Abstract
Objective
To examine whether adherence to a Mediterranean-based dietary pattern is predictive of depressive symptoms among older adults.
Design
Generalized estimating equation models were used to test the association between a Mediterranean-based dietary pattern and depressive symptoms over time. Models were adjusted for age, sex, race, education, income, widowhood, antidepressant use, total calorie intake, body mass index, smoking, alcohol consumption, number of self-reported medical conditions, cognitive function, and physical disability.
Setting
Chicago, Illinois.
Participants
Community-dwelling participants (n=3502) of the Chicago Health and Aging Project aged 65+ years (59% African American) who had no evidence of depression at the baseline.
Measurements
Adherence to a Mediterranean-based dietary pattern was assessed by the MedDietScore. Dietary evaluation was performed with a food frequency questionnaire at baseline and related to incident depression as measured by the presence of four or more depressive symptoms from the 10-item version of the Center for Epidemiologic Studies Depression scale.
Results
Over an average follow-up of 7.2 years, greater adherence to a Mediterranean-based diet was associated with a reduced number of newly occurring depressive symptoms (parameter estimate = -0.002, standard error = 0.001; p = 0.04). The annual rate of developing depressive symptoms was 98.6% lower among persons in the highest tertile of a Mediterranean-based dietary pattern compared with persons in the lowest tertile group.
Conclusion
Our results support the hypothesis that adherence to a diet comprised of vegetables, fruits, whole grains, fish, and legumes may protect against the development of depressive symptoms in older age.
Keywords: Diet, mediterranean dietary pattern, depressive symptoms, older adults
The percentage of older adults who have clinically-relevant depression has been reported to range from 7% to 49% (1) and depressive symptomatology is also common (2-6), persistent (7), and has been associated with declines in physical performance (8) and even mortality (9). Despite its prevalence, reports have estimated that 70-90% of depression in older age is undiagnosed, mis-diagnosed, or dismissed as a normal part of aging (10). Lifestyle behaviors may be an effective, low-cost intervention to improve overall well-being in older adults.
Adherence to a Mediterranean diet, characterized by an abundance of whole grains, plant foods, and olive oil, and moderate intake of fish and wine has been associated with a variety of disease outcomes (see review in Sofi et al., 2010) (11), including reduced odds of cognitive decline and deficit (12-17) and cancers (18-20), improvements in cardiovascular risk factors (19, 21-23), and reduced all-cause and cause-specific mortality (24-28). However, there has been very little attention to the relation of the Mediterranean diet to overall well-being. One study of young adults in Spain suggests that the Mediterranean diet may reduce clinical depression (29). Therefore, we examined this relation in our study of community-dwelling older adults living in a mid-western U.S. population.
Methods
The study was conducted among participants of the Chicago Health and Aging Project (CHAP), a longitudinal study of Black and White residents 65 years and older living in three southside Chicago neighborhoods. A total of 6,158 age-eligible residents (78.9%) who were identified in a door-to-door census participated in the 1993-1996 baseline interview survey. Follow-up interviews were conducted at approximately three-year intervals from 1997 to 2000 (N = 4,320), 2000 to 2003 (N = 2,943), and 2003 to 2006 (N = 2,351), or up to 12 years. The structured, in-home interviews included sociodemographic questions, health history, medication use, lifestyle behaviors, psycho-social characteristics, and cognitive performance. All participants provided written, informed consent.
Study Variables
CHAP study participants completed a validated, semi-quantitative food-frequency questionnaire (FFQ) (30, 31). A Mediterranean diet score (the MedDietScore) was computed from responses to reported consumption of 11 food groups (22) that characterize the Mediterranean diet. Questionnaire items were assigned to the food groups as follows: non-refined cereals (3 items), potatoes (3 items), fruits (11 items), vegetables (16 items), legumes, nuts, beans (7 items), fish (3 items), olive oil (2 items), red meat and meat products (11 items), poultry (4 items), full fat dairy (6 items), and alcohol (3 items). Weekly consumption of the food groups characteristic of the Mediterranean pattern (i.e., fruits, vegetables, legumes, olive oil, fish, potatoes, and non-refined cereals) were assigned scores ranging from 5 for weekly consumption to 0 for rare consumption. Frequency of consumption of food groups not characteristic of the Mediterranean diet (i.e., red meat, poultry, full-fat dairy) was scored in the reverse (i.e., a score of 0 for consumption > 10 times per week to a score of 5 for once per week consumption or less often). Scoring for alcohol consumption was non-monotonic; a score of 5 was assigned for alcohol consumption <300 mL per week and >0, a score of 0 was assigned for consumption >700 mL/week or never consumed, and intermediate scores for 300 mL-700 mL. Possible scores ranged from 0 to 55, with higher scores representing greater consumption of food groups characteristic of a Mediterranean diet.
