Abstract
Improved treatments for pancreatic cancer remain a clinical imperative. Sabutoclax, a small molecule BH3 mimetic, inhibits the function of anti-apoptotic Bcl-2 proteins. Minocycline, a synthetic tetracycline, displays antitumor activity. Here we offer evidence of the combinatorial antitumor potency of these agents in several preclinical models of pancreatic cancer. Sabutoclax induced growth arrest and apoptosis in pancreatic cancer cells and synergized with Minocycline to yield a robust mitochondria-mediated caspase-dependent cytotoxicity. This combinatorial property relied upon loss of phosphorylated Stat3 insofar as reintroduction of activated Stat3 rescued cells from toxicity. Tumor growth was inhibited potently in both immune-deficient and immune-competent models with evidence of extended survival. Overall, our results showed that that the combination of Sabutoclax and Minocycline was highly cytotoxic to pancreatic cancer cells and safely efficacious in vivo.
Keywords: Pancreatic Cancer, Sabutoclax, BH3 mimetic, Minocycline
Introduction
Pancreatic ductal adenocarcinoma (PDAC) is an extremely aggressive cancer that is predicted to cause almost 40,000 deaths in the US this year (NCI 2014). PDAC is fairly resistant to most standard therapies and results in a 5-year survival rate of about 4% (1). These dire statistics, combined with the fact that there have been minimal new therapies developed for PDAC over the last decade, highlight the need for new approaches to effectively treat this invariably fatal disease.
The aggressive nature and dismal prognosis of patients with pancreatic cancer results partly from the plethora of molecular changes that occur during PDAC development, one of which is overexpression of the anti-apoptotic proteins of the Bcl-2 family (2–5). Cancer cells exploit this overexpression to evade cell death and as a mechanism promoting resistance to diverse chemotherapeutic agents. Apoptosis reflects a balance between pro- and anti-apoptotic proteins within cells. The ability of a cancer cell to shift the balance toward survival promotes resistance to toxic factors (6).
Consequently, the anti-apoptotic Bcl-2 proteins have emerged as a novel therapeutic target. While multiple strategies have attempted to target these molecules, BH3 mimetics have shown significant promise. Pro-apoptotic or anti-apoptotic effects in cells arise, ultimately, as a consequence of physical interactions between anti- and pro-apoptotic Bcl-2 proteins (7,8). Based on modeling predictions of these interactions, small molecules have been developed that mimic the BH3 domain of pro-apoptotic proteins and bind to the anti-apoptotic proteins, thereby impeding their ability to inhibit apoptosis. These drugs represent a novel and exciting new strategy in cancer therapeutic development (6).
Sabutoclax (BI-97C1) is a novel Apogossypol derivative BH3 mimetic developed by Wei et al. (9–12). This compound binds to the Bcl-2 anti-apoptotic proteins Bcl-2, Mcl-1, Bcl-XL, and Bfl-1. It was originally identified based on its ability to bind Bcl-XL with low to submicromolar binding affinity (11). We have previously shown that Sabutoclax shows efficacy against prostate and colorectal cancers, two cancers that also overexpress anti-apoptotic Bcl-2 proteins (13,14). Minocycline is a synthetic tetracycline antibiotic that displays marginal activity against multiple cancers (15–19). However, less than stellar outcomes have diminished enthusiasm for using these drugs in cancer research. The marginal single agent effects of Minocycline against cancer may be due to the fact that it also impedes cell death in the face of toxicity or injury by inhibiting mitochondrial apoptosis and upregulation of Bcl-2 (20–22). In an attempt to develop a unique therapeutic strategy for PDAC, we hypothesized that Sabutoclax and Minocycline might show therapeutic efficacy against this disease when used in combination because of both the reliance of PDAC on the Bcl-2 proteins for survival as well as the theoretical ability of Sabutoclax to counteract the anti-apoptotic effects of Minocycline, thereby uncovering the true therapeutic potential of this previously overlooked drug.
Materials and Methods
Human Cell Lines
MIA PaCa-2, PANC-1, BxPC-3, AsPC-1, and HPNE cells were all obtained from the American Type Culture Collection (ATCC). LT2 cells were purchased from Millipore. MIA PaCa-2 and PANC-1 were maintained in DMEM plus 10% FBS. BxPC-3 and AsPC-1 cells were maintained in RMPI plus 10% FBS. HPNE and LT2 cells were maintained with media according to distributor’s instructions. Cell lines were expanded and cryopreserved at early passages and new vials were thawed out and used for experiments approximately every 3 months.
Creation of KPC Mouse Cell Lines
Cell lines were derived from the ascites of tumor bearing KPC mice. At the time of necropsy, ascitic fluid was collected from the mice and centrifuged to pellet tumor cells. The pellet was repeatedly washed in PBS and centrifuged before being resuspended in RPMI supplemented with 4% FBS and placed in culture. This media was used to maintain these cell lines.
Drugs and Drug Administration
For all in vitro studies, Sabutoclax (produced by Dr. Maurizio Pellecchia) was diluted in DMSO and Minocycline (Sigma) in PBS. For combination treatments, Sabutoclax and Minocycline were administered to cells simultaneously. zVAD-FMK (20 μM, Promega) was incubated with cells for 1 hour prior to treatment with Sabutoclax and Minocycline. Caspase 8 specific inhibitor, z-IETD-FMK (20 μM, BD Pharmingen) was also incubated with cells for 1 hour before treatment with Sabutoclax and Minocycline.
Proliferation Studies
5 × 103 cells were plated in 96-well plates and treated with Sabutoclax and/or Minocycline for 72 hours. Proliferation was assessed by MTT assay as previously described (23). All data were normalized to the control.
Cell Death Assays
For Trypan Blue exclusion assays, 5 × 105 cells were plated in 6-cm dishes, treated as indicated for 48 hours, and then assayed as previously described (24).
LDH Cytotoxicity Assays
5 × 105 cells were plated in 6-cm dishes and treated as described. After 48 hours, media was collected from each dish and assayed according to the manufacturer’s instructions (Cytotoxicity Detection Kit (LDH), Roche).
Cell Cycle Studies
1 × 106 cells were plated in 10-cm dishes and cultured in normal media with 0.5% serum for 48 hours. Cells for the zero hour time point were collected and fixed at this point. Remaining plates were kept in either normal media or 750 nM Sabutoclax for indicated time points. Once all cells were collected and fixed, they were incubated with propidium iodide and FACS was used for cell cycle analysis. Cell cycle studies were done as previously described (25).
Colony Forming Assay
MIA PaCa-2 cells were treated with Sabutoclax (500 nM), Minocycline (50 μM), or a combination of both for 24 hours. Cells were then trypsinized and 1,000 cells were plated into 6-cm plates in triplicate. Cells were allowed to grow and form colonies in normal media for approximately 14 days. Plates were then fixed and stained with Giemsa.
