Abstract
Background:
Caesarean deliveries are on the increase in Greece and around the world. The objective of the present study was to assess the frequency of planned and emergency caesarean deliveries and their socio-demographic predictors in women with singleton pregnancies followed-up from early pregnancy to delivery.
Methods:
The mother-child cohort in Crete examines a population sample of pregnant women recruited during one year beginning in February 2007. A cohort of 1096 women, with singleton pregnancies, was included in the present analyses. Multivariable Poisson regression models with robust error variance were used.
Results:
Overall, 48% of the women had a caesarean delivery, with a higher percentage observed in women having their first child (52%). Maternal age was a predictor for caesarean deliveries; type of hospital was associated with the risk for an emergency caesarean, whereas women with lower education were at an increased risk of having a planned caesarean delivery among primiparae. Prior caesarean delivery was by far the strongest predictor (RR=7.68, 95% CI 5.71, 10.33) for a subsequent one among multiparae.
Conclusions:
Caesarean deliveries are almost as frequent as vaginal births in the study population and even more frequent in first-time mothers. The study findings support that risk factors are indeed mode of delivery and parity status specific. As such, it is becoming clearer which groups of women, especially first-time mothers, need to be targeted in future research and interventions so as to understand better and achieve an appropriate caesarean delivery risk.
Keywords: Caesarean delivery, emergency caesarean delivery, planned caesarean delivery, delivery mode
Introduction
The aim of a caesarean delivery is to avoid significant risks for the mother and the newborn if performed at the appropriate time1, and can be life-saving when medically indicated. The World Health Organization (WHO) has suggested a caesarean delivery (CD) rate ranging between 5% and 15%2-3. Later, in 2009, WHO and collaborating agencies indicated that although both very high and very low CD rates can be dangerous, the optimum CD rate is unknown awaiting further research, although the 5-15% range could continue to be used or different CD rate standards could be set by different institutions for their catchment’s areas4. Nowadays, in several countries, caesarean delivery is the most common major surgery performed and its increasing rate might also be contributed in part to the improvement in maternal outcomes giving the impression that it is mostly a procedure without much risk5.
It is well documented that there has been an increase in the CD rates in middle and high-income countries6 around the world, regardless of the efforts of several countries to curtail such increase6-7, adding to the economic burden of health services8. The reasons of such an increase and its range of consequences are not well understood9. Several reasons have been implicated for the increased use of CDs, including maternal characteristics (such as age, parity, education, race/ethnicity, amount of prenatal care), the place of birth such as country regions or types of hospital10, medical insurance11, previous caesarean delivery, maternal request, financial incentives or convenient scheduling11 and even technological advances improving safety on operations12.
In Greece, the estimated CD frequency, based either on retrospective medical records abstraction or a cross-sectional study design, has been increasing in the last 3 decades with the latest reported estimate in the Athens area being 41.6% in public hospitals and 53% in the private sector11.
The objective of the present study was to assess the frequency of both planned and emergency caesarean deliveries and their socio-demographic predictors in pregnant women with singleton pregnancies followed-up from early pregnancy to delivery.
Material and methods
The mother-child cohort in Crete (Rhea study)
The mother-child cohort study in Crete (Rhea study) is a prospective cohort examining a population sample of pregnant women recruited during one year starting in February 2007 at the prefecture of Heraklion, Crete, Greece13. Women were approached to participate in the study and also delivered their babies at the 4 major gynaecology and obstetrics departments located in the Heraklion prefecture, two in the public and two in the private sector. The first contact was made before 15 weeks’ gestation, at the time of the first major ultrasound examination. Women were then contacted multiple times during pregnancy and the postpartum period. The study was approved by the Ethical Committee of the University Hospital, Scientific Council, Heraklion, Crete, Greece, and all participants provided written, informed consent after complete description of the study. During the study recruitment period, 1765 eligible women were approached, 1610 (91%) agreed to participate and 1388 (86%) were followed up until delivery. A cohort of 1096 women with live singleton pregnancies and complete information on mode of delivery and birth outcomes were included in the present analyses.
