Abstract
Extracellular matrix (ECM) structure, composition, and stiffness have profound effects on tissue development and pathologies such as cardiovascular disease and cancer. Accordingly, a variety of synthetic hydrogel systems have been designed to study the impact of ECM composition, density, mechanics, and topography on cell and tissue phenotype. However, these synthetic systems fail to accurately recapitulate the biological properties and structure of the native tissue ECM. Natural three dimensional (3D) ECM hydrogels, such as collagen or hyaluronic acid, feature many of the chemical and physical properties of tissue, yet, these systems have limitations including the inability to independently control biophysical properties such as stiffness and pore size. Here, we present a 3D tension bioreactor system that permits precise mechanical tuning of collagen hydrogel stiffness, while maintaining consistent composition and pore size. We achieve this by mechanically loading collagen hydrogels covalently-conjugated to a polydimethylsiloxane (PDMS) membrane to induce hydrogel stiffening. We validated the biological application of this system with oncogenically transformed mammary epithelial cell organoids embedded in a 3D collagen I hydrogel, either uniformly stiffened or calibrated to create a gradient of ECM stiffening, to visually demonstrate the impact of ECM stiffening on transformation and tumor cell invasion. As such, this bioreactor presents the first tunable 3D natural hydrogel system that is capable of independently assessing the role of ECM stiffness on tissue phenotype.
Keywords: Cell culture, Bioreactor, 3D collagen hydrogel, ECM stiffness, Mechanotransduction
The biophysical properties of the extracellular matrix (ECM) are important determinants of cell and tissue behavior, as shown by prior studies that highlight effects on cell migration, proliferation, survival, and tissue morphogenesis (Paszek et al., 2005; Guo et al., 2012). In particular, ECM rigidity and organization play essential roles in biological processes such as stem cell differentiation, wound healing, and pathologies such as cancer (Engler et al., 2006; Lu et al., 2011; Mouw et al., 2014). Nevertheless, how cells sense and respond to these biophysical cues from the ECM remains poorly understood.
Studies examining the relationship between ECM mechanics and cell phenotype have thus far been hampered by limitations in the experimental approaches used to manipulate biophysical properties of the ECM. Current state-of-the-art systems pre-dominantly employ mechanically tunable two-dimensional (2D) polymer hydrogels conjugated with ECM ligands (e.g., collagen, fibronectin, laminin, etc.) (Tse et al., 2010; Young et al., 2011). These 2D substrates, unfortunately, fail to model the heterogeneous and three-dimensional (3D) structure of native tissue. More recent approaches that employ 3D hydrogel substrates are fraught with limitations, including the failure to control for pore size, lack of ECM remodeling, and gel inconsistencies. For instance, while synthetic polymer systems are amenable to careful tuning of mechanical properties and ECM presentation, these systems fail to recapitulate the complex, multicomponent composition of native tissue, do not enable cells to remodel the matrix, and lack the architecture of natural ECM hydrogels (Miroshnikova et al., 2011; Miller et al., 2010). By contrast, the use of native ECM materials such as type I collagen, fibrin, or hyaluronic acid for 3D hydrogel studies more faithfully reconstitute the native tissue matrix composition and function, including the binding and presentation of growth factors and cell-mediated matrix remodeling (Yamada and Cukierman, 2007). However, the use of native hydrogels is compromised by lack of uniformity and consistency and the profound changes in pore size and ligand binding induced when protein concentration or cross-linking are used to modify biophysical properties (Ulrich et al., 2010; Provenzano et al., 2010; Miroshnikova et al., 2011).
We developed a novel tension bioreactor system that employs a native collagen I (Col I) hydrogel and permits consistent manipulation of ECM stiffness in the absence of modifications to the structure, composition, or pore size of the gel. Briefly, our method involves casting a polydimethylsiloxane (PDMS) membrane using a 3D printed negative mold to create a membrane with wells of defined depth to accommodate the collagen hydrogel and a surrounding media reservoir. The PDMS membrane is surface activated through a combination of plasma cleaning, a (3-Aminopropyl)triethoxysilane (APTES) incubation, followed by glutaraldehyde incubation, as previously described (Wipff et al., 2009). Following surface activation, Col I solution is prepared by neutralizing acid-solubilized rat tail collagen I (BD Bioscience) with 1 N NaOH and a DMEM buffer, and polymerized at 37 °C within wells in the PDMS membrane. After polymerization, the PDMS membrane is attached to an aluminum-loading frame, which, through connections to a sliding rail system, permits uniaxial stretching of the membrane and the attached collagen gel up to 10% strain (Fig. 1A).
