Abstract
Background
The advancement in the healthcare systems, stringent interventions for infectious diseases and improved diet has significantly shifted the patterns of morbidities, and consequently hereditary and congenital anomalies (CA) and non-communicable diseases (NCDs) have emerged as the most common causes of morbidity and mortality. In Pakistan, there is no systematic health surveillance system to assess the impact of such diseases particularly on the young and adult populations.
Methods
In order to glean into the health and morbidity profile of Azad Jammu and Kashmir we have carried out an epidemiological study in Bhimber District in the north-east of Pakistan. A total of 1,731 female subjects of age 12-75 yr originating from Bhimber were recruited through a cross-sectional study.
Results
There were 74 cases (and 15 types) of CA with a prevalence estimate of 42.75/1,000. CA was significantly higher in subjects who were illiterate and married, speaking Pahari language and belonged to rural areas and nuclear families. Additionally, there were 104 cases (and 21 types) of NCDs (prevalence 60.08/1,000). NCDs were observed to have higher prevalence in subjects who were illiterate and married, speaking Punjabi language, and belonged to higher age groups and nuclear families.
Conclusion
This study explores the types and dynamics of morbidity across the major socio-demographic parameters of adult females of Bhimber and would be helpful in estimating the impact of morbidity in this population. A comprehensive country-wide study is the need of the time to identify specific risk factors associated with certain morbidity types and help prioritize areas for interventions.
Keywords: Congenital anomalies, Non-communicable disorders, Epidemiology, Azad Kashmir, Pakistan
Introduction
The advancement in the healthcare systems, stringent interventions for infectious diseases and improved diet have significantly shifted the pattern of morbidities in many parts of the world. Consequently, hereditary and congenital anomalies (CA) and non-communicable diseases (NCDs) which previously contributed only a minor fraction have emerged as the most common causes of morbidity and mortality (1). Health surveillance systems implemented in various countries monitor the impact of such morbidities in the society (2). CA are important to monitor in order to access the genetic load in the populations (3).
Of the estimated 57 million global deaths in 2008, 36 million (63%) were due to NCDs (2,4). Population growth and increased longevity are leading to a rapid increase in the total number of middle-aged and older adults with a corresponding increase in the number of deaths caused by NCDs. Epidemiological studies have identified a number of risk factors associated with certain NCDs. For instance, behavioral risk factors including tobacco use, physical inactivity, unhealthy diet and the harmful use of alcohol, are estimated to be responsible for about 80% of coronary heart disease and cerebrovascular disease (4).
In Pakistan, there is no systematic health surveillance registry for CA and NCDs, particularly among the young and adult population strata (5-6). Better understanding of the epidemiological correlates of morbidities is essential for the intervention programs, planning rational health care strategies, and for estimating any possible future increase due to any associated risk factor (3).
Azad Jammu and Kashmir (AJK) in the north-east of Pakistan is a relatively less developed territory. There is no study available which could show a comprehensive picture of CA and NCDs prevalent in AJK. We have therefore, conducted a study in order to generate base-line information on the morbidity profile of the adult women in Bhimber District of AJK.
Materials and Methods
District Bhimber
Bhimber District of Mirpur Division is the southernmost of the ten districts of AJK (Fig. 1). Tehsil Bhimber is the chief town of District Bhimber besides two other tehsils, Barnala and Samahni. More than 85% of its population lives in rural areas. District's population comprises 401 thousand individuals (2009 projections), with an annual growth rate of 2.6% (7). Bhimber has an agriculture/livestock based economy and majority of the rural population is connected with it. Bhimber District is a heterogeneous assemblage of various sub-populations. There are a number of ethnic/caste groups most prominent of which are Jatt, Rajput, Gujjar and Mirza. The primary languages are Punjabi and Pahari, and the literacy rate is 60% which is higher than the adjoining districts (8).
Fig. 1.
