Abstract
Background
The optimal use of various therapeutic combinations for moderate/severe chronic obstructive pulmonary disease (COPD) is unclear. The GLISTEN trial compared the efficacy of two long-acting anti-muscarinic antagonists (LAMA), when combined with an inhaled corticosteroid (ICS) and a long-acting β2 agonist (LABA).
Methods
This randomised, blinded, placebo-controlled trial in moderate/severe COPD patients compared once-daily glycopyrronium (GLY) 50 µg, once-daily tiotropium (TIO) 18 µg or placebo (PLA), when combined with salmeterol/fluticasone propionate (SAL/FP) 50/500 µg twice daily. The primary objective was to determine the non-inferiority of GLY+SAL/FP versus TIO+SAL/FP on trough FEV1 after 12 weeks. An important secondary objective was whether addition of GLY to SAL/FP was better than SAL/FP alone.
Results
773 patients (mean FEV1 57.2% predicted) were randomised; 84.9% completed the trial. At week 12, GLY+SAL/FP demonstrated non-inferiority to TIO+SAL/FP for trough FEV1: least square mean treatment difference (LSMdiff) −7 mL (SE 17.4) with a lower limit for non-inferiority of −60 mL. There was significant increase in week 12 trough FEV1 with GLY+SAL/FP versus PLA+SAL/FP (LSMdiff 101 mL, p<0.001). At 12 weeks, GLY+SAL/FP produced significant improvement in St George's Respiratory Questionnaire total score versus PLA+SAL/FP (LSMdiff −2.154, p=0.02). GLY+SAL/FP demonstrated significant rescue medication reduction versus PLA+SAL/FP (LSMdiff −0.72 puffs/day, p<0.001). Serious adverse events were similar for GLY+SAL/FP, TIO+SAL/FP and PLA+SAL/FP with an incidence of 5.8%, 8.5% and 5.8%, respectively.
Conclusions
GLY+SAL/FP showed comparable improvements in lung function, health status and rescue medication to TIO+SAL/FP. Importantly, addition of GLY to SAL/FP demonstrated significant improvements in lung function, health status and rescue medication compared to SAL/FP.
Trial registration number
Keywords: COPD Pharmacology
Key messages.
What is the key question?
Are the long-acting muscarinic antagonists (LAMAs) glycopyrronium (GLY) and tiotropium (TIO) comparable to each other when added to a long-acting β2 agonist (LABA)/inhaled corticosteroid (ICS) combination, and is triple therapy with GLY better than therapy with LABA/ICS (salmeterol/fluticasone propionate (SAL/FP)) alone in moderate to severe chronic obstructive pulmonary disease (COPD)?
What is the bottom line?
Triple therapy with GLY+SAL/FP is clinically superior to SAL/FP alone in COPD while GLY and TIO are equally efficacious when added to SAL/FP.
Why read on?
This is the first demonstration that a LAMA/LABA/ICS combination (using GLY) is superior to LABA/ICS alone in terms of lung function, health-related quality of life and rescue medication in patients with moderate to severe COPD over 12 weeks.
Introduction
Chronic obstructive pulmonary disease (COPD) is an important cause of mortality and poor health worldwide.1 Treatment goals for the management of COPD include relief of symptoms, improved exercise tolerance, prevention of disease progression, and reduction of exacerbations and mortality, while minimising adverse effects.1
Long-acting bronchodilators—muscarinic antagonists (LAMA) and β2-receptor agonists (LABA)—improve lung function, dyspnoea, health status, exercise tolerance and exacerbation rates in patients with COPD.2–7 This underpins the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2014 COPD Strategy recommendation that bronchodilators are the cornerstone of COPD symptom management.1 The strategy further recommends that patients who exhibit a high risk of exacerbations and/or an FEV1 <50% should receive combined inhaled corticosteroids (ICS) and LABA as this combination improves exacerbation rates, lung function, health status and symptoms in patients with moderate to severe COPD.1 5 8–12
There is limited evidence comparing the efficacy of LAMA versus LABA/ICS,13 and when combined it is unclear if additional benefits ensue as studies assessing this are very limited. Karner and Cates searched the Cochrane Airways Group Specialised Register of trials and cross references for parallel randomised controlled trials conducted over 3 months or longer in which comparisons were made between tiotropium (TIO)+LABA/ICS, TIO alone or LABA/ICS alone.14 Only three studies met their criteria. However, of these only one compared triple therapy (LAMA/LABA/ICS) with LABA/ICS and it was a pilot study of 81 patients.15 They concluded that further research was necessary in this area.14
Use of 50 μg of a once-daily inhaled dry powder formulation of the LAMA glycopyrronium bromide (GLY) via a Breezhaler provides comparable improvement in lung function, dyspnoea, health status and exacerbations to that of 18 μg of a once-daily inhaled dry powder formulation of TIO via a HandiHaler, the current standard of care for once-daily inhaled LAMA.16 17 GLY also has a fast onset of bronchodilation on the first day when compared to TIO and is highly efficacious in placebo-controlled studies.4 17 18
The GLISTEN study is a placebo-controlled blinded multicentre trial conducted to assess the non-inferiority of GLY compared to TIO when combined with an LABA/ICS, salmeterol (SAL)/fluticasone propionate (FP). The study was designed to support reimbursement and registration of GLY but importantly was also designed to allow comparison between GLY+SAL/FP and placebo (PLA)+SAL/FP in terms of efficacy and safety.
Methods
Patients
Patients were recruited if aged ≥40 years, had a smoking history of ≥10 pack years, a diagnosis of moderate to severe stable COPD (GOLD guidelines 201019), a post-bronchodilator FEV1/FVC ratio <0.7 and an FEV1 ≥30% and <80% of predicted values. Patients were recruited from primary, secondary and tertiary care sites in Australia and New Zealand.
The main exclusion criteria were lower respiratory tract infections/COPD exacerbations in the 6 weeks prior to screening, significant co-existing pulmonary disease, a history of asthma or α1-antitrypsin deficiency, pre-existing conditions that might be worsened by anticholinergic therapy, and clinically significant renal or cardiovascular abnormalities.
