Abstract
Atraumatic instability or microinstability of the hip is a recognized cause of groin pain and hip instability. Risk factors include female sex, ligamentous laxity, and borderline dysplasia. Arthroscopically, the joint may distract easily, and there may be associated ligamentum teres tears and laxity of the capsule on manual probing. The use of arthroscopic capsular plication in this cohort of patients has shown good to excellent results. Biomechanically, a capsular plication aims to create an imbrication and inferior shift of the capsule to augment the screw-home mechanism of the capsuloligamentous structures and thereby improve stability in extension and external rotation. The purpose of this article is to detail the step-by-step surgical technique of arthroscopic capsular plication, in addition to the indications, pearls, and pitfalls of the technique.
Hip arthroscopy requires a detailed understanding of the stabilizers of the hip joint to adequately treat the symptoms of instability and to avoid iatrogenic complications. In addition to inherent bony stability, static and dynamic soft-tissue stabilizers are important in maintaining hip joint congruity throughout a physiological and supraphysiological range of motion.1,2 The leash-like fibers of the zona orbicularis and anterior capsular ligaments form a spiral configuration that tightens in a screw-home mechanism during terminal extension and external rotation, stabilizing the joint.3 As the hip moves into flexion, the fibers unwind and loosen, rendering the joint less stable. From a biomechanical standpoint, capsulotomy in hip arthroscopic procedures could theoretically have an adverse effect on joint stability.4 Routine capsular repair may mitigate this adverse effect, restoring the normal capsular stability. Furthermore, in cases of ligamentous laxity or microinstability, tightening of the capsuloligamentous structures may reinforce the screw-home mechanism and help restore stability.5
The main indication for capsular plication is treatment of hip instability. Table 1 summarizes the indications for capsulotomy/capsulectomy, capsular closure, and capsular plication. Atraumatic hip instability is a diagnosis that is increasingly being recognized and clinically defined. It occurs with damage to the anterior capsular stabilizers, particularly the iliofemoral ligament, with repetitive rotation and axial loading of the hip joint.3 The capsule undergoes plastic deformation, and patients commonly present with groin pain and the sensation of the joint giving way anteriorly with extension and external rotation activities. On examination, patients may have signs of generalized ligamentous laxity and positive apprehension signs.6 Associated radiologic features may include acetabular dysplasia, defined as a lateral center-edge angle (LCEA) of less than 25°7 and/or an acetabular index of greater than 12°.8 Domb and colleagues9 defined a “stability index” that found that ligamentum teres tears (a marker of hip instability) were associated with a lower LCEA and higher inclination of the acetabular sourcil in hips without retroversion. On magnetic resonance imaging, there may be features of capsular redundancy.3
Table 1.
Clinical, Radiologic, and Arthroscopic Factors That Influence Need for Capsulotomy/Capsulectomy, Capsular Closure, or Capsular Plication
| Factor | Capsulotomy/Capsulectomy | Capsular Closure | Capsular Plication |
|---|---|---|---|
| Clinical | |||
| History | Conditions causing capsular contracture and stiffness (e.g., adhesive capsulitis, synovial proliferative disorders, or rheumatologic conditions) | Athletes or female patients | History of capsular plication of another joint |
| ROM | Decreased | Normal | Normal/supraphysiological |
| Ligamentous laxity | Negative | Negative | Positive |
| Neuromuscular dysfunction | Negative | Negative | Positive |
| Apprehension signs | Negative | Negative | Positive |
| Radiographic | |||
| CEA, ° | >30 | 25-30 | <25 |
| AI, ° | >12 | >12 | <12 |
| MRI | Capsular redundancy, ligamentum teres tears, or hypertrophy | ||
| Arthroscopic | |||
| Intraoperative joint distraction | Limited | Easy | Positive intraoperative vacuum sign |
| Manual probing | Capsular hypertrophy Thickening Reduced compliance on probing Synovitis |
Ligamentum teres tear Normal appearance of synovium Normal capsular compliance Sufficient capsule remaining to allow appropriate tensioned closure Concern for excessive acetabular rim recession |
Capsular redundancy on manual probing Weakened thin capsule Ligamentum teres tear |
AI, acetabular index; CEA, center-edge angle; MRI, magnetic resonance imaging; ROM, range of motion.
The aim of a capsular plication is to create an imbrication and inferior shift in the capsule that augment the screw-home mechanism of the hip by accentuating the spiral orientation of the capsular fibers. This increases the degree to which the capsule tightens in extension. The combination of an imbrication and inferior shift increases the tightness of the capsule in both external rotation and extension and thus diminishes potential anterior instability in that position. An understanding of the indications and techniques of capsular plication will help improve the outcomes of hip arthroscopy. The purpose of this article is to describe our surgical technique for capsular plication.
