Abstract
An arthroscopically assisted technique for the treatment of acute acromioclavicular joint dislocations is presented. This pathology-based procedure aims to achieve anatomic healing of both the acromioclavicular ligament complex (ACLC) and the coracoclavicular ligaments. First, the acromioclavicular joint is reduced anatomically under macroscopic and radiologic control and temporarily transfixed with a K-wire. A single-channel technique using 2 suture tapes provides secure coracoclavicular stabilization. The key step of the procedure consists of the anatomic repair of the ACLC (“AC-Reco”). Basically, we have observed 4 patterns of injury: clavicular-sided, acromial-sided, oblique, and midportion tears. Direct and/or transosseous ACLC repair is performed accordingly. Then, an X-configured acromioclavicular suture tape cerclage (“AC-Bridge”) is applied under arthroscopic assistance to limit horizontal clavicular translation to a physiological extent. The AC-Bridge follows the principle of internal bracing and protects healing of the ACLC repair. The AC-Bridge is tightened on top of the repair, creating an additional suture-bridge effect and promoting anatomic ACLC healing. We refer to this combined technique of anatomic ACLC repair and protective internal bracing as the “AC-RecoBridge.” A detailed stepwise description of the surgical technique, including indications, technical pearls and pitfalls, and potential complications, is given.
Operative treatment of acute acromioclavicular joint (ACJ) injuries is indicated for type 4 and type 5 injuries, as well as some type 3 injuries, according to the Rockwood classification.1 Operative treatment aims to achieve healing of the acromioclavicular and coracoclavicular (conoid and trapezoid) ligaments to stabilize the ACJ in an anatomic position. In recent years, several arthroscopically assisted techniques have been presented for coracoclavicular stabilization, most of them aiming at anatomic reconstruction of the coracoclavicular ligament complex (CCLC) using cortical fixation buttons.2,3 However, reported complication rates reach up to 30%, including coracoid fracture, hardware failure, and secondary displacement.4 Persistent horizontal ACJ instability was found to be another major reason for less favorable radiologic and clinical results, occurring in up to 40% of cases.5 Recent biomechanical studies have shown that reconstruction of the CCLC does not provide sufficient horizontal stability of the lateral clavicle and therefore have suggested use of an additional acromioclavicular cerclage.6,7
The presented arthroscopically assisted technique reflects a sophisticated pathology-oriented approach to reconstruction of acute ACJ dislocations and was designed to achieve the best possible anatomic healing of all injured ligaments. At the same time, drawbacks of previous techniques are addressed to minimize the risk of complications. The single-channel technique using 2 suture tapes provides secure coracoclavicular stabilization. A coracoclavicular drill diameter of only 2.4 mm reduces the risk of coracoid fracture. Anatomic reconstruction of the acromioclavicular ligament complex (ACLC) represents the most important and novel step of the procedure. Primary ACLC repair is performed according to the underlying type of injury. An additional acromioclavicular suture tape cerclage is applied under arthroscopic assistance on top of this repair to control horizontal clavicular translation. The suture tape cerclage follows the principle of internal bracing, thereby providing biomechanical protection of the repaired ACLC. It creates an additional suture-bridge effect, which promotes anatomic ACLC healing. Thus the resulting “AC-RecoBridge” represents a combination of primary, anatomic ACLC repair and protective internal bracing. Table 1 outlines the philosophy and key points of the AC-RecoBridge technique. This article provides a detailed step-by-step description of the operative procedure of arthroscopically assisted reconstruction of acute ACJ dislocations with the AC-RecoBridge technique. Indications, technical pearls and pitfalls, and potential complications are presented.
Table 1.
Philosophy and Key Points of AC-RecoBridge Technique
| General aspects |
| Pathology-based procedure addressing all injured structures |
| “Reversion” of pathologic sequence of acute ACJ dislocations |
| Aims for best possible anatomic ligament healing |
| Provides primary biomechanical stability for biological healing |
| Minimal risk of complications |
| AC-Reco |
| Identification of ACLC injury |
| Classification of ACLC injury |
| Anatomic repair of ACLC injury |
| AC-Bridge |
| Limitation of horizontal clavicular translation |
| Reattachment of scapula to clavicle |
| Buttresses ACLC repair |
| Suture-bridge effect promotes ACLC healing |
| Anatomic ACLC healing under biomechanical protection |
| Safe and reproducible technique |
| Minimal iatrogenic damage and local irritation |
| Minimal risk of complications |
| No need for implant removal |
ACJ, acromioclavicular joint; ACLC, acromioclavicular ligament complex.
