Abstract
Objectives:
Most types of population-based cancer screening require repeat participation to be effective. This study investigated predictors of repeat participation in the NHS Bowel Cancer Screening Programme (BCSP).
Methods:
The BCSP in England offers biennial colorectal cancer screening using a guaiac fecal occult blood test (gFOBt) from age 60–74 years. This analysis included 62 081 individuals aged 60–64 years at the time of the first invitation (R1). The main outcome was repeat participation at their second (R2) or third (R3) invitation. Behavioural measures derived from screening records included late return of the gFOBt kit, compliance with follow-up investigations and previous screening participation. Other potential predictors of repeat participation included results of individual test kit analysis (normal, weak positive, strong positive, spoilt) and the definitive result of the gFOBt screening episode (normal or abnormal). Age, sex and socioeconomic deprivation were also recorded.
Results:
Overall repeat uptake was 86.6% in R2 and 88.6% in R3. Late return of the test kit was consistently associated with lower uptake (R2: 82.3% vs 88.6%, P<0.001; R3: 84.5% vs 90.5%, P<0.001). A definitive abnormal gFOBt result in the previous screening episode was a negative predictor of repeat uptake (R2: 61.4% vs 86.8%, P<0.001; R3: 65.7% vs 88.8%, P<0.001). Weak positive (R2: 76.9% vs 86.8%, P<0.001; R3: 81.7% vs 88.8%, P<0.05) and spoilt test kits (R2: 79.0% vs 86.6%, NS; R3: 84.2% vs 92.2%, P<0.05) were associated with lower repeat uptake, but were not consistently independent predictors in all invitation rounds or subgroups. Among those with a definitive abnormal gFOBt result, noncompliance with follow-up in a previous screening episode was also associated with lower repeat uptake (R2: 24.3% vs 67.1%, P<0.001; R3: 43.2% vs 69.9%, P<0.001).
Conclusions:
Behavioural markers and test results from previous screening episodes have been implicated in subsequent gFOBt uptake.
Keywords: colorectal cancer screening, repeat screening, behavioural markers, reminders, weak positives, abnormal results, colonoscopy attendance
Most tests for population-based cancer screening rely on repeated participation for optimal public health outcomes. Since 2006, the NHS Bowel Cancer Screening Programme (BCSP) in England has invited men and women aged 60–69 years (currently extended to 74 years) who are registered with a general practitioner (GP) to complete a guaiac-based fecal occult blood test (gFOBt) every 2 years. Randomised controlled trials have shown that regular, repeated screening with gFOBt reduces colorectal cancer (CRC) mortality by up to 25% among participants (Scholefield et al, 2002; Hewitson et al, 2008). Because of the low sensitivity of gFOBt, repeated participation is extremely important for the effectiveness of FOB screening (Soares-Weiser et al, 2007).
Encouragingly, repeat uptake among people who have previously responded to a screening invitation is generally high. Uptake of the first repeat screening invitation was ∼87% in a recent study of the NHS BCSP (Lo et al, 2014). High repeat uptake rates were also reported in a Spanish CRC pilot programme (87% Garcia et al, 2012), an Australian pilot programme (80% Cole et al, 2012) and a Dutch pilot programme (85% Denters et al, 2013).
However, the small amount of attrition at each round adds up across several screening rounds. Consistent screening uptake over three rounds was only 44% in the NHS BCSP Southern Hub in England (Lo et al, 2014) and 39.2% in an earlier pilot study in Scotland (Steele et al, 2014). Major factors known to contribute to attrition are an irregular screening participation history and being more socioeconomically deprived (Lo et al, 2014).
Some other characteristics of an individual's previous screening episode(s) also have been identified as risk factors for nonresponse to repeat screening invitations. The need for a reminder before test kit return in the previous round was negatively associated with subsequent screening uptake in the Spanish pilot programme (Garcia et al, 2012). Research on procrastination in general suggests that task aversiveness, self-efficacy and other person-related characteristics could contribute to delayed action (Steel, 2007). Late kit return is therefore a likely indicator of the degree of adversity an individual experiences in completing the test. Possible causes include an aversion to stool sampling (Consedine et al, 2011) and general life difficulties (Power et al, 2008).
The need for multiple gFOBts within one screening episode, most commonly because the first test kit gave a weak positive result (also known as inconclusive or unclear test results), may lead to incomplete gFOBt screening within one episode (Lo et al, 2014). In the Australian and Spanish pilot studies, weak positives and a definitive abnormal FOB result were also associated with lower repeat uptake (Cole et al, 2012; Garcia et al, 2012). However, it is unknown whether factors related to the experience of gFOBt screening (i.e., late kit return and test results) are predictors of repeat uptake independent of other known predictors, including sociodemographics and previous screening participation (Cole et al, 2012; Garcia et al, 2012; Denters et al, 2013; Lo et al, 2014).
Follow-up of abnormal gFOBt results (most commonly a colonoscopy) is integral to the success of a gFOBt screening programme (Smith et al, 2013), and the determinants of follow-up colonoscopy compliance have been studied elsewhere (Morris et al, 2012). However, to our knowledge, no previous studies have examined the role of follow-up after a definitive abnormal gFOBt result in subsequent gFOBt uptake.
