Abstract
Objective
This meta-analysis is to evaluate the overall diagnostic yield and accuracy of electromagnetic navigation bronchoscopy (ENB)-based targeted biopsies in detecting peripheral lesions.
Methods
A systematic search in PubMed was performed using “electromagnetic navigation bronchoscopy” crossed with “peripheral lesions” and “lung nodules”. Test performance characteristics with the use of forest plots, summary receiver operating characteristic curves (SROCs) and bivariate random effects were summarized using Meta-Disc software. Adverse events and complications were recorded if reported.
Results
A total of 17 studies (1,106 patients with peripheral lung lesions) were included in this analysis. The pooled sensitivity, specificity, positive likelihood ratios (PLRs), negative likelihood ratios (NLRs), and diagnostic odds ratios (DORs) of ENB was 82%, 100%, 19.36, 0.23, and 97.62, respectively. The area under the curve (AUC) for the SROC was 0.9786. No procedure-related complication was found.
Conclusions
ENB is an effective and safe procedure in diagnosing peripheral lung lesions.
Keywords: Electromagnetic navigation bronchoscopy (ENB), lung nodules, diagnostic yield, meta-analysis
Introduction
Lung cancer is maintaining as the leading cause of cancer mortality worldwide (1). A low cure rate of lung cancer is not only attributed to intrinsic aggressive biological behavior, but also little attention to lung cancer screening. A large number of patients with lung cancers present locally advanced or metastatic disease when diagnosed. Since then, early detection of small lung nodules is urgently needed, and may improve lung cancer mortality (2). And the cure rate for lung cancer in stage I is 70% (3).
Current methods of diagnosing lung cancer are limited by several factors, such as the size, location, and morphology of the suspected lesion, the presence of metastasis, and the clinical history and status of the patient. Although surgical biopsy and resection is the best option for the treatment of malignancy, the probability of malignancy is uncertain, and moreover, some high-risk cases are not suitable for surgery. In this respect, computed tomography (CT) screening programs are widely recommended for a large number of potentially resectable small lung nodules can be identified by CT scanning. However, the high frequency of using CT scanning in cardiopulmonary disease is accompanied with high proportion of false-positive CT findings, reaching to 70% (4), which requires further histological confirmation. In addition, CT screening is advent for a significant number of lung cancer patients, who may be medically inoperable due to comorbid medical illness or poor pulmonary function (5,6).
Diagnosis of peripheral pulmonary lesions (PPL) is more challenging, since PPLs account for 25-30% of all lung cancers and are defined as lesions located beyond the segmental bronchus that are less than 2 cm in diameter (7). Although the flexible bronchoscopy is the least invasive diagnostic tool available to the clinician, the value of this conventional bronchoscopy is limited by the size and location of the lesions of interest. The diagnostic yield of the flexible bronchoscopy for peripheral lung nodules is low, ranging from 14% to 62% (8), highly dependent on the size and location of lung lesions. In these cases, other modalities such as CT-guided biopsy can help determine the malignancy of peripheral lung nodules. However, this modality is generally applicable to lung lesions located in the outer third of the lung, and more severely, led to high occurrence of pneumothorax in patients with advanced chronic obstructive pulmonary disease (9,10). Hence, a guided endoscopic approach may be the best alternative approach for patients with lung nodules. To this end, electromagnetic navigation bronchoscopy (ENB) is a promising option in the diagnosis of lung nodules.
ENB, a newly developed technology, is recognized as an ideal platform to biopsy, localize, and even mark the small peripheral lesions for treatment (11). More importantly, ENB has allowed thoracic surgeons not only to localize these small deep lesions but to biopsy these lesions intra-operatively when combined with rapid on-site cytological evaluation (ROSE) (12). The ENB system consists of four essential components, which are (I) computer software that creates a three-dimensional (3D) and virtual bronchoscopy reconstruction from CT-scan data of patients airways; (II) an electromagnetic location board generating a low-dose magnetic field surrounding the patients’ chest; (III) a sensor probe that located in the electromagnetic field to guide a steerable endoscopic probe to peripheral lung lesions; and (IV) an extended working channel that enables the placement of the bronchoscopic tools to biopsy the lung periphery (5).
This minimally invasive approach for sampling a peripheral lung nodule has not been well confirmed. The diagnostic yields with ENB were inconsistently reported in different research group, After Gex et al. released a meta-analysis on the evaluation of ENB for lung nodules (8), four more manuscripts were released to report the utility of ENB for the diagnosis yield of peripheral lung lesions (7,13-15). Hence, in this study, we updated the meta-analysis to assess the diagnosis accuracy and safety of ENB for the peripheral lung nodules.
Materials and methods
Data sources
A total of 145 literatures were found after the key words, “electromagnetic navigation bronchoscopy”, “bronchoscopy”, “peripheral nodule” or “lung cancer” were used to search on the PubMed database from 2000 to 2015. The search was limited to human subjects and to English language studies.
Study selection
Review and editorial articles were excluded from the meta-analysis, but the reference lists of these papers were searched manually for additional relevant articles. Studies were included in this meta-analysis when it met the following criteria: (I) each trial enrolling more than ten patients; (II) the diagnostic yield of ENB was reported for peripheral lung nodules or lesions without any restriction; (III) the enrolled patients with peripheral nodules were confirmed by radiographic evidence.