Assessment of depressive symptoms was based on the 10-item, yes-no version of the Center for Epidemiologic Studies Depression scale (CES-D) (32, 33). Because the distribution of CES-D scores is highly, positively skewed, we computed a dichotomous CES-D variable - scores of 3 or less versus scores of 4 and higher. A score of 4 or higher is the standard cutpoint and has shown reasonable specificity and sensitivity in identifying older adults with major depression (34).
We examined a number of potential confounders and effect modifiers: age (in years); sex; race (non-Hispanic Black vs. Non-Hispanic White); education (years of schooling); yearly personal income (income ranges scored from 1 [lowest] to 10 [highest]); widowhood (yes/no); total calorie intake; body mass index (BMI); smoking (pack years); alcohol consumption (mL per day); and number of self-reported medical conditions (myocardial infarction, stroke, cancer, diabetes, high blood pressure, Parkinson's disease, shingles, thyroid disease, and hip fracture). We also controlled for global cognitive function -computed from the average of standardized scores from 4 tests (the Mini-Mental State Examination, Symbol Digit Modalities Test, the East Boston Test of Immediate Memory, and the East Boston Test of Delayed Memory). We also controlled for physical disability -assessed using six self-reported activities of daily living (ADLs) and instrumental activities of daily living (IADLs) measures based on the work of Katz (35).
Statistical Analysis
Of the 6,158 CHAP participants, 12% (n = 747) were excluded from analyses due to incomplete data. We also excluded 991 participants with evidence of depression (CES-D score ≥ 4 symptoms) at baseline and 918 participants who died before their first follow-up. The remaining 3,502 participants comprised our final analytic sample, of which, 50% completed all four interview cycles, 22% completed three cycles, and 28% completed two interview cycles, resulting in 11,263 depression assessments over four observation cycles. Death was the primary reason for non-participation at each follow-up cycle. The average follow-up was 7.2 years.
We used generalized estimating equation (GEE) models to model the vector of CES-D scores from each person as a function of age, sex, race, time since baseline, and other covariates. GEE is particularly suitable for this as it offers a choice of link functions to model the outcome variable and accounts for the within-person correlation across repeated measurements (36). The number of depressive symptoms (where CES-D score >= 4) was modeled as a poisson-distributed count variable with a canonical log link function (37, 38). The basic model was adjusted for age, sex, race, education, income, widowhood, total caloric intake, and BMI. We tested separate models adjusting for multiple covariates, time lag (i.e., follow-up years since baseline), and interaction terms for each covariate and time lag. effect modification (where p < 0.05) was also examined by including 3-way interaction terms between each of the covariates, MedDietScore, and time lag in the basic model. Widowhood and medical conditions were modeled as time-varying covariates, all other covariates were based on baseline measurements. All longitudinal analyses were performed using the GENMOD® procedure of SAS® version 9.2 (38).
Results
The analytic sample had a mean MedDietScore of 28.2 (SD = 4.7), age of 73.5, 12.3 years of education, and a mean annual income between $20,000-$24,999. The sample was 41% male, 59% Black, and 39% widowed. The mean daily calorie consumption was 1,750 (SD = 610.5), the mean smoking pack years was 18 (SD = 27.4), the mean weekly alcohol intake was 4.3 mL (SD = 10.6), and the mean number of medical conditions reported was 1.2 (SD = 1.0). The mean baseline CES-D score was 0.8. During follow-up, the occurrence of 4 or more depressive symptoms was reported by 13.7% (471 participants) at the first follow-up (cycle 2), by 10.7% (256 participants) at cycle 3, and by 13.4% (260 participants) at cycle 4.
