Abstract
Context
Routine electronic patient-reported outcome collection in patients with advanced disease could improve communication among patients, caregivers and providers and improve the timeliness of identifying problems and effectiveness of follow-up.
Objective
To develop a web-based tool to collect symptoms and need data and provide feedback to hospice and palliative care patients, caregivers and providers.
Methods
We developed Tell Us™ based on an existing pure web technology platform, the Medical Decision Logic, Inc. (“mdlogix”) Health Science Process Framework (HSPF™). The software development process included eliciting information on systems and needs and mapping care processes with three diverse hospices, and soliciting ideas for the software from clinicians and researchers. We developed a prototype software product, incorporated the hospices’ processes, assessment questions, and educational materials, and refined the product with feedback from other hospice and palliative care professionals.
Results
Tell Us includes modules for authoring and deploying clinical queries and completion schedules; for enrolling clinical sites and patients for patients and/or families to complete assigned assessments on a scheduled basis; and for providers to view patient-reported data. Tell Us provides customizable automated provider e-mail alerts based on patient responses (such as uncontrolled symptoms or need for medication refills) and provides educational materials targeted to patient needs.
Conclusions
This web-based toolset may be useful for improving communication between hospice and palliative care patients, caregivers, and providers and proactive patient management. Future research will involve integrating the software into care and evaluating its feasibility and use for data collection, patient education, and improving outcomes.
Keywords: Patient-reported outcomes, hospice, palliative care, flexible web technology, health science software architecture
Introduction
Delivering high-quality palliative and hospice care, particularly for terminally-ill patients in the home setting, has many challenges. Needs include monitoring patients frequently for worsening symptoms or signs of developing complications, providing timely information and educational materials to patients and providers, coordinating patient information efficiently among multiple providers and disciplines, and collecting data for quality measurement. One potential solution is routine collection of patient-reported outcomes (PROs), such as structured questionnaires to assess health-related quality of life, symptoms, or needs, to supplement clinical encounter and medical record data (1). Recently, there has been increased interest in including PROs in clinical care, as screening tools, for patient assessment, or for regular patient monitoring (1).
Recent research has found that routine collection of PRO data also may help in monitoring patients and identifying areas of concern in the hospice setting (2). Although a substantial research literature has addressed incorporating PRO information into oncology clinical practice, and studies have shown evidence for improved detection of problems and patient-provider communication when PROs are collected routinely in this setting (1), many challenges to routine use of PROs exist, particularly among persons with advanced illness, including efficient and effective methods for collecting key data from patients and presenting information to providers (3). Incorporating PROs requires demonstrating benefits to providers and payors and showing patients that the data they provide will add to their care (1).
Information technology may facilitate PRO assessment. In particular, with the incorporation of information technology, PROs can be collected independently from provider-patient encounters, allowing for more frequent monitoring; PRO data collection can be easily tailored to patient needs, and can be used across settings (4). These advantages are particularly relevant to hospice, where patient status may change rapidly and/or need regular monitoring. In both palliative and hospice care, PROs, such as symptom distress and quality of life, are often the main outcomes of interest. In addition, the involvement of multiple providers across settings makes use of an integrated information system particularly appealing in this population.
We therefore developed a web-based software product, Tell Us™, in partnership with palliative care and hospice providers, to collect routine data on patient symptoms and needs for care, and provide feedback to patients and providers. Tell Us includes modules to enroll clinical and research sites, as well as individual patients, and to author and deploy clinical assessments. Tell Us permits patients to enter data on a scheduled basis and providers to view cumulative patient data, as well as receive programmable automated e-mail notifications. In this article, we describe the development of Tell Us, including qualitative description of the needs and barriers identified by providers and administrators through the development process.
Methods
We developed Tell Us™ based on an existing pure web application platform, the Medical Decision Logic, Inc. (mdlogix™) Health Science Process Framework (HSPF™), architected using Health Level 7 (HL7) version 3 Reference Information Model (RIM) (Health Level Seven International, Ann Arbor, MI), Clinical Data Interchange Standards Consortium (CDISC, Austin, TX), and cancer Biomedical Informatics Grid (caBIG) (National Cancer Institute, Bethesda, MD) models and standards. The HL7 RIM is an abstract software object specification that provides a meta-model for the clinical care domain. Based on part on HL7, CDISC is a specification for clinical trials data designed to meet U.S. Food and Drug Administration (FDA) requirements. caBIG models are designed to support the design, implementation, and use of information technology for cancer research.