Outcomes
The outcome of interest of the present study was mode of delivery categorized as planned caesarean delivery, emergency caesarean delivery or vaginal delivery. Information was collected through a questionnaire completed while the mother was still in the maternity wards minimizing misclassification bias on mode of delivery.
Potential Predictors
Potential predictors of caesarean deliveries considered in the analyses were demographic, socio-economic, health and pregnancy related events, which have an established or potential association with caesarean delivery, including: maternal age at delivery; maternal education (low level: ≤9 years of mandatory schooling, medium level: >9 years of schooling up to attending post-secondary school education (but not attending university or having a technical college degree), high level: attending university or having a university/technical college degree; marital status (married / engaged / alone); ethnic origin (Greek/non-Greek); parity (primipara - a woman having her first child / multipara - a woman having already other children before current pregnancy); residential area (urban / rural); type of delivery hospital (prefecture public hospital / tertiary teaching public hospital / private clinic); treatment to get pregnant (yes/no); previous caesarean delivery (yes/no); hospitalisation during pregnancy (yes/no); pre-pregnancy body mass index [weight (kg)/height (m)2]; preterm birth (<37 weeks of gestation) (yes/no); fetal weight growth restriction (FwGR) (yes/no).
A customized definition of impaired growth for the newborns of this study was developed taking into account their constitutional characteristics. The maternal and newborn characteristics considered a priori were as follows: gestational age (in weeks), maternal and paternal height (in centimetres), and age (in years); maternal pre-pregnancy weight (in kilograms), primiparous mother, and infant’s gender. More information on this customized definition of impaired growth can be found in Chatzi et al13. A neonate was classified with fetal weight growth restriction (FwGR) if his/her actual birth weight fell below the 10th percentile of the predicted birth weight distribution.
Statistical analysis
Descriptive statistics were used to summarize the baseline characteristics of participants. Bivariate associations between mode of delivery and categorical potential predictors were studied using Pearson’s Chi-square test or Fisher exact test (when less than five participants were expected in a cell). Bivariate associations between mode of delivery and continuous potential predictors were studied using either one-way analysis of variance (normally distributed continuous variables) or non parametric statistical methods (Kruskal-Wallis test) for non-normally distributed continuous variables. Multivariable Poisson regression models with robust error variance were fit to estimate the longitudinal associations [Relative Risk (RRs) and 95% Confidence Intervals (CI)] of the potential predictors with caesarean delivery. Separate analyses were conducted in primiparous and multiparous women. Maternal age, education, and ethnic origin, type of birth hospital, history of previous caesarean delivery (for multiparae), hospitalisation during pregnancy, history of treatment to get pregnant, FwGR and preterm birth were included in the final multivariable models. All but one of these variables (i.e. FwGR) were associated with the mode of delivery with p≤0.05 in the univariate analysis (Table 1). All hypothesis testing was conducted assuming a 0.05 significance level and a two-sided alternative hypothesis. All analyses were conducted using STATA software, version Intercooled 9.2 (StataCorp LP, College Station, TX, USA).
Table 1. Frequency distributions and/or means (SD) of women’s selected socio-demographic, health and pregnancy related characteristics, by mode of delivery - Rhea Birth Cohort, Crete.

*: Chi-squared or one-way analysis of variance or Kruskal-Wallis nonparametric test, T.T. Public Hospital: Tertiary Teaching Public Hospital, P. Public Hospital: Prefecture Public Hospital, ƒ: only among multiparous women, SD: Standard deviation, BMI: body mass index (Kg/m2), §: completed weeks.
Results
In this cohort of pregnant women, approximately half of them (48 %) had a caesarean delivery with a significantly higher CD incidence among primiparae (52%) compared with multiparae (44%) (p=0.006). Overall 63.5 % of all deliveries took place in public institutions. More than half (55%) of women giving birth in private clinics had a CD, whereas 47% of women giving birth in the general prefecture hospital and 40% of women giving birth in the tertiary teaching hospital had a CD (p<0.001), as well.
