Abstract
Objective
The objective of this study was to assess the predictive value of lactate and base deficit in determining outcomes in trauma patients who are positive for ethanol.
Methods
Retrospective cohort study of patients admitted to a level 1 trauma center between 2005 and 2014. Adult patients who had a serum ethanol, lactate, base deficit, and negative urine drug screen obtained upon presentation were included.
Results
Data for 2482 patients were analyzed with 1127 having an elevated lactate and 1092 an elevated base deficit. In these subgroups, patients with a positive serum ethanol had significantly lower 72-hour mortality, overall mortality, and hospital length of stay compared with the negative ethanol group. Abnormal lactate (odds ratio [OR], 2.607; 95% confidence interval [CI], 1.629–4.173; P = .000) and base deficit (OR, 1.917; 95% CI, 1.183–3.105; P = .008) were determined to be the strongest predictors of mortality in the ethanol-negative patients. Injury Severity Score was found to be the lone predictor of mortality in patients positive for ethanol (OR, 1.104; 95% CI, 1.070–1.138; P=.000). Area under the curve and Youden index analyses supported a relationship between abnormal lactate, base deficit, and mortality in ethanol-positive patients when the serum lactate was greater than 4.45 mmol/L and base deficit was greater than −6.95 mmol/L.
Conclusions
Previously established relationships between elevated lactate, base deficit, and outcome do not remain consistent in patients presenting with positive serum ethanol concentrations. Ethanol skews the relationship between lactate, base deficit, and mortality thus resetting the threshold in which lactate and base deficit are associated with increased mortality.
1. Introduction
Lactate and base deficit have been widely used in clinical practice as surrogate markers of decreased tissue perfusion in the critically ill [1]. When tissues are poorly perfused, the resulting oxygen deficiency promotes a conversion to anaerobic metabolism and the formation of lactate. Accordingly, lactate is used as a clinical marker of oxygen use in critically ill patients. Clinical complications of hypoperfusion, anaerobic metabolism, and the resulting lactate production are numerous, including the development of a metabolic acidosis. In this setting, the body’smetabolic buffering system will become depleted of bicarbonate in an attempt to maintain normal serum pH. The deficiency in bicarbonate that develops is often referred to as a base deficit. Specifically, base deficit is defined as the amount of strong base that is required to titrate the pH of 1 L of blood to 7.40 and, therefore, correlates with the degree of acidosis in patients who are not maintaining normal perfusion requirements. Animal research suggested that alterations in lactate and base deficit correlated with the degree of tissue hypoperfusion and oxygen debt in the setting of hemorrhage [2]. This finding has led to additional research in humans evaluating the predictive value of lactate and base deficit as markers of morbidity and mortality in various patient populations including trauma [3,4].
Abnormal lactate and base deficit have been shown to be predictors of morbidity and mortality in the trauma population [1]. Paladino et al [3] found that the addition of lactate and base deficit to vital signs in trauma patients increased sensitivity for detecting major trauma by approximately 36% when compared with using vital signs alone. Additional data by Aslar et al [5] showed that lactate was a also predictor of mortality in patients experiencing traumatic injuries to the torso. The sensitivity and specificity of lactate in this study were 79.2% and 94.6%, respectively. Furthermore, this study revealed that lactates above 4 at the time of admission were statistically associated with higher mortality rates (P < .001). The addition of base deficit further enhanced the author’s ability to predict mortality in this patient population, likely because of its association with the severity and clearance rate of metabolic acidosis. Davis et al [6] provided additional evidence supporting the use of base deficit to identify trauma patients who would likely require early transfusion. Other markers of morbidity have also been linked to admission base deficits, such as hospital stay and the likelihood of a patient developing shock-related complications [1,6].
There are concomitant factors that can affect derivations of lactate and base deficit from normal values in trauma patients. One commonly encountered scenario occurs in patients who are found to have positive toxicology screenings upon admission. Substance use and abuse is frequently involved in the events leading up to a trauma and can often have significant implications in the subsequent medical management of traumatic injuries. Accordingly, inebriation due to ethanol will frequently confound the management of patients posttrauma because of its metabolic effects in promoting the production of lactate and a resulting base deficit. This process may in turn skew serum lactate values in trauma patients presenting to the emergency department (ED) and complicate their interpretation and clinical application. The typical indication of tissue malperfusion that is signaled by elevated lactate and base deficit may not be consistently represented in patients concomitantly presenting with ethanol intoxication. In addition, the use of these markers as predictors of morbidity and mortality may also be affected. As a result, these markers that are typically used in conjunction with other parameters to guide clinical management of critically ill trauma patients may result in unnecessary interventions and resuscitation strategies.
To date, literature investigating the application of lactate and base deficit in predicting morbidity and mortality in trauma patients with positive serum ethanol levels has been inconsistent in design and findings [7–10]. With this study, we will assess the predictive value of lactate and base deficit in determining morbidity and mortality from traumatic injuries sustained by patients after ethanol ingestion. Data provided by this study will be useful for all emergency department providers that treat trauma patients. Accurate identification of trauma patients at a high risk of morbidity and mortality using early predictive markers such as lactate and base deficit is useful in ensuring that appropriate and optimal clinical management is implemented. Understanding the effects of alcohol on these early predictive markers will aid providers in interpreting them in patients who have consumed alcohol before their trauma and presentation to the ED. The aim of this investigation is to evaluate the effect of ethanol on the use of lactate and base deficit as predictors of morbidity and mortality in trauma patients.