Western Blotting
5 × 105 cells were plated in 6-cm dishes and treated as described. After 48 hours, whole cell lysates were prepared and western blotting analysis was carried out as previously described (24). Primary antibodies used for these studies are PARP (1:1,000), Stat3 (1:1,000), pStat3 (1:750), Mcl-1 (1:1,000), Survivin (1:750), p21 (1:750), p27 (1:1,000), Cyclin D1(1:500), Caspase 2 (1:1,000), Caspase 3 (1:1,000), Caspase 6 (1:1,000), Caspase 7 (1:1,000), Caspase 8 (1:1,000), Caspase 10 (1:1,000), Caspase 12 (1:1,000), AIF (1:1,000), pRB (1:750) (Cell Signaling), EF1-α (1:1,000, Millipore), and Actin (1:5,000, Sigma). Densitometric analysis was done using ImageJ software (National Institutes of Health).
Constructs and Transfection
Stat3Y705F Clones
MIA PaCa-2 or PANC-1 cells were transfected with a plasmid expressing a mutated form of Stat3 (pRc.CMV.Stat3Y705F, Addgene). Clones were selected with Neomycin for approximately 2 weeks and then picked and grown up individually. Whole cell lysates were made and samples were used for western blotting to characterize clones.
Luciferase Clones
MIA PaCa-2 or PANC-1 cells were transfected with pGL3.CMV.luc (Promega). Transfections used Lipofectamine 2000 (Invitrogen, Carlsbad, CA) according to the manufacturer's protocol.
Immunohistochemistry
Tumors were fixed in formalin, embedded in paraffin, and sectioned for staining. Staining was done as previously described (26) with anti-p-Stat3 (1:100, Abcam), anti-PCNA (1:100, Abcam), and anti-Mcl-1 (1:100, Abcam) per the manufacturer’s instructions.
Combination Index Calculation
Combination index (CI) values were determined for the combination of Sabutoclax and Minocycline in MIA PaCa-2 cells. Values were calculated using CompuSyn software (ComboSyn, Inc.) according to the Chou-Talalay method.
In vivo studies
Subcutaneous Xenograft Studies
5 × 106 MIA PaCa-2 and 3.5 × 106 PANC-1 cells were used to establish bilateral subcutaneous tumors on the flanks of 8–10 week old male athymic nude mice. Studies were done as previously described (13). Treatment began when tumors reached ~100-mm3. Sabutoclax was given at a dose of 1 mg/kg for both studies and was dissolved in a 10:10:80 solution of 100% ethanol:Cremophor:PBS. Minocycline was given at a dose of 20 mg/kg and dissolved in PBS. Both drugs were given via IP injection 3 times per week. n = 5 mice/group
Quasi-Orthotopic Xenograft Studies
Low Tumor Burden
In this model, we injected 1 × 106 MIA PaCa-2-luc cells IP into 8–10 week old male athymic nude mice. We allowed 1 week for tumor cells to attach and grow and then began treatment with PBS, 1 mg/kg Sabutoclax, 20 mg/kg Minocycline, or both Sabutoclax and Minocycline. Sabutoclax and Minocycline were given via IP injection 3x/week. Mice were imaged by BLI at 3 weeks after treatment was initiated and then sacrificed at 4 weeks. At time of sacrifice, mice were imaged pre-necropsy. After necropsy, organs from a few mice/group were imaged to determine tumor specificity. n = 7 mice/group
High Tumor Burden
5 × 106 MIA PaCa-2-luc cells were injected IP into 8–10 week old male athymic nude mice. We allowed 1 week for tumor cells to attach and grow and then began treatment with PBS, 1 mg/kg Sabutoclax, 20 mg/kg Minocycline, or both Sabutoclax and Minocycline. Sabutoclax and Minocycline were given via IP injection 3x/week. Mice were sacrificed at 4 weeks. The pancreas from each mouse was removed and weighed during necropsy. n = 10 mice/group
Syngeneic Mouse Study
KPC (Pdx-1-Cre/K-rasLSL-G12D/p53flox/wt) mouse cell line 48 was injected subcutaneously into both flanks of non-tumorigenic KPC mice (Pdx-1-Cre negative/K-rasLSL-G12D/p53flox/wt). Tumors were given 1 week to establish before treatment was initiated. Mice were treated with PBS, 1.5 mg/kg Sabutoclax, 10 mg/kg Minocycline, or both Sabutoclax and Minocycline. Sabutoclax was dissolved in a 10:10:80 solution of 100% ethanol:Cremophor:PBS. Minocycline was dissolved in PBS. Mice were treated with Sabutoclax, Minocycline, or both drugs every 2–3 days via IP injection for a total of 6 injections. Tumors were measured with calipers to obtain tumor volumes. n = 5 mice/group
Survival Study
KPC mice (Pdx-1-Cre/K-rasLSL-G12D/p53flox/flox) were started on a Sabutoclax and Minocycline treatment regimen at 1 month of age. Mice were treated with a combination of Sabutoclax (1.5 mg/kg) and Minocycline (10 mg/kg) via IP injection 3 times per week. Mice were kept on this treatment until reaching a moribund status. At this point, mice were sacrificed and necropsied. Tumor sections were obtained from these mice and subjected to immunohistochemistry. n = 12 mice (control group); n = 10 mice (Sabutoclax + Minocycline group).
Statistical Analysis
The data presented are the mean ± S.D. of the values from three independent experiments. For in vivo studies, data shown are the mean ± 95% confidence interval. Significance was determined using the Student’s t-test. p<0.05 was considered statistically significant.
Results
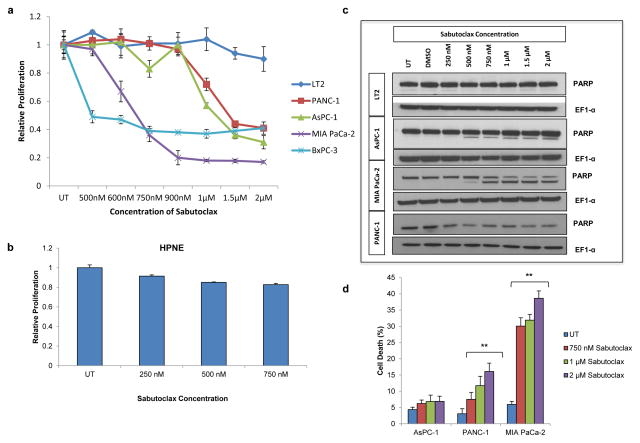
Sabutoclax inhibits cell growth and induces apoptosis in PDAC
Multiple PDAC cell lines and two normal pancreatic cell lines were treated with increasing doses of Sabutoclax and assessed for effects on proliferation. The normal cell lines displayed little change in cell growth (Fig. 1a–b), while all of the cancer cell lines were growth inhibited. Interestingly, the sensitivity of the cancer cell lines varied, with some being very sensitive to Sabutoclax (MIA PaCa-2) and others more resistant (AsPC-1) (Fig. 1a). The ability of Sabutoclax to induce cell death and apoptosis was also evaluated (Fig. 1c–d). Again, MIA PaCa-2 was most sensitive to Sabutoclax. However, despite not showing a potent cell death phenotype, cells like AsPC-1 still showed profound growth inhibition following Sabutoclax treatment. Furthermore, Sabutoclax displayed greater growth inhibitory effects than the BH3 mimetic ABT-737 (Supplementary Fig. 1).
