Abstract
Introduction:
Manual ability and performance of dexterity tasks require both gross and fine hand motions and coordination. The aim of this study was to determine the level of manual dexterity (capacity) and investigate its relationship with manual ability (performance) in children with cerebral palsy.
Method:
This study was designed as a cross-sectional study of 30 children with cerebral palsy (aged 8-15 years). In order to assess gross manual dexterity the Box and Block Test was used. Manual ability was assessed according to Manual Ability Classification System (MACS).
Results:
A relationship between the level of manual ability impairment and performance on manual dexterity tasks was expressed. Participants at MACS level IV demonstrated slowest times and transferred the smallest number of blocks (p<0.01). This study also found that correlation between Gross Motor Function Classification Scale (GMFCS) and MACS is statistically significant (p<0.001). All hand skills were more impaired in the non-dominant hand compared to the dominant hand but there were no statistically significant difference (p=0.06).
Conclusion:
The results suggest that gross manual dexterity is a good predictor of manual abilities in children with cerebral palsy. These results provide better understanding of the relationship between manual dexterity and activity limitations and lend credibility to the use of these classification systems and assessments in order to optimize treatment planning and evaluate interventions and progress. Hippokratia 2014; 18 (4): 310-314.
Keywords: Cerebral palsy, gross manual dexterity, fine finger dexterity
Introduction
Cerebral palsy (CP) is characterized by motor dysfunction caused by non-progressive brain damage, which occurs early in life1. Various impairments could affect the child's ability to respond to environmental and socio-cultural needs, including limitations in strength, sensibility, fluency, accuracy, dexterity2-4. The limitations can affect body structure and function, as well as activity and participation domains5.
More than a half of the children, diagnosed with CP experience various upper limb problems, of different severity and heterogeneity1-7. Manual ability refers to the child's attempt to perform a particular activity. Manual ability and performance of dexterity tasks require both gross and fine hand motions and coordination. Children with CP usually have difficulties performing manual activities such as grasping, releasing or manipulating objects, which is crucial in the performance of many activities of daily life4,6-9. Hand function problems in children with CP are often associated with problems of motor control, active range of motion, grip strength and persistence of primitive grasp reflex8, but are not always correlated with manual ability impairments6,10. Moreover, manual ability and achievement in motor tasks can be influenced by motivation and cognition1. Manual activities require the cooperation of both hands, where the dominant hand performs both fine and gross manipulations, and the non-dominant hand is used to stabilize objects11. Children with CP develop their handedness on the less affected side. Gross manual dexterity and grip strength on both hands, followed by fine finger dexterity are the strongest predictors of manual ability, while tactile pressure detection and proprioception show lowest correlation with manual ability12,13. Manual dexterity was found to be a strong predictor of functional independence in activities of daily living14,15. The limited arm function is present in all types of CP, but the characteristics of the disorder vary depending on the subtypes of CP16. Recent reviews of the relationship between upper limb impairments and functional abilities focused on activity limitations and restrictions in participation1,17-19.
The need to measure efficiency, body structure and function, activity level as well as participation outcomes effectively in children with CP is important in order to optimize treatment planning and evaluate interventions and progress11. Previous studies on children with CP had a tendency to focus on analyzing their gross motor functions. However, as reviewed by some authors, many reliable and valid assessment tools became available to measure functional skills in children with CP20,21. This shift in focus and increasing interest in manual ability and dexterity of children diagnosed with CP improved the understanding of the condition and facilitated the design of appropriate treatments22.
The general purpose of this study was to apply instruments that were not applied in this area and thus contribute to the assessment of manual ability and dexterity of children diagnosed with CP. A more specific aim of the study was to determine the level of manual dexterity (capacity) and research its relationship with manual ability (performance) in children with CP.
Materials and Methods
Participants
The study population consisted of 30 children with congenital CP aged 8-15 years [mean 11.95 standard deviation (SD) 2.56], included 17 male (56.7%) and 13 female (43.3%) participants. The sample was comprised of CP of 12 hemiparetic children (40%), 6 diparetic children (20%) and 12 quadriparetic children (40%). Nineteen children (63.3%) were right handed, 9 left handed (30%) and two ambidextrous (6.7%). Intellectual disability was present in 5 participants (16.7%).
