Abstract
Background:
Alcohol is a risk factor for cancer of the oral cavity, pharynx, oesophagus, colorectum, liver, larynx and female breast, whereas its impact on other cancers remains controversial.
Methods:
We investigated the effect of alcohol on 23 cancer types through a meta-analytic approach. We used dose–response meta-regression models and investigated potential sources of heterogeneity.
Results:
A total of 572 studies, including 486 538 cancer cases, were identified. Relative risks (RRs) for heavy drinkers compared with nondrinkers and occasional drinkers were 5.13 for oral and pharyngeal cancer, 4.95 for oesophageal squamous cell carcinoma, 1.44 for colorectal, 2.65 for laryngeal and 1.61 for breast cancer; for those neoplasms there was a clear dose–risk relationship. Heavy drinkers also had a significantly higher risk of cancer of the stomach (RR 1.21), liver (2.07), gallbladder (2.64), pancreas (1.19) and lung (1.15). There was indication of a positive association between alcohol consumption and risk of melanoma and prostate cancer. Alcohol consumption and risk of Hodgkin's and Non-Hodgkin's lymphomas were inversely associated.
Conclusions:
Alcohol increases risk of cancer of oral cavity and pharynx, oesophagus, colorectum, liver, larynx and female breast. There is accumulating evidence that alcohol drinking is associated with some other cancers such as pancreas and prostate cancer and melanoma.
Keywords: alcohol, meta-analysis, dose–response, epidemiology
It is estimated that alcohol is responsible for ∼2.5 million deaths each year and for 4.5% of the global burden of disease and injury (World Health Organization, 2011). Alcohol is an established causal factor for cirrhosis of the liver, epilepsy, poisoning, road traffic accidents, violence and some types of cancer. With regard to cancer, alcohol consumption was estimated to have caused ∼500 000 cancer deaths worldwide in 2004 (Rehm et al, 2009), and accounted for 4.4% of cancer deaths in China in 2005 (Liang et al, 2010) and 3.5% in the United States in 2009 (Nelson et al, 2013). In Europe, a large heterogeneity was observed in patterns and trends of alcohol consumption between countries (Boniol and Autier, 2010; La Vecchia et al, 2014), with proportion of cancer cases attributable to alcohol varying accordingly (Boffetta et al, 2006).
The first published exploratory study on the carcinogenic effect of alcohol dates back to the beginning of the twentieth century, when an excess of cancer mortality due to alcohol consumption was reported (Newsholme, 1903). In the wake of the accumulating evidence on the carcinogenicity of alcohol (Lamy, 1910; Martinez, 1969; Olsen et al, 1985; Trichopoulos et al, 1987), in 1988 the International Agency for Research on Cancer (IARC) listed alcohol among the carcinogens for oral cavity and pharynx, oesophagus, liver and larynx (IARC Working Group, 1988). Afterwards, given the consolidating data for a link between alcohol and cancer of colorectum and female breast (Hamajima et al, 2002; Ferrari et al, 2007), these two sites were added to the above list in 2010 (IARC Working Group, 2010). The results on the association between alcohol and cancer at other sites, such as stomach, pancreas and prostate, are still conflicting.
Given the vast and sometimes contradictory literature on the carcinogenicity of alcohol, our group has conducted in recent years a series of meta-analytic studies on the association between alcohol and several single cancers (Islami et al, 2010, 2011; Tramacere et al, 2010, 2012a, 2012b, 2012c, 2012d; Turati et al, 2010a, 2010b; Bagnardi et al, 2011; Fedirko et al, 2011; Bellocco et al, 2012; Pelucchi et al, 2012; Seitz et al, 2012; Rota et al, 2012a, 2012b; Galeone et al, 2013) to shed light on the subject. With the present meta-analysis, we aim to provide a more global picture of the association between alcohol drinking and a large variety of cancers.
Materials and methods
Search strategy
We performed a literature search in MEDLINE, ISI Web of Science (Science Citation Index Expanded) and EMBASE for epidemiological studies published online before September 2012. For the sake of completeness, we also reviewed references from all relevant studies, reviews and meta-analyses published on the alcohol–cancer association to identify additional studies. We limited our search to solid tumours. The key words used for the literature search are reported in Supplementary Material S1. We considered only studies published in English.
Inclusion criteria
Articles were included in the meta-analysis only if they satisfied the following criteria:
(1) Case–control, cohort or nested case–control studies published as original articles (abstracts, letters, reviews and meta-analyses were excluded).
(2) Studies that reported findings expressed as odds ratio (OR), relative risk (RR) or hazard ratio (or reporting sufficient data to compute them) for at least two levels of alcohol consumption vs nondrinkers and/or occasional drinkers.
(3) Studies that reported standard errors or confidence intervals (CIs) of the risk estimates or provided sufficient data to calculate them.
We excluded studies reporting on a specific type of alcoholic beverage only (e.g., beer only) because in those studies the nondrinkers of a specific beverage could possibly be drinkers of other types of alcoholic beverages.
We included all cancer sites for which five or more papers were available.
Data abstraction
The reports available for each cancer site were independently reviewed by one of the authors to determine the eligibility of each article for inclusion in the meta-analysis. Doubts or disagreements were resolved by consensus among all the investigators. When the results of the same study were published in more than one paper, only the most recent and/or complete article was included in the analysis. However, when results from a study were published in a single paper but also within a pooled analysis that included other unpublished results, we chose the pooled analysis, even if the individual study provided the most detailed or recent information.
For each included study, we extracted details on study design, outcome, country, gender, RR estimates and 95% CIs, adjustment variables and, when available, the number of cases and controls (case–control studies) or number of events and subjects at risk/person-years (cohort studies) for the reported exposure levels. Case–control studies nested within prospective cohorts were categorised as case–control studies. We also recorded whether the reference category of nondrinkers included occasional drinkers or not. Where possible, separate risk estimates were extracted for men and women.
Data extraction from the original studies for the meta-analysis was carried out according to the following procedure. First, as different studies used different units of measure to express alcohol consumption (g, ml, ounces or drinks consumed every day, week, month or year), we used g per day as a standard measure of ethanol intake using the following equivalencies: 0.8 g ml−1, 28 g per ounce and 12.5 g per drink. Second, as the levels of consumption were often given by a range, the value x of exposure was assigned as the midpoints of the ranges of the reported categories of alcohol intake (as suggested by Berlin et al, 1993; the x values were calculated as 1.2 times the lower bound for the open-ended upper category). We decided to consider as light, moderate and heavy drinking every interval whose midpoint was respectively ⩽12.5, ⩽50 and >50 g per day of alcohol. As several studies reported two or more adjusted risk estimates for a single dose category (e.g., 6 and 12 g per day for light drinking) we combined them into a single estimate using the method for pooling nonindependent estimates within a single study described by Hamling et al (2008). This method uses the number of exposed to different levels of alcohol and nonexposed subjects and the associated reported risk estimates to derive a set of pseudo-numbers of cases and controls/subjects at risk by taking into account the correlation between the original estimates due to the common reference group. These pseudo-numbers can then be used to calculate a single pooled adjusted risk estimate and its 95% CI.
Statistical methods
Because cancer is a relatively rare outcome, we assumed that ORs, risk ratios and rate ratios were all comparable estimates of the RR. When available, we used the risk estimates adjusted for the main site-specific confounders. Otherwise, we calculated the unadjusted RRs from the raw data presented in the paper. Measures of association and the corresponding CIs were translated into log(RR)s and their variances (Greenland, 1987).
We computed a pooled RR of site-specific cancer for light drinkers vs nondrinkers, moderate drinkers vs nondrinkers and heavy drinkers vs nondrinkers using random-effects models. We used random-effects models to estimate pooled RRs in order to take into account the heterogeneity, although small, of the risk estimates. Each study log(RR) was weighted by the inverse of its variance plus the between-study variance component τ2. The moment estimator of τ2 was used (DerSimonian and Laird, 1986).
We evaluated the statistical heterogeneity among studies using I2, the proportion of total variation contributed by between-study variance (Higgins and Thompson, 2002). We carried out subgroup analyses and meta-regression models to investigate potential sources of between-study heterogeneity (i.e., study design, gender, geographic area and publication year). Only cancer sites for which more than 10 studies were available were considered in the subgroup analyses. We tested the overall difference of summary estimates among subgroups using a linear model including as the dependent variable the logarithm of the pooled estimate and as factors the dose (light, moderate or heavy) and the group (e.g., study design: case–control or cohort). The model was weighted by the inverse of the variance of the pooled estimate. The F-statistics associated with group was taken as a global test of heterogeneity of pooled estimates between strata. Finally, we carried out a dose–risk analysis using a random-effect meta-regression model based on a nonlinear dose–response relationship framework (Rota et al, 2010), providing the best fitting two-term fractional polynomial model. The method is based on a two-step process. First, two-term fractional polynomial models are fitted within each study included in the meta-analysis, taking into account the correlation between the reported estimates for different exposure levels, as described by Greenland and Longnecker (1992). Second, the pooled dose–response relationship is estimated considering the between-studies heterogeneity, using a bivariate random-effects model.
We performed all analyses with SAS software, version 9.1 (SAS Institute Inc., Cary, NC, USA) and R-software (R Development Core Team, 2008). All P-values were two sided.
Results
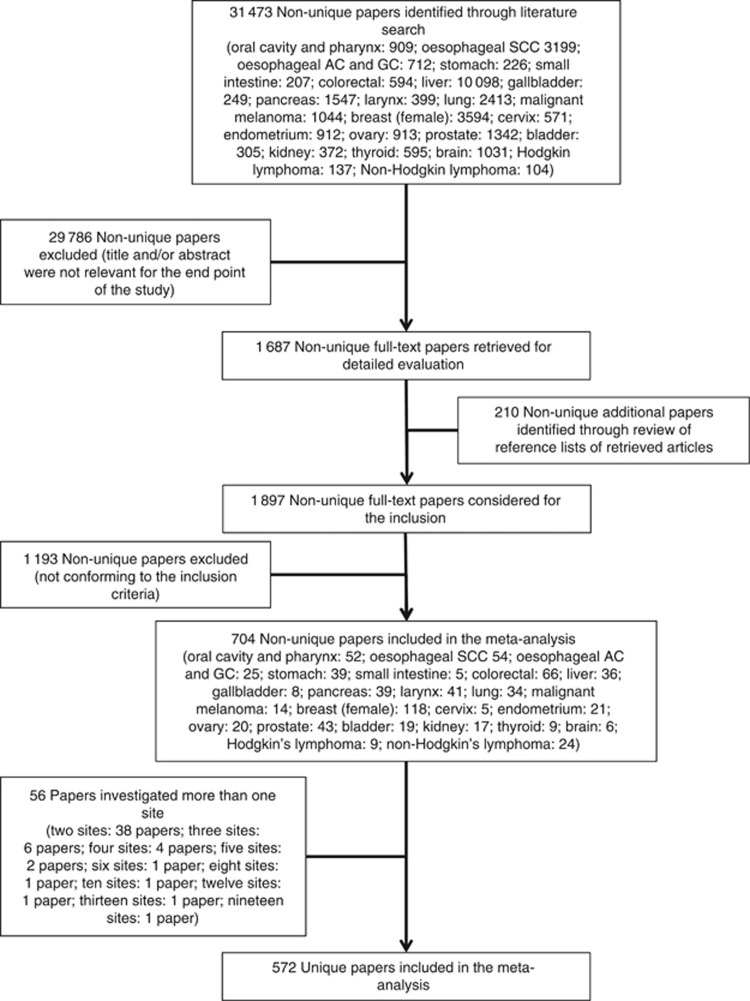
A total of 572 studies published between 1956 and 2012, including a total of 486 538 cancer cases, met the inclusion criteria and were analysed in the present study (Table 1 and Figure 1): 409 (71.5%) were case–control studies and 163 (28.5%) cohort studies; 541 (94.6%) reported incidence and 31 (5.4%) mortality as the outcome of interest; 236 (41.3%) were conducted in North America, 184 (32.2%) in Europe, 101 in Asia (17.7%), 51 (8.9%) in mixed or other areas; 219 (38.3%) reported estimates for men, 256 (44.8%) for women and 179 (31.3%) for both men and women together; 297 (51.9%) reported adjusted estimates whereas 138 (24.1%) included occasional drinkers in the reference category together with abstainers.