At the time of the first biennial invitation, only sex, age and postcode of invitees are known. However, as more previous screening episode data become available with each biennial invitation round, an increasingly detailed picture of each invitee emerges. Examining previous screening episode patterns over a higher number of invitation rounds has the potential to generate powerful insights that could be used to promote repeat uptake and improve communication with screening invitees. Studies to date have only examined the relationship between first screening episode characteristics and the first repeat screening (Cole et al, 2012; Garcia et al, 2012). It is not known whether factors related to previous screening experience(s) remain useful indicators of individuals ‘at risk' of dropout after the first repeat screening. The present paper examines the role of previous screening episodes in repeat screening uptake using data from three biennial invitation rounds of the NHS BCSP.
Materials and methods
Colorectal cancer screening in England
The NHS BCSP in England provides CRC screening using a gFOBt kit that is completed at home and sent back in a freepost envelope. A pre-invitation letter is sent 8 days before the test kit (hema-screen, Immunostics Inc., Ocean, NJ, USA). To complete the test, two fecal samples from three consecutive stools are applied to three pairs of application windows in turn. Invitees who do not return the test kit are sent a reminder 28 days after the test kit was mailed. Test kits are returned to a laboratory where each window is tested for the presence of blood.
Participants who return a test kit with five or six positive windows (a ‘strong positive' and thus a definitive ‘abnormal' result) are offered a consultation with a Specialist Screening Practitioner (SSP) to discuss a follow-up examination (usually colonoscopy). If the first test kit has one to four positive windows (a ‘weak positive' or ‘unclear' result), a repeat gFOBt is required. The participant is referred to an SSP if any windows on a second or a third test kit are positive (a definitive ‘abnormal' result). If a second and third test kit both yield a negative result (a definitive ‘normal' result), the individual is referred back to routine biennial screening. A repeat gFOBt is also required when a test kit is designated ‘spoilt' (i.e., inadequate or undated sample collection) or ‘technically failed' (i.e., laboratory-based reading error).
Sample
The analysis used anonymised data from the Southern Hub of the NHS BCSP. Each year, the Southern Hub invites ∼1.1 million people in the south of England (excluding London).
All people (n=62 099) aged 60–64 years at the time of the first invitation (R1) to screening between September 2006 and February 2008 were included in the data set. The specified age range ensured that individuals were age-eligible for screening over three biennial invitation rounds, irrespective of the age extension. Three invitation rounds therefore refer to a cohort of people who have received three biennial invitations (R1, R2 and R3) in which they may, or may not, have participated. Follow-up of invitees until December 2012 allowed for a minimum of 3 months for a response after invitation, any further investigations and minor adjustments made to the timing of screening invitations (‘invitation smoothing') for each of the three rounds (BCSP Southern Hub, 2011). Individuals may not receive three invitations for reasons that include clinical status, death, relocation outside the catchment area of the Hub or a written request declining further screening invitations. After exclusion of 18 people because of incomplete or ambiguous screening episode records, 62 081 cases were included in the analysis. A screening episode record was considered ambiguous if there was a mismatch between the records of the individual's screening uptake, the number of test kits completed and test results of each completed kit (e.g., adequately screened, but only one completed test kit with a weak positive result). Of the 62 081 included cases who received a first biennial screening invitation, 58 531 received a second invitation of whom 34 856 were invited for repeat screening (i.e., responders in R1). A third invitation was sent to 55 028 cases of whom 38 373 were invited for repeat screening (i.e., responders in R1 and/or R2).
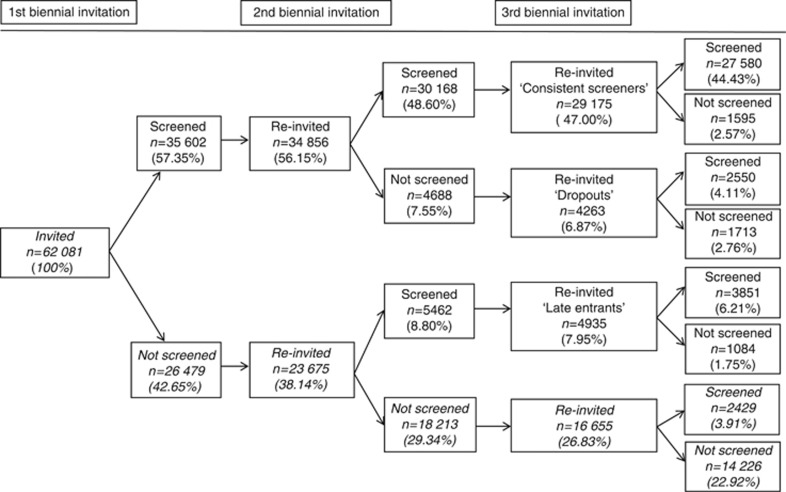
Figure 1 illustrates the number of people receiving a screening invitation in each of the three biennial rounds. The sample eligible for repeat screening in the second round (R2) consisted of participants who had responded to the first screening invitation (R1). Participants in repeat screening in the third round (R3) consisted of three subgroups (‘Consistent Screeners', ‘Dropouts' and ‘Late Entrants') that varied by previous screening participation. Box 1 defines each R3 subgroup by previous screening participation and states the ‘last screening episode' for each subgroup. The last screening episode refers to the last active screening round of any given individual. Uptake in each round and uptake by subgroup are described in Tables 1A and B respectively. A previous publication has discussed uptake by sociodemographics and previous screening participation in more detail (Lo et al, 2014).
Figure 1.