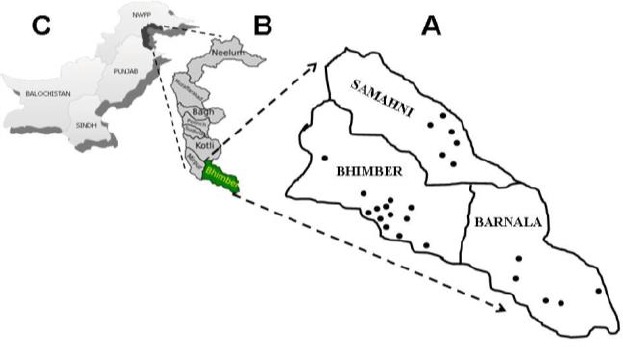
Map of District Bhimber (A) superimposed on map of Azad Jammu and Kashmir (B) and Pakistan (C). Sampling sites in three Tehsils namely Bhimber, Samahni and Barnala are depicted as dots
Methodology and sample ascertainment
Women comprise approximately 50% of Bhimber's population and play an active role in the agro-based economy of the District. To get an insight into the morbidity profile of young and adult women of Bhimber District a cross-sectional epidemiological study was conducted from February to October 2010. Only the female subjects belonging to Bhimber District and consenting to provide complete information were recruited in the study.
There were a total of 24 different sampling sites encompassing essentially the main towns/villages in the three tehsils of Bhimber District (Fig. 1A). There were 13, 5 and 6 sites from tehsils Bhimber, Barnala and Samahni, respectively.
Each recruited subject was interviewed and physically examined to access the morbidity status. Photographs depicting the phenotypic detail and relevant medical record were obtained from the subjects with any kind of morbidity. Multiple anomalies presented in a subject were accounted for separately. The anomalies were categorized in two broad groups: congenital/ hereditary anomalies (CA) and non-communicable diseases (NCDs). CA were mainly the developmental disorders present since birth while the NCDs had mostly late onset and non-genetic etiologies with no evidence of familial history. CA and NCDs was classified according to the standard medical databases (9-10).
Prevalence in married females was estimated in the total sample and was represented as per 1,000 subjects. Confidence intervals (CI) were calculated from the proportion of anomalies in the respective socio-demographic category. Descriptive summaries were generated and the departure from random distributions was evaluated with χ2 test and Fisher's exact test statistics with 0.05 significance level. Spearman's linear correlation was calculated to assess the relationships between some variables (11).
Results
Data were obtained from 1,731 female respondents belonging to District Bhimber and with an age range of 12-75 years (33.22±11.58 years). There were 764 (44.14%) subjects originating from tehsil Bhimber, 454 (26.23%) from Barnala, and 513 (29.63%) from Samahni (range of sample: 20-214; mean 72.13±51.95). The key findings for CA and NCDs have been separately described.
Congenital anomalies (CA)
A total of 74 CA were observed in the sample (Table 1). Hence, the prevalence of congenital anomalies in the female participants was 42.75/1,000 (CI of prevalence: 0.0332-0.0523). Limb anomalies had the highest proportion among the CA (n=51; prev.: 29.44/1,000; CI: 0.0215-0.0374), followed by the deaf-mute cases (n=7; prev.: 4.04/1,000; CI: 0.0011-0.0070) (Table 1). It is worthwhile to mention that 74 CA were witnessed in 67 subjects, hence, the prevalence of affected subjects was 38.64/1,000 (CI: 0.0296-0.0477).
Table 1.
Prevalence of congenital anomalies in recruited females of Bhimber, AJK
| Anomaly | No. | Percentile | Prevalence/1,000 | 95% CI | OMIM | ICD-10 |
|---|---|---|---|---|---|---|
| Limb defects (n=51) | 51 | 0.6892 | 29.46 | 0.6674-0.7110 | ||
| Club-thumb | 18 | 0.2432 | 10.40 | 0.2230-0.2634 | 113200 | Q68.1 |
| Brachydactyly | 12 | 0.1622 | 6.93 | 0.1448-0.1796 | 112500 | |
| Camptodactyly | 8 | 0.1081 | 4.62 | 0.0935-0.1227 | 114200 | |
| Clinodactyly | 7 | 0.0946 | 4.04 | 0.0808-0.1084 | 112700 | |