Table 1. Characteristics of studies included in the meta-analysis.
|
Study design |
Outcome |
Area |
Sexa |
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cancer site | No. of studies (cases in drinking categories/cases in reference category) | Cohort | C–C | Incidence | Death | Europe | North America | Asia | Others /mixed | M | W | M+W | Adjusted estimatesb | Occasional drinker in reference category |
| Oral cavity and pharynx | 52 (13 895/4942) | 5 | 47 | 49 | 3 | 18 | 15 | 12 | 7 | 29 | 9 | 20 | 41 | 20 |
| Oesophageal SCC | 54 (10 633/3685) | 13 | 41 | 47 | 7 | 13 | 13 | 23 | 5 | 31 | 9 | 19 | 32 | 21 |
| Oesophageal AC and gastric cardia | 25 (4247/1480) | 4 | 21 | 25 | 0 | 9 | 10 | 4 | 2 | 6 | 2 | 18 | 13 | 5 |
| Stomach | 39 (17 346/8612) | 19 | 20 | 33 | 5 | 12 | 8 | 16 | 3 | 20 | 7 | 17 | 27 | 7 |
| Small intestine | 5 (563/321) | 1 | 4 | 4 | 1 | 2 | 2 | 1 | 0 | 1 | 1 | 4 | 4 | 1 |
| Colorectum | 66 (26 932/14 783) | 33 | 33 | 57 | 9 | 13 | 27 | 24 | 2 | 37 | 25 | 22 | 32 | 15 |
| Liver | 36 (8879/4086) | 9 | 27 | 30 | 6 | 9 | 8 | 18 | 1 | 16 | 9 | 19 | 14 | 7 |
| Gallbladder | 8 (410/470) | 4 | 4 | 5 | 3 | 0 | 3 | 5 | 0 | 5 | 4 | 3 | 6 | 1 |
| Pancreas | 39 (14 935/12 391) | 18 | 21 | 30 | 9 | 11 | 16 | 9 | 3 | 20 | 15 | 16 | 28 | 7 |
| Larynx | 41 (7059/2575) | 3 | 38 | 40 | 1 | 20 | 15 | 4 | 2 | 25 | 3 | 15 | 21 | 22 |
| Lung | 34 (26 509/11 914) | 18 | 16 | 26 | 8 | 4 | 14 | 12 | 4 | 22 | 11 | 9 | 31 | 8 |
| Malignant melanoma | 14 (4631/1465) | 2 | 12 | 14 | 0 | 5 | 6 | 0 | 3 | 3 | 4 | 9 | 7 | 5 |
| Breast (female) | 118 (117 317/48 433) | 43 | 75 | 110 | 8 | 41 | 57 | 9 | 11 | 0 | 118 | 0 | 41 | 15 |
| Cervix | 5 (704/884) | 2 | 3 | 4 | 1 | 1 | 2 | 2 | 0 | 0 | 5 | 0 | 0 | 0 |
| Endometrium | 21 (8824/4646) | 8 | 13 | 21 | 0 | 8 | 11 | 2 | 0 | 0 | 21 | 0 | 9 | 1 |
| Ovary | 20 (10 382/5019) | 4 | 16 | 20 | 0 | 7 | 11 | 0 | 2 | 0 | 20 | 0 | 16 | 1 |
| Prostate | 43 (34 065/8593) | 20 | 23 | 39 | 4 | 11 | 24 | 5 | 3 | 43 | 0 | 0 | 11 | 11 |
| Bladder | 19 (7 190/3 473) | 3 | 16 | 19 | 0 | 8 | 9 | 2 | 0 | 12 | 7 | 6 | 15 | 5 |
| Kidney | 17 (9 111/3782) | 6 | 11 | 15 | 2 | 7 | 6 | 2 | 2 | 11 | 9 | 5 | 5 | 5 |
| Thyroid | 9 (2503/1582) | 6 | 3 | 9 | 0 | 2 | 6 | 0 | 1 | 3 | 7 | 2 | 4 | 1 |
| Brain | 6 (1366/442) | 4 | 2 | 5 | 1 | 1 | 1 | 1 | 3 | 1 | 2 | 4 | 5 | 0 |
| Hodgkin's lymphoma | 9 (931/404) | 2 | 7 | 9 | 0 | 5 | 2 | 1 | 1 | 1 | 0 | 8 | 7 | 5 |
| Non-Hodgkin's lymphoma | 24 (9534/4590) | 9 | 15 | 23 | 1 | 9 | 10 | 3 | 2 | 9 | 8 | 11 | 13 | 8 |
| Totalc | 572 (337 966/148 572) | 163 | 409 | 541 | 31 | 184 | 236 | 101 | 51 | 219 | 256 | 179 | 297 | 138 |
Abbreviations: AC=adenocarcinoma; C–C=case–control; M=men; SCC=squamous cell carcinoma; W=women.
Studies that reported gender-specific estimates were counted twice (in both M and W columns).
The site-specific list of main confounders considered is reported in Supplementary Material S2.
Fifty-six studies reported more than one site-specific estimate, and therefore numbers in columns do not sum up to totals (with the exception of the number of cases in brackets).
Figure 1.
Flowchart of selection of studies for inclusion in meta-analysis.
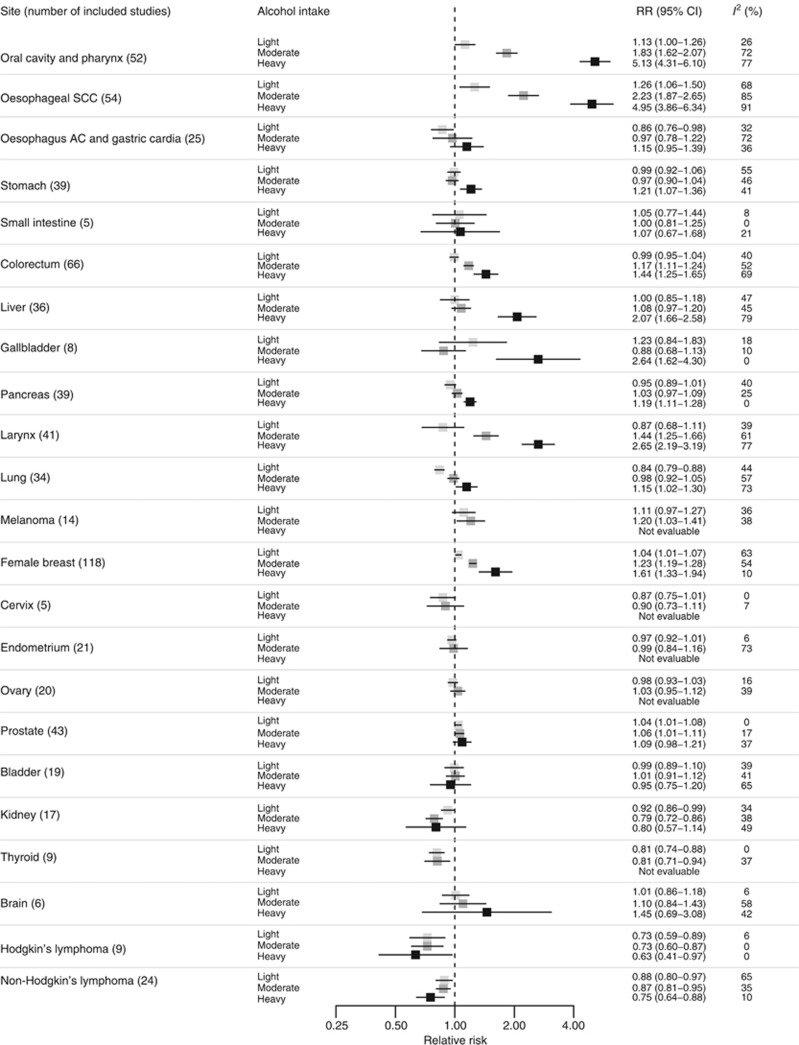
In Figure 2, we reported the pooled RR estimates for light, moderate and heavy drinking as compared with nondrinkers and occasional drinkers. Every category of alcohol consumption, from light to heavy drinking, was associated with an increased risk of cancer – in a dose–risk manner – of oral cavity and pharynx (RR 1.13 (95% CI 1.00–1.26) for light, RR 1.83 (1.62–2.07) for moderate and 5.13 (4.31–6.10) for heavy drinking; 52 studies), oesophagus (squamous cell carcinoma (SCC); RR 1.26 (1.06–1.50) for light, RR 2.23 (1.87–2.65) for moderate and 4.95 (3.86–6.34) for heavy drinking; 54 studies) and female breast (RR 1.04 (1.01–1.07) for light, RR 1.23 (1.19–1.28) for moderate and 1.61 (1.33–1.94) for heavy drinking; 118 studies). Moderate and heavy drinking, but not light drinking, was associated with an increased risk of cancer of colorectum (RR 1.17 (95% CI 1.11–1.24) for moderate and 1.44 (1.25–1.65) for heavy drinking; 66 studies) and larynx (RR 1.44 (1.25–1.66) for moderate and 2.65 (2.19–3.19) for heavy drinking; 41 studies). Heavy drinking was significantly associated with an increased risk of cancer of liver (RR 2.07 (95% CI 1.66–2.58); 36 studies), stomach (RR 1.21 (1.07–1.36); 39 studies), pancreas (RR 1.19 (1.11–1.28); 39 studies), lung (RR 1.15 (1.02–1.30); 34 studies) and gallbladder (RR 2.64 (1.62–4.30); 8 studies), as compared with nondrinkers and occasional drinkers. There was little indication of an association between consumption of alcohol and risk of melanoma (RR 1.11 (95% CI 0.97–1.27) for light and 1.20 (1.03–1.41) for moderate drinking; 14 studies) and prostate cancer (RR 1.04 (1.01–1.08) for light, RR 1.06 (1.01–1.11) for moderate and 1.09 (0.98–1.21) for heavy drinking; 43 studies). Alcohol was not significantly associated with the risk of adenocarcinoma of the oesophagus and gastric cardia (25 studies), cancer of the small intestine (5 studies), cervix (5 studies), endometrium (21 studies), ovary (20 studies), bladder (19 studies) and brain (6 studies). Hodgkin's lymphoma (RR 0.73 (95% CI 0.59–0.89) for light, RR 0.73 (0.60–0.87) for moderate and 0.63 (0.41–0.97) for heavy drinking; 9 studies) and non-Hodgkin's lymphoma (RR 0.88 (0.80–0.97) for light, RR 0.87 (0.81–0.95) for moderate and 0.75 (0.64–0.88) for heavy drinking; 24 studies) had statistically significant inverse associations with the consumption of alcohol. Finally, the risk of cancer of the kidney (RR 0.92 (95% CI 0.86–0.99) for light and RR 0.79 (0.72–0.86) for moderate; 17 studies) and thyroid (RR 0.81 (0.74–0.88) for light and RR 0.81 (0.71–0.94) for moderate; 9 studies) was significantly lower for light or moderate drinkers compared with nondrinkers or occasional drinkers.