All patients gave written informed consent to participate in the study. The protocol was approved by ethics committees at participating centres. The study was registered with ClinicalTrials.gov, NCT01513460.
Study design and treatment
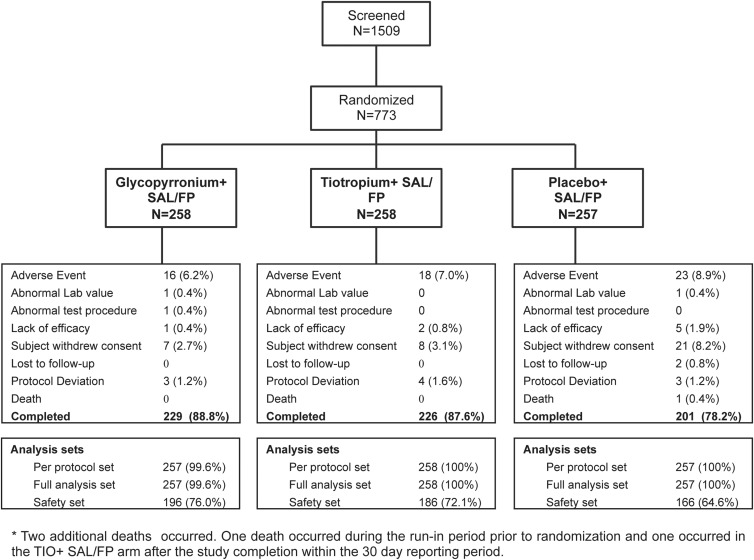
This was a multicentre, blinded, placebo-controlled parallel group 12-week study. After a pre-defined screening and washout period (washout up to 7 days, rescue medication allowed), patients entered a 7-day run-in period and received twice-daily SAL/FP 50/500 µg (via an Accuhaler). They were then randomised to receive once-daily GLY 50 µg (Breezhaler), matching PLA (Breezhaler) or once-daily TIO 18 µg (HandiHaler) (1:1:1 ratio; figure 1); all study medication was taken between 8:00 and 11:00. Patients continued to take SAL/FP twice daily and had salbutamol to use as rescue medication during the study.
Figure 1.
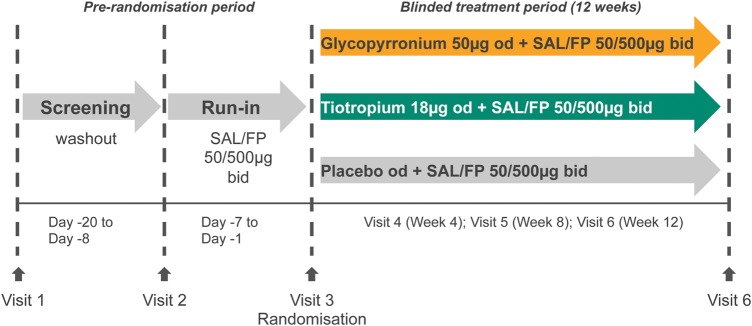
Study design. FP, fluticasone propionate; SAL, salmeterol.
Efficacy assessment
The primary goal was to demonstrate the non-inferiority of GLY+SAL/FP versus TIO+SAL/FP using trough FEV1 (mean of 23 h 15 min and 23 h 45 min post-dose values) following 12 weeks of treatment as the primary efficacy variable. This was assessed using the per protocol population (PPS=all patients in the full analysis set (FAS) who had no major protocol or non-protocol deviations). The FAS was all randomised patients receiving at least one study drug dose. All other efficacy variables were assessed in the FAS.
The next key assessment compared GLY+SAL/FP with PLA+SAL/FP for trough FEV1 after 12 weeks of treatment. Secondary variables for the comparisons of GLY+SAL/FP versus TIO+SAL/FP as well as GLY+SAL/FP versus PLA+SAL/FP included trough FEV1 at 4 and 8 weeks, health status (St George's Respiratory Questionnaire (SGRQ) total score at 12 weeks), mean daily rescue medication use over 12 weeks, and performance of usual daily activities and night-time awakenings.
Pulmonary function assessments were performed using centralised spirometry and adhered to the American Thoracic Society/European Respiratory Society standards.20
Safety assessment
The safety population was all patients receiving study treatment at least once, and patients were analysed per the treatment received. All treatment-emergent adverse events (AEs), serious AEs (SAEs) and vital sign abnormalities were recorded. AEs were coded using the Medical Dictionary for Regulatory Activities (MedDRA, V.15.1.21) and summarised primary organ class, preferred term, maximum severity and relationship to study drug.
Statistical analysis
The primary analysis was performed on the PPS using a mixed model. Treatment was the fixed effect with baseline trough FEV1, FEV1 before and after short-acting bronchodilator at run-in being covariates. This model also included randomisation stratification factors such as baseline smoking status (current/ex-smoker), baseline COPD severity (moderate/severe) and visit and interaction of treatment arms by visit as fixed effects and subjects as a random effect.
Non-inferiority of GLY+SAL/FP to TIO+SAL/FP would be inferred if the lower bound of the two-sided CI (adjusted for multiple assessments via sequential trial techniques) was greater than −60 mL.
Superiority of GLY+SAL/FP versus PLA+SAL/FP in terms of trough FEV1 after 12 weeks of treatment was evaluated using the FAS using a similar mixed model as specified for the primary analysis.
Secondary trough FEV1 data, SGRQ scores, rescue medication use and performance of usual daily activities/night-time awakenings were analysed with the same mixed model on the FAS with baseline SGRQ, rescue medication and performance of usual daily activities/night-time awakening scores replacing baseline FEV1 as covariates, respectively.
All safety endpoints were summarised by treatment for the safety set.
Sample size calculation
For detailed information on sample size and non-inferiority margin calculation, please refer to the online supplement. In essence, 170 evaluable patients per treatment group were required for adequate power to determine non-inferiority for the primary variable. One pre-specified unblinded interim analysis after 80 evaluable patients were recruited was accounted for in the statistical planning. Planned study numbers were also deemed adequate to make assessments on differences in key efficacy outcomes between GLY+SAL/FP and PLA+SAL/FP.
