Abstract
A clinician’s effectiveness in treatment depends substantially on his or her attitude toward -- and understanding of -- the patient as a person endowed with self-awareness and the will to direct his or her own future. The assessment of personality in the therapeutic encounter is a crucial foundation for forming an effective working alliance with shared goals. Helping a person to reflect on their personality provides a mirror image of their strengths and weaknesses in adapting to life’s many challenges. The Temperament and Character Inventory (TCI) provides an effective way to describe personality thoroughly and to predict both the positive and negative aspects of health. Strengths and weaknesses in TCI personality traits allow strong predictions of individual differences of all aspects of well-being. Diverse therapeutic techniques, such as diet, exercise, mood self-regulation, meditation, or acts of kindness, influence health and personality development in ways that are largely indistinguishable from one another or from effective allopathic treatments. Hence the development of well-being appears to be the result of activating a synergistic set of mechanisms of well-being, which are expressed as fuller functioning, plasticity, and virtue in adapting to life’s challenges
Keywords: Treatment, health promotion, well-being, personality, person-centered therapy, personhood
What is person-centered therapeutics?
Person-centered therapeutics is the use of an interpersonal alliance and humanistic dialogue to orchestrate lifestyle change and other procedures as needed to heal illness, prevent disease and promote health [1]. Randomized controlled trials of person-centered treatments that promote well-being have lower drop-out, relapse and recurrence rates than other treatment approaches [2]. For therapeutics to be effectively person-centered, it must involve an awareness and respect for the whole person, whose health is certainly more than his or her symptoms of illness and past medical history [3]. The unique experiences, goals, and values of each person are assessed and treated in a person-centered therapeutic alliance, which optimally seeks to promote complete physical, mental, social, cultural and spiritual well-being. Person-centered therapeutics addresses the needs of the person (of the totality of the person’s health, both ill and positive aspects), and are engaged by the person (with clinicians extending themselves as full human beings), for the person (assisting the fulfillment of the person’s health aspirations and life project), and with the person (in a respectful and empowering relationship with the person who consults) [4]. Essentially, person-centered therapeutics is a practical application of the science of well-being to health care and health promotion [4–6].
A person is more than his or her symptoms
Unfortunately, most contemporary medical treatment is focused on relief of acute symptoms of illness rather than the promotion of health and well-being [7, 8]). As a result, contemporary medical practice is ineffective in the prevention and management of chronic diseases, which are common and complex in their etiology and treatment. Drop-out, relapse and recurrence rates are also high even for acute illness when treatments are not directed toward promotion of well-being [2]. Furthermore, impersonal approaches to therapeutics have failed to increase the average level of physical, emotional, or social well-being in the general population, despite substantial advances in technical capacities and health care expenditure [4, 6]. Treatments directed at acute symptoms of illness, rather than its causes, result in temporary relief, frequent relapse and recurrence, and no lasting improvement in public health [5].
The inadequacies of impersonal therapeutics have led to a widespread and growing interest in alternative therapies that are more personal and holistic. Evidence-based treatments used by adults for medical conditions are highly diverse, including physical exercise, diet, sleep hygiene, deep breathing exercises, muscular relaxation, mood self-regulation, guided imagery, meditation, and acts of kindness and gratitude [9–11]. Such self-regulatory and alternative treatments produce results that are often indistinguishable from more conventional allopathic interventions, suggesting that a common mechanism is being influenced by complementary pathways [12]. Success in self-regulation from repeated practice in one type of situation, such as exercises for monitoring and improving posture, monitoring and regulating mood, or monitoring and recording eating, consistently leads to greater self-control (i.e., willpower or free will) in other unpracticed situations, again suggesting a common underlying mechanism, or a synergistic set of mechanisms of well-being [13–15].
Person-centered care enhances treatment outcomes
The conditions that promote well-being and recovery from illness involve a set of common features of health that include hope, empathy and respect for one’s self and others [16]. These common characteristics of well-being emerge from a self-transcendent outlook on life with a sense of participation in the boundless unity of all things or inseparable connectedness with nature and other people [6, 17]. Self-transcendent outlooks and values are typical of healthy and creative people in all human cultures [18]. An outlook of separation predisposes a person to feelings of fear, alienation, and individual pride or shame, thereby predisposing to dissatisfaction with life and ill health.
Person-centered care promotes health by providing the experience of an outlook of unity in the therapeutic alliance, which can later be generalized beyond the alliance. An outlook of unity fosters well-being by activation of a synergistic spiral of increasing self-directedness, cooperativeness, and self-transcendence [5–7, 19, 20]. Only about 15 % of the variance in treatment outcome is attributable to specific techniques of different psychotherapeutic schools whereas about 85% of the variance in psychotherapy outcomes is explained by common factors shared by different approaches [21–23]. What is attributed to the strong placebo effects observed in most drug or psychotherapy trials is substantially determined by common psychosocial factors, which can be as large or larger than putatively specific treatments [22].