Figure 2.
Pooled RR estimates by cancer site and alcohol intake. Squares indicate the RR estimates and whiskers their 95% confidence intervals. Abbreviations: AC=adenocarcinoma; CI= confidence interval; RR= relative risk; SCC=squamous cell carcinoma.
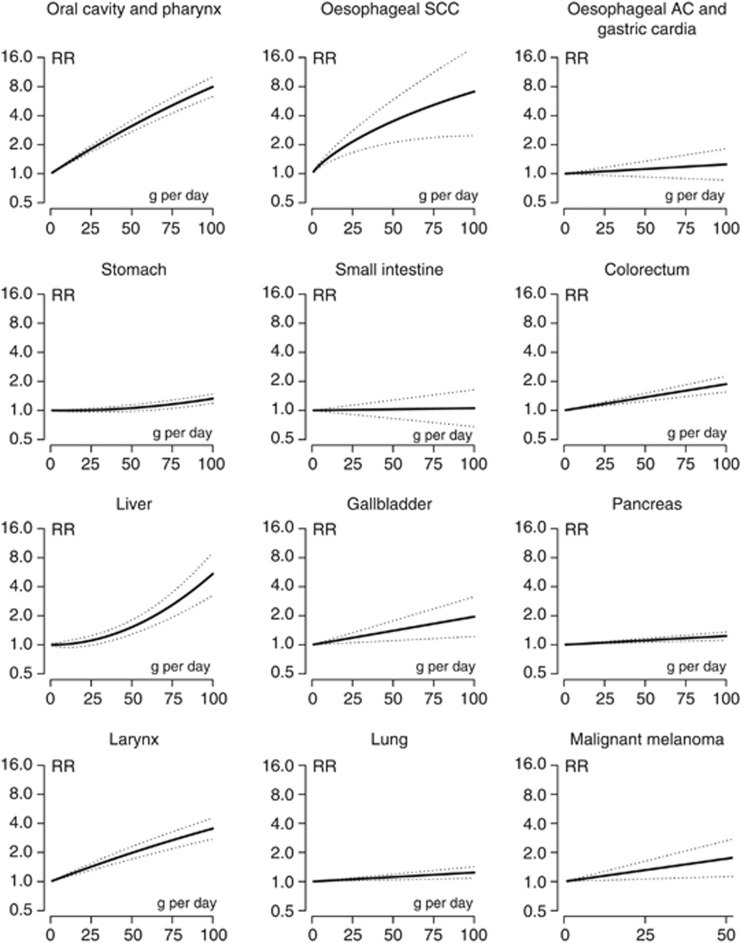
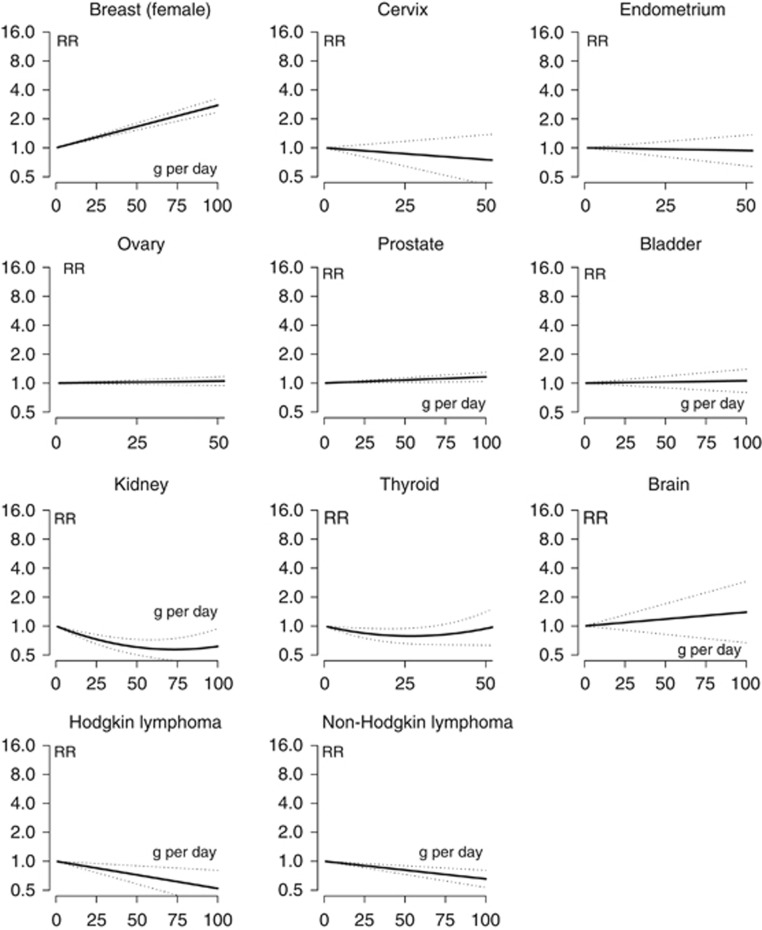
Figure 3 illustrates the association between site-specific cancer risk and doses of alcohol treated as a continuous variable. Results mirrored the above reported trends. The risk of cancer of oral cavity and pharynx and oesophageal SCC steeply increased with increasing dose of alcohol. Similar trends, but of lower magnitude, were observed for melanoma and cancer of the colorectum, gallbladder, larynx and breast. A slight but significant linear increase was observed for cancers of the pancreas, lung and prostate. An increased risk for stomach and liver cancer was observed with doses of ∼25 g per day (i.e., two drinks per day). No significant dose–response effect was observed for adenocarcinoma of the oesophagus and gastric cardia, and cancers of the small intestine, cervix, endometrium, ovary, bladder and brain. The risk of lymphomas linearly decreased as the dose of alcohol increased. Finally, lower doses were inversely associated with kidney and thyroid cancer risk.
Figure 3.
Relative risk functions and corresponding 95% confidence intervals describing the dose–response relationship between alcohol consumption and cancer risk obtained by fitting meta-regression models, by cancer site. Abbreviations: AC=adenocarcinoma; RR=relative risk; SCC=squamous cell carcinoma.
The results of heterogeneity analyses by study design, gender and geographic area are shown in Tables 2, 3, 4, respectively. Case–control studies reported a stronger association with alcohol on oral cavity and pharynx cancer as compared with cohort studies (heterogeneity P=0.007; Table 2). Similarly, the association was somewhat stronger in case–control than in cohort studies for cancers of the oesophagus (SCC), liver and larynx, although the corresponding heterogeneity tests were not significant. On the other hand, alcohol drinking was significantly associated with an increased risk of melanoma only in cohort studies (RRs of 1.25 for light and 1.27 for moderate drinking). The association between alcohol and colorectal cancer was stronger in men than in women (heterogeneity P=0.010; Table 3), and no significant detrimental effect of drinking on colorectal cancer risk was observed in women. The effect of light drinking on the risk of oral cavity and pharynx and oesophageal SCC was statistically significant only in studies carried out in Asian populations (RRs of 1.33 for oral cavity and pharynx and 1.54 for oesophageal SCC, Table 4). Furthermore, alcohol drinking was significantly associated with an increased risk of melanoma (RRs of 1.32 for light and 1.47 for moderate drinking) and prostate cancer (RRs of 1.05 for light, 1.09 for moderate and 1.20 for heavy drinking) only in studies conducted in North America. The effect of alcohol on non-Hodgkin's lymphoma differed according to geographic areas: evidence of a protective effect was found in studies conducted in Asian and North American countries, whereas no association was found in studies conducted in Europe (heterogeneity P=0.013). We found no significant evidence for an effect of the year of study publication on the association between alcohol and cancer (data not shown).
Table 2. Comparison of pooled relative risks in cohort and case–control studies.
