Abstract
Background and aim:
In type 2 diabetes mellitus (T2DM), therapies to maintain blood glucose control usually fail after several years. The aim of this study was to estimate the time to insulin initiation, the glycemic burden that patients are exposed prior to conversion to insulin and their HbA1c level at that time and a year later.
Material and Methods:
Five hundred nine patients were included in this retrospective study. We identified patients with T2DM who started insulin therapy from 01/01/2002 to 30/06/2011, from the Scottish Care Information-Diabetes Collaboration (SCI-DC) database of Western General Hospital, Edinburgh, Scotland. We estimated the duration of diabetes prior to conversion to insulin therapy, the months they spent with glycated hemoglobin (HbA1c) above 7%, 8% or 9% until starting insulin, HbA1c and body weight (BW) at the time of conversion, at 6 and at 12 months before and after conversion.
Results:
Patients started insulin therapy after a median period of 6.2 (1-30) years after diagnosis of T2DM. Median HbA1c was 10% (range 7.2-17.9) at the time of conversion, 8.8% (5. 8-16.9) at six months before and 8.3% (5.2-15) at 12 months before conversion, and 8.4% (4.7-14.3) at 6 months and 8.2% (5-14.7) at 12 months after conversion. Body weight (BW) was 86.6 kg (39.6-179.8) at the time of conversion and 91 kg (42.7-196) at 12 months after conversion. Patients spent a median period of 49 (0-325) months with HbA1c >7%, 25 (0-163) months with HbA1c >8% and 10 (0-135) months with HbA1c >9%. Insulin treatment resulted in a decrease in HbA1c at 12 months of 1.8% (p<0.05) but in an increase in BW by 2.9 kg (p<0.05).
Conclusion:
Healthcare professionals delay the initiation of insulin in patients with type 2 diabetes until their HbA1c exceeds 10%. As a result, patients are exposed to a significant glycemic burden. Change in treatment improves their glycemic control for the next 12 months. Hippokratia 2014; 18 (4): 306-309.
Keywords: Diabetes mellitus type 2, insulin therapy, glycemic burden
Introduction
Diabetes mellitus is a chronic disease associated with macrovascular and microvascular complications1-3. Although it is well known that glycemic control plays a crucial role in preventing these complications4,5, less than half of the patients with diabetes achieve their glycemic target6. Moreover, oral antidiabetic drugs (OAD) fail to maintain glucose levels and sooner or later many patients require insulin therapy. An important issue is that healthcare professionals or patients often delay starting insulin and patients are therefore exposed to significant hyperglycemia for a long period of time.
In this study we aimed to evaluate how long it takes from diagnosis, for our patients with type 2 diabetes mellitus (T2DM) to start insulin therapy, how many months they spend with uncontrolled diabetes, meaning months with glycated hemoglobin (HbA1c) above 7%, 8% or 9%, and at what HbA1c level, insulin therapy is commenced when other treatments fail to maintain glycemic control.
Subjects and methods
In this retrospective study, we analysed medical records of patients with T2DM who were converted to insulin therapy from 01/01/2002 to 30/06/2011 at the Metabolic Unit of Western General Hospital, Edinburgh, Scotland. We used the Scottish Care Information-Diabetes Collaboration (SCI-DC) of Western General Hospital to define a cohort of patients with diabetes who were on any insulin therapy over this period. SCI-DC database covers the majority of the Scottish population with diagnosed T2DM, as almost all adult patients are registered on the SCI-DC database since 2000. SCI-DC database contains also retrospective data, uploaded from other electronic healthcare records at the time of the initial entry of a patient onto the database, so we had information regarding our patients before their first visit to the clinic. Data from all patients receiving an insulin prescription during this period and HbA1c, Body Weight (BW) and Body Mass Index (BMI) were extracted from this database. To retrieve the files we used key-words involving all the names of insulin used.