The common factors in all treatment include the patient’s characteristics, the therapist’s qualities of respect (i.e., prizing, unconditional positive regard, acceptance, trust), empathic understanding, and genuineness (i.e., realness, authenticity), and the quality of the therapeutic alliance between them (shared goals, emotional engagement and exchange) [24, 25]. These common factors are characteristic of all truly healthy interpersonal relationships [26], and are important for maintenance and recovery of all aspects of well-being, whether physical, mental, or spiritual [27–29]. Claims of the evidence for the specificity of particular techniques for specific disorders are rarely justified because of inadequate assessment of these common factors [21]. Nevertheless, in research under the auspices of the Anthropedia Foundation, we have found it is essential to go beyond a simple common factor approach to assess and understand the mechanisms by which a person changes as part of a dynamic multi-step process involving a spiral of synergistic changes in functioning, plasticity and virtue [5, 30–33].
In other words, a clinician’s effectiveness in treatment depends substantially on his or her attitude toward -- and understanding of -- the patient. The interpersonal attitudes of respect, genuineness and empathic understanding are crucial for the development of well-being [5, 34]. When physicians rely only on symptom-based diagnosis and treat patients without respectful exchange in dialogue, there are usually high rates of drop-out and non-compliance with treatment prescriptions, as well as high rates of burn-out in the physician and stigma in the patient [5]. Accordingly, effective clinical practice depends on tools that facilitate non-stigmatizing personality assessment, rapid facilitation of a therapeutic alliance and guided development of self-awareness for people to learn how to live well.
In this article, we describe the example of personality assessment as it is used in the Know Yourself program about well-being promoted by the Anthropedia Foundation as an illustration of illustrate the active roles of both patients and clinicians in person-centered therapeutics. Today, physicians will often describe a person’s illness only in terms of a checklist of symptoms and perhaps the course of their past medical history without integration of additional information about personal, social, cultural, and spiritual history. Even with a thorough symptom-based diagnosis, most physicians do not really appreciate who the person is, or, if they do know intuitively, they have still not integrated their appreciation of the patient with an understanding of the causes of the illnesses or the unique set of strengths that will allow the person to recover their health.
Individual differences in a person’s outlook on life strongly determine their capacity to work, love, and serve others with satisfaction and health. Personality assessment helps a clinician to know who the person is, stimulates the patient to reflect on their strengths and weaknesses in regulating their emotions in accord with their goals and values. Instead of merely generating a pejorative categorical label of personality traits and disorders [35], both the clinician and patient need to understand how a patient’s personality profile is organized and may contribute to his or her health and illness.
So, what is personality?
If a person is more than their symptoms, then clinicians need a way to describe the person as a being that learns and adapts to situations in life. Personality is defined as the organization within the individual of the psychobiological systems by which a person shapes and adapts to ever-changing internal and external influences [36,37]. The Temperament and Character Inventory (TCI) is a tool for personality assessment that was developed to provide a comprehensive psychobiological model of personality as it develops within individuals [37]. It deconstructs personality into seven dimensions that vary widely in the general population, rather than focusing only on pathology or abnormal traits [38]. Nevertheless, it was designed to be equally applicable to clinical populations without being stigmatizing or pathologizing.
The TCI is based on a psychobiological model of complex interactions among genetic, psychological, social, cultural, and spiritual variables, rather than assuming that personality can be decomposed into independent dimensions [39,40]. Prospective studies of personality and the experience of clinicians consistently show that the same clinical disorder may have many different pathways that lead to it, a characteristic of open systems with nonlinear development called “equifinality” [19,41]. Likewise, experienced clinicians know the same set of antecedent traits may develop in many different ways that lead to divergent outcomes, another hallmark of non-linear development called “multifinality” [20]. Unfortunately most modern inventories for measuring personality are linear models derived by factor analytic methods, which are actually invalid for non-linear systems like personality. Without claiming that it is the only way to understand personality rigorously, we use the TCI, because it is a well-validated system for assessment, recognizes the non-linear nature of personality development that is crucial for treatment planning and has been shown to be useful and practical in clinical practice for treatment across the full range of personality and psychopathology [6,19,42,43].
Understanding the Temperament and Character Inventory (TCI)
The TCI provides a quick, reliable, and clinically meaningful description of the person you are encountering in a respectful manner that describes without judging or blaming. We, the authors, usually administer the TCI on the first or second visit, often while the patient is waiting to be seen. The test has 240 questions, either true-false or on a 5-point Likert scale and can be completed by the patient in 35 to 45 minutes. The patient is asked to complete his responses in one sitting, if possible. The test is usually administered and scored online from home or the office, either alone or as part of a psychoeducational course to promote well-being [17]. Information about administration is available online (http://anthropedia.org).
The automated scoring of the patient’s self-reported profile can then be reviewed and discussed with the patient. The review and discussion of the patient’s personality profile not only informs the clinician but also allows the patient to reflect on how s/he has described him- or herself. This discussion gives the clinician and his/her patient a shared language to understand who s/he is and what are his or her strengths and vulnerabilities. Such discussion allows the patient to see that the clinician understands and can predict things about him or her even before they have revealed it to the clinician explicitly. A recent review of the many predictions that can be made from TCI profiles is provided elsewhere [7]. For example, people who are easily bored and impulsive are more likely to have experimented with drugs than others. Discussion of the patient’s needs and vulnerabilities in a mutually respectful dialogue rapidly builds respect, rapport, and a therapeutic alliance with shared treatment goals. The information about the individual’s personality invites him or her to engage in further reflection, which sometimes activates rapid and spontaneous recovery.