Figure 1.
Sabutoclax inhibits cell growth and induces apoptosis in pancreatic cancer cells. (a) Sabutoclax dose response curves via MTT proliferation assays in pancreatic fibroblast cell line, LT2, and pancreatic cancer cell lines PANC-1, AsPC-1, MIA PaCa-2, and BxPC-3. Experiments done in triplicate and independently repeated three times. (b) Sabutoclax dose response curve via MTT proliferation assay in pancreatic epithelial-derived cell line, HPNE. Experiments done in triplicate and independently repeated three times. (c) Western blotting for PARP and EF1-α (loading control). Data representative of three independent experiments. (d) Trypan Blue assays in AsPC-1, PANC-1, and MIA PaCa-2. **p<0.001 as compared to UT sample. Experiments done in triplicate and independently repeated three times.
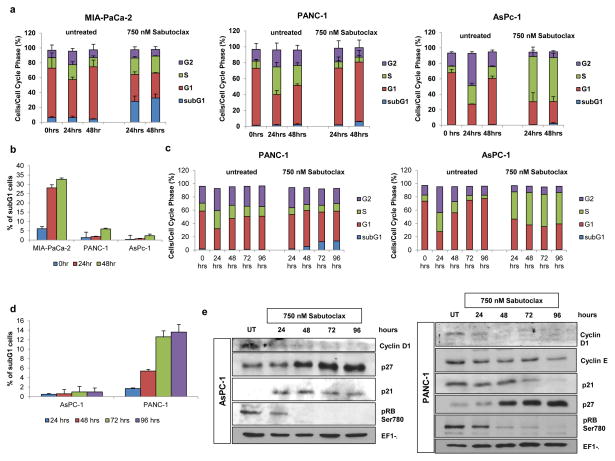
Sabutoclax induces G1-S phase arrest
Sabutoclax induces cell death in MIA PaCa-2 cells, without promoting potent cell death in either AsPC-1 or PANC-1. Despite this, there is still a dramatic reduction in cell growth after drug treatment. To interrogate the mechanism of growth suppression in these cell lines, we performed cell cycle analysis (Fig. 2a) (Supplementary Fig. 2a-c). Sabutoclax increased MIA PaCa-2 subG1 phase after 24 and 48 hours (Fig. 2b), without affecting cell cycle, which is consistent with our previous data. In PANC-1 and AsPC-1, however, potent G1-S phase cell cycle arrest was evident. These experiments only evaluated cells up to 48 hours post-treatment. A second set of experiments also included 72 and 96 hours time points (Fig. 2c) (Supplementary Fig. 2d-e) to determine if longer drug incubations promoted cell cycle arrest or resulted in a switch to apoptosis. In AsPC-1, the G1-S phase arrest was sustained throughout all time points evaluated. However, at 72 and 96 hours, PANC-1 showed an increase in the subG1 population of cells, indicating that there is an initial cell cycle arrest in these cells that later switches to apoptosis (Fig. 2d). These results emphasize the complexity of responses observed in PDAC to a single agent, such as Sabutoclax.
Figure 2.
Sabutoclax causes a G1-S phase cell cycle arrest. (a,c) Cell cycle analysis. (b,d) Percentage of cells analyzed in the subG1 phase, indicating cell death. E. Western blotting of whole cell lysates for Cyclin D1, Cyclin E, p27, p21, and phospho-Rb. EF1-α was used as a loading control. Data representative of three independent experiments.
Evaluation of cell cycle protein markers (Fig. 2e) confirmed decreased Cyclin D1 and increased p27 expression in AsPC-1 and PANC-1 cells. Additionally, there was a dramatic decrease in levels of phosphorylated Rb (Ser780). This corresponded with the observed G1-S phase arrest. Interestingly, while levels of p21 in AsPC-1 cells increased, p21 levels decreased in PANC-1 cells. This difference may account for the switch from growth arrest to apoptosis in these cells (27,28).
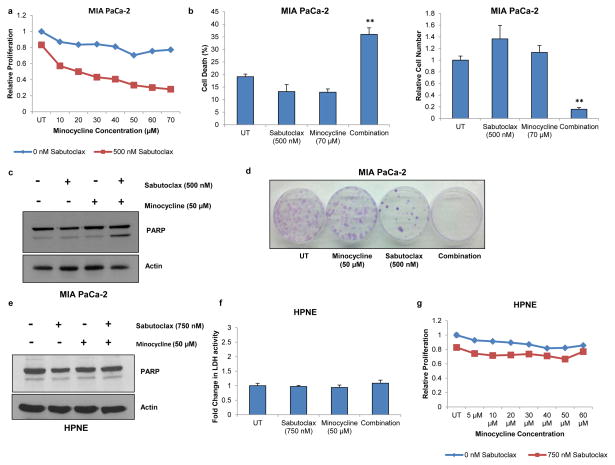
Sabutoclax synergizes with synthetic tetracycline, Minocycline, in PDAC
It is now almost axiomatic that to successfully combat cancer multiple targeting strategies may be necessary. Cancer cells develop resistance to initially effective treatments and acquire avoidance mechanisms preventing toxicity. Accordingly, combinatorial approaches attacking multiple pathways in a cancer cell can increase drug efficacy, reduce toxicity, and increase the time to resistance. Based on this concept, we sought to identify an agent that would promote synergy when combined with Sabutoclax. Minocycline, a commonly used antibiotic, can negatively impact cancer growth and survival (15–19). Despite this, it paradoxically also protects cells in the face of an insult through inhibition of mitochondrial apoptosis and upregulation of Bcl-2 (20–22). For these reasons, we hypothesized that these drugs might work well in combination, given their cancer-selective toxicities as single agents and the potential of Sabutoclax to counteract the pro-survival effects of Minocycline.
Minocycline is fairly nontoxic to several PDAC cells (MIA PaCa-2 and PANC-1), but is inhibitory in others (AsPC-1 and BxPC-3) (Supplementary Fig. 3). In resistant cells, the combination of Sabutoclax and Minocycline is very toxic. It significantly reduces cell proliferation and overall cell number, and induces cell death to a much greater extent than either agent alone in MIA PaCa-2 (Fig. 3a–d) and PANC-1 cells (Supplementary Fig. 4). Combination index values also demonstrate synergy between these two compounds (Supplementary Fig. 5). It also promotes increased apoptosis and reduced colony formation in PDAC cells. Importantly, this synergistic effect is not evident in the normal cell line, HPNE (Fig. 3e–g).