Patients who started insulin in less than 12 months from diagnosis were excluded to avoid undiagnosed type 1 diabetes, as well as patients who were converted to insulin during pregnancy or planning pregnancy, during acute illness other than uncontrolled diabetes or hospitalization. Finally, files with insufficient data, as those having less than 3 visits in our clinic or no information regarding HBA1c and BW before and after conversion, were omitted. Time of conversion was considered the last visit of a patient to our clinic before starting insulin. We retrieved data from that visit regarding HbA1c and BW. For the 6 months information we used any data between 3-9 months before or after conversion and when there were more visits or results, we used those which were closest to the 6 month point. For the 12 months the data was collected between 9-15 months and nearest to the date of the 12 month.
We estimated the time of uncontrolled diabetes by counting the months that a patient had HbA1c above 7%, 8% or 9%. Our patients usually had a repeat HbA1c every 6 months, or sooner if they are not well controlled, so we counted the months from an elevated HbA1c until the next measurement to be bellow 7% or 8% or 9%. If a patient was lost to follow up for 2 years or more, we excluded this period of time. We finally calculated the time from diagnosis until their conversion to insulin therapy and the time from their initial entry in the SCI-DC database, considering it as their first visit to a health professional [General Practitioner (GP) or Diabetologist (DT)].
Statistical analysis
All data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 13 (SPSS Inc., Chicago, IL, USA). Normality of distribution was assessed by Kolmogorov-Smirnov test. Continuous data are presented as median and range and categorical data as absolute numbers and percentages. Comparisons were performed by paired t test and Wilcoxon Signed rank test for normal and non-normal distributions respectively. In all cases, a 2-tailed p value less than 0.05 was considered statistically significant.
Results
From 11,029 patients with type 2 diabetes, 1,364 had an insulin prescription. From these, 529 had started insulin before 2002, 99 were on insulin from their first visit or started insulin in less than 12 months from diagnosis, 22 were converted during pregnancy or planning pregnancy, 5 proved to have type 1 diabetes, 32 were converted during hospitalization for acute illness and 10 proved not to be on insulin. Finally from 1,221 files with sufficient data, 509 fulfilled the inclusion criteria.
Median age of the patients at the time of conversion was 63 (range 27-91) years. Two hundred fifty were women and 54 were deceased. The median time until a patient started insulin therapy after failure of other treatments was 73 (12-360) months after diabetes diagnosis and 65 (4-360) months from their first visit at GP or DT. HbA1c at time of conversion was 10% (7.2-17.9) and they spent 49 (0-325) months with HbA1c >7%, 25 (0-163) months with HbA1c >8% and 10 (0-135) months with HbA1c >9% which were 90%, 45% and 17% of their time under consultation respectively. HbA1c was 8.3% (5.2-15) at 12 months before conversion and decreased to 8.2% (5-14.7) at 12 months after conversion. There was a 2.9 kg [(-18.4)-(+11.7), p<0.05] increase in BW at 12 months after the initiation of insulin.
There was no difference in HbA1c level at the time of initiation of insulin between older and younger patients, but patients younger than 55 years were more overweight, 93.9 kg (43-166.6), were converted to insulin earlier (47 vs. 65 months) from their first consultation, and spent more time with uncontrolled diabetes (HbA1c >9%: 25.6 % of time vs. 11.9 % in patients older than 65 years) (Table 1).
Table 1. Demographic and clinical data of the 509 patients from the Scottish Care Information-Diabetes Collaboration (SCIDC) database, divided in three age groups (>65 years, ≤65 years, ≤55 years).