Sample sizes in each biennial invitation round by previous uptake (in percentages of the initial sample). Text in normal font indicates incidence (i.e., repeat) screening subgroups, and text in italics indicates prevalence screening subgroups excluded from analysis.
Box 1. Definitions of subgroups in the third biennial invitation round (R3).
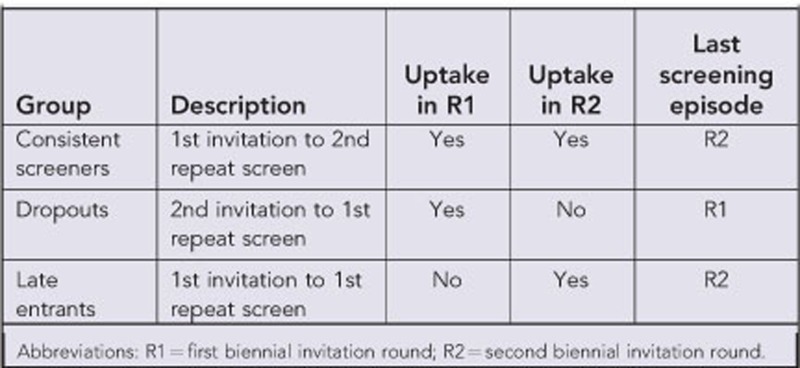
Table 1A. Repeat screening uptake per biennial invitation round by previous screening episode factors in percentages with the denominator (n).
| R2 | R3 | |
|---|---|---|
| Total repeat screening uptake | 86.55 (34 856) | 88.55 (38 373) |
|
By previous screening episode factors | ||
| Time to kit return | ||
| ⩽28 Days | 88.64 (23 361) | 90.48 (26 136) |
| >28 Days | 82.30 (11 495) | 84.45 (12 237) |
| Weak positives | ||
| None | 86.81 (33 930) | 88.82 (36 941) |
| One or more | 76.89 (926) | 81.70 (1432) |
| Definitive gFOBt result | ||
| Normal | 86.75 (34 576) | 88.84 (37 907) |
| Abnormal | 61.43 (280) | 65.67 (466) |
| Spoilt kit | ||
| None | 86.59 (34 651) | 88.62 (38 067) |
| One or more | 79.02 (205) | 80.72 (306) |
| Follow-up compliance | ||
| Not complied | 24.32 (37) | 43.24 (74) |
| Complied | 67.08 (243) | 69.90 (392) |
Abbreviations: gFOBt=guaiac fecal occult blood test; R2=second biennial invitation round; R3=third biennial invitation round.
Measures
The gFOBt screening uptake
Whether an invited individual was adequately screened (i.e., received a definitive gFOBt result) or not. Uptake in previous invitation rounds was used to define subgroups in R3 (Box 1).
Late return of gFOBt kit in the previous screening episode
The sent and return dates of the first gFOBt kit in each screening episode were used to calculate the number of days an individual had taken to return the test kit. The outcome was dichotomised into a late return variable (>28 days).
The gFOBt results in the previous screening episode
The number of completed test kits in the last screening episode and the test result of each completed kit (i.e., normal, weak positive, strong positive, spoilt, technical failure). Technical failures were not examined further because of their low occurrence (n=20 in R2; n=14 in R3). For individuals who were adequately screened, the definitive gFOBt result was also recorded.
Follow-up compliance
For people who had received a definitive abnormal gFOBt result, attendance at the SSP appointment and colonoscopy (or another follow-up examination) was recorded. A dichotomous variable for follow-up compliance was used and defined as failure to attend SSP OR colonoscopy/other follow-up examination (0) and attendance of SSP AND colonoscopy/other follow-up examination (1).
Sociodemographics
Sex, age at the time of invitation and a neighbourhood-level measure of socioeconomic deprivation (index of multiple deprivation (IMD) score 2004, based on the 2001 Census; scale 0–80, with a score of 0 being the least deprived and 80 being the most deprived) were recorded for each individual (National Office of Statistics, 2004). Some people received a subsequent invitation when they were >2 years older than at the previous invitation because of the precise timing of their birthdays, (very) late return of previous test kits, time elapsed until follow-up investigations and invitation smoothing practices. Age was therefore divided into three categories (young, middle and old) per invitation round for the analysis. The first two categories each represented a 2-year time span, whereas the third category covered all older ages.
Data analysis
Repeat screening uptake (where ‘uptake' is defined as the proportion of the invited population that was adequately screened) and all predictors are described by biennial invitation round (R2 and R3). Repeat uptake, gFOBt-related predictors and follow-up compliance are also described for each subgroup in R3.
Multivariable logistic regression analysis was used with repeat uptake as the outcome variable and gFOBt-related previous screening episode variables, sociodemographic variables and previous screening participation (only for uptake in R3) as explanatory variables. Repeat uptake of each subgroup in R3 was also examined separately with gFOBt-related previous screening episode factors and sociodemographics as explanatory variables. The gFOBt-related previous screening episode predictors included late return of the test kit (>28 days), weak positives, spoilt test kits and a definitive abnormal gFOBt result. The sociodemographic predictors were age, sex and socioeconomic deprivation. Variables derived from the last screening episode were used for all analyses, except for a late return variable based on both R1 and R2, that was used in the subgroup analysis for ‘Consistent Screeners'.