2. Materials and methods
2.1. Study design, setting, and population
This is a retrospective cohort study that was conducted in an 821-bed tertiary care center in West Virginia. The institution provides level 1 trauma services to southwestern West Virginia and areas of bordering states. Patients meeting inclusion criteria were separated into 2 comparator groups depending on whether they were positive for alcohol upon presentation to the ED. After approval of the investigational review board, patients admitted as priority 1 and 2 traumas between January 2005 and August 2014 were identified using the institution’s trauma registry. Priority designation was performed by emergency medical services based on the West Virginia’s Trauma and Emergency Medical System’s Field Trauma Triage Guidelines. Hemodynamic instability, mental status, respiratory effort, and type of injury were used for priority categorization [11]. Patients aged 18 years or older who had at least 1 serum lactate above 2.0 mmol/L or a base deficit of more than −2 mmol/L and a negative urine toxicology screen upon presentation to the ED were included in the final analyses. Patients were excluded if they did not have a negative urine drug screen, were transferred to another facility from the ED, or had no lactate or base deficit drawn upon presentation to the ED.
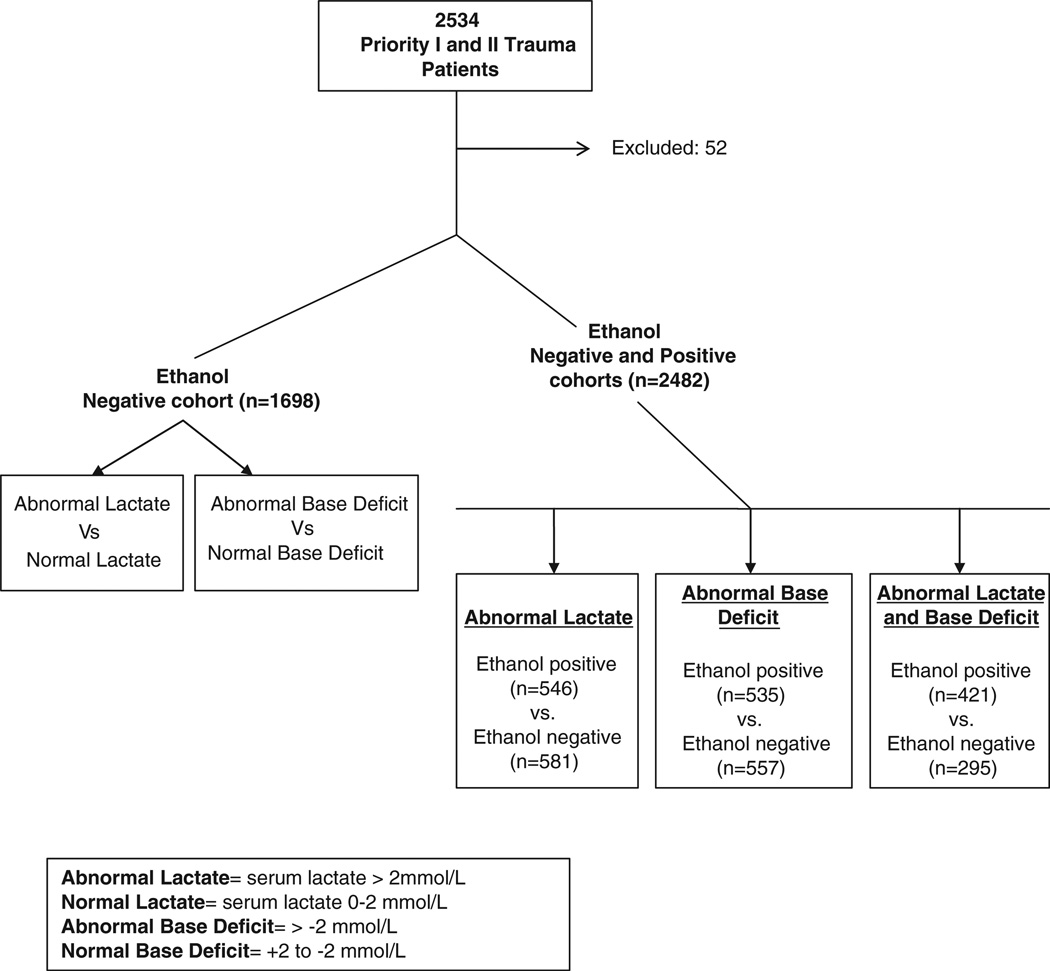
An initial analysis was performed on ethanol-negative patients to confirm that lactate and base deficit remained predictors of outcome in this study’s patient population. After this confirmatory analysis, additional analyses were executed comparing outcomes of ethanol-positive vs ethanol-negative patients to evaluate the effect of ethanol exposure on outcomes in patients with abnormal lactate and base deficit values (Figure).
Figure.
Study flow chart.
2.2. Data collection and measurements
After approval by the Charleston Area Medical Center/West Virginia University Charleston Investigational Review Board, this retrospective review was performed by using the trauma registry database and Soarian ® Enterprise Document Management (Siemens Medical Solutions USA, Inc., Malvern, Pennsylvania, United States) at the study institution. Variables collected included age, sex, initial lactate and base deficit values, vitals upon presentation to ED, Injury Severity Score (ISS), ED transfer to an operating room, intensive care unit (ICU) admission, administration of blood products, hospital and ICU length of stay (LOS), shock index, and status upon discharge. Data obtained from the trauma registry were verified by electronic data reports generated by the institution’s department of information services. All collected data were recorded in a Microsoft Excel (Microsoft, Redmond, Washington) spreadsheet for use with statistical analysis software. For the purpose of the analyses carried out in this study, an abnormal lactate was defined as a serum concentration of greater than 2.0 mmol/L. Abnormal base deficits were defined as values greater than −2 mmol/L and those falling between +2 to −2 mmol/L were considered normal. Patients with a base excess of greater than 2 mmol/L were not included in the outcomes analysis as values greater than 2 mmol/L have not been associated with increased mortality. Those with ICU or hospital stays less than 24 hours were excluded from respective LOS analyses; however, their data were included in the analysis of all other outcome measures.
2.3. Outcome variables
The aim of this study is to determine whether lactate and/or base deficit can be used to predict outcomes in priority 1 and priority 2 trauma patients with positive serum ethanol levels. Patients presenting with positive serum ethanol levels were compared with those without positive findings to determine the effect of ethanol exposure on the predictive value of lactate and base deficit. The primary end point studied was overall mortality. Additional outcomes studied were ICU and hospital LOS, ISS, need for transfusion, shock index, and 72-hour mortality.