All participants were diagnosed with spastic CP, and were able to understand the test instructions. The participants were recruited from two schools for students with special needs. The exclusion criteria were other diagnosis of CP, insufficient cooperation, surgery interventions on upper limb, and botulinum toxin injections administered in the last 6 months. The study was approved by the School's Ethical Committee. Informed consent was obtained from children's parents or guardians as well as school administrators, who were informed about the aim and course of this research.
Instruments
Motor skills were assessed using the Gross Motor Function Classification Scale (GMFCS), while manual abilities were assessed with the Manual Ability Classification System (MACS). The Box and Blocks test (BBT) was used to study manual dexterity. GMFCS and MACS were completed by the examiners who are experts in the field of special education and rehabilitation, based on their observation of the child's behaviour.
The GMFCS is a five level classification system used to determine which level best represents the child's present abilities and limitations in gross motor function. Level I, includes children with minimal or no disability, while level V, includes children who are totally dependent on external assistance for mobility23.
The MACS, like the GMFCS, is a five level system, where level I includes children with minor limitations, while children with severe functional limitations are to be found at level IV and V24,25. Gross manual dexterity was measured using the BBT according to the procedure described by Mathiowetz26. The equipment for the BBT is consisted of a wooden box size 53.7 x 25.4 cm divided into two compartments by a partition, 15.2 cm in height. Participants were instructed to grasp the blocks (diameter of 2.5 cm) individually from one compartment of the box, transport them over the partition, and release them into the opposite compartment of the box as quickly as possible within 60 seconds. They performed the test once with each hand, starting with the dominant hand.
Statistical analysis
Descriptive statistics were used to report general characteristics of the sample. The non-parametric Kruskal Wallis analysis of variance was used to compare more than two groups with multiple comparisons of ranks as a post hoc test. The relationship between manual dexterity and MACS levels was analyzed using the Spearman rank order correlation, with correlation coefficients >0.70 considered as high, 0.50-0.70 as good, 0.30-0.50 as fair and <0.30 as weak or no association. Statistical significance was defined as a p-value of <0.0527.
Results
The largest number of children was classified at GMFCS level II and MACS level III. Fourteen children (46.7%) of the total sample were classified at GMFCS level II while 11 children (36.7%) were classified at MACS level III. Based on the type of CP, most children were classified at the highest levels (IV, V) in both classifications and they were diagnosed with quadriparesis.
In order to measure manual dexterity, the Box and Block Test was used. Firstly, the performance of these tasks was observed depending on whether they were carried out using the dominant or the non-dominant hand. Wilcoxon matched pairs test, which was used for comparison, did not show statistically significant difference (p=0.06) in the performance of the tasks regardless whether the measurements were made on the dominant or non-dominant hand (Table 1). The results of the task showed a clear trend toward significance on the gross manual dexterity task (mean value was 20.75 on the dominant hand and 16.23 on the non-dominant hand).
Table 1. Performance on the dominant and non-dominant hand on manual dexterity test.
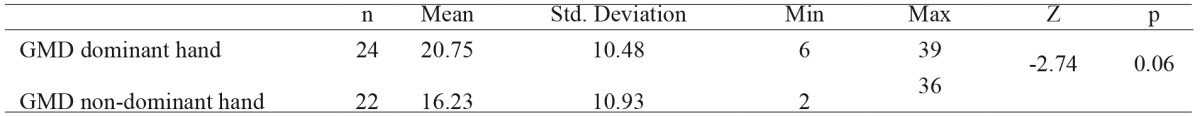
GMD: gross manual dexterity.
The Kruskal Wallis test was used to analyze performance on manual dexterity tasks related to CP subgroups and MACS levels (Table 2). Multiple comparisons of ranks as a post hoc test showed statistically significant difference in gross manual dexterity (p<0.00) between hemiparetic and diparetic subgroups, as well as between hemiparetic and quadriparetic subgroups, with achievement in hemiparetic subgroup higher than in the other two. Same statistical test was used to analyze performance on manual dexterity task related to MACS levels. The participants who were classified at MACS level V were not able to perform these tasks, while the participants at MACS level IV recorded slowest and transferred the smallest number of blocks. Multiple comparisons of ranks as a post hoc test showed statistically significant difference in gross manual dexterity performance across MACS levels I-IV (p<0.01).