Hopeful dialogue also provides a greater awareness of his or her path of inner transformation as the patient and clinician map out the ways in which s/he needs to develop in order to lessen the impact of what has been troubling. Discussion of the person’s strengths as well as vulnerabilities assists in the recognition of the tools and resources available for achieving increased life satisfaction, happiness and overall well-being. The resources available to patients may include medications the clinician will prescribe as well as other exercises, activities, and meditations that will help them understand themselves and their situations more fully.
Distinguishing Temperament and Character
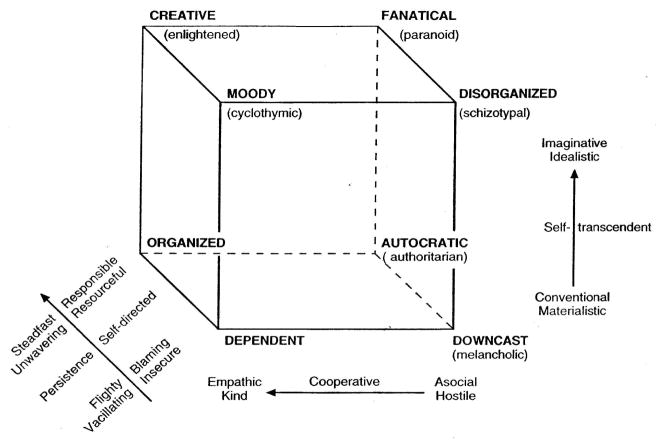
Temperament refers to individual differences in the strength of drives underlying basic emotions, such as fear, anger, disgust, and surprise, which are moderately stable throughout a person’s life. In contrast, character refers to individual differences in a person’s goals and values that develop in a step-like manner as a person matures in insight through experience over his or her lifespan [44, 45]. The four dimensions of temperament and three dimensions of character measured by the TCI are summarized in Figure 1.
Figure 1.
Psychobiological Model of Temperament and Character (Reproduced with permission of Washington University Center for Well-Being)
Initially temperament was described in terms of three heritable dimensions – Harm Avoidance, Novelty Seeking, and Reward Dependence, as measured by the Tridimensional Personality Questionnaire (TPQ) [46, 47]. Later work identified a fourth heritable temperament dimension called Persistence [48, 49]. These four temperaments correspond to people with anxiety proneness (i.e., high Harm Avoidance, as in DSM Cluster C), impulsivity and anger proneness (i.e., high Novelty Seeking, as in DSM Cluster B), social detachment (i.e., low Reward Dependence as in DSM Cluster A), and perseverance or obsessionality (i.e., high Persistence, as in anankastic personalities) [50, 51]. These four clusters have been called the “four A’s”: asthenic, antisocial, asocial, and anankastic respectfully [52]. Configurations of these dimensions provide a reliable way to describe a person’s emotional style or to subtype personality disorders [43, 53].
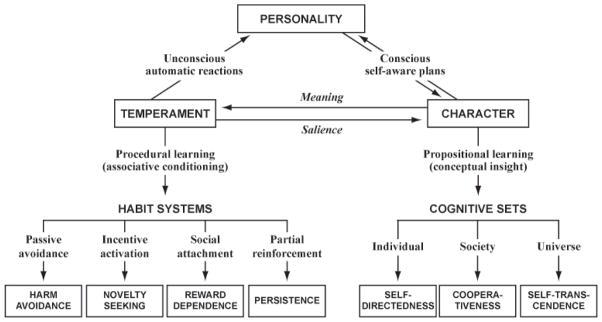
Groups of people with different configurations of temperament are depicted in Figure 2. Each of these temperament configurations differs on average as a group in their level of maturity [54]. For example, individuals who are high in Harm Avoidance (H) and Novelty Seeking (N), but low in Reward Dependence (r), are described as having an explosive or borderline temperament profile (NHr). They are much more likely to be immature than those with most other configurations, but there are a substantial number of people with an explosive Temperament who are nevertheless mature and responsible (that is, who do not have a personality disorder).
Figure 2.
The TCI Temperament Cube: Descriptors of different configurations of TCI Harm Avoidance, Novelty Seeking, and Reward Dependence (reproduced with permission of the Washington University Center for Well-Being)
The identification of configurations is useful because they are moderately stable in the absence of major trauma or behavioral conditioning. Identifying a configuration also allows a clinician to consider the interactions that are likely to occur among the dimensions of a person and thereby influence the path they take in developing their life narrative [20, 55].
Temperament alone is not adequate to determine whether an individual person does or does not have a personality disorder. Someone can be healthy and mature regardless of their temperament profile, even though groups of temperament profiles differ in maturity on average, as shown in Table 1. Therefore, the TCI character dimensions were developed to measure additional aspects of personality that allow people to regulate their emotional impulses and conflicts in such a way that they are mature and healthy regardless of the temperament.
Table 1.
The probability of being immature in Character as a function of the configuration of TCI Temperament traits (reproduced with permission of the Washington University Center for Well-Being)
| Temperament Type | Configuration Code (a) | Number of Subjects | % Immature (b) |
|---|---|---|---|
| Explosive | NHr | 39 | 72 |
| Methodical | nHr | 44 | 59 |
| Adventurous | Nhr | 25 | 48 |
| Sensitive | NHR | 30 | 40 |
| Average | --- | 15 | 33 |
| Avoidant | nHR | 30 | 17 |
| Independent | Nhr | 31 | 16 |
| Passionate | NhR | 50 | 12 |
| Staid | nhR | 36 | 6 |
| (Total) | (300) | (33) |
Code indicates Novelty Seeking is high (N) or low (n), Harm Avoidance is high (H) or low (h), and Reward Dependence is high (R) or low (r).
