An investigation of BIU regarding a virtual world–based system for practicing IADLs among people with stroke found four themes to support system use.
MeSH TERMS: activities of daily living, behavior, stroke, user-computer interface, video games
Abstract
OBJECTIVE. The purpose of this study was to investigate the behavioral intention to use (BIU) regarding a virtual system for practicing instrumental activities of daily living (IADLs) among people with stroke.
METHOD. Fourteen people who had sustained a stroke used a virtual world–based system over four sessions to participate in virtual occupations of preparing meals and putting away groceries. To investigate intention to use the technology, participants responded to a questionnaire based on the Technology Acceptance Model and were interviewed about the experience.
RESULTS. Analysis of questionnaire responses revealed favorable attitudes toward the technology and statistically significant correlations between these attitudes and positive BIU. Analysis of qualitative data revealed four themes to support system use: Use of the affected arm increased, the virtual practice was enjoyable, the technology was user-friendly, and the system reflected real-life activities.
CONCLUSION. This study shows that participants reported a positive BIU for the virtual system for practicing IADLs.
In the United States, approximately 7 million adults age 20 or older have experienced a stroke (Go et al., 2013). Annually, approximately 795,000 people sustain a new or recurrent stroke, the equivalent of one stroke every 40 s (Russo & Andrews, 2008). For the person sustaining a stroke, the functional impact can be profound. Stroke is the leading cause of serious long-term disability (Go et al., 2013), and resulting hemiparesis can lead to substantial problems with occupational performance, including activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
The use of virtual reality systems in rehabilitation is growing and has the potential to positively influence outcomes for patients. The emergence of low-cost human motion sensors in commercial gaming systems has facilitated the use of computer games for therapy (Halton, 2008; Kwon, Park, Yoon, & Park, 2012; Lange, Flynn, & Rizzo, 2009). Examples of off-the-shelf hardware systems include the Microsoft (Redmond, WA) Xbox Kinect™, Nintendo (Redmond, WA) Wii™, and Sony (Tokyo, Japan) PlayStation Move™. Specifically, the use of virtual reality systems in rehabilitation has been shown to produce functional MRI (fMRI) results consistent with sensorimotor cortex reorganization (Schuster-Amft et al., 2014; You et al., 2005). Moreover, recent studies have found that performance in a virtual kitchen task predicted actual task performance (Allain et al., 2014), virtual practice of shopping improved actual shopping performance (Kizony, Korman, Sinoff, Klinger, & Josman, 2012), and movements learned in virtual contexts frequently transferred to real-life environments (Holden, 2005).
Examples of existing interventions for daily activities in a virtual context include grocery shopping, kitchen tasks, driving, using public transportation, and crossing a street (Allain et al., 2014; Katz et al., 2005; Lam, Man, Tam, & Weiss, 2006; Lee et al., 2003; Ruparel, Johnson, Strachota, McGuire, & Tchekanov, 2009; Whitney et al., 2006; Yamaguchi, Foloppe, Richard, Richard, & Allain, 2012; Zhang et al., 2003). Additionally, other published reports include clients interacting with virtual worlds to successfully complete multiple virtual household and community activities (da Costa & de Carvalho, 2004).
Evidence is emerging that gaming technologies have become accepted in rehabilitation settings and among the stroke population as a result of patient enjoyment and motivation (Bower, Clark, McGinley, Martin, & Miller, 2014; Celinder & Peoples, 2012; Lewis, Woods, Rosie, & McPherson, 2011; Reid & Hirji, 2004; Taylor, McCormick, Shawis, Impson, & Griffin, 2011). Off-the-shelf games, however, often encourage nonspecific movements and are not adaptable to different levels of motor and cognitive function (Plow & Finlayson, 2014). Such games can be intimidating or frustrating, especially for people with more severe impairments (Rand, Kizony, & Weiss, 2008). Additionally, some patients have reported that age-inappropriate games are perceived as childish or too difficult (Bower, 2009; Celinder & Peoples, 2012).
The Technology Acceptance Model (TAM; Davis, 1989) offers a powerful explanation of the relationship among client perception, behavioral preferences, sociodemographic factors, and system use (Davis, 1989; Fetscherin & Lattemann, 2008; Gell, Rosenberg, Demiris, Lacroix, & Patel, 2013). The model, which is based on the Theory of Reasoned Action (Fishbein & Ajzen, 1975), suggests that a person’s actual behavior in using a system can be predicted by intention, referred to as behavioral intention to use (BIU). Two other important factors in determining acceptance are perceived usefulness (PU) and perceived ease of use (PEOU; McCreadie & Tinker, 2005). With respect to PU, research has suggested that older adults accept new technology if they believe it might improve their quality of life and independence (Mahmood, Yamamoto, Lee, & Steggell, 2008; Steele, Lo, Secombe, & Wong, 2009). Regarding PEOU, older adults accept technology more readily if it incorporates simple interfaces that are easy to understand (Gell et al., 2013).