Technique
The patient is placed supine on a hip traction table with the feet secured in well-padded boots and a large well-padded perineal post abutting the medial thigh. The operative extremity is placed in neutral abduction and slight flexion, with 15° of internal rotation of the foot. The operative extremity is prepared and draped in standard fashion. Safe access to the hip joint to minimize damage to the labrum and femoral head is performed as previously described by Domb et al.10 Anterolateral and modified anterior portals are established. A distal lateral anterior portal is established 2 cm distal to the midanterior portal to allow for suture management. A capsulotomy is performed with a beaver blade, incising the capsule parallel to the acetabular rim from the 12- to 3-o'clock position, connecting the 2 portals. A diagnostic arthroscopy is performed consisting of a circumferential examination of the entire labrum and central compartment. Particular attention is given to patterns of injury suggestive of instability. These may include easy joint distraction with minimal force; a positive intraoperative vacuum sign; labral or ligamentum teres hypertrophy; capsular redundancy or laxity on manual probing; a weakened, thin capsule; or associated ligament tears or insufficiency.9 Intra-articular procedures to treat labral tears, ligamentum teres tears, femoroacetabular impingement, and cartilage damage are performed as indicated. At the end of the procedure, the capsule is tightened.
Capsular Plication
For patients with microinstability of the hip, capsular plication is performed at the conclusion of all intracapsular procedures. Traction is released from the operative extremity, and the hip is flexed to 45°. A disposable cannula (Arthrex, Naples, FL) is introduced through the midanterior portal. A SutureLasso (Arthrex) is passed through the midanterior portal and is used to pass a suture loop through the capsule on the proximal side of the capsulotomy from superficial to deep (Table 2). A BirdBeak penetrator (Arthrex) is then used to retrieve the lasso through the capsule on the distal side of the capsulotomy near the zona orbicularis and is brought out through the distal lateral anterior portal (Fig 1). A suture (No. 1 Vicryl; Johnson & Johnson, New Brunswick, NJ) is passed through the SutureLasso and delivered through both limbs of the capsulotomy through the midanterior portal. One of the limbs of the suture is retrieved with a grasper (Smith & Nephew, Memphis, TN) so that both limbs of the suture exit through 1 portal. A capsular plication differs from a standard closure in that the sutures are passed in such a fashion that larger bites of the capsule are taken on the distal side, passing the suture through the zona orbicularis itself. Taking larger bites leads to imbrication of the capsule, increasing the tightness of the capsule in external rotation. Furthermore, the location of the suture passage through the zona orbicularis is more medial than the corresponding point of passage of the same suture on the proximal side of the capsule. When the sutures are tied outside of the capsule, this produces an inferior capsular shift (Fig 2). In contrast to capsular closure, which uses 1 to 2 stitches, a total of between 3 and 5 stitches are used for capsular plication. The hip is then brought into extension while the surgeon is watching the capsular closure to ensure that the capsule has not been over-tightened (Fig 3). The capsule is closed using a standard arthroscopic knot-tying technique (Video 1).
Table 2.
Pearls and Pitfalls of Capsular Plication
| Pearls |
| Adequate capsular tissue should be retained from the proximal origin adjacent to the acetabulum. |
| A SutureLasso can aid subsequent retrieval without inadvertent SutureLasso removal. |
| Frequent dynamic examination can aid in the assessment of adequate tension. |
| Sutures should be tied with the joint in a reduced position. |
| A cannula should be placed just outside the capsule to prevent a “soft-tissue bridge” when performing blind arthroscopic knot tying. |
| Pitfalls |
| Insufficient tissue can compromise the plication or lead to an over-tensioned construct. |
| Closure in flexion may lead to suture cutout when the hip is extended. |
Fig 1.
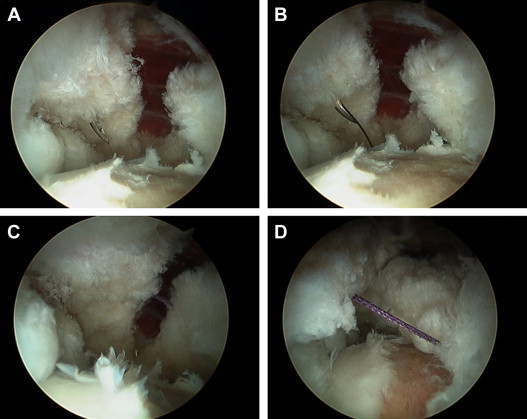
Passage of sutures through hip capsule. The patient is placed in the supine position on an arthroscopic traction table. The hip capsule is viewed from the anterolateral portal. (A) A SutureLasso is passed through the proximal hip capsule from superficial to deep from the midanterior portal. (B) The loop within the SutureLasso is advanced 1 to 2 cm under arthroscopic vision. (C) The lasso is retrieved using the BirdBeak penetrator through the capsule distally and brought out through the distal lateral anterior portal. (D) A suture (No. 1 Vicryl) is placed through the loop and through both limbs of the capsule using the lasso as a shuttle. One of the limbs is retrieved through one of the anterior portals so that both limbs exit through the same portal to facilitate arthroscopic knot tying.