| Polydactyly | 4 | 0.0541 | 2.31 | 0.0434-0.0648 | 603596 | Q69.1 |
| Synpolydactyly | 1 | 0.0135 | 0.58 | 0.0081-0.0189 | 186000 | Q70.4 |
| Brachy-syndactyly | 1 | 0.0135 | 0.58 | 0.0081-0.0189 | ||
| Other anomalies (n=23) | 23 | 0.3108 | 13.29 | 0.2890-0.3326 | ||
| Deaf-mute | 7 | 0.0946 | 4.04 | 0.0808-0.1084 | 304400 | Q16 |
| Stuttering/mute | 3 | 0.0405 | 1.73 | 0.0312-0.0498 | 607485 | Q18 |
| Microtia | 3 | 0.0405 | 1.73 | 0.0312-0.0498 | 600674 | Q17.2 |
| Mental retardation | 3 | 0.0405 | 1.73 | 0.0312-0.0498 | 300243 | F03 |
| Squint eyes | 2 | 0.0270 | 1.16 | 0.0194-0.0346 | 231000 | Q10 |
| Orofacial defects | 2 | 0.0270 | 1.16 | 0.0194-0.0346 | ||
| Hand-feet allergy | 2 | 0.0270 | 1.16 | 0.0194-0.0346 | T78.4 | |
| Trembling body | 1 | 0.0135 | 0.58 | 0.0081-0.0189 | 245180 | |
| Total | 74 | 1.0000 | 42.75 | 1 |
OMIM= Online Mendelian Inheritance in Man; ICD-10= International Classification of Disease criteria
Cases of CA were categorized into 15 distinct types. Among the total hereditary anomalies and within the limb defects category, club-thumb had the highest representation (n=18), followed by brachydactyly (n=12), camptodactyly (n=8; 10.81%), and clinodactyly (n=7) (Table 1).
Majority of the CA had sporadic occurrences (n=63; 85.14%), while there were 11 cases with familial evidence of segregation (Table 2). Inheritance pattern in most of the familial cases was autosomal dominant (n=4). The detailed distributions of CA across different variables are provided in Table 2.
Table 2.
Hereditary nature and total affected family members in cases with congenital anomalies (n=74)
| Anomaly type | Cases | Hereditary nature | Familial cases | |||
|---|---|---|---|---|---|---|
| Sporadic | Familial | Total no. of affected in all families | Affected male/female ratio | |||
| Limb defects | 51 | 42 | 9 | 27 | 7:20 | |
| Club-thumb | 18 | 16 | 2 | 5 | 1:4 | |
| Brachydactyly | 12 | 7 | 5 | 14 | 3:11 | |
| Camptodactyly | 8 | 7 | 1 | 6 | 2:4 | |
| Clinodactyly | 7 | 6 | 1 | 2 | 1:1 | |
| Polydactyly | 4 | 4 | ||||
| Synpolydactyly | 1 | 1 | ||||
| Brachy-syndactyly | 1 | 1 | ||||
| Other anomalies | 23 | 21 | 2 | 9 | 5:4 | |
| Deaf-mute | 7 | 6 | 1 | 3 | 1:2 | |
| Stuttering/mute | 3 | 3 | ||||
| Microtia | 3 | 3 | ||||
| Mental retardation | 3 | 3 | ||||
| Squint eyes | 2 | 2 | ||||
| Orofacial defects | 2 | 2 | ||||
| Hand-feet allergy | 2 | 1 | 1 | 6 | 4:2 | |
| Trembling body | 1 | 1 | ||||
| Total | 74 | 63 | 11 | 36 | 12/24 | |
Congenital limb anomalies
The limb defects appeared as the largest representatives among the CA. There were seven distinct types of limb anomalies which were primarily affecting the autopod/digits. Majority of the limb defects were sporadic (n=42; 82.35%), while there were only nine malformations with an evidence of familial segregation. The involvement of upper limbs was more common compared to the lower limbs (36 vs. 15) (Table 3). Among the cases with affected upper limbs, majority had the involvement of both limbs (n=25; 69.44%). Among the unilateral cases of upper limbs, there was a preferential involvement of left hand (n=9; 81.81%). In the subjects with lower limbs involvement, the left foot was more frequently affected (n=7; 46.67%). Preaxial and postaxial defects were almost in equal proportions. Collectively, there were 31 cases with bilateral presentations and 20 had unilateral involvement. Of the 31 bilateral cases, 15 (48.39%) had symmetrical phenotypes in both limbs (Table 3).
Table 3.