Operative Technique
The indications for the AC-RecoBridge technique are acute ACJ dislocations, type 4 and 5 according to the Rockwood classification, as well as high-grade type 3 injuries with dynamic horizontal ACJ instability (Table 2). Even though the timeline for acute ACJ dislocations has not been conclusively clarified, we recommend performing surgery as soon as possible, but within 2 post-traumatic weeks at the latest. Thereafter anatomic repair might be complicated by post-traumatic changes of the ACLC. The technique is not recommended for chronic ACJ instability and if anatomic ACLC repair cannot be accomplished. Table 2 lists indications and contraindications for the AC-RecoBridge technique.
Table 2.
Indications and Contraindications of AC-RecoBridge Technique
| Indications |
| Acute ACJ dislocation—Rockwood type 5 |
| Acute ACJ dislocation—Rockwood type 4 |
| Acute, high-grade ACJ injury—Rockwood type 3—with dynamic horizontal instability |
| Contraindications |
| Chronic ACJ instability |
| Failure to achieve anatomic ACLC repair |
| Acromion fracture compromising acromial stability of suture tape cerclage |
| Clavicular fracture compromising clavicular stability of suture tape cerclage |
| Os acromiale compromising acromial stability of suture tape cerclage |
| Osteoporosis |
| Previous ACJ surgery (e.g., resection of lateral clavicle) |
ACJ, acromioclavicular joint; ACLC, acromioclavicular ligament complex.
The patient is placed in the beach-chair position. An oblique 5-cm saber incision is carried out parallel to the Langer lines of skin cleavage 1 cm medial to the ACJ. Preparation down to the deltotrapezoidal fascia is performed. Meticulous preparation of the fascia is crucial because complete closure of the fascia during finalization of the procedure is an important step to support horizontal stability. The fascia is incised longitudinally in line with the clavicle. The fascia is separated from the ACLC, and the type of rupture is evaluated (Fig 1A). Basically, we have observed 4 patterns of ACLC injury: clavicular-sided, acromial-sided, oblique, and midportion ACLC tears. Mostly, the articular disk remains intact and attached to the adherent (contralateral) ACLC. So far, we have preserved the articular disk in all acute cases.
Fig 1.
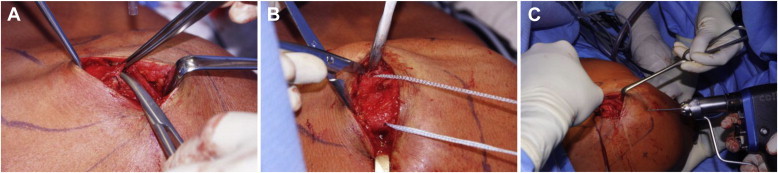
Preparation and reduction of acromioclavicular joint. (A) For reconstruction of the acromioclavicular ligament complex, the complex is carefully separated from the deltotrapezoidal fascia. (B) Next, a 2.0-mm FiberTape is shuttled through a 2.0-mm clavicular drill hole using a SutureLasso. (C) Afterward, anatomic reconstruction of the acromioclavicular joint and temporary transfixation using a 1.8-mm K-wire are performed.
An anteroposterior (horizontal) 2.0-mm drill hole is created parallel to the ACJ, 1.5 cm medial to the lateral end of the clavicle (medial to the clavicular ACLC insertion). The lateral clavicle can be elevated with a forceps for ease of drilling. A SutureLasso (Arthrex, Naples, FL) is passed through the drill hole to shuttle a 2.0-mm FiberTape (Arthrex) for later acromioclavicular cerclage (Fig 1B). Both limbs of the FiberTape are secured with a clamp. Next, the ACJ is anatomically reduced under both macroscopic and fluoroscopic control. A 1.8-mm K-wire is inserted through the acromion for temporary ACJ transfixation (Fig 1C). Care must be taken not to fix the clavicular-sided FiberTape with the K-wire. Anatomic ACJ reduction is a crucial step of the procedure. To achieve a true anteroposterior view of the ACJ, it might be necessary to tilt back the beach chair to a more supine position.
The next step of the procedure consists of arthroscopically assisted coracoclavicular suture tape stabilization using a single-channel technique. Diagnostic glenohumeral arthroscopy is performed through a posterior standard portal to exclude concomitant injuries. Routinely, one additional anterior portal with optional use of a 70° arthroscope is sufficient to perform the coracoid procedure. This anterior portal is created just above the subscapularis tendon slightly more lateral than usual. A flexible silicone cannula is inserted. Alternatively, a third approach is created through the rotator interval just anterior to the biceps tendon. This anterosuperolateral portal would then be used as the viewing portal instead of the posterior portal.