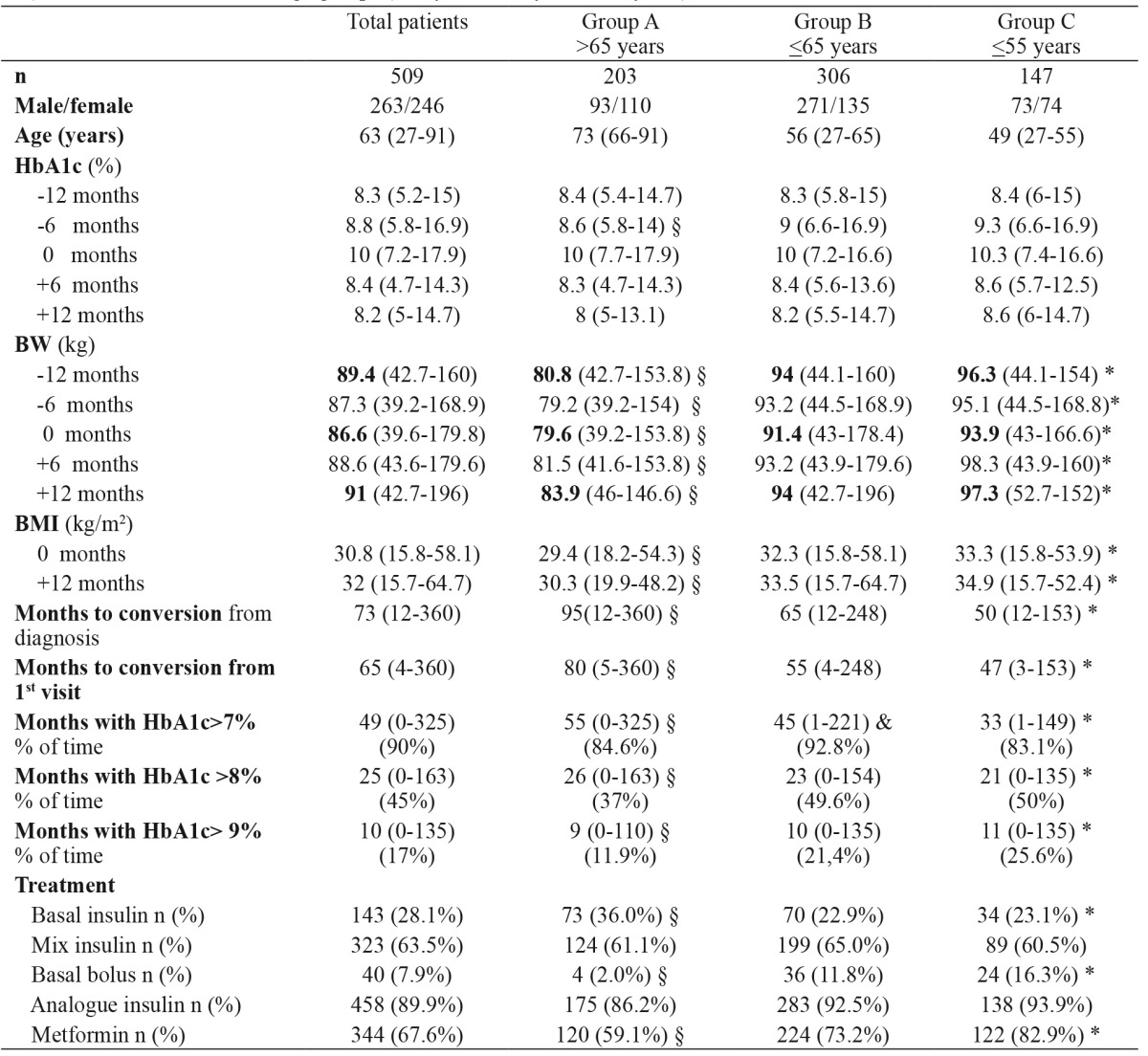
Results are shown as median and range. Months before conversion to insulin are indicated as -6 months and -12 months. Months after conversion to insulin are indicated as +6 months and +12 months and the time of conversion is indicated as 0 months. n: number of patients, HbA1c: glycated hemoglobin, BW: body weight, BMI: body mass index, §: p<0.05 between groups A and B, *: p<0.05 between groups A and C, &: p<0.05 between groups B and C.