Participants who were in the lowest tertile of MedDietScores -indicating lower Mediterranean diet consumption- were more likely to be older, Blacks, and to have lower educational level and income than participants in the higher tertiles. They also had lower caloric intake and alcohol consumption. persons in the highest tertile of MedDietScores had higher educational and income levels and higher alcohol use (Table 1). Figure 1 shows the mean weekly consumption of Mediterranean food groups in our sample at baseline relative to the ideal number of food group servings (i.e., a perfect score of 5 per food group) (17, 22). Consumptions of fruit and legumes were closest to the target ranges (69% and 49% respectively), but consumption of red meat was in excess (by 360%) of target.
Table 1. Characteristics of the study sample, by Mediterranean diet score tertiles at baseline (1993-1996), the Chicago Health and Aging Project, N=3,502.
| Total Sample | MedDietScore, tertiles | |||
|---|---|---|---|---|
| MedDietScore, x̄ (SD) | 28.2 (4.7) | (15-25) | (26-29) | (30-44) |
| Age, x̄ (SD) | 73.5 (6.1) | 74.0 (6.5) | 73.6 (6.2) | 73.1 (5.8) |
| Male sex, % | 41.0 | 40.1 | 39.3 | 43.3 |
| Black race, % | 59.3 | 69.0 | 62.0 | 49.2 |
| Education, x̄ (SD) | 12.3 (3.6) | 11.3 (3.4) | 12.1 (3.6) | 13.3 (3.6) |
| Income1, x̄ (SD) | 4.9 (2.5) | 4.2 (2.3) | 4.8 (2.3) | 5.6 (2.5) |
| Widowed, % | 38.6 | 40.3 | 41.8 | 34.4 |
| Calories, x̄ (SD) | 1,750.3 (610.5) | 1,500.2 (572.8) | 1,753.9 (598.0) | 1,945.0 (578.0) |
| Smoke (pack years), x̄ (SD) | 18.0 (27.4) | 18.8 (28.1) | 17.1 (26.6) | 18.3 (27.6) |
| Alcohol use (mL/day), x̄ (SD) | 4.3 (10.6) | 2.2 (11.1) | 4.1 (10.7) | 6.0 (9.8) |
| Medical conditions, x̄ (SD) | 1.2 (1.0) | 1.2 (1.0) | 1.2 (1.0) | 1.2 (1.0) |
| Cognition function, x̄ (SD) | 0.2 (0.7) | 0.1 (0.7) | 0.2 (0.7) | 0.4 (0.6) |
| Physical disability, x̄ (SD) | 0.1 (0.6) | 0.2 (0.8) | 0.1 (0.5) | 0.1 (0.5) |
| BMI, x̄ (SD) | 27.2 (5.4) | 27.3 (5.7) | 27.4 (5.5) | 26.8 (5.1) |
| CES-D score, x̄ (SD)[range:0-10] | 0.8 (1.0) | 0.9 (1.0) | 0.8 (1.0) | 0.8 (1.0) |
Range: 1 (< $5,000) to 10 (> $75,000). A score of 4 represents an annual income of $15,000 - $19,999 and a score of 5 represents an annual income of $20,000 - $24,999.
Figure 1.
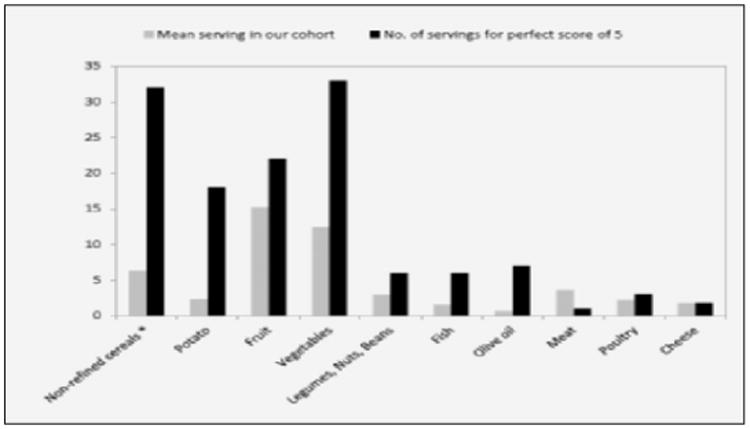
Mean number of servings per week of the Mediterranean diet food categories reported by study participants at baseline, compared to the ideal number of servings (maximum score of 5)
* ‘non-refined cereals’ actually includes such items on our FFQ as hot breakfast cereals like oatmeal and grits, dark breads, and other grains such as kasha, couscous, bulgar, etc. A perfect score of 5 is given if the participant reports consuming at least 32 servings of non-refined cereals per week. See text “Study variables” for additional information.