Preparation of the coracoid base is performed from the anterior portal through the subcoracoid recess (Weitbrecht foramen) using a soft-tissue shaver and an electrothermal device. The coracoid base is visualized until its lateral-to-medial extension can be clearly assessed. A partial monocortical 2.0-mm pilot hole is created about 3.5 cm (ranging from 3.0 to 4.0 cm, depending on body size and sex) medial to the lateral end and in the center of the superior cortex of the clavicle according to preoperative radiographic evaluation. The clavicular bone channel should be placed directly above the center of the coracoid base and lateral to the conoid tubercle. Trans–clavicular-coracoid drilling (2.4 mm) is performed using a commercially available aiming device particularly made for this purpose. The clavicular part of the aiming device is first placed into the clavicular pilot hole to prevent displacement. Then, the coracoid part of the aiming device is positioned centrally at the base of the coracoid under arthroscopic control. Thereby, clavicular drilling is performed between the footprints of the conoid and trapezoid ligaments to avoid additional iatrogenic damage to the ligaments (Fig 2A). Drilling is performed under continuous fluoroscopic and arthroscopic control to guarantee correct placement of the bone channel (Fig 2B). The sharp trocar is removed, and a SutureLasso (or nitinol wire) is passed and retrieved through the anterior portal. The free ends of the 2 FiberTapes loaded with a DogBone button (Arthrex) are inserted into the SutureLasso and passed through the coracoid and clavicular bone tunnel in a retrograde fashion (Fig 2C). Then, a second DogBone button is loaded onto the free suture limbs exiting the clavicle. Both FiberTapes are firmly tied over the superior DogBone button with 8 alternating half-hitches. Later, the resulting knot chains can be laid down posteriorly underneath the deltotrapezoidal fascia (Fig 2D). Radiographic controls should be performed to document correct positioning of the ACJ and implants.
Fig 2.
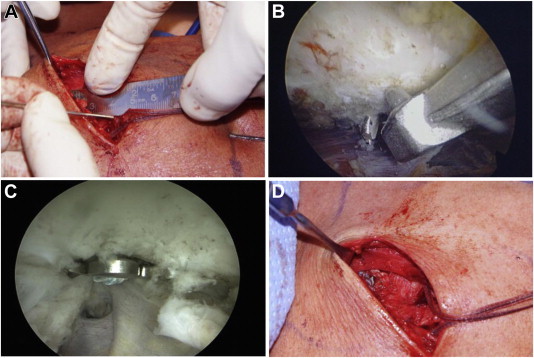
Single-channel coracoclavicular suture tape stabilization. Trans–clavicular-coracoid drilling (2.4 mm) is carried out. Clavicular drilling is performed between the footprints of the conoid and trapezoid to avoid additional iatrogenic damage to the ligaments. (A) A ruler can be used to determine the intersection between the clavicular footprints of the coracoclavicular ligament complex. Drilling is performed using the AC Guide (Arthrex). (B) The coracoid part of the aiming device is positioned centrally at the base of the coracoid under arthroscopic control. (C) Coracoclavicular suture tape stabilization is established using 2 FiberTapes loaded with DogBone buttons. (D) The FiberTapes are tightened and tied. The resulting knot chains located over the superior DogBone button can be laid down posteriorly underneath the deltotrapezoidal fascia.
AC-RecoBridge
In the first step, the ACLC is reconstructed according to the type of injury (“AC-Reco”). We frequently find a clavicular-sided tear partially with deperiostation of the lateral clavicle (Fig 3A). This type of tear is repaired by clavicular-sided transosseous reinsertion using an absorbable (1-0) polydioxanone (PDS) suture (Ethicon, Somerville, NJ). An acromial-sided tear (Fig 3B) is reconstructed by acromial-sided transosseous reinsertion. In case of clavicular-sided tears, a detachment of the deltotrapezoid fascia might be present (Fig 3 C and D). In case of a midportion tear, the ACLC is directly repaired with absorbable (1-0) PDS sutures. An oblique type of tear may require both transosseous and direct repair. Table 3 outlines the classification of acute ACLC tears including corresponding strategies of anatomic repair.