Phenotypic variability in limb anomalies (n=51)
| Anomaly | No. | Laterality | Symmetry* | Upper limb | Lower limb | Axis involved | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unilateral | Bilateral | Sym. | Asym. | R | L | B | R | L | B | Pre-axial | Meso-axial | Post-axial | ||
| Club-thumb | 18 | 4 | 14 | 7 | 7 | 1 | 3 | 14 | 18 | |||||
| Brachydactyly | 12 | 6 | 6 | 1 | 5 | 1 | 2 | 4 | 5 | 12 | ||||
| Camptodactyly | 8 | 3 | 5 | 2 | 3 | 1 | 2 | 4 | 1 | 8 | ||||
| Clinodactyly | 7 | 1 | 6 | 5 | 1 | 1 | 6 | 7 | ||||||
| Polydactyly | 4 | 4 | 3 | 1 | 1 | 1 | 2 | |||||||
| Synpolydactyly | 1 | 1 | 1 | 1 | ||||||||||
| Brachy-syndactyly | 1 | 1 | 1 | 1 | ||||||||||
| Total | 51 | 20 | 31 | 15 | 16 | 2 | 9 | 25 | 2 | 7 | 6 | 19 | 2 | 30 |
* Symmetrical presentations among the bilateral cases. /Sym.=symmetrical; Asym.= asymmetrical; R=right, L=left, B=both.
Eleven limb anomalies demonstrated co-occurrence with certain other anomaly types. For instance, there were 12 individuals with brachydactyly, and five (41.67%) of them also exhibited certain other malformation (Table 4).
Table 4.
Co-occurrence of limb anomalies with other CA and/or NCDs in the same subject
| Limb anomaly | Total cases | Associated anomalies | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Club-thumb | Deaf | Limb amputation | Arthritis | Acroosteolysis | Stomach problem | Nail problem | Total associations | ||
| Club-thumb | 18 | 1 | 1 | 2 | |||||
| Brachydactyly | 12 | 2 | 1 | 1 | 1 | 5 | |||
| Camptodactyly | 8 | 1 | 1 | 1 | 3 | ||||
| Polydactyly | 4 | 1 | 1 | ||||||
| Total | 42 | 3 | 1 | 2 | 1 | 1 | 2 | 1 | 11 |
The prevalence of CA was quite variable across various socio-demographic attributes of Bhimber population. Among the three tehsils, Bhimber was observed to have the highest prevalence of CA as compared to Barnala and Samahni. The prevalence of CA was significantly higher among the subjects speaking Pahari language, belonging to rural areas and having no education (P<0.0001) (Table 6). The prevalence of CA was not associated with variables like parental consanguinity, linguistic groups, and family/house-hold type. With respect to ethnicity, the highest prevalence was observed in caste systems of Malik and Mirza (75.47/1,000 and 71.06/1,000, respectively) (data not shown).
Table 6.
Distribution of CA and NCDs across socio-demographic attributes of Bhimber population
| Congenital anomalies | Non-communicable diseases | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Demographic variable | Affected | Unaffected | Proportion of anomaly | Prevalence/1,000 | Affected | Unaffected | Proportion of anomaly | Prevalence/1,000 | |
| Tehsil | |||||||||
| Bhimber | 42 | 722 | 0.57 | 54.97 | 53 | 711 | 0.51 | 69.37 | |
| Barnala | 9 | 445 | 0.12 | 19.82 | 25 | 429 | 0.24 | 55.07 | |
| Samahni | 23 | 490 | 0.31 | 44.83 | 26 | 487 | 0.25 | 50.68 | |
| Total | 74 | 1657 | 1.00 | 42.75 | 104 | 1627 | 1.00 | 60.08 | |
| χ2=8.675, df. 2, P=0.0131, Sig. | χ2=2.172, df. 2, P=0.3375, NS | ||||||||
| Linguistic groups | |||||||||
| Punjabi | 50 | 1166 | 0.68 | 41.12 | 78 | 1138 | 0.75 | 64.14 | |
| Pahari | 24 | 491 | 0.32 | 46.60 | 26 | 489 | 0.25 | 50.49 | |
| Fisher's P=0.6047, NS | Fisher's P=0.3195; NS | ||||||||
| Origin/locality | |||||||||
| Rural | 64 | 180 | 0.86 | 262.30 | 93 | 151 | 0.89 | 381.15 | |
| Peri-Urban | 10 | 142 | 0.14 | 65.79 | 8 | 144 | 0.08 | 52.63 | |