The majority of patients (89.9%) started therapy with insulin analogues and continued with that. More than half were commenced an analogue mixture and the rest were treated with combination therapy (OAD + basal insulin) or with multiple day insulin therapy. There was a significant reduction in HBA1c (p<0.05) after the initiation of insulin at all age groups with all insulin regimen at 12 months but there was also an significant increase in BW(p<0.05).
Results
From 11,029 patients with type 2 diabetes, 1,364 had an insulin prescription. From these, 529 had started insulin before 2002, 99 were on insulin from their first visit or started insulin in less than 12 months from diagnosis, 22 were converted during pregnancy or planning pregnancy, 5 proved to have type 1 diabetes, 32 were converted during hospitalization for acute illness and 10 proved not to be on insulin. Finally from 1,221 files with sufficient data, 509 fulfilled the inclusion criteria.
Median age of the patients at the time of conversion was 63 (range 27-91) years. Two hundred fifty were women and 54 were deceased. The median time until a patient started insulin therapy after failure of other treatments was 73 (12-360) months after diabetes diagnosis and 65 (4-360) months from their first visit at GP or DT. HbA1c at time of conversion was 10% (7.2-17.9) and they spent 49 (0-325) months with HbA1c >7%, 25 (0-163) months with HbA1c >8% and 10 (0-135) months with HbA1c >9% which were 90%, 45% and 17% of their time under consultation respectively. HbA1c was 8.3% (5.2-15) at 12 months before conversion and decreased to 8.2% (5-14.7) at 12 months after conversion. There was a 2.9 kg [(-18.4)-(+11.7), p<0.05] increase in BW at 12 months after the initiation of insulin.
There was no difference in HbA1c level at the time of initiation of insulin between older and younger patients, but patients younger than 55 years were more overweight, 93.9 kg (43-166.6), were converted to insulin earlier (47 vs. 65 months) from their first consultation, and spent more time with uncontrolled diabetes (HbA1c >9%: 25.6 % of time vs. 11.9 % in patients older than 65 years) (Table 1).
The majority of patients (89.9%) started therapy with insulin analogues and continued with that. More than half were commenced an analogue mixture and the rest were treated with combination therapy (OAD + basal insulin) or with multiple day insulin therapy. There was a significant reduction in HBA1c (p<0.05) after the initiation of insulin at all age groups with all insulin regimen at 12 months but there was also an significant increase in BW(p<0.05).
Limitations
The main limitation of the current study is its retrospective design, as there is no available data regarding complications, co-morbidities or symptoms that perhaps could affect clinicians' decisions to initiate insulin therapy. Moreover, there is no information regarding the factors that influenced both physicians and patients in delaying the change in therapy.
Conclusions
The current study shows that there is a gap between national and International Guidelines Recommendations and real-life clinical practice. There is a delay in the initiation of insulin therapy after other treatment failure resulting in patients been exposed to prolonged period of hyperglycemia. After the initiation of insulin, there is a significant improvement in glycemic control but also an increase in BW. It is important to investigate the factors that act as barriers for insulin therapy initiation and perhaps a change in practical clinical guidelines is needed, in order to shorten the time period from patient's treatment failure to insulin therapy initiation.
Conflict of interest
Authors report no conflict of interest.