Results
Patient disposition and baseline characteristics
Study recruitment took place between April 2012 and September 2013. A total of 1059 patients were screened, 773 randomised (GLY+SAL/FP: 258; TIO+SAL/FP: 258; PLA+SAL/FP: 257) and 656 (84.9%) completed the study (figure 2). Patients were enrolled at 56 primary care sites and 18 secondary/tertiary care sites. Baseline characteristics were similar between the three treatment arms (table 1). Mean age was 68 years, 64.4% were male, 67.7% had moderate COPD, and the mean time since diagnosis was 7 years. The mean post-bronchodilator FEV1 was 57.2% of predicted and the FEV1/FVC ratio was 47.1%. In the 12 months before enrolment, 35% of patients had experienced an exacerbation. At baseline, ICS were used by 62.6% of patients randomised to the GLY+SAL/FP arm, 66.3% of those randomised to the TIO+SAL/FP arm and 68.1% of those randomised to the PLA+SAL/FP arm (table 1).
Figure 2.
Patient disposition. FP, fluticasone propionate; SAL, salmeterol; TIO, tiotropium.
Table 1.
Baseline demographics and spirometry (full analysis set)
| Glycopyrronium +SAL/FP |
Tiotropium +SAL/FP |
Placebo +SAL/FP |
|
|---|---|---|---|
| N=257 | N=258 | N=257 | |
| Mean (SD) age, years | 68.2 (8.38) | 68.0 (7.74) | 67.8 (8.49) |
| Male, n (%) | 163 (63.4) | 160 (62.0) | 174 (67.7) |
| Race, n (%) | |||
| Caucasian | 247 (96.1) | 242 (93.8) | 250 (97.3) |
| Asian | 1 (0.4) | 4 (1.6) | 1 (0.4) |
| Pacific Islander | 3 (1.2) | 3 (1.2) | 3 (1.2) |
| Black | 0 | 1 (0.4) | 0 |
| Other | 6 (2.3) | 8. (3.1) | 3 (1.2) |
| Mean (SD) duration of COPD, years | 7.0 (7.29) | 6.5 (5.82) | 7.2 (6.57) |
| Severity of COPD (GOLD 2010), n (%) | |||
| Moderate | 172 (66.9) | 175 (67.8) | 176 (68.5) |
| Severe | 85 (33.1) | 83 (32.2) | 81 (31.5) |
| Presence of exacerbation in past year, n (%) | |||
| Yes | 90 (35.0) | 92 (35.7) | 87 (33.9) |
| No | 167 (65.0) | 166 (64.3) | 170 (66.1) |
| ICS use at baseline | 161 (62.6) | 171 (66.3) | 175 (68.1) |
| LABA/ICS | 144 (56) | 154 (59.7) | 152 (59.1) |
| Other ICS | 17 (6.6) | 17 (6.6) | 23 (8.9) |
| Smoking status at screening, n (%) | |||
| Ex-smoker | 166 (64.6) | 166 (64.3) | 164 (63.8) |
| Smoker | 91 (35.4) | 92 (35.7) | 93 (36.2) |
| Mean (SD) duration of smoking, pack years | 47.2 (24.29) | 49.4 (26.98) | 49.7 (27.33) |
| Mean (SD), post-bronchodilator FEV1, L | 1.52 (0.50) | 1.49 (0.47) | 1.55 (0.48) |
| Mean (SD), post-bronchodilator FEV1% predicted | 57.36 (13.98) | 56.86 (13.81) | 57.35 (13.64) |
| Mean (SD), post-bronchodilator FEV1 reversibility, % | 21.10 (16.49) | 23.45 (16.50) | 22.41 (14.65) |
| Mean (SD), post-bronchodilator FEV1/FVC, % | 47.90 (11.01) | 46.68 (10.99) | 46.64 (11.26) |
COPD, chronic obstructive pulmonary disease; FP, fluticasone propionate; ICS, inhaled corticosteroid; LABA, long-acting β2 agonist; SAL, salmeterol.
A higher percentage of patients discontinued the study in the PLA+SAL/FP arm compared to the GLY+SAL/FP and TIO+SAL/FP arms (22%, 11% and 12%, respectively; χ2: p<0.00012), the majority due to AEs and withdrawal of consent.
Efficacy
Spirometry
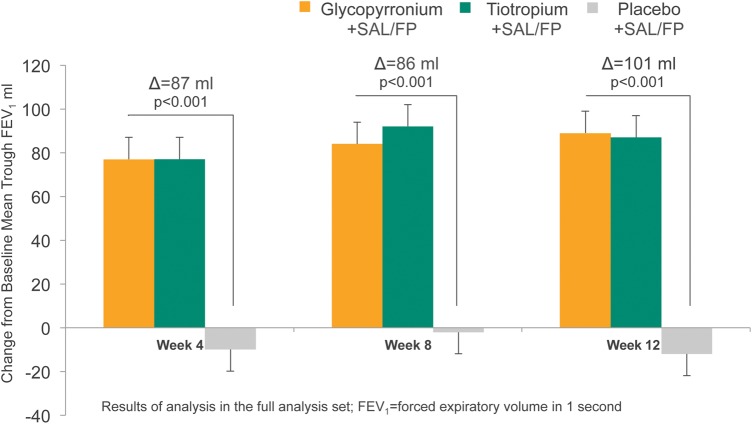
The primary endpoint was met: the two-sided 97.16% CI for the 12-week trough FEV1 treatment difference between GLY+SAL/FP and TIO+SAL/FP was higher than −60 mL, thus meeting the pre-specified criterion for non-inferiority (least square mean (LSM) treatment difference: −7 mL, CI −45 to 31 mL). GLY+SAL/FP generated a statistically and clinically significant bronchodilation with an improvement of 101 mL in trough FEV1 above that seen with PLA+SAL/FP at week 12 (p<0.001; figure 3). Similarly significant improvements in trough FEV1 were observed at week 4 (87 mL, p<0.001) and week 8 (86 mL, p<0.001).
Figure 3.
Trough forced expiratory volume in 1 s (FEV1) at weeks 4, 8 and 12 (full analysis set). FP, fluticasone propionate; SAL, salmeterol.