Data extraction and quality assessment
Two investigators independently reviewed the enrolled manuscripts for eligible articles and extracted the data using a standardized form. Disagreements were solved through discussion with the third person to reach a consensus. Further, the quality of included studies was assessed with the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool, consisting of four key domains: patient selection, index test, reference standard, and the flow and timing. The data for each study was entered in the RevMan (Version 5.3, the Cochrane Collaboration), and the methodological quality graph was constructed for all the included studies.
The following data from each study: (I) publication details (title, authors, and other citation details); (II) type of study (prospective or retrospective); (III) exact criteria of inclusion in the study; (IV) type of sedation used and number of biopsies taken; (V) data necessary for diagnostic meta-analysis, such as the number of lesions and the number of diagnoses obtained; (VI) major and minor complications associated with procedure; (VII) reference tests and follow-up duration. The primary outcome was diagnostic yield. ENB success (true positive) was defined as a definitive malignant diagnosis that was yielded by ENB biopsy. When the benign diagnosis was initially yielded by ENB biopsy, which was confirmed by the follow-up treatment, it was also considered as ENB success (true negative). ENB failure represented as an ENB biopsy that yielded a non-diagnostic or a benign diagnosis was overturned when follow-up yielded a malignant diagnosis (false negative).
Statistical analysis
Standard methods recommended for meta-analyses of diagnostic accuracy studies were used (16). All analyses were performed using Meta-DiSc 1.4 (Cochrane Colloquium, Barcelona, Spain) and RevMan (version 5.3). The diagnostic accuracy of ENB was determined by calculating the sensitivity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), and diagnostic odds ratio (DOR) for each study. Sensitivity analyses, conducted to check the robustness of the results, were pooled using the fixed effects model, and the PLR, NLR and DOR were pooled using the DerSimonian-Laird random effects model to derive a pooled estimate with 95% confidential index (CI). In addition, a summary receiver operating characteristic curve (SROC) was constructed using the random effects model. Heterogeneity, measuring the extent of inconsistency among the results of the studies, was assessed by the indicator I2. The Cochran Q test was used to find potential heterogeneity factors. All statistical tests were two-sided, and significance was set as P<0.05.
Sensitivity analysis was determined by using the following subgroups, which were considered as potential sources of heterogeneity: (I) prospective vs. retrospective studies; and (II) studies with small or large sample size (small sample defined as studies with less than 25 selected participants); (III) type of sedation; (IV) whether or not the fluoroscopy was used; and (V) whether or not the ROSE was used.
Results
Study selection
A total of 145 studies were yielded after systematic database searches. Following two investigators reviewing, 121 papers were excluded for not meeting the inclusion criteria. Finally, 17 papers on the diagnostic yield and safety of ENB in lung nodules were included in present meta-analysis (7,13-15,17-31). The flow of search strategy is showed in Figure 1.
Figure 1.
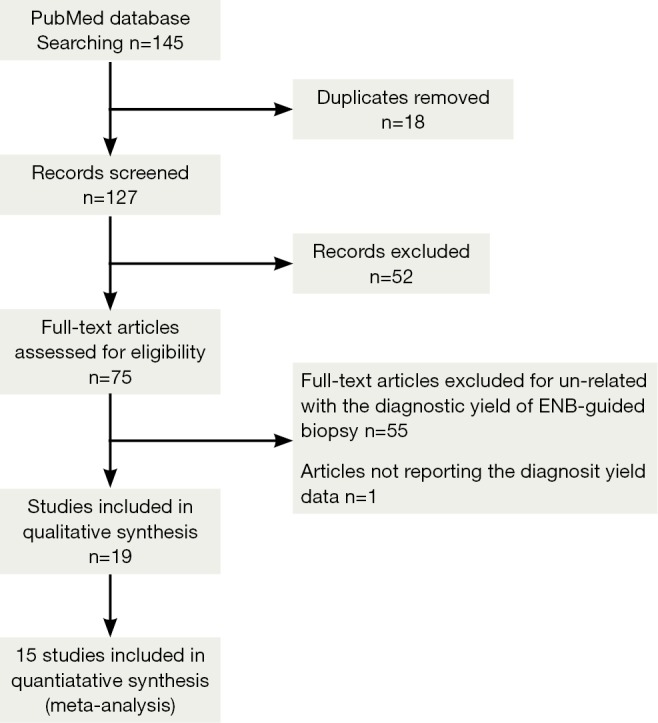
Flow diagram.
Study description
Main demographics of selected patients were depicted in Table 1. A total of 1,161 lung nodules or masses in 1,106 patients were enrolled. The SuperDimension ENB system was used in all studies. Additional techniques or strategies were used in several studies to enhance performance, such as fluoroscopy, endobronchial ultrasound (EBUS) radial probe, ROSE, which were summarized in Table 2.