The highest frequency for vaginal deliveries was at the teaching hospital both in multiparae and primiparae, while for planned caesareans, the highest one was in the private clinics (among multiparae) and finally the highest emergency CD frequency was in the public prefecture hospital in both multiparae and primiparae. A 14.7% (161) of all deliveries happened during weekends, with the lowest percent of planned CDs in daily deliveries happening during the weekend (Figure 1).
Figure 1. Mode of delivery by day of the week, as percent of all deliveries.

As presented in Table 1, women with a planned CD were more likely to be of Greek origin, have a higher mean pre-pregnancy BMI, and give birth in a private clinic. Information regarding the history of prior caesarean delivery was available for 95% of multiparae (n=590), of whom 37.5% (n=221) had a prior CD. Only 8 women (3.6%) with a prior CD had a subsequent vaginal delivery and 91% of women with a planned CD had already a previous CD.
Among primiparae, for every year increase in age there was a 4% increase in the risk for having a caesarean delivery. Women giving birth in the teaching hospital were at an estimated 48% lower risk for having an emergency CD instead of a vaginal delivery (VD) compared with women giving birth in a private clinic, after adjusting simultaneously for other predictors (Table 2). In multiparous women, the history of prior CD was the strongest factor predicting a current CD with age also significantly associated with having a caesarean delivery after adjusting simultaneously for other predictors (Table 3). Multiparae giving birth in the prefecture public hospital were twice as likely to have an emergency caesarean delivery (vs. a VD) compared with women giving birth in private clinics (Table 3). It was estimated that hospitalisation during pregnancy doubled the risk for planned CD in primiparae and fetal weight growth restriction was associated with CD in primiparae, while preterm birth was associated with CD in multiparae (Tables 2 and 3).
Table 2. Associations of socio-demographic and mother’s health-related variables with Caesarean Delivery among primiparous women, Rhea Birth Cohort, Crete.

CD: caesarean delivery, n*: number of observations included in analysis, RR: Relative Risk, CI: Confidence Interval, †: Mutually adjusted estimates, results retained from Poisson regression with robust error variance, FwGR: fetal weight growth restriction.
Table 3. Associations of socio-demographic and mother’s health-related variables with Caesarean Delivery among multiparous women, Rhea Birth Cohort, Crete.
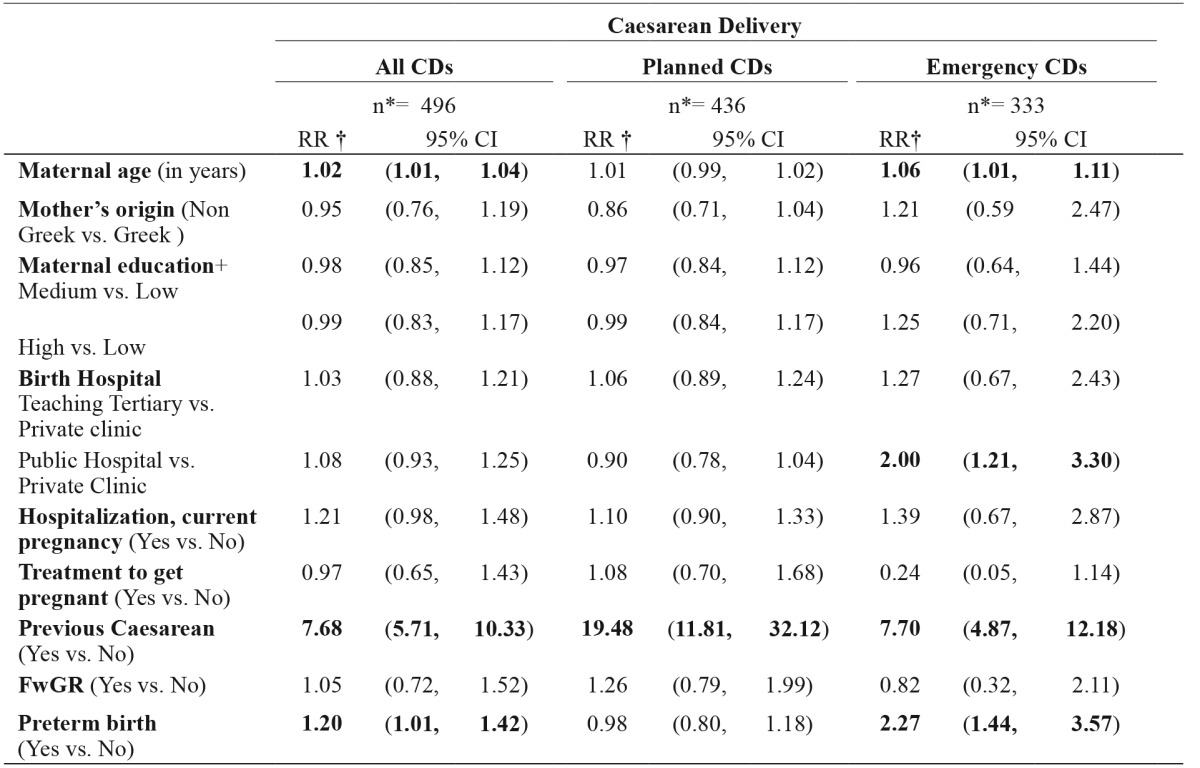
CD: caesarean delivery, n*: number of observations included in analysis, RR: Relative Risk, CI: Confidence Interval, †: Mutually adjusted estimates, results retained from Poisson regression with robust error variance, FwGR: fetal weight growth restriction.