| Cancer site | Alcohol intake | N | Cohort Pooled RR (95% CI) | I2 | N | Case–control Pooled RR (95% CI) | I2 | Pa |
|---|---|---|---|---|---|---|---|---|
| Oral cavity and pharynx | Light | 4 | 0.86 (0.60–1.23) | 68 | 22 | 1.22 (1.10–1.35) | 0 | 0.007 |
| Moderate | 5 | 1.25 (1.02–1.53) | 16 | 47 | 1.91 (1.69–2.16) | 70 | ||
| Heavy | 3 | 3.13 (1.59–6.19) | 69 | 35 | 5.34 (4.46–6.39) | 77 | ||
| Oesophageal SCC | Light | 10 | 1.20 (0.84–1.71) | 84 | 24 | 1.29 (1.07–1.55) | 49 | 0.157 |
| Moderate | 13 | 1.92 (1.44–2.58) | 83 | 40 | 2.34 (1.87–2.92) | 86 | ||
| Heavy | 9 | 3.56 (2.25–5.64) | 91 | 32 | 5.43 (4.04–7.32) | 91 | ||
| Oesophageal AC and gastric cardia | Light | 4 | 0.88 (0.74–1.03) | 6 | 17 | 0.88 (0.74–1.04) | 38 | 0.474 |
| Moderate | 4 | 0.82 (0.62–1.07) | 50 | 17 | 1.06 (0.78–1.43) | 75 | ||
| Heavy | 1 | 1.11 (0.48–2.56) | 0 | 17 | 1.16 (0.95–1.41) | 40 | ||
| Stomach | Light | 19 | 0.94 (0.87–1.03) | 55 | 16 | 1.08 (0.93–1.26) | 57 | 0.227 |
| Moderate | 19 | 0.96 (0.88–1.06) | 62 | 20 | 0.98 (0.89–1.08) | 11 | ||
| Heavy | 9 | 1.15 (1.03–1.28) | 0 | 11 | 1.22 (0.97–1.54) | 65 | ||
| Colorectum | Light | 33 | 1.01 (0.95–1.06) | 22 | 32 | 0.97 (0.89–1.06) | 53 | 0.129 |
| Moderate | 33 | 1.20 (1.12–1.29) | 45 | 33 | 1.14 (1.05–1.25) | 58 | ||
| Heavy | 14 | 1.41 (1.23–1.63) | 46 | 15 | 1.46 (1.15–1.86) | 78 | ||
| Liver | Light | 9 | 0.85 (0.74–0.97) | 32 | 12 | 1.31 (0.97–1.78) | 23 | 0.226 |
| Moderate | 9 | 1.00 (0.87–1.17) | 58 | 27 | 1.15 (0.97–1.35) | 40 | ||
| Heavy | 7 | 1.12 (1.02–1.23) | 0 | 24 | 2.79 (2.00–3.87) | 76 | ||
| Pancreas | Light | 18 | 0.95 (0.89–1.01) | 40 | 18 | 0.97 (0.84–1.13) | 42 | 0.363 |
| Moderate | 18 | 1.06 (0.99–1.13) | 28 | 21 | 0.97 (0.88–1.06) | 8 | ||
| Heavy | 9 | 1.18 (1.08–1.28) | 0 | 13 | 1.16 (0.98–1.37) | 17 | ||
| Larynx | Light | 3 | 0.81 (0.61–1.07) | 21 | 11 | 0.88 (0.61–1.27) | 45 | 0.216 |
| Moderate | 3 | 1.09 (0.70–1.72) | 46 | 34 | 1.48 (1.28–1.73) | 62 | ||
| Heavy | 3 | 1.12 (0.75–1.67) | 0 | 33 | 2.81 (2.33–3.39) | 76 | ||
| Lung | Light | 18 | 0.85 (0.82–0.89) | 26 | 11 | 0.71 (0.57–0.89) | 57 | 0.882 |
| Moderate | 18 | 0.97 (0.91–1.04) | 60 | 14 | 1.03 (0.87–1.21) | 51 | ||
| Heavy | 13 | 1.07 (0.93–1.25) | 75 | 7 | 1.33 (1.07–1.66) | 51 | ||
| Malignant melanoma | Light | 2 | 1.25 (1.13–1.38) | 0 | 12 | 1.06 (0.90–1.25) | 32 | 0.156 |
| Moderate | 2 | 1.27 (1.13–1.42) | 0 | 10 | 1.16 (0.92–1.45) | 47 | ||
| Heavy | – | n.e. | n.e. | – | n.e. | n.e. | ||
| Breast (female) | Light | 42 | 1.06 (1.03–1.10) | 41 | 73 | 1.04 (0.99–1.09) | 69 | 0.745 |
| Moderate | 37 | 1.22 (1.17–1.27) | 31 | 58 | 1.23 (1.16–1.32) | 62 | ||
| Heavy | 6 | 1.50 (1.19–1.89) | 0 | 5 | 1.78 (1.27–2.50) | 28 | ||
| Endometrium | Light | 8 | 0.97 (0.92–1.02) | 4 | 13 | 0.95 (0.87–1.03) | 14 | 0.631 |
| Moderate | 5 | 1.06 (0.89–1.26) | 67 | 8 | 0.87 (0.64–1.18) | 78 | ||
| Heavy | – | n.e. | n.e. | – | n.e. | n.e. | ||
| Ovary | Light | 4 | 1.02 (0.96–1.08) | 0 | 16 | 0.94 (0.87–1.01) | 17 | 0.007 |
| Moderate | 4 | 1.08 (0.99–1.19) | 20 | 13 | 0.99 (0.88–1.12) | 43 | ||
| Heavy | – | n.e. | n.e. | – | n.e. | n.e. | ||
| Prostate | Light | 19 | 1.04 (1.01–1.08) | 0 | 17 | 1.04 (0.97–1.11) | 0 | 0.773 |
| Moderate | 20 | 1.06 (0.99–1.13) | 24 | 21 | 1.06 (0.99–1.14) | 15 | ||
| Heavy | 8 | 1.04 (0.90–1.21) | 45 | 10 | 1.12 (0.95–1.33) | 37 | ||
| Bladder | Light | 3 | 1.10 (0.87–1.41) | 49 | 16 | 0.96 (0.85–1.09) | 37 | 0.342 |
| Moderate | 3 | 1.03 (0.76–1.40) | 56 | 16 | 1.01 (0.90–1.13) | 42 | ||
| Heavy | – | n.e. | n.e. | 10 | 0.95 (0.75–1.20) | 65 | ||
| Kidney | Light | 6 | 0.93 (0.85–1.02) | 37 | 11 | 0.92 (0.82–1.03) | 36 | 0.549 |
| Moderate | 6 | 0.74 (0.64–0.86) | 46 | 11 | 0.82 (0.72–0.94) | 32 | ||
| Heavy | 2 | 0.88 (0.16–4.92) | 81 | 3 | 0.81 (0.67–0.98) | 0 | ||
| Non-Hodgkin's lymphoma | Light | 9 | 1.02 (0.93–1.12) | 39 | 15 | 0.78 (0.69–0.88) | 46 | 0.360 |
| Moderate | 9 | 0.87 (0.77–0.97) | 36 | 15 | 0.88 (0.78–0.99) | 37 | ||
| Heavy | 3 | 0.74 (0.59–0.92) | 0 | 4 | 0.82 (0.60–1.13) | 50 |
Abbreviations: AC=adenocarcinoma; CI=confidence interval; n.e.= not evaluable; RR=relative risk; SCC=squamous cell carcinoma.
Only cancer sites for which more than 10 studies were available were considered.
Heterogeneity test.
Table 3. Comparison of pooled relative risks in men and women.
| Cancer site | Alcohol intake | N | Men Pooled RR (95% CI) | I2 | N | Women Pooled RR (95% CI) | I2 | Pa |
|---|---|---|---|---|---|---|---|---|
| Oral cavity and pharynx | Light | 12 | 1.20 (1.06–1.35) | 0 | 8 | 1.00 (0.78–1.27) | 51 | 0.165 |
| Moderate | 26 | 2.01 (1.69–2.40) | 73 | 9 | 1.67 (1.25–2.22) | 52 | ||
| Heavy | 21 | 5.33 (4.28–6.63) | 71 | 3 | 5.70 (3.75–8.66) | 0 | ||
| Oesophageal SCC | Light | 16 | 1.39 (1.11–1.74) | 61 | 8 | 1.14 (0.87–1.49) | 43 | 0.548 |
| Moderate | 28 | 2.25 (1.78–2.85) | 85 | 8 | 2.18 (1.42–3.35) | 72 | ||
| Heavy | 24 | 4.69 (3.49–6.31) | 88 | 3 | 8.32 (2.95–23.45) | 72 | ||
| Oesophageal AC and gastric cardia | Light | 3 | 0.94 (0.42–2.08) | 78 | 2 | 0.85 (0.63–1.14) | 0 | 0.858 |
| Moderate | 5 | 0.92 (0.46–1.86) | 76 | 2 | 0.62 (0.42–0.93) | 0 | ||
| Heavy | 6 | 1.17 (0.72–1.88) | 57 | 1 | 3.80 (0.89–16.32) | 0 | ||
| Stomach | Light | 14 | 1.00 (0.92–1.10) | 17 | 6 | 1.08 (0.76–1.54) | 73 | 0.817 |
| Moderate | 20 | 1.07 (1.00–1.14) | 2 | 5 | 0.90 (0.66–1.22) | 62 | ||
| Heavy | 12 | 1.20 (0.99–1.45) | 63 | 1 | 3.23 (0.80–13.07) | 0 | ||
| Colorectum | Light | 29 | 1.05 (0.95–1.16) | 44 | 23 | 0.95 (0.89–1.01) | 27 | 0.010 |
| Moderate | 36 | 1.21 (1.11–1.32) | 40 | 20 | 1.07 (0.99–1.16) | 32 | ||
| Heavy | 20 | 1.53 (1.30–1.80) | 70 | 4 | 1.24 (0.68–2.25) | 69 | ||
| Liver | Light | 10 | 1.05 (0.84–1.32) | 53 | 6 | 0.81 (0.59–1.12) | 26 | 0.953 |
| Moderate | 16 | 1.08 (0.88–1.32) | 57 | 8 | 1.24 (0.88–1.75) | 39 | ||
| Heavy | 11 | 1.59 (1.21–2.09) | 69 | 3 | 3.89 (1.60–9.48) | 10 | ||
| Pancreas | Light | 15 | 0.98 (0.86–1.11) | 46 | 13 | 0.93 (0.86–1.01) | 39 | 0.196 |
| Moderate | 20 | 1.08 (1.00–1.15) | 0 | 11 | 1.04 (0.93–1.17) | 51 | ||
| Heavy | 12 | 1.16 (1.06–1.27) | 0 | 4 | 1.17 (0.98–1.40) | 2 | ||
| Larynx | Light | 8 | 0.85 (0.61–1.19) | 51 | 3 | 0.89 (0.62–1.29) | 0 | 0.935 |
| Moderate | 21 | 1.50 (1.23–1.83) | 66 | 3 | 1.59 (1.06–2.38) | 0 | ||
| Heavy | 22 | 2.77 (2.15–3.57) | 83 | 1 | 1.55 (0.45–5.34) | 0 | ||
| Lung | Light | 17 | 0.86 (0.82–0.91) | 0 | 11 | 0.85 (0.77–0.93) | 59 | 0.828 |
| Moderate | 22 | 0.98 (0.89–1.08) | 60 | 11 | 1.01 (0.89–1.15) | 70 | ||
| Heavy | 14 | 1.14 (1.00–1.31) | 78 | 4 | 1.20 (0.75–1.92) | 65 | ||
| Malignant melanoma | Light | 3 | 1.19 (0.82–1.72) | 0 | 4 | 1.25 (1.13–1.38) | 0 | 0.844 |
| Moderate | 3 | 1.32 (0.90–1.92) | 0 | 3 | 1.27 (1.14–1.43) | 0 | ||
| Heavy | – | n.e. | n.e. | – | n.e. | n.e. | ||
| Bladder | Light | 9 | 1.13 (0.97–1.32) | 32 | 7 | 0.88 (0.70–1.12) | 52 | 0.055 |
| Moderate | 12 | 1.07 (0.95–1.22) | 23 | 6 | 0.93 (0.72–1.20) | 44 | ||
| Heavy | 5 | 1.24 (0.87–1.78) | 70 | 1 | 0.81 (0.38–1.73) | 0 | ||
| Kidney | Light | 10 | 0.99 (0.87–1.11) | 30 | 9 | 0.85 (0.78–0.92) | 0 | 0.133 |
| Moderate | 10 | 0.83 (0.71–0.97) | 46 | 6 | 0.65 (0.52–0.81) | 42 | ||
| Heavy | 3 | 0.88 (0.29–2.63) | 65 | – | n.e. | n.e. | ||
| Non-Hodgkin's lymphoma | Light | 7 | 0.96 (0.78–1.18) | 50 | 8 | 0.90 (0.78–1.04) | 62 | 0.065 |
| Moderate | 9 | 0.91 (0.76–1.08) | 47 | 5 | 0.86 (0.72–1.03) | 44 | ||
| Heavy | 2 | 0.87 (0.52–1.43) | 0 | – | n.e. | n.e. |
Abbreviations: AC=adenocarcinoma; CI=confidence interval; n.e.= not evaluable; RR=relative risk; SCC=squamous cell carcinoma.