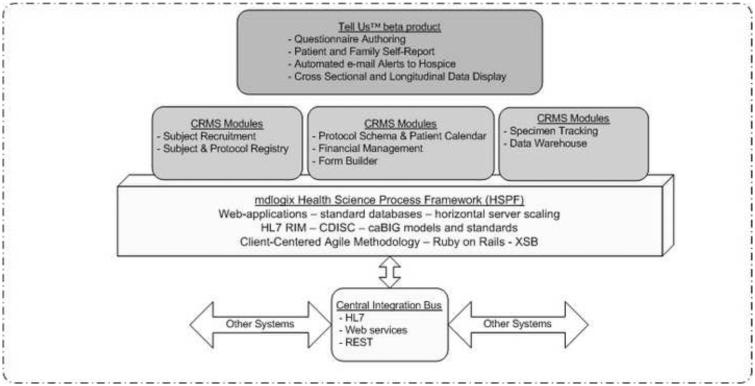
Building on all these conceptual models and standards, HSPF is a conceptual framework as well as a software architectural structure intended to support flexible end-user applications while maintaining commonalities and generalizability. The mdlogix Clinical Research Management System (CRMS™), based on HSPF (Fig. 1), is an enterprise-scale application that organizes scientific workflows, the specification and collection of data, and assurance of regulatory compliance. Use of HSPF as the web technology platform provides Tell Us with substantial functionality for administrative workflows, including the authoring of the self-report data items and the associated navigation and alert rules, the interfaces for patient and caregiver self-report, and the reporting and display of information. The system database is Microsoft SQL Server 2005 (Microsoft Corp., Redmond, WA), a standard relational database.
Fig. 1.
Relationship of Tell Us with the Clinical Research Management System (CRMS) and Health Science Process Framework (HSPF). This figure illustrates the high-level relationships between HSPF, CRMS, and Tell Us. HSPF is the web technology platform upon which the CRMS modules operate to support clinical research processes. Tell Us functions were derived from CRMS functions, thereby gaining the advantages inherent in the complex functionality provided by HSPF, including the ability to scale to very large numbers of users, and to readily link to and interoperate with other systems.
The purpose of the development process was to focus on how information technology could facilitate hospice processes, with a focus on routine collection of patient and caregiver-reported data and regular interaction with hospice patients and families, and potential application in palliative care practice as well. The underlying software development approach was based on an appreciation that busy and burdened hospice staff, patients, and caregivers would only use a system if they felt that it was actually useful in improving clinical care.
The development of Tell Us (Table 1) began with constructing user stories from hospice staff, with the goal of exploring specific situations where patient care problems need to be solved (5). Subsequent steps included soliciting ideas for the system; developing an algorithm for care processes; developing prototype software; prioritizing and incorporating tailored clinical queries and educational materials; and review of the software for face validity by outside clinicians and researchers. Three hospices participated in the initial development. Although operating in three different geographical areas (both suburban and rural), the hospices were already partnering to develop shared information technology goals and resources. A variety of employees of the hospices, including chief executive officers, administrators, information technology specialists, nurses, and a clinical therapist, participated in regular development meetings led by the software development team.
Table 1.
Tell Us Development Steps
|
For the user stories, the software development team conducted group development meetings with clinicians at different hospice sites to identify and map both local and common needs, and to formulate the approach. We also held development meetings with hospice administrators to understand their current and future business issues and needs, in particular increasing requirements from the Centers for Medicare and Medicaid Services (CMS) for more data and documentation on care processes and outcomes (6). We also elicited information on key barriers to implementing this type of system. We used feedback from these hospice groups throughout the software development process to evaluate iterations of screen designs and test operational prototype software. We reviewed currently used hospice assessment forms with the participating hospices and used these as the initial basis for the electronic assessments.
The initial assessment forms underwent multiple iterations of feedback and analysis from the staff of the initial three participating hospices, which also developed educational materials for each priority area. Finally, we developed an alternate version of the tool designed for palliative care outpatients, and obtained feedback on face validity on both the hospice and palliative care versions from a variety of hospice and palliative care providers. The project was approved by the Johns Hopkins Institutional Review Board.