MedDietScore was inversely associated with risk of developing depressive symptoms in the adjusted models (Table 2). Whereas the depressive symptom rate generally increased by 7.4% (lag estimate = 0.0716) annually, for every 5-point increase in MedDietScore, the annual depressive symptom rate increased by only 6.4%. The estimate of effect for MedDietScore remained virtually unchanged with additional adjustment for smoking and alcohol use (model 2), chronic medical conditions (model 3), and cognitive function (model 4). Further adjustment for physical disability also did not change the effect estimates. We also examined potential modifications and found that the dietary association was stronger among Whites than Blacks (data not shown).
Table 2. Poisson regression models for the longitudinal associations between adherence to Mediterranean diet and depressive symptoms, N=3,502.
| MedDietScore × time lag1 | ||
|---|---|---|
| Estimate (SE) | P-value | |
| Model 1: adjusted for age, sex, race, education, income, widowhood, calories, BMI, MedDietScore, time lag, and interactions of each variable with time lag (lag). | -0.002 (0.001) | 0.01 |
| Model 2: model 1 + smoking, alcohol use, and both variables' interactions with lag | -0.002 (0.001) | 0.02 |
| Model 3: model 2 + medical conditions and its interaction with lag | -0.002 (0.001) | 0.04 |
| Model 4: model 1 + global cognitive function and its interaction with lag | -0.002 (0.001) | 0.02 |
Time lag (lag) = (follow-up years since baseline)
In an attempt to more clearly depict the nature of association between adherence to the Mediterranean diet and depressive symptoms, we re-analyzed the basic adjusted model with MedDietScore modeled in tertiles (Figure 2). persons in Tertile 1 – the lowest adherence group – had the highest rate of developing depressive symptoms over time (β = 0.03, SE = 0.01, p-value = 0.05). The slope for persons in Tertile 2 was not as steep as for Tertile 1 (slope difference: β = -0.01, SE = 0.01, p-value = 0.25). The slope for persons in Tertile 3 – the highest adherence – was almost flat (slope difference: β = -0.03, SE = 0.01, p-value < 0.001), indicating a very low occurrence (close to zero) of depressive symptoms. In fact, the annual rate of developing depressive symptoms was 98.6% lower among persons in Tertile 3 compared with persons in Tertile 1.
Figure 2.
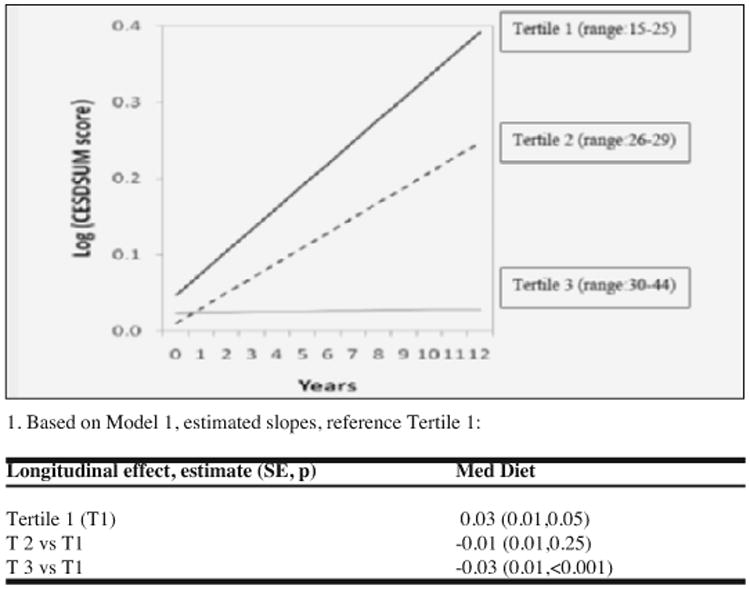
The estimated1 association of Mediterranean diet and depressive symptomatology over time, showing that adherence to a Mediterranean diet is inversely related to developing depressive symptoms over time. persons in the top tertile of MedDietScore (range: 30-44) have a lower risk of depressive symptoms represented by the flatter slope of CESDSUM score than those in the middle tertile (range: 26-29) and lowest tertile (range: 15-25)
Discussion
In this large, biracial community study of older adults, greater consumption of a dietary pattern that was higher in whole grains, vegetables, fruits, olive oil, fish, legumes, and lower in meats and high-fat dairy was associated with decreased likelihood of developing depressive symptoms over an average 7.2 years, independent of demographic factors, medical conditions, and cognitive and functional decline. The association appeared to be stronger in Whites than in Blacks, but this may have been due to lower adherence to the diet or lower variation in the diet among Blacks and thus less variability in the MedDietScore to show association as opposed to a differential effect of the diet by race.