Lack of technology acceptance and lack of BIU are barriers to the adoption of new technology, especially among older adults. One study found that older adults did not prefer—and many were unable to use—an off-the-shelf gaming system for exercise and fitness (Laver, Ratcliffe, George, Burgess, & Crotty, 2011). The requirement of some systems to use a computer mouse, keyboard, or joystick for practicing virtual daily activities makes it difficult for many older adults to use such systems (da Costa & de Carvalho, 2004; Josman, Klinger, & Kizony, 2008; Kizony et al., 2012; Yamaguchi et al., 2012). In a broad sense, the issue of acceptance of various types of technology, including assistive technology, has been linked to a client’s perception of a device, psychosocial impact of use, access, and congruence with unique client goals (Jutai, Rigby, Ryan, & Stickel, 2000; Scherer, Sax, Vanbiervliet, Cushman, & Scherer, 2005; Scherer & Glueckauf, 2005).
The Virtual Occupational Therapy Assistant™ (VOTA; Barron Associates, Charlottesville, VA), a virtual world–based system, was developed from the simple premise that the best way to acquire (or reacquire) the capability to perform an occupation after a stroke is to practice that occupation. Occupational therapy that emphasizes ADLs is effective for improving patient performance of ADLs (Kristensen, Persson, Nygren, Boll, & Matzen, 2011; Legg et al., 2007). The Occupational Therapy Practice Framework: Domain and Process (3rd ed.; American Occupational Therapy Association, 2014) includes virtual contexts within the domain of occupational therapy. VOTA offers a unique approach that incorporates natural motor and cognitive demands into the practice of virtual IADLs within a fun, engaging, and safe artificial environment. Activities incorporate elements of strength, motor control, range of motion, memory, sequencing, spatial awareness, attention, safety awareness, and judgment. During practice, the upper-extremity motion of a patient’s virtual self (an avatar) matches real-world upper-extremity motion, enabled by an advanced real-time motion estimation algorithm that uses tracking data from a Kinect sensor (Figure 1).
Figure 1.
The Virtual Occupational Therapy Assistant system uses a Kinect sensor to immerse the patient in a suite of virtual activities of daily living.
The patient experience of virtual IADL practice has been investigated with other systems. Virtual practice of driving was motivating to patients (Ruparel et al., 2009), virtual practice of shopping was enjoyable and perceived to be beneficial (Kizony et al., 2012), and virtual kitchen tasks were motivating and generated enthusiasm among some participants (Yamaguchi et al., 2012). Because VOTA is a novel system, it was important to explore the patient experience with VOTA. Therefore, the research question at the center of this study was, “Will people with stroke exhibit a positive BIU the VOTA to practice simulated IADLs?”
Method
Participants
A convenience sample of 14 stroke survivors (for characteristics, see Table 1) was recruited for participation through telephone or in-person communication. Inclusion criteria included antigravity elbow flexion to at least 45°; antigravity shoulder flexion, abduction, and adduction to at least 30°; 15° active shoulder external rotation; visual acuity with corrective lenses of 20/50 or better; no hemispatial neglect; and ability to understand and follow verbal directions. Participants were recruited from occupational therapy caseloads and schedule review and included inpatient rehabilitation patients, outpatient patients, and discharged former patients. Study participation did not replace or interfere with any prescribed course of therapy intervention.
Table 1.
Participant Characteristics
| Participant | Age, yr | Gender | Time Since Stroke, Mo | Handedness | Affected Arm | Uses Computer | Uses Web Browser | Has Played Computer Games |
| 1 | 48 | F | 36 | R | L | SA | SA | SA |
| 2 | 49 | F | 24 | R | R | SA | SA | A |
| 3 | 53 | F | 72 | R | L | A | A | SA |
| 4 | 60 | F | 24 | R | L | A | SA | SA |
| 5 | 61 | F | 12 | R | L | SA | SA | A |
| 6 | 63 | F | 60 | R | R | SA | D | D |
| 7 | 63 | M | 36 | R | L | SA | SA | A |
| 8 | 74 | M | 9 | R | R | A | A | A |
| 9 | 77 | M | 36 | R | L | D | A | A |
| 10 | 78 | F | 96 | R | L | D | D | A |
| 11 | 83 | F | 0.5 | R | R | D | D | D |
| 12 | 84 | F | 3 | R | R | A | A | D |
| 13 | 85 | F | 96 | R | R | D | D | D |
| 14 | 87 | M | 9 | R | R | A | A | D |
Note. A = Agree; D = Disagree; F = female; L = left; M = male; R = right; SA = strongly agree.