Figure 3.
The combination of Sabutoclax and Minocycline produce synergistic cytotoxic effects. (a) MTT proliferation assay in MIA PaCa-2 cells 72 hours post treatment. Experiments done in triplicate and independently repeated three times. (b) Trypan blue assays evaluating cell death and cell numbers in MIA PaCa-2 cells 48 hours post treatment. **p<0.0001. Experiments done in triplicate and independently repeated three times. (c) Western blotting of whole cell lysates for PARP expression in MIA PaCa-2 cells 48 hours post treatment. Actin was used as a loading control. Data representative of three independent experiments. (d) Colony forming assay in MIA PaCa-2 cells. Experiments done in triplicate and independently repeated three times. (e) Western blotting for PARP using whole cell lysates from HPNE cells 48 hours post treatment. Data representative of three independent experiments. (f) MTT proliferation assays in HPNE cells 72 hours post treatment. Experiments done in triplicate and independently repeated three times. (g) LDH cytotoxicity assay in pancreatic epithelial cell line, HPNE. Experiments done in triplicate and independently repeated three times.
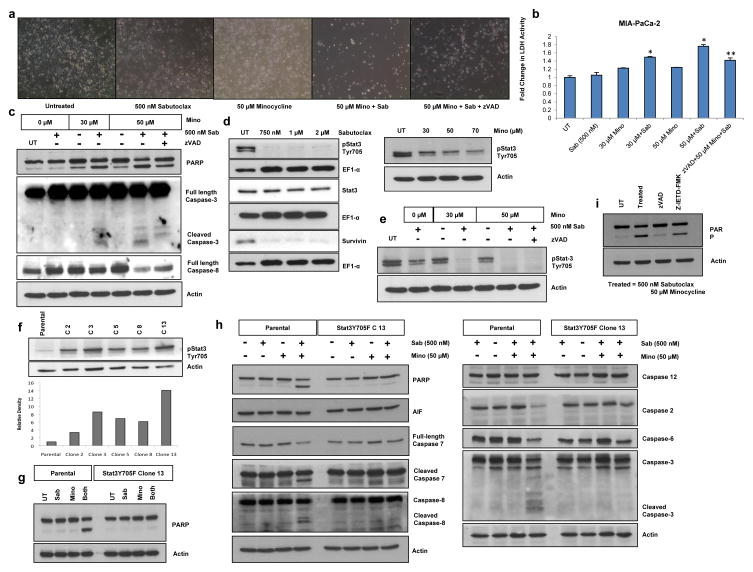
We next sought to define the mechanism underlying this synergy. The combination of subtoxic doses of Sabutoclax and Minocycline induced potent cell death that was partially abrogated by pretreatment with zVAD, indicating that this toxic effect is, in part, caspase-mediated. This rescue phenotype is evident in the morphology of treated cells (Fig. 4a; Supplementary Fig. 4c) and through reductions in LDH activity, indicating lower levels of cell death (Fig. 4b; Supplementary Fig. 4b). Furthermore, PARP cleavage was reduced in cells pretreated with zVAD (Fig. 4c; Supplementary Fig. 4a). When specific caspases were evaluated, the combination treatment showed caspase-3 cleavage and loss of full-length caspase-8, which was not found in zVAD-treated samples.
Figure 4.
The cytotoxicity induced by Sabutoclax and Minocycline is caspase-dependent and dependent upon loss of Stat3 activation. (a) Phase contrast images showing MIA PaCa-2 cellular morphology 48 hours post Sabutoclax and/or Minocycline treatment. Experiments done in triplicate and independently repeated three times. (b) Media from plates photographed in panel A was collected and used for LDH activity assays. *p<0.005 as compared to single drug treated samples. **p=0.006 as compared to 50 μM Minocycline + Sabutoclax-treated samples. Experiments done in triplicate and independently repeated three times. (c) Western blotting of whole cell lysates for expression of PARP, caspase-3, and caspase-8. Actin was used as a loading control. Data representative of three independent experiments. (d) Western blotting of whole cell lysates for pStat3 Tyr705, Stat3, Survivin, Actin (loading control) and EF1-α (loading control) 48 hours post treatment. Data representative of three independent experiments. (e) Western blotting of whole cell lysates for pStat3 Tyr705 48 hours post treatment. Actin was used as a loading control. Cells were incubated with zVAD for 1 hour prior to Sabutoclax and Minocycline treatment. Data representative of three independent experiments. (f) Western blotting of whole cell lysates from MIA-PaCa-2-Stat3Y705F stable clones for pStat3 Tyr705. Actin was used as a loading control. Graph below blot shows quantification. Data representative of three independent experiments. (g) Western blotting of whole cell lysates for PARP in parental MIA Paca-2 and Stat3Y705F stable clone 13. Actin was used as a loading control. Sab = 500 nM Sabutoclax, Mino = 50 μM Minocycline. Data representative of three independent experiments. (h) Western blotting of whole cell lysates 48 post treatment for PARP, AIF, Caspase-7, Caspase-8, Caspase-12, Caspase-2, Caspase-6, and Caspase-3. Actin was used as a loading control. Data representative of three independent experiments. (i) Western blotting 48 hours post treatment for PARP and Actin (loading control). Cells were incubated with zVAD or z-IETD-FMK for 1 hour prior to treatment with Sabutoclax and Minocycline. Data representative of three independent experiments.
The cytotoxic effect of Sabutoclax and Minocycline is Stat3-dependent
Stat3 activation is clinically relevant for PDAC as constitutive activation of Stat3 has been reported in 30–100% of human tumor specimens, and is crucial for PDAC initiation, progression, and maintenance (29). Sabutoclax treatment resulted in a potent loss of Stat3 phosphorylation (Tyr 705), as well as a loss of downstream Stat3 targets, such as survivin (Fig. 4d). Minocycline alone induced similar changes (Fig. 4d). Subtoxic doses of each drug lowered Stat3 activation, but the combination of both drugs almost completely eliminated pStat3 expression (Fig. 4e). To determine whether this would affect the cytotoxicity of the combination, we created MIA PaCa-2 clones stably expressing an activated Stat3 mutant, Stat3 Y705F, e.g. C 13 (Fig. 4f). As compared to the parental cell line, C 13 showed enhanced resistance to combination treatment (Fig. 4g). A similar elevated resistance was observed in other Stat3 Y705F overexpressing MIA PaCa-2 clones (data not shown). Because pretreatment with zVAD partially rescued cells from Sabutoclax and Minocycline-induced cell death, we evaluated expression of a variety of caspases to determine their potential involvement not only in death induced by the combination, but which ones might be affected in C 13 cells (Figure 4h). In parental MIA PaCa-2 cells, caspases 3, 7, and 8 were cleaved. Loss of full-length caspases 2 and 6 was evident, whereas AIF, caspase 12, and caspase 10 (caspase 10 data not shown) were not significantly altered. In C 13 cells, however, we did not see any significant changes in any caspase examined, supporting the observation that loss of Stat3 activation is necessary for caspase-dependent cell death by Sabutoclax and Minocycline. We also created stable cell lines overexpressing Stat3 Y705F in PANC-1 cells. Similar to what we observed in MIA PaCa-2 cells, constitutive Stat3 activation in these clones protected them from cytotoxicity induced by the combination of Sabutoclax and Minocycline (Supplementary Fig. 6b–c).