Results
Key Needs Identified in Software Development Meetings
The key concepts from the software development meetings regarding how an interactive information technology intervention could be of most use in hospice care, including interaction with and gaps in their current information technology options (such as the electronic medical record) are listed in Table 2. Key functionality required by the user stories and developed for the software included interactive, scheduled (but flexible) data collection with patients and/or families; educational information for families; addressing multidisciplinary issues including caregiving and spiritual needs; and the practical need of ensuring adequate medications and supplies.
Table 2.
Key Concepts from Hospice Software Development Meetings: Electronic Collection of Patient-Reported Data
|
The key concepts from the development meetings on the potential value of the software (Table 3) included improved communication, such as the need for rapid e-mail notification of staff when there were patient needs that required attention; and support for proactive approaches to patient needs, such as routine monitoring of patient symptoms. Other key concepts included flexibility of the system (in particular, easy editing of questions and educational materials) to meet the different and evolving desires of individual programs and the needs of both hospice and palliative care settings; and the ability to generate reports and track data over time, for patients and families, for hospice and palliative care staff to use in clinical monitoring, and for administrators to use in quality assessment.
Table 3.
Key Aspects of Potential Value of Tell Us
|
Structure of the Software
The software is accessed though standard web browsers running in various operating system and hardware platforms. It provides:
A module to enroll and manage research and clinical sites;
- A module for providers to structure data collection and presentation of information, with:
- - Functions for the authoring and deployment of clinical assessments or questionnaires and educational materials, including Navigation (Skip) Logic;
- - Functions for authoring of Alert Logic (to trigger e-mail alerts) in the assessments;
- - Functions to manage enrollment of patients and caregivers;
A module for patients and family caregivers to use on a scheduled basis to enter data and comments;
Automated generation of e-mail alerts to staff; and
A module for staff and researchers to view patient data cross-sectionally and longitudinally.
The software is fully configurable by a provider or administrator to include any domains or questionnaires desired by an individual hospice or palliative care program, and can be modified for particular diagnoses or the individual patients.
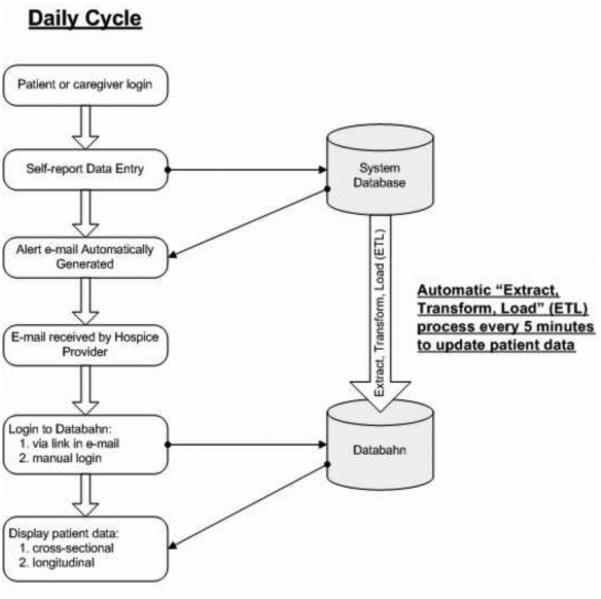
Figure 2 shows the flowchart for the process from login to provider data viewing. After patient or family login, the prototype Tell Us has an option for one or more questions per screen, structured to address key issues within each priority area. The system is configurable to reset for regular monitoring; the prototype resets at 18 hours with a new blank assessment, designed for daily respondent input. The system also is configurable for alerts to specified providers (e.g., a pain score greater than 6 or greater than a patient’s prespecified pain limit alerts the patient’s hospice nurse and/or the administrator). When an alert is triggered, the system shows a screen that says that an alert will be sent, giving the patient or caregiver an option to add a comment. The e-mail is then automatically sent, arriving at the recipient's e-mail address within a few seconds. The prototype Tell Us also provides patients and family caregivers with targeted educational materials linked to domains in the assessment. For example, if the patient or family responds that they are experiencing spiritual distress, one or more pages of educational information about spiritual issues and available support services can be provided.