| Urban | 0 | 1335 | 0.00 | 0.00 | 3 | 1332 | 0.03 | 2.25 | |
| χ2=349.0, df. 2, P<0.0001, Sig. | χ2=524.6, df. 2, P<0.0001, Sig. | ||||||||
| Education | |||||||||
| Illiterate | 40 | 488 | 0.54 | 75.76 | 65 | 463 | 0.63 | 123.11 | |
| Literate (all) | 34 | 1169 | 0.46 | 28.26 | 39 | 1164 | 0.38 | 32.42 | |
| Fisher's P<0.0001, Sig. | Fisher's P<0.0001, Sig. | ||||||||
Sig. =significant; NS=not significant
Non-communicable diseases (NCDs)
There were a total of 104 NCDs observed in the sample (prevalence 60.08/1,000). Majority of the NCDs were involving the skeleton (Table 5). There was highest representation of subjects with certain type of limb amputations (n=19; prev.: 10.98/1,000; CI: 0.0061-0.0159), followed by subjects with arthritis (n=15; prev.: 8.66/1,000; CI: 0.0043-0.0130), and acro-osteolysis (n=12; prev.: 6.92/1,000; CI: 0.0030-0.0108) (Table 5). Subjects with limb amputations included the cases with accidental loss of either upper or lower limb due to the encounter with crossfire, agriculture tools or domestic violence. The 104 anomalies were observed in 82 subjects, hence, the prevalence of affected subjects was 47.29/1,000 (CI: 0.0373-0.0573).
Table 5.
Prevalence of non-communicable disorders (n=104) in the female participants of Bhimber
| Non-communicable disorder | No. | Percentile | Prevalence/1,000 | 95% CI * | ICD-10 |
|---|---|---|---|---|---|
| Limb amputations (accidental) | 19 | 0.1827 | 10.98 | 0.1645-0.2009 | Y83.5 |
| Arthritis (generalized) | 15 | 0.1442 | 8.67 | 0.1277-0.1607 | M00 |
| Acro-osteolysis | 12 | 0.1154 | 6.93 | 0.1003-0.1305 | |
| Stomach problem | 6 | 0.0577 | 3.47 | 0.0467-0.0687 | K31.9 |
| Vitiligo | 6 | 0.0577 | 3.47 | 0.0467-0.0687 | L80 |
| Diabetes # | 6 | 0.0577 | 3.47 | 0.0467-0.0687 | E10 |
| High blood pressure # | 5 | 0.0481 | 2.89 | 0.0380-0.0582 | I11 |
| Tumors # | 5 | 0.0481 | 2.89 | 0.0380-0.0582 | D28 |
| Goiter # | 4 | 0.0385 | 2.31 | 0.0294-0.0476 | E04 |
| Asthma # | 4 | 0.0385 | 2.31 | 0.0294-0.0476 | J45 |
| Hepatitis | 4 | 0.0385 | 2.31 | 0.0294-0.0476 | B16 |
| Nail problems | 4 | 0.0385 | 2.31 | 0.0294-0.0476 | L60 |
| Skin allergy | 4 | 0.0385 | 2.31 | 0.0294-0.0476 | L23.6 |
| Eye loss (traumatic) | 2 | 0.0192 | 1.16 | 0.0127-0.0257 | S05 |
| Insane/mental ailment | 2 | 0.0192 | 1.16 | 0.0127-0.0257 | F99 |
| Hernia | 1 | 0.0096 | 0.58 | 0.0050-0.0142 | K40 |
| Stiff jaw | 1 | 0.0096 | 0.58 | 0.0050-0.0142 | K07.5 |
| Paralysis | 1 | 0.0096 | 0.58 | 0.0050-0.0142 | G83.9 |
| TB of spinal cord | 1 | 0.0096 | 0.58 | 0.0050-0.0142 | M49.0 |
| Body swelling/allergy | 1 | 0.0096 | 0.58 | 0.0050-0.0142 | T78.4 |
| Anemia | 1 | 0.0096 | 0.58 | 0.0050-0.0142 | D50 |
| Total | 104 | 1.0000 | 60.08 |
# late onset/ * calculated from percentile
Among the three tehsils, NCDs were witnessed to be highest in Bhimber as compared to Barnala and Samahni. With respect to ethnicity morbidity was quite variable and ranged from 34/1,000 to 193/1,000. The prevalence of NCDs was significantly higher among the subjects belonging to rural areas, speaking Punjabi language, and having no education (P<0.0001) (Table 6). An increasing trend in the prevalence of NCDs was witnessed with the increasing age of subject (Spearman correlation, r=0.9643; P=0.0028) (Fig. 2). The prevalence of NCDs was not associated with variables like linguistic groups, ethnicity, family/house-hold type, and parental consanguinity (data not shown).