Immaturity is based on being in the bottom third of general population in sum of Self-Directedness and Cooperativeness, a strong measure of personality disorder or immaturity [37]
In order to understand the person you are encountering, it is essential to assess both his temperament and his character. The temperament traits are biases in emotional responses that are fully developed early in life and moderately stable thereafter. On the other hand, character involves higher cognitive processes that develop in a stepwise manner over the life course to enable a person to regulate emotions, achieve certain goals, and express particular values. Initially, it was thought that character was less heritable than temperament, but empirical studies have shown that both are moderately heritable [56]. The key difference is the difference in the pattern of their development and underlying type of learning involved. The procedural learning of habits and skills influences the conditioning of temperament, so temperament remains stable throughout life, except in response to behavioral conditioning that is unique for each individual. Propositional or semantic learning of goals and values influences the development of character, so character profiles are pulled toward the norm favored in a person’s culture. Likewise, parental role-models and attachments have a greater influence on character than on temperament, in excess of the effects attributable to genetic inheritance. Both temperament and character interact with one another in self-aware consciousness, so that a person can maintain a personal sense of continuity throughout many episodes of experience as his or her life history unfolds.
Describing temperaments and their interactions
Temperament can be assessed in terms of the four TCI dimensions previously mentioned. The four TCI temperaments correspond roughly to the ancient Greek temperaments as described by Hippocrates and others: Harm Avoidance and melancholic humor, Novelty Seeking and choleric humor, Reward Dependence and sanguine humor, and Persistence and phlegmatic humor. However, the ancient Greeks thought of the humors as present or absent, whereas the TCI dimensions are quantitative with roughly bell-shaped distributions with most people near average and only the top third being noticeably “high” and the bottom third being noticeably “low”.
The TCI temperaments are described in Table 2, which shows that each trait is manifest in slightly different ways in different situations. Shyness in social situations and fearfulness in risky or dangerous situations both are indicators of anxiety-proneness or high TCI Harm Avoidance. A situation necessarily depends on both the person’s outlook and the external circumstances themselves. For example, a person is described as high in Harm Avoidance if s/he is easily fatigued, fearful, shy, pessimistic, and inhibited. On the other hand, a person is described as low in Harm Avoidance if s/he is vigorous, risk-taking, outgoing, optimistic, and uninhibited.
Table 2.
Description of people who are high and low on the four TCI Temperament Dimensions (reproduced with permission of the Washington University Center for Well-Being)*
| Temperament Dimension | Descriptors of High Variant | Descriptors of Low Variant |
|---|---|---|
| Harm Avoidance | Pessimistic Fearful Shy Fatigable |
Optimistic Daring Outgoing Energetic |
| Novelty Seeking | Exploratory Impulsive Extravagant Irritable |
Reserved Rigid Frugal Stoical |
| Reward Dependence | Sentimental Sociable Warm Approval-seeking |
Practical Aloof Detached Self-sufficient |
| Persistence | Industrious Determined Ambitious Perfectionistic |
Lazy Spoiled Underachieving Irresolute |
Each descriptor is measured by a specific TCI subscale.
However, the level of Harm Avoidance varies moderately between situations. For example, some people who are shy are not easily fatigued and some people who are shy meeting strangers are risk-takers when driving an automobile. The components of Harm Avoidance that are manifest in different situations are moderately correlated, so it is useful for general discussions to consider all these as part of a higher order trait that is moderately heritable and moderately stable across time and situations. Likewise, Novelty Seeking, Reward Dependence, and Persistence are also moderately heritable and stable dimensions of temperament. Each extreme of temperament has both advantages and disadvantages, so there is no “good” or “bad” temperament, just different emotional styles of adaptation. The interactions between each pair of temperaments are described in detail elsewhere [46].
Describing character traits and their interactions
Assessment of the three TCI dimensions of character provides a description of a person’s goals and values (Table 3). Each of the character traits is comprised of components that are expressed in different situations. The character dimensions also correspond to key functions of a person’s mental self-government. As a result, high character development is socially desirable for each of the TCI dimensions, although the development of high Self-Transcendence may seem countercultural in materialistic Western societies. Despite the Western ambivalence about spirituality and self-transcendence, available data strongly indicates that in fact high Self-Transcendence is extremely important for emotional well-being, especially when a person faces suffering or death [7, 57–59].
Table 3.
Description of people who are high or low on the three TCI Character Dimensions (reproduced with permission of the Washington University Center for Well-Being)*
| Character Dimension | Descriptor of High Variant | Descriptor of Low Variant |
|---|---|---|
| Self-Directedness | Responsible Purposeful Resourceful Self-accepting Self-disciplined |
Blaming Aimless Inept Pretentious Self-defeating |
| Cooperativeness | Tolerant Empathic Helpful Compassionate Principled |
Prejudiced Insensitive Hostile Revengeful Opportunistic |
| Self-Transcendence | Self-forgetful (light) Holistic (transpersonal) Spiritual |
Self-striving (controlling) Individualistic (defensive) Secular (non-religious) |
Self-Directedness provides a useful clinical measure of the executive branch of a person’s system of mental self-government. A self-directed person is responsible, purposeful, and resourceful in dealing with life’s challenges. As a result, a person’s Self-Directedness is an important indicator of reality testing, maturity, and vulnerability to mood disturbance. Self-Directedness is high in people who are mature and happy, whereas it is low in people with personality disorders and those vulnerable to psychoses and mood disorders.