Fig. 2.
Flowchart for process from patient login to provider viewing of summary patient data.
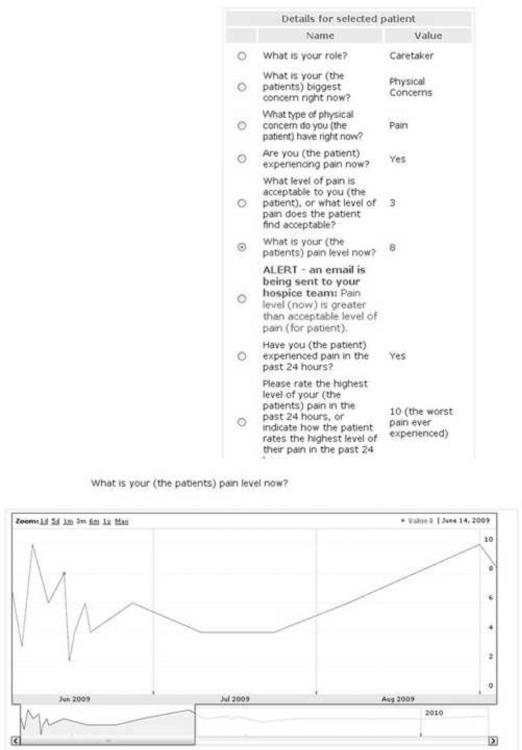
Clinicians and administrators interact with the system through the e-mail alerts and through summary information at the patient or designated population level. The alert e-mail provides information about the patient, the reason for the alert and patient or caregiver comments, and provides a link to Tell Us that provides one click to login. After login, the system provides a display of the patient’s immediate data; the clinician can click on any data item (e.g., pain level) to see a longitudinal, graphical display (Fig. 3). This prototype Data Dashboard also lets the clinician or administrator easily access his or her entire list of patients and examine patient or population data cross-sectionally (for any selected date) or longitudinally.
Fig. 3.
Example prototype Data Dashboard for a patient with an alert for pain and longitudinal display of pain scores.
Description of the Prototype
The hospices identified five priority areas for the prototype for data collection and education: pain, shortness of breath, anxiety, nausea, and medication supply. The provider view of a caregiver’s responses for pain, and the sequence of questions that the hospices selected for this issue, is shown in Fig. 2 (these data were entered by the investigators as part of the software testing process). The software is easily programmable by a provider or administrator to ask different questions for a particular patient or population. In this prototype version, the hospices first have the respondent enter whether the patient or caregiver is answering the questions, and then what the most important current concern is. Since this caregiver answered pain, a series of questions are then asked to screen for pain, ask what the patient’s pain goal is, and to determine the patient’s pain now and worst pain in the last 24 hours.
In this situation, the hospices programmed the software to send an e-mail alert whenever the patient’s current pain rating was higher than the patient’s pain goal; since the patient’s pain was 8/10, an alert was sent. The provider (in this case one of the investigators) then logged in to the system to see this screen, with the caregiver’s responses and a graph of the patient’s pain level over time. Given the patient’s current uncontrolled pain, after intervening, the provider might choose to program the software at this point to collect daily information on pain ratings and medication use.
Review by Providers for Face Validity and Feedback
Providers found that the prototype was easy to use and understand, when used from both the patient and provider perspective, and was modifiable to meet the needs of a different population (outpatient palliative care). Providers indicated that they would often prefer customization of questions (e.g., more emphasis on social services), or educational material (e.g., links to key websites) depending on the setting or population. The other major area of feedback was suggestions on simplifying and clarifying the functionality of the questions and responses. Another expressed provider need was how to better engage patients and families and provide more tangible benefits by providing more flexibility and data access to families, or meeting specific family needs such as caregiving schedules or interfamily communication.