Our findings are in agreement with a study of more than 10,000 young (average age 37) Spanish adults that reported a reduced risk of clinical depression and antidepressant medication use among those who had greatest adherence to the Mediterranean diet (29) and with previous studies that related the Mediterranean diet to higher quality of life (39) and slower rates of cognitive decline (12-17).
The Mediterranean diet may be linked to mental health outcomes via the high number of dietary constituents such as B-vitamins, antioxidant nutrients, and fat composition. For example, B-vitamins play important roles in the synthesis of neurotransmitters that affect mood (11) including serotonin, norepinephrine, and dopamine (40, 41) and in a previous study, we found that vitamins B6 and B12 were associated with decreased likelihood of developing depressive symptoms (42). Two other prospective studies also found associations between B-vitamin deficiencies and depression (43-45). Antioxidant nutrients (e.g., vitamin E, carotenoids) are also rich in the Mediterranean diet and may protect neuronal cells against oxidative damage and impaired functioning (46). Moreover, several Mediterranean components - nuts, seeds, legumes, and fish - are important contributors to unsaturated fatty acids that have vasodilatory and anti-inflammatory properties which may be involved in the neurodegenerative process (47-49). Mediterranean diets may also improve overall mental health in part through an improvement of endothelial function (50, 51).
This study has a number of strengths that lend confidence to the finding. The observed associations are based on data from a large, prospective, community-based study with high rates of participation, up to four assessments of depressive symptoms over 12 years, and comprehensive dietary assessment using a validated questionnaire. The primary limitation is that CHAP is an observational study and therefore confounding is always an alternative explanation for observed associations; however, we tested for a large number of potential confounders. The CHAP population comes from a large, biracial, midwestern U.S. city, and as such, the results of our study may not be generalizable to smaller, rural, or other racial/ethnic populations.
Conclusion
We found that greater consumption of food groups characteristic of a Mediterranean-based diet was associated with lower likelihood of depressive symptoms in older adults over time. Although the exact mechanism for this association is unclear, our study provides further evidence that adopting a healthy diet in older age confers many benefits, including protection against depressive symptoms. Future research should examine the practical aspects of application, such as the ease or difficulty in adhering to this dietary pattern in countries outside the Mediterranean basin as well as overall cost-effectiveness.
Acknowledgments
Funding: This research was supported by grants from the national institutes of Health: national institute on Aging (AG11101, AG13170, AG021972).
This research was presented at a symposium at the Gerontological Society of America Annual Conference, in Boston, MA, on November 18, 2011.
Footnotes
Conflict of Interest: The authors declare no conflicts of interest, financial or otherwise. Dr. Skarupski takes responsibility for the integrity of the data and the accuracy of the data analysis; all authors had full access to the data in the study.
Sponsor's Role: The sponsor did not have a role in the design, methods, or other aspects of this manuscript.
Author Contributions: Kimberly S., Christy T., and Martha Clare M.: conceived of the study hypothesis, designed the overall analysis plan, interpreted the data, and prepared the manuscript. Denis E. designed the primary study and the data collection process. Hong L. contributed to the analysis plan, conducted the analyses, and aided in the interpretation of the data.