The reference category for the weak positive effect differed between individuals with a definitive normal (ref. cat.: normal result for the first test kit) and a definitive abnormal (ref. cat.: strong positive result for the first test kit) gFOBt result. Differences in the effect of weak positives between definitive normal and definitive abnormal individuals were therefore examined. An interaction between weak positives and the definitive FOB test result was tested and included in the reported models if the interaction was statistically significant at the P<0.05 level. Previous screening participation is associated with incomplete gFOBt screening because of multiple testing (Lo et al, 2014). For this reason, interactions between previous screening participation and weak positives/spoilt test kits were also tested and reported if statistically significant.
A simple logistic regression analysis was conducted to examine the effect of follow-up compliance on subsequent gFOBt screening uptake in R2 and R3 among individuals who had received a definitive abnormal gFOBt result in the previous screening episode.
Results
Neighbourhood-level socioeconomic deprivation was the only sociodemographic factor consistently associated with repeat uptake, independent of other sociodemographic and previous screening episode factors. Being socioeconomically deprived was associated with lower repeat uptake in both R2 and R3 (P<0.001; Table 2A). Lower repeat uptake in R3 was consistently observed among Consistent Screeners (P<0.001), Dropouts (P<0.001) as well as Late Entrants (P<0.01; Table 2B).
Table 2A. Repeat screening uptake by invitation round: multivariable logistic regression results of sociodemographic and previous screening episode factors.
|
R2 |
R3 |
|||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
|
Sociodemographics | ||||
| Men | 1.00 (ref.) | 1.00 (ref.) | ||
| Women | 1.03 | 0.97–1.10 | 0.98 | 0.91–1.05 |
| IMD score (0–80) | 0.98*** | 0.98–0.99 | 0.99*** | 0.98–0.99 |
|
Age at second invitation (62–70) | ||||
| 62–63 | 1.00 (ref.) | — | ||
| 64–65 | 1.05 | 0.99–1.13 | — | |
| 66+ | 0.99 | 0.88–1.11 | — | |
|
Age at third invitation (63–72 years) | ||||
| 64–65 | — | 1.00 (ref.) | ||
| 66–67 | — | 0.94 | 0.88–1.01 | |
| 68+ | — | 0.84** | 0.74–0.95 | |
|
Previous screening episode factors | ||||
| Kit return – ⩽28 days | 1.00 (ref.) | 1.00 (ref.) | ||
| Kit return – >28 days | 0.60*** | 0.56–0.64 | 0.69*** | 0.64–0.74 |
| Weak positives – none | 1.00 (ref.) | 1.00 (ref.) | ||
| Weak positives – one or more | 0.70*** | 0.57–0.85 | 0.70* | 0.56–0.88 |
| Definitive gFOBt result – normal | 1.00 (ref.) | 1.00 (ref.) | ||
| Definitive gFOBt result – abnormal | 0.12*** | 0.06–0.23 | 0.27*** | 0.21–0.35 |
| Spoilt kit – none | 1.00 (ref.) | 1.00 (ref.) | ||
| Spoilt kit – one or more | 0.73 | 0.52–1.03 | 0.71* | 0.52–0.98 |
| Weak positive × definitive result | 3.29** | 1.54–7.06 | — | |
|
Previous uptake subgroups | ||||
| Consistent Screeners | — | 1.00 (ref.) | ||
| Late Entrants | — | 0.21*** | 0.19–0.23 | |
| Dropouts | — | 0.09*** | 0.08–0.10 | |
| Weak positive × previous uptake | — | 1.40*** | 1.16–1.67 | |
Abbreviations: CI=confidence interval; gFOBt=guaiac fecal occult blood test; IMD=index of multiple deprivation; OR=odds ratio; ref.=reference category; R2=second biennial invitation round; R3=third biennial invitation round.
*P<0.05; **P<0.01; ***P<0.001.
Table 2B. Repeat screening uptake in the third biennial invitation round per subgroup: multivariable logistic regression results of sociodemographic and previous screening episode factors.
|
R3 Consistent Screeners |
R3 Dropouts |
R3 Late Entrants |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
|
Sociodemographics | ||||||
| Men | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |||
| Women | 0.99 | 0.90–1.10 | 0.93 | 0.82–1.05 | 0.99 | 0.87–1.14 |
| IMD score (0–80) | 0.98*** | 0.98–0.99 | 0.99*** | 0.98–0.99 | 0.99** | 0.99–1.00 |
|
Age at third invitation (63–72 years) | ||||||
| 64–65 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |||
| 66–67 | 0.94 | 0.85–1.05 | 0.92 | 0.81–1.05 | 0.95 | 0.83–1.10 |
| 68+ | 0.76** | 0.63–0.91 | 0.84 | 0.66–1.06 | 0.99 | 0.77–1.26 |
|
Previous screening episode factors | ||||||
| Kit return – ⩽28 days | — | 1.00 (ref.) | 1.00 (ref.) | |||
| Kit return – >28 days | — | 0.85* | 0.75–0.96 | 0.81** | 0.70–0.93 | |
| Kit return – ⩽28 days in R1 and R2 | 1.00 (ref.) | — | — | |||
| Kit return – >28 days in R1 | 0.69*** | 0.60–0.80 | — | — | ||
| Kit return – >28 days in R2 | 0.55*** | 0.48–0.64 | — | — | ||
| Kit return – >28 days in R1 and R2 | 0.43*** | 0.37–0.49 | — | — | ||
| Weak positives – none | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |||
| Weak positives – one or more | 0.66** | 0.51–0.86 | 1.42 | 0.97–2.08 | 0.91 | 0.61–1.35 |
| Definitive gFOBt result – normal | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |||
| Definitive gFOBt result – abnormal | 0.12*** | 0.06–0.24 | 0.21*** | 0.11–0.38 | 0.43** | 0.25–0.74 |
| Weak positive × definitive result | 2.44* | 1.07–5.55 | — | — | ||
Abbreviations: CI=confidence interval; gFOBt=guaiac fecal occult blood test; IMD=index of multiple deprivation; OR=odds ratio; ref.=reference category; R1=first biennial invitation round; R2=second biennial invitation round; R3=third biennial invitation round.
