Abstract
Background
Non-communicable diseases (NCDs) exist in slums as the inhabitants adopt an urbanized lifestyle which places them at a higher risk for. Lack of knowledge about the morbidity, complications and the method of control contributes to a large percentage of undetected and untreated cases.
Methods
This cross-sectional survey polled 2,434 respondents from Ijora Oloye, Ajegunle and Makoko, three urban slums in Lagos metropolis, southwestern Nigeria between June 2010 and October 2012. We investigated the prevalence of hypertension, diabetes and obesity. Respondents signed consent forms and their health conditions were documented based on self-reported history of diabetes, hypertension and family history using a semi-structured questionnaire. Diagnostic tests; weight and height for body mass index, blood glucose, and blood pressure were performed.
Results
More than one quarter of the participants were suffering from hypertension and only half of this were diagnosed earlier, while a further few were already on treatment. Therefore on screening, it had been possible to diagnose over three hundred more respondents, who were not previously aware of their health status. The respondents’ BMI showed that more than half of them were either overweight or obese and are at risk for diabetes, while 3.3% were confirmed as being diabetic, with their sugar levels greater than the normal range.
Conclusion
This study therefore revealed the near absence of screening programs for chronic diseases such as hypertension, diabetes and obesity in these urban slums. This was further confirmed by the detection of new and undiagnosed cases of hypertension in about one quarter of the respondents.
Keywords: Survey, Non-communicable diseases, Hypertension, Diabetes, Obesity, Urban slums
Introduction
United Nations Human Settlements gave a comprehensive global description of urban slum communities and attempted to identify different approaches to address this problem to achieve the United Nations Millennium Development Goals (MDGs). At the United Nations Expert Group meeting held in Nairobi in 2002, a slum was operationally defined as a human settlement that has the following characteristics: inadequate access to safe water, sanitation and other infrastructure, poor structural quality of housing, overcrowding and insecure residential status (1, 2). Currently, these characteristics describe communities that comprise 43% of the combined urban populations in all developing countries, and 78% of the urban population in least developed countries (2). Apart from the standard social indices, such as life expectancy at birth, under five mortality rates and access to improved water sources and sanitation, the report did not address disease spectrum or burden in these communities. Hence little is known about the spectrum and burden of disease morbidity in urban slums of the world, whereas lack of such data hampers adequate health care resource allocation and provision of appropriate disease prevention services. In many countries, most disease burden or mortality information on urban slum dwellers is largely based on clinic, hospital, or national mortality registry data. This type of information is not sufficient to plan health care expenditures, and grossly underestimates or misdirects the health care resource allocation needs.
Non-communicable diseases refer to diseases or conditions that occur in, or are known to affect, individuals over an extensive period of time and for which there are no known causative agents that are transmitted from one affected individual to another (3). Hypertension, diabetes, cardiovas-cular disease, lung diseases, chronic respiratory diseases, cancer, mental health problems, asthma, atherosclerosis and allergy are non-communicable diseases that are rapidly emerging as public health challenge to urban slum populations, whereas 72% of the total global burden of disease in adults thirty years or older are due to these chronic diseases (4–7). They also noted that formal health sector becomes aware of the health problems of slum populations relatively late in the course of their illnesses. As such, it inevitably deals with the severe and end-stage complications of these diseases at a substantially greater cost than what it costs to manage non-slum community populations.
Nigeria relies mainly on data from the national health management information systems in order to estimate the national burden of NCDs as it has not conducted surveys to establish the national base line prevalence rates of these diseases so as to accurately quantify the magnitude of the problem. Nevertheless, it has been estimated that about 5 million Nigerians may die of NCDs by the year 2015, while diabetes alone is projected to cause about 52% of the mortality by 2015 (8). Presently, about 8 million Nigerians suffer from hypertension and 4 million has diabetes, also 100, 000 new cases of cancers are diagnosed each year, and about ten thousand Nigerians die annually due to injuries from road traffic accidents (9). However, due to the informal nature of slum settlements, and cultural, social, and behavioral factors unique to the slum populations, little is known about the burden of these chronic but preventable diseases in the three communities surveyed for this study. Besides, the inhabitants are often unable to access the education and services required to prevent and treat NCDs. This study therefore aimed at determining the prevalence of hypertension, diabetes and obesity in three urban slums within Lagos metropolis, southwestern Nigeria. It is hoped that this will shed more light on some health challenges facing the inhabitants and also inform local health authorities for timely intervention.