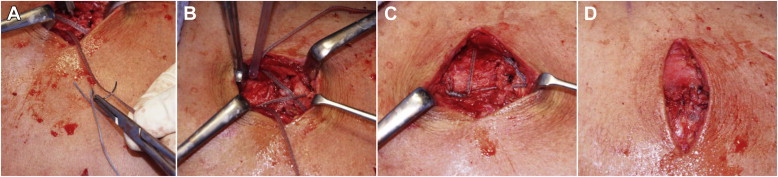
Fig 3.
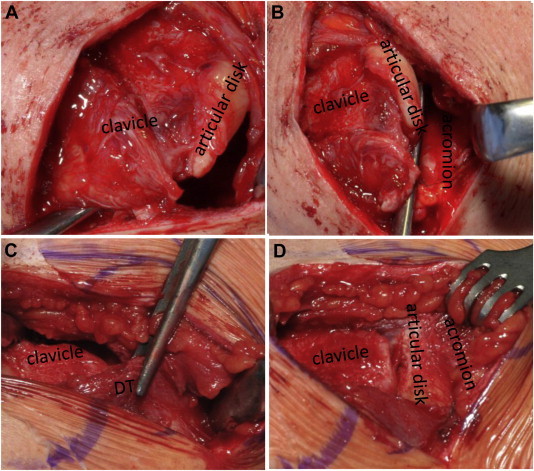
Morphology of acromioclavicular ligament tear patterns. (A, B) Acromial-sided tear of acromioclavicular ligaments. The articular disk is intact and remains attached to the lateral clavicle. (C, D) Clavicular-sided tear. A complete detachment of the deltotrapezoidal fascia (DT) occurred. The articular disk is intact and remains attached to the acromion.
Table 3.
Morphologic Classification of Acute ACLC Tears With Corresponding Repair Strategies
| ACLC Tear | Repair Strategy |
|---|---|
| Clavicular-sided ACLC tear | Clavicular-sided transosseous repair |
| Acromial-sided ACLC tear | Acromial-sided transosseous repair |
| Oblique ACLC tear | Combined transosseous and direct repair |
| Midportion ACLC tear | Direct repair |
ACLC, acromioclavicular ligament complex.
Next, the acromioclavicular cerclage is created in an arthroscopically assisted fashion to provide protective internal bracing for the reconstructed ACLC (“AC-Bridge”). The arthroscope is placed into the subacromial space. An anterolateral portal is created for subacromial bursectomy. The anterosuperolateral portal also can be used if previously established. The undersurface of the acromion is visualized without bony decompression. After bursectomy, a 5.75-mm crystal cannula is inserted. From superiorly, we perform epiperiosteal preparation of the central part of the acromion, which reflects a zone free of muscle insertions. Two 2.0-mm acromial-sided vertical drill holes are created within this zone for passage of the acromioclavicular cerclage. First, the posterior hole is drilled under arthroscopic control in continuation of the posterior border of the lateral clavicle 1.5 cm lateral to the ACJ (lateral to the acromial ACLC insertion) (Fig 4A). Care must be taken not to injure the rotator cuff or humeral head (Fig 4B). Directly after removal of the drill, a SutureLasso is inserted in a craniocaudal direction and retrieved subacromially through the anterolateral portal (Fig 4 C and D). Intermittent stopping of pump pressure and continuous suction facilitate insertion of the SutureLasso into the small drill hole.
Fig 4.