*P<0.05; ** P<0.01; *** P<0.001.
Late return of test kit in the previous screening episode
Repeat uptake in R2 was lower among those who, in the first round, had been late in returning their gFOBt kit and had received a reminder letter than those who had returned it within 28 days (82.3% vs 88.6%, P<0.001; Tables 1A and 2A). Late return was also associated with lower uptake in R3 overall (84.5% vs 90.5%, P<0.001) and in all R3 subgroups. ‘Dropouts' (58.1% vs 61.1%, P<0.05) and ‘Late Entrants' (75.8% vs 79.4%, P<0.01; Tables 1B and 2B) had lower uptake in R3 if they had returned the kit late in their previous episode. Late return had a graded effect on repeat uptake in R3 among ‘Consistent Screeners', the only subgroup that had two previous screening episodes. ‘Consistent Screeners' who had returned the kit promptly in both R1 and R2 had an R3 uptake rate of 95.9%. Those who had returned the kit late in either R1 (94.2%, P<0.001) or R2 (93.0%, P<0.001) were slightly less likely to respond in R3 than consistent prompt responders (95.9%, ref.). ‘Consistent Screeners' who had returned the kit late in both R1 and R2 were least likely to respond (91.1%, P<0.001).
Table 1B. Repeat screening uptake in the third biennial invitation round per subgroup by previous screening episode factors in percentages with the denominator (n).
| R3 Consistent Screeners | R3 Dropouts | R3 Late Entrants | |
|---|---|---|---|
| Total repeat screening uptake | 94.53 (29 175) | 59.82 (4263) | 78.03 (4935) |
|
By previous screening episode factors | |||
| Time to kit return | |||
| ⩽28 Days | — | 61.10 (2414) | 79.43 (3039) |
| >28 Days | — | 58.14 (1849) | 75.79 (1896) |
| ⩽28 Days in R1 and R2 | 95.93 (15 739) | — | — |
| >28 Days in R1 | 94.24 (4944) | — | — |
| >28 Days in R2 | 92.99 (4451) | — | — |
| >28 Days in R1 and R2 | 91.14 (4041) | — | — |
| Weak positives | |||
| None | 94.77 (28 106) | 60.05 (4080) | 78.32 (4755) |
| One or more | 88.21 (1069) | 54.64 (183) | 70.56 (180) |
| Definitive gFOBt result | |||
| Normal | 94.73 (28 864) | 60.34 (4188) | 78.35 (4855) |
| Abnormal | 75.88 (311) | 30.67 (75) | 58.75 (80) |
| Follow-up compliance | |||
| Not complied | 61.76 (34) | 9.09 (22) | 50.00 (18) |
| Complied | 77.62 (277) | 39.62 (53) | 61.29 (62) |
Abbreviations: gFOBt=guaiac fecal occult blood test; R1=first biennial invitation round; R2=second biennial invitation round; R3=third biennial invitation round.
The gFOBt results in the previous screening episode
A definitive abnormal gFOBt result in the previous screening episode was strongly associated with lower repeat uptake in R2 (61.4% vs 86.6%, P<0.001) and R3 (65.7% vs 88.8%, P<0.001; Tables 1A and 2A). The effect of a definitive abnormal result on uptake in R3 was similar among ‘Consistent Screeners' (75.9% vs 94.7%, P<0.001), ‘Dropouts' (30.7% vs 60.3%, P<0.001) and ‘Late Entrants' (58.8% vs 78.4%, P<0.01; Tables 1B and 2B).
Repeat uptake in R2 was lower if the participant had received a weak positive result in the previous screening episode (76.9% vs 86.8%, P<0.001; Tables 1A and 2A). In contrast, weak positives were not significantly associated with uptake in R3 (81.7% vs 88.8%, NS), although uptake figures showed a similar trend. Among the R3 subgroups, weak positives were a significant independent predictor of uptake only among ‘Consistent Screeners' (88.2% vs 94.8%, P<0.01; Tables 1B and 2B). Weak positives were not a significant predictor of uptake for ‘Dropouts' (54.6% vs 60.1%, NS) and ‘Late Entrants' (70.6% vs 78.3%, NS).