2.4. Analysis
Descriptive analyses were performed. Continuous variables were presented as means and SDs and compared by using univariate t test. Categorical variables were reported as percentages and compared using χ2/Fisher exact test as necessary. Logistic regression was performed to determine predictors of hospital mortality with all statistically significant outcomes. Age and ISS were included as continuous variables. Base deficit, lactate, and comorbidities were included as dichotomous variables. Additional analyses were completed to determine cutoff points for continuous measurements of ethanol, lactate, and base deficit that discriminated between survivors and nonsurvivors in the ethanol-positive group. For this evaluation, area under receiver operating characteristic curve (AUC) was conducted, and simultaneously, Youden index (J) was calculated to determine the optimal cutoff points. The Youden index was calculated using the formula [J = sensitivity + specificity − 1]. The best cutoff threshold was asserted using the maximum Youden index. All comparisons were done at level of significance of ≤0.05. Analysis was performed using SPSS version 22.0 (IBM Corp, Armonk, NY).
3. Results
3.1. Characteristics of study subjects
Two thousand five hundred thirty-four priority 1 and 2 traumas met inclusion criteria. Of these patients, 52 were excluded because of missing laboratory data (no baseline lactate and/or base deficit) or an ED disposition of transfer to another facility. These exclusions left a final study population of 2482 patients whose data were included in the analyses. Of those patients, 1503 patients were identified as having an abnormal lactate and/or base deficit. The mean age of the study population was 44.91 years with 72% of the included patients being male. Emergency department disposition varied among patients, however, with approximately one half (n = 1165; 46.95%) being admitted to the ICU for further care. An additional 243 (9.79%) were taken to the operating room for emergent procedures. Of the remaining 1073 patients, 938 (37.80%) were transferred to floor and/or held for observation; 129 (5.19%) patients were sent home and/or left against medical advice; and 6 (0.24%) died. Seventy-two–hour mortality rate for the entire study population was 3.70% (n = 91). Overall hospital mortality was slightly higher with 145 (5.80%) mortalities occurring before hospital discharge.
3.2. Main results
The first study analysis evaluated outcomes in patients who were ethanol negative and had an elevated lactate (n = 581) vs those who did not (n= 1117). Patients in this study arm were found to have significantly higher shock index (0.74 vs 0.62, P = .000) and ISS (16.85 vs 11.75, P = .000) in the setting of an elevated lactate. Length of stay measures including ICU (6.38 vs 4.48 days, P = .000) and hospital (10.43 vs 6.28 days, P = .000) LOS were significantly higher in patients with elevated lactates. Additional measures evaluating requirements for blood products as well as derangements in base deficit measurements were all significantly higher in patients with an elevated lactate. Seventy-two–hour (9.81% vs 1.52%, P = .000) and hospital (13.08% vs 3.58%, P = .000) mortality rates were also significantly higher in the study subgroup with an elevated serum lactate (Table 1).
Table 1.
Comparison of outcomes with lactate in ethanol-negative patients
| Normal (n = 1117) | Abnormal (n = 581) | P | |
|---|---|---|---|
| Sex (male) | 736 (65.89%) | 397 (68.33%) | .311 |
| Age | 47.14 (18 to 97) | 47.79 (18 to 99) | .523 |
| ISS | 11.75 (1 to 59) | 16.85 (1 to 75) | .000* |
| Initial lactate | 1.31 (0.50 to 2.0) | 3.69 (2.1 to 20.0) | .000* |
| Mortality 72 hours | 17 (1.52%) | 57 (9.81%) | .000* |
| Hospital mortality | 40 (3.58%) | 76 (13.08%) | .000* |
| Base deficit | −0.59 (−15.0 to 26.0) | −3.21 (−27.0 to 16.0) | .000* |
| Initial pulse | 88.17 (22 to 162) | 97.54 (0 to 178) | .000* |
| Initial systolic BP | 145.90 (52 to 236) | 137.12 (0 to 259) | .000* |
| Shock index | 0.62 (0 to 1.47) | 0.74 (0 to 4.03) | .000* |
| ICU days | 4.48 (1 to 31) | 6.38 (1 to 65) | .000* |
| HLOS | 6.28 (1 to 43) | 10.43 (1 to 78) | .000* |
| Total blood products | 5.72 (1 to 106) | 10.52 (1 to 177) | .000* |
Abbreviations: BP, blood pressure; HLOS, hospital LOS.
Statistically significant at ≤0.05.
Similar analysis was conducted on the study population comparing outcomes in patients based on the presence of a base deficit. In the subgroup of patients who were negative for ethanol, the presence of an abnormal base deficit was shown to have a significant association with worsening morbidity. Shock index (0.75 vs 0.62, P = .000), ISS (18.23 vs 11.44, P = .000), ICU (6.68 vs 4.18 days, P .000) and hospital (10.85 vs 6.02 days, P = .000) LOS were all significantly higher for the subgroup with an abnormal base deficit. Mortality end points were also found to be significantly higher in the setting of abnormal base deficits. Seventy-two–hour mortality rates were 8.97% vs 2.13% (P = .000) and hospital mortality more than tripled in the setting of an abnormal base deficit (13.10% vs 3.65%, P = .000). Interestingly, an abnormal lactate, which was associated with an increased mortality rate in ethanol-negative patients, was also found to be significantly higher in the group of patients who had an abnormal base deficit (2.97 vs 1.72, P = .000). Moreover, blood transfusion requirements for patients with an abnormal base deficit were significantly higher (10.25 vs 5.55, P = .000) (Table 2).
Table 2.