Fig 2.
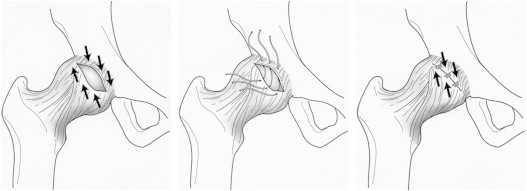
Steps involved in creating capsular plication by imbrication and shifting of capsule inferiorly. Larger bites of the capsule are taken on the distal side, passing the suture through the zona orbicularis itself. Taking larger bites leads to imbrication of the capsule, increasing the tightness of the capsule in external rotation. The location of the suture passage through the zona orbicularis is more medial than the corresponding point of passage of the same suture on the proximal side of the capsule. When the sutures are tied outside of the capsule, this produces an inferior capsular shift.
Reprinted with permission.5
Fig 3.
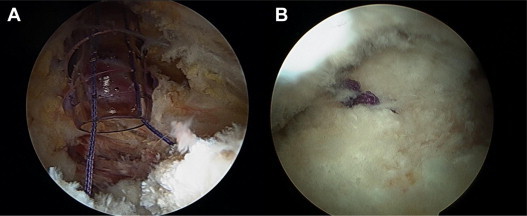
Closure of hip capsule. (A) The hip capsule is closed with the cannula placed outside the capsule. (B) This prevents a soft-tissue bridge when tying the capsule arthroscopically.
Postoperative Rehabilitation
The postoperative rehabilitation is tailored to the patient and the specific concomitant arthroscopic procedures performed in addition to the capsular plication. Typically, weight bearing is restricted for 2 weeks, with patients instructed to maintain 20 lb of heel-touch weight bearing. A hip brace (DJO Global, San Diego, CA) is used to limit range of motion to 90° of flexion for the first 2 weeks. Range of motion is then allowed to progress within a pain-free zone. Therapy is advanced when the patient is fully weight bearing and achieves full range of motion. Gentle strengthening exercises begin with a stationary bicycle and isometrics. As strengthening progresses, patients start using an elliptical machine and slide board and perform hip girdle (gluteus medius) strengthening. Specific to capsular plication, patients are instructed to avoid combined extension and external rotation, joint mobilization, or over-stretching range-of-motion exercises and prone range-of-motion exercises for 6 weeks.
Discussion
We have described a technique for arthroscopic capsular plication for the management of microinstability of the hip. As outlined in this article, the risk factors for microinstability of the hip include female sex, ligamentous laxity, and supraphysiological range of motion. Plain radiographic findings may include an LCEA of 25° or less and an acetabular index of greater than 12°. Arthroscopic findings include easy joint distractibility, capsuloligamentous laxity on capsular probing, and ligamentum teres tears. The capsular plication technique that we have described aims to improve the stability of the hip by accentuating the screw-home mechanism of the capsuloligamentous structures.
The senior author (B.G.D.) has previously published on the outcomes of this technique in patients with an LCEA between 18° and 25°.11 This case series reported on the results of capsular plication and labral preservation in 22 patients with a mean length of follow-up of 27.5 ± 5.5 months. The authors reported significant improvements in 4 patient-reported outcome scores and visual analog pain scores. The overall patient satisfaction rating was 8.4 of 10, and 77% of patients had good to excellent results. The authors concluded that patients with borderline dysplasia who may have symptoms of microinstability had favorable results at 2 years' follow-up with an arthroscopic technique that included labral repair augmented with capsular plication with an inferior shift. In this article we have detailed the operative steps to achieve capsular plication.
Thermal capsulorrhaphy is another alternative to suture plication for arthroscopic capsular tightening. Philippon12,13 has reported on a number of elite professional athletes who have returned to a high level of competition after thermal capsulorrhaphy for symptomatic hip instability. The adverse effects of capsulorrhaphy, such as thermal necrosis, chondrolysis, and capsular attenuation, though reported in the shoulder, have not yet been reported in the hip.14
Although the focus of this article is the capsular management of atraumatic hip instability, inadequate capsular management with adequate restoration of soft-tissue function in at-risk patients may be a cause of iatrogenic microinstability. In one published series, 35% of patients with refractory pain after arthroscopy had unaddressed instability.15 To prevent such complications, it is important to identify clinical and arthroscopic signs of atraumatic instability as outlined earlier. Arthroscopic intervention should not compromise bony and soft-tissue constraints. Specifically, acetabular resection should be minimal, an uncompromised labral seal should be achieved, and the screw-home mechanism of the capsuloligamentous structures should be reinforced.