References
- 1.He W, Sengupta M, Velkoff VA, DeBarros KA. US Census Bureau, Current population reports, P23-209, 65+ in the united States, 2005. Washington D.C.: U.S.Government Printing Office; 2005. [Google Scholar]
- 2.Djernes JK. Prevalence and predictors of depression in populations of elderly: A review. Acta Psychiatr Scand. 2006;113(5):372. doi: 10.1111/j.1600-0447.2006.00770.x. [DOI] [PubMed] [Google Scholar]
- 3.Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. 1999;174:307–311. doi: 10.1192/bjp.174.4.307. [DOI] [PubMed] [Google Scholar]
- 4.Cole MG, Bellavance F, Mansour A. Prognosis of depression in elderly community and primary care populations: A systematic review and meta-analysis. Am J Psychiatry. 1999;156(8):1182–1189. doi: 10.1176/ajp.156.8.1182. [DOI] [PubMed] [Google Scholar]
- 5.Mills TL. Comorbid depressive symptomatology: Isolating the effects of chronic medical conditions on self-reported depressive symptoms among community-dwelling older adults. Soc Sci Med. 2001;53(5):569–578. doi: 10.1016/s0277-9536(00)00361-0. [DOI] [PubMed] [Google Scholar]
- 6.Skarupski KA, Mendes de Leon CF, Bienias JL, Barnes LL, Everson-rose SA, et al. Black-white differences in depressive symptoms among older adults over time. J Gerontol B Psychol Sci Soc Sci. 2005;60(3):136–42. doi: 10.1093/geronb/60.3.p136. [DOI] [PubMed] [Google Scholar]
- 7.Harris T, Cook D, Victor C, DeWilde S, Beighton C. Onset and persistence of depression in older people--results from a 2-year community follow-up study. Age Ageing. 2006;35(1):25–32. doi: 10.1093/ageing/afi216. [DOI] [PubMed] [Google Scholar]
- 8.Everson-Rose SA, Skarupski KA, Bienias JL, Wilson RS, Evans DA, et al. Do depressive symptoms predict declines in physical performance in an elderly, biracial population? Psychosom Med. 2005;67(4):609–615. doi: 10.1097/01.psy.0000170334.77508.35. [DOI] [PubMed] [Google Scholar]
- 9.Whooley MA, Browner WS. Association between depressive symptoms and mortality in older women. Study of osteoporotic fractures research group. Arch Intern Med. 1998;158(19):2129. doi: 10.1001/archinte.158.19.2129. [DOI] [PubMed] [Google Scholar]
- 10.Koenig HG. Interview by Alice V. 5. Vol. 54. Luddington: Geriatrics; 1999. Late-life depression: How to treat patients with comorbid chronic illness; pp. 56–61. [PubMed] [Google Scholar]
- 11.Sofi F, Abbate R, Gensini G, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92(5):1189–1196. doi: 10.3945/ajcn.2010.29673. 2010. [DOI] [PubMed] [Google Scholar]
- 12.Berr C, Portet F, Carriere I, Akbaraly T, Feart C, et al. Olive oil and cognition: Results from the Three-City Study. Dement Geriatr Cogn Disord. 2009;28(4):357–64. doi: 10.1159/000253483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Féart C, Samieri C, Rondeau V, Amieva H, Portet F, et al. Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. JAMA. 2009;302(6):638–48. doi: 10.1001/jama.2009.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scarmeas N, Stern Y, Tang MX, Mayeux R, Luchsinger JA. Mediterranean diet and risk for Alzheimer's disease. Ann Neurol. 2006;59(6):912–921. doi: 10.1002/ana.20854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scarmeas N, Stern Y, Mayeux R, Manly JJ, Schupf N, et al. Mediterranean diet and mild cognitive impairment. Arch Neurol. 2009;66(2):216–225. doi: 10.1001/archneurol.2008.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Solfrizzi V, Colacicco AM, D'Introno A, Capurso C, Torres F, et al. Dietary intake of unsaturated fatty acids and age-related cognitive decline: A 8.5-year follow-up of the Italian longitudinal study on aging. Neurobiol Aging. 2006;27(11):1694–1704. doi: 10.1016/j.neurobiolaging.2005.09.026. [DOI] [PubMed] [Google Scholar]
- 17.Tangney CC, Kwasny MJ, Li H, Wilson RS, Evans DA, et al. Adherence to a Mediterranean-type dietary pattern and cognitive decline in a community population. Am J Clin Nutr. 2011;93(3):601–607. doi: 10.3945/ajcn.110.007369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bosetti C, Gallus S, Trichopoulou A, Talamini R, Franceschi S, et al. Influence of the Mediterranean diet on the risk of cancers of the upper aerodigestive tract. Cancer Epidemiol Biomarkers Prev. 2003;12(10):1091–1094. [PubMed] [Google Scholar]