Comparison of outcomes with base deficit in ethanol-negative patients
| Normal (n = 985) | Abnormal (n = 557) | P | |
|---|---|---|---|
| Sex (male) | 702 (71.26%) | 325 (58.34%) | .000* |
| Age | 47.01 (18 to 99) | 45.99 (18 to 95) | .321 |
| ISS | 11.44 (1 to 45) | 18.23 (1 to 75) | .000* |
| Initial lactate | 1.72 (0.50 to 9.6) | 2.97 (0.5 to 20.0) | .000* |
| Mortality 72 hours | 21 (2.13%) | 50 (8.97%) | .000* |
| Hospital mortality | 36 (3.65%) | 73 (13.10%) | .000* |
| Base deficit | −0.18 (−2.0 to 2.0) | −5.26 (−27.0 to −2.10) | .000* |
| Initial pulse | 88.68 (0 to 162) | 97.55 (0 to 178) | .000* |
| Initial systolic BP | 146.41 (61 to 236) | 134.45 (0 to 259) | .000* |
| Shock index | 0.62 (0 to 2.02) | 0.75 (0 to 4.03) | .000* |
| ICU days | 4.18 (1 to 33) | 6.68 (1 to 65) | .000* |
| HLOS | 6.02 (1 to 43) | 10.85 (1 to 78) | .000* |
| Total blood products | 5.55 (1 to 45) | 10.25 (1 to 177) | .000* |
Statistically significant at ≤0.05.
The next analysis compared outcomes in ethanol-negative and ethanol-positive patients who had an elevated lactate. In this subgroup, there were 581 patients who were negative for ethanol and 546 who were positive. Among the outcomes measured, ISS, base deficit, hospital LOS, 72-hour and overall mortality were statistically different between the 2 groups. Injury Severity Score was significantly higher for negative ethanol patients (16.85 vs 14.66, P = .001). On the other hand, base deficit in this subgroup was higher for patients who were ethanol positive (−5.03 vs −3.21 mmol/L, P = .000) while hospital LOS (10.43 vs 8.69 days, P = .014), 72-hour (9.81% vs 3.11%, P = .000), and hospital (13.08% vs 5.31%, P = .000), mortality were higher in the ethanol-negative patients. There was no significant difference in transfusion requirements between these 2 groups (10.52 vs 8.59, P=.211) (Table 3).
Table 3.
Comparison of outcomes between ethanol-negative and ethanol-positive patients with a lactate greater than 2 mmol/L
| Negative alcohol (n = 581) |
Positive alcohol (n = 546) |
P | |
|---|---|---|---|
| Sex (male) | 397 (68.33%) | 459 (84.06%) | .000* |
| Age | 47.79 (18 to 99) | 40.36 (18 to 83) | .000* |
| ISS | 16.85 (1 to 75) | 14.66 (1 to 59) | .001* |
| Initial lactate | 3.69 (2.1 to 20.0) | 3.61 (2.1 to 23.0) | .592 |
| Mortality 72 hours | 57 (9.81%) | 17 (3.11%) | .000* |
| Hospital mortality | 76 (13.08%) | 29 (5.31%) | .000* |
| Base deficit | −3.21 (−27.0 to 16.0) | −5.03 (−36.6 to 19.0) | .000* |
| Initial pulse | 97.54 (0 to 178) | 98.67 (0 to 182) | .385 |
| Initial systolic BP | 137.12 (0 to 259) | 137.14 (0 to 228) | .991 |
| Shock index | 0.74 (0 to 4.03) | 0.74 (0 to 1.95) | .950 |
| ICU days | 6.38 (1 to 65) | 5.76 (1 to 36) | .276 |
| HLOS | 10.43 (1 to 78) | 8.69 (1 to 72) | .014* |
| Total blood products | 10.52 (1 to 177) | 8.59 (1 to 73) | .211 |
Statistically significant at ≤0.05.
Patients with an abnormal base deficit were also compared based on whether they had positive serum ethanol concentrations upon presentation to the ED. In this subanalysis, there were 535 patients who were positive and 557 who were negative for ethanol. The ethanol-negative subgroup had higher 72-hour (8.97% vs 2.99%, P = .000) and hospital (13.10% vs 5.04%, P = .000) mortality rates. Furthermore, hospital LOS was significantly higher for the ethanol-negative subgroup (10.85 vs 8.57 days, P = .001) (Table 4).
Table 4.
Comparison of outcomes between ethanol-negative and ethanol-positive patients with a base deficit greater than −2 mmol/L
| Negative alcohol (n = 557) |
Positive alcohol (n = 535) |
P | |
|---|---|---|---|
| Sex (male) | 325 (58.34%) | 438 (81.86%) | .000* |
| Age | 45.99 (18 to 95) | 39.99 (18 to 83) | .000* |
| ISS | 18.23 (1 to 75) | 14.64 (1 to 59) | .000* |
| Initial lactate | 2.97 (0.5 to 20.0) | 3.38 (0.9 to 23.0) | .010* |
| Mortality 72 hours | 50 (8.97%) | 16 (2.99%) | .000* |
| Hospital mortality | 73 (13.10%) | 27 (5.04%) | .000* |
| Base deficit | −5.26 (−27.0 to −2.10) | −5.81 (−36.6 to −2.10) | .016* |
| Initial pulse | 97.55 (0 to 178) | 97.67 (0 to 182) | .930 |
| Initial systolic BP | 134.45 (0 to 259) | 136.92 (0 to 225) | .140 |
| Shock index | 0.75 (0 to 4.03) | 0.73 (0 to 1.95) | .150 |
| ICU days | 6.68 (1 to 65) | 5.79 (1 to 36) | .115 |
| HLOS | 10.85 (1 to 78) | 8.57 (1 to 72) | .001* |
| Total blood products | 10.25 (1 to 177) | 8.45 (1 to 73) | .206 |
Statistically significant at ≤ 0.05.