Health status
The improvement in SGRQ total score at 12 weeks was significantly better in patients receiving GLY+SAL/FP when compared to PLA+SAL/FP with an LSM treatment difference of −2.15 (95% CI −3.97 to −0.34, p=0.02). There was no statistical difference for the 12-week SGRQ score or in the mean improvements from baseline for GLY+SAL/FP versus TIO+SAL/FP (figure 4).
Figure 4.
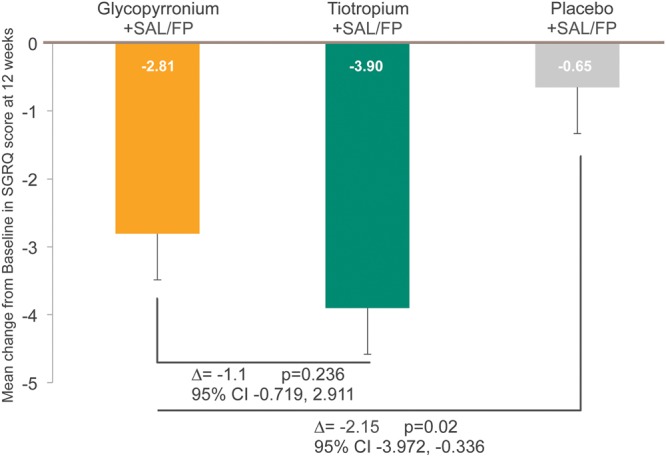
SGRQ-C total scores at 12 weeks. FP, fluticasone propionate; SAL, salmeterol; SGRQ, St George's Respiratory Questionnaire. Data are least-squares means; error bars show standard error.
Rescue medication
Rescue medication use was significantly lower in GLY+SAL/FP patients than PLA+SAL/FP patients over 12 weeks, with a between-group mean difference of −0.72 puffs per day (p<0.001; figure 5A and 5B). The difference between GLY+SAL/FP and TIO+SAL/FP was small and non-significant (figure 5A). Patients receiving GLY+SAL/FP had 8.1% more days without rescue medication than PLA+SAL/FP patients (p<0.001, figure 5B).
Figure 5.
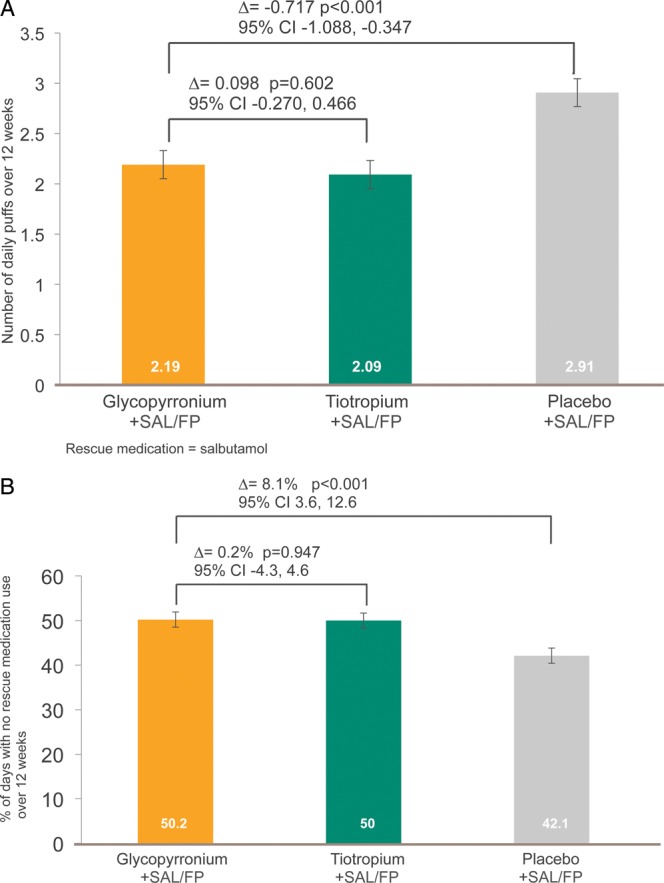
(A) Rescue medication use (puffs per day). (B) Percentage of days without rescue medication use. FP, fluticasone propionate; SAL, salmeterol. Data show least-squares means; error bars show standard error.
Night-time awakening and performance of daily activities
The percentage of nights with no awakenings was high and similar between the different treatment arms: GLY+SAL/FP (83.4%), TIO+SAL/FP (81.6%) and PLA+SAL/FP (82.3%). The percentage of days on which patients were able to perform usual daily activities was also high among all three treatment groups (93.4% for GLY+SAL/FP, 94.6% for TIO+SAL/FP and 90.3% for PLA+SAL/FP). There was a small but significant difference between GLY+SAL/FP and PLA+SAL/FP (LSM treatment difference 3%, p=0.011), while the difference between GLY+SAL/FP and TIO+SAL/FP was non-significant (p=0.31).
Exacerbations
The number of patients experiencing a moderate or severe COPD exacerbation over the 12 weeks of study was small in all three treatment arms: GLY+SAL/FP (29 patients, 11.3%), TIO+SAL/FP (24 patients, 9.3%) and PLA+SAL/FP (32 patients, 12.5%), and there was no statistical difference between the treatment arms.
Safety
There were no significant differences in the number of AEs or SAEs between treatment groups, ranging from 57.4% to 64% and 5.8% to 8.5%, respectively (table 2). There were fewer cardiac-related AEs in the GLY+SAL/FP arm (1.2%) compared to the other treatment arms (3.9% and 2.7%) (table 3). Pneumonia was not reported in the GLY+SAL/FP arm, but did occur in two patients in each of the TIO+SAL/FP and PLA+SAL/FP arms.
Table 2.