Table 1. Main characteristics of the enrolled studies.
| Study (first author) | Pro/retro | Patients selection | Participants, n (M/F) | Mean age (years) | No. of lung nodules | Mean diameter (mm) |
|---|---|---|---|---|---|---|
| Becker, 2005 (18) | Pro | PPL beyond the field of FB, regardless of lesion size | 30 (23/7) | 65.00 | 30 | 39.8 |
| Hautmann, 2005 (17) | Pro | PPL beyond the field of FB | 16 (10/6) | 63.70 | 16 | ND |
| Gildea, 2006 (19) | Pro | PPL difficult to reach with standard bronchoscopic technique | 58 (35/23) | 67.91 | 54 | 22.8 |
| Schwarz, 2006 (20) | Pro | PPL beyond the field of FB, regardless of lesion size | 13 | ND | 13 | 33.5 |
| Wilson, 2007 (21) | Retro | PPL difficult to reach using a standard bronchoscopic approach | 222 (112/110) | 63.1. | 271 | 21.0 |
| Makris, 2007 (24) | Pro | PPL located beyond the visible range of FB; suspicion of cancer by CT/PET scan; suggestive malignancy, after TTNA and MLN-TBNA, high-risk surgery | 40 (30/10) | 60.00 | 25 | 23.5 |
| Eberhardt, 2007 (23) | Pro | PPL beyond the field of FB | 89 (50/39) | 67.00 | 93 | 24.0 |
| Eberhardt, 2007 (a) (22) | Pro | PPL beyond the field of FB | 39 (20/19) | 55.00 | 39 | 28.0 |
| Eberhardt, 2007 (b) (22) | Pro | PPL beyond the field of FB | 40 (25/15) | 51.00 | 40 | 24.0 |
| Bertoletti, 2009 (25) | Pro | PET-positive PPL beyond the field of FB, high-risk surgery | 54 (47/7) | 67.00 | 54 | 31.2 |
| Lamprecht, 2009 (26) | Retro | PPL beyond the field of FB and/or too small to be visible on fluoroscopy | 13 (10/3) | 64.20 | 13 | 30.0 |
| Eberhardt, 2010 (27) | Pro | Referral for small PPL suggestive of malignancy | 54 (40/14) | 65.10 | 55 | 23.3 |
| Seijo, 2010 (28) | Pro | PPL, straightforward surgery or TTNA deemed suboptimal | 51 (37/14) | 62.00 | 51 | 25.0 |
| Mahajan, 2011 (29) | Retro | PPL beyond the field of FB, high-risk surgery | 48 | ND | 49 | 20.0 |
| Brownback, 2012 (13) | Retro | PPL not accessible by conventional bronchoscopy | 55 (33/22) | 63.00 | 55 | 30.0 |
| Jensen, 2012 (14) | Retro | 20 consecutive performed ENB cases in 5 institutions | 92 (44/48) | 67.00 | 92 | 26.1 |
| Lamprecht, 2012 (30) | Pro | PPL beyond the field of FB, located in the peripheral third of the chest, endobronchially invisible, too small to be visible for fluoroscopy | 112 (75/37) | 66.70 | 112 | 27.0 |
| Pearlstein, 2012 (31) | Retro | PPL suggestive of malignancy based on CT/PET, unsuitable for TTNA, high-risk surgery, no other available biopsy site | 101 (62/39) | 69.00 | 101 | 28.0 |
| Loo, 2014 (7) | Retro | Patients with suspected PLL | 40 (12/28) | 67.00 | 50 | 26.0 |
| Bowling, 2015 (15) | Retro | Patients with suspected cancer based on clinical history and radiographic abnormalities | 107 (60/47) | 67.00 | 120 | ND |
Pro, prospective; Retro, retrospective; PPL, peripheral pulmonary lesions; FB, flexible bronchoscopy; MLN-TBNA, mediastinal lymph node transbronchial needle aspiration; TTNA, transthoracic needle aspiration; ND, no data available.
Table 2. Main characteristics of included studies (methods and interventions).