An additional analysis was performed with all patients who had an abnormal lactate and base deficit. These patients were again compared based on the status of the serum ethanol laboratory that was obtained upon presentation. There were 295 patients who were negative and 421 patients who were positive for ethanol that were included in this subanalysis. Morbidity markers of ISS (20.13 vs 15.90, P = .000), shock index (0.82 vs 0.75, P = .002), ICU (7.51 vs 6.02 days, P = .040) and hospital (12.76 vs 9.33 days, P = .000) LOS were again found to be significantly higher in the ethanol-negative group. Similarly, 72-hour (13.89% vs 3.80%, P = .000) and overall (18.98% vs 6.41%, P = .000) mortality were also found to be significantly higher for the ethanol-negative group (Table 5).
Table 5.
Comparison of outcomes between ethanol-negative and ethanol-positive patients with a lactate greater than 2 mmol/L and base deficit greater than −2 mmol/L
| Negative alcohol (n = 295) |
Positive alcohol (n = 421) |
P | |
|---|---|---|---|
| Sex (male) | 189 (64.06%) | 349 (82.89%) | .000* |
| Age | 47.18 (18 to 93) | 40.44 (18 to 83) | .000* |
| ISS | 20.13 (1 to 75) | 15.90 (1 to 59) | .000* |
| Initial lactate | 4.39 (2.1 to 20.0) | 3.84 (2.1 to 23.0) | .011* |
| Mortality 72 hours | 41 (13.89%) | 16 (3.80%) | .000* |
| Hospital mortality | 56 (18.98%) | 27 (6.41%) | .000* |
| Base deficit | −6.45 (−27.0 to −2.10) | −6.36 (−36.6 to −2.10) | .783 |
| Initial pulse | 102.95 (0 to 178) | 98.48 (0 to 182) | .012* |
| Initial systolic BP | 131.05 (0 to 259) | 136.11 (0 to 201) | .022* |
| Shock index | 0.82 (0 to 4.03) | 0.75 (0 to 1.95) | .002* |
| ICU days | 7.51 (1 to 65) | 6.02 (1 to 36) | .040* |
| HLOS | 12.76 (1 to 78) | 9.33 (1 to 72) | .000* |
| Total blood products | 11.60 (1 to 177) | 8.97 (1 to 73) | .146 |
Statistically significant at ≤ 0.05.
The presence of comorbidities was assessed in patients with abnormal lactate and base deficit values. Patients who were ethanol negative tended to more frequently have preexisting histories of diabetes (17.62% vs 9.02%, P = .001) and hypertension (36.61% vs 19.47%, P = .000). All other comorbidities such as chronic pulmonary disease, heart failure, and hepatic dysfunction were not different between these study groups (Table 6). Further analyses were performed to ensure that the relationship between worsening outcomes and an abnormal lactate and base deficit remained after patients with diabetes and hypertension were excluded. Markers of morbidity and mortality remained significantly higher in the ethanol-negative group when the patients with diabetes were excluded. Significant relationships also remained for morbidity and mortality outcomes when the same analysis was performed without patients who had a preexisting history of hypertension.
Table 6.
Comparison of comorbidities between ethanol-negative and ethanol-positive patients with a lactate greater than 2 mmol/L and base deficit greater than −2 mmol/L
| Negative alcohol (n = 295) |
Positive alcohol (n = 421) |
P | |
|---|---|---|---|
| Chemotherapy | 1 (0.33%) | 0 (0.00%) | .412 |
| Liver impairment | 2 (0.67%) | 2 (0.47%) | 1.000 |
| Cerebrovascular accident | 4 (1.35%) | 2 (0.47%) | .236 |
| Chronic pulmonary condition | 19 (6.44%) | 34 (8.07%) | .470 |
| Cancer metastasis | 1 (0.33%) | 0 (0.00%) | .412 |
| Congestive heart failure | 6 (2.03%) | 4 (0.95%) | .332 |
| Diabetes mellitus | 52 (17.62%) | 38 (9.02%) | .001* |
| Hypertension | 108 (36.61%) | 82 (19.47%) | .000* |
| Steroid use | 1 (0.33%) | 0 (0.00%) | .412 |
Statistically significant at ≤ 0.05.
A final data analysis was performed to compare findings of the current study to findings of a study published in 1997 by Davis et al [7]. In this last analysis, patients who presented with a base deficit of greater than or equal to −6 mmol/L were compared based on the status of their serum ethanol screening. Seventy-two–hour mortality, overall mortality, and ICU and hospital LOS were compared in 332 patients (150 ethanol negative and 182 ethanol positive). Both mortality end points had a significantly higher total number of mortalities in the ethanol negative group with hospital mortality being 17.37% (P = .000) and 72-hourmortality 14.97% (P = .000) higher in ethanol negative patients. Intensive care and hospital LOS end points were found to be higher in the ethanol-negative group; however, there were no statistically significant differences in these findings.
A regression analysis was performed on all significant findings to identify predictors of mortality in patients who were negative and positive for ethanol upon presentation to the ED. Age, ISS, abnormal lactate, and an abnormal base deficit were determined to be predictors of mortality in the group of patients who were negative for ethanol. Mortalities were 2.5 times more likely with an abnormal lactate (odds ratio [OR], 2.607; 95% confidence interval [CI], 1.629–4.173; P = .000) and 2 times more likely with an abnormal base deficit (OR, 1.917; 95% CI, 1.183–3.105; P = .008). Injury Severity Score was found to be the lone predictor of mortality in the group of patients who were positive for ethanol upon presentation (OR, 1.104; 95% CI, 1.070–1.138; P = .000).
After analyzing the data by positive and negative ethanol patients, further analysis was conducted comparing abnormal lactates and base deficits in patients who were legally intoxicated (ethanol >80 mg/dL) vs those who were negative for ethanol. The trend of higher mortality in the ethanol-negative group was again seen in this analysis with hospital mortality being 7.03% higher (P = .031) and 72-hourmortality 5.91% higher in ethanol-negative patients (P = .046).