Most frequent adverse events (at least 5 patients in any treatment group), serious adverse events (at least 2 patients in any treatment group), death and discontinuations due to adverse events (safety set)
| Glycopyrronium +SAL/FP |
Tiotropium +SAL/FP |
Placebo +SAL/FP |
|
|---|---|---|---|
| N=257 | N=258 | N=257 | |
| Patients with AEs | 150 (58.4%) | 165 (64.0%) | 148 (57.6%) |
| Upper respiratory tract infection | 17 (6.6%) | 13 (5.0%) | 11 (4.3%) |
| Oral candidiasis | 12 (4.7%) | 13 (5.0%) | 9 (3.5%) |
| Lower respiratory tract infection | 7 (2.7%) | 5 (1.9%) | 4 (1.6%) |
| Nasopharyngitis | 3 (1.2%) | 7 (2.7%) | 5 (1.9%) |
| Viral upper respiratory tract infection | 3 (1.2%) | 4 (1.6%) | 5 (1.9%) |
| Sinusitis | 2 (0.8%) | 2 (0.8%) | 5 (1.9%) |
| Cough | 16 (6.2%) | 15 (5.8%) | 11 (4.3%) |
| Oropharyngeal pain | 9 (3.5%) | 10 (3.9%) | 8 (3.1%) |
| Dyspnoea | 7 (2.7%) | 9 (3.5%) | 10 (3.9%) |
| Dysphonia | 6 (2.3%) | 15 (5.8%) | 5 (1.9%) |
| Rhinorrhoea | 6 (2.3%) | 1 (0.4%) | 3 (1.2%) |
| COPD | 0 | 4 (1.6%) | 6 (2.3%) |
| Diarrhoea | 5 (1.9%) | 2 (0.8%) | 2 (0.8%) |
| Dry mouth | 5 (1.9%) | 9 (3.5%) | 2 (0.8%) |
| Nausea | 3 (1.2%) | 9 (3.5%) | 3 (1.2%) |
| Muscle spasms | 11 (4.3%) | 9 (3.5%) | 5 (1.9%) |
| Back pain | 4 (1.6%) | 8 (3.1%) | 5 (1.9%) |
| Fatigue | 0 | 5 (1.9%) | 2 (0.8%) |
| Headache | 3 (1.2%) | 4 (1.6%) | 13 (5.1%) |
| Hypertension | 3 (1.2%) | 6 (2.3%) | 5 (1.9%) |
| Number of SAE(s) | 18 | 36 | 18 |
| Patients with SAE(s) | 15 (5.8%) | 22 (8.5%) | 15 (5.8%) |
| Small intestinal obstruction | 2 (0.8%) | 0 | 0 |
| Chronic obstructive pulmonary disease | 0 | 1 (0.4%) | 2 (0.8%) |
| Atrial fibrillation | 0 | 2 (0.8%) | 1 (0.4%) |
| Pneumonia | 0 | 2 (0.8%) | 2 (0.8%) |
| Death | 0 | 0 | 1 (0.4%) |
| Discontinued due to AE(s) | 14 (5.4%) | 17 (6.6%) | 17 (6.6%) |
AE, adverse event; COPD, chronic obstructive pulmonary disease; FP, fluticasone propionate; SAL, salmeterol; SAE, serious adverse event.
Table 3.
Cardiac disorder adverse events and serious adverse events (safety set)
| Glycopyrronium +SAL/FP |
Tiotropium +SAL/FP |
Placebo +SAL/FP |
|
|---|---|---|---|
| N=257 | N=258 | N=257 | |
| Cardiac disorders: adverse events | 3 (1.2%) | 10 (3.9%) | 7 (2.7%) |
| Arrhythmia | 1 (0.4%) | 0 | 0 |
| Atrial fibrillation | 1 (0.4%) | 2 (0.8%) | 3 (1.2%) |
| Atrial flutter | 1 (0.4%) | 1 (0.4%) | 0 |
| Ischaemic cardiomyopathy | 1 (0.4%) | 0 | 0 |
| Acute coronary syndrome | 0 | 1 (0.4%) | 1 (0.4%) |
| Angina pectoris | 0 | 1 (0.4%) | 2 (0.8%) |
| Atrioventricular block complete | 0 | 1 (0.4%) | 0 |
| Cardiac failure congestive | 0 | 1 (0.4%) | 0 |
| Left ventricular failure | 0 | 1 (0.4%) | 0 |
| Palpitations | 0 | 3 (1.2%) | 0 |
| Tachyarrhythmia | 0 | 1 (0.4%) | 0 |
| Ventricular fibrillation | 0 | 0 | 1 (0.4%) |
| Cardiac disorders: serious adverse events | 1 (0.4%) | 6 (2.3%) | 4 (1.6%) |
| Atrial flutter | 1 (0.4%) | 1 (0.4%) | 0 |
| Acute coronary syndrome | 0 | 1 (0.4%) | 1 (0.4%) |
| Angina pectoris | 0 | 1 (0.4%) | 1 (0.4%) |
| Atrial fibrillation | 0 | 2 (0.8%) | 1 (0.4%) |
| Atrioventricular block complete | 0 | 1 (0.4%) | 0 |
| Cardiac failure congestive | 0 | 1 (0.4%) | 0 |
| Tachyarrhythmia | 0 | 1 (0.4%) | 0 |
| Ventricular fibrillation | 0 | 0 | 1 (0.4%) |
FP, fluticasone propionate; SAL, salmeterol.
Three deaths were reported during the study, one during run-in (congestive cardiac failure), one in the PLA+SAL/FP arm (ventricular fibrillation) and one in the TIO+SAL/FP arm (multi-organ failure, ischaemic hepatitis and pneumonia).
Discussion
Combining inhaler therapies from different classes of drugs for COPD is commonly recommended (GOLD 2014) and often pursued.1 22 23 However, it is important to know if there is merit in doing so; in particular if there is comparable efficacy for medications from the same therapeutic class and whether therapy with GLY+LABA/ICS has advantages over therapy with LABA/ICS in patients with moderate to severe disease. The GLISTEN study demonstrates that TIO and GLY are comparable when added to a LABA/ICS combination in moderate to severe COPD patients, but more importantly shows the superiority of using GLY+LABA/ICS over using a LABA/ICS alone. This is the first time this has been effectively demonstrated.
