR.0b013e31828006f7. [DOI] [PubMed] [Google Scholar]
- 20.Can MF, Sevinc MM, Hancerliogullari O, Yilmaz M, Yagci G. Multicenter prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg. 2010;200(3):318–327. doi: 10.1016/j.amjsurg.2009.08.042. [DOI] [PubMed] [Google Scholar]
- 21.Arslan K. Said Kokcam S, Koksal H, Turan E, Atay A, Dogru O. Which flap method should be preferred for the treatment of pilonidal sinus? A prospective randomized study. Tech Coloproctol. 2014;18(1):29–37. doi: 10.1007/s10151-013-0982-2. [DOI] [PubMed] [Google Scholar]
- 22.Karaca T, Yoldaş O, Bilgin BÇ, Ozer S, Yoldaş S, Karaca NG. Comparison of short-term results of modified Karydakis flap and modified Limberg flap for pilonidal sinus surgery. Int J Surg. 2012;10(10):601–606. doi: 10.1016/j.ijsu.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Muzi MG, Milito G, Cadeddu F, Nigro C, Andreoli F, Amabile D, et al. Randomized comparison of Limberg flap versus modified primary closure for the treatment of pilonidal disease. Am J Surg. 2010;200(1):9–14. doi: 10.1016/j.amjsurg.2009.05.036. [DOI] [PubMed] [Google Scholar]
- 24.Allen-Mersh TG. Pilonidal sinus: finding the right track for treatment. Br J Surg. 1990;77(2):123–132. doi: 10.1002/bjs.1800770203. [DOI] [PubMed] [Google Scholar]