During the development process and subsequent feedback, providers expressed needs for many other areas of functionality. One key issue was integration across palliative care and hospice programs. Such integration could potentially address the challenges of engaging patients with the system at the time of enrollment into hospice, when there are many other priorities and patients and families are often overwhelmed with transitions, symptoms, caregiving, and other burdens. Providers postulated that interaction of patients with the Tell Us system prior to hospice enrollment could not only provide potentially useful information and improve recognition of pain and other issues in oncology care, but could provide earlier notification of development of problematic issues and decline in functional status indicating that hospice would be appropriate and beneficial. Valuable information on the patients’ needs and trajectory also would be available to the hospice, potentially facilitating better quality of care during the critical early days of a hospice admission.
Discussion
We developed a web-based system for eliciting PRO data, in partnership with an information technology consortium among three community hospice programs and a variety of hospice and palliative care professionals in diverse settings. Use of the mdlogix HSPF, a web technology platform, designed to support scientific health processes, enabled the rapid implementation of a Tell Us prototype that was user-friendly but also had significant underlying complex functionality. The Tell Us prototype is a flexible system that allows for individualization of PRO questionnaires and other queries, skip logic to minimize respondent burden and tailor educational materials, and adaptation to and embedding in local hospice and palliative care practice. Tell Us also allows for inclusion of educational materials and automatic notification of providers when there are needs to be addressed or symptom severity is above a specified level, as well as a data mining interface for providers to monitor individual patient status over time as well as the overall status of any defined population.
Other electronic systems for patient data collection in the home and clinic setting have recently been developed and implemented for cancer and palliative care patients in clinical practice, research and clinical trials, and have some demonstrated effectiveness for improving patient outcomes. For clinical practice, a number of studies have evaluated electronic versions of the pain diary, a critical component for the careful monitoring of pain. These diaries have been evaluated in various cancer and noncancer populations, including randomized trials in children and patients unfamiliar with the use of computers, and have improved compliance and satisfaction, with increased accuracy in some studies (7,8). Electronic versions have the additional advantage of streamlining data collection, as well as the possibility of real-time monitoring of patients and response by clinical staff. However, since these diaries are not integrated into clinical practice, they may often not be used by clinicians and may be less beneficial to patients (9).
Several projects have implemented electronic collection of more general PRO data in clinical care and clinical trials. Implementation in one cancer center has been useful for clinical care, research, and quality measurement, as well as integration across sites (10). Ontario has implemented electronic data collection across the province; the ISAAC (Interactive Symptom Assessment and Collection Tool) allows patients to electronically enter severity scores for nine symptoms at home or at the cancer center. Results can be reviewed by the patients’ care team and clinicians are notified by email when symptoms are moderate to severe (11).
Electronic systems also can be helpful in other settings where collecting PRO data can improve the quality of information, such as adverse event reporting in oncology clinical trials (12). All of these systems work only to collect data, and are not designed to integrate into clinical care or provide feedback. A recent randomized trial in cancer patients with pain and depression found that scheduled collection of relevant PRO data through a telephone- or web-based system, with the frequency tailored to patient needs, together with nurse case management, was effective for improving outcomes for these symptoms (13). The interactive functionality and adaptability to different settings of Tell Us could potentially facilitate implementing this type of intervention in clinical practice.
Implementing PRO software in hospice and palliative care has both challenges and opportunities. Some ill patients and stressed caregivers could find using the system difficult; however, having an electronic monitoring system also could allow patients to report information on their own schedule when they feel most able to do so, rather than whenever the hospice nurse is able to come. One study implementing computerized PRO assessment in a variety of palliative care settings found that it was generally well-tolerated and could be completed by most patients (14). Electronic tools for the palliative care setting also can provide targeted questions on a prespecified schedule or tailored to patients’ identified needs (15). Monitoring electronic symptom information would be an additional task for health care professionals. However, if this task can be integrated into their workflow and both provide valuable information on their patients and help them organize and prioritize care, the overall benefits can exceed the burden, making care more targeted and more efficient and effective. Finally, although many hospices now have electronic medical records and increasing numbers of patients have internet access, solutions for those who do not will need to be developed.
In conclusion, in this developmental project, we constructed a prototype of a system to collect PRO data and integrate it into hospice and palliative care practice, incorporating input and feedback from providers and administrators. Although more research is needed on evaluating implementation of the system into actual practice and patients’ lives, initial feedback has shown the potential for the acceptance and usefulness of this type of software. High-quality, routinely collected PRO data could help improve the quality and efficiency of hospice and palliative care outside of the regular visit, as well as provide critical information for initiatives such as quality measurement and improved interdisciplinary care. Most importantly, organizations, providers, patients, and caregivers will not use a system well unless it clearly improves their work processes or the quality of their care, and further research is needed to ensure that the software can be feasibly incorporated into clinical practice and has value for all involved.