Results for the pre-specified primary outcome (trough FEV1 at 12 weeks) demonstrated the non-inferiority of GLY to TIO when combined with SAL/FP. Comparable outcomes for GLY versus TIO were also demonstrated for all other outcomes measures: health status, rescue medication use, nocturnal symptoms and activity performance. These findings are consistent with results for GLY versus TIO non-inferiority studies in a monotherapy setting, as demonstrated in both open-label17 and blinded16 randomised controlled trials. Although not measured in the current study, GLY has been shown in other studies to be superior to TIO in terms of time to onset and on peak FEV1 results.16 17
GLY in combination with SAL/FP demonstrated statistically and clinically significant improvements in lung function compared to PLA+SAL/FP at 4, 8 and 12 weeks. In addition, over 12 weeks GLY+SAL/FP provided statistically significant improvements in health status, symptom relief and rescue medication in comparison to SAL/FP alone. Furthermore, there was no increase in AEs when GLY was used with SAL/FP and specifically there was no increase in cardiovascular events or any other SAEs. This adds to existing clinical trial data concerning GLY safety and tolerability.4 17
There have been many studies comparing LABA/ICS therapy with individual monotherapies (ICS, LABA, LAMA). A systematic review by Kew et al11 of 71 randomised controlled trials (n=73 062; >6 months’ duration) comparing LABA, LAMA, ICS or combined LABA/ICS and PLA, showed health status and lung function were improved most if taking LABA/ICS. The review also concluded that LAMAs and LABAs had similar efficacy11 although triple therapies were not included in their analysis.
At the time of writing there are seven published studies assessing triple therapy.15 24–29 These studies were identified by systematic reviews14 30 and our own literature searches. Three of the seven compared triple therapy with TIO monotherapy.25 28 29 Of these, two28 29 used SAL/FP as their LABA/ICS and one formoterol/budesonide;25 they were 3–6 months in duration and one was open label.29 In these studies triple therapy was better than TIO monotherapy. Another study compared triple therapy with the dual bronchodilator combination of TIO+SAL (without ICS).24 Over 12 months there was no reduction in exacerbations, but there was improvement in health status and lung function with triple therapy. However, the authors acknowledged a large number of patient withdrawals and use of inappropriate treatments during the study, creating some doubt about the final data.
We were able to identify only three studies comparing triple therapy with LABA/ICS therapy.15 26 27 One26 was a 2-week treatment period crossover study of 41 patients, in which only 66% of patients finished the study. Another15 was a 3-month pilot study with 26–29 patients in each arm and showed no superiority of any one treatment, while the third study, published in Chinese,27 is a 12-month non-blinded study that showed no difference between active treatments. Despite their study limitations, all three showed some positive benefits from triple therapy. Studies currently presented in abstract form at international meetings suggest further positive evidence for using triple therapy may emerge.31 On this background, the GLISTEN study is the first to provide strong evidence for using a LAMA with an LABA/ICS combination as it demonstrated significant benefits in lung function, health status and rescue medication when GLY was combined with SAL/FP. The extent to which these results can be extrapolated to other β2-receptor agonists and corticosteroids will require further studies.
Improving daily symptoms, health status and lung function are important goals in COPD therapy, while reducing exacerbations is equally important. These outcomes may be independent or interactive. The data from studies addressing triple therapy, including this one, show less obvious impact on exacerbations and more on health status and lung function. A recent study32 suggests that removing ICS does little to change exacerbation rates but is associated with an incremental reduction in FEV1, suggesting a complex interplay between drug therapy and clinical outcomes that needs more careful evaluation.
There are potential limitations in the GLISTEN study. Both moderate and severe COPD patients were enrolled despite at the time of the study triple therapy only being recommended for patients with severe obstruction and/or frequent exacerbations (two or more/year or one requiring hospitalisation).19 This means that some patients with moderate obstruction and infrequent exacerbations may have been enrolled. This enrolment decision allowed the efficacy of the treatments to be assessed in a broader spectrum of disease severity as these patients are commonly treated in real world practice with LABA/ICS therapy.22 23 This is reflected in the baseline characteristics of the study populations (table 1). About 60% of patients were taking ICS prior to recruitment into the trial, although only half of these had experienced exacerbations and had FEV1 <50% of predicted. Another potential limitation is that despite patients with a history of asthma and onset of symptoms prior to the age of 40 being excluded, the degree of FEV1 reversibility was relatively high (average 22%). This may be due to adding ipratropium to salbutamol for reversibility testing; however, such findings have also occurred in other comparably designed COPD studies.33 34 Improvements in health status as measured by SGRQ scores were statistically significant, favouring GLY+SAL/FP over SAL/FP alone. Although the minimum clinically important difference (MCID) of four points was not reached, it is important to appreciate that the MCIDs for SGRQ were determined from placebo-controlled studies35 and may not be appropriate for assessing differences between two active treatment arms. Furthermore, the study duration of 12 weeks may not have been sufficient to maximise this benefit as lung function parameters showed a progressive increase during the course of the study.
Conclusion
Once-daily GLY demonstrated similar effects to TIO when combined with SAL/FP in patients with moderate and severe COPD. GLY when used with SAL/FP demonstrated superior efficacy compared with SAL/FP alone in terms of lung function, health status and rescue medication use in patients with moderate and severe COPD. This is the first study that conclusively demonstrates the benefits of triple therapy (LAMA+LABA/ICS) compared to LABA/ICS as well as demonstrating the efficacy and safety of GLY when combined with an LABA/ICS.
Supplementary Material
Acknowledgments
The authors thank the patients who participated and the staff at the participating clinical centres.
Footnotes
Collaborators: The Glisten study group principal investigators: Ainslie Waddell, Alexander Daniel, Alireza Khoussousi, Andrew Springfield, Andrew Veale, Anthony Neil Graham, Brad Gallagher, Braj Raj Pande, Brendan O'Kane, Christopher Jones, Claudio Baldi, Colin Helm, Conor O'Dochartaigh, Daniel Chambers, Dean Quinn, Derek Yull, Dhanalakshi Karthigesu, Edward Then, Frank Graham, Fred Faigenbaum, Geetha Geddam, Gillian Cameron, Hans Blom, Hershel Goldman, Hilary Snell, Imagard Chia, James Jeong, James Liew, James Salvaris, Jason Pryke, Jim Reid, John Kolbe, John O'Sullivan, John Pak, John Upham, Joseph Feiber, Judith O'Malley Ford, Kevin Yong, Kyle Perrin, Lawrence Noonan, Len Atlas, Louise Murdoch, Margaret Pearce, Mark Bloch, Mark Holmes, Michael Chia, Michael Epton, Michelle Leadston, MK Tandon, Mohan Chitgopeker, Naomi Liebenberg, Neil Hendry, Olakunle Olaniyi, Omesh Singh, Peter Kendall, Peter Van Niekerk, Rodney Willet, Ronald Tomlins, Salven Pillay, Sammy Sharifeh, Simon Carson, Stephen Bingham, Ted Walford, Tersia Erasmus, Trevor Claridge, Zofia Hess.