Methods
Study sites and sample size calculation
The study population consisted of individuals who were 5 years and above living permanently in Ajegunle in Ajeromi Ifelodun Local Government Area (LGA); Ijora Oloye in Apapa( LGA); Makoko in Mainland (LGA). The current populations (Ajegunle - 429,381; Ijora Oloye - 18,278; Makoko - 141,277) were calculated based on the projected growth rate of 7.5% using the 1991 national census figures as baseline. Sample size of single proportion method using EPI Info version 6 was used to calculate the sample size of 2,434 individuals. The calculated sample size was equally divided within the three communities.
Ethical consideration and consent documentation
Prior to the commencement of the project, ethical clearance was obtained from the Institutional Review Board of the Nigerian Institute of Medical Research. Informed consent of the leaders and stakeholders in the three communities was received. Permission to carry out the project in the selected communities was obtained from the three Local Government Area authorities overseeing the study communities.
Research design and sampling techniques
A cross-sectional survey was employed to elicit essential information from the respondents. Before the commencement of the survey, training was provided on a one to one basis to all research assistants selected to participate in the study, with the aim of enhancing their understanding of the research protocols and competence in administering the questionnaire. They were also trained to use the electronic machine to measure blood pressure and glucometer for estimating blood glucose. The training helped to avoid biases or errors in the procedures employed and ensured their understanding and unified interpretation of basic terminologies that were used in the study. After the training, there was a pilot study which helped the team to have a foretaste of problems that might be encountered during the main survey and also to test the reliability, validity and applicability of the research instruments.
Cross sectional survey
A multi-stage sampling method was used to sample 2,434 household members across different socioeconomic background. The first stage of this technique involved the stratification of each community into two groups on the basis of geographical closeness. The second stage was the clustering of each of the 2 groups into different Enumeration Areas (EAs) on the basis of existing delineation by National Population Commission of Lagos State in the 2006 population census exercise. Third stage involved random selection of four EAs from each of the three selected slum communities. The fourth stage involved numbering of houses in each of the selected EAs and selection of houses from the numbered houses within each of the strata using systematic random sampling. The final step was the random sampling of households from each of the sampled houses by writing the identification numbers of the households on pieces of paper and the desired sample was selected by picking the required number of papers. Each household corresponding to the numbers chosen was then included in the sample. Thereafter, same method was adopted to select eligible households within a sampled building. However, names of heads of the households were used in place of identification numbers. A total of 2,434 respondents were polled from Ijora Oloye (805), Ajegunle (814) and Makoko (815) communities. Figure 1 and 2 shows maps of Nigeria and the study communities in Lagos state, southwestern Nigeria. The survey made use of a semi-structured questionnaire, while the units of analysis for the survey were households. The questionnaire included details regarding demographic and socio-economic characteristics like participant’s self reported age, sex, educational status and occupational status. Health conditions were documented based on self-reported history of diabetes, and hypertension and family history for the conditions was also collected.
Fig. 1.

Map of Nigeria showing states and zones, with arrow pointing to Lagos state
Fig. 2.
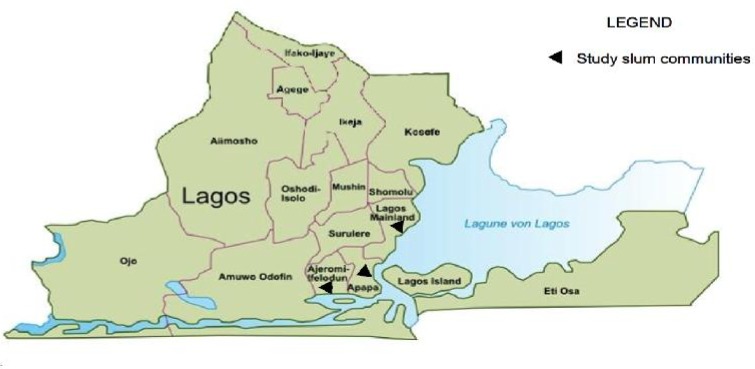
Map of Lagos state showing the sixteen Local Government Areas
Body mass index, blood pressure/glucose measurements
Body mass index (BMI) was calculated using the formula weight (Kg)/height (m2). Weight was measured with traditional weighing balance that was kept on a firm horizontal surface.