Table 2. Distribution of achievements on manual dexterity tests across cerebral palsy subgroups and manual ability classification system (MASC) levels.
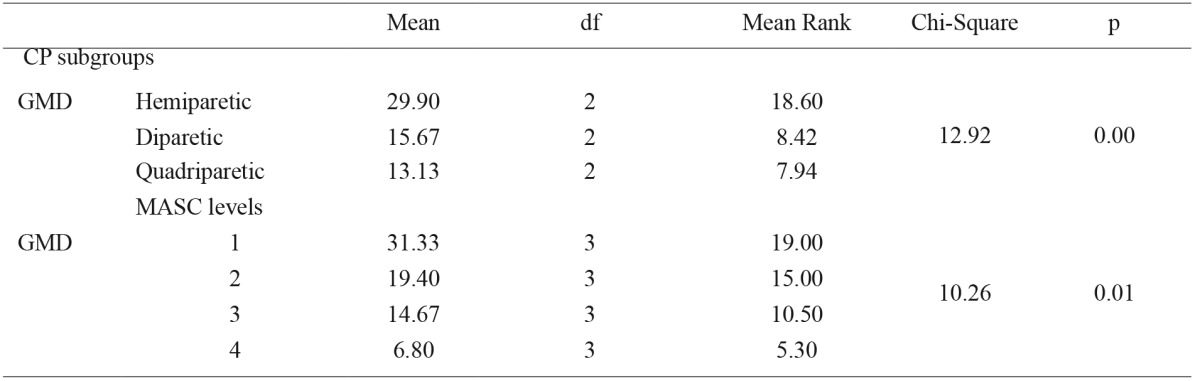
CP: cerebral palsy, MACS: manual ability classification system, GMD: gross manual dexterity, df: degrees of freedom.
Correlation between GMFCS and MACS in the sample was high (Spearman r=0.73, p<0.01). In terms of CP subgroups, the most pronounced correlation between these tests was noted in the group of children with quadriparesis (Spearman r=0.83, p<0.01), followed by the group of children with hemiparesis (Spearman r= 0.63, p< 0.03). Conversely, in the group of children with diparesis, the correlation was not statistically significant (Spearman r=0.48, p>0.05), which may be explained by the type of impairment where muscle stiffness is mainly in the legs, and small sample size (n = 6) in this subgroup.
Manual abilities represented through MACS significantly but moderately correlated with gross manual dexterity (r=-0.467, p<0.05). At the same time GMFCS levels significantly correlated with gross manual dexterity (r=-0.654, p<0.01).
Discussion
In this study participants' manual ability was initially categorized by assessing their performance when handling objects in daily life and their movement ability by measuring gross motor functions. Based on the results obtained using the MACS it can be observed that 73.33% participants required assistance in preparation and/or adaptation to the activity, otherwise they experienced limitations when performing even the simplest activities. These results are consistent with the findings of other researchers who reported that children with CP show limitations in performing activities of daily living28-30.
The study concurs with similar studies, where quadriparetic children are presented with considerably impaired manual abilities and gross motor functions16,24,31-33. The results revealed that the participants with quadriparesis recorded slowest and transferred the smallest number of blocks.
The degree of deformity, impairments, and motor control affected the hand function and performance of gross motor activities of CP participants2. Those with pronounced deformities, contractures and reduced motor control reduced capacity and performance in carrying out everyday activities. In more than 30% of hemiparetic children impairments are present on non-paretic dominant hand13. Therefore children with CP had more problems when performing daily manual activities than gross motor abilities. These findings are in line with previous studies9,25,32.
The correlation values across the CP subgroups were different, with the most significant correlation reported in quadriparetic children. The degree of deformity, impairments, body conditions, cognition and motivation could effect on motor skills in children with CP6,34-38. These findings imply that GMFCS and MACS classifications work well together. The data obtained using these two classification systems, provides for a comprehensive overview of the child's capabilities, facilitating the design of the treatment plan and monitoring.
While it is true that gross motor functions are important predictors of daily living activity in children with CP39, they are not the only predictive instruments. In the present study, manual dexterity was explored with respect to CP subgroups and its relationship with manual abilities. The results emphasize the importance of manual dexterity as presented through gross manual dexterity.