Fig. 2.
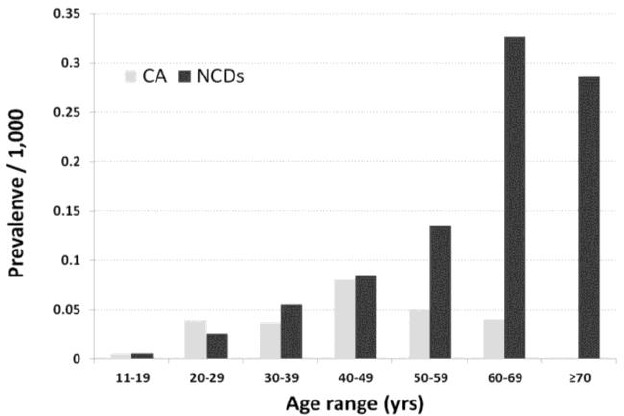
Prevalence of CA and NCDs plotted against the age range of subjects
Discussion
The prevalence of CA was estimated to be 42.75/1,000 in the female participants in the present study. Previously, an urban community based study in Pakistan showed that CA account for 40/1,000 live births (12). However, hospital based studies conducted by Yaqoob et al. (13), and Khaskheli et al. (14) established higher estimates (128/1,000, and 161/1,000, respectively). This variation in the prevalence rate could be due to the variability in the ascertainment methods, sampling and study design, and the underlying heterogeneity among the populations.
Limb defects appeared as the largest category among the CA (n=51). Interestingly, all of these limb defects were pertaining to the autopod/digits. Due to their non-lethal characteristics the limb defects are usually ignored in the surveillance and epidemiological studies. Particularly, partial cutaneous syndactyly, minor polydactyly, camptodactyly and clinodactyly do not get attention of the medical practitioner (15-16). The pattern of limb defects observed in the present study was quite distinct, and club thumb and brachydactyly were the most common anomalies. Other studies have shown that polydactyly was the most frequent type of CA in various Pakistani populations, which was only represented by four cases in the present sample (17). Furthermore, there is a published report on Kashmiri individual with thumb deficiency and toe webbing (18). No such phenotype was witnessed in this study.
There were a total of 104 NCDs observed in the recruited subjects. Curiously, accidental limb amputations appeared as the largest group. These included the subjects with loss of limb due to encounter with crossfire which is common due to the volatile political situation at the line-of-control between AJK and the Indian held Jammu and Kashmir (19). The second important cause witnessed was the accident with agriculture tools, used for mowing grass and cutting fodder for cattle. Thirdly, a rare reason for the loss of limb was observed to be the domestic violence. Acro-osteolysis, a rare limb anomaly with progressive loss of terminal digits, was witnessed to be the third most common NCDs in the recruited individuals. All of these cases were sporadic and hence, may have a common non-genic etiology.
All of the NCDs encountered in the present study had late-onset and no evidence of familial aggregation. However, we could not exclude the possibility for few of the cases of being hereditary in nature. It is of note that the NCDs of complex nature like cardio-vascular defects; diabetes, hypertension, etc. were not observed in significant proportions. It is quite likely that these disorders are more prevalent in urban areas which are not well-represented in the current study. Our data suggests a highly significant increase in the prevalence of NCDs with age. This situation is quite alarming due to the fact that several of the NCDs could be easily prevented by simple safety measures.
The present study has several limitations. For instance, it only focuses married females and does not present the spectrum of morbidities in the male population. Male subjects not only have a different pattern of malformations but also have higher estimates of morbidities. Hence, the true prevalence estimates of several diseases may be compromised while reporting only the female sample. Additionally, there are a number of early onset and lethal CA which may not appear in the adult population. Furthermore, the present study does not focus on the etiology of malformations. It would also be worthwhile to explore the causative factors of anomalies which are more prominent in Bhimber population. This however, would require an independent molecular genetics study to identify both genetic and non-genetic factors underlying CA and NCDs, respectively.