Lastly, the relationship between alcohol, lactate, base deficit levels, and hospital mortality were analyzed using the AUC. There was no statistically significant correlation between alcohol level and hospital mortality. The relationship between lactate, base deficit, and hospital mortality, however, was good with lactate having an AUC of 0.866 (95% CI, 0.810–0.921; P = .000) and base deficit an AUC of 0.835 (95% CI, 0.750–0.919, P = .000). The optimal cutoff points for lactate and base deficit values were analyzed using the Youden index to determine the lactate and base deficit values that yielded the highest sensitivity and specificity for discriminating between survivors and nonsurvivors in the ethanol-positive group. A lactate of greater than 4.45 mmol/L showed the strongest correlation with 66% sensitivity and 91% specificity for mortality. The base deficit value that showed the strongest sensitivity and specificity (76% sensitivity and 88% specificity) for discriminating between survivors and nonsurvivors was greater than −6.95 mmol/L.
4. Discussion
Elevated lactate and base deficits have consistently been shown to be useful indicators of outcome in the trauma patient population. Studies have linked derangements in lactate and base deficit to a broad range of morbidities such as transfusion requirements, multiorgan failure, and the need for surgical intervention. Additional findings suggest that derivations from normal concentrations of these substances may also be a predictor of mortality [1,5,6,12,13]. The predictive application of these laboratory parameters, however, has been questioned in patients who present to medical facilities after traumatic events involving ethanol or other illicit substances [7–10].
Lactate is a byproduct of the body’s conversion from aerobic to anaerobic metabolism, which typically occurs in the setting of hypoperfusion and impaired oxygen delivery. Bicarbonate will precipitously decrease in relation to the extent of lactate production as the buffer is consumed in an attempt to maintain normal serum pH. As lactate production increases and the resulting metabolic acidosis worsens, a deficiency in the body’s basic stores (base deficit) will ensue. In the trauma patient population, lactate and base deficit have been shown to be effective markers of hypoperfusion and predictors of outcome [1,5,6,12,13]. Exposure to ethanol, however, is known to promote significant changes in serum lactate and base deficit without the presence of concomitant injuries or illnesses [14]. Ethanol metabolism involves the conversion of nicotinamide adenine dinucleotide (NAD+) to nicotinamide adenine dinucleotide reduced (NADH) and causes disruption of the NADH/NAD+ ratio. This ratio drives the conversion of pyruvate to lactate via lactate dehydrogenase causing an elevation in serum lactate, lactic acidosis, and the likely development of a base deficit [9,10,15]. Accordingly, the association between elevations in lactate and outcomes appears to become less meaningful and may not require as heightened a level of clinical urgency in patients with concomitant ethanol exposure [10,15]. Nevertheless, there have been a few publications suggesting that elevated lactate and the resulting base deficit remain predictive markers of morbidity and mortality in trauma patients with concomitant ethanol exposure [7–10]. The relationship and predictive value, however, have varied among the available literature.
Preexisting substance use is commonly encountered in the trauma patient population and is often implicated in patients’ traumatic events. Previous studies have suggested that illicit substances are implicated in 20% to 50% of all traumas presenting to trauma centers [9,10,16]. Similarly, 30% of patients tested positive for ethanol or an illicit substance upon presentation to our institution during the study period. Unfortunately, the presence of illicit substances can prove to significantly complicate patients’ management as some substances can obscure initial assessment of clinical status as well as facilitate the development of withdrawal syndromes later in patients’ stay. Ethanol and other illicit substances often precipitate or worsen acidotic states, which may serve to skew lactates and base deficits from their normal parameters. The presence of these substances in trauma patients has been shown to cause deviations in serum lactate and base deficit values that are not directly associated with patients’ injury severity or other markers of clinical status [17]. Given the importance of appropriate interpretation and clinical use of this laboratory data, it becomes increasingly vital that practitioners understand how these substances may affect the evaluation and use of these key pieces of laboratory data.
A study conducted by Davis et al [7] in more than 2000 trauma patients found that base deficit of greater or equal to −6 mmol/L was associated with higher transfusion requirements, ICU and hospital LOS regardless of the patients’ ethanol level [7]. These findings were confirmed by Zehtabchi et al [8] in a prospective, observational study of 520 trauma patients. Patients in this study were stratified based on injury severity and the presence of ethanol or other illicit substances. Patients stratified to the major injury group consistently had higher serum lactate and base deficit concentrations when compared with the minor injury group regardless of the presence of ethanol or illicit substances. The authors concluded that the presence of ethanol or illicit substances did not affect the predictive value of lactate and base deficit in their trauma patient population [8]. A third, much larger study was completed by Dunne et al [9] in which outcomes for 15 179 patients were prospectively evaluated. Patients who had positive screenings for ethanol or illicit substances were found to have significantly higher lactate, base deficit, and injury severity when compared with patients with negative screenings. Length of stay end points and mortality, however, did not differ significantly between the patients with positive and negative screens. Despite higher lactate and base deficit values in patients with positive screenings not correlating with an increase in morbidity and mortality, regression analysis did reveal that elevated lactates and base deficits were predictive of outcome regardless of the presence of ethanol or an illicit substance [9]. The final study completed before the currently presented data evaluated 1083 trauma patients who were positive for ethanol and negative for other toxicologies. In this study, Herbert et al [10] assessed the utility of lactate and base deficit in predicting trauma severity in patients who were positive for alcohol. Patients were stratified into mild, moderate, or severe injury categories based on ISS. Lactate was found to be elevated in more than 70% of patients across all groups regardless of injury severity. Base deficit, however, was more frequently elevated as patients’ ISS increased. The authors concluded that, in this setting, base deficit is a useful predictor of severity of illness and mortality; however, lactate may be an inadequate measure of injury severity in the trauma patient population [10].
Because of the inconsistencies in the design and findings of existing research on this topic, the current study sought to further investigate the relationship between ethanol exposure and the utility of lactate and base deficit as useful tools in the assessment and clinical management of trauma patients. The current study excluded patients who were positive for substances other than ethanol. This exclusion served to prevent potential confounding effects that could have been observed with initial lactate and based deficit values as well as any effect that may have been seen on patients’ outcomes. This is in contrast to previous study designs described above.