Information on the reason for a planned CD was not available. However, we asked a non-random sample of 85 women who underwent planned CD regarding the reason(s) for this mode of delivery and the most common reason reported was previous caesarean delivery (47 of the 85 women). Only one woman reported that she wanted to have a planned CD and two women reported they were anxious about their health.
Discussion
This is the first mother-child cohort study in Greece with mothers recruited in early pregnancy (and not at delivery or postpartum), to report on the CD risk and the first to examine this risk in association with different potential predictors for both planned and emergency CDs in Greece. In the current population-based study, findings suggest that almost half women with a live singleton pregnancy underwent a caesarean delivery, and the major risk factors for CDs were not necessarily the same for planned or emergency deliveries among multiparae or primiparae, which finding is of major significance when reporting CDs or intervening to achieve a lower CD risk. Such overall high CD frequency is in agreement with previous estimates in Greece based on medical records or cross-sectional maternity ward studies, suggesting overall a rising trend over almost the last 3 decades11,14-18.
A significantly higher CD frequency was observed among women giving birth to their first child, suggesting a reproduction or even higher CD frequency in cohorts of first-time mothers. However, such CD frequency among primiparae is almost twice the one reported in 199315 and about the same as the one reported in 200511 in Greece. Unfortunately, the study suggests that the current CD rates are perpetuated and definitely do not seem to subside or show signs of reversing but rather are stabilized, to say the least, closely to 1 CD in every 2 primiparous women. Consequently, it is of utmost importance to understand separately the factors that increase the risk of having a caesarean delivery among first-time mothers and also among multiparous women, as it is investigated in the present study.
Maternal age was a common positive predictor for caesarean deliveries among both first-time mothers and multiparae with age specifically being a significant predictor for planned caesarean deliveries among primiparous women, and emergency CDs among multiparous women. These findings are in agreement with previous reports indicating that older age is associated with an increased risk for a CD19, although the reasons are not clarified, and stress the need for women to be aware of sequellae of their choices regarding the timing of childbearing.
Women having their first child, with a medium level education were less likely to have a caesarean section compared with women with less than 9 years of mandatory education. The same trend of association was suggested for women with a higher education level although such association did not reach statistical significance. Previous studies, however, have shown inconsistent results regarding the association of educational level with mode of delivery16,20-21.