Only cancer sites for which more than 10 studies were available were considered.
Heterogeneity test.
Table 4. Comparison of pooled relative risks between main population groups.
| Cancer site | Alcohol intake | N | European Pooled RR (95% CI) | I2 | N | North American Pooled RR (95% CI) | I2 | N | Asian Pooled RR (95% CI) | I2 | Pa |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Oral cavity and pharynx | Light | 5 | 0.95 (0.80–1.12) | 0 | 11 | 1.09 (0.92–1.29) | 38 | 7 | 1.33 (1.06–1.68) | 21 | 0.375 |
| Moderate | 16 | 1.51 (1.22–1.89) | 67 | 15 | 2.02 (1.74–2.34) | 46 | 12 | 2.18 (1.64–2.91) | 78 | ||
| Heavy | 14 | 5.41 (3.79–7.72) | 81 | 12 | 5.58 (4.35–7.15) | 71 | 4 | 3.02 (1.93–4.73) | 62 | ||
| Oesophageal SCC | Light | 7 | 1.05 (0.79–1.38) | 22 | 12 | 1.07 (0.84–1.37) | 32 | 11 | 1.54 (1.18–2.00) | 71 | 0.503 |
| Moderate | 10 | 1.91 (1.32–2.77) | 71 | 13 | 2.95 (2.38–3.67) | 37 | 23 | 2.20 (1.65–2.94) | 91 | ||
| Heavy | 8 | 4.76 (2.69–8.41) | 85 | 10 | 7.63 (5.34–10.91) | 59 | 18 | 4.24 (2.93–6.14) | 93 | ||
| Oesophageal AC and gastric cardia | Light | 7 | 0.79 (0.68–0.93) | 0 | 10 | 0.95 (0.78–1.16) | 41 | 2 | 1.18 (0.24–5.79) | 82 | 0.213 |
| Moderate | 5 | 0.90 (0.60–1.36) | 61 | 10 | 0.99 (0.78–1.25) | 56 | 4 | 0.97 (0.24–3.83) | 91 | ||
| Heavy | 4 | 1.52 (0.80–2.88) | 65 | 9 | 1.23 (0.93–1.63) | 38 | 3 | 0.89 (0.49–1.64) | 36 | ||
| Stomach | Light | 12 | 0.98 (0.84–1.15) | 66 | 6 | 0.95 (0.75–1.22) | 50 | 15 | 1.01 (0.94,1.08) | 25 | 0.738 |
| Moderate | 11 | 0.90 (0.79,1.04) | 46 | 7 | 0.90 (0.76,1.06) | 1 | 16 | 1.01 (0.91,1.12) | 59 | ||
| Heavy | 5 | 1.21 (1.04,1.42) | 0 | 3 | 1.42 (0.86,2.34) | 21 | 10 | 1.08 (0.93,1.26) | 35 | ||
| Colorectum | Light | 13 | 1.03 (0.97–1.10) | 21 | 27 | 0.96 (0.90–1.03) | 44 | 22 | 1.03 (0.91–1.18) | 38 | 0.215 |
| Moderate | 13 | 1.17 (1.07–1.29) | 57 | 27 | 1.14 (1.05–1.24) | 48 | 24 | 1.24 (1.08–1.42) | 56 | ||
| Heavy | 7 | 1.22 (0.98–1.52) | 61 | 9 | 1.29 (1.01–1.66) | 65 | 13 | 1.73 (1.39–2.16) | 67 | ||
| Liver | Light | 6 | 0.92 (0.58–1.46) | 31 | 3 | 1.24 (0.73–2.10) | 0 | 12 | 1.02 (0.83–1.26) | 58 | 0.118 |
| Moderate | 9 | 0.83 (0.70–0.97) | 0 | 8 | 1.23 (0.97–1.56) | 33 | 18 | 1.14 (0.97–1.33) | 59 | ||
| Heavy | 8 | 2.00 (1.07–3.74) | 85 | 7 | 3.40 (2.54–4.55) | 0 | 15 | 1.59 (1.27–2.00) | 69 | ||
| Pancreas | Light | 11 | 0.90 (0.85–0.96) | 0 | 16 | 0.99 (0.89–1.09) | 52 | 8 | 1.01 (0.71–1.45) | 45 | 0.074 |
| Moderate | 11 | 0.97 (0.90–1.04) | 0 | 16 | 1.03 (0.95–1.12) | 13 | 9 | 1.19 (0.97–1.46) | 30 | ||
| Heavy | 4 | 0.79 (0.50–1.24) | 0 | 9 | 1.17 (1.08–1.28) | 0 | 8 | 1.18 (0.96–1.44) | 0 | ||
| Larynx | Light | 4 | 0.83 (0.41–1.67) | 54 | 7 | 0.90 (0.67–1.21) | 37 | 4 | 0.72 (0.34–1.50) | 52 | 0.291 |
| Moderate | 16 | 1.36 (1.12–1.65) | 64 | 15 | 1.54 (1.20–1.98) | 57 | 4 | 1.57 (0.78–3.16) | 69 | ||
| Heavy | 18 | 2.71 (2.02–3.63) | 82 | 13 | 2.74 (2.15–3.48) | 60 | 3 | 1.63 (0.70–3.79) | 81 | ||
| Lung | Light | 4 | 0.80 (0.76–0.85) | 0 | 14 | 0.87 (0.80–0.94) | 44 | 9 | 0.81 (0.69–0.94) | 45 | 0.045 |
| Moderate | 4 | 0.88 (0.83–0.94) | 0 | 14 | 1.06 (0.98–1.15) | 45 | 12 | 0.93 (0.80–1.08) | 51 | ||
| Heavy | 4 | 0.96 (0.74–1.26) | 40 | 6 | 1.26 (1.10–1.45) | 53 | 6 | 0.92 (0.87–0.98) | 0 | ||
| Malignant melanoma | Light | 5 | 0.97 (0.74–1.28) | 76 | 6 | 1.32 (1.11–1.59) | 0 | – | n.e. | n.e. | 0.110 |
| Moderate | 5 | 1.01 (0.75–1.36) | 68 | 5 | 1.47 (1.14–1.88) | 0 | – | n.e. | n.e. | ||
| Heavy | – | n.e. | n.e. | – | n.e. | n.e. | – | n.e. | n.e. | ||
| Breast (female) | Light | 41 | 1.03 (0.98–1.10) | 67 | 55 | 1.06 (1.03–1.10) | 55 | 8 | 0.89 (0.72–1.11) | 75 | 0.557 |
| Moderate | 33 | 1.19 (1.10–1.28) | 60 | 46 | 1.25 (1.20–1.31) | 51 | 8 | 1.44 (1.21–1.71) | 20 | ||
| Heavy | 5 | 1.82 (1.14–2.89) | 43 | 4 | 1.67 (1.33–2.09) | 0 | 1 | 3.44 (0.47–25.14) | 0 | ||
| Endometrium | Light | 8 | 1.00 (0.93–1.07) | 10 | 11 | 0.93 (0.86–1.00) | 13 | 2 | 0.93 (0.68–1.26) | 0 | 0.589 |
| Moderate | 4 | 1.15 (0.84–1.57) | 86 | 7 | 0.97 (0.80–1.18) | 60 | 2 | 0.43 (0.25–0.74) | 0 | ||
| Heavy | – | n.e. | n.e. | – | n.e. | n.e. | – | n.e. | n.e. | ||
| Ovary | Light | 7 | 0.96 (0.89–1.05) | 23 | 11 | 1.00 (0.92–1.09) | 0 | – | n.e. | n.e. | 0.160 |
| Moderate | 5 | 1.02 (0.93–1.11) | 22 | 10 | 1.09 (0.95–1.24) | 27 | – | n.e. | n.e. | ||
| Heavy | – | n.e. | n.e. | – | n.e. | n.e. | – | n.e. | n.e. | ||
| Prostate | Light | 11 | 1.02 (0.94–1.11) | 0 | 21 | 1.05 (1.01–1.09) | 5 | 3 | 0.91 (0.70–1.19) | 0 | 0.214 |
| Moderate | 11 | 1.00 (0.90–1.11) | 18 | 22 | 1.09 (1.02–1.16) | 29 | 5 | 1.05 (0.85–1.31) | 0 | ||
| Heavy | 4 | 0.95 (0.75–1.21) | 36 | 7 | 1.20 (1.09–1.31) | 13 | 4 | 1.00 (0.58–1.72) | 50 | ||
| Bladder | Light | 8 | 1.09 (0.85–1.40) | 51 | 9 | 0.95 (0.84–1.09) | 41 | 2 | 1.00 (0.64–1.56) | 0 | 0.130 |
| Moderate | 8 | 1.07 (0.89–1.28) | 43 | 9 | 0.96 (0.84–1.09) | 40 | 2 | 1.49 (0.54–4.09) | 65 | ||
| Heavy | 4 | 1.23 (0.76–1.99) | 81 | 4 | 0.80 (0.56–1.14) | 68 | 2 | 0.89 (0.51–1.54) | 0 | ||
| Kidney | Light | 7 | 1.01 (0.86–1.17) | 32 | 6 | 0.89 (0.80–1.00) | 41 | 1 | 0.63 (0.35–1.13) | 0 | 0.510 |
| Moderate | 7 | 0.81 (0.69–0.94) | 34 | 6 | 0.80 (0.69–0.92) | 38 | 2 | 1.07 (0.18–6.41) | 84 | ||
| Heavy | 2 | 0.75 (0.60–0.93) | 0 | 1 | 0.98 (0.68–1.41) | 0 | 2 | 0.88 (0.16–4.92) | 81 | ||
| Non-Hodgkin's lymphoma | Light | 9 | 0.97 (0.83–1.12) | 35 | 10 | 0.87 (0.77–0.99) | 66 | 2 | 0.75 (0.41–1.36) | 88 | 0.013 |
| Moderate | 9 | 0.95 (0.82–1.12) | 53 | 9 | 0.84 (0.76–0.94) | 32 | 3 | 0.77 (0.61–0.98) | 0 | ||
| Heavy | 2 | 0.97 (0.71–1.34) | 0 | 1 | 0.77 (0.59–1.00) | 0 | 3 | 0.62 (0.50–0.78) | 0 |
Abbreviations: AC=adenocarcinoma; CI=confidence interval; n.e.= not evaluable; RR=relative risk; SCC=squamous cell carcinoma.
Only cancer sites for which more than 10 studies were available were considered.
Heterogeneity test.
The list of main confounders by cancer site is reported in Supplementary Material S2. In a first sensitivity analysis, we limited the analysis to studies reporting adjusted estimates only, and results did not materially change (Supplementary Material S3). In a second sensitivity analysis, we excluded the estimates from studies that included occasional drinkers in the reference category, and again results did not materially change (Supplementary Material S3). Notably, the association between alcohol and prostate cancer emerged more clearly in those sensitivity analyses than in the overall analysis. A list of all included studies by site is reported in Supplementary Material S4, and study-specific relative risk estimates for increasing level of alcohol consumption by cancer site are reported in Supplementary Material S5.