Properly results on gross manual dexterity, in this study, could be explained by the fact that when manipulating bigger objects children use different manual strategies to perform the tasks contrary to fine finger dexterity, which requires more complex movements. These findings lend support to previous studies and imply that training should address gross manual dexterity, finger coordination, distal muscles strength, as well as increasing bimanual skills, which can result in developing more effective movement strategies36,40.
Results were analyzed on gross manual dexterity as associated with to MACS levels. The results revealed that the participants with quadriparesis recorded slowest and transferred the smallest number of blocks, and needed extra time when tasking.
In this study gross manual dexterity was significantly but moderately correlated with MACS. These results lend support to previous studies showing that gross manual dexterity is the strongest predictor of manual ability12,13. Nevertheless, current results showed marked differences in manual dexterity depending on the level of manual ability, thus demonstrating that manual dexterity has an important impact on activity measures.
Further research is necessary in order to overcome limitations of this study, and to explore these problems on a larger sample, while taking hand impairments, training and motivation into account with the aim of providing guidelines for assessment and better planning of rehabilitation programs.
Limitations of the study
Since this cross-sectional study included a small sample of children with CP, the ability to generalize the results is limited. The composition and size of the sample may have had an effect on the absence of differences between the results related to the dominant and non-dominant hand. Moreover, the smallest number of participants was in the diparetic group of children, where the best results in manual activities can be expected. The disparity might be further explained by the fact that hemiparetic children experience problems in the non-dominant hand as well.
No other different assessment tool results were used.
Conclusions
This study investigated the relationship between manual abilities and manual dexterity in children with CP. The results showed that gross manual dexterity was the best predictor of manual abilities in children with CP. Moreover, children at a lower MACS level had more success in manual dexterity tasks. In particular, manual activities were determined by the degree of impairment. These results provide a better understanding of the relationship between manual dexterity and activity limitations and lend credibility to the usage of these classification systems and assessments to optimize treatment planning and evaluate interventions and progress.
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Levitt S. Treatment of Cerebral Palsy and Motor Delay. Wiley-Blackwell, John Wiley & Sons, Chichester, United Kingdom. 2010:1–13. [Google Scholar]
- 2.Law K, Lee EY, Fung BK, Yan LS, Gudushauri P, Wang KW, et al. Evaluation of deformity and hand function in cerebral palsy patients. J Orthop Surg Res. 2008;3:52. doi: 10.1186/1749-799X-3-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sorsdahl AB, Moe-Nilssen R, Kaale HK, Rieber J, Strand LI. Change in basic motor abilities, quality of movement and everyday activities following intensive, goal-directed, activity-focused physiotherapy in a group setting for children with cerebral palsy. BMC Pediatr. 2010;10:26–26. doi: 10.1186/1471-2431-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park ES, Sim EG, Rha DW. Effect of upper limb deformities on gross motor and upper limb functions in children with spastic cerebral palsy. Res Dev Disabil. 2011;32:2389–2397. doi: 10.1016/j.ridd.2011.07.021. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization International Classification of Functioning, Disability and Health (ICF). World Health Organization, Geneva. 2001 [Google Scholar]
- 6.Arnould C, Penta M, Thonnard JL. Hand impairments and their relationship with manual ability in children with cerebral palsy. J Rehabil Med. 2007;39:708–714. doi: 10.2340/16151977-0111. [DOI] [PubMed] [Google Scholar]