Cooperativeness provides a clinical measure of a person’s ability to get along well with others. Cooperativeness represents the legislative branch of self-government, which makes the rules that allow us to get along with others. A cooperative person is tolerant, empathic, helpful, compassionate, and principled. In contrast, an uncooperative person is prejudiced, egocentric, hostile, revengeful, and unfair.
The third branch of mental self-government is the judicial branch. Self-Transcendence is the ability to know when rules apply to a particular situation. Self-transcendent people are described as self-forgetful (intuitive and light), transpersonal (holistic and joyful), and spiritual in perspective, whereas those who are low in Self-Transcendence are self-striving (controlling), individualistic (defensive), and secular (materialistic and non-religious).
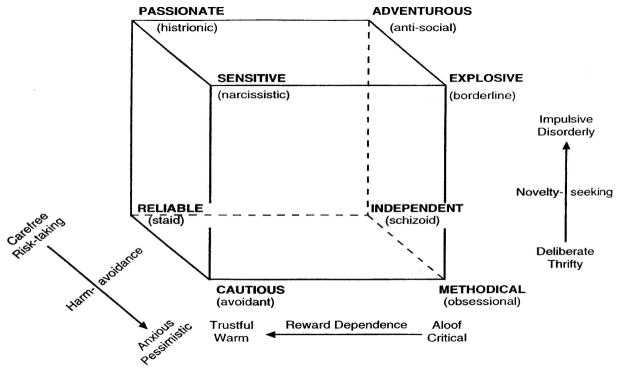
Each of the three branches of mental self-government is essential for well-being. Having one component excessively advanced, and not held “with checks and balances” by the other two branches, can lead to particular pathologies. The interactions among the three branches of self-government are depicted in Figure 3.
Figure 3.
The Character Cube (reproduced with permission of the Washington University Center for Well-Being)
For example, excessive imagination associated with high Self-Transcendence often leads to perceptual aberrations and vulnerability to over-valued ideas or psychosis if there is not the solid reality testing associated with high Self-Directedness [60, 61]. Such magical thinking is seen in the disorganized (schizotypal) and moody (cyclothymic) character configurations in Figure 3. Unless both Self-directedness and Self-transcendence are high, a person is likely to have an attitude of separateness, which leads to superstitious or magical thinking without the realistic and selfless qualities of truly self-transcendent attitudes like altruism and benevolence to others.
The creative and organized character configurations consistently have the highest levels of well-being, whereas the downcast (melancholic) and disorganized (schizotypal) configurations consistently have the lowest levels of well-being [6, 19]. Downcast people are low in all three traits of character, so they often say “life is hard, people are mean, and then you just die!” Not surprisingly, they are unhappy, alienated, and physically unhealthy and fearful of death with high rates of mental and physical disorders [19]. In contrast, creative people are high in all three traits of character, so they often regard life as filled with opportunities to learn from their mistakes and to serve others, enjoy helping others with tolerance and compassion, and seek to grow in awareness of the inexhaustible mysteries of life and what is beyond human existence.
Nevertheless, a creative outlook on life is often associated with challenges and disappointments, as exemplified in the lives of positive philosophers like Lamartine or Gandhi [6]. Failure and suffering are often the stimulus for development of greater well-being by means of reflection and contemplation on the causes of our ill-being. Creative characters are self-transcendent enough to accept the human condition with its unavoidable disappointments, suffering, and death. Such humble acceptance of one’s limitations promotes well-being by helping people to let go of complaining and selfish striving so that a person can be more grateful and enjoy the wonders and mysteries of life.
The health, happiness, and wisdom of creative people comes from their actually living the three practices of well-being: Working in the service of others (i.e., acts of unconditional kindness), letting go (i.e., no fighting or worrying), and growing in awareness (i.e., seeking to understand the mysteries and wonders of life and what is beyond human existence) [6, 17]. As a result of their outlook and practices, people with a creative character configuration have integrity, resilience, and are well satisfied with their life despite all its challenges, difficulties, and disappointments. As a result, a creative character is strongly predictive of all aspects of well-being, including health, happiness, and virtue in prospective studies of both mental and physical health [7, 20, 55].
Activating the motor of well-being
The methods for promoting healthy character development are described more fully elsewhere [7]. The promotion of well-being must begin by a person recognizing what brings them health and lasting satisfaction. Dialogue about a person’s self-description of their personality traits allows reflection and contemplation of any discrepancy between how to live well and how a person is currently living.
Humanistic dialogue is the foundation for developing shared goals in a therapeutic alliance that will lead to well-being [1, 8, 62]. Dialogue about the way the components of personality interact to produce illness or health is what makes the therapeutic encounter truly person-centered and often initiates a process of rapid spontaneous change [8]. In our experience, reflection on the relations between personality and health often (but not always) leads spontaneous improvement. In some, but not all people, an increase in self-awareness automatically potentiates synergy among a person’s way of functioning, plasticity, and virtue, as described elsewhere in this issue [33]. More work is needed to recognize what blocks this synergy in other people.