Initial analyses in the current study were conducted in ethanol-negative patients and targeted toward confirming the correlation of abnormal lactates and base deficits with outcome. Patients included in these analyses who had elevated lactates or base deficits were consistently found to have significantly higher ISS, shock index, transfusion requirements, ICU and hospital LOS as well as overall mortality. These findings support the concept of the physiologic changes induced by the anaerobic production of lactate, onset of metabolic acidosis, and the subsequent development of a base deficit being associated with injury severity, morbidity, and mortality. Regression analysis confirmed that an elevated lactate and base deficit were predictors of mortality in patients who were ethanol negative confirming data from previous studies [1,3,5,6,12,13,18,19]. Additional data comparisons, however, assessing the impact of ethanol exposure on abnormal lactate and base deficit confirmed that these laboratory markers may not be consistently reflective of severity of illness and outcomes. Logistic regression model documented that neither abnormal lactate nor base deficit were predictors of overall mortality in patients presenting with positive serum ethanol. These findings remained consistent when variations in the rate of baseline comorbidities between the study groups were accounted for in the statistical analysis. Findings were also unchanged when the analyses were limited to a comparison of patients who were intoxicated (serum ethanol level >80 mg/dL) vs those who were negative for ethanol.
A separate analysis was not able to confirm the LOS findings of the study conducted by Davis et al. As discussed above, the authors of this study concluded that, even in the presence of ethanol, a base deficit of greater than or equal to −6 mmol/L was associated with an increased LOS. The current study was not able to replicate this finding in the population of patients who presented with a base deficit of this magnitude. The findings were the exact opposite in that these patients had a lower duration of both hospital and ICU LOS when compared with the ethanol-negative portion of the study population.
Despite the current study’s initial analysis between lactate and base deficit in ethanol-positive patients not revealing a relationship with mortality, we endeavored to further evaluate this cohort to determine if there was a specific concentration of ethanol, lactate, or base deficit that was an effective discriminator of mortality. There was no relationship seen with respect to ethanol concentration and mortality. A serum lactate of greater than 4.45 mmol/L, however, did highly correlate with the likelihood of mortality in the ethanol-positive group. A similar relationship was found in ethanol-positive patients who had a base deficit greater than −6.95 mmol/L. These data support the concept that the presence of ethanol skews the relationship between lactate, base deficit, and mortality. As previously discussed, the alterations in predictive values are likely because of the change in NADH/NAD+ ratio leading to an increased production of lactate and resulting base deficit. Therefore, the threshold for which abnormal values represent altered perfusion and impaired oxygen delivery are further elevated than that seen in ethanol-negative patients.
The current study is the first to compare outcomes in patients with abnormal lactate and base deficits based on the positivity of serum ethanol assays performed upon presentation to a trauma center. Previous studies have differed in their design, which may have limited their ability to truly assess the impact of ethanol exposure on outcomes in the trauma patient population. Several former studies have reported data that were exclusively collected on patients who were positive for ethanol exposure upon presentation. Comparator arms within these studies compared patients based on level of intoxication or in other scenarios comparisons were based on severity of illness assessments [7,8,10]. The lone study previously referenced that performed comparisons between ethanol-negative and ethanol-positive patients also included patients with other toxicologic findings in their analysis [9]. Although logistic regression performed in this study confirmed the utility of lactate and base deficit in predicting outcomes in trauma patients with positive toxicology screens, it did not prove the utility of these markers in the setting of ethanol exposure alone [9].
In contrast, the current study sought to first confirm the predictive value of lactate and base deficit in trauma patients who were ethanol negative. Second, the study assessed the impact of ethanol exposure on the predictive value of lactate and base deficits. In these analyses, ethanol-negative patients who had abnormal lactate and base deficits were consistently found to have significantly higher morbidity and mortality. Base deficit and lactate were both determined to be predictors of mortality when the significant findings from the univariate evaluations were entered into a logistic regression analysis. The predictive value of lactate and base deficit did not remain significant when the same logistic regression analysis was performed on the ethanol-positive patients. Furthermore, an additional analysis of the ethanol-positive patients suggested that the presence of ethanol skews the relationship between abnormal lactates, base deficits, and mortality in these patients resulting in a higher threshold of elevation being associated with mortality.
Although this study reports important findings in relation to the reliability of lactate and base deficit in trauma patients with positive alcohol, the study is not without limitations. The retrospective design of the study lends itself to the introduction of several potential flaws including the potential for selection bias. In addition, the utility of evaluated data is dependent upon the accuracy in which events that occurred in the past were recorded. This serves to significantly limit researchers’ ability to practice quality control with the data. The current study did not evaluate patients based on the mechanism of injury (penetrating vs blunt) nor did it account for the amount of blood lost by patients before their presentation to the trauma center, which may have influenced the significance of deviations in their lactate or base deficits.
5. Conclusions
Based on this study’s findings, the previously established relationship between elevated lactate, base deficit, and outcome does not remain consistent in trauma patients who present with positive serum ethanol concentrations. In addition, we have determined that the presence of ethanol skews the relationship between these markers thus resetting the threshold in which elevations in lactate and base deficit are associated with increased mortality in this patient population. This data serve to further highlight the importance of using additional markers and parameters of clinical status when evaluating and managing trauma patients who present after ethanol exposure.
Footnotes
Dr Bethea is a research scientist for the West Virginia Clinical Translational Science Institute. Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under award number U54GM104942. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Mark L. Gustafson, Email: markgustafsondo@gmail.com.
Steve Hollosi, Email: stevehollosi@gmail.com.
Julton Tomanguillo Chumbe, Email: julton.tomanguillochumbe@camc.org.
Damayanti Samanta, Email: damayanti.samanta@camc.org.
Asmita Modak, Email: asmita.modak@camc.org.
Audis Bethea, Email: audis.bethea@camc.org.