Licensed occupational therapists conducted recruitment and protocol administration under the approval and supervision of the University of Virginia institutional review board for health sciences research. All study activity took place in the clinical facilities of the University of Virginia HealthSouth Rehabilitation Hospital (Charlottesville, VA) and was completed between September and December 2013. All participants who consented to the study completed the study; there was no attrition.
Procedure
Participants attended four sessions of approximately 1 hr in duration in which they used their stroke-affected arm to practice two virtual IADL activities: meal preparation and putting away groceries (Figure 2). A combination of auditory and visual cues guided participants. The same virtual IADLs were repeated in each session, allowing participants to gain familiarity with the VOTA system and with the tasks within each occupation. Activities consisted of a sequence of tasks and subtasks designed to elicit desired functional movements. Participants were seated at all times during virtual IADL practice.
Figure 2.
Virtual Occupational Therapy Assistant instrumental activities of daily living include putting away groceries (left panels) and preparing meals. Point values appear on the screen as feedback to the patient regarding the efficiency of performance.
Although participants were able to freely move their torso and unaffected limb, only the affected arm was actively tracked and articulated in the virtual environment to discourage trunk compensation. The Kinect-based tracking algorithm estimates arm joint angles independent of trunk movement. Thus, trunk compensation does not aid in accomplishing the virtual reach, and participants learn to use just their arm to complete the reach.
In the initial session, participants were asked four open-ended questions to gauge their current use of and comfort with technology. On the fourth and final session, participants were asked four different open-ended questions about their experience using the VOTA system. Participants also responded to a 32-item VOTA questionnaire, which was based on the TAM and was adapted in part from instruments used by Davis (1993) and Venkatesh (2000), and asked questions in the context of VOTA system use for stroke recovery. The questionnaire used a 4-point Likert scale with two unfavorable and two favorable response options (strongly disagree, disagree, agree, strongly agree). It was divided into eight categories: PEOU; PU; BIU; attitude toward technology (ATT); subject norms; performance expectancy; demographic variables such as gender, experience, and age; and anxiety. Participants’ responses to the questionnaire in Supplemental Table 1 (25.8KB, pdf) (available online at http://otjournal.net; navigate to this article, and click on “Supplemental”).
All interviews were audio recorded and transcribed immediately after the session by the occupational therapists, who also kept field notes. The interview transcripts were analyzed using published methods, including coding, grouping, and categorizing data according to emerging themes (Denzin & Lincoln, 2008; Elo & Kyngäs, 2008). To maintain rigor and consistency, the occupational therapists checked the themes against the original transcripts and their field notes, and the second author (Adams) confirmed the results. This mixed-methods approach qualitatively explored BIU among participants and quantitatively confirmed it (Denzin & Lincoln, 2008).
Results
Questionnaire Data
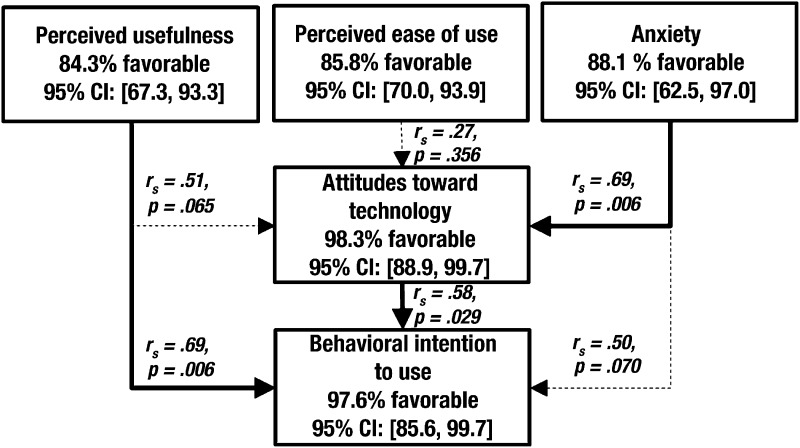
Participants ranked each VOTA questionnaire category as extremely unfavorable, unfavorable, favorable, or extremely favorable (see Supplemental Table 2 (25.8KB, pdf) for rankings). Results of this ranking showed that participants had overall favorable opinions of their experience with the VOTA system and exhibited a positive BIU with regard to the technology for virtual practice of IADLs. Figure 3 shows the results of a categorical analysis (of five categories) of the VOTA questionnaire responses using a modified version of the TAM (Davis, Bagozzi, & Warshaw, 1989). For each category, the percentage of favorable and extremely favorable responses is provided along with the 95% confidence interval.