References
- 1.Williams R, Van Gaal L, Lucioni C, CODE-2 Advisory Board Assessing the impact of complications on the costs of type II diabetes. Diabetologia. 2002;45:S13–S17. doi: 10.1007/s00125-002-0859-9. [DOI] [PubMed] [Google Scholar]
- 2.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2005. prevalence, numerical estimates, projections. Diabetes Care. 1998;21:1414–1431. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 3.Brand FN, Abbott RD, Kannel WB. Diabetes, intermittent claudication and risk of cardiovascular events. The Framingham Study. Diabetes. 1989;38:504–509. doi: 10.2337/diab.38.4.504. [DOI] [PubMed] [Google Scholar]
- 4.UK Prospective Diabetes Study (UKPDS) Group Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34) Lancet. 1998;352:854–865. [PubMed] [Google Scholar]
- 5.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 6.Koro CE, Bowlin SJ, Bourgeois N, Fedder DO. Glycemic control from 1988 to 2000 among U.S. adults diagnosed with type 2 diabetes: a preliminary report. Diabetes Care. 2004;27:17–20. doi: 10.2337/diacare.27.1.17. [DOI] [PubMed] [Google Scholar]
- 7.Inherited Clinical Guideline G. Management of type 2 Diabetes. Management of glucose control. National Institute for Clinical Excellence, London, 2002, S4, available at: http://www.clinbiochem.info/nicehba1c.pdf. last accessed: 20/1/15.
- 8.American Diabetes Association Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2002;25:213–229. doi: 10.2337/diacare.25.1.213. [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association Standard of medical care for patients with diabetes mellitus (position statement) Diabetes Care. 2004;27:S15–S35. doi: 10.2337/diacare.27.2007.s15. [DOI] [PubMed] [Google Scholar]
- 10.Kilpatrick ES, Das AK, Orskov C, Berntorp K. Good glycaemic control: an international perspective on bridging the gap between theory and practice in type 2 diabetes. Curr Med Res Opin. 2008;24:2651–2661. doi: 10.1185/03007990802347209. [DOI] [PubMed] [Google Scholar]
- 11.Currie CJ, Gale EA, Poole CD. Estimation of primary care treatment costs and treatment efficacy for people with Type 1 and Type 2 diabetes in the United Kingdom from 1997 to 2007*. Diabet Med. 2010;27:938–948. doi: 10.1111/j.1464-5491.2010.03040.x. [DOI] [PubMed] [Google Scholar]
- 12.Brown JB, Nichols GA, Perry A. The burden of treatment failure in type 2 diabetes. Diabetes Care. 2004;27:1535–1540. doi: 10.2337/diacare.27.7.1535. [DOI] [PubMed] [Google Scholar]
- 13.Rubino A, McQuay LJ, Gough SC, Kvasz M, Tennis P. Delayed initiation of subcutaneous insulin therapy after failure of oral glucose-lowering agents in patients with Type 2 diabetes: a population-based analysis in the UK. Diabet Med. 2007;24:1412–1428. doi: 10.1111/j.1464-5491.2007.02279.x. [DOI] [PubMed] [Google Scholar]
- 14.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. American Diabetes Association (ADA);European Association for the Study of Diabetes (EASD). Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association fot the Study of Diabetes (EASD) Diabetes Care. 2012;35:1364–1379. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunt LM, Valenzuela MA, Pugh JA. NIDDM patients' fears and hopes about insulin therapy: the basis of patient reluctance. Diabetes Care. 1997;20:292–298. doi: 10.2337/diacare.20.3.292. [DOI] [PubMed] [Google Scholar]
- 16.Wolffenbuttel BH, Drossaert CH, Visser AP. Determinants of injecting insulin in elderly patients with type II diabetes mellitus. Patient Educ Couns. 1993;22:117–125. doi: 10.1016/0738-3991(93)90091-a. [DOI] [PubMed] [Google Scholar]
- 17.Zambanini A, Newson RB, Maisey M, Feher MD. Injection related anxiety in insulin-treated diabetes. Diabetes Res Clin Pract. 1999;46:239–246. doi: 10.1016/s0168-8227(99)00099-6. [DOI] [PubMed] [Google Scholar]
- 18.Bashoff EC, Beaser RS. Insulin therapy and the reluctant patient. Overcoming obstacles to success. Postgrad Med. 1995;97:86–90. [PubMed] [Google Scholar]