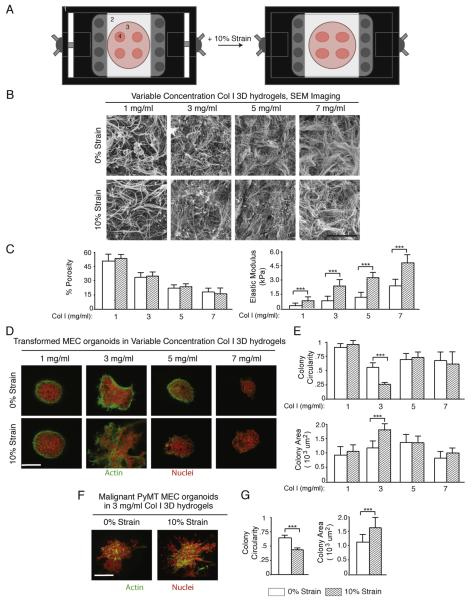
Fig. 1.
Characterization and biological application of tension bioreactor. (A) Schematic of tension bioreactor system, consisting of (1) stretching frame, (2) PDMS stretchable membrane, (3) media reservoir, (4) Col I hydrogels. (B) SEM images of Col I hydrogels of varying collagen concentration at 0 and 10% strain in the bioreactor system (scale bar = 2 μm). (C) Quantification of gel pore size and elastic modulus as a function of Col I concentration and the application of uniaxial strain (error bars represent standard deviation, *** denotes p < 0.05 evaluated by t-test). (D) Premalignant mammary epithelial cells pre-grown in rBM as spherical multicellular organoids embedded in Col I hydrogels of varying concentration and then placed under either 0 or 10% strain in the tension bioreactor. After 2 days cultures were fixed and stained for actin cytoskeleton and nuclei to assess the extent of tumor cell invasion and migration (scale bar = 20 μm). (E) Quantification of organoid spread area and circularity. (F) Malignant mammary epithelial cells pre-grown in rBM as spherical multicellular organoids embedded in 3 mg/ml Col I hydrogels and then placed under either 0 or 10% strain in the tension bioreactor. After 2 days cultures were fixed and stained for actin cytoskeleton and nuclei to assess the extent of tumor cell invasion and migration (scale bar = 20 μm). G) Quantification of PyMT organoid spread area and circularity.
Using atomic force microscopy (AFM) with a Bio-AFM (Aslyum Research) and a beaded silicon tip (5 mm diameter, Novascan), we measured the elastic modulus of the Col I hydrogel under 0 and 10% applied strain over a range of Col I concentrations (1–7 mg/ml). Force measurements were performed at 1 pN indentation with 100 measurements per condition and force curves were fitted with the Hertz model and averaged to determine the gel elastic modulus. Using these measurements, we observed that, depending on collagen concentration, upon stretching of the PDMS membrane, we were able to increase the ECM elastic modulus up to fourfold (Fig. 1C). Samples were retested 7 days later and showed no change in elastic modulus, suggesting that the stiffening effect is permanent due to collagen strain hardening as previously described (Gautieri et al., 2011).
We then used scanning electron microscopy (SEM) to determine the effect of strain on hydrogel architecture, porosity, and organization. Collagen gels were fixed and prepared as previously described (Miroshnikova et al., 2011), then imaged on a JEOL JCM-6000 Neo-scope SEM (JEOL USA Inc., Peabody, MA). SEM images were used to determine hydrogel porosity and organization with ctFire analysis software (LOCI, UW Madison), with porosity defined as the ratio of fiber surface area to total image area and gel organization determined by the average individual fiber orientation and straightness. With this analysis, we concluded that porosity and fiber organization do not significantly change with mechanical loading for a given Col I concentration (evaluated by Student’s t-test). Thus, we have the first 3D natural material hydrogel system in which we can alter the ECM stiffness independently of the ECM structure across a range of different substrate concentrations (Fig. 1B–C).