Height was measured with a calibrated pole to the nearest cm. Subjects were requested to stand upright without shoes with their back against the wall, heels together and eyes directed forward. Participant’s blood pressure levels were measured in mmHg in a sitting position and after a rest of five minutes using a pre-tested electronic OMRON machine (Omron Corporation, Tokyo, Japan), while random blood glucose was determined using the glucometer (On Call Plus, California, USA).
Data quality control and analysis
The survey made use of a semi-structured questionnaire, while the units of analysis for the survey were households. The questionnaire included details regarding demographic and socio-economic characteristics like participant’s self reported age, sex, educational status and occupational status. Health conditions were documented based on self-reported history of diabetes, and hypertension and family history for the conditions was also collected. In order to ensure quality control, credibility, reliability and precision of data collected, the research assistants were recruited among undergraduates with previous fieldwork experience. In addition, they had both written and spoken competence of the local and English languages, and good geographical knowledge of the three slums. To further enhance rapport, quality of information and report, interviews and discussions were conducted in English, Pidgin or local languages as was convenient for the participants. Completed questionnaires were checked on the spot and re-checked in the office for validation before data entry. Similarly, the electronic BP apparatus and glucometers were validated. The glucometer was calibrated every day with a standard provided along with the machine.
Data was entered in MS-Excel and was analyzed using the Statistical Package for Social Sciences (SPSS) Window version 16.0.
Results
All respondents were interviewed directly using personal interview method in order to avoid incomplete information. A sample of 2,434 respondents was recruited from Ijora Oloye (805), Ajegunle (814) and Makoko (815) communities. Table 1 shows the various languages used for the interview and the demographic characteristics of the respondents.
Table 1.
Language of interview and demographic characteristics of the respondents
| Language | Number (%) interviewed (Ijora Oloye | Number (%) interviewed (Ajegunle) | Number (%) interviewed (Makoko) | Total |
|---|---|---|---|---|
| English | 77 (9.6) | 277 (34) | 192 (23.6) | 546 |
| Yoruba | 650 (80.7) | 247 (30.3) | 562 (69) | 1,45 |
| Igbo | 1 (0.1) | 2 (0.2) | 7 (0.9) | 10 |
| Hausa | 2 (0.2) | 12 (1.5) | 1 (0.1) | 15 |
| Pidgin | 67 (8.3) | 234 (28.7) | 38 (4.7) | 339 |
| Others | 8 (1) | 42 (5.1) | 15 (1.8) | 65 |
| Sex | ||||
| Male | 348 (43.2) | 387(47.5) | 417 (51.2) | 1152 |
| Female | 457 (56.8) | 427(52.5) | 398 (48.8) | 1282 |
| Ethnic Group | ||||
| Yoruba | 746 (92.7) | 337(41.4) | 634 (77.8) | 1717 |
| Igbo | 17 (2.1) | 227(27.9) | 125 (15.3) | 369 |
| Hausa | 19 (2.4) | 8 (1.0) | 4 (0.5) | 31 |
| Others | 23(2.8) | 242 (29.8) | 52(6.4) | 317 |
| Educational status | ||||
| No formal schooling | 179 (22.2) | 86(10.6) | 107 (13.1) | 372 |
| Less than Primary school | 33(4.1) | 32(3.9) | 33 (4.0) | 98 |
| Primary school completed | 224 (27.8) | 194 (23.8) | 201 (24.7) | 619 |
| Secondary school completed | 276(34.3) | 417 (51.2) | 377(46.3) | 1070 |
| Post secondary school completed | 51(6.3) | 70(8.6) | 70(8.7) | 191 |