Discussion
The present work, based on the results published in 572 studies, represents the most up-to-date, exhaustive and comprehensive review on the association between alcohol and cancer. It updates and expands two previous meta-analyses by our group: the first based on 235 studies, published in 2001 (Bagnardi et al, 2001), and the second, which focussed on light alcohol drinking, published in 2013 (Bagnardi et al, 2013). We determined RR estimates and dose–response risk functions for the association between alcohol consumption and a large number of neoplasms, some of which were never investigated using a meta-analytic approach.
The mechanisms by which alcohol consumption exerts its carcinogenic effect are various and not fully understood. Acetaldehyde, the first metabolite of ethanol, is accountable for part of the carcinogenicity of alcohol drinking on the liver and the upper aerodigestive tract (Boffetta and Hashibe, 2006). Polymorphisms of the genes that encode enzymes for ethanol metabolism affect the ethanol/acetaldehyde oxidising capacity, and are responsible for the limited action of the enzyme that converts acetaldehyde to acetate that is not toxic to the body (Pöschl and Seitz, 2004; Seitz and Stickel, 2007; Yu et al, 2010). Along this line, we observed a significant increased risk of cancers of the upper aerodigestive tract associated with light alcohol drinking in Asian countries only, where 28–45% of the population has a variation of the gene ALDH2 (Goedde et al, 1992; Oze et al, 2011). Many other factors in addition to acetaldehyde might be related to carcinogenesis (Boyle et al, 2013) such as the alcohol-related increase of oestrogens and androgen levels in women that might promote the development of breast cancer (Singletary and Gapstur, 2001), or the alcohol-related immunodeficiency and immunosuppression that might facilitate carcinogenesis at various organs (Watson et al, 1994). In addition, ethanol-related folate malabsorption and deficiency are associated with different forms of cancer, of which colon cancer is the most commonly described (Hamid et al, 2009). Finally, alcohol may cause direct lesions to the epithelium of the upper digestive and respiratory tract, and favour the absorption of carcinogens (Doll et al, 1999).
There is accumulating evidence that alcohol might increase the risk of cancer of the pancreas and prostate. With regard to pancreatic cancer, heavy consumption of alcohol increased the risk by 19% compared with nondrinkers or occasional drinkers. This association was homogeneously reported across studies. Residual confounding by other risk factors, such as smoking, overweight and diabetes, is a major concern. However, when we limited the calculation of the pooled RR to fully adjusted estimates only, we still obtained a significant 20% increase in the risk of pancreatic cancer. Pancreatitis related to heavy alcohol consumption is a possible mechanism. As for prostate cancer, we found a moderate but statistically significant risk increase with increasing doses of alcohol consumption. This observation was mainly driven by studies conducted in North America that showed pooled RR estimates of 1.05, 1.09 and 1.20 for light, moderate and heavy drinking, respectively. Similarly, two recent studies published during the drafting of this review reported a significant positive association between alcohol consumption and prostate cancer (McGregor et al, 2013; Sawada et al, 2014).
Consumption of alcoholic beverages increases the risk of colorectal cancer. We found significant heterogeneity between men and women and, differently from our older findings (Fedirko et al, 2011), we found no significant effect of alcohol in women. In support of this, authors of a recent meta-analysis did not find any significant association between alcohol and colorectal cancer mortality in women (Cai et al, 2014). We found some evidence that alcohol is associated with an increased risk of melanoma. This evidence was principally apparent in cohort studies and in studies conducted in North America. The mechanisms for the harmful effect of alcohol drinking on skin cancer are not clear. However, in the presence of UV radiation, alcohol intake can substantially enhance cellular damage and subsequently lead to formation of skin cancers (Saladi et al, 2010). Another plausible hypothesis is that alcohol intake increases immunodeficiency and immunosuppression (Watson et al, 1994), the conditions that facilitate melanoma formation (Mukherji, 2013). Because of limited data, it was not possible to evaluate the effect of heavy drinking on the risk of melanoma.
Heavy drinkers had a significant 15% increase of lung cancer risk as compared with nondrinkers or occasional drinkers. As drinking and smoking are strongly associated, residual confounding by smoking might have biased this result. In a recent meta-analysis published by our group, alcohol consumption was not associated with lung cancer risk in never smokers (Bagnardi et al, 2011). A weaker still significant residual confounding by smoking might also partly explain the observed positive association between heavy drinking and stomach cancer. In addition, although the pooled RR from age-, sex- and smoking-adjusted estimates maintained a statistical significance, as heavy alcohol drinking is commonly associated with meager nutrition, residual confounding by poor diet (Klatsky, 2001) could not be ruled out.
The evidence for an association between alcohol and cancer of the endometrium and ovary is inconsistent, and the number of studies investigating the association of alcohol with cancer of the cervix, thyroid and brain is too small to draw any conclusion. Moreover, the studies on cancer of the bladder, adenocarcinoma of the oesophagus and gastric cardia indicate an absence of association. We found a positive significant association between high doses of alcohol consumption and risk of cancer of the gallbladder that was homogeneous across the studies. However, the paucity of data does not allow us to make any strong conclusion.
We consistently observed an inverse association of alcohol with both Hodgkin's and non-Hodgkin's lymphomas, as previously reported by our group (Tramacere et al, 2012c, 2012d). The mechanisms accounting for a possible alcohol-induced decrease in the risk of lymphomas remain largely unknown. The inverse relationship observed could be partially attributable to a misclassification of drinkers among cases, as early symptoms of lymphomas may cause subjects to either quit or reduce their drinking (Bryant and Newman, 2013; Brewin, 1966). A recent study from a European cohort consisting of 120 852 individuals did not show an inverse association between alcohol consumption and lymphoid neoplasms (Heinen et al, 2013).
Our meta-analysis supports the hypothesis of a protective effect of moderate alcohol consumption on the risk of renal cell cancer. Despite the lack of a clear biological explanation, alcohol could protect from renal cell cancer because of its effect on insulin sensitivity (Kiechl et al, 1996; Lee et al, 2007) or because of its diuretic effect, even though the association between total fluid intake and cancer risk remains still open to debate (Altieri et al, 2003).
In the present study, alcohol drinking was associated with cancer of the oral cavity and pharynx, oesophagus (SCC) and female breast even at low doses. These results represent an update and corroboration of previously published findings on the link between light alcohol drinking and cancer (Bagnardi et al, 2013). Given the high proportion of light drinkers in the population and the high incidence of these tumours, especially breast cancer (Ferlay et al, 2010), even small increases in cancer risk might be of great public health relevance. Approximately 5000 deaths from oral and pharyngeal cancer, 24 000 from oesophageal SCC and 5000 from breast cancer were attributable to light drinking in 2004 worldwide (Bagnardi et al, 2013).
Our study has several limitations typical of meta-analyses of observational studies (Stroup et al, 2000). The first one is that heterogeneity across studies was high for some types of cancer. Therefore, even if we used random-effects models to take heterogeneity into account and performed several heterogeneity analyses, some of the estimates should be interpreted with caution. A second limitation is that we could not investigate the role of different drinking patterns and different types of beverages in modifying the effect of the total amount of alcohol consumed (Bagnardi et al, 2008). Third, an underreporting of alcohol consumption in drinkers may partly or largely explain the association with light alcohol drinking. Another problem regarding misclassification is the possible inclusion of former drinkers in the nondrinkers category, as subjects with preclinical cancer symptoms might tend to stop drinking more frequently than healthy individuals (Brewin, 1966), thus diluting the risk of cancer among drinkers. Heterogeneity among studies with regard to the approaches used to measure alcohol consumption, modalities of interview and measures to ensure confidentiality, together with the lack of beverage-specific analyses, represent other limitations of our study. Some other issues (e.g., publication bias and the differentiation between hospital-based and population-based controls) were extensively treated by our group in a series of meta-analytic studies on the association between alcohol and single cancers (Islami et al, 2010, 2011; Tramacere et al, 2010, 2012a, 2012b, 2012c, 2012d; Turati et al, 2010a, 2010b; Bagnardi et al, 2011; Fedirko et al, 2011; Bellocco et al, 2012; Pelucchi et al, 2012; Seitz et al, 2012; Rota et al, 2012a, 2012b; Galeone et al, 2013).
In conclusion, consumption of alcoholic beverages increases the risk of cancer of the oral cavity and pharynx, oesophagus (SCC), colorectum, liver, larynx and female breast. Some other cancers, such as pancreas and prostate cancer and melanoma, appear to be associated with consumption of alcohol, but more studies are needed to draw any final conclusion. The link of alcohol with stomach and lung cancer and lymphomas could be biased by unaccounted confounders and misclassification of exposure and should be further investigated. There seems to be no association between consumption of alcohol and adenocarcinoma of the oesophagus and gastric cardia, and cancer of the endometrium, urinary bladder and kidney.