| Study (first author) | QUADAS score | Type of sedation | Additional technique | AFTRE (mm) | Mean distance between tip of sensor and center of nodule (mm) | Sampling technique | Mean exam duration (min) |
|---|---|---|---|---|---|---|---|
| Becker, 2005 (18) | 3 | GA | Fluoroscopy, radial probe EBUS | 6.12 | 8.4 | Forceps, brush, curette | ND |
| Hautmann, 2005 (17) | 3 | CS | Fluoroscopy | ND | ND | Forceps | ND |
| Gildea, 2006 (19) | 3 | CS | Fluoroscopy | 6.60 | 9.0 | Forceps, brush, BAL, needle | 51.0 |
| Schwarz, 2006 (20) | 3 | CS | Fluoroscopy | 5.70 | ND | Forceps, brush | 46.0 |
| Wilson, 2007 (21) | 3 | CS | Fluoroscopy, ROSE | 5.00 | 8.0 | Forceps, needle | ND |
| .Makris, 2007 (24) | 4 | GA | None | 4.00 | 8.7 | Forceps | ND |
| Eberhardt, 2007 (23) | 3 | GA/CS | None | 4.60 | 9.0 | Forceps, brush, BAL, needle | 26.9 |
| Eberhardt, 2007 (a) (22) | 3 | GA/CS | None | ND | ND | Forceps | ND |
| Eberhardt, 2007 (b) (22) | 3 | GA/CS | Radio-probe EBUS | ND | ND | Forceps | ND |
| Bertoletti, 2009 (25) | 3 | CS | None | 4.70 | 10 | Forceps, brush | 29.5 |
| Lamprecht, 2009 (26) | 3 | GA | ROSE | 3.80 | 8.4 | Forceps, brush, needle | 60.0 |
| Eberhardt, 2010 (27) | 3 | GA | None | 3.60 | 9.0 | Forceps, suction | 25.7 |
| Seijo, 2010 (28) | 3 | CS | ROSE | 4 | 8.0 | Forceps, needle | 56.0 |
| Mahajan, 2011 (29) | 3 | CS | Fluoroscopy | ND | ND | Forceps, brush, BAL | ND |
| Brownback, 2012 (13) | 3 | GA | Fluoroscopy, ROSE | ND | ND | Forceps, brush, needle | ND |
| Jensen, 2012 (14) | 3 | GA | None | ND | ND | ND | ND |
| Lamprecht, 2012 (30) | 4 | GA | ROSE | ND | ND | Forceps, brush, needle | 45.2 |
| Pearlstein, 2012 (31) | 3 | GA | ROSE | 4.00 | 7.4 | Forceps, brush, needle | 70.0 |
| Loo, 2014 (7) | 4 | GA | ROSE | ND | ND | Brush, needle, resection | ND |
| Bowling, 2015 (a) (15) | 3 | IVS | Fluoroscopy | ND | ND | Forceps, brush, BAL, needle | 43.0 |
| Bowling, 2015 (b) (15) | 3 | GA | Fluoroscopy | ND | ND | Forceps, brush, BAL, needle | 58.0 |
GA, general anesthesia; EUBS, endobronchial ultrasound; ND, no data available; CS, conscious sedation; BAL, bronchoalveolar lavage; ROSE, rapid on-site cytological evaluation.
The overall low QUADAS scores indicated that the methodological quality of the enrolled studies was poor (Table 2). Since none of the included studies compared ENB to surgery as a gold standard, QUADAS scores were only evaluated in 6 of the 14 domains. In almost all publications, it was uncertain whether the selected patients were representatives of the patients who were suitable to undergo ENB-sampling, consequently inducing selection bias.