| Postgraduate degree | 6(0.7) | 9(1.1) | 11(1.3) | 26 |
| Quranic | 28(3.5) | 8(1.0) | 36 | |
| No response | 8(1.0) | 6(0.7) | 8(1.0) | 22 |
| Marital Status | ||||
| Single | 170(21.1) | 226(27.8) | 246 (30.2) | 642 |
| Currently Married | 559(69.4) | 518(63.6) | 496 (60.6) | 1573 |
| Separated | 6(0.7) | 13 (1.6) | 9(1.1) | 28 |
| Divorced | 2(0.2) | 9(1.1) | 10(1.2) | 21 |
| Widowed | 66(8.2) | 45(5.5) | 49(6.0) | 160 |
| Cohabitating | 1(0.1) | 3(0.4) | 4(0.5) | 8 |
| No response | 1(0.1) | 3(0.4) | 4 | |
| Religion | ||||
| Christianity | 77(9.6) | 564(69.3) | 526 (64.5) | 1167 |
| Islam | 715(88.8) | 245(30.1) | 276 (33.9) | 1236 |
| Traditional | 11(1.4) | 3 (0.4) | 11(1.3) | 25 |
| Others | 1(0.1) | 1(0.1) | 2 | |
| No response | 1(0.1) | 1(0.1) | 2(0.2) | 4 |
| Occupational Status | ||||
| Civil servant | 34(4.2) | 36(4.4) | 32 (3.9) | 102 |
| Private sector employee | 46 (5.7) | 67(8.2) | 85 (10.4) | 198 |
| Trading | 367 (45.6) | 362 (44.5) | 342(42.0) | 1071 |
| Farming | 14(1.7) | 5(0.6) | 2(0.1) | 21 |
| Artisan | 133(16.5) | 161(19.8) | 130(16.0) | 424 |
| Fisherman | 1(0.1) | 1(0.1) | 8(1.0) | 10 |
| Student | 81(10.1) | 54(6.6) | 74(9.1) | 209 |
| Housewife | 11(1.4) | 25(3.1) | 14(1.7) | 50 |
| retiree | 30(3.7) | 26(3.2) | 25(3.1) | 81 |
| Unemployed | 22(2.7) | 30(3.7) | 19(2.3) | 71 |
| Others | 63(7.8) | 41(5.0) | 83(10.2) | 186 |
| No response | 3(0.4) | 6(0.7) | 2(0.2) | 11 |
Only 312 (12.9%) out of the 2,434 admitted being previously diagnosed of hypertension (Table 2), while of the 312, just 29 (9.3%) were currently on treatment. Out of 2,434 respondents whose blood pressure measurements were taken, 650 (26.7%) had systolic pressure greater than 140 mmHg, 562 (23.1%) had diastolic pressure greater than 90mmHg, while 635 (26.7%) had their pulse rates greater than 100 beats per minute (Table 3). They were considered to be hypertensive as indicated by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7, 2004). Also, about 635 (26.7%) respondents had pulse rates greater than 100 beats per minute.
Table 2.
Respondents’ responses (%) to questions on history of raised blood pressure and diabetes
| High blood pressure | Ijora Oloye | Ajegunle | Makoko |
|---|---|---|---|
| Ever had blood pressure measured by a doctor or other health workers | 37.4 | 66.8 | 56.9 |
| Ever been told you have blood pressure | 9.2 | 11.1 | 18.3 |
| Have been told in the past 12 months. | 7.7 | 14.6 | 16.9 |
| Have ever taken medication for high blood pressure in the past two weeks | 8.1 | 6.4 | 13.7 |
| Advised to reduce salt intake | 4.9 | 4.8 | 15.7 |
| Advised to lose weight | 1.8 | 1.7 | 6.4 |
| Advised to stop smoking | 1.3 | 1.0 | 1.6 |
| Advised to start exercise | 2.1 | 3.9 | 9.6 |
| Currently taken herbal remedy. | 1.3 | 1.2 | 2.8 |
| Diabetes | |||
| Ever had raised blood sugar measured by doctor or other healthworkers | 7.2 | 24.8 | 20.8 |
| Ever been told you have raised blood sugar | 1.5 | 5.9 | 5.5 |
| Have been told in the past 12 months. | 0.9 | 3.8 | 5.5 |
| Currently taking insulin | 0.4 | 0.7 | 1.8 |
| Have ever taken medication for raised blood sugar in the past two weeks | 1.0 | 1.0 | 5.3 |
| Special diet | 1.6 | 1.4 | 5.3 |
| Advised to lose weight | 0.4 | 0.6 | 4.8 |
| Advised to stop smoking | 0.1 | 0.4 | 1.0 |
| Advised to start exercise | 0.7 | 1.4 | 5.6 |
| Taking traditional remedy for diabetes (raised sugar) | 0.2 | 0.6 | 1.3 |
Table 3.