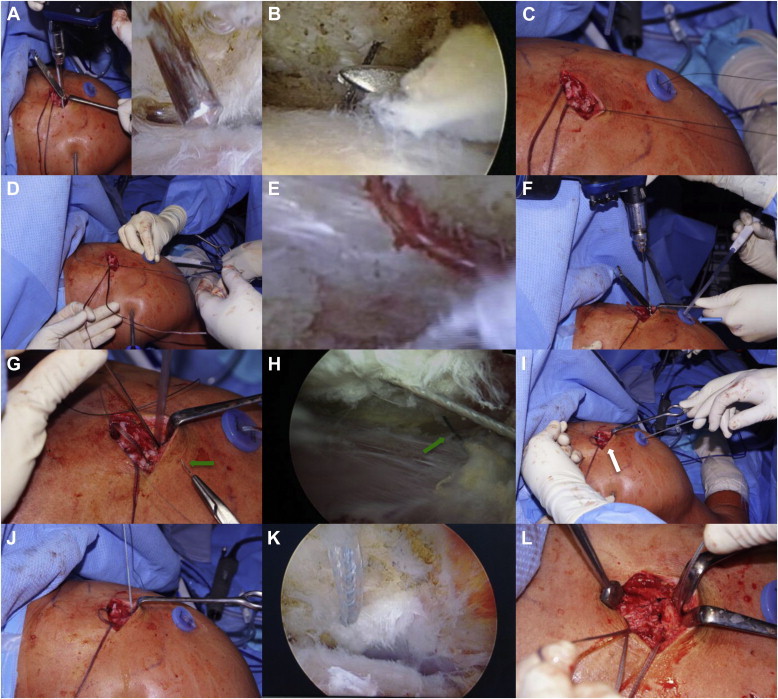
Shuttling of FiberTape in AC-RecoBridge technique. First, the acromioclavicular ligament complex is reconstructed according to the type of injury (AC-Reco). Afterward, the acromioclavicular cerclage is created in an arthroscopically assisted fashion to provide protective internal bracing for the reconstructed acromioclavicular ligament complex (AC-Bridge). (A) A posterior 2.0-mm acromial-sided vertical drill hole is created. (B, C) A SutureLasso is passed through the drill hole and shuttled out the anterolateral portal. (D-F) The anterior limb of the clavicular-sided FiberTape is passed through the SutureLasso, is pulled through the posterior acromial drill hole subacromially, and then exits the anterolateral cannula (blue arrow). The second, anterior drill hole is created in the craniocaudal direction at the acromion. (G, H) A SutureLasso is passed through this anterior drill hole and shuttled out the anterolateral portal (green arrows). (I-L) The suture tape limb already located within the cannula is inserted into the SutureLasso and shuttled from subacromially to the surface of the acromion, exiting the anterior drill hole (white arrow). Underneath the acromion, a U-shaped configuration of the FiberTape develops. Patients are placed in the beach-chair position. The arthroscope is placed in the posterior portal.
Next, the anterior limb of the previously advanced clavicular-sided FiberTape is shuttled subacromially and then exits the anterolateral cannula (Fig 4 D and E). Another vertical drill hole is created about 2.0 cm anterior to the posterior hole, again at a distance of 1.5 cm lateral to the ACJ. The SutureLasso is inserted through this anterior drill hole, again in a craniocaudal direction, and retrieved subacromially through the anterolateral portal. The previously shuttled suture tape limb already located within the cannula is inserted into the SutureLasso, is shuttled from subacromially to the surface of the acromion, and then exits the anterior drill hole. This creates a “U” underneath the acromion type of configuration (Fig 4 F-L). The suture tape limb is now shuttled from posterior to anterior through the existing horizontal hole in the clavicle. For this purpose, the already present part of the suture tape can be used as a self-made shuttle. An eyelet needle is used to pass the limb through the part of the suture tape exiting the posterior clavicle. Then, the limb can be shuttled by pulling the tape anteriorly and can be retrieved anteriorly. We found this to be the easiest way to shuttle a second suture tape limb through the small 2.0-mm clavicular drill hole rather than using a SutureLasso.
The completed cerclage (AC-RecoBridge) is tightened under arthroscopic control. Finally, the “U” should closely align to the undersurface of the acromion. The X-configured cerclage lies on top of the reconstructed ACLC, creating a suture-bridge effect comparable with double-row rotator cuff reconstruction. The tightened cerclage is locked by 8 alternating half-hitches with the knot chain being located at the posterior border of the clavicle. We recommend extracting the transfixing K-wire under radiographic control to document constant and correct reduction of the ACJ. All knot chains are laid down posteriorly underneath the deltotrapezoidal fascia (Fig 5). Finally, the deltotrapezoidal fascia is reconstructed with absorbable (0) PDS sutures, and the wounds are closed with absorbable sutures. Table 4 summarizes the major technical pearls and Table 5 summarizes the pitfalls of the operative technique. Table 6 lists potential complications (so far not experienced).
Fig 5.
Knotting and closure of deltotrapezoidal fascia in AC-RecoBridge technique. The suture tape limb exiting the anterior acromial drill hole is shuttled from posterior to anterior at the clavicle. (A) An eyelet needle is used to pass the limb through the part of the suture tape exiting the posterior clavicle. (B) By pulling this limb anteriorly, the passage is executed. The X-configured cerclage lies on top of the reconstructed acromioclavicular ligament complex, creating a suture-bridge effect comparable with double-row rotator cuff reconstruction. (C) The tightened cerclage is locked, with the knot chain being located at the posterior border of the clavicle. (D) The AC-RecoBridge will be covered after closure of the deltotrapezoidal fascia.