Figure 3.
Categorical analysis of favorability and statistical correlation in Virtual Occupational Therapy Assistant questionnaire responses. Arrows between the categories are labeled to indicate correlation, calculated using Spearman’s rank-order coefficient. Bold arrows indicate statistical significance (p ≤ .05); dotted arrows indicate nonsignificance; CI = confidence interval.
A statistically significant (p = .006) relationship was found between PU and BIU, indicating that participants linked the perceived benefit with their intentions to use the VOTA system. Additionally, the relationship between anxiety and ATT was statistically significant (p = .006) as was the relationship between ATT and BIU (p = .029), indicating that anxiety is a relevant factor in participants’ attitudes toward the VOTA system, which then influences their likelihood to use the system.
Interview Data
Participants provided responses that supported the VOTA system and provided constructive feedback for modifications to the system. Four themes emerged relating to positive aspects of the VOTA experience:
Use of affected arm increased. Despite participants’ considerable variations in length of time since their stroke (see Table 1), the most common theme related to an increase in the use of the affected arm during typical day-to-day activities. Participant 1 stated, “It especially got my arm moving.” Participant 8 compared movement during practice of virtual IADLs to movement during at-home exercise: “When you’re doing exercises at home [holding my arm still is] not something that I do. I move, but I don’t have to hold it still.” Other participants reported that VOTA highlighted residual deficits in upper-extremity function. For example, Participant 5 reported that “the positive side is I realize that the left side is not good. I’m saying that’s positive because normally I forget and don’t use my left side a lot—I use it but not a lot—so I thought it was stronger than it is.”
Using VOTA was enjoyable. Although participants had different experiences with technology before this study, many participants commented that their experience with the VOTA system was enjoyable or rewarding. Participants used the words good, interesting, useful, and worthwhile to describe their engagement with VOTA. Participant 13 stated that “anything we can use to help us get back our lives is alright in my book.”
Technology was user-friendly. Participants represented a wide spectrum of prior knowledge and experience with technology. Participant 3 commented, “I was wondering how I would do in a situation like this, and I think I did good. I was a little surprised.” Overall, participants were pleased with the usability of the VOTA system and the extent to which their abilities improved quickly over the four sessions. Participant 3 said, “The cooking seemed to get easier, each of the four sessions was easier. I think it helped doing the first three sessions, but the last session, I was more confident.” Participant 12 stated, “I think particularly when you’ve had a stroke, it’s hard to feel proficient at anything, and this lets you do that.” Additionally, field notes confirmed that participants rapidly improved their performance with the system. They required fewer verbal prompts from the occupational therapists, independently incorporated strategies suggested by the therapists, and frequently logged higher scores at each subsequent attempt.
VOTA reflected real-life occupations. Participants related to the realism of the virtual environment. They reported that “it was a real-life situation” and “it gives me normal things to do such as cooking and putting groceries away just like I do at home.” In particular, Participant 3 verbalized how she immersed herself in the virtual environment and began thinking ahead to the logical next steps. She stated, “They need to put knives and forks on the tray so you can really eat [the eggs] instead of just looking at [them].”
Three themes emerged relating to constructive feedback for modifications to the system:
VOTA lacks fine motor integration. Two participants mentioned the lack of fine motor use in the virtual occupations selected for this study. Participant 8 explained, “I think it needs a different Kinect [to] pick up any movement from my hand.” Participant 14 stated, “It’s helpful, but it’s still hard for me to use the avatar [with] only the shoulder. I want to use my hand.”
Cueing should be improved. Although all participants were successful in learning and completing the virtual IADL occupations, some participants suggested improvements to the cueing integrated into the system. Participant 6 reported, “I still get confused with all the arrows,” whereas Participant 13 stated, “Gear down the enthusiasm level of my cheerleader.”
Virtual targets should be more sensitive. The software was custom built for the VOTA application, but participants suggested improving the sensitivity of virtual targets to allow easier and more consistent acquisition and placing of virtual objects. Participant 1 mentioned, “I couldn’t always tell when they wanted it to be dropped.”