Our group and others have previously demonstrated that ECM remodeling and stiffening can potentiate tumor malignant progression (Provenzano et al., 2009; Levental et al., 2009). Thus, to demonstrate the biological applications of our system, we aimed to determine the impact of altered ECM stiffness on tumor cell migration and invasion in a 3D context independently of structural changes to the ECM. We cultured oncogenically transformed (Ha-Ras) pre-malignant mammary epithelial cell organoids (pre-grown for 8 days in rBM) embedded in Col I hydrogels of varying concentrations supplemented with FN (1 μg/ml) and rBM (5%) and in the tension bioreactor with 0 or 10% strain for up 2 days. To assess the extent and penetrance of tumor cell invasion and migration, we paraformaldehyde fixed and stained Col I hydrogels with propridium iodide and AlexaFluor 488-phalloidin and imaged the gels using a 2-photon microscope (Olympus upright microscope, Olympus 20X .95 NA objective). Organoid invasion and tumor cell migration was quantified by thresholding fluorescence images for signal above 3× background and measuring colony spread area and circularity with ImageJ (Schneider et al., 2012).
These experiments revealed that increasing collagen concentration to increase the ECM rigidity initially induced tumor cell invasion. However, once collagen concentration reached 5 mg/ml, cell invasion was greatly reduced, likely due to decreasing pore size (Wolf et al., 2013; Haeger et al., 2014; Rubashkin et al., 2014). In marked contrast, we quantified a profound increase in tumor cell invasion induced by increasing ECM stiffness via our bioreactor, illustrating that when pore size is not limiting, ECM stiffness independently enhances tumor cell invasion and migration (Fig. 1D and E). Following these studies, we aimed to assess the effect of ECM stiffness in our system with malignant tumor cells. We isolated tumor cells from MMTV PyMT transgenic tumor model mice and grew the tumor cells as organoids prior to embedding in 3 mg/ml collagen gels, the optimum composition for premalignant cell invasion, in the bioreactor. As with premalignant organoids, cultures were fixed and stained after 2 days. From these studies we found that ECM stiffness was not necessary to induce tumor cell invasion but did accelerate organoid dissociation (Fig. 1F and G).
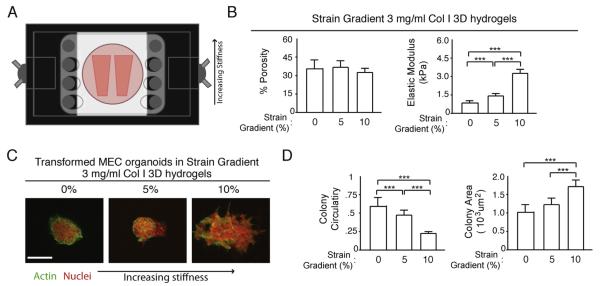
Prior work suggests that the structural heterogeneity of native tissue may create gradients in ECM stiffness, which promotes morphogenetic processes such as branching morphogenesis and pathologies such as cancer (Guo et al., 2012; Isenberg et al., 2009; Lopez et al., 2011). To address this possibility, we leveraged the unique mechanical loading principle of our system and designed an alternative PDMS membrane to allow for generation of ECM stiffness gradients. This was achieved by modifying the PDMS membrane connections to the loading apparatus by stepwise increases in the major axis length of each set of connections across the width of the membrane, consequently decreasing the maximum possible strain and mechanical loading of the hydrogel in a gradient fashion (Fig. 2A). Testing this modification with a 3 mg/ml Col I hydrogel, we can demonstrate with AFM and SEM that we are able to create a gradient of ECM stiffness ranging from (0.4–4 kPa, 0.12 kPa/mm) independently of structural changes (Fig. 2B). To illustrate a biological application of the gradient mechanical loading tension bioreactor, we again used oncogenically transformed (Ha-Ras) mammary epithelial cell organoids embedded in a Col I hydrogel (3 mg/ml). Organoids were fixed, stained, and imaged as described in uniform stiffness experiments. ECM stiffness for a given gel region was determined by measuring the length of the gel in the direction of the applied strain relative to the initial length to calculate the local strain and then fit to AFM elastic modulus measurements for that specific strain.
Fig. 2.
Characterization and biological application of gradient tension bioreactor. (A) Schematic of gradient strain tension bioreactor. (B) Quantification of pore size based on SEM imaging (not shown) and elastic modulus across strain gradient (error bars represent standard deviation, *** denotes p < 0.05 evaluated by pairwise t-test). (C) Premalignant mammary epithelial cells pre-grown in rBM as spherical multicellular organoids embedded in gradient stiffness Col I hydrogels. After two days cultures were fixed and stained for actin cytoskeleton and nuclei to assess the extent of tumor cell invasion and migration (scale bar = 20 μm). (D) Quantification of organoid spread area and circularity.