Caspase-8 activation is an integral part of the extrinsic pathway of apoptosis. However, it can also be activated independent of this pathway by other caspases (30). To determine if caspase-8 involvement was due to extrinsic pathway activation or downstream intrinsic pathway activation, we used Z-IETD-FMK to specifically inhibit caspase 8 before drug treatment. Unlike the pan caspase inhibitor, zVAD, pretreatment with Z-IETD-FMK did not protect cells from Sabutoclax and Minocycline-induced cell death (Fig. 4i) (Supplementary Fig. 6a). This indicates that caspase-8 activation is dispensable for Sabutoclax and Minocycline-induced cell death and is most likely a secondary effect of other caspases. Therefore, our data support the hypothesis that Sabutoclax and Minocycline induce a cytotoxic phenotype through activation of the intrinsic pathway of apoptosis.
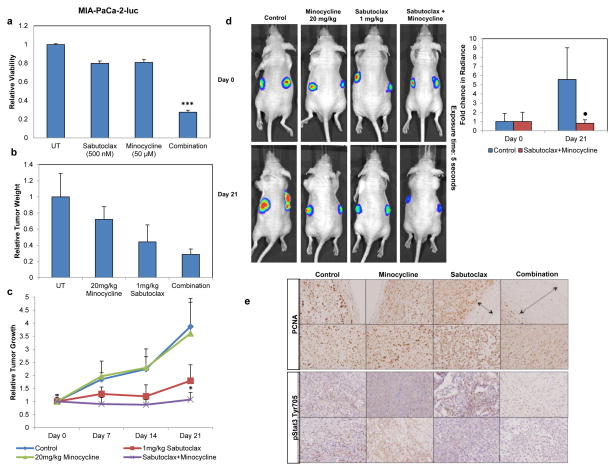
Sabutoclax alone reduces tumor growth in a xenograft model of pancreatic cancer and this effect is enhanced with the addition of Minocycline
Luciferase-expressing MIA PaCa-2 cells, displaying a similar phenotype as parental cells (Fig. 5a), were established as subcutaneous xenografts in athymic nude mice and were treated with Sabutoclax (1 mg/kg), Minocycline (20 mg/kg), or both agents. Minocycline treatment alone showed minimal effects, while Sabutoclax alone showed greater reductions in tumor weight and (Fig. 5b–c). Despite this, animals treated with a combination of Sabutoclax and Minocycline showed a synergistic reduction in tumor growth, with a significantly smaller tumor growth rate, even as compared to Sabutoclax alone (Fig. 5c). This was confirmed with bioluminescence imaging (BLI) (Fig. 5d). A similar experiment was conducted using PANC-1-luc cells resulting in the same trend, with the combination group showing significant inhibition of tumor growth (Supplementary Fig. 7).
Figure 5.
Sabutoclax reduces tumor growth in a subcutaneous xenograft model and is enhanced by the addition of Minocycline. n= 5 mice/group. (a) MTT proliferation assay of MIA PaCa-2 cells stably expressing luciferase after treatment with Sabutoclax and/or Minocycline. ***p<0.0001. Experiments done in triplicate and independently repeated three times. (b) Tumor weight as normalized to the control animals at the end of the experience. (c) Tumor growth kinetics of MIA PaCa-2-luc cell subcutaneous tumors on the flanks of athymic mice. *p<0.04 as compared to all other groups. (d) Bioluminesence imaging (BLI) of tumors and image quantification. Exposure time = 5 seconds. (e) Tumors were fixed in formalin, embedded in paraffin, and sectioned for staining. Representative images of immunohistochemistry (IHC) stained with p-Stat3 Y705 and PCNA. Arrows in PCNA images show margin of negatively stained tumor area at the periphery of each tumor. Data representative of three independent experiments.
Immunohistochemistry of tumor sections (Fig. 5e) demonstrated higher intensity PCNA staining in control, Sabutoclax, and Minocycline-treated groups as compared to the combination-treated group. Furthermore, combination-treated tumors showed significantly less phosphorylated Stat3 expression, consistent with in vitro observations.
Quasi-orthotopic xenograft mouse model
While subcutaneous xenograft studies are useful in evaluating in vitro observations in an in vivo setting, flank tumors do not accurately mimic natural disease states. To study the effect of our drugs in a more natural setting, we used a quasi-orthotopic model of PDAC (31). We found that MIA PaCa-2-luc cells, when injected intraperitoneally, specifically homed to the pancreas, with the majority of tumors or tumor nodules found in this organ. Other locations in which we found tumors (liver, peritoneal lining) are common places for this cancer to metastasize and more closely mimic the clinical picture of this disease.
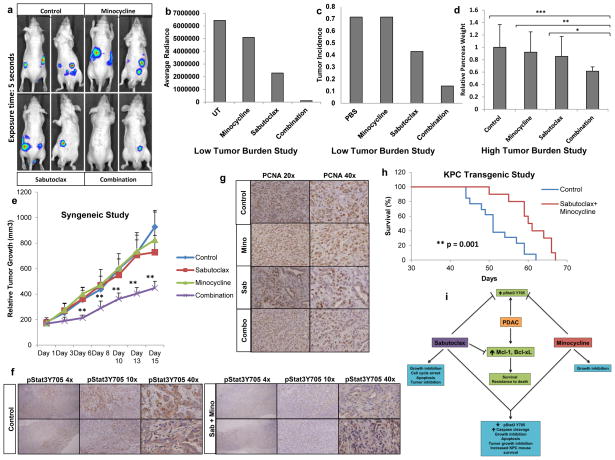
In an initial set of experiments, we injected 1 × 106 cells i.p. and allowed 1 week for tumor establishment before treating mice with Sabutoclax and Minocycline, alone or in combination. Consistent with our previous data, Minocycline as a single agent did not have any effect and mice presented similarly to control animals. Sabutoclax showed a potent single-agent effect, with fewer animals showing evidence of disease. The combination group showed even more promise (Fig. 6c), with only 1/7 mice showing tumors by BLI (Fig. 6a–b). Pancreas weight did not show significant differences, though the trend supported our other observations (data not shown).
Figure 6.