Table 4.
Technical Pearls of AC-RecoBridge Technique
| Operative Step | Technical Pearl |
|---|---|
| Anatomic ACJ reduction | ACJ reduction and K-wire transfixation under macroscopic and fluoroscopic control |
| Anatomic ACLC reconstruction (AC-Reco) | Meticulous and sufficient preparation for correct assessment of ACLC tear type Transosseous and/or direct anatomic ACLC repair according to underlying tear type |
| Acromioclavicular suture tape cerclage (AC-Bridge) | Elevation of lateral clavicle eases horizontal clavicular drilling, SutureLasso insertion, and suture tape passage Intermittent pausing of pump pressure eases insertion of SutureLassos through vertical 2.0-mm acromial drill holes Perform sufficient subacromial bursectomy Vertical acromial drillings under arthroscopic control within insertion-free zone lateral to lateral ACL Use of a crystal cannula in anterolateral portal avoids soft-tissue bridges Use part of suture tape posterior to clavicle as self-made shuttle for passage of crossing limb from posteriorly to anteriorly Create knot chain (8 alternating half-hitches) and lay down posteriorly underneath deltotrapezoidal fascia to avoid local knot irritation |
ACJ, acromioclavicular joint; ACL, anterior cruciate ligament; ACLC, acromioclavicular ligament complex.
Table 5.
Technical Pitfalls of AC-RecoBridge Technique
| Operative Step | Technical Pitfall |
|---|---|
| Anatomic ACJ reduction | ACJ malreduction |
| Anatomic ACLC reconstruction (AC-Reco) | Displacement of articular disk or incarceration of ACLC may cause ACJ malreduction and nonanatomic ACLC healing |
| Acromioclavicular suture tape cerclage (AC-Bridge) | Fixation/damage of clavicular part of AC-Bridge caused by transfixing K-wire Fluid outflow caused by continuation of pump pressure may complicate insertion of SutureLassos through vertical acromial drillings Insufficient subacromial bursectomy may complicate subacromial visualization and extraction of SutureLassos Insufficient tightening prior to locking may result in AC-Bridge that is too loose Local irritation by superiorly placed knot |
ACJ, acromioclavicular joint; ACLC, acromioclavicular ligament complex.
Table 6.
Potential Complications (Not Experienced Thus Far) of AC-RecoBridge Technique
| Complications associated with prolongation of operative time (e.g., critical local swelling, infection) |
| Subacromial irritation caused by subacromial part of AC-Bridge |
| Local irritation with potential need for suture tape removal |
| Primary loosening of AC-Bridge (e.g., caused by insufficient tightening prior to locking) |
| Secondary loosening of AC-Bridge (e.g., caused by progressive cutting through of acromioclavicular suture tape cerclage due to low bone quality or absent/biomechanically insufficient healing of ACLC) |
| Iatrogenic clavicle, coracoid, or acromion fracture |
ACLC, acromioclavicular ligament complex.
Rehabilitation
The patient wears a protective sling for 6 weeks postoperatively. Supervised physiotherapy includes passive and active-assisted abduction/elevation limited to 45° for 3 weeks postoperatively and limited to 60° for another 3 weeks (weeks 3 to 6). Active and unlimited range of motion is started from week 7 and strengthening exercises after 12 weeks postoperatively. These relatively strict limitations of range of motion were established based on clinical experience and in vivo studies of ACJ kinematics showing significant lengthening of the conoid ligament and horizontal clavicular translation with greater than 60° of abduction.8,9 Thereby, early failure of synthetic coracoclavicular and acromioclavicular stabilization should be prevented until biological ligament healing has occurred.
Discussion
As early as 1986, Fukuda et al.10 stated, “if maximum strength of healing after an injury to the acromioclavicular joint is the goal, all ligaments should be allowed to participate in the healing process.” Both the CCLC and ACLC importantly contribute to ACJ stability. Debski et al.11 found that the CCLC alone is not able to sufficiently stabilize the ACJ in the anteroposterior (horizontal) direction. Therefore operative ACJ reconstruction techniques should address all ligamentous stabilizers. However, for a long time, arthroscopically assisted procedures only focused on the best possible anatomic reconstruction of the CCLC using strong synthetic suture material and cortical fixation buttons. Indeed, rates of persistent horizontal ACJ instability of up to 40% have been reported and seem to be associated with inferior clinical outcomes.4,5 A recent biomechanical study showed that additional acromioclavicular cerclage limits horizontal ACJ translation to an almost physiological extent.7 However, significant cerclage loosening occurred over time, resulting in complete consumption of its stabilizing effect. Thus the acromioclavicular cerclage may only be regarded as a temporary stabilizer, and final horizontal ACJ stability will depend on the quality of biological healing of the ACLC.