References
- 1.Wilson M, Davis DP, Coimbra R. Diagnosis and monitoring of hemorrhagic shock during the initial resuscitation of multiple trauma patients: a review. J Emerg Med. 2003;24(4):413–422. doi: 10.1016/s0736-4679(03)00042-8. [DOI] [PubMed] [Google Scholar]
- 2.Davis JW. The relationship of base deficit to lactate in porcine hemorrhagic shock and resuscitation. J Trauma. 1994;36(2):168–172. doi: 10.1097/00005373-199402000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Paladino L, Sinert R, Wallace D, Anderson T, Yadav K, Zehtabchi S. The utility of base deficit and arterial lactate in differentiating major from minor injury in trauma patients with normal vital signs. Resuscitation. 2008;77(3):363–368. doi: 10.1016/j.resuscitation.2008.01.022. http://dx.doi.org/10.1016/j.resuscitation.2008.01.022 [Epub 2008 Mar 25]. [DOI] [PubMed] [Google Scholar]
- 4.Vandromme MJ, Griffin RL, Weinberg JA, Rue LW, III, Kerby JD. Lactate is a better predictor than systolic blood pressure for determining blood requirement and mortality: could prehospital measures improve trauma triage? J Am Coll Surg. 2010;210(5):861–867. doi: 10.1016/j.jamcollsurg.2010.01.012. http://dx.doi.org/10.1016/j.jamcollsurg.2010.01.012 [867-9]. [DOI] [PubMed] [Google Scholar]
- 5.Aslar AK, Kuzu MA, Elhan AH, Tanik A, Hengirmen S. Admission lactate level and the APACHE II score are the most useful predictors of prognosis following torso trauma. Injury. 2004;35(8):746–752. doi: 10.1016/j.injury.2003.09.030. [DOI] [PubMed] [Google Scholar]
- 6.Davis JW, Parks SN, Kaups KL, Gladen HE, O’Donnell-Nicol S. Admission base deficit predicts transfusion requirements and risk of complications. J Trauma. 1996;41(5):769–774. doi: 10.1097/00005373-199611000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Davis JW, Kaups KL, Parks SN. Effect of alcohol on the utility of base deficit in trauma. J Trauma. 1997;43(3):507–510. doi: 10.1097/00005373-199709000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Zehtabchi S, Baron BJ, Sinert R, Yadav K, Lucchesi M. Ethanol and illicit drugs do not affect the diagnostic utility of base deficit and lactate in differentiating minor from major injury in trauma patients. Acad Emerg Med. 2004;11(10):1014–1020. doi: 10.1197/j.aem.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 9.Dunne JR, Tracy JK, Scalea TM, Napolitano LM. Lactate and base deficit in trauma: does alcohol or drug use impair their predictive accuracy? J Trauma. 2005;58(5):959–966. doi: 10.1097/01.ta.0000158508.84009.49. [DOI] [PubMed] [Google Scholar]
- 10.Herbert HK, Dechert TA, Wolfe L, Aboutanos MB, Malhotra AK, Ivatury RR, et al. Lactate in trauma: a poor predictor of mortality in the setting of alcohol ingestion. Am Surg. 2011;77(12):1576–1579. [PubMed] [Google Scholar]
- 11.West Virginia Office of Emergency Medical Services Field Trauma Triage Guidelines. [Accessed on January 14, 2014]; Available at: http://www.wvoems.org/media/157590/9103%20field%20trauma%20triage%20protocol%2002262010.pdf. [Google Scholar]
- 12.Manikis P, Jankowski S, Zhang H, Kahn RJ, Vincent JL. Correlation of serial blood lactate levels to organ failure and mortality after trauma. Am J Emerg Med. 1995;13(6):619–622. doi: 10.1016/0735-6757(95)90043-8. [DOI] [PubMed] [Google Scholar]
- 13.Guyette F, Suffoletto B, Castillo JL, Quintero J, Callaway C, Puyana JC. Prehospital serum lactate as a predictor of outcomes in trauma patients: a retrospective observational study. J Trauma. 2011;70(4):782–786. doi: 10.1097/TA.0b013e318210f5c9. http://dx.doi.org/10.1097/TA.0b013e318210f5c9. [DOI] [PubMed] [Google Scholar]
- 14.Lamminpaa A, Vilska J. Acid-base balance in alcohol users seen in an emergency room. Vet Hum Toxicol. 1991;33(5):482–485. [PubMed] [Google Scholar]
- 15.Luft FC. Lactic acidosis update for critical care clinicians. J Am Soc Nephrol. 2001;12(Suppl. 17):S15–S19. [Review]. [PubMed] [Google Scholar]
- 16.O'Keeffe T, Shafi S, Sperry JL, Gentilello LM. The implications of alcohol intoxication and the Uniform Policy Provision Law on trauma centers; a national trauma data bank analysis of minimally injured patients. J Trauma. 2009;66(2):495–498. doi: 10.1097/TA.0b013e31818234bf. http://dx.doi.org/10.1097/TA.0b013e31818234bf. [DOI] [PubMed] [Google Scholar]
- 17.Dunham CM, Watson LA, Cooper C. Base deficit level indicating major injury is increased with ethanol. J Emerg Med. 2000;18(2):165–171. doi: 10.1016/s0736-4679(99)00188-2. [DOI] [PubMed] [Google Scholar]
- 18.Neville AL, Nemtsev D, Manasrah R, Bricker SD, Putnam BA. Mortality risk stratification in elderly trauma patients based on initial arterial lactate and base deficit levels. Am Surg. 2011;77(10):1337–1341. [PubMed] [Google Scholar]
- 19.Cerović O, Golubović V, Spec-Marn A, Kremzar B, Vidmar G. Relationship between injury severity and lactate levels in severely injured patients. Intensive Care Med. 2003;29(8):1300–1305. doi: 10.1007/s00134-003-1753-8. [DOI] [PubMed] [Google Scholar]