Acknowledgments
This work was supported by the Italian Association of Cancer Research (AIRC), Project No. 10258 (My First AIRC Grant), and by the Italian Foundation of Cancer Research (FIRC). FT was supported by a fellowship from FIRC. MR and CG were supported by Fondazione Umberto Veronesi.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Material
References
- Altieri A, La Vecchia C, Negri E. Fluid intake and risk of bladder and other cancers. Eur J Clin Nutr. 2003;57 (Suppl 2:S59–S68. doi: 10.1038/sj.ejcn.1601903. [DOI] [PubMed] [Google Scholar]
- Bagnardi V, Blangiardo M, La Vecchia C, Corrao G. A meta-analysis of alcohol drinking and cancer risk. Br J Cancer. 2001;85:1700–1705. doi: 10.1054/bjoc.2001.2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagnardi V, Rota M, Botteri E, Scotti L, Jenab M, Bellocco R, Tramacere I, Pelucchi C, Negri E, La Vecchia C, Corrao G, Boffetta P. Alcohol consumption and lung cancer risk in never smokers: a meta-analysis. Ann Oncol. 2011;22 (12:2631–2639. doi: 10.1093/annonc/mdr027. [DOI] [PubMed] [Google Scholar]
- Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, Turati F, Pasquali E, Pelucchi C, Bellocco R, Negri E, Corrao G, Rehm J, Boffetta P, La Vecchia C. Light alcohol drinking and cancer: a meta-analysis. Ann Oncol. 2013;24 (2:301–308. doi: 10.1093/annonc/mds337. [DOI] [PubMed] [Google Scholar]
- Bagnardi V, Zatonski W, Scotti L, La Vecchia C, Corrao G. Does drinking pattern modify the effect of alcohol on the risk of coronary heart disease? Evidence from a meta-analysis. J Epidemiol Community Health. 2008;62 (7:615–619. doi: 10.1136/jech.2007.065607. [DOI] [PubMed] [Google Scholar]
- Bellocco R, Pasquali E, Rota M, Bagnardi V, Tramacere I, Scotti L, Pelucchi C, Boffetta P, Corrao G, La Vecchia C. Alcohol drinking and risk of renal cell carcinoma: results of a meta-analysis. Ann Oncol. 2012;23 (9:2235–2244. doi: 10.1093/annonc/mds022. [DOI] [PubMed] [Google Scholar]
- Berlin JA, Longnecker MP, Greenland S. Meta-analysis of epidemiologic dose response data. Epidemiology. 1993;4 (3:218–228. doi: 10.1097/00001648-199305000-00005. [DOI] [PubMed] [Google Scholar]
- Boffetta P, Hashibe M. Alcohol and cancer. Lancet Oncol. 2006;7 (2:149–156. doi: 10.1016/S1470-2045(06)70577-0. [DOI] [PubMed] [Google Scholar]
- Boffetta P, Hashibe M, La Vecchia C, Zatonski W, Rehm J. The burden of cancer attributable to alcohol drinking. Int J Cancer. 2006;119 (4:884–887. doi: 10.1002/ijc.21903. [DOI] [PubMed] [Google Scholar]
- Boniol M, Autier P. Prevalence of main cancer lifestyle risk factors in Europe in 2000. Eur J Cancer. 2010;46 (14:2534–2544. doi: 10.1016/j.ejca.2010.07.049. [DOI] [PubMed] [Google Scholar]
- Boyle P, Boffetta P, Lowenfels A, Burns Harry, Brawley Otis, Zatonski Witold, Rehm Jürgen.(eds) (2013Alcohol: Science, Policy and Public Health Oxford University Press: Oxford [Google Scholar]
- Brewin TB. Alcohol intolerance in neoplastic disease. Br Med J. 1966;2:437–441. doi: 10.1136/bmj.2.5511.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant AJ, Newman JH. Alcohol intolerance associated with Hodgkin lymphoma. CMAJ. 2013;185 (8:E353. doi: 10.1503/cmaj.120974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai S, Li Y, Ding Y, Chen K, Jin M. Alcohol drinking and the risk of colorectal cancer death: a meta-analysis. Eur J Cancer Prev. 2014;23 (6:532–539. doi: 10.1097/CEJ.0000000000000076. [DOI] [PubMed] [Google Scholar]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Doll R, Forman D, La Vecchia C, Woutersen R.1999Alcoholic beverages and cancers of the digestive tract and larynx Health Issues Related to Alcohol Consumption2nd edn351–393.Blackwell: Oxford [Google Scholar]
- Fedirko V, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F, Negri E, Straif K, Romieu I, La Vecchia C, Boffetta P, Jenab M. Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Ann Oncol. 2011;22 (9:1958–1972. doi: 10.1093/annonc/mdq653. [DOI] [PubMed] [Google Scholar]
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- Ferrari P, Jenab M, Norat T, Moskal A, Slimani N, Olsen A, Tjønneland A, Overvad K, Jensen MK, Boutron-Ruault MC, Clavel-Chapelon F, Morois S, Rohrmann S, Linseisen J, Boeing H, Bergmann M, Kontopoulou D, Trichopoulou A, Kassapa C, Masala G, Krogh V, Vineis P, Panico S, Tumino R, van Gils CH, Peeters P, Bueno-de-Mesquita HB, Ocké MC, Skeie G, Lund E, Agudo A, Ardanaz E, López DC, Sanchez MJ, Quirós JR, Amiano P, Berglund G, Manjer J, Palmqvist R, Van Guelpen B, Allen N, Key T, Bingham S, Mazuir M, Boffetta P, Kaaks R, Riboli E. Lifetime and baseline alcohol intake and risk of colon and rectal cancers in the European prospective investigation into cancer and nutrition (EPIC) Int J Cancer. 2007;121 (9:2065–2072. doi: 10.1002/ijc.22966. [DOI] [PubMed] [Google Scholar]
- Galeone C, Malerba S, Rota M, Bagnardi V, Negri E, Scotti L, Bellocco R, Corrao G, Boffetta P, La Vecchia C, Pelucchi C. A meta-analysis of alcohol consumption and the risk of brain tumours. Ann Oncol. 2013;24 (2:514–523. doi: 10.1093/annonc/mds432. [DOI] [PubMed] [Google Scholar]
- Goedde HW, Agarwal DP, Fritze G, Meier-Tackmann D, Singh S, Beckmann G, Bhatia K, Chen LZ, Fang B, Lisker R, Paik YK, Rothhammer F, Saha N, Segal B, Srivastava LM, Czeizel A. Distribution of ADH2 and ALDH2 genotypes in different populations. Hum Genet. 1992;88:344–346. doi: 10.1007/BF00197271. [DOI] [PubMed] [Google Scholar]
- Greenland S.1987Quantitative methods in the review of epidemiologic literature Epidemiol Rev 91–30.1-30. [DOI] [PubMed] [Google Scholar]
- Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135:1301–1309. doi: 10.1093/oxfordjournals.aje.a116237. [DOI] [PubMed] [Google Scholar]
- Hamajima N, Hirose K, Tajima K, Rohan T, Calle EE, Heath CW, Jr, Coates RJ, Liff JM, Talamini R, Chantarakul N, Koetsawang S, Rachawat D, Morabia A, Schuman L, Stewart W, Szklo M, Bain C, Schofield F, Siskind V, Band P, Coldman AJ, Gallagher RP, Hislop TG, Yang P, Kolonel LM, Nomura AM, Hu J, Johnson KC, Mao Y, De Sanjosé S, Lee N, Marchbanks P, Ory HW, Peterson HB, Wilson HG, Wingo PA, Ebeling K, Kunde D, Nishan P, Hopper JL, Colditz G, Gajalanski V, Martin N, Pardthaisong T, Silpisornkosol S, Theetranont C, Boosiri B, Chutivongse S, Jimakorn P, Virutamasen P, Wongsrichanalai C, Ewertz M, Adami HO, Bergkvist L, Magnusson C, Persson I, Chang-Claude J, Paul C, Skegg DC, Spears GF, Boyle P, Evstifeeva T, Daling JR, Hutchinson WB, Malone K, Noonan EA, Stanford JL, Thomas DB, Weiss NS, White E, Andrieu N, Brêmond A, Clavel F, Gairard B, Lansac J, Piana L, Renaud R, Izquierdo A, Viladiu P, Cuevas HR, Ontiveros P, Palet A, Salazar SB, Aristizabel N, Cuadros A, Tryggvadottir L, Tulinius H, Bachelot A, Lê MG, Peto J, Franceschi S, Lubin F, Modan B, Ron E, Wax Y, Friedman GD, Hiatt RA, Levi F, Bishop T, Kosmelj K, Primic-Zakelj M, Ravnihar B, Stare J, Beeson WL, Fraser G, Bullbrook RD, Cuzick J, Duffy SW, Fentiman IS, Hayward JL, Wang DY, McMichael AJ, McPherson K, Hanson RL, Leske MC, Mahoney MC, Nasca PC, Varma AO, Weinstein AL, Moller TR, Olsson H, Ranstam J, Goldbohm RA, van den Brandt PA, Apelo RA, Baens J, de la Cruz JR, Javier B, Lacaya LB, Ngelangel CA, La Vecchia C, Negri E, Marubini E, Ferraroni M, Gerber M, Richardson S, Segala C, Gatei D, Kenya P, Kungu A, Mati JG, Brinton LA, Hoover R, Schairer C, Spirtas R, Lee HP, Rookus MA, van Leeuwen FE, Schoenberg JA, McCredie M, Gammon MD, Clarke EA, Jones L, Neil A, Vessey M, Yeates D, Appleby P, Banks E, Beral V, Bull D, Crossley B, Goodill A, Green J, Hermon C, Key T, Langston N, Lewis C, Reeves G, Collins R, Doll R, Peto R, Mabuchi K, Preston D, Hannaford P, Kay C, Rosero-Bixby L, Gao YT, Jin F, Yuan JM, Wei HY, Yun T, Zhiheng C, Berry G, Cooper Booth J, Jelihovsky T, MacLennan R, Shearman R, Wang QS, Baines CJ, Miller AB, Wall C, Lund E, Stalsberg H, Shu XO, Zheng W, Katsouyanni K, Trichopoulou A, Trichopoulos D, Dabancens A, Martinez L, Molina R, Salas O, Alexander FE, Anderson K, Folsom AR, Hulka BS, Bernstein L, Enger S, Haile RW, Paganini-Hill A, Pike MC, Ross RK, Ursin G, Yu MC, Longnecker MP, Newcomb P, Bergkvist L, Kalache A, Farley TM, Holck S, Meirik O, Collaborative Group on Hormonal Factors in Breast Cancer Alcohol, tobacco and breast cancer—collaborative reanalysis of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067 women without the disease. Br J Cancer. 2002;87 (11:1234–1245. doi: 10.1038/sj.bjc.6600596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamid A, Wani NA, Kaur J. New perspectives on folate transport in relation to alcoholism-induced folate malabsorption—association with epigenome stability and cancer development. FEBS J. 2009;276 (8:2175–2191. doi: 10.1111/j.1742-4658.2009.06959.x. [DOI] [PubMed] [Google Scholar]
- Hamling J, Lee P, Weitkunat R, Ambuhl M. Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med. 2008;27:954–970. doi: 10.1002/sim.3013. [DOI] [PubMed] [Google Scholar]
- Heinen MM, Verhage BA, Schouten LJ, Goldbohm RA, Schouten HC, van den Brandt PA. Alcohol consumption and risk of lymphoid and myeloid neoplasms: results of the Netherlands cohort study. Int J Cancer. 2013;133 (7:1701–1712. doi: 10.1002/ijc.28175. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- IARC Working Group . IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Alcohol Drinking. International Agency for Research on Cancer: Lyon; 1988. [PMC free article] [PubMed] [Google Scholar]
- IARC Working Group . IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: A Review of Human Carcinogens: Personal Habits and Indoor Combustions. International Agency for Research on Cancer: Lyon; 2010. [Google Scholar]