All these fundamental issues were considered in the design of the AC-RecoBridge. This pathology-based procedure aims to achieve anatomic healing of both the ACLC and the coracoclavicular ligaments (Table 1). Anatomic reconstruction (transosseous and/or primary repair) of the ACLC (AC-Reco) is a crucial step of the procedure because it provides the basis for achieving the best possible anatomic healing. In this context, meticulous surgical preparation and visualization of the ACLC (both clavicular and acromial parts) are essential for correct assessment of the underlying ACLC tear type and choice of repair strategy (Table 3). We found the ACLC, or parts thereof, displaced and/or incarcerated within the ACJ, literally acting as a mechanical obstacle for reduction. In such cases, only such mini-open repair is able to accomplish anatomic ACLC healing. The presented classification of ACLC tear patterns evolved from our intraoperative observations (Table 3). We were able to distinguish 4 recurring types of ACLC injuries (clavicular-sided, acromial-sided, oblique, and midportion tears). All of them could be surgically repaired in an anatomic fashion.
The acromioclavicular suture tape cerclage (AC-Bridge) has 2 major functions: Most importantly, it protects healing of the primary ACLC repair. Following the principle of internal bracing, the AC-Bridge serves as a protective stabilizer buttressing the reconstructed ACLC and limiting horizontal clavicular translation to an almost physiological extent.7 As is known from basic biomechanical research, isolated ACLC injury already leads to significant alteration (internal and downward rotation) of scapula positioning.12 These findings additionally support the importance of ACLC repair and stabilization in ACJ reconstruction. In this context the AC-Bridge represents an effective method to reattach the scapula to the clavicle. Second, it creates a suture-bridge effect, pressing the repaired/reinserted ACLC onto its clavicular and acromial “footprints,” comparable with double-row repair of the rotator cuff.
The arthroscopically assisted technique is minimally invasive, safe, and reproducible. Because of its vertical orientation, the distance of drilling corresponds only to the diameter of the acromion (8 to 10 mm), minimizing the risk of iatrogenic fractures. Other techniques require substantially longer lateromedial or anteroposterior drillings through the acromion and affect the insertion zone of the deltoid muscle. The acromial part of the AC-RecoBridge is located in a zone on top of the acromion without relevant muscle insertions. Instead of the suture tape, use of a 1.5-mm absorbable PDS suture could be considered. However, the suture tape displays biomechanical properties comparable with those of the ACLC7 and does not cause absorption reactions such as known from bioresorbable suture material. To our knowledge, removal of the synthetic AC-Bridge is not necessary. So far, we have observed neither radiologic signs of “cutting through” nor drill hole enlargements. Obviously, anatomic/stable ACLC healing reduces or even eliminates biomechanical stress acting on the acromioclavicular cerclage. On the other hand, absent or insufficient healing will inevitably result in loosening and/or failure of the cerclage.
Coracoclavicular stabilization using cortical fixation devices is associated with high complication rates. This is particularly true for the so-called anatomic double-channel techniques.4 As a consequence, we prefer to use a single-channel technique (2.4-mm drill diameter) featuring even superior biomechanical stability and minimizing the risk of iatrogenic fractures and/or tunnel misplacement. “Anatomic” double-channel techniques for coracoclavicular stabilization involve (partial) synthetic CCLC replacement. To date, the biological effects on CCLC healing are unclear. However, it appears obvious that iatrogenic damage and (partial) synthetic CCLC replacement most likely adversely affect anatomic healing. For this reason, we try to preserve the CCLC in the acute situation as far as possible. Ideally, the coracoclavicular bone channel is placed between the footprints of the conoid and trapezoid ligaments to prevent iatrogenic damage potentially caused by coracoclavicular drilling and manipulation. Still, this extra-anatomic coracoclavicular stabilization reliably and securely restores the physiological coracoclavicular distance, leading to anatomic reduction and healing of the CCLC. Again for biological reasons, we choose an intra-articular approach instead of an extra-articular approach because less growth factor–containing hematoma is washed out (pearls, pitfalls, and complications are described in Tables 4, 5, and 6, respectively).