Results of blood pressure, body mass index (BMI) and random blood sugar of the respondents
| Blood pressure | Frequency | Percentage |
|---|---|---|
| Systolic (mmHg) | ||
| ≤ 110 | 316 | 13.0 |
| 110-140 | 1468 | 60.3 |
| ≥ 140 | 650 | 26.7 |
| Total | 2,434 | 100 |
| Diastolic (mmHg) | ||
| ≤ 70 | 416 | 17.0 |
| 70-90 | 1456 | 59.9 |
| ≥ 90 | 562 | 23.1 |
| Total | 2,434 | 100 |
| Pulse (beats per minute) | ||
| ≤ 60 | 317 | 13.0 |
| 60-100 | 1482 | 60.3 |
| ≥ 100 | 635 | 26.7 |
| Body mass index (BMI) range | ||
| 18.5-24.9 (Normal) | 1088 | 44.7 |
| 25.0-29. (Over weight) | 881 | 36.2 |
| > 29.9 (Obese) | 465 | 19.1 |
| Random blood sugar (mg/dl) | ||
| < 201 (Normal) | 2354 | 96.6 |
| > 200 (Diabetic) | 80 | 3.4 |
Our data also showed that more males than females had systolic range greater than 140mmHg. The same could also be said about diastolic pressure and pulse rates as more men than women have theirs above the normal range. In addition, we observed that cases of high blood pressure were more common among respondents aged between 45 and54 years. The results of the respondents’ BMI showed that more than half (55.3%) of them were either overweight or obese (Table 3) and are at risk for diabetes due to their weights, however, about 3.3% had their sugar levels greater than 200mg/dl and thus were said to be diabetic. However, there were no significant differences between the prevalence of hypertension and high glucose in the three communities.
Discussion
A non communicable disease or NCD is a disease which is not contagious. Associated factors such as person’s lifestyle, genetics or environment are known to determine the likelihood of certain non communicable diseases. Of these three risk factors, 50% of all non communicable diseases are a result of poor lifestyle choices such as drug use, alcohol and tobacco use, diet, lack of exercise or stress management. NCDs such as hypertension, diabetes are recognized to exist in slums. This study was conducted in three informal settlements otherwise referred to as slums in Lagos state, southwestern Nigeria to identify the prevalence NCDs in the communities. It was observed that more than one quarter of the participants were suffering from hypertension and only half of this were diagnosed earlier, while a further few were on treatment. Therefore on screening, it had been possible to diagnose over three hundred more respondents. Thus high prevalence of undiagnosed hypertension points out to the fact that there is the need to devise comprehensive strategy for early identification and prompt treatment of hypertension to prevent its end-stage complications. It is also important to note that more than half of the respondents were either overweight or obese and are at risk for diabetes. In addition, what is most disturbing was the absence of regular follow up and treatment. Our findings are in agreement with similar studies (8–11). High hypertension prevalence and low levels of awareness and treatment as observed in this study point to a high cardiovascular disease burden in these slums.
This should be of great concern to health planners in Nigeria. Whereas interventions to improve the health of slum dwellers are not cutting-edge science. Effective interventions involve not only treating disease but also addressing the underlying social and living conditions of slums, while it has been shown that health promotion and primary prevention have the potential to prevent or delay the onset of chronic diseases and its risk factors (12–14). Looking at the growing urban population and almost one third contribution of slum population in cities, the high prevalence of hypertension should be a matter of concern to the local and national health authorities.