Positive history of previous caesarean delivery was the strongest predictor for a caesarean (planned or emergency) delivery among multiparae. This is not surprising as one of the main worldwide indications for a CD is prior CD12,14. Due to the increasing CD rate over the last 3 decades, there is a significant percentage of women who have already a previous caesarean22 and account for a high percentage of the increase in the CD rate overall, underscoring the importance of preventing, when appropriate, the first (primary) caesarean delivery23-24.
Most of the 20th century, a woman having a caesarean section would imply that future deliveries would be caesarean deliveries, as well. After a discussion that started in the 1960s, the practice of having a vaginal birth after a caesarean delivery (VBAC) has increased up to the mid-1990s25 with a decline later due mainly to the fear of uterine rapture. A debate has been generated on the appropriate restrictions on VBAC with medical but also non-medical factors (e.g., fear of medical litigation) to have contributed to its decline. Since maternal morbidity increases as the number of CDs increases, family planning as far as intended future pregnancies is concerned should also be discussed when deciding about an elective repeat CD or a trial of labor. However, this decision might be a significant ethical dilemma for the mother and the health professional as what might be decided could result into a higher risk of adverse events for the infant or the mother. Good judgment is needed as the progress of any labour cannot be predicted, and this seems more useful than imposing specific CD rates26. We also need to have in mind that vaginal delivery has benefits for the mother and the infant27 and women should have the opportunity to be well informed about the benefits and consequences of a CD or a VD for their babies and themselves in the short and also long-term23 and be involved in the decision making regarding the mode of delivery28.
In the present study, the rates for CDs, emergency and planned, differ in different types of hospitals and the differences are not entirely between public vs. private status of clinics. This is in agreement with current literature where there are CD frequency variations not only between the public and private sector11, but also amongst hospitals of the same health system12 or different practices in the same hospital29 or different payer health insurance groups30. Different modes of delivery have different demands on staffing and other resources (i.e. staffing, use of operating theatre or not, length of labour, postnatal hospital stay, short or long-term effects, etc.) with estimated short term health services costs for a caesarean section of about 1.5-3.0 times the health services cost of an uncomplicated vaginal delivery, not considering long-term costs and costs outside health services8.
We stand in front of these rates with justified perplexity on what should be done to halt the reproduction of the present CD risk in future cohorts of mothers, especially first-time mothers. Having reached such a high risk for caesarean delivery among pregnant women in Greece - and several other counties - the scientific community and relevant stakeholders have initiated a discussion about the need to achieve appropriate CD rates23, contemplate and manage the complexity of practice changes31 needed with a realistic timetable to reach such rates.
Caesarean delivery can be without a doubt a life-saving operation for the mother and the infant, but if not medically indicated both are exposed needlessly to sequellae not fully understood9. Although severe complications due to caesarean sections are rare, we need to acknowledge the meaningful32 short term morbidity (e.g., infection, pulmonary embolism, neonatal respiratory problems)5 and long term morbidity (e.g., maternal, fetal, neonatal complications in subsequent pregnancies, like placenta accreta and uterine rupture)5 associated with them. The current discussion and debate regarding the increased CD rate during the last decades arises from the fact that similar increase is not true for the majority of the CD indications, which have become broader or even too broad21.
The question of what is an appropriate CD rate is still a topic of debate33, is hard to be defined as it varies according to several factors23 and the reply cannot be simple34. Detailed data on groups of women need to be available, outcomes need to be taken into consideration, as well as, local resources and expertise33-34. Our findings support the complex aetiology and synergy of multiple factors resulting in such increase in caesarean deliveries the last decades.
Such complexity deserves an equally multi-faceted approach to target a decrease in future caesarean deliveries24 including, but not limited to, quality improvement (so as to reduce development of CD indications), better measurement and public reporting, education of patients, families and providers, reform of hospital policies24, classification systems to track caesareans, audits while providing feedback and indentifying areas of possible interventions35. It has also been suggested that it would be more effective to undertake several approaches simultaneously taking into account both medical and cultural factors as appropriate in local contexts24.