In summary, the AC-RecoBridge represents an arthroscopically assisted technique designed for the best possible anatomic healing of both the CCLC and ACLC. Although technically demanding, the procedure is safe and reproducible and the risk of complications is minimized.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
A combination of arthroscopic video sequences and images of the operative site give a step-by-step tutorial of how to create the AC-RecoBridge. The patient is placed in the beach-chair position, and the arthroscope is placed in the posterior portal. Two 2.0-mm acromial-sided vertical drill holes are created. A SutureLasso is inserted into the posterior drill hole in a craniocaudal direction and retrieved subacromially through the anterolateral portal, and the anterior limb of the previously advanced clavicular-sided FiberTape is shuttled subacromially, exiting the anterolateral cannula. Another SutureLasso is inserted through the anterior drill hole, and the previously shuttled suture tape limb already located within the cannula is inserted into the SutureLasso and shuttled from subacromially to the surface of the acromion.
References
- 1.Beitzel K., Cote M.P., Apostolakos J. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy. 2013;29:387–397. doi: 10.1016/j.arthro.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 2.Venjakob A.J., Salzmann G.M., Gabel F. Arthroscopically assisted 2-bundle anatomic reduction of acute acromioclavicular joint separations: 58-month findings. Am J Sports Med. 2013;41:615–621. doi: 10.1177/0363546512473438. [DOI] [PubMed] [Google Scholar]
- 3.Scheibel M., Dröschel S., Gerhardt C., Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39:1507–1516. doi: 10.1177/0363546511399379. [DOI] [PubMed] [Google Scholar]
- 4.Martetschläger F., Horan M.P., Warth R.J., Millett P.J. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013;41:2896–2903. doi: 10.1177/0363546513502459. [DOI] [PubMed] [Google Scholar]
- 5.Scheibel M., Ifesanya A., Pauly S., Haas N.P. Arthroscopically assisted coracoclavicular ligament reconstruction for chronic acromioclavicular joint instability. Arch Orthop Trauma Surg. 2007;128:1327–1333. doi: 10.1007/s00402-007-0547-9. [DOI] [PubMed] [Google Scholar]
- 6.Beitzel K., Obopilwe E., Apostolakos J. Rotational and translational stability of different methods for direct acromioclavicular ligament repair in anatomic acromioclavicular joint reconstruction. Am J Sports Med. 2014;42:2141–2148. doi: 10.1177/0363546514538947. [DOI] [PubMed] [Google Scholar]
- 7.Saier T, Venjakob AJ, Minzlaff P, et al. Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: A biomechanical study. Knee Surg Sports Traumatol Arthrosc in press, available online 21 February, 2014. doi:10.1007/s00167-014-2895-7. [DOI] [PubMed]
- 8.Izadpanah K., Weitzel E., Honal M. In vivo analysis of coracoclavicular ligament kinematics during shoulder abduction. Am J Sports Med. 2012;40:185–192. doi: 10.1177/0363546511423015. [DOI] [PubMed] [Google Scholar]
- 9.Seo Y.-J., Yoo Y.-S., Noh K.-C. Dynamic function of coracoclavicular ligament at different shoulder abduction angles: A study using a 3-dimensional finite element model. Arthroscopy. 2012;28:778–787. doi: 10.1016/j.arthro.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Fukuda K., Craig E., An K., Cofield R., Chao E. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am. 1986;68:434–440. [PubMed] [Google Scholar]
- 11.Debski R.E., Parsons I.M., Woo S.L., Fu F.H. Effect of capsular injury on acromioclavicular joint mechanics. J Bone Joint Surg Am. 2001;83:1344–1351. doi: 10.2106/00004623-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Oki S., Matsumura N., Iwamoto W. The function of the acromioclavicular and coracoclavicular ligaments in shoulder motion: A whole-cadaver study. Am J Sports Med. 2012;40:2617–2626. doi: 10.1177/0363546512458571. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A combination of arthroscopic video sequences and images of the operative site give a step-by-step tutorial of how to create the AC-RecoBridge. The patient is placed in the beach-chair position, and the arthroscope is placed in the posterior portal. Two 2.0-mm acromial-sided vertical drill holes are created. A SutureLasso is inserted into the posterior drill hole in a craniocaudal direction and retrieved subacromially through the anterolateral portal, and the anterior limb of the previously advanced clavicular-sided FiberTape is shuttled subacromially, exiting the anterolateral cannula. Another SutureLasso is inserted through the anterior drill hole, and the previously shuttled suture tape limb already located within the cannula is inserted into the SutureLasso and shuttled from subacromially to the surface of the acromion.