Discussion
The results of this study indicate that people who have sustained a stroke exhibit a positive BIU for a technology application incorporating both motor and cognitive skills for the virtual practice of IADLs. One of the strengths of the VOTA system is the opportunity for clients to complete an entire virtual IADL task. The system incorporates many reaching movements in all planes; physical and mental endurance; and cognitive engagement to sequence, recall, plan, and anticipate safety hazards. The results showing BIU for the VOTA system align closely with published results showing positive feelings with the virtual practice of IADLs (Kizony et al., 2012; Ruparel et al., 2009; Yamaguchi et al., 2012).
The strong correlation found between PU and BIU is consistent with the TAM (Davis, 1989) and with previous observations on the importance of PU for acceptance of technology (Mahmood et al., 2008). Likewise, the strong correlation found between attitude and BIU supports Davis’s (1989) supposition that people’s intention to perform certain behaviors is linked to positive feeling or emotion. The VOTA data indicate that low anxiety-related factors (e.g., lack of fear or intimidation) in participants supported formation of these positive attitudes. For participants in this study, presentation of familiar environments and easy-to-understand tasks within the virtual world may have reduced anxiety, thus playing an important role in positive attitudes toward the technology. These positive attitudes, along with a strong perception that the system would have a positive impact on recovery, contribute to the likelihood that patients would use VOTA for stroke rehabilitation, which is consistent with the TAM.
The constructive feedback about the participant experience is helpful in refining the VOTA system for future study and clinical use. In this study, a one-size-fits-all experience was created. The importance of a virtual reality system facilitating specific and appropriately challenging activities has been established (Lange et al., 2011); therefore, future versions will incorporate graded cueing and levels of motor challenge. Last, tools to enable capture and integration of hand function are being explored.
Overall, this study found that people with stroke, regardless of previous experience with technology, exhibited a positive BIU for a system for the virtual practice of IADLs. A significant relationship was found between participant anxiety and attitude toward the technology, between ATT and BIU, and between PU and BIU. Moreover, participants identified positive aspects and features of the system, including a targeted emphasis on the impaired arm, an enjoyable experience, ease of use, and relevance to real-life activities.
Study Limitations
The primary limitation of this study is that participants were interviewed by the occupational therapist researchers, which may have resulted in reporting bias. Additionally, for this study, the VOTA system included the practice of only two virtual IADLs.
Implications for Occupational Therapy Practice
The results of this research show that a virtual world–based system for the practice of IADLs is very well accepted by stroke survivors. This study has the following implications for occupational therapy practice:
Virtual world–based systems dedicated to the virtual practice of ADLs and IADLs should continue to be developed as an adjunct to current best practices in occupational therapy for patients after a stroke.
Virtual worlds may provide a safe environment for clients who are unable to practice ADLs and IADLs in a natural context because of physical, cognitive, or social support barriers.
Clients even many years after stroke are interested and motivated to practice virtual ADLs and IADLs.
Conclusion
On the basis of the results of this study, people with stroke exhibit a positive BIU with regard to a low-cost virtual environment for practice of IADLs. In future studies, the efficacy of the VOTA intervention should be explored. Additionally, expanded software applications to increase the levels of challenge and variety of IADLs available should be developed and tested. This study should be replicated in the future by other clinicians using the same or similar virtual system to further develop the body of knowledge surrounding the provision of occupational therapy services using virtual world–based technology.
Supplementary Material
Acknowledgments
The VOTA project was sponsored by the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development, through Grant 1R43HD071745-01A1 to Barron Associates. The authors would like to thank the University of Virginia, HealthSouth Corporation, and Designing Digitally for their important contributions to the program.
Contributor Information
Allison Ellington, Allison Ellington, MS, OTR/L, is Director of Clinical Education, Department of Occupational Therapy, Murphy Deming College of Health Sciences, Mary Baldwin College, Staunton, VA, and occupational therapist, University of Virginia HealthSouth Rehabilitation Hospital, Charlottesville; aellington@mbc.edu.
Richard Adams, Richard Adams, PhD, is Principal Research Scientist, Barron Associates, Charlottesville, VA.
Marga White, Marga White, MS, OTL, is Occupational Therapist, University of Virginia HealthSouth Rehabilitation Hospital, Charlottesville.
Paul Diamond, Paul Diamond, MD, is Director of Neurorehabilitation and Associate Professor, Physical Medicine and Rehabilitation Department, University of Virginia School of Medicine, Charlottesville.