Contributors: PAF was the principal investigator of the study. PAF and PJT contributed equally to the generation of this manuscript. The following authors were the main investigators in the collaborating centres and directly involved in patient recruitment and data collection: PAF, PJT, RR, CLC, PB and PD. CF and NK were involved in the design, coordination and project execution of the study. All authors reviewed and approved the final version of the manuscript.
Funding: The study was sponsored and funded by Novartis Pharmaceuticals Australia Pty Limited.
Competing interests: In the past 5 years PAF has received honoraria for advisory work and lectures from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, MediMark International, Menarini, MundiPharma, Novartis, Remedy Healthcare, Servier and Takeda; and has received travel grants to conferences and other meetings from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Global Alliance for Respiratory Disease, Lung Foundation Australia, MediMark International, Menarini and Novartis; no payment was received for preparation of this manuscript. Over the last 5 years, PJT has sat on advisory boards for Novartis and Astra Zeneca and has given public lectures sponsored by Astra Zeneca and Novartis. No personal payments were received with respect to this study or its production. RR has participated in research projects funded by Bioxyne, Novartis and GlaxoSmithKline with grants paid to his employing institution. RR was the recipient of a travel grant from Novartis. CLC has participated in research projects funded by Novartis, Boehringer-Ingelheim, Grifols, Bayer and Pearl Therapeutics with grants paid to the institution where she is employed. PB has received honoraria from GSK, AZ, Novartis and BI for presenting at medical meetings and symposia, and has contributed to clinical research trials funded by the same and other pharmaceutical companies. PD participated in research projects funded by Sanofi and Novartis. CF and NK are full-time employees of Novartis Pharmaceuticals Australia.
Ethics approval: The Therapeutic Goods Administration (TGA) approved this study.
Provenance and peer review: Not commissioned; internally peer reviewed.
Contributor Information
Collaborators: Ainslie Waddell, Alexander Daniel, Alireza Khoussousi, Andrew Springfield, Andrew Veale, Anthony Neil Graham, Brad Gallagher, Braj Raj Pande, Brendan O'Kane, Christopher Jones, Claudio Baldi, Colin Helm, Conor O'Dochartaigh, Daniel Chambers, Dean Quinn, Derek Yull, Dhanalakshi Karthigesu, Edward Then, Frank Graham, Fred Faigenbaum, Geetha Geddam, Gillian Cameron, Hans Blom, Hershel Goldman, Hilary Snell, Imagard Chia, James Jeong, James Liew, James Salvaris, Jason Pryke, Jim Reid, John Kolbe, John O'Sullivan, John Pak, John Upham, Joseph Feiber, Judith O'Malley Ford, Kevin Yong, Kyle Perrin, Lawrence Noonan, Len Atlas, Louise Murdoch, Margaret Pearce, Mark Bloch, Mark Holmes, Michael Chia, Michael Epton, Michelle Leadston, MK Tandon, Mohan Chitgopeker, Naomi Liebenberg, Neil Hendry, Olakunle Olaniyi, Omesh Singh, Peter Kendall, Peter Van Niekerk, Rodney Willet, Ronald Tomlins, Salven Pillay, Sammy Sharifeh, Simon Carson, Stephen Bingham, Ted Walford, Tersia Erasmus, Trevor Claridge, and Zofia Hess
References
- 1.The Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD), 2014. http://www.goldcopd.org.
- 2.Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008;359:1543–54. 10.1056/NEJMoa0805800 [DOI] [PubMed] [Google Scholar]
- 3.Karner C, Chong J, Poole P. Tiotropium versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012;7:CD009285 10.1002/14651858.CD009285.pub3 [DOI] [PubMed] [Google Scholar]
- 4.Beeh KM, Singh D, Di Scala L, et al. Once-daily NVA237 improves exercise tolerance from the first dose in patients with COPD: the GLOW3 trial. Int J Chron Obstruct Pulmon Dis 2012;7:503–13. 10.2147/COPD.S32451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calverley P, Pauwels R, Vestbo J, et al. Combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial. Lancet 2003;361:449–56. 10.1016/S0140-6736(03)12459-2 [DOI] [PubMed] [Google Scholar]
- 6.Donohue JF, Fogarty C, Lotvall J, et al. Once-daily bronchodilators for chronic obstructive pulmonary disease: indacaterol versus tiotropium. Am J Respir Crit Care Med 2010;182:155–62. 10.1164/rccm.200910-1500OC [DOI] [PubMed] [Google Scholar]
- 7.Dahl R, Chung KF, Buhl R, et al. Efficacy of a new once-daily long-acting inhaled beta2-agonist indacaterol versus twice-daily formoterol in COPD. Thorax 2010;65:473–9. 10.1136/thx.2009.125435 [DOI] [PubMed] [Google Scholar]
- 8.Calverley PM, Boonsawat W, Cseke Z, et al. Maintenance therapy with budesonide and formoterol in chronic obstructive pulmonary disease. Eur Respir J 2003;22:912–19. 10.1183/09031936.03.00027003 [DOI] [PubMed] [Google Scholar]
- 9.Mahler DA, Wire P, Horstman D, et al. Effectiveness of fluticasone propionate and salmeterol combination delivered via the Diskus device in the treatment of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2002;166:1084–91. 10.1164/rccm.2112055 [DOI] [PubMed] [Google Scholar]
- 10.Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007;356: 775–89. 10.1056/NEJMoa063070 [DOI] [PubMed] [Google Scholar]
- 11.Kew KM, Dias S, Cates CJ. Long-acting inhaled therapy (beta-agonists, anticholinergics and steroids) for COPD: a network meta-analysis. Cochrane Database Syst Rev 2014;3:CD010844 10.1002/14651858.CD010844.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nannini LJ, Poole P, Milan SJ, et al. Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2013;11:CD003794 10.1002/14651858.CD003794.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wedzicha JA, Calverley PM, Seemungal TA, et al. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med 2008;177:19–26. 10.1164/rccm.200707-973OC [DOI] [PubMed] [Google Scholar]