Performance outcomes
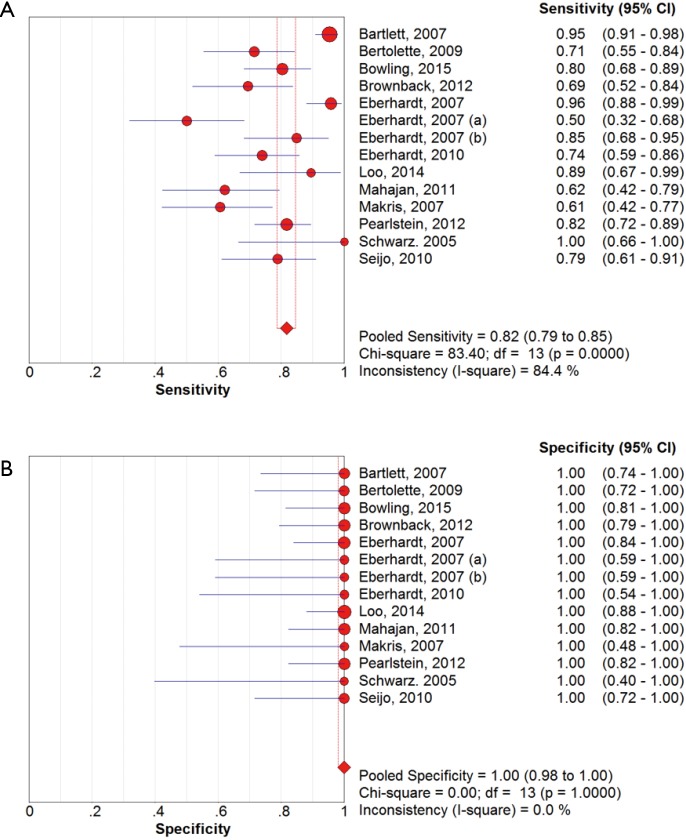
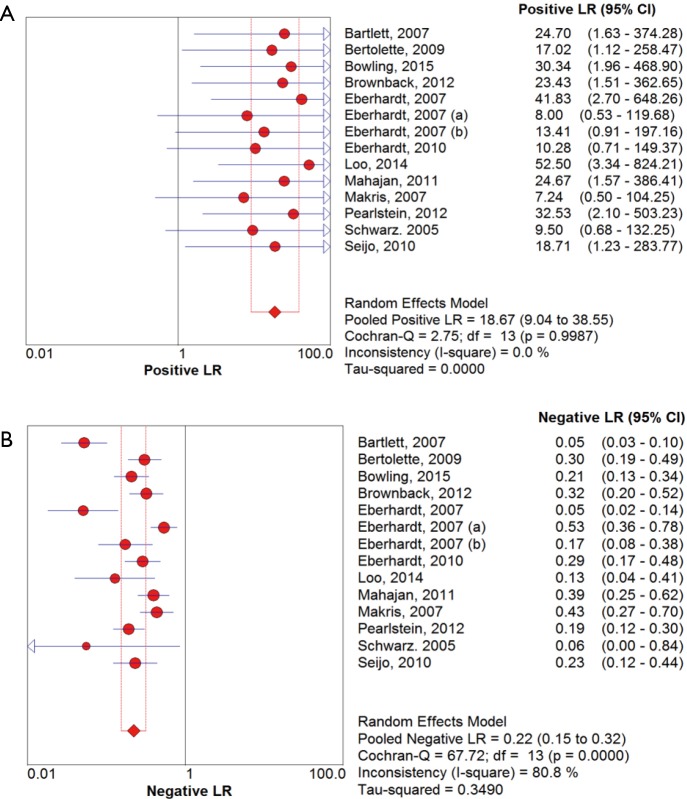
The overall diagnostic yield was summarized in Table 3. Furthermore, 15 out of 19 studies, including 892 patients, reported the TP and TN data of ENB-guided biopsy. Hence, these 15 studies were enrolled for the meta-analysis. The sensitivity of ENB in diagnosis of peripheral lung lesions ranged from 50% to 100%, with the pooled sensitivity being 82% (95% CI, 78-85%). The pooled specificity of ENB procedure was 100% (Figure 2). The pooled PLRs and NLRs were 18.67 (95% CI, 9.04-38.55), and 0.22 (95% CI, 0.15-0.32), respectively (Figure 3). The DOR was 97.36 (95% CI, 43.75-216.69) (Figure 4). The area under the curve (AUC) was 0.98 and the Q-value for the included studies in our meta-analysis was 0.94 (Figure 5), suggesting an overall level of diagnostic accuracy.
Table 3. Overall diagnostic yield.
| Study | No. Lesions | No. Diagnosed | Yield (%) | Adverse |
|---|---|---|---|---|
| Becker, 2005 (18) | 29 | 20 | 69.0 | 1 PTX |
| Hautmann, 2005 (17) | 5 | 3 | 60.0 | None |
| Schwarz, 2006 (20) | 13 | 9 | 69.2 | None |
| Gildea, 2006 (19) | 54 | 40 | 74.1 | 2 PTX (2 CTI) |
| Makris, 2007 (24) | 40 | 25 | 62.5 | 3 PTX (1 CTI) |
| Eberhardt, 2007 (23) | 92 | 62 | 67.4 | 2 PTX, 1 intub |
| Eberhardt, 2007 (a) (22) | 39 | 29 | 74.4 | 2 PTX |
| Eberhardt, 2007 (b) (22) | 40 | 35 | 87.5 | 3 PTX |
| Wilson, 2007 (21) | 279 | 167 | 59.9 | 3 PTX |
| Lamprecht, 2009 (26) | 13 | 10 | 76.9 | None |
| Bertoletti, 2009 (25) | 53 | 41 | 77.4 | 2 PTX (1 CTI) |
| Seijo, 2010 (28) | 51 | 34 | 66.7 | None |
| Eberhardt, 2010 (27) | 55 | 40 | 72.7 | 1 PTX |
| Mahajan, 2011 (29) | 48 | 37 | 77.1 | 5 PTX |
| Brownback, 2012 (13) | 55 | 41 | 74.5 | 2 respiratory failure |
| Jensen, 2012 (14) | 92 | 60 | 65.2 | 3 PTX, 1 bleeding |
| Lamprecht, 2012 (30) | 112 | 94 | 83.9 | 2 PTX |
| Pearlstein, 2012 (31) | 101 | 86 | 85.1 | 6 PTX |
| Loo, 2014 (7) | 50 | 47 | 94.0 | None |
| Bowling, 2015 (15) | 120 | 89 | 74.2 | 5 PTX |
PTX, pneumothorax; CTI, chest tube insertion; intub, intubation.
Figure 2.
Forest plot for sensitivity (A) and specificity (B).
Figure 3.
Forest plot for positive likelihood ratio (A) and negative likelihood ratio (B).
Figure 4.
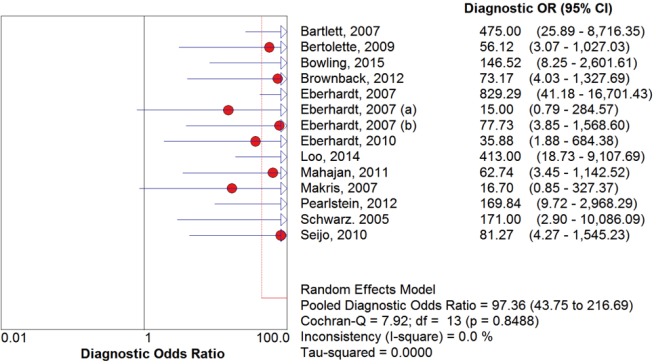
Forest plot for diagnostic odds ratio.
Figure 5.