- 19.de Lorgeril M, Salen P. Modified Cretan Mediterranean diet in the prevention of coronary heart disease and cancer: An update. World Rev Nutr Diet. 2007;97:1–32. doi: 10.1159/000097870. [DOI] [PubMed] [Google Scholar]
- 20.Dixon LB, Subar A, Peters U, Weissfeld J, Bresalier R, et al. Adherence to the USDA food guide, DASH eating plan, and Mediterranean dietary pattern reduces risk of colorectal adenoma. J Nutr. 2007;137(11):2443–50. doi: 10.1093/jn/137.11.2443. [DOI] [PubMed] [Google Scholar]
- 21.de Lorgeril M, Salen P. The Mediterranean-style diet for the prevention of cardiovascular diseases. Public Health Nutr. 2006;9(1A):118–123. doi: 10.1079/phn2005933. [DOI] [PubMed] [Google Scholar]
- 22.Panagiotakos D, Pitsavos C, Arvaniti F, Stefanadis C. Adherence to the Mediterranean food pattern predicts the prevalence of hypertension, hypercholesterolemia, diabetes and obesity, among healthy adults; The accuracy of the MedDietScore. Prev Med. 2007;44(4):335–340. doi: 10.1016/j.ypmed.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 23.Chrysohoou C, Liontou C, Aggelopoulos P, Kastorini C, Panagiotakos D, et al. Mediterranean diet mediates the adverse effect of depressive symptomatology on short-term outcome in elderly survivors from an acute coronary event. Cardiol Res and Pract. 2011:429487–429487. doi: 10.4061/2011/429487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barzi F, Woodward M, Marfisi RM, Tavazzi L, Valagussa F, et al. Mediterranean diet and all-causes mortality after myocardial infarction: Results from the GISSI-prevenzione trial. Eur J Clin Nutr. 2003;57(4):604–611. doi: 10.1038/sj.ejcn.1601575. [DOI] [PubMed] [Google Scholar]
- 25.Fung T, Rexrode K, Mantzoros C, Manson J, Willett W, et al. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119(8):1093–1100. doi: 10.1161/CIRCULATIONAHA.108.816736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Knoops KTB, de Groot K, Daan, Perrin A, Moreiras-Varela O, Menotti A, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: The HALE project. JAMA. 2004;292(12):1433–1439. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 27.Mitrou P, Kipnis V, Thiébaut ACM, Reedy J, Subar A, et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: Results from the NIH-AARP diet and health study. Arch Intern Med. 2007;167(22):2461–2468. doi: 10.1001/archinte.167.22.2461. [DOI] [PubMed] [Google Scholar]
- 28.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 29.Sánchez-villegas A, Delgado-Rodríguez M, Alonso A, Schlatter J, Lahortiga F, et al. Association of the mediterranean dietary pattern with the incidence of depression: The seguimiento universidad de Navarra/University of Navarra follow-up (SUN) cohort. Arch Gen Psychiatry. 2009;66(10):1090–1098. doi: 10.1001/archgenpsychiatry.2009.129. [DOI] [PubMed] [Google Scholar]
- 30.Morris MC, Colditz GA, Evans DA. Response to a mail nutritional survey in an older biracial community population. Ann Epidemiol. 1998;8(5):342. doi: 10.1016/s1047-2797(97)00236-6. [DOI] [PubMed] [Google Scholar]
- 31.Morris MC, Tangney CC, Bienias JL, Evans DA, Wilson RS. Validity and reproducibility of a food frequency questionnaire by cognition in an older biracial sample. Am J Epidemiol. 2003;158(12):1213. doi: 10.1093/aje/kwg290. [DOI] [PubMed] [Google Scholar]
- 32.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (center for epidemiological studies depression) depression symptoms index. J Aging Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 33.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1997;1(3):385–401. [Google Scholar]