Consistent with our previous results in uniform-stiffness collagen gels, increasing ECM stiffness potentiates tumor cell migration. Yet, in our gradient system, we can also observe ranges of cell behavior within the same hydrogel in response to increasing stiffness (Fig. 2C–D). These data show that we have generated a tractable system for creating gradients of mechanical stiffness in collagen hydrogels without altering ECM structure or organization.
In conclusion, we have outlined a new strategy for the design and implementation of a 3D bioreactor that can be used to accurately manipulate the stiffness of type I collagen hydrogels without changing substrate concentration or altering pore size. The system also can be adopted to generate shallow gradients of ECM stiffening in 3D. We have described the validation of our system and demonstrated how it can be used to study malignant transformation and the invasive and migratory phenotype of tumor cells. Importantly, the system is amenable for rapid incorporation into research programs aimed at clarifying the impact of ECM stiffness on tissue morphogenesis, wound healing, and a range of other tissue functions.
Acknowledgments
We wish to thank Dr. Jan Liphardt Stanford University for helpful suggestions. Work was supported by NIH F31CA183255 to LC, NSF GRFP DGE 1144247 and NIH F31CA180422 to YAM, NSF GRFP DGE 1106400 to GO, NIH R01 CA138818, DoD W81XWH-13-1-0216, NIH U01ES019458, and NIH R01 CA085492 to VW.
References
- Engler AJ, Sen S, Sweeney HL, Discher DE. Matrix elasticity directs stem cell lineage specification. Cell. 2006 Aug;126(4):677–689. doi: 10.1016/j.cell.2006.06.044. (print) [DOI] [PubMed] [Google Scholar]
- Gautieri A, Vesentini S, Redaelli A, Buehler MJ. Hierarchical structure and nanomechanics of collagen microfibrils from the atomistic scale up. Nano Lett. 2011 Jan;11(2):757–766. doi: 10.1021/nl103943u. http://dx.doi.org/10.1021/nl103943u. ACS, Web. [DOI] [PubMed] [Google Scholar]
- Guo C-L, Ouyang M, Yu J-Y, Maslov J, Price A, Shen C-Y. Long-range mechanical force enables self-assembly of epithelial tubular patterns. Proc. Natl. Acad. Sci. U. S. A. 2012 Apr;109(15):5576–5582. doi: 10.1073/pnas.1114781109. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeger A, Krause M, Wolf K, Friedl P. Cell jamming: collective invasion of mesenchymal tumor cells imposed by tissue confinement. Biochim. Biophys. Acta. 2014 Aug;1840(8):2386–2395. doi: 10.1016/j.bbagen.2014.03.020. http://dx.doi.org/10.1016/j.bbagen.2014.03.020, Epub 2014 Apr 8 (print) [DOI] [PubMed] [Google Scholar]
- Isenberg BC, Dimilla PA, Walker M, Kim S, Wong JY. Vascular smooth muscle cell durotaxis depends on substrate stiffness gradient strength. Biophys. J. 2009 Sep;97(5):1313–1322. doi: 10.1016/j.bpj.2009.06.021. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, Fong SF, Csiszar K, Giaccia A, Weninger W, Yamauchi M, Gasser DL, Weaver VM. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009 Nov;139(5):891–906. doi: 10.1016/j.cell.2009.10.027. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez JI, Kang I, You W-K, McDonald DM, Weaver VM. In situ force mapping of mammary gland transformation. Integr. Biol. (Camb.) 2011 Sep;3(9):910–921. doi: 10.1039/c1ib00043h. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu P, Takai K, Weaver VM, Werb Z. Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb. Perspect. Biol. 2011 Dec;3(12) doi: 10.1101/cshperspect.a005058. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JS, Colette JS, Wesley RL, Jan DB, Brandon LB, Christopher SC. Bioactive hydrogels made from step-growth derived PEG-peptide macromers. Biomaterials. 2010 May;31(13):3736–3743. doi: 10.1016/j.biomaterials.2010.01.058. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miroshnikova YA, Jorgens DM, Spirio L, Auer M, Sarang-Sieminski AL, Weaver VM. Engineering strategies to recapitulate epithelial morphogenesis within synthetic three-dimensional extracellular matrix with tunable mechanical properties. Phys. Biol. 2011 Apr;8(2):026013. doi: 10.1088/1478-3975/8/2/026013. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouw JK, Yui Y, Damiano L, Bainer RO, Lakins JN, Acerbi I, Ou G, Wijekoon AC, Levental KR, Gilbert PM, Hwang ES, Chen Y-Y, Weaver VM. Tissue mechanics modulate MicroRNA-dependent PTEN expression to regulate malignant progression. Nat. Med. 2014 Apr;20(4):360–367. doi: 10.1038/nm.3497. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paszek MJ, Zahir N, Johnson KR, Lakins JN, Rozenberg GI, Gefen A, Reinhart-King CA, Margulies SS, Dembo M, Boettiger D, Hammer DA, Weaver VM. Tensional homeostasis and the malignant phenotype. Cancer Cell. 2005 Sep;8(3):241–254. doi: 10.1016/j.ccr.2005.08.010. (print) [DOI] [PubMed] [Google Scholar]
- Provenzano PP, Inman DR, Eliceiri KW, Keely PJ. Matrix density-induced mechanoregulation of breast cell phenotype, signaling and gene expression through a FAK-ERK linkage. Oncogene. 2009 Dec;28(49):4326–4343. doi: 10.1038/onc.2009.299. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provenzano PP, Eliceiri KW, Inman DR, Keely PJ. Engineering three-dimensional collagen matrices to provide contact guidance during 3D cell migration. Curr. Protoc. Cell Biol. 2010 doi: 10.1002/0471143030.cb1017s47. Chapter 10: Unit 10.17 (June) (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubashkin MG, Cassereau L, Bainer R, Dufort CC, Yui Y, Ou G, Paszek MJ, Davidson MW, Chen YY, Weaver VM. Force engages vinculin and promotes tumor progression by enhancing PI3K activation of phosphatidylinositol (3,4,5)-triphosphate. Cancer Res. 2014 Sep 1;74(17):4597–4611. doi: 10.1158/0008-5472.CAN-13-3698. http://dx.doi.org/10.1158/0008-5472.CAN-13-3698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider CA, Rasband WS, Eliceiri KW. NIH image to ImageJ: 25 years of image analysis. Nat. Methods. 2012 Jun;9(7):671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tse JR, Engler AJ. Preparation of hydrogel substrates with tunable mechanical properties. Curr. Protoc. Cell Biol. 2010 doi: 10.1002/0471143030.cb1016s47. Chapter 10: Unit 10.16 (June) (print) [DOI] [PubMed] [Google Scholar]
- Ulrich TA, Jain A, Tanner K, MacKay JL, Kumar S. Probing cellular mechanobiology in three-dimensional culture with collagen-agarose matrices. Biomaterials. 2010 Mar;31(7):1875–1884. doi: 10.1016/j.biomaterials.2009.10.047. (print) [DOI] [PubMed] [Google Scholar]
- Wipff P-J, Majd H, Acharya C, Buscemi L, Meister J-J, Hinz B. The covalent attachment of adhesion molecules to silicone membranes for cell stretching applications. Biomaterials. 2009 Mar;30(9):1781–1789. doi: 10.1016/j.biomaterials.2008.12.022. (print) [DOI] [PubMed] [Google Scholar]
- Wolf K, Te Lindert M, Krause M, Alexander S, Te Riet J, Willis AL, Hoffman RM, Figdor CG, Weiss SJ, Friedl P. Physical limits of cell migration: control by ECM space and nuclear deformation and tuning by proteolysis and traction force. J. Cell Biol. 2013 Jun;201(7):1069–1084. doi: 10.1083/jcb.201210152. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada KM, Cukierman E. Modeling tissue morphogenesis and cancer in 3D. Cell. 2007 Aug;130(4):601–610. doi: 10.1016/j.cell.2007.08.006. (print) [DOI] [PubMed] [Google Scholar]
- Young JL, Engler AJ. Hydrogels with time-dependent material properties enhance cardiomyocyte differentiation in vitro. Biomaterials. 2011 Feb;32(4):1002–1009. doi: 10.1016/j.biomaterials.2010.10.020. (print) [DOI] [PMC free article] [PubMed] [Google Scholar]