References
- Allain P., Foloppe D. A., Besnard J., Yamaguchi T., Etcharry-Bouyx F., Le Gall D., . . . Richard P. (2014). Detecting everyday action deficits in Alzheimer’s disease using a nonimmersive virtual reality kitchen. Journal of the International Neuropsychological Society, 20, 468–477. http://dx.doi.org/10.1017/S1355617714000344 [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process (3rd ed.). American Journal of Occupational Therapy, 68(Suppl. 1), S1–S48. http://dx.doi.org/10.5014/ajot.2014.682005 [PubMed] [Google Scholar]
- Bower K. (2009). Virtual reality: More than a Wii role in rehabilitation. Paper presented at the meeting of Game Connect Asia Pacific: Games for Health Conference, Melbourne, Victoria, Australia. [Google Scholar]
- Bower K. J., Clark R. A., McGinley J. L., Martin C. L., & Miller K. J. (2014). Clinical feasibility of the Nintendo Wii™ for balance training post-stroke: A Phase II randomized controlled trial in an inpatient setting. Clinical Rehabilitation, 28, 912–923. http://dx.doi.org/10.1177/0269215514527597 [DOI] [PubMed] [Google Scholar]
- Celinder D., & Peoples H. (2012). Stroke patients’ experiences with Wii Sports® during inpatient rehabilitation. Scandinavian Journal of Occupational Therapy, 19, 457–463. http://dx.doi.org/10.3109/11038128.2012.655307 [DOI] [PubMed] [Google Scholar]
- da Costa R. M. E. M., & de Carvalho L. A. V. (2004). The acceptance of virtual reality devices for cognitive rehabilitation: A report of positive results with schizophrenia. Computer Methods and Programs in Biomedicine, 73, 173–182. http://dx.doi.org/10.1016/S0169-2607(03)00066-X [DOI] [PubMed] [Google Scholar]
- Davis F. (1989). Perceived usefulness, perceived ease of use, and user acceptance of information technology. Management Information Systems Quarterly, 13, 319–340. http://dx.doi.org/10.2307/249008 [Google Scholar]
- Davis F. D. (1993). User acceptance of information technology: System characteristics, user perceptions and behavioural impacts. International Journal of Man-Machine Studies, 38, 475–487. http://dx.doi.org/10.1006/imms.1993.1022 [Google Scholar]
- Davis F., Bagozzi R. P, & Warshaw P. R. (1989). User acceptance of computer technology: A comparison of two theoretical models. Management Science, 35, 982–1003. http://dx.doi.org/10.1287/mnsc.35.8.982 [Google Scholar]
- Denzin N. K., & Lincoln Y. S. (2008). Introduction: The discipline and practice of qualitative research. In Denzin N. K. & Lincoln Y. S. (Eds.), Strategies of qualitative inquiry (3rd ed., pp. 1–44). Thousand Oaks, CA: Sage. [Google Scholar]
- Elo S., & Kyngäs H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62, 107–115. http://dx.doi.org/10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Fetscherin M., & Lattemann C. (2008). User acceptance of virtual worlds. Journal of Electronic Commerce Research, 9, 231–242. Retrieved from http://www.csulb.edu/journals/jecr/issues/20083/paper5.pdf [Google Scholar]
- Fishbein M., & Ajzen I. (1975). Belief, attitude, intention, and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley. [Google Scholar]
- Gell N. M., Rosenberg D. E., Demiris G., Lacroix A. Z., & Patel K. V. (2013). Patterns of technology use among older adults with and without disabilities. Gerontologist. Advance online publication. http://dx.doi.org/10.1093/geront/gnt166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go A. S., Mozaffarian D., Roger V. L., Benjamin E. J., Berry J. D., Borden W. B., . . . Turner M. B.; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. (2013). Heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation, 127, e6–e245. http://dx.doi.org/10.1161/CIR.0b013e31828124ad [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halton J. (2008). Virtual rehabilitation with video games: A new frontier for occupational therapy. Occupational Therapy Now, 9, 12–14. [Google Scholar]
- Holden M. K. (2005). Virtual environments for motor rehabilitation: Review. Cyberpsychology and Behavior, 8, 187–211, discussion 212–219. http://dx.doi.org/10.1089/cpb.2005.8.187 [DOI] [PubMed] [Google Scholar]