Conclusion
In Nigeria, the last national survey on NCD was carried out in 1999. As a result of changes in the peoples’ lifestyles due to adoption of western lifestyle, cases of NCDs in the country may be on the increase and these diseases may rapidly emerge as a public health challenge in both urban and rural areas. There is also paucity of programs to detect, manage and prevent these diseases in the country, and unless urgent and specific focus on preventing, treating and control of NCDs are targeted, the burden of the NCDs will be unbearable to the poor. This study had provided a background data on NCDs in slums and concerned organizations should focus and contribute to the prevention, control and reduction of NCDs burden and their risk factors. Their prevention requires an integrated action across a range of sectors at local and national levels. Federal and state Ministries of Health can develop priority based infrastructures and modules to prevent and control the NCDs at different stages. They can also develop local and national levels policies and plans of action for good planning and implementation. Advocacy campaigns such as awareness raising programs, street dramas, concerts can also be conducted for the general people on how to prevent NCDs, while involvement of public figures at the local and national media in these events can boost the impact. We therefore recommend that government should take the lead in developing a comprehensive promotional campaign to highlight the dangers of some lifestyles/behaviors such as drug abuse, smoking and excessive alcohol intake, particularly among the youth. Also continued funding by donors and governments is critical if sustainable strides are to be made in controlling these diseases and alleviating their effects on families and communities. In addition, further research is needed on the current burden of NCDs in Nigeria so as to generate a more current national database on these diseases, and help move evidence to policy and practice. It will also assist the government to put a priority setting on the control and treatment of NCDs in Nigeria.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgement
The authors appreciate the authorities of Ajeromi Ifelodun, Apapa and Mainland Local Government Areas for granting the team access to the study communities. We are also grateful to the community leaders and residents of Ajegunle, Ijora Oloye and Makoko communities for their cooperation while the study lasted. This study was funded by a seed grant awarded to OPA by the International Association of National Public Health Institutes (IANPHI). We declare that we have no competing interest with the preparation and publication of this manuscript.
References
- UN General Assembly, United Nations Millennium Declaration, Resolution Adop-ted by the General Assembly, 18 September 2000, A/RES/55/2. Available from: http://-www.refworld.org/-docid/3b00f4ea3.html[accessed 2 August 2013] [Google Scholar]
- UN-HABITAT (2003). The challenge of slums: global report on human settlements. London and Sterling, Earthscan Publications Ltd, pp.: 1–345. [Google Scholar]
- Daar AS, Singer PA, Persad DL, Pramming SK, Matthews DR, Beaglehole R, et al. (2007). Grand challenges in chronic non-communicable diseases. Nat, 450 (7169): 494–496. [DOI] [PubMed] [Google Scholar]
- Lee WR, Albert IK, Alon U, Mitermayer GR. (2007). Slum health: Diseases of neglected populations. BMC Int H & H R, 7(2). doi: 10.1186/1472-698X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Report (2002). Reducing Risks, Promoting Healthy Life: World Health Organization, Geneva, pp.: 1–250. [DOI] [PubMed] [Google Scholar]
- Boutayeb A, Boutayeb S. (2005). The burden of non communicable diseases in developing countries. Int J Equity Health, 4(2). doi: 10.1186/1475-9276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khuwaja AK, Qureshi R, Fatmi Z (2007). Non-communicable Diseases and Injuries: Action Needed in South Asia Too. PLoS Med, 4(1): e38. doi: 10.1371/journal.pmed.-0040038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Reform Foundation of Nigeria (HERFON) (2011). Diabetes to top cause of death in 2015. Available from http://www.-vanguardngr.com/-2011/10/diabetes-to-top-cause-of-deathin-2015. [Google Scholar]
- Chukwu O (2011). Heart disease, stroke cost Nigerian $800m yearly. Pmnews September 21 Available from http://www.pmnewsnigeria.com-/2011-/09/21/heart-diseasestroke-cost-nigeria-800. [Google Scholar]
- World Health Organization (2001). Hypertension study Group. Prevalence, awareness, treatment and control of hypertension among elderly in Bangladesh and India: a multicentre study. Bulletin WHO, 79 (6): 490–500. [PMC free article] [PubMed] [Google Scholar]
- Ramachandran A, Snehalatha C, Vijay V, King H (2002). Impact of poverty on the prevalence of diabetes and its complications in urban southern India. Diab Med, 19 (2):130–5. [DOI] [PubMed] [Google Scholar]
- Anand K, Shah B, Yadav K, Singh R, Mathur P, Paul E, Kapoor SK. (2007). Are the urban poor vulnerable to non-communicable diseases? A survey of risk factors for non-communicable diseases in urban slums of Faridabad. Nat Med J India, 20 (3):115–20. [PubMed] [Google Scholar]
- PawarAB, Bansal RK, Bharodiya Paresh Panchal Shaishav, Patel HB, Padariya PK, Patel GH (2010). Prevalence of hypertension among elderly women. Nat J Comm Med, 1 (1): 39–40. [Google Scholar]
- World Bank (2005). Dying Too Young: Addressing Premature Mortality and Ill Health Due to Non-Communicable Diseases in the Russian Federation. Washington DC. The World Bank. [Google Scholar]