- Islami F, Fedirko V, Tramacere I, Bagnardi V, Jenab M, Scotti L, Rota M, Corrao G, Garavello W, Schüz J, Straif K, Negri E, Boffetta P, La Vecchia C. Alcohol drinking and esophageal squamous cell carcinoma with focus on light-drinkers and never-smokers: a systematic review and meta-analysis. Int J Cancer. 2011;129 (10:2473–2484. doi: 10.1002/ijc.25885. [DOI] [PubMed] [Google Scholar]
- Islami F, Tramacere I, Rota M, Bagnardi V, Fedirko V, Scotti L, Garavello W, Jenab M, Corrao G, Straif K, Negri E, Boffetta P, La Vecchia C. Alcohol drinking and laryngeal cancer: overall and dose-risk relation—a systematic review and meta-analysis. Oral Oncol. 2010;46 (11:802–810. doi: 10.1016/j.oraloncology.2010.07.015. [DOI] [PubMed] [Google Scholar]
- Kiechl S, Willeit J, Poewe W, Egger G, Oberhollenzer F, Muggeo M, Bonora E. Insulin sensitivity and regular alcohol consumption: large, prospective, cross sectional population study (Bruneck study) BMJ. 1996;313 (7064:1040–1044. doi: 10.1136/bmj.313.7064.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klatsky AL. Diet, alcohol, and health: a story of connections, confounders, and cofactors. Am J Clin Nutr. 2001;74:279–280. doi: 10.1093/ajcn/74.3.279. [DOI] [PubMed] [Google Scholar]
- La Vecchia C, Bosetti C, Bertuccio P, Castro C, Pelucchi C, Negri E. Trends in alcohol consumption in Europe and their impact on major alcohol-related cancers. Eur J Cancer Prev. 2014;23 (4:319–322. doi: 10.1097/CEJ.0b013e32836562f1. [DOI] [PubMed] [Google Scholar]
- Lamy L. Étude clinique et statistique de 134 cas de cancer de l'oesophage et du cardia. Arch Mal App Dig. 1910;4:451–475. [Google Scholar]
- Lee JE, Hunter DJ, Spiegelman D, Adami HO, Albanes D, Bernstein L, van den Brandt PA, Buring JE, Cho E, Folsom AR, Freudenheim JL, Giovannucci E, Graham S, Horn-Ross PL, Leitzmann MF, McCullough ML, Miller AB, Parker AS, Rodriguez C, Rohan TE, Schatzkin A, Schouten LJ, Virtanen M, Willett WC, Wolk A, Zhang SM, Smith-Warner SA. Alcohol intake and renal cell cancer in a pooled analysis of 12 prospective studies. J Natl Cancer Inst. 2007;99 (10:801–810. doi: 10.1093/jnci/djk181. [DOI] [PubMed] [Google Scholar]
- Liang H, Wang J, Xiao H, Wang D, Wei W, Qiao Y, Boffetta P. Estimation of cancer incidence and mortality attributable to alcohol drinking in China. BMC Public Health. 2010;10:730. doi: 10.1186/1471-2458-10-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez I. Factors associated with cancer of the esophagus, mouth, and pharynx in Puerto Rico. J Natl Cancer Inst. 1969;42:1069–1094. [PubMed] [Google Scholar]
- McGregor SE, Courneya KS, Kopciuk KA, Tosevski C, Friedenreich CM. Case-control study of lifetime alcohol intake and prostate cancer risk. Cancer Causes Control. 2013;24 (3:451–461. doi: 10.1007/s10552-012-0131-7. [DOI] [PubMed] [Google Scholar]
- Mukherji B. Immunology of melanoma. Clin Dermatol. 2013;31 (2:156–165. doi: 10.1016/j.clindermatol.2012.08.017. [DOI] [PubMed] [Google Scholar]
- Nelson DE, Jarman DW, Rehm J, Greenfield TK, Rey G, Kerr WC, Miller P, Shield KD, Ye Y, Naimi TS. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Public Health. 2013;103 (4:641–648. doi: 10.2105/AJPH.2012.301199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newsholme A. The possible association of the consumption of alcohol with excessive mortality from cancer. Br Med J. 1903;2 (2241:1529–1531. doi: 10.1136/bmj.2.2241.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen J, Sabreo S, Fasting U. Interaction of alcohol and tobacco as risk factors in cancer of the laryngeal region. J Epidemiol Community Health. 1985;39 (2:165–168. doi: 10.1136/jech.39.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oze I, Matsuo K, Wakai K, Nagata C, Mizoue T, Tanaka K, Tsuji I, Sasazuki S, Inoue M, Tsugane S, Research Group for the Development and Evaluation of Cancer Prevention Strategies in Japan Alcohol drinking and esophageal cancer risk: an evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn J Clin Oncol. 2011;41:677–692. doi: 10.1093/jjco/hyr026. [DOI] [PubMed] [Google Scholar]
- Pelucchi C, Galeone C, Tramacere I, Bagnardi V, Negri E, Islami F, Scotti L, Bellocco R, Corrao G, Boffetta P, La Vecchia C. Alcohol drinking and bladder cancer risk: a meta-analysis. Ann Oncol. 2012;23 (6:1586–1593. doi: 10.1093/annonc/mdr460. [DOI] [PubMed] [Google Scholar]
- Pöschl G, Seitz HK. Alcohol and cancer. Alcohol Alcohol. 2004;39 (3:155–165. doi: 10.1093/alcalc/agh057. [DOI] [PubMed] [Google Scholar]
- R Development Core Team 2008. R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna, Austria. http://www.R-project.org .
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373 (9682:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Rota M, Bellocco R, Scotti L, Tramacere I, Jenab M, Corrao G, La Vecchia C, Boffetta P, Bagnardi V. Random-effects meta-regression models for studying nonlinear dose-response relationship, with an application to alcohol and esophageal squamous cell carcinoma. Stat Med. 2010;29 (26:2679–2687. doi: 10.1002/sim.4041. [DOI] [PubMed] [Google Scholar]
- Rota M, Pasquali E, Scotti L, Pelucchi C, Tramacere I, Islami F, Negri E, Boffetta P, Bellocco R, Corrao G, La Vecchia C, Bagnardi V. Alcohol drinking and epithelial ovarian cancer risk. a systematic review and meta-analysis. Gynecol Oncol. 2012;125 (3:758–763. doi: 10.1016/j.ygyno.2012.03.031. [DOI] [PubMed] [Google Scholar]
- Rota M, Scotti L, Turati F, Tramacere I, Islami F, Bellocco R, Negri E, Corrao G, Boffetta P, La Vecchia C, Bagnardi V. Alcohol consumption and prostate cancer risk: a meta-analysis of the dose-risk relation. Eur J Cancer Prev. 2012;21 (4:350–359. doi: 10.1097/CEJ.0b013e32834dbc11. [DOI] [PubMed] [Google Scholar]
- Saladi RN, Nektalova T, Fox JL. Induction of skin carcinogenicity by alcohol and ultraviolet light. Clin Exp Dermatol. 2010;35 (1:7–11. doi: 10.1111/j.1365-2230.2009.03465.x. [DOI] [PubMed] [Google Scholar]
- Sawada N, Inoue M, Iwasaki M, Sasazuki S, Yamaji T, Shimazu T, Tsugane S. Alcohol and smoking and subsequent risk of prostate cancer in Japanese men: the Japan public health center-based prospective study (JPHC Study) Int J Cancer. 2014;134 (4:971–978. doi: 10.1002/ijc.28423. [DOI] [PubMed] [Google Scholar]
- Seitz HK, Pelucchi C, Bagnardi V, La Vecchia C. Epidemiology and pathophysiology of alcohol and breast cancer: update 2012. Alcohol Alcohol. 2012;47 (3:204–212. doi: 10.1093/alcalc/ags011. [DOI] [PubMed] [Google Scholar]
- Seitz HK, Stickel F. Molecular mechanisms of alcohol-mediated carcinogenesis. Nat Rev Cancer. 2007;7 (8:599–612. doi: 10.1038/nrc2191. [DOI] [PubMed] [Google Scholar]
- Singletary KW, Gapstur SM. Alcohol and breast cancer: review of epidemiologic and experimental evidence and potential mechanisms. JAMA. 2001;286 (17:2143–2151. doi: 10.1001/jama.286.17.2143. [DOI] [PubMed] [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283 (15:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Tramacere I, Scotti L, Jenab M, Bagnardi V, Bellocco R, Rota M, Corrao G, Bravi F, Boffetta P, La Vecchia C. Alcohol drinking and pancreatic cancer risk: a meta-analysis of the dose-risk relation. Int J Cancer. 2010;126 (6:1474–1486. doi: 10.1002/ijc.24936. [DOI] [PubMed] [Google Scholar]
- Tramacere I, Pelucchi C, Bagnardi V, Rota M, Scotti L, Islami F, Corrao G, Boffetta P, La Vecchia C, Negri E. A meta-analysis on alcohol drinking and esophageal and gastric cardia adenocarcinoma risk. Ann Oncol. 2012;23 (2:287–297. doi: 10.1093/annonc/mdr136. [DOI] [PubMed] [Google Scholar]
- Tramacere I, Negri E, Pelucchi C, Bagnardi V, Rota M, Scotti L, Islami F, Corrao G, La Vecchia C, Boffetta P. A meta-analysis on alcohol drinking and gastric cancer risk. Ann Oncol. 2012;23 (1:28–36. doi: 10.1093/annonc/mdr135. [DOI] [PubMed] [Google Scholar]
- Tramacere I, Pelucchi C, Bonifazi M, Bagnardi V, Rota M, Bellocco R, Scotti L, Islami F, Corrao G, Boffetta P, La Vecchia C, Negri E. A meta-analysis on alcohol drinking and the risk of Hodgkin lymphoma. Eur J Cancer Prev. 2012;21 (3:268–273. doi: 10.1097/CEJ.0b013e328350b11b. [DOI] [PubMed] [Google Scholar]
- Tramacere I, Pelucchi C, Bonifazi M, Bagnardi V, Rota M, Bellocco R, Scotti L, Islami F, Corrao G, Boffetta P, La Vecchia C, Negri E. Alcohol drinking and non-Hodgkin lymphoma risk: a systematic review and a meta-analysis. Ann Oncol. 2012;23 (11:2791–2798. doi: 10.1093/annonc/mds013. [DOI] [PubMed] [Google Scholar]
- Trichopoulos D, Day NE, Kaklamani E, Tzonou A, Muñoz N, Zavitsanos X, Koumantaki Y, Trichopoulou A. Hepatitis B virus, tobacco smoking and ethanol consumption in the etiology of hepatocellular carcinoma. Int J Cancer. 1987;39 (1:45–49. doi: 10.1002/ijc.2910390109. [DOI] [PubMed] [Google Scholar]
- Turati F, Gallus S, Tavani A, Tramacere I, Polesel J, Talamini R, Montella M, Scotti L, Franceshi S, La Vecchia C. Alcohol and endometrial cancer risk: a case-control study and a meta-analysis. Cancer Causes Control. 2010;21 (8:1285–1296. doi: 10.1007/s10552-010-9556-z. [DOI] [PubMed] [Google Scholar]
- Turati F, Garavello W, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F, Corrao G, Boffetta P, La Vecchia C, Negri E. A meta-analysis of alcohol drinking and oral and pharyngeal cancers. Part 2: results by subsites. Oral Oncol. 2010;46 (10:720–726. doi: 10.1016/j.oraloncology.2010.07.010. [DOI] [PubMed] [Google Scholar]
- Watson RR, Nixon P, Seitz HK, Maclennan R. Alcohol and cancer. Alcohol Alcohol Suppl. 1994;2:453–455. [PubMed] [Google Scholar]
- World Health Organization . Global Status Report on Alcohol and Health. World Health Organization: Geneva, Switzerland; 2011. [Google Scholar]
- Yu HS, Oyama T, Isse T, Kitagawa K, Pham TT, Tanaka M, Kawamoto T. Formation of acetaldehyde-derived DNA adducts due to alcohol exposure. Chem Biol Interact. 2010;188:367–375. doi: 10.1016/j.cbi.2010.08.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.