Sabutoclax and Minocycline reduce tumor growth in a quasi-orthotopic xenograft model, a syngeneic KPC model, and enhance survival in the KPC transgenic mouse model. (a) Low Tumor Burden study: BLI images of mice post treatment. Exposure time = 5 seconds. (b) Image quantification of panel A. (c) Tumor incidence in pancreas – measured by imaging and by gross examination of animals at necropsy. n= 7 mice/group. (d) High Tumor Burden study: pancreas weight at necropsy. Treatment groups normalized to the control. *p=0.03, **p=0.01, ***p=0.004. n= 10 mice/group(e) Syngeneic study: Tumor growth kinetics of control Pdx-1-Cre/K-rasLSL-G12D/p53flox/flox mice bearing subcutaneous Pdx-1-Cre/K-rasLSL-G12D/p53flox/wt–derived tumors. **p<0.01 as compared to all other groups. n= 5 mice/group. (f-g) IHC for PCNA and pStat3 Y705. Data representative of three independent experiments. (h) Kaplan-Meier survival curve for Pdx-1-Cre/K-rasLSL-G12D/p53flox/flox mice treated with Sabutoclax and Minocycline. *p=0.001. n = 12 mice (control group); n = 10 mice (Sabutoclax + Minocycline group). (i) Overview model showing therapeutic effects of Sabutoclax and Minocycline in PDAC.
A second quasi-orthotopic study was conducted using similar drug dosing parameters. Tumors, though, were initiated with the injection of 5 × 106 cells as opposed to 1 × 106. In our first study, the use of fewer cells allowed testing whether Sabutoclax and Minocycline could prevent tumor formation. However, the use of fewer cells also means that the overall tumor burden was less when therapy was initiated, which prevented determining the true magnitude of the effect Sabutoclax and Minocycline would have in the context of a greater tumor burden, which might more closely imitate the clinical setting.
As anticipated, injecting a greater number of cells resulted in a larger overall tumor burden in the animals. Mice from all groups developed tumors or tumor nodules in the pancreas. However, the weight of the pancreas from mice treated with both Sabutoclax and Minocycline was significantly less than those from animals in all 3 other groups (Fig. 6d).
Sabutoclax and Minocycline in a transgenic mouse model of PDAC (KPC)
The KPC transgenic PDAC mouse model is used frequently in PDAC research (32–36). This animal spontaneously develops precursor pancreatic lesions, PanINs, which progress and eventually develop into invasive disease. Tumors form as a result of activated K-ras and functional loss of p53 in the pancreas, genetic changes also seen in a high percentage of human tumors. Histological analysis shows extensive local invasion as well as metastasis in a subset of animals (37).
Pancreatic tumors from these mice overexpress Mcl-1 as shown by immunohistochemistry (Supplementary Fig. 8a). This is consistent with the disease observed in humans (2–5) and provides a rationale for using Sabutoclax in these animals. Additionally, cell lines derived from these animals show combination effects with Sabutoclax and Minocycline (Supplementary Fig. 8b). These cells were injected subcutaneously into the flanks of control KPC mice (Pdx-1-Cre-negative/K-rasLSL-G12D/p53flox/wt) and allowed to grow for approximately one week. Mice were treated with Sabutoclax, Minocycline, or both drugs every 2–3 days via i.p. injection for a total of 6 injections. Sabutoclax or Minocycline alone did not significantly affect tumor growth. The combination of drugs, however, significantly inhibited tumor growth as compared to controls (Fig. 6e). Immunohistochemistry of tumor sections demonstrated decreased staining for PCNA and pStat3 in combination-treated tumors (Fig. 6f–g).
Additionally, a survival study was done using KPC mice (Pdx-1-Cre/K-rasLSL-G12D/p53flox/flow) to determine the effects of Sabutoclax and Minocycline. Mice were treated with Sabutoclax (1 mg/kg), Minocycline (10 mg/kg), or a combination of both three times a week via i.p. injection starting at around 1 month of age and continuing until animals reached a moribund state. Mice receiving combination treatment showed a significant survival advantage as compared to control mice (Fig. 6h). Tumors from these animals were isolated, sectioned, and stained for pStat3Y705. In correlation with our other studies, tumors from animals treated with Sabutoclax and Minocycline showed significantly less staining as compared to control tumors (Supplementary Fig. 9). Importantly, no toxicity was seen from either drug in any of the animals studies conducted.
Discussion
Pancreatic cancer is one of the most lethal cancers remaining largely untreatable. Moreover, advances in therapy have been minimal over the last 15 years, due in part to the aggressive nature of PDAC and the difficulty in developing selective and effective therapeutics. We presently describe an efficacious novel drug combination for PDAC that uses a new BH3 mimetic and uncovers the hidden therapeutic potential of Minocycline as an anti-cancer agent. Considering overexpression of the anti-apoptotic Bcl-2 proteins in PDAC, we initially evaluated the efficacy of Sabutoclax, a BH3 mimetic that targets these anti-apoptotic proteins inhibiting their function. Sabutoclax was effective as a single agent. It induced cancer-inhibitory effects in multiple genetically diverse PDAC cell lines. Potent apoptosis-inducing activity was evident in some PDAC cell lines and in those that only showed minor increases in death, we found instead a potent cell cycle arrest. Tumor heterogeneity is a problem manifested to some degree in all cancers, but is especially relevant in PDAC, contributing to the global resistance seen in this cancer to conventional chemotherapeutics. A beneficial aspect of Sabutoclax is its anti-cancer activity in multiple PDAC cell lines, irrespective of genetic background.
Despite the potential of Sabutoclax as a single-agent, there is a pressing need for combination therapy in the clinical setting. Cancer is an adaptive disease and effectively combatting it requires a multifaceted approach. Because of this, we sought to find a second drug that would potentially synergize with Sabutoclax to further promote its clinical applicability. We focused on the antibiotic, Minocycline, which has a small literature base supporting a novel role for this drug in the field of cancer (15–19). Despite these reports, translational cancer research using tetracyclines never expanded as only minor efficacy was evident with these drugs. In addition to its classical role as an antibiotic, Minocycline has also been studied extensively as a neuroprotective agent. Zhu, et. al. showed that this neuroprotection develops, in part, through the inhibition of caspase-9 and caspase-3 activation after exposure to death-inducing stimuli due to the inhibition of cytochrome c release from mitochondria (22). Minocycline has also been shown to lead to increases in the expression of anti-apoptotic Bcl-2 proteins like Bcl-2 (20,21). We hypothesized that these properties might actually mask the true potential of Minocycline as a cancer therapeutic and contribute to the disappointing results seen in the past. However, we hypothesized that these properties might make it an ideal combination partner for Sabutoclax. Sabutoclax works by directly acting at the level of the mitochondria specifically inducing apoptosis driven by cytochrome c release. In combination with Sabutoclax, the block on apoptosis in cells treated with Minocycline may be released thereby leading to synergistic anti-cancer properties.