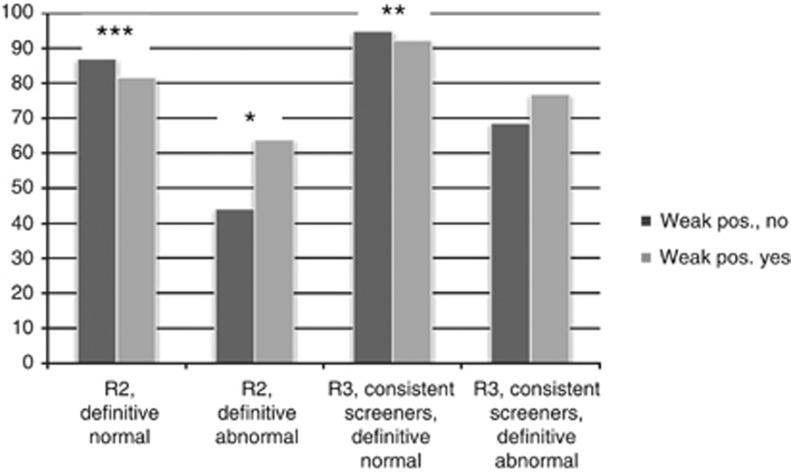
The effect of weak positives on subsequent repeat uptake in R2 interacted significantly with the definitive gFOBt result (P<0.01; Tables 1A and 2A). This interaction was not significant for overall repeat uptake in R3. However, a significant interaction effect was observed among ‘Consistent Screeners' (P<0.05) but no effect was found for ‘Dropouts' and ‘Late Entrants' (Tables 1B and 2B). Figure 2 illustrates the interaction effect. Among individuals who had a definitive normal gFOBt result in the previous screening episode, repeat uptake in R2 (81.6% vs 86.9%, crude OR=0.67, 95% CI: 0.55–0.82, P<0.001) and among ‘Consistent Screeners' in R3 (92.2% vs 94.8%, crude OR=0.65, 95% CI: 0.50–0.84, P<0.01) was lower among those who had received a weak positive result than among those who had a normal (first test kit) result in the previous screening episode. In contrast, among individuals who had a definitive abnormal gFOBt result, subsequent uptake in R2 was higher among individuals who had a weak positive result than those who had a strong positive (first test kit) result in the previous screening episode (63.8% vs 44.1%, crude OR=2.23, 95% CI: 1.08–4.61, P<0.05). A similar nonsignificant trend was observed among Consistent Screeners in R3 (76.8% vs 68.6%, crude OR=1.52, 95% CI: 0.71–3.27, NS). The significant interactions in R2 and among Consistent Screeners in R3 (the largest subgroup in the third round) suggest that multiple testing within one screening episode because of weak positives can be a deterrent to future screening if the weak positive had turned out to be a ‘false alarm'.
Figure 2.
% Subsequent gFOBt uptake by weak positives and definitive gFOB result in a previous screening episode. Results of simple logistic regression analyses of weak positives as the predictor of subsequent uptake: *P<0.05; **P<0.01; ***P<0.001.
Spoilt test kits were an independent, negative predictor of overall repeat uptake only in R3 (80.7% vs 88.6%, P<0.05; Tables 1A and 2A). Uptake figures for repeat screening in R2 (spoilt: 79.0% vs no spoilt: 86.6%, NS; Tables 1A and 2A) showed a similar trend towards lower uptake, but were not statistically significant. This suggests that the multivariable analysis was underpowered to detect moderate-sized differences, as the number of people with spoilt test kits was low. Spoilt test kits were therefore not included in the reported R3 subgroup analyses.
Follow-up noncompliance in the previous screening episode
Among individuals who returned to routine screening following a definitive abnormal gFOBt result, simple logistic regression analysis was used to examine the effect of follow-up compliance on subsequent screening uptake. Subsequent uptake in R2 (24.3% vs 67.1%, P<0.001) and R3 (43.2% vs 69.9%, P<0.001) was significantly lower among people who had not complied with follow-up examinations in R1 than among those who had complied (Tables 1A and 3A). In the R3 subgroups, subsequent uptake among noncompliers was significantly lower than among compliers among ‘Consistent Screeners' (61.8% vs 77.6%, P<0.05) and ‘Dropouts' (9.1% vs 39.6%, P<0.05; Tables 1B and 3B). Subsequent uptake was not significantly different among ‘Late Entrants', although results were in a similar direction (50.0% vs 61.3%, NS; Tables 1B and 3B).
Table 3A. Repeat screening uptake by invitation round: simple logistic regression results of follow-up compliance in the previous screening episode.
|
R2 |
R3 |
|||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
|
Follow-up compliance in previous episode | ||||
| Follow-up – complied | 1.00 (ref.) | 1.00 (ref.) | ||
| Follow-up – not complied | 0.16*** | 0.07–0.35 | 0.33*** | 0.20–0.55 |
Abbreviations: CI=confidence interval; OR=odds ratio; ref.=reference category; R2=second biennial invitation round; R3=third biennial invitation round.
***P<0.001.
Table 3B. Repeat screening uptake in the third biennial invitation round per subgroup: simple logistic regression results of follow-up compliance in the previous screening episode.
|
R3 Consistent Screeners |
R3 Dropouts |
R3 Late Entrants |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
|
Follow-up compliance in previous episode | ||||||
| Follow-up – complied | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |||
| Follow-up – not complied | 0.47* | 0.22–0.98 | 0.15* | 0.03–0.72 | 0.63 | 0.22–1.82 |
Abbreviations: CI=confidence interval; OR=odds ratio; ref.=reference category; R3=third biennial invitation round.
*P<0.05.