Acknowledgments
This project was funded by an SBIR (Small Business Innovation Research) Phase I contract from the National Cancer Institute to Medical Decision Logic, Inc. We also acknowledge the contributions of Hospice of the Chesapeake, Hospice of Washington County, and Coastal Hospice, as participants in the software development meetings developing the user stories and assessment tools.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors declare no conflicts of interest.
References
- 1.Snyder CF, Aaronson NK. Use of patient-reported outcomes in clinical practice. Lancet. 2009;374:369–370. doi: 10.1016/S0140-6736(09)61400-8. [DOI] [PubMed] [Google Scholar]
- 2.Schulman-Green D, Cherlin EJ, McCorkle R, et al. Benefits and challenges in use of a standardized symptom assessment instrument in hospice. J Palliat Med. 2010;13:155–159. doi: 10.1089/jpm.2009.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donaldson MS. Taking stock of health-related quality-of-life measurement in oncology practice in the United States. J Natl Cancer Inst Monogr. 2004;33:155–167. doi: 10.1093/jncimonographs/lgh017. [DOI] [PubMed] [Google Scholar]
- 4.Jones JB, Snyder CF, Wu AW. Issues in the design of Internet-based systems for collecting patient-reported outcomes. Qual Life Res. 2007;16:1407–1417. doi: 10.1007/s11136-007-9235-z. [DOI] [PubMed] [Google Scholar]
- 5.Hackos J, Redish J. User and task analysis for interface design. Wiley and Sons, Inc.; New York: 1998. [Google Scholar]
- 6.Centers for Medicare & Medicaid Services Hospice conditions of participation final rule. 2008 Available from: www.cms.hhs.gov/CFCsAndCoPs/05_Hospice.asp. [PubMed]
- 7.Gaertner J, Elsner F, Pollmann-Dahmen K, Radbruch L, Sabatowski R. Electronic pain diary: a randomized crossover study. J Pain Symptom Manage. 2004;28:259–267. doi: 10.1016/j.jpainsymman.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 8.Palermo TM, Valenzuela D, Stork PP. A randomized trial of electronic versus paper pain diaries in children: impact on compliance, accuracy, and acceptability. Pain. 2004;107:348–356. doi: 10.1016/j.pain.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Marceau LD, Link CL, Smith LD, Carolan SJ, Jamison RN. In-clinic use of electronic pain diaries: barriers of implementation among pain physicians. J Pain Symptom Manage. 2010;40:391–404. doi: 10.1016/j.jpainsymman.2009.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abernethy AP, Ahmad A, Zafar SY, et al. Electronic patient-reported data capture as a foundation of rapid learning cancer care. Med Care. 2010;48:S32–38. doi: 10.1097/MLR.0b013e3181db53a4. [DOI] [PubMed] [Google Scholar]
- 11.ancer Care Ontario (CCO) Interactive Symptom Assessment and Collection (ISAAC) tool. Available from: http://www.cancercare.on.ca/cms/One.aspx?portalId=1377&pageId=57699.
- 12.Basch E. The missing voice of patients in drug-safety reporting. N Engl J Med. 2010;362:865–869. doi: 10.1056/NEJMp0911494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kroenke K, Theobald D, Wu J, et al. Effect of telecare management on pain and depression in patients with cancer: a randomized trial. JAMA. 2010;304:163–171. doi: 10.1001/jama.2010.944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fyllingen EH, Oldervoll LM, Loge JH, et al. Computer-based assessment of symptoms and mobility in palliative care: feasibility and challenges. J Pain Symptom Manage. 2009;38:827–836. doi: 10.1016/j.jpainsymman.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 15.Chang CH, Boni-Saenz AA, Durazo-Arvizu RA, et al. A system for interactive assessment and management in palliative care. J Pain Symptom Manage. 2007;33:745–755. doi: 10.1016/j.jpainsymman.2006.09.018. [DOI] [PubMed] [Google Scholar]