Our study has shown that Sabutoclax plus Minocycline is exceptionally effective against pancreatic cancer (Fig. 6i). Subtoxic individual doses of each drug produced a dramatic synergistic cytotoxic effect. Furthermore, we found that this combination resulted in a loss of Stat3 activation, which was not seen in response to Sabutoclax treatment in non-tumorigenic LT2 cells (data not shown). This may help to explain the absence of sensitivity seen in these cells. Reintroduction of a constitutively active Stat3 mutant into cancer cells rendered them resistant to the combination of Sabutoclax and Minocycline. This combination shows promise in vivo using multiple mouse models, both immune-compromised and immune-competent transgenic models of PDAC, showing significant anti-cancer activity without any signs of gross toxicities.
In summary, we describe an innovative combinatorial therapeutic approach with remarkable activity against pancreatic cancer cells in vitro and in vivo in three animal PDAC models. Considering the paucity of effective therapies for PDAC, it is clear that new approaches are mandatory to impact clinically on this invariably fatal cancer. The ability to target the Bcl-2 family for inactivation, using Sabutoclax, and combining this with a simple synthetic tetracycline antibiotic, such as Minocycline, opens up new areas of research with the potential to lead to an effective therapy for pancreatic cancer.
Supplementary Material
Acknowledgments
The present study was supported in part by National Cancer Institute Grants R01 CA127641 (PBF) and R01 CA168517 (MP and PBF) and a VCU Massey Cancer Center (MCC) development award. DS is a Harrison Scholar in the MCC and a Blick Scholar in the VCU School of Medicine. PBF holds the Thelma Newmeyer Corman Chair in Cancer Research in the MCC.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
References
- 1.Hezel AF, Kimmelman AC, Stanger BZ, Bardeesy N, Depinho RA. Genetics and biology of pancreatic ductal adenocarcinoma. Genes & development. 2006;20:1218–49. doi: 10.1101/gad.1415606. [DOI] [PubMed] [Google Scholar]
- 2.Evans JD, Cornford PA, Dodson A, Greenhalf W, Foster CS, Neoptolemos JP. Detailed tissue expression of bcl-2, bax, bak and bcl-x in the normal human pancreas and in chronic pancreatitis, ampullary and pancreatic ductal adenocarcinomas. Pancreatology : official journal of the International Association of Pancreatology. 2001;1:254–62. doi: 10.1159/000055820. [DOI] [PubMed] [Google Scholar]
- 3.Guoan X, Hanning W, Kaiyun C, Hao L. Adenovirus-mediated siRNA targeting Mcl-1 gene increases radiosensitivity of pancreatic carcinoma cells in vitro and in vivo. Surgery. 2010;147:553–61. doi: 10.1016/j.surg.2009.10.033. [DOI] [PubMed] [Google Scholar]
- 4.Miyamoto Y, Hosotani R, Wada M, Lee JU, Koshiba T, Fujimoto K, et al. Immunohistochemical analysis of Bcl-2, Bax, Bcl-X, and Mcl-1 expression in pancreatic cancers. Oncology. 1999;56:73–82. doi: 10.1159/000011933. [DOI] [PubMed] [Google Scholar]
- 5.Takahashi H, Chen MC, Pham H, Matsuo Y, Ishiguro H, Reber HA, et al. Simultaneous knock-down of Bcl-xL and Mcl-1 induces apoptosis through Bax activation in pancreatic cancer cells. Biochimica et biophysica acta. 2013;1833:2980–7. doi: 10.1016/j.bbamcr.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quinn BA, Dash R, Azab B, Sarkar S, Das SK, Kumar S, et al. Targeting Mcl-1 for the therapy of cancer. Expert opinion on investigational drugs. 2011;20:1397–411. doi: 10.1517/13543784.2011.609167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muchmore SW, Sattler M, Liang H, Meadows RP, Harlan JE, Yoon HS, et al. X-ray and NMR structure of human Bcl-xL, an inhibitor of programmed cell death. Nature. 1996;381:335–41. doi: 10.1038/381335a0. [DOI] [PubMed] [Google Scholar]
- 8.Ni Chonghaile T, Letai A. Mimicking the BH3 domain to kill cancer cells. Oncogene. 2008;27 (Suppl 1):S149–57. doi: 10.1038/onc.2009.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kitada S, Kress CL, Krajewska M, Jia L, Pellecchia M, Reed JC. Bcl-2 antagonist apogossypol (NSC736630) displays single-agent activity in Bcl-2-transgenic mice and has superior efficacy with less toxicity compared with gossypol (NSC19048) Blood. 2008;111:3211–9. doi: 10.1182/blood-2007-09-113647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wei J, Kitada S, Rega MF, Emdadi A, Yuan H, Cellitti J, et al. Apogossypol derivatives as antagonists of antiapoptotic Bcl-2 family proteins. Molecular cancer therapeutics. 2009;8:904–13. doi: 10.1158/1535-7163.MCT-08-1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wei J, Stebbins JL, Kitada S, Dash R, Placzek W, Rega MF, et al. BI-97C1, an optically pure Apogossypol derivative as pan-active inhibitor of antiapoptotic B-cell lymphoma/leukemia-2 (Bcl-2) family proteins. Journal of medicinal chemistry. 2010;53:4166–76. doi: 10.1021/jm1001265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wei J, Stebbins JL, Kitada S, Dash R, Zhai D, Placzek WJ, et al. An optically pure apogossypolone derivative as potent pan-active inhibitor of anti-apoptotic bcl-2 family proteins. Frontiers in oncology. 2011;1:28. doi: 10.3389/fonc.2011.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Azab B, Dash R, Das SK, Bhutia SK, Shen XN, Quinn BA, et al. Enhanced delivery of mda-7/IL-24 using a serotype chimeric adenovirus (Ad. 5/3) in combination with the Apogossypol derivative BI-97C1 (Sabutoclax) improves therapeutic efficacy in low CAR colorectal cancer cells. Journal of cellular physiology. 2012;227:2145–53. doi: 10.1002/jcp.22947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dash R, Azab B, Quinn BA, Shen X, Wang XY, Das SK, et al. Apogossypol derivative BI-97C1 (Sabutoclax) targeting Mcl-1 sensitizes prostate cancer cells to mda-7/IL-24-mediated toxicity. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:8785–90. doi: 10.1073/pnas.1100769108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu WT, Lin CH, Hsiao M, Gean PW. Minocycline inhibits the growth of glioma by inducing autophagy. Autophagy. 2011;7:166–75. doi: 10.4161/auto.7.2.14043. [DOI] [PubMed] [Google Scholar]