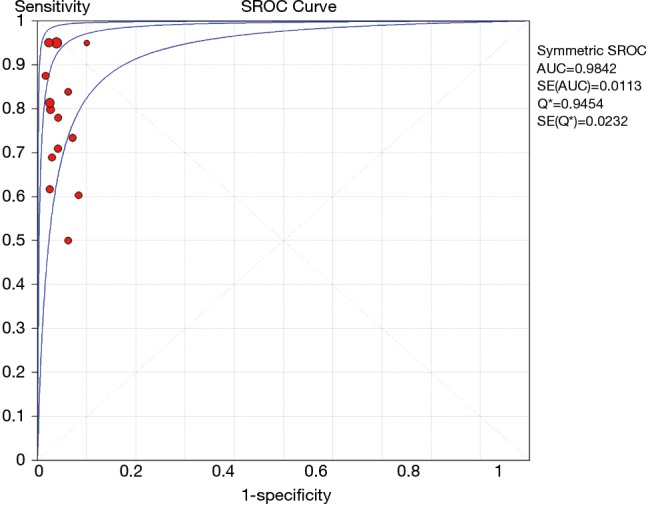
The summary receiver operating characteristic curve.
There was clinical heterogeneity caused by the type of study (prospective versus retrospective), varying patients’ inclusion criteria, and the difference in the number of biopsies obtained. Since then, significant statistical heterogeneity for the outcome of sensitivity (I2 =84.4%) and NLRs (I2 =80.8%) were found, while no heterogeneity was detected in other outcomes including specificity, PLRs and DOR.
The first sensitivity analysis was conducted by including only prospective studies (9 studies with 551 patients), which did not explain the heterogeneity (pooled sensitivity, 84%; I2 =88.9%). The next analysis excluded studies less than 20 enrolled patients (13 studies, 866 patients). However, there was no improvement in either the sensitivity (81%) or the heterogeneity (I2 =84.9%). The third analysis included only studies with general anesthesia (10 studies with 553 patients), but there was no influence on the heterogeneity (I2 =80%). The fourth analysis included studies with fluoroscopy as additional technique (5 studies with 373 patients) showed no impact on the heterogeneity as well (pooled sensitivity, 86%; I2 =86%). Final analysis included studies with ROSE as additional technique (6 studies with 439 patients), but there was no decline in heterogeneity (pooled sensitivity, 87%; I2 =83.5%).
Variables influencing the performance of ENB
Like the previous meta-analysis, we systematically reviewed all 19 original studies and identified 16 variables for their postulated influence on ENB’s diagnostic yield (Table 4). Six statistically significant variables were identified by univariate analyses. Two trials reported that location of lower lobe was correlated with decreased yields (15,22), while greater nodule size (15,28), nodule visualization with radial-probe EBUS (22,27), presence of bronchus sign (28), lower registration error (AFTRE) (24), and catheter suction technique (27) were associated with increased yields.
Table 4. Systematic review: predicting factors of ENB’s yield.
| Analyzed variables | No. of studies |
|---|---|
| Nodule characteristics | |
| Location of the nodule | 12 |
| Size of the nodule | 13 |
| Etiology of the nodule | 4 |
| Distance to visceral pleura | 4 |
| Bronchus sign | 2 |
| Uptake on PET-CT | 1 |
| Patients characteristics | |
| Predicted FFV1 | 1 |
| Procedure characteristics | |
| AFTRE | 6 |
| Navigation error | 4 |
| Type of sedation | 3 |
| Nodule visualization with radial-probe EBUS | 2 |
| Sampling technique | 1 |
| Number of biopsies obtained | 1 |
| Total procedure time | 2 |
| Navigation time | 1 |
| Learning curve | 2 |
| Reported significant predicting factors in univariate analysis | |
| Location in lower lobe | 2 (15,22) |
| Size of the nodule | 2 (15,28) |
| Bronchus sign | 1 (28) |
| AFTRE | 1 (24) |
| Nodule visualization with radial-probe EBUS | 2 (22,27) |
| Catheter suction technique versus forceps biopsies | 1 (27) |
| Bronchus sign | 1 (28) |
Safety
Additional complications caused by ENB sampling of peripheral lung nodules were listed in Table 3. A total of 40 pneumothoraces occurred in 681 procedures, in which two cases were induced using transbronchial biopsy, otherwise, none pneumothorax was ENB procedure-related. In addition, minor or moderate bleeding was reported in seven cases, and two of post-procedure respiratory failure were recorded, none of them requiring specific treatment. Other adverse events included two of chest drainage, five of chest pain, three of fever, seven of sore throat, four of hemoptysis, and four of emesis, attributed to sedation or biopsy procedure.
Discussion
The results of this meta-analysis (19 studies, 1,106 patients with peripheral lung nodules) indicated that electromagnetic-guided bronchoscopy has good sensitivity (82%) and excellent specificity (100%) in diagnosing PPLs, suggesting a hugely potential diagnostic value. Given that the likelihood ratios are accepted more useful clinically (32), we calculated the PLR and NLR of ENB-guided diagnosis in PPL patients. The pooled PLR was 18.75, which meant that NPC patients have more than eighteen-fold higher chance of carrying positive ENB-guided biopsies than do healthy people. Since PLR is high above 10, the ENB-guided diagnosing is strong enough to confirm the peripheral lung nodules. Meanwhile, the pooled NLR was 0.22, suggesting that approximately 22% chance of negative ENB-guided diagnostic results is likely to be a false-negative, which is not low enough to rule out peripheral lung lesions. DOR is more widely used to evaluate the test performance as it stands for the single indicator of diagnostic test accuracy, which combines the sensitivity and specificity data into a single number (33). Therefore, a higher value of DOR indicates a better discriminatory test performance. In this meta-analysis, DOR value was 97.36. Furthermore, our AUC was higher to 0.95, all of which suggested an overall high diagnostic accuracy by ENB-guided diagnosis in peripheral lung lesions.