Discussion
Previous screening episode factors related to both the gFOBt and follow-up are predictive of subsequent gFOBt uptake, independent of sociodemographic and other previous screening episode factors. This is remarkable in the light of high overall uptake of repeat screening invitations. Socioeconomic deprivation was the only sociodemographic factor consistently associated with repeat uptake, independent of previous screening episode factors.
Similar to previous findings from a Spanish pilot programme (Garcia et al, 2012), late return of the previous test kit (>28 days) was consistently associated with lower uptake in R2 and R3. Most interestingly, the negative association between late return and subsequent uptake was graded among ‘Consistent Screeners', who had all participated twice before. ‘Consistent Screeners' who had responded promptly in both episodes were most likely to respond in R3, followed by those who had returned a kit late once and, finally, those who had returned the kit late in both previous screening episodes. The fact that effect of late return was not smaller among ‘Consistent Screeners' compared with ‘Dropouts' and ‘Late Entrants' is also noteworthy. It suggests that more frequent participation in the past does not help overcome difficulties related to late kit return, such as task aversiveness (Steel, 2007; Consedine et al, 2011).
Future studies should investigate whether planning methods, such as implementation intentions, could promote continued uptake among people with a history of late kit returns (Gollwitzer and Sheeran, 2006). Implementation intentions are often used to promote self-regulation and help people overcome anticipated barriers by formulating ‘if-then' plans (Gollwitzer, 1999). If this is an effective method, the individual-level data available from the NHS database could be used to target planning interventions specifically to this at-risk group.
Among those who remained eligible for routine screening, a definitive abnormal gFOBt result was strongly associated with lower subsequent uptake, consistent with results from an Australian pilot programme (Cole et al, 2012). Further research is needed to examine whether this is because of a lack of perceived necessity to engage with further gFOBt screening after a colonoscopy or another type of follow-up investigation, a more general negative attitude change or other reasons (e.g., patient experience of the follow-up investigation). Also consistent with previous studies (Cole et al, 2012; Garcia et al, 2012), a weak positive test result in the previous screening episode was a negative predictor of repeat uptake in R2 and uptake among Consistent Screeners in R3. This suggests that the requirement for multiple gFOB testing within one screening episode can be a deterrent to subsequent screening. The results also show tentative evidence of an association between spoilt test kits (another reason for multiple gFOB testing) and lower subsequent uptake.
A subgroup analysis showed that weak positives only had a negative effect on subsequent uptake among individuals with a definitive normal gFOBt result. Screening with multiple gFOBt kits therefore appears to be a deterrent only when the final test result was normal, possibly because of a perceived lack of benefit resulting from screening. Consistent with this hypothesis, a breast screening study showed that experienced pain was negatively associated with re-attendance only if the individual had previously received a false positive (vs negative) screening outcome (Hofvind et al, 2003). In other words, individuals might be more resilient to adverse events if the perceived usefulness of screening remains unchallenged.
Because of sample size limitations, the current study could not examine the effect of diagnostic outcomes from follow-up examinations on subsequent uptake among individuals who were referred back to routine screening. Future national studies should examine the role of diagnostic outcomes, as it could add further evidence to whether screening test outcomes affect (perceived usefulness of) repeat screening participation. National-level studies could also use routinely collected data of patient-reported outcomes to address the potential role of patient experiences with follow-up investigations in subsequent gFOBt uptake. Qualitative research on the appraisal of screening test results would also be a valuable addition to the current evidence base. This could inform communication about test results and reduce the potential negative impact of test results on subsequent screening uptake. Although some adverse screening events are inevitable, the use of fecal immunochemical test for haemoglobin (FIT) would be one strategy to greatly reduce multiple testing, thus avoiding the adverse consequences resulting from weak-positive gFOBt results. A recent FIT study reported higher consistent uptake over three rounds (54%) than those reported for gFOBt uptake (39–44%) (Kapidzic et al, 2014; Lo et al, 2014; Steele et al, 2014).
Compliance with follow-up examinations was also associated with subsequent gFOBt screening uptake in R2 and among ‘Consistent Screeners' and ‘Dropouts' in R3 (if people remained eligible for routine screening). The figures for ‘Late Entrants' showed similar trends but failed to reach statistical significance, possibly because of the smaller sample size in this subgroup. This indicates that some people with an abnormal gFOBt result do not comply with follow-up nor do they return to routine screening. Although few in number, they are part of a small, high-risk group that is more likely to reap tangible health benefits from full compliance with all screening recommendations.
To conclude, although gFOBt repeat screening uptake was generally high, previous screening episode characteristics were associated with lower repeat uptake. Late test kit return, a definitive abnormal gFOBt result and failure to comply with follow-up examinations in a previous screening episode were consistently and independently associated with lower repeat uptake. Screening records and other data related to previous screening episodes could therefore be used to identify groups at higher risk of nonresponse to repeat screening invitations. Although previous screening episode factors often cannot be modified, tailored communication and assistance throughout the screening process could reduce the impact of the identified risk factors. The present study has demonstrated the potential for information about screening trajectories to inform and streamline screening programmes through tailoring services and communication to the individual. Future research should examine the full potential of data related to previous screening experiences to promote regular participation in CRC screening programmes.
Acknowledgments
This study was supported by a programme grant from Cancer Research UK to JW (C1418/A14134). HS was supported by the GUTS Charity (Guildford Undetected Tumour Screening).
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
References
- BCSP Southern Hub 2011Summary Report Bowel Cancer Screening Programme Southern Hub2006–2010.