- 16.Pourgholami MH, Ataie-Kachoie P, Badar S, Morris DL. Minocycline inhibits malignant ascites of ovarian cancer through targeting multiple signaling pathways. Gynecologic oncology. 2013;129:113–9. doi: 10.1016/j.ygyno.2012.12.031. [DOI] [PubMed] [Google Scholar]
- 17.Pourgholami MH, Mekkawy AH, Badar S, Morris DL. Minocycline inhibits growth of epithelial ovarian cancer. Gynecologic oncology. 2012;125:433–40. doi: 10.1016/j.ygyno.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 18.Regen F, Heuser I, Herzog I, Hellmann-Regen J. Striking growth-inhibitory effects of minocycline on human prostate cancer cell lines. Urology. 2014;83:509.e1–6. doi: 10.1016/j.urology.2013.10.029. [DOI] [PubMed] [Google Scholar]
- 19.Tang C, Yang L, Jiang X, Xu C, Wang M, Wang Q, et al. Antibiotic drug tigecycline inhibited cell proliferation and induced autophagy in gastric cancer cells. Biochemical and biophysical research communications. 2014;446:105–12. doi: 10.1016/j.bbrc.2014.02.043. [DOI] [PubMed] [Google Scholar]
- 20.Kernt M, Neubauer AS, Eibl KH, Wolf A, Ulbig MW, Kampik A, et al. Minocycline is cytoprotective in human trabecular meshwork cells and optic nerve head astrocytes by increasing expression of XIAP, survivin, and Bcl-2. Clinical ophthalmology. 2010:591–604. doi: 10.2147/opth.s11216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang J, Wei Q, Wang CY, Hill WD, Hess DC, Dong Z. Minocycline up-regulates Bcl-2 and protects against cell death in mitochondria. The Journal of biological chemistry. 2004;279:19948–54. doi: 10.1074/jbc.M313629200. [DOI] [PubMed] [Google Scholar]
- 22.Zhu S, Stavrovskaya IG, Drozda M, Kim BY, Ona V, Li M, et al. Minocycline inhibits cytochrome c release and delays progression of amyotrophic lateral sclerosis in mice. Nature. 2002;417:74–8. doi: 10.1038/417074a. [DOI] [PubMed] [Google Scholar]
- 23.Lebedeva IV, Sarkar D, Su ZZ, Kitada S, Dent P, Stein CA, et al. Bcl-2 and Bcl-x(L) differentially protect human prostate cancer cells from induction of apoptosis by melanoma differentiation associated gene-7, mda-7/IL-24. Oncogene. 2003;22:8758–73. doi: 10.1038/sj.onc.1206891. [DOI] [PubMed] [Google Scholar]
- 24.Dash R, Richards JE, Su ZZ, Bhutia SK, Azab B, Rahmani M, et al. Mechanism by which Mcl-1 regulates cancer-specific apoptosis triggered by mda-7/IL-24, an IL-10-related cytokine. Cancer research. 2010;70:5034–45. doi: 10.1158/0008-5472.CAN-10-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Venkatesan P, Puvvada N, Dash R, Prashanth Kumar BN, Sarkar D, Azab B, et al. The potential of celecoxib-loaded hydroxyapatite-chitosan nanocomposite for the treatment of colon cancer. Biomaterials. 2011;32:3794–806. doi: 10.1016/j.biomaterials.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 26.Das SK, Bhutia SK, Azab B, Kegelman TP, Peachy L, Santhekadur PK, et al. MDA-9/syntenin and IGFBP-2 promote angiogenesis in human melanoma. Cancer research. 2013;73:844–54. doi: 10.1158/0008-5472.CAN-12-1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bissonnette N, Hunting DJ. p21-induced cycle arrest in G1 protects cells from apoptosis induced by UV-irradiation or RNA polymerase II blockage. Oncogene. 1998;16:3461–9. doi: 10.1038/sj.onc.1201899. [DOI] [PubMed] [Google Scholar]
- 28.Canfield SE, Zhu K, Williams SA, McConkey DJ. Bortezomib inhibits docetaxel-induced apoptosis via a p21-dependent mechanism in human prostate cancer cells. Molecular cancer therapeutics. 2006;5:2043–50. doi: 10.1158/1535-7163.MCT-05-0437. [DOI] [PubMed] [Google Scholar]
- 29.Corcoran RB, Contino G, Deshpande V, Tzatsos A, Conrad C, Benes CH, et al. STAT3 plays a critical role in KRAS-induced pancreatic tumorigenesis. Cancer research. 2011;71:5020–9. doi: 10.1158/0008-5472.CAN-11-0908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cowling V, Downward J. Caspase-6 is the direct activator of caspase-8 in the cytochrome c-induced apoptosis pathway: absolute requirement for removal of caspase-6 prodomain. Cell death and differentiation. 2002;9:1046–56. doi: 10.1038/sj.cdd.4401065. [DOI] [PubMed] [Google Scholar]
- 31.Lebedeva IV, Su ZZ, Vozhilla N, Chatman L, Sarkar D, Dent P, et al. Chemoprevention by perillyl alcohol coupled with viral gene therapy reduces pancreatic cancer pathogenesis. Molecular cancer therapeutics. 2008;7:2042–50. doi: 10.1158/1535-7163.MCT-08-0245. [DOI] [PubMed] [Google Scholar]
- 32.Bailey JM, Alsina J, Rasheed ZA, McAllister FM, Fu YY, Plentz R, et al. DCLK1 marks a morphologically distinct subpopulation of cells with stem cell properties in preinvasive pancreatic cancer. Gastroenterology. 2014;146:245–56. doi: 10.1053/j.gastro.2013.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Courtin A, Richards FM, Bapiro TE, Bramhall JL, Neesse A, Cook N, et al. Anti-tumour efficacy of capecitabine in a genetically engineered mouse model of pancreatic cancer. PloS one. 2013;8:e67330. doi: 10.1371/journal.pone.0067330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li H, Yang AL, Chung YT, Zhang W, Liao J, Yang GY. Sulindac inhibits pancreatic carcinogenesis in LSL-KrasG12D-LSL-Trp53R172H-Pdx-1-Cre mice via suppressing aldo-keto reductase family 1B10 (AKR1B10) Carcinogenesis. 2013;34:2090–8. doi: 10.1093/carcin/bgt170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rao CV, Mohammed A, Janakiram NB, Li Q, Ritchie RL, Lightfoot S, et al. Inhibition of pancreatic intraepithelial neoplasia progression to carcinoma by nitric oxide-releasing aspirin in p48(Cre/+)-LSL-Kras(G12D/+) mice. Neoplasia. 2012;14:778–87. doi: 10.1593/neo.121026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yip-Schneider MT, Wu H, Hruban RH, Lowy AM, Crooks PA, Schmidt CM. Efficacy of dimethylaminoparthenolide and sulindac in combination with gemcitabine in a genetically engineered mouse model of pancreatic cancer. Pancreas. 2013;42:160–7. doi: 10.1097/MPA.0b013e318254f455. [DOI] [PubMed] [Google Scholar]
- 37.Bardeesy N, Aguirre AJ, Chu GC, Cheng KH, Lopez LV, Hezel AF, et al. Both p16(Ink4a) and the p19(Arf)-p53 pathway constrain progression of pancreatic adenocarcinoma in the mouse. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:5947–52. doi: 10.1073/pnas.0601273103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.