- 14.Karner C, Cates CJ. Combination inhaled steroid and long-acting beta(2)-agonist in addition to tiotropium versus tiotropium or combination alone for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2011;(3):CD008532 10.1002/14651858.CD008532.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cazzola M, Ando F, Santus P, et al. A pilot study to assess the effects of combining fluticasone propionate/salmeterol and tiotropium on the airflow obstruction of patients with severe-to-very severe COPD. Pulm Pharmacol Ther 2007;20:556–61. 10.1016/j.pupt.2006.06.001 [DOI] [PubMed] [Google Scholar]
- 16.Chapman KR, Beeh KM, Beier J, et al. A blinded evaluation of the efficacy and safety of glycopyrronium, a once-daily long-acting muscarinic antagonist, versus tiotropium, in patients with COPD: the GLOW5 study. BMC Pulm Med 2014;14:4 10.1186/1471-2466-14-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kerwin E, Hebert J, Gallagher N, et al. Efficacy and safety of NVA237 versus placebo and tiotropium in patients with COPD: the GLOW2 study. Eur Respir J 2012;40:1106–14. 10.1183/09031936.00040712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D'Urzo A, Ferguson GT, van Noord JA, et al. Efficacy and safety of once-daily NVA237 in patients with moderate-to-severe COPD: the GLOW1 trial. Respir Res 2011;12:156 10.1186/1465-9921-12-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Global Initiative for Chronic Obstructive Lung Disease (GOLD): Global strategy for diagnosis, management and prevention of COPD, 2010. http://www.goldcopd.org/Guidelines/guideline-2010-gold-report.html.
- 20.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319–38. 10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 21.Medical Dictionary of Medical Activities (MedDRA). Version 15.1, 2012.
- 22.Bourbeau J, Sebaldt RJ, Day A, et al. Practice patterns in the management of chronic obstructive pulmonary disease in primary practice: the CAGE study. Can Respir J 2008;15:13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White P, Thornton H, Pinnock H, et al. Overtreatment of COPD with inhaled corticosteroids—implications for safety and costs: cross-sectional observational study. PLoS One 2013;8:e75221 10.1371/journal.pone.0075221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aaron SD, Vandemheen KL, Fergusson D, et al. Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2007;146:545–55. 10.7326/0003-4819-146-8-200704170-00152 [DOI] [PubMed] [Google Scholar]
- 25.Welte T, Miravitlles M, Hernandez P, et al. Efficacy and tolerability of budesonide/formoterol added to tiotropium in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2009;180:741–50. 10.1164/rccm.200904-0492OC [DOI] [PubMed] [Google Scholar]
- 26.Singh D, Brooks J, Hagan G, et al. Superiority of “triple” therapy with salmeterol/fluticasone propionate and tiotropium bromide versus individual components in moderate to severe COPD. Thorax 2008;63:592–8. 10.1136/thx.2007.087213 [DOI] [PubMed] [Google Scholar]
- 27.Fang LZ, Liang X, Zhang JQ, et al. [Combination of inhaled salmeterol/fluticasone and tiotropium in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial]. Zhonghua Jie He He Hu Xi Za Zhi 2008;31:811–14. [PubMed] [Google Scholar]
- 28.Hanania NA, Crater GD, Morris AN, et al. Benefits of adding fluticasone propionate/salmeterol to tiotropium in moderate to severe COPD. Respir Med 2012;106:91–101. 10.1016/j.rmed.2011.09.002 [DOI] [PubMed] [Google Scholar]
- 29.Jung KS, Park HY, Park SY, et al. Comparison of tiotropium plus fluticasone propionate/salmeterol with tiotropium in COPD: a randomized controlled study. Respir Med 2012;106:382–9. 10.1016/j.rmed.2011.09.004 [DOI] [PubMed] [Google Scholar]
- 30.Rodrigo GJ, Plaza V, Castro-Rodriguez JA. Comparison of three combined pharmacological approaches with tiotropium monotherapy in stable moderate to severe COPD: a systematic review. Pulm Pharmacol Ther 2012;25:40–7. 10.1016/j.pupt.2011.10.006 [DOI] [PubMed] [Google Scholar]
- 31.Siler T, Kerwin E, Sousa A, et al. Efficacy and safety of once-daily umeclidinium added to fluticasone furoate/vilanterol in chronic obstructive pulmonary disease: results of two replicate randomized 12-week studies. Chest 2014;146(4_MeetingAbstracts):340A 10.1378/chest.2059234 [DOI] [Google Scholar]
- 32.Magnussen H, Watz H, Kirsten A, et al. Stepwise withdrawal of inhaled corticosteroids in COPD patients receiving dual bronchodilation: WISDOM study design and rationale. Respir Med 2014;108:593–9. 10.1016/j.rmed.2014.01.002 [DOI] [PubMed] [Google Scholar]
- 33.Bateman ED, Ferguson GT, Barnes N, et al. Dual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE study. Eur Respir J 2013;42:1484–94. 10.1183/09031936.00200212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Decramer M, Anzueto A, Kerwin E, et al. Efficacy and safety of umeclidinium plus vilanterol versus tiotropium, vilanterol, or umeclidinium monotherapies over 24 weeks in patients with chronic obstructive pulmonary disease: results from two multicentre, blinded, randomised controlled trials. Lancet Respir Med 2014;2:472–86. 10.1016/S2213-2600(14)70065-7 [DOI] [PubMed] [Google Scholar]
- 35.Jones PW, Beeh KM, Chapman KR, et al. Minimal clinically important differences in pharmacological trials. Am J Respir Crit Care Med 2014;189:250–5. 10.1164/rccm.201310-1863PP [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.