- Josman N., Klinger E., & Kizony R. (2008). Performance within the Virtual Action Planning Supermarket (VAP–S): An executive function profile of three different populations suffering from deficits in the central nervous system. In Sharkey P. M., Lopes-dos-Santos P., Weiss P. L., & Brooks A. L. (Eds.), Proceedings of the 7th International Conference on Disability, Virtual Reality and Associated Technologies With ArtAbilitation (pp. 33–38). Reading, England: University of Reading. [Google Scholar]
- Jutai J., Rigby P., Ryan S., & Stickel S. (2000). Psychosocial impact of electronic aids to daily living. Assistive Technology, 12, 123–131. http://dx.doi.org/10.1080/10400435.2000.10132018 [DOI] [PubMed] [Google Scholar]
- Katz N., Ring H., Naveh Y., Kizony R., Feintuch U., & Weiss P. L. (2005). Interactive virtual environment training for safe street crossing of right hemisphere stroke patients with unilateral spatial neglect. Disability and Rehabilitation, 27, 1235–1243. http://dx.doi.org/10.1080/09638280500076079 [DOI] [PubMed] [Google Scholar]
- Kizony R., Korman M., Sinoff G., Klinger E., & Josman N. (2012). Using a virtual supermarket as a tool for training executive functions in people with mild cognitive impairment. In Sharky P. M. & Klinger E. (Eds.), Proceedings of the 9th International Conference on Disability, Virtual Reality and Associated Technologies (pp. 41–46). Reading, England: University of Reading. [Google Scholar]
- Kristensen H. K., Persson D., Nygren C., Boll M., & Matzen P. (2011). Evaluation of evidence within occupational therapy in stroke rehabilitation. Scandinavian Journal of Occupational Therapy, 18, 11–25. http://dx.doi.org/10.3109/11038120903563785 [DOI] [PubMed] [Google Scholar]
- Kwon J. S., Park M. J., Yoon I. J., & Park S. H. (2012). Effects of virtual reality on upper extremity function and activities of daily living performance in acute stroke: A double-blind randomized clinical trial. NeuroRehabilitation, 31, 379–385. 10.3233/NRE-2012-00807. [DOI] [PubMed] [Google Scholar]
- Lam Y. S., Man D. W., Tam S. F., & Weiss P. L. (2006). Virtual reality training for stroke rehabilitation. NeuroRehabilitation, 21, 245–253. [PubMed] [Google Scholar]
- Lange B., Chang C., Suma E., Newman B., Rizzo A. S., & Bolas M. (2011). Development and evaluation of low cost game-based balance rehabilitation tool using the Microsoft Kinect sensor. Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2011, 1831–1834. http://dx.doi.org/10.1109/IEMBS.2011.6090521 [DOI] [PubMed] [Google Scholar]
- Lange B., Flynn S., & Rizzo A. (2009). Initial usability assessment of off-the-shelf video game consoles for clinical game-based motor rehabilitation. Physical Therapy Review, 14, 355–363. http://dx.doi.org/10.1179/108331909X12488667117258 [Google Scholar]
- Laver K., Ratcliffe J., George S., Burgess L., & Crotty M. (2011). Is the Nintendo Wii Fit really acceptable to older people? A discrete choice experiment. BioMed Central Geriatrics, 11, 64. Retrieved from http://www.biomedcentral.com/1471-2318/11/64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. H., Ku J., Cho W., Hahn W. Y., Kim I. Y., Lee S. M., . . . Kim S. I. (2003). A virtual reality system for the assessment and rehabilitation of the activities of daily living. Cyberpsychology and Behavior, 6, 383–388. http://dx.doi.org/10.1089/109493103322278763 [DOI] [PubMed] [Google Scholar]
- Legg L., Drummond A., Leonardi-Bee J., Gladman J. R., Corr S., Donkervoort M., . . . Langhorne P. (2007). Occupational therapy for patients with problems in personal activities of daily living after stroke: Systematic review of randomised trials. British Medical Journal, 335, 922–925. http://dx.doi.org/10.1136/bmj.39343.466863.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis G. N., Woods C., Rosie J. A., & McPherson K. M. (2011). Virtual reality games for rehabilitation of people with stroke: Perspectives from the users. Disability and Rehabilitation: Assistive Technology, 6, 453–463. http://dx.doi.org/10.3109/17483107.2011.574310 [DOI] [PubMed] [Google Scholar]
- Mahmood A., Yamamoto T., Lee M., & Steggell C. (2008). Perceptions and use of gerotechnology: Implications for aging in place. Journal of Housing for the Elderly, 22, 104–126. http://dx.doi.org/10.1080/02763890802097144 [Google Scholar]
- McCreadie C., & Tinker A. (2005). The acceptability of assistive technology to older people. Ageing and Society, 25, 91–110. http://dx.doi.org/10.1017/S0144686X0400248X [Google Scholar]