Everyone has a spontaneous need to be self-actualizing, that is, to become a fully functioning human being [6, 34, 62]. However, different people may be receptive and responsive to different treatments depending on their personality and circumstances. The evidence-based treatments used by adults for medical conditions are highly diverse, including physical, mental, and spiritual interventions [9–11]. Such alternative treatments produce results that are often indistinguishable from one another and from more conventional allopathic interventions when they are effective, suggesting the operation of a synergistic set of mechanisms, or the operation of a common mechanism that is being influenced by complementary pathways.
Nevertheless, there are also often obstacles to change so a person must learn many things in order to live well [17]. What a person needs and wants to learn must be tailored skillfully to their individual needs using person-centered therapeutics [4, 7]. As a result, effective person-centered therapeutics is based on describing and understanding the personalities of the people involved in any therapeutic encounter as soon as possible while preserving a person’s life.
Person-centered care promotes self-awareness with a feeling of connectedness with an interpersonal outlook of unity. In turn, an outlook of unity promotes attitudes of hope, empathy, and respect. Such shifts in outlook facilitate the development of fuller functioning, plasticity and virtue, which are a synergistic triad of self-actualizing mechanisms that consistently promote well-being.
Available evidence indicates that plasticity, functioning and virtue are irreducible aspects of the motor of well-being, which means that all three must be addressed for effective clinical therapeutics. This observation has strong implications for the organization and goals of clinical practice. Most contemporary medical systems attempt to care for people by focusing only on symptoms, which leads to dissatisfaction in patients and clinicians along with weak, transient, and inconsistent health benefits. If medicine is dedicated to health promotion, then there can be no merit in neglecting any of the aspects of the causes of well-being. Treatments that synergistically potentiate the triad of well-being can be expected to promote a flourishing of health beyond the results of conventional treatments.
References
- 1.Tournier P. The Best of Paul Tournier: Guilt & Grace, The Meaning of Persons, The Person Reborn, To Understand Each Other. New York: Iverson-Norman; 1997. [Google Scholar]
- 2.Cloninger CR. The science of well being: An integrated approach to mental health and its disorders. Psychiatry Danub. 2006;18(3–4):218–24. [PubMed] [Google Scholar]
- 3.WHO. Definition of Health: Preamble to the Constitution of the World Health Organization. World Health Organization; New York: 1946. [Google Scholar]
- 4.Mezzich JE, et al. Person-centred integrative diagnosis: conceptual bases and structural model. Canadian Journal of Psychiatry. 2010;55(11):701–8. doi: 10.1177/070674371005501103. [DOI] [PubMed] [Google Scholar]
- 5.Cloninger CR. The science of well-being: an integrated approach to mental health and its disorders. World Psychiatry. 2006;5(2):71–6. [PMC free article] [PubMed] [Google Scholar]
- 6.Cloninger CR. Feeling Good: The Science of Well-Being. New York: Oxford University Press; 2004. p. 374. [Google Scholar]
- 7.Cloninger CR, Zohar AH, Cloninger KM. Promotion of well-being in person-centered mental health care. Focus. 2010;8(2):165–179. doi: 10.1176/foc.8.2.foc165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong K, Cloninger CR. A person-centered approach to clinical practice. Focus. 2010;8(2):199–215. doi: 10.1176/foc.8.2.foc199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Servan-Schreiber D. Healing Without Freud or Prozac. London: Rodale International; 2005. [Google Scholar]
- 10.Chiesa A, Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psycholical Medicine. 2009:1–14. doi: 10.1017/S0033291709991747. [DOI] [PubMed] [Google Scholar]
- 11.Bertisch SM, et al. Alternative mind-body therapies used by adults with medical conditions. Journal of Psychosomatic Research. 2009;66(6):511–9. doi: 10.1016/j.jpsychores.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Targ EF, Levine EG. The efficacy of a mind-body-spirit group for women with breast cancer: a randomized controlled trial. General Hospital Psychiatry. 2002;24(4):238–48. doi: 10.1016/s0163-8343(02)00191-3. [DOI] [PubMed] [Google Scholar]
- 13.Baumeister RF, et al. Self-regulation and personality: how interventions increase regulatory success, and how depletion moderates the effects of traits on behavior. Journal of Personality. 2006;74(6):1773–801. doi: 10.1111/j.1467-6494.2006.00428.x. [DOI] [PubMed] [Google Scholar]
- 14.Muraven M, Baumeister RF, Tice DM. Longitudinal improvement of self-regulation through practice: Building self-control strength through repeated exercise. Journal of Social Psychology. 1999;139(4):446–457. doi: 10.1080/00224549909598404. [DOI] [PubMed] [Google Scholar]
- 15.Baumeister RF, Bauer IM, Lloyd SA. Choice, Free Will, and Religion. Psychology of Religion and Spirituality. 2010;2(2):67–82. [Google Scholar]
- 16.Amering M, Schmolke M. Recovery in Mental Health. In: Herrman H, editor. World Psychiatric Association Evidence and Experience in Psychiatry. New York: John Wiley & Sons; 2009. [Google Scholar]
- 17.Anthropedia F. Know Yourself. 2009 [cited 2011; Available from: http://anthropedia.org.