- 7.Koman LA, Williams RM, Evans PJ, Richardson R, Naughton MJ, Passmore L, et al. Quantification of upper extremity function and range of motion in children with cerebral palsy. Dev Med Child Neurol. 2008;50:910–917. doi: 10.1111/j.1469-8749.2008.03098.x. [DOI] [PubMed] [Google Scholar]
- 8.Li-Tsang CWP. The hand functions of children with and without neurological motor disorders. Int J Dev Disabil. 2003;49:99–110. [Google Scholar]
- 9.Öhrvall AM, Eliasson AC, Löwing K, Ödman P, Krumlinde-Sundholm L. Self-care and mobility skills in children with cerebral palsy, related to their manual ability and gross motor function classifications. Dev Med Child Neurol. 2010;52:1048–1055. doi: 10.1111/j.1469-8749.2010.03764.x. [DOI] [PubMed] [Google Scholar]
- 10.Penta M, Tesio L, Arnould C, Zancan A, Thonnard JL. The ABILHAND questionnaire as a measure of manual ability in chronic stroke patients: Rasch-based validation and relationship to upper limb impairment. Stroke. 2001;32:1627–1634. doi: 10.1161/01.str.32.7.1627. [DOI] [PubMed] [Google Scholar]
- 11.Kimmerle M, Mainwaring L, Borenstein M. The functional repertoire of the hand and its application to assessment. Am J Occup Ther. 2003;57:489–498. doi: 10.5014/ajot.57.5.489. [DOI] [PubMed] [Google Scholar]
- 12.Krumlinde-Sundholm L, Eliasson AC. Comparing tests of tactile sensibility: aspects relevant to testing children with spastic hemiplegia. Dev Med Child Neurol. 2002;44:604–612. doi: 10.1017/s001216220100264x. [DOI] [PubMed] [Google Scholar]
- 13.Arnould C. Hand functioning in children with cerebral palsy. Louvian la Neuve, CIACO. 2006 doi: 10.3389/fneur.2014.00048. available from: http://www. abilhand.org/download/ABILHAND_thesis_2006.pdf, accessed: 15/01/2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flunn NA, Trombly-Latham CA, Podolski CR. Assessing abilities and capacities: Range of motion, strength and endurance. Radomski MV, Trombly-Latham CA (eds) Occupational therapy for physical dysfunction, Lippincott Williams & Wilkins, Philadelphia. 2007:91–186. [Google Scholar]
- 15.Rand D, Eng JJ. Arm-hand use in healthy older adults. Am J Occup Ther. 2010;64:877–885. doi: 10.5014/ajot.2010.09043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arner M, Eliasson AC, Nicklasson S, Sommerstein K, Hägglund G. Hand function in cerebral palsy. Report of 367 children in a population-based longitudinal health care program. J Hand Surg Am. 2008;33:1337–1347. doi: 10.1016/j.jhsa.2008.02.032. [DOI] [PubMed] [Google Scholar]
- 17.Harvey A, Robin J, Morris ME, Graham HK, Baker R. A systematic review of measures of activity limitation for children with cerebral palsy. Dev Med Child Neurol. 2008;50:190–198. doi: 10.1111/j.1469-8749.2008.02027.x. [DOI] [PubMed] [Google Scholar]
- 18.Klingels K, Feys H, De Wit L, Jaspers E, Van de Winckel A, Verbeke G, et al. Arm and hand function in children with unilateral cerebral palsy: a one-year follow-up study. Eur J Paediatr Neurol. 2012;16:257–265. doi: 10.1016/j.ejpn.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 19.McConnell K, Johnston L, Kerr C. Upper limb function and deformity in cerebral palsy: a review of classification systems. Dev Med Child Neurol. 2011;53:799–805. doi: 10.1111/j.1469-8749.2011.03953.x. [DOI] [PubMed] [Google Scholar]
- 20.Gilmore R, Sakzewski L, Boyd R. Upper limb activity measures for 5- to 16-year-old children with congenital hemiplegia: a systematic review. Dev Med Child Neurol. 2010;52:14–21. doi: 10.1111/j.1469-8749.2009.03369.x. [DOI] [PubMed] [Google Scholar]
- 21.Wagner LV, Davids JR. Assessment tools and classification systems used for the upper extremity in children with cerebral palsy. Clin Orthop Relat Res. 2012;470:1257–1271. doi: 10.1007/s11999-011-2065-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arnould C, Bleyenheuft Y, Thonnard JL. Hand functioning in children with cerebral pasly. Front Neurol. 2014;5:48–48. doi: 10.3389/fneur.2014.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- 24.Eliasson A, Krumlinde-Sundholm L, Rösblad B, Beckung E, Arner M, Ohrvall A, et al. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. 2006;48:549–554. doi: 10.1017/S0012162206001162. [DOI] [PubMed] [Google Scholar]