- Cole SR, Gregory T, Whibley A, Ward P, Turnbull D, Wilson C, Flight I, Esterman A, Young GP. Predictors of re-participation in faecal occult blood test-based screening for colorectal cancer. Asian Pac J Cancer Prev. 2012;13:5989–5994. doi: 10.7314/apjcp.2012.13.12.5989. [DOI] [PubMed] [Google Scholar]
- Consedine NS, Ladwig I, Reddig MK, Broadbent EA. The many faeces of colorectal cancer screening embarrassment: preliminary psychometric development and links to screening outcome. Br J Health Psychol. 2011;16:559–579. doi: 10.1348/135910710X530942. [DOI] [PubMed] [Google Scholar]
- Denters MJ, Deutekom M, Bossuyt PM, van Rijn AF, Fockens P, Dekker E. Involvement of previous non-participants cannot fully compensate for lower participation in a second round of FIT-screening. Cancer Epidemiol. 2013;37:330–335. doi: 10.1016/j.canep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Garcia M, Maria Borras J, Binefa G, Mila N, Alfons Espinas J, Moreno V. Repeated screening for colorectal cancer with fecal occult blood test in Catalonia, Spain. Eur J Cancer Prev. 2012;21:42–45. doi: 10.1097/CEJ.0b013e32834a7e9b. [DOI] [PubMed] [Google Scholar]
- Gollwitzer PM. Implementation intentions - strong effects of simple plans. Am Psychol. 1999;54:493–503. [Google Scholar]
- Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol. 2006;38:69–119. [Google Scholar]
- Hewitson P, Glasziou P, Watson E, Towler B, Irwig L. Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (Hemoccult): an update. Am J Gastroenterol. 2008;103:1541–1549. doi: 10.1111/j.1572-0241.2008.01875.x. [DOI] [PubMed] [Google Scholar]
- Hofvind SSH, Wang H, Thoresen S. The Norwegian Breast Cancer Screening Program: re-attendance related to the women's experiences, intentions and previous screening result. Cancer Causes Control. 2003;14:391–398. doi: 10.1023/a:1023918610664. [DOI] [PubMed] [Google Scholar]
- Kapidzic A, Grobbee EJ, Hol L, van Roon AH, van Vuuren AJ, Spijker W, Izelaar K, van Ballegooijen M, Kuipers EJ, van Leerdam ME. Attendance and yield over three rounds of population-based fecal immunochemical test screening. Am J Gastroenterol. 2014;109:1257–1264. doi: 10.1038/ajg.2014.168. [DOI] [PubMed] [Google Scholar]
- Lo SH, Halloran S, Snowball J, Seaman H, Wardle J, von Wagner C.2014Colorectal cancer screening uptake over three biennial invitation rounds in the English bowel cancer screening programmee-pub ahead of print 7 May 2014doi: 10.1136/gutjnl-2013-306144 [DOI] [PMC free article] [PubMed]
- Morris S, Baio G, Kendall E, von Wagner C, Wardle J, Atkin W, Halloran SP, Handley G, Logan RF, Obichere A, Rainbow S, Smith S, Snowball J, Raine R. Socioeconomic variation in uptake of colonoscopy following a positive faecal occult blood test result: a retrospective analysis of the NHS Bowel Cancer Screening Programme. Br J Cancer. 2012;107:765–771. doi: 10.1038/bjc.2012.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Office of Statistics . Key Statistics for Postcode Sectors in England and Wales, 2001. Crown Copyright: London; 2004. [Google Scholar]
- Power E, Van Jaarsveld CHM, McCaffery K, Miles A, Atkin W, Wardle J. Understanding intentions and action in colorectal cancer screening. Ann Behav Med. 2008;35:285–294. doi: 10.1007/s12160-008-9034-y. [DOI] [PubMed] [Google Scholar]
- Scholefield JH, Moss S, Sufi F, Mangham CM, Hardcastle JD. Effect of faecal occult blood screening on mortality from colorectal cancer: results from a randomised controlled trial. Gut. 2002;50:840–844. doi: 10.1136/gut.50.6.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith RA, Brooks D, Cokkinides V, Saslow D, Brawley OW. Cancer Screening in the United States, 2013. a review of current American Cancer Society Guidelines, current issues in cancer screening, and new guidance on cervical cancer screening and lung cancer screening. CA Cancer J Clin. 2013;63:88–105. doi: 10.3322/caac.21174. [DOI] [PubMed] [Google Scholar]
- Soares-Weiser K, Burch J, Duffy S, St, John J, Smith S, Westwood M, Kleijnen J. Diagnostic Accuracy and Cost-Effectiveness of Faecal Occult Blood Tests (FOBT) Used in Screening for Colorectal Cancer: A Systematic Review. University of York: York, United Kingdom; 2007. [DOI] [PubMed] [Google Scholar]
- Steel P. The nature of procrastination: a meta-analytic and theoretical review of quintessential self-regulatory failure. Psychol Bull. 2007;133:65–94. doi: 10.1037/0033-2909.133.1.65. [DOI] [PubMed] [Google Scholar]
- Steele RJC, McClements PL, Libby G, Carey FA, Fraser CG. Patterns of uptake in a biennial faecal occult blood test (FOBT) screening programme for colorectal cancer. Colorectal Dis. 2014;16:28–32. doi: 10.1111/codi.12393. [DOI] [PubMed] [Google Scholar]