- 18.Schwartz S. Universals in the content and structure of values: Theoretical advances and empirical tersts in 20 countries. In: Zanna M, editor. Advances in Experimental Social Psychology. Academic Press; Orlando, FL: 1992. pp. 1–65. [Google Scholar]
- 19.Cloninger CR, Zohar AH. Personality and the perception of health and happiness. Journal of Affective Disorders. 2011;128(1–2):24–32. doi: 10.1016/j.jad.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 20.Cloninger CR, Svrakic NM, Svrakic DM. Role of personality self-organization in development of mental order and disorder. Development and Psychopatholy. 1997;9(4):881–906. doi: 10.1017/s095457949700148x. [DOI] [PubMed] [Google Scholar]
- 21.Joyce AS, et al. Psychotherapy research at the start of the 21st century: the persistence of the art versus science controversy. Canadian Journal of Psychiatry. 2006;51(13):797–809. doi: 10.1177/070674370605101302. [DOI] [PubMed] [Google Scholar]
- 22.Lambert MJ. Early response in psychotherapy: further evidence for the importance of common factors rather than “placebo effects”. Journal of Clinical Psychology. 2005;61(7):855–69. doi: 10.1002/jclp.20130. [DOI] [PubMed] [Google Scholar]
- 23.Lambert MJ. Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change. 5. New York: Wiley; 2003. [Google Scholar]
- 24.Castonguay LG, et al. Predicting the effect of cognitive therapy for depression: a study of unique and common factors. Journal of Consulting Clinical Psychology. 1996;64(3):497–504. [PubMed] [Google Scholar]
- 25.Clarkson P. The psychotherapeutic relationship. In: Clarkson P, Pokorny M, editors. Handbook of Psychotherapy. Routledge; London: 1994. pp. 28–48. [Google Scholar]
- 26.Strupp HH, Hadley SW. Specific vs nonspecific factors in psychotherapy. A controlled study of outcome. Archives of General Psychiatry. 1979;36(10):1125–36. doi: 10.1001/archpsyc.1979.01780100095009. [DOI] [PubMed] [Google Scholar]
- 27.Burns JW, Evon D. Common and specific process factors in cardiac rehabilitation: independent and interactive effects of the working alliance and self-efficacy. Health Psychology. 2007;26(6):684–92. doi: 10.1037/0278-6133.26.6.684. [DOI] [PubMed] [Google Scholar]
- 28.Burns JW, et al. Cognitive factors influence outcome following multidisciplinary chronic pain treatment: a replication and extension of a cross-lagged panel analysis. Behavioral Research and Therapy. 2003;41(10):1163–82. doi: 10.1016/s0005-7967(03)00029-9. [DOI] [PubMed] [Google Scholar]
- 29.Cloninger CR. Spirituality and the science of feeling good. Southern Medical Journal. 2007;100(7):740–3. doi: 10.1097/SMJ.0b013e318070d177. [DOI] [PubMed] [Google Scholar]
- 30.Sexton TL, Ridley CR, Kleiner AJ. Beyond common factors: multilevel-process models of therapeutic change in marriage and family therapy. Journal of Marital and Family Therapy. 2004;30(2):131–49. doi: 10.1111/j.1752-0606.2004.tb01229.x. [DOI] [PubMed] [Google Scholar]
- 31.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. American. Journal of Health Promotion. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 32.Cicchetti D. Resilience under conditions of extreme stress: a multilevel perspective. World Psychiatry. 2010;9(3):145–54. doi: 10.1002/j.2051-5545.2010.tb00297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cloninger CR, Cloninger KM. Development of instruments and evaluative procedures on contributors to health and illness. International Journal of Person-centered Medicine. 2011 doi: 10.5750/ijpcm.v1i3.99. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rogers CR. A Way of Being. Boston: Houghton Mifflin; 1995. [Google Scholar]
- 35.Cloninger CR. Foreword. In: O’Donohue WT, Fowler KA, Lilienfeld SO, editors. Personality Disorders: Toward the DSM-V. Sage Publications; Los Angeles: 2007. pp. vii–xvi. [Google Scholar]
- 36.Allport GW. Personality: A psychological interpretation. New Hork: Holt, Rinehart & Winston; 1937. [Google Scholar]
- 37.Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Archives of General Psychiatry. 1993;50(12):975–90. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- 38.Strack S, editor. Differentiating normal and abnormal personality. 2. Springer Publishing; New York: 2006. [Google Scholar]
- 39.Cloninger CR. The psychobiological theory of temperament and character: comment on Farmer and Goldberg (2008) Psychological Assessment. 2008;20(3):292–9. doi: 10.1037/a0012933. discussion 300–4. [DOI] [PubMed] [Google Scholar]
- 40.Cloninger CR. The evolution of human brain functions: the functional structure of human consciousness. Australian and New Zealand Journal of Psychiatry. 2009;43(11):994–1006. doi: 10.3109/00048670903270506. [DOI] [PubMed] [Google Scholar]
- 41.Cicchetti D, Rogosch FA. Equifinality and multifinality in developmental psychopatology. Development and Psychopathology. 1996;8:597–600. [Google Scholar]