- 25.Gunel MK, Mutlu A, Tarsuslu T, Livanelioglu A. Relationship among the Manual Ability Classification System (MACS), the Gross Motor Function Classification System (GMFCS), and the functional status (WeeFIM) in children with spastic cerebral palsy. Eur J Pediatr. 2009;168:477–485. doi: 10.1007/s00431-008-0775-1. [DOI] [PubMed] [Google Scholar]
- 26.Mathiowetz V, Federman S, Wiemer D. Box and Block Test of manual dexterity: Norms for 6-19 year olds. Can J Occup Ther. 1985;52:241–245. [Google Scholar]
- 27.Fajgelj S. Psihometrija Metod i teorija psiholo kog merenja. Centar za primenjenu psihologiju, Belgrade. 2009 [Google Scholar]
- 28.Donkervoort M, Roebroeck M, Wiegerink D, van der Heijden-Maessen H, Stam H; Transition Research Group South West Netherlands. Determinants of functioning of adolescents and young adults with cerebral palsy. Disabil Rehabil. 2007;29:453–463. doi: 10.1080/09638280600836018. [DOI] [PubMed] [Google Scholar]
- 29.Kerr C, McDowell B, McDonough S. The relationship between gross motor function and participation restriction in children with cerebral palsy: an exploratory analysis. Child Care Health Dev. 2007;33:22–27. doi: 10.1111/j.1365-2214.2006.00634.x. [DOI] [PubMed] [Google Scholar]
- 30.van Eck M, Dallmeijer AJ, van Lith IS, Voorman JM, Becher J. Manual ability and its relationship with daily activities in adolescents with cerebral palsy. J Rehabil Med. 2010;42:493–498. doi: 10.2340/16501977-0543. [DOI] [PubMed] [Google Scholar]
- 31.Beckung E, Hagberg G. Neuroimpairments, activity limitations, and participation restrictions in children with cerebral palsy. Dev Med Child Neurol. 2002;44:309–316. doi: 10.1017/s0012162201002134. [DOI] [PubMed] [Google Scholar]
- 32.Carnahan KD, Arner M, Hägglund G. Association between gross motor function (GMFCS) and manual ability (MACS) in children with cerebral palsy. A population-based study of 359 children. BMC Musculoskelet Disord. 2007;8:50–50. doi: 10.1186/1471-2474-8-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Howard J, Soo B, Graham HK, Boyd RN, Reid S, Lanigan A, et al. Cerebral palsy in Victoria: motor types, topography and gross motor function. J Paediatr Child Health. 2005;41:479–483. doi: 10.1111/j.1440-1754.2005.00687.x. [DOI] [PubMed] [Google Scholar]
- 34.Ostensjø S, Carlberg EB, Vøllestad NK. Motor impairments in young children with cerebral palsy: relationship to gross motor function and everyday activities. Dev Med Child Neurol. 2004;46:580–589. doi: 10.1017/s0012162204000994. [DOI] [PubMed] [Google Scholar]
- 35.Park ES, Rha DW, Park JH, Park DH, Sim EG. Relation among the gross motor function, manual performance and upper limb functional measures in children with spastic cerebral palsy. Yonsei Med J. 2013;54:516–522. doi: 10.3349/ymj.2013.54.2.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klingels K, Demeyere I, Jaspers E, De Cock P, Molenaers G, Boyd R, et al. Upper limb impairments and their impact on activity measures in children with unilateral cerebral palsy. Eur J Paediatr Neurol. 2012;16:475–484. doi: 10.1016/j.ejpn.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 37.Houwink A, Aarts PB, Geurts AC, Steenbergen B. A neurocognitive perspective on developmental disregard in children with hemiplegic cerebral palsy. Res Dev Disabil. 2011;32:2157–2163. doi: 10.1016/j.ridd.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 38.Chu S. Occupational therapy for children with handwriting difficulties: A framework for evaluation and treatment. Br J Occup Ther. 1997;60:514–520. [Google Scholar]
- 39.Ostensjø S, Carlberg EB, Vøllestad NK. Everyday functioning in young children with cerebral palsy: functional skills, caregiver assistance, and modifications of the environment. Dev Med Child Neurol. 2003;45:603–612. doi: 10.1017/s0012162203001105. [DOI] [PubMed] [Google Scholar]
- 40.Holmefur M, Krumlinde-Sundholm L, Bergström J, Eliasson AC. Longitudinal development of hand function in children with unilateral cerebral palsy. Dev Med Child Neurol. 2010;52:352–357. doi: 10.1111/j.1469-8749.2009.03364.x. [DOI] [PubMed] [Google Scholar]