- Plow M., & Finlayson M. (2014). A qualitative study exploring the usability of Nintendo Wii Fit among persons with multiple sclerosis. Occupational Therapy International, 21, 21–32. http://dx.doi.org/10.1002/oti.1345 [DOI] [PubMed] [Google Scholar]
- Rand D., Kizony R., & Weiss P. T. (2008). The Sony PlayStation II EyeToy: Low-cost virtual reality for use in rehabilitation. Journal of Neurologic Physical Therapy, 32, 155–163. http://dx.doi.org/10.1097/NPT.0b013e31818ee779 [DOI] [PubMed] [Google Scholar]
- Reid D., & Hirji T. (2004). The influence of a virtual reality leisure intervention program on the motivation of older adult stroke survivors: A pilot study. Physical and Occupational Therapy in Geriatrics, 21, 1–19. http://dx.doi.org/10.1080/J148v21n04_01 [Google Scholar]
- Ruparel R., Johnson M. J., Strachota E., McGuire J., & Tchekanov G. (2009). Evaluation of the TheraDrive system for robot/computer assisted motivating rehabilitation after stroke. Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2009, 811–814. http://dx.doi.org/10.1109/IEMBS2009.5332386 [DOI] [PubMed] [Google Scholar]
- Russo C., & Andrews R. (2008). Hospital stays for stroke and other cerebrovascular diseases, 2005 (NCIB Statistical Brief 51). Rockville, MD: Agency for Health Care Policy and Research. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK56044/ [PubMed]
- Scherer M., & Glueckauf R. (2005). Assessing the benefits of assistive technologies for activities and participation. Rehabilitation Psychology, 50, 132–141. http://dx.doi.org/10.1037/0090-5550.50.2.132 [Google Scholar]
- Scherer M. J., Sax C., Vanbiervliet A., Cushman L. A., & Scherer J. V. (2005). Predictors of assistive technology use: The importance of personal and psychosocial factors. Disability and Rehabilitation, 27, 1321–1331. http://dx.doi.org/10.1080/09638280500164800 [DOI] [PubMed] [Google Scholar]
- Schuster-Amft C., Henneke A., Hartog-Keisker B., Holper L., Siekierka E., Chevrier E., . . . Eng K. (2014). Intensive virtual reality-based training for upper limb motor function in chronic stroke: A feasibility study using a single case experimental design and fMRI. Disability and Rehabilitation: Assistive Technology. Advance online publication. http://dx.doi.org/10.3109/17483107.2014.908963. [DOI] [PubMed] [Google Scholar]
- Steele R., Lo A., Secombe C., & Wong Y. K. (2009). Elderly persons’ perception and acceptance of using wireless sensor networks to assist healthcare. International Journal of Medical Informatics, 78, 788–801. http://dx.doi.org/10.1016/j.ijmedinf.2009.08.001 [DOI] [PubMed] [Google Scholar]
- Taylor M. J., McCormick D., Shawis T., Impson R., & Griffin M. (2011). Activity-promoting gaming systems in exercise and rehabilitation. Journal of Rehabilitation Research and Development, 48, 1171–1186. http://dx.doi.org/10.1682/JRRD.2010.09.0171 [DOI] [PubMed] [Google Scholar]
- Venkatesh V. (2000). Determinants of perceived ease of use: Integrating control, intrinsic motivation, and emotion into the technology acceptance model. Information Systems Research, 11, 342–365. http://dx.doi.org/10.1287/isre.11.4.342.11872 [Google Scholar]
- Whitney S. L., Sparto P. J., Hodges L. F., Babu S. V., Furman J. M., & Redfern M. S. (2006). Responses to a virtual reality grocery store in persons with and without vestibular dysfunction. Cyberpsychology and Behavior, 9, 152–156. http://dx.doi.org/10.1089/cpb.2006.9.152 [DOI] [PubMed] [Google Scholar]
- Yamaguchi T., Foloppe D., Richard P., Richard E., & Allain P. (2012). A dual-modal virtual reality kitchen for (re)learning of everyday cooking activities in Alzheimer’s disease. Presence, 21, 43–57. [Google Scholar]
- You S. H., Jang S. H., Kim Y. H., Hallett M., Ahn S. H., Kwon Y. H., . . . Lee M. Y. (2005). Virtual reality-induced cortical reorganization and associated locomotor recovery in chronic stroke: An experimenter-blind randomized study. Stroke, 36, 1166–1171. http://dx.doi.org/10.1161/01.STR.0000162715.43417.91 [DOI] [PubMed] [Google Scholar]
- Zhang L., Abreu B. C., Seale G. S., Masel B., Christiansen C. H., & Ottenbacher K. J. (2003). A virtual reality environment for evaluation of a daily living skill in brain injury rehabilitation: Reliability and validity. Archives of Physical Medicine and Rehabilitation, 84, 1118–1124. http://dx.doi.org/10.1016/S0003-9993(03)00203-X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.