- 42.Grucza RA, Goldberg LR. The comparative validity of 11 modern personality inventories: predictions of behavioral acts, informant reports, and clinical indicators. Journal of Personality Assessment. 2007;89(2):167–87. doi: 10.1080/00223890701468568. [DOI] [PubMed] [Google Scholar]
- 43.Svrakic DM, et al. Differential diagnosis of personality disorders by the seven-factor model of temperament and character. Archives of General Psychiatry. 1993;50(12):991–9. doi: 10.1001/archpsyc.1993.01820240075009. [DOI] [PubMed] [Google Scholar]
- 44.Cloninger CR. Temperament and personality. Current Opinion in Neurobiology. 1994;4(2):266–73. doi: 10.1016/0959-4388(94)90083-3. [DOI] [PubMed] [Google Scholar]
- 45.Cloninger CR. Completing the psychobiological architecture of human personality development: Temperament, Character, and Coherence. In: Staudinger UM, Lindenberger UER, editors. Understanding Human Development: Dialogues with Lifespan Psychology. Kluwer Academic Publishers; London: 2003. pp. 159–182. [Google Scholar]
- 46.Cloninger CR. A systematic method for clinical description and classification of personality variants. A proposal. Archives of General Psychiatry. 1987;44(6):573–88. doi: 10.1001/archpsyc.1987.01800180093014. [DOI] [PubMed] [Google Scholar]
- 47.Cloninger CR. A unified biosocial theory of personality and its role in the development of anxiety states. Psychiatric Development. 1986;4(3):167–226. [PubMed] [Google Scholar]
- 48.Heath AC, Cloninger CR, Martin NG. Testing a model for the genetic structure of personality: a comparison of the personality systems of Cloninger and Eysenck. Journal of Personality and Social Psychology. 1994;66(4):762–75. doi: 10.1037//0022-3514.66.4.762. [DOI] [PubMed] [Google Scholar]
- 49.Stallings MC, et al. Genetic and environmental structure of the Tridimensional Personality Questionnaire: three or four temperament dimensions? Journal of Personality and Social Psychology. 1996;70(1):127–40. doi: 10.1037//0022-3514.70.1.127. [DOI] [PubMed] [Google Scholar]
- 50.Cloninger CR. A practical way to diagnosis personality disorder: a proposal. Journal of Personlity Disorders. 2000;14(2):99–108. doi: 10.1521/pedi.2000.14.2.99. [DOI] [PubMed] [Google Scholar]
- 51.Conrad R, et al. Temperament and character personality profiles and personality disorders in chronic pain patients. Pain. 2007;133(1–3):197–209. doi: 10.1016/j.pain.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 52.Mulder RT, Joyce PR. Temperament and the structure of personality disorder symptoms. Psychological Medicine. 1997;27(1):99–106. doi: 10.1017/s0033291796004114. [DOI] [PubMed] [Google Scholar]
- 53.Karwautz A, et al. Personality disorders and personality dimensions in anorexia nervosa. Journal of Personality Disorders. 2003;17(1):73–85. doi: 10.1521/pedi.17.1.73.24057. [DOI] [PubMed] [Google Scholar]
- 54.Agrawal A, et al. Linkage scan for quantitative traits identifies new regions of interest for substance dependence in the Collaborative Study on the Genetics of Alcoholism (COGA) sample. Drug and Alcohol Dependence. 2008;93(1–2):12–20. doi: 10.1016/j.drugalcdep.2007.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cloninger CR, Svrakic DM. Integrative psychobiological approach to psychiatric assessment and treatment. Psychiatry. 1997;60(2):120–41. doi: 10.1080/00332747.1997.11024793. [DOI] [PubMed] [Google Scholar]
- 56.Gillespie NA, et al. The genetic and environmental relationship between Cloninger’s dimensions of temperament and character. Personality and Individual Differences. 2003;35:1931–1946. doi: 10.1016/S0191-8869(03)00042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Coward DD, Reed PG. Self-transcendence: a resource for healing at the end of life. Issues in Mental Health Nursing. 1996;17(3):275–88. doi: 10.3109/01612849609049920. [DOI] [PubMed] [Google Scholar]
- 58.Ellermann CR, Reed PG. Self-transcendence and depression in middle-age adults. Western Journal of Nursing Research. 2001;23(7):698–713. doi: 10.1177/01939450122045492. [DOI] [PubMed] [Google Scholar]
- 59.Runquist JJ, Reed PG. Self-transcendence and well-being in homeless adults. Journal of Holistic Nursing. 2007;25(1):5–13. doi: 10.1177/0898010106289856. discussion 14–5. [DOI] [PubMed] [Google Scholar]
- 60.Smith MJ, et al. Temperament and character as schizophrenia-related endophenotypes in non-psychotic siblings. Schizophrenia Research. 2008;104(1–3):198–205. doi: 10.1016/j.schres.2008.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gendall KA, et al. Personality and dimensions of dietary restraint. International Journal of Eating Disorders. 1998;24(4):371–9. doi: 10.1002/(sici)1098-108x(199812)24:4<371::aid-eat4>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 62.Ryan RM, Deci EL. On happiness and human potentials: a review of research on hedonic and eudaimonic well-being. Annual Reviews in Psychology. 2001;52:141–66. doi: 10.1146/annurev.psych.52.1.141. [DOI] [PubMed] [Google Scholar]