- 34.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: Criterion validity of the 10-item center for epidemiological studies depression scale (CES-D) Arch Intern Med. 1999;159(15):1701. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- 35.Branch LG, Katz S, Kniepmann K, Papsidero JA. A prospective study of functional status among community elders. Am J Public Health. 1984;74(3):266. doi: 10.2105/ajph.74.3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Diggle PJ, Heagerty P, Liang KY, Zeger SL. Analysis of longitudinal data. Oxford; New York: Oxford University Press; 2002. p. 379. [Google Scholar]
- 37.Allison PD SAS institute. Logistic regression using the SAS system: Theory and application. Cary, N.C.: SAS Institute; 1999. [Google Scholar]
- 38.SAS Institute. SAS/STAT® user's guide (version 9.2) Cary, NC: SAS Institute; [Google Scholar]
- 39.Muñoz M, Fíto M, Marrugat J, Covas M, Schröder H. Adherence to the Mediterranean diet is associated with better mental and physical health. Br J Nutr. 2008;101(12):1821–1827. doi: 10.1017/S0007114508143598. 2009. [DOI] [PubMed] [Google Scholar]
- 40.Bruinsma KA, Taren DL. Dieting, essential fatty acid intake, and depression. Nutr Rev. 2000;58(4):98–108. doi: 10.1111/j.1753-4887.2000.tb07539.x. [DOI] [PubMed] [Google Scholar]
- 41.Delgado PL. Depression: The case for a monoamine deficiency. J Clin Psychiatry. 2000;61(Suppl 6):7–11. [PubMed] [Google Scholar]
- 42.Skarupski K, Tangney C, Li H, Ouyang B, Evans D, et al. Longitudinal association of vitamin B-6, folate, and vitamin B-12 with depressive symptoms among older adults over time. Am J Clin Nutr. 2010;92(2):330–335. doi: 10.3945/ajcn.2010.29413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tolmunen T, Hintikka J, Ruusunen A, Voutilainen S, Tanskanen A, et al. Dietary folate and the risk of depression in Finnish middle-aged men. A prospective follow-up study. Psychother Psychosom. 2004;73(6):334. doi: 10.1159/000080385. [DOI] [PubMed] [Google Scholar]
- 44.Kim J, Stewart R, Kim S, Yang S, Shin I, et al. Predictive value of folate, vitamin B12 and homocysteine levels in late-life depression. Brit J Psychiat. 2008;192(4):268. doi: 10.1192/bjp.bp.107.039511. [DOI] [PubMed] [Google Scholar]
- 45.Selhub J, Bagley LC, Miller J, Rosenberg IH. B vitamins, homocysteine, and neurocognitive function in the elderly. Am J Clin Nutr. 2000;71(2):614S–620S. doi: 10.1093/ajcn/71.2.614s. [DOI] [PubMed] [Google Scholar]
- 46.Sarandol A, Sarandol E, Eker SS, Erdinc S, Vatansever E, et al. Major depressive disorder is accompanied with oxidative stress: Short-term antidepressant treatment does not alter oxidative-antioxidative systems. Hum Psychopharm. 2007;22(2):67–73. doi: 10.1002/hup.829. [DOI] [PubMed] [Google Scholar]
- 47.Barbizan R, Oliveira A. impact of acute inflammation on spinal motoneuron synaptic plasticity following ventral root avulsion. J Neuroinflammation. 2010;7:29–29. doi: 10.1186/1742-2094-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Delion S, Chalon S, Guilloteau D, Besnard JC, Durand G. Alpha-linolenic acid dietary deficiency alters age-related changes of dopaminergic and serotoninergic neurotransmission in the rat frontal cortex. J Neurochem. 1996;66(4):1582–1591. doi: 10.1046/j.1471-4159.1996.66041582.x. [DOI] [PubMed] [Google Scholar]
- 49.Lin P, Su K. A meta-analytic review of double-blind, placebo-controlled trials of antidepressant efficacy of omega-3 fatty acids. J Clin Psychiatry. 2007;68(7):1056–1061. doi: 10.4088/jcp.v68n0712. [DOI] [PubMed] [Google Scholar]
- 50.Guo S, Kim W, Lok J, Lee S, Besancon E, et al. Neuroprotection via matrix-trophic coupling between cerebral endothelial cells and neurons. Proc Natl Acad Sci U S A. 2008;105(21):7582–7587. doi: 10.1073/pnas.0801105105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sánchez-Villegas A, Galbete C, Martinez-González M, Martinez JA, Razquin C, et al. The effect of the Mediterranean diet on plasma brain-derived neurotrophic factor (BDNF) levels: The PREDIMED-NAVARRA randomized trial. Nutr Neurosci. 2011;14(5):195–201. doi: 10.1179/1476830511Y.0000000011. [DOI] [PubMed] [Google Scholar]