Conclusion
This study presents a preliminary overview of morbidity in the young and adult female population of Bhimber which is a representative Kashmiri population. A comprehensive country-wide epidemiological study is vital to quantify a national impact of morbidity in the adult population of Pakistan, and that data would promise better intervention and prudent management plans to combat diseases.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgments
We are grateful to the subjects for their volunteer participation in this study. Logistic support by the doctors and LHVs at District Hospital Bhimber is highly appreciated. The helpful comments of Profs. Afsar Mian, Mahmud Ahmad and SA Shami are highly acknowledged. This study was supported by HEC-Pakistan and PSF-Islamabad. The authors declare that there is no conflict of interest.
References
- WHO (2012). World Health Organization. Prevention and control of NCDs: Guidelines for primary health care in low-resource settings. Geneva: (http://www.who.int/nmh/publications/phc2012/en/index.html) [PubMed] [Google Scholar]
- EUROCAT (2012). http://www.eurocat-network.eu/ (accessed Dec. 2012)
- Baird PA, Anderson TW, Newcombe HB, Lowry RB (1988). Genetic disorders in children and young adults: a population study. Am J Hum Genet, 42 (5) :677–693. [PMC free article] [PubMed] [Google Scholar]
- WHO (2011). Cause-specific mortality: regional estimates for 2008 Geneva, 2011. (http://www.who.int/healthinfo/global_burden_disease/estimates_regional/en/index.html). [Google Scholar]
- PDHS (2008). Pakistan Demographic and Health Survey Report 2006–2007. National Institute of Population Studies, Islamabad.
- Shami SA, Schmitt LH, Bittles AH (1989). Consanguinity related prenatal and postnatal mortality of the populations of seven Pakistani Punjab cities. J Med Genet, 26 (4): 267–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PAP (2012). Population Association of Pakistan. http://www.pap.org.pk/index.htm (accessed Jun. 2012)
- GOA (2012). Government of Azad Jammu and Kashmir. http://www.ajk.gov.pk/index.php (accessed June. 2012)
- OMIM. Online Mendelian Inheritance in Man. http://www.ncbi.nlm.nih.gov/omim
- ICD (2012). International Classification of Disease. 2012. http://apps.who.int/classifications/icd10/browse/2010/en
- Garstman BB (2006). Basic Biostatistics. Sudbury, Massachusetts: Jones and Bartlett Publishers. [Google Scholar]
- Jehan I, McClure EM, Salat S, Rizvi S, Pasha O, Harris H, Moss N, Goldenberg RL (2007). Stillbirths in an urban community in Pakistan. Am J Obstet Gynecol, 197 (3): 257 e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaqoob M, Gustavson KH, Jalil F, Karlberg J, Iselius L (1993). Early child death in Lahore, Punjab. II Inbreeding. Acta PaediatScand,390 (Suppl.): 17–26. [DOI] [PubMed] [Google Scholar]
- Khaskheli M, BalochKhushk S.IA (2007). Pattern of fetal deaths at University Hospital of Sindh. J Ayub Med Coll Pak, 19 (2): 32–34. Malik S, Schott J, Ali SW, Oeffner F, Amin-ud-Din M, Ahmad W, Grzeschik K-H Koch MC (2005). Evidence for clinical and genetic heterogeneity of syndactyly type I: the phenotype of second and third toe syndactyly maps to chromosome 3p21.31. Eur J Hum Genet, 13 (12): 1268–1274. [Google Scholar]
- Malik S, Schott J, Ali SW, Oeffner F, Amin-ud-Din M, Ahmad W, Grzeschik K-H, Koch MC (2005).Syndactyly: phenotypes, genetics and current classification. Eur J Hum Genet, 20 (8): 817–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik S, Ullah S, Afzal M, Lal K, Haque S (2013). Clinical and descriptive genetic study of polydactyly: a Pakistani experience of 313 cases Clin Genet, doi: 10; 1111/cge.12217. [DOI] [PubMed] [Google Scholar]
- Malik S, Jabeen N (2011). Zygodactyly with thumb aplasia: an unusual variant in a male subject. J Col Phy Surg Pak, 21 (11): 710–712. [PubMed] [Google Scholar]
- de Jong K, Ford N, Kam Sv, Lokuge K, Fromm S, van Galen R, Reilley B, Kleber R (2008). Conflict in the Indian Kashmir Valley I: exposure to violence. Confl Health, 2: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]