Strength of the present study is its prospective cohort design, as this is a cohort with a detailed prospective follow-up of pregnant women since early pregnancy; as such minimizing also misclassification bias related to both predictor and mode of delivery information. To our knowledge no previous study had a cohort design so as to assess prospectively potential predictors for caesarean deliveries, both planned and emergency, from early pregnancy to delivery in Greece. Another major strength of the study is that it was able to differentiate planned and emergency caesarean deliveries, thus estimating the association of each type of CD with variable socio-demographic predictors in primiparae and multiparae. A limitation, however, of the study is the lack of information on the indication for CD. To remediate this, we included in the analysis maternal and infant health and pregnancy related variables so as to diminish as much as possible confounding by unmeasured clinical CD predictors.
Conclusion
Study findings suggest that caesarean deliveries are almost as frequent as vaginal births in the study population with higher CD frequency probably perpetuated to cohorts of first-time mothers compared with multiparae, having at the same time almost all women with prior CD undergoing repeat CDs. Such combination of factors deserves immediate attention in order to reverse such a trend. In addition, study findings support that risk factors are indeed mode of delivery and parity-status specific. As such, it is becoming clearer which women groups should be targeted in future research and interventions in order to understand better and achieve an appropriate caesarean delivery risk.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
We are grateful to all those who participated in the study especially the mothers and their infants, and the whole Rhea team for their contribution.
Funding
The Rhea project was financially supported by European projects (EU FP6-2003-Food-3-NewGeneris, EU FP6. STREP Hiwate, EU FP7 ENV.2007.1.2.2.2. Project No 211250 Escape, EU FP7-2008-ENV-1.2.1.4 Envirogenomarkers, EU FP7-HEALTH-2009- single stage CHICOS, EU FP7 ENV.2008.1.2.1.6. Proposal No 226285 ENRIECO, EU- FP7- HEALTH-2012 Proposal No 308333 HELIX), MeDALL (FP7 European Union project, No. 264357), and the Greek Ministry of Health (Program of Prevention of obesity and neurodevelopmental disorders in preschool children, in Heraklion district, Crete, Greece: 2011-2014; “Rhea Plus”: Primary Prevention Program of Environmental Risk Factors for Reproductive Health, and Child Health: 2012-15; Program of prevention and early diagnosis of cardiovascular disease risk factors in women in Crete: 2012-2015).
References
- 1.Lavender T, Hofmeyr GJ, Neilson JP, Kingdon C, Gyte GM. Caesarean section for non-medical reasons at term. Cochrane Database Syst Rev. 2006;CD004660 doi: 10.1002/14651858.CD004660.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Appropriate technology for birth. Lancet. 1985;2:436–437. [PubMed] [Google Scholar]
- 3.Chalmers B, Mangiaterra V, Porter R. WHO principles of perinatal care: the essential antenatal, perinatal, and postpartum care course. Birth. 2001;28:202–207. doi: 10.1046/j.1523-536x.2001.00202.x. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Indicators for EmOC. 2.5. Indicator 5: Caesarean sections as a proportion of all births. Monitoring emergency obstertric care: a handbook. World Health Organization. United Nations Population Fund. UNICEF. Mailman School of Public Health-Averting Maternal Death and Disability (Geneva), 2009: 25-30, available at: http://www.unfpa.org/sites/default/files/pub-pdf/obstetric_monitoring.pdf. last accessed: 12-1-2015.