In summary, our technique to achieve a capsular plication by imbrication and shifting of the capsule inferiorly is reproducible and may reinforce the screw-home mechanism to promote joint stability. Along with appropriate and measured bony resection and restoration of the labral seal, capsular plication when indicated may help improve outcomes after hip arthroscopy for patients with microinstability.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.G.D. receives support from American Hip Institute (AHI): board member and research support. Arthrex: research support to AHI/consulting/ royalties. MAKO Surgical and Pacira: research support to AHI/consulting. Breg and ATI: research support to AHI. Stryker: stock owned. Orthomerica and DJO Global: royalties.
Supplementary Data
A SutureLasso is passed through the proximal leaf of the capsulotomy and retrieved with a BirdBeak penetrator through the distal leaf. The bites of capsular tissue on the distal leaf are larger and more medial than those on the proximal side. When the sutures are tied outside of the capsule, this produces an inferior capsular shift. A total of between 3 and 5 stitches are used. The sutures are tied in extension to avoid over-tightening.
References
- 1.Elkins J.M., Stroud N.J., Rudert M.J. The capsule’s contribution to total hip construct stability—A finite element analysis. J Orthop Res. 2011;29:1642–1648. doi: 10.1002/jor.21435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Myers C.A., Register B.C., Lertwanich P. Role of the acetabular labrum and the iliofemoral ligament in hip stability: An in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39:85S–91S. doi: 10.1177/0363546511412161. (suppl) [DOI] [PubMed] [Google Scholar]
- 3.Shindle M.K., Ranawat A.S., Kelly B.T. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med. 2006;25:309–326. doi: 10.1016/j.csm.2005.12.003. ix-x. [DOI] [PubMed] [Google Scholar]
- 4.Sansone M., Ahlden M., Jonasson P., Sward L., Eriksson T., Karlsson J. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21:420–423. doi: 10.1007/s00167-012-2300-3. [DOI] [PubMed] [Google Scholar]
- 5.Domb B.G., Philippon M.J., Giordano B.D. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: Relation to atraumatic instability. Arthroscopy. 2013;29:162–173. doi: 10.1016/j.arthro.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 6.Shu B., Safran M.R. Hip instability: Anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30:349–367. doi: 10.1016/j.csm.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Wiberg G. Studies of acetabular and congenital subluxation of the hip joint with special reference to complication of osteoarthritis. Acta Chir Scand. 1939;83(suppl 58) [Google Scholar]
- 8.Lequesne M., de Seze S. Le faux profil du bassin. Nouvelle incidence radiographique pour l’étude de la hanche. Son utilité dans les dysplasies et les differentes coxopathies. Rev Rhum. 1961;28:643–652. [Google Scholar]
- 9.Botser I, Martin DE, Domb BG. Relationship between tears of the ligament teres and acetabular undercoverage: Does microinstability play a role? Presented at the 2011 International Society of Hip Arthroscopy Meeting, Paris, France, September 2011.
- 10.Domb B., Hanypsiak B., Botser I. Labral penetration rate in a consecutive series of 300 hip arthroscopies. Am J Sports Med. 2012;40:864–869. doi: 10.1177/0363546512437152. [DOI] [PubMed] [Google Scholar]
- 11.Domb B.S., Stake C.E., Linder D., El-Bitar Y., Jackson T.J. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: Two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41:2591–2598. doi: 10.1177/0363546513499154. [DOI] [PubMed] [Google Scholar]
- 12.Philippon M.J. The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med. 2001;20:817–829. doi: 10.1016/s0278-5919(05)70287-8. [DOI] [PubMed] [Google Scholar]
- 13.Philippon M.J. New frontiers in hip arthroscopy: The role of arthroscopic hip labral repair and capsulorrhaphy in the treatment of hip disorders. Instr Course Lect. 2006;55:309–316. [PubMed] [Google Scholar]
- 14.Wong K.L., Williams G.R. Complications of thermal capsulorrhaphy of the shoulder. J Bone Joint Surg Am. 2001;83:151–155. doi: 10.2106/00004623-200100022-00013. (suppl 2, pt 2) [DOI] [PubMed] [Google Scholar]
- 15.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A SutureLasso is passed through the proximal leaf of the capsulotomy and retrieved with a BirdBeak penetrator through the distal leaf. The bites of capsular tissue on the distal leaf are larger and more medial than those on the proximal side. When the sutures are tied outside of the capsule, this produces an inferior capsular shift. A total of between 3 and 5 stitches are used. The sutures are tied in extension to avoid over-tightening.