Given that conventional transbronchial needle aspiration (TBNA) lacks a real-time visualization, making it difficulty guiding to the target location, EBUS-driven biopsy has been widely used to increase the diagnostic yield for peripheral lung lesions (34). Besides this, ROSE of transbronchial aspirates has been reported to be capable of providing accurate evaluation, although inadequate specimens were collected, which is another factor limiting the yield of bronchoscopy (35). Based on these, ENB in combination with EBUS or ROSE seems the best alternative diagnosing strategy. Six studies included in this meta-analysis conducted ROSE as additional technique to ENB. The sensitivity and specificity reported in these studies ranged from 85% to 92%, and 96.5% to 100%, respectively. Interestingly, the overall diagnostic yield of ENB-ROSE combination exhibited increasing trend, from 59.9% to 94% (7,13,21,26,28,31). The explanation for this increasing may be overcoming of the learning curve and the optimization of the ENB system.
Finally, the limitation in our study is primarily due to the study design. In a diagnostic accuracy meta-analysis, the results of the index test (ENB-guided diagnosing in this study) needs to be verified against a reference standard ideally on the whole included patients or at least in a random sample. In this case, surgery can be recognized as the gold standard, while high-risk patients are unsuitable for resection. Because of the nature of the ENB, it is difficult to undergo experimental and standard tests. Thus, a reference test was performed only in those with negative index test, whereas all positive results on index test were assumed as TPs. In addition, owing to the nature of the disease, assessment of specificity is difficult, as it is rare to obtain the normal pleura in those with PPL. All of these limitations may be the attribution of the high heterogeneity of this meta-analysis.
In conclusion, ENB is an effective and safe procedure in diagnosing peripheral lung lesion. The outstanding strength of using ENB-guided biopsy is low frequency of adverse events, especially regarding the risk of procedure-related pneumothorax. This new, real-time guidance system seems to be a promising strategy for diagnosis of peripheral lung nodules, which would be confirmed by further analysis and more powered prospective studies.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012;62:10-29. [DOI] [PubMed] [Google Scholar]
- 2.Molina JR, Yang P, Cassivi SD, et al. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc 2008;83:584-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flehinger BJ, Kimmel M, Melamed MR. The effect of surgical treatment on survival from early lung cancer. Implications for screening. Chest 1992;101:1013-8. [DOI] [PubMed] [Google Scholar]
- 4.Swensen SJ, Jett JR, Hartman TE, et al. CT screening for lung cancer: five-year prospective experience. Radiology 2005;235:259-65. [DOI] [PubMed] [Google Scholar]
- 5.Weiser TS, Hyman K, Yun J, et al. Electromagnetic navigational bronchoscopy: a surgeon's perspective. Ann Thorac Surg 2008;85:S797-801. [DOI] [PubMed] [Google Scholar]
- 6.Manser RL, Wright G, Byrnes G, et al. Validity of the Assessment of Quality of Life (AQoL) utility instrument in patients with operable and inoperable lung cancer. Lung Cancer 2006;53:217-29. [DOI] [PubMed] [Google Scholar]
- 7.Loo FL, Halligan AM, Port JL, et al. The emerging technique of electromagnetic navigation bronchoscopy-guided fine-needle aspiration of peripheral lung lesions: promising results in 50 lesions. Cancer Cytopathol 2014;122:191-9. [DOI] [PubMed] [Google Scholar]
- 8.Gex G, Pralong JA, Combescure C, et al. Diagnostic yield and safety of electromagnetic navigation bronchoscopy for lung nodules: a systematic review and meta-analysis. Respiration 2014;87:165-76. [DOI] [PubMed] [Google Scholar]
- 9.Shulman L, Ost D. Advances in bronchoscopic diagnosis of lung cancer. Curr Opin Pulm Med 2007;13:271-7. [DOI] [PubMed] [Google Scholar]
- 10.Gupta S, Krishnamurthy S, Broemeling LD, et al. Small (</=2-cm) subpleural pulmonary lesions: short- versus long-needle-path CT-guided Biopsy--comparison of diagnostic yields and complications. Radiology 2005;234:631-7. [DOI] [PubMed] [Google Scholar]
- 11.Zaric B, Stojsic V, Sarcev T, et al. Advanced bronchoscopic techniques in diagnosis and staging of lung cancer. J Thorac Dis 2013;5 Suppl 4:S359-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Port J, Harrison S. Electromagnetic navigational bronchoscopy. Semin Intervent Radiol 2013;30:128-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brownback KR, Quijano F, Latham HE, et al. Electromagnetic navigational bronchoscopy in the diagnosis of lung lesions. J Bronchology Interv Pulmonol 2012;19:91-7. [DOI] [PubMed] [Google Scholar]