- 5.Branch DW, Silver RM. Managing the primary cesarean delivery rate. Clin Obstet Gynecol. 2012;55:946–960. doi: 10.1097/GRF.0b013e318263c547. [DOI] [PubMed] [Google Scholar]
- 6.Althabe F, Sosa C, Belizán JM, Gibbons L, Jacquerioz F, Bergel E. Cesarean section rates and maternal and neonatal mortality in low-, medium-, and high-income countries: an ecological study. Birth. 2006;33:270–277. doi: 10.1111/j.1523-536X.2006.00118.x. [DOI] [PubMed] [Google Scholar]
- 7.What is the right number of caesarean sections? Lancet. 1997;349:815. doi: 10.1016/s0140-6736(97)21012-3. [DOI] [PubMed] [Google Scholar]
- 8.Henderson J, McCandlish R, Kumiega L, Petrou S. Systematic review of economic aspects of alternative modes of delivery. BJOG. 2001;108:149–157. doi: 10.1111/j.1471-0528.2001.00044.x. [DOI] [PubMed] [Google Scholar]
- 9.Belizán JM, Althabe F, Cafferata ML. Health consequences of the increasing caesarean section rates. Epidemiology. 2007;18:485–486. doi: 10.1097/EDE.0b013e318068646a. [DOI] [PubMed] [Google Scholar]
- 10.Hurst M, Summey PS. Childbirth and social class: the case of cesarean delivery. Soc Sci Med. 1984;18:621–631. doi: 10.1016/0277-9536(84)90290-9. [DOI] [PubMed] [Google Scholar]
- 11.Mossialos E, Allin S, Karras K, Davaki K. An investigation of Caesarean sections in three Greek hospitals: the impact of financial incentives and convenience. Eur J Public Health. 2005;15:288–295. doi: 10.1093/eurpub/cki002. [DOI] [PubMed] [Google Scholar]
- 12.Bragg F, Cromwell DA, Edozien LC, Gurol-Urganci I, Mahmood TA, Templeton A, et al. Variation in rates of caesarean section among English NHS trusts after accounting for maternal and clinical risk: cross sectional study. BMJ. 2010;341:c5065. doi: 10.1136/bmj.c5065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chatzi L, Plana E, Daraki V, Karakosta P, Alegkakis D, Tsatsanis C, et al. Metabolic syndrome in early pregnancy and risk of preterm birth. Am J Epidemiol. 2009;170:829–836. doi: 10.1093/aje/kwp211. [DOI] [PubMed] [Google Scholar]
- 14.Tampakoudis P, Assimakopoulos E, Grimbizis G, Zafrakas M, Tampakoudis G, Mantalenakis S, et al. Cesarean section rates and indications in Greece: data from a 24-year period in a teaching hospital. Clin Exp Obstet Gynecol. 2004;31:289–292. [PubMed] [Google Scholar]
- 15.Skalkidis Y, Petridou E, Papathoma E, Revinthi K, Tong D, Trichopoulos D. Are operative delivery procedures in Greece socially conditioned? Int J Qual Health Care. 1996;8:159–165. doi: 10.1093/intqhc/8.2.159. [DOI] [PubMed] [Google Scholar]
- 16.Papaioannou A, Patelarou E, Chatzi L, Koutis A, Kafatos A, Kogevinas M. Use of healthcare services and risk factors among pregnant women in Crete. Int J Gynaecol Obstet. 2008;103:253–255. doi: 10.1016/j.ijgo.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 17.Dinas K, Mavromatidis G, Dovas D, Giannoulis C, Tantanasis T, Loufopoulos A, et al. Current caesarean delivery rates and indications in a major public hospital in northern Greece. Aust N Z J Obstet Gynaecol. 2008;48:142–146. doi: 10.1111/j.1479-828X.2008.00839.x. [DOI] [PubMed] [Google Scholar]
- 18.Bakoula C, Matsaniotis N. Why choose caesarean section? Lancet. 2001;357:636. doi: 10.1016/S0140-6736(05)71427-6. [DOI] [PubMed] [Google Scholar]
- 19.Bayrampour H, Heaman M. Advanced maternal age and the risk of cesarean birth: a systematic review. Birth. 2010;37:219–226. doi: 10.1111/j.1523-536X.2010.00409.x. [DOI] [PubMed] [Google Scholar]
- 20.Gilbert A, Benjamin A, Abenhaim HA. Does education level influence the decision to undergo elective repeat caesarean section among women with a previous caesarean section? J Obstet Gynaecol Can. 2010;32:942–947. doi: 10.1016/s1701-2163(16)34681-3. [DOI] [PubMed] [Google Scholar]
- 21.Tollånes MC, Thompson JM, Daltveit AK, Irgens LM. Cesarean section and maternal education; secular trends in Norway, 1967-2004. Acta Obstet Gynecol Scand. 2007;86:840–848. doi: 10.1080/00016340701417422. [DOI] [PubMed] [Google Scholar]
- 22.Curtin SC, Kozak LJ, Gregory KD. U.S. cesarean and VBAC rates stalled in the mid-1990s. Birth. 2000;27:54–57. doi: 10.1046/j.1523-536x.2000.00054.x. [DOI] [PubMed] [Google Scholar]
- 23.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol. 2012;120:1181–1193. doi: 10.1097/aog.0b013e3182704880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Main EK, Morton CH, Melsop K, Hopkins D, Giuliani G, Gould JB. Creating a public agenda for maternity safety and quality in cesarean delivery. Obstet Gynecol. 2012;120:1194–1198. doi: 10.1097/aog.0b013e31826fc13d. [DOI] [PubMed] [Google Scholar]
- 25.National Institutes of Health Consensus Development Conference Panel National Institutes of Health Consensus Development conference statement: vaginal birth after cesarean: new insights March 8-10, 2010. Obstet Gynecol. 2010;115:1279–1295. doi: 10.1097/AOG.0b013e3181e459e5. [DOI] [PubMed] [Google Scholar]
- 26.Caesarean section on the rise. Lancet. 2000;356:1697. [PubMed] [Google Scholar]
- 27.Feldman P, Cymbalist R, Vedam S, Kotaska A. Roundtable discussion: «no one can condemn you to a C-section!». Birth. 2010;37:245–251. doi: 10.1111/j.1523-536X.2010.00412.x. [DOI] [PubMed] [Google Scholar]
- 28.Kolip P, Büchter R. Involvement of first-time mothers with different levels of education in the decision-making for their delivery by a planned Caesarean section. Women’s satisfaction with information given by gynaecologists and midwives. J Public Health. 2009;17:273–280. [Google Scholar]
- 29.Chauhan SP, Justice L, Sanderson M, Davis D, Watkins M, Morrison JC. Primary cesarean delivery among uncomplicated term nulliparous parturients: the influence of group practice within a community hospital. Am J Perinatol. 2008;25:119–123. doi: 10.1055/s-2008-1040345. [DOI] [PubMed] [Google Scholar]
- 30.Lipkind HS, Duzyj C, Rosenberg TJ, Funai EF, Chavkin W, Chiasson MA. Disparities in cesarean delivery rates and associated adverse neonatal outcomes in New York City hospitals. Obstet Gynecol. 2009;113:1239–1247. doi: 10.1097/AOG.0b013e3181a4c3e5. [DOI] [PubMed] [Google Scholar]
- 31.Lumbiganon P, Laopaiboon M, Gülmezoglu AM, Souza JP, Taneepanichskul S, Ruyan P, et al. World Health Organization Global Survey on Maternal and Perinatal Health Research Group. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet. 2010;375:490–499. doi: 10.1016/S0140-6736(09)61870-5. [DOI] [PubMed] [Google Scholar]
- 32.Silver RM. Implications of the first cesarean: perinatal and future reproductive health and subsequent cesareans, placentation issues, uterine rupture risk, morbidity, and mortality. Semin Perinatol. 2012;36:315–323. doi: 10.1053/j.semperi.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 33.Robson M, Hartigan L, Murphy M. Methods of achieving and maintaining an appropriate caesarean section rate. Best Pract Res Clin Obstet Gynaecol. 2013;27:297–308. doi: 10.1016/j.bpobgyn.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 34.Robson MS. Can we reduce the caesarean section rate? Best Pract Res Clin Obstet Gynaecol. 2001;15:179–194. doi: 10.1053/beog.2000.0156. [DOI] [PubMed] [Google Scholar]
- 35.Torloni MR, Betran AP, Souza JP, Widmer M, Allen T, Gulmezoglu M, et al. Classifications for cesarean section: a systematic review. PloS One. 2011;6:e14566. doi: 10.1371/journal.pone.0014566. [DOI] [PMC free article] [PubMed] [Google Scholar]