- 14.Jensen KW, Hsia DW, Seijo LM, et al. Multicenter experience with electromagnetic navigation bronchoscopy for the diagnosis of pulmonary nodules. J Bronchology Interv Pulmonol 2012;19:195-9. [DOI] [PubMed] [Google Scholar]
- 15.Bowling MR, Kohan MW, Walker P, et al. The effect of general anesthesia versus intravenous sedation on diagnostic yield and success in electromagnetic navigation bronchoscopy. J Bronchology Interv Pulmonol 2015;22:5-13. [DOI] [PubMed] [Google Scholar]
- 16.Devillé WL, Buntinx F, Bouter LM, et al. Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol 2002;2:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hautmann H, Schneider A, Pinkau T, et al. Electromagnetic catheter navigation during bronchoscopy: validation of a novel method by conventional fluoroscopy. Chest 2005;128:382-7. [DOI] [PubMed] [Google Scholar]
- 18.Becker HD, Herth F, Ernst A, et al. Bronchoscopic Biopsy of Peripheral Lung Lesions Under Electromagnetic Guidance: A Pilot Study. J Bronchol 2005;12:9-13. [Google Scholar]
- 19.Gildea TR, Mazzone PJ, Karnak D, et al. Electromagnetic navigation diagnostic bronchoscopy: a prospective study. Am J Respir Crit Care Med 2006;174:982-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwarz Y, Greif J, Becker HD, et al. Real-time electromagnetic navigation bronchoscopy to peripheral lung lesions using overlaid CT images: the first human study. Chest 2006;129:988-94. [DOI] [PubMed] [Google Scholar]
- 21.Wilson DS, Bartlett RJ. Improved diagnostic yield of bronchoscopy in a community practice: combination of electromagnetic navigation system and rapid on-site evaluation. J Bronchol 2007;14:227-32. [Google Scholar]
- 22.Eberhardt R, Anantham D, Ernst A, et al. Multimodality bronchoscopic diagnosis of peripheral lung lesions: a randomized controlled trial. Am J Respir Crit Care Med 2007;176:36-41. [DOI] [PubMed] [Google Scholar]
- 23.Eberhardt R, Anantham D, Herth F, et al. Electromagnetic navigation diagnostic bronchoscopy in peripheral lung lesions. Chest 2007;131:1800-5. [DOI] [PubMed] [Google Scholar]
- 24.Makris D, Scherpereel A, Leroy S, et al. Electromagnetic navigation diagnostic bronchoscopy for small peripheral lung lesions. Eur Respir J 2007;29:1187-92. [DOI] [PubMed] [Google Scholar]
- 25.Bertoletti L, Robert A, Cottier M, et al. Accuracy and feasibility of electromagnetic navigated bronchoscopy under nitrous oxide sedation for pulmonary peripheral opacities: an outpatient study. Respiration 2009;78:293-300. [DOI] [PubMed] [Google Scholar]
- 26.Lamprecht B, Porsch P, Pirich C, et al. Electromagnetic navigation bronchoscopy in combination with PET-CT and rapid on-site cytopathologic examination for diagnosis of peripheral lung lesions. Lung 2009;187:55-9. [DOI] [PubMed] [Google Scholar]
- 27.Eberhardt R, Morgan RK, Ernst A, et al. Comparison of suction catheter versus forceps biopsy for sampling of solitary pulmonary nodules guided by electromagnetic navigational bronchoscopy. Respiration 2010;79:54-60. [DOI] [PubMed] [Google Scholar]
- 28.Seijo LM, de Torres JP, Lozano MD, et al. Diagnostic yield of electromagnetic navigation bronchoscopy is highly dependent on the presence of a Bronchus sign on CT imaging: results from a prospective study. Chest 2010;138:1316-21. [DOI] [PubMed] [Google Scholar]
- 29.Mahajan AK, Patel S, Hogarth DK, et al. Electromagnetic navigational bronchoscopy: an effective and safe approach to diagnose peripheral lung lesions unreachable by conventional bronchoscopy in high-risk patients. J Bronchology Interv Pulmonol 2011;18:133-7. [DOI] [PubMed] [Google Scholar]
- 30.Lamprecht B, Porsch P, Wegleitner B, et al. Electromagnetic navigation bronchoscopy (ENB): Increasing diagnostic yield. Respir Med 2012;106:710-5. [DOI] [PubMed] [Google Scholar]
- 31.Pearlstein DP, Quinn CC, Burtis CC, et al. Electromagnetic navigation bronchoscopy performed by thoracic surgeons: one center's early success. Ann Thorac Surg 2012;93:944-9; discussion 949-50. [DOI] [PubMed] [Google Scholar]
- 32.Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ 2004;329:168-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Glas AS, Lijmer JG, Prins MH, et al. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol 2003;56:1129-35. [DOI] [PubMed] [Google Scholar]
- 34.Paone G, Nicastri E, Lucantoni G, et al. Endobronchial ultrasound-driven biopsy in the diagnosis of peripheral lung lesions. Chest 2005;128:3551-7. [DOI] [PubMed] [Google Scholar]
- 35.Diacon AH, Schuurmans MM, Theron J, et al. Utility of rapid on-site evaluation of transbronchial needle aspirates. Respiration 2005;72:182-8. [DOI] [PubMed] [Google Scholar]