Abstract
Objectives:
To evaluate medical students’ satisfaction with simulation based learning strategy (SBL).
Methods:
A cross-sectional survey was conducted between October and November 2013 at the College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia. All third and fourth year medical students (n=185) both males and females were included. A self-developed questionnaire on the effect of SBL was used. Items included were related to knowledge, skill, environment, resources, and faculty. The questionnaire was validated by an expert reviewer, and the reliability was calculated for all the questionnaire items. Responses were measured on a 5 point Likert-type scale, and statistical analysis was carried out.
Results:
The response rate for this study was 62% (n=115). The alpha coefficient for all items was 0.73. Overall, respondents from both years’ students were satisfied with teaching strategy, use of mannequins, and learning environment. The challenges reported were lack of skill-laboratories facilities, students’ cooperation, allocated time for skill-laboratories, and knowledge of instructor. There was a small, but significant difference between the satisfaction scores among genders (p=0.001). Whereas no difference was identified between the participants’ scores on satisfaction with SBL and year of education (p=0.62).
Conclusion:
Although there were few challenges, most of the students were satisfied that SBL improved their knowledge retention, skills, and communication.
Medical education programs are increasingly adopting simulation in both undergraduate and postgraduate curricula. Many reasons were cited on the use of simulation in clinical teaching including the changes in healthcare delivery, lack of objectivity of clinical examinations,1 limited clinical placement positions, and potential of simulation to improve clinical learning.2 Numerous reports support the introduction of simulation based medical education as an important step in curriculum development.3 Especially in training of high risk disciplines such as resuscitation, airway management, procedural training, trauma, and disaster management.4 Positive results in relation to enhancing knowledge, skills, and attitude toward technology-enhanced simulation have been reported in many studies.5-7 Two studies conducted in Saudi Arabia regarding usage of simulators for teaching laparoscopic surgery skills among junior surgical residents8 and local anesthesia teaching9 showed significant enhancement and improvement at a cognitive as well as psychomotor level. The technique has been widely used for the acquisition of specific clinical skill in specialties such as pediatrics, emergency medicine, intensive care medicine, obstetrics, anesthesia, radiology, and allied medical sciences.10,11 The potential advantages of simulation to student’s learning have stimulated the use of simulation in medical teaching in Kingdom of Saudi Arabia. In graduate medical education, the evidence is equivocal regarding whether simulation compared with traditional teaching methods improves learning or clinical performance.6 On literature review, we were unable to find research in relation to undergraduate medical students on their perceptions related to the effectiveness of simulation based learning (SBL) strategies. It is important to understand students’ satisfaction with the new teaching method to integrate simulation as a teaching learning strategy in medical education curricula. In the present study, we aimed to determine students’ satisfaction with this educational strategy in undergraduate medical students enrolled in King Saud bin Abdulaziz University for Health Sciences (KSAU-HS), Riyadh, Saudi Arabia. Also, to identify any challenges associated. The findings of their research could be utilized for future training and implementation of simulated activities in the curricula.
Methods
This cross-sectional study was conducted at the College of Medicine, King Saud bin Abdulaziz University for Health Sciences in Riyadh, Saudi Arabia between October and November 2013. Simulation based learning is one of numerous educational strategies, that the colleges have been employing since 2004. The clinical skill-laboratories are equipped with numerous simulators varying from low to high fidelity, and are being used by medical students under the supervision of assigned instructors and also being used for assessment purposes.
In the present study, the sample was comprised of all the third year (n= 125; 90 males and 35 females) and fourth year (n=60, only males) medical students from batch 7 and 8 (approximately 185 students) studying at KSAU- HS, who are exposed to SBL. The university started accepting female students from 2010; therefore, only one group of females was included. As the sample size was very small, we used the convenience sampling technique. Subjects who refused to participate in the study, or any incomplete questionnaires were excluded. To gain a better understanding of students’ satisfaction, a self-developed questionnaire on a 5-point Likert scale that indicated degrees of satisfaction was used to assess most of the dimensions in the questionnaire. The questionnaire was relevant to the following 2 themes: 1) overall satisfaction, and 2) challenges related to the SBL. The items for the questionnaire were selected after a thorough literature review. Literature was searched using PubMed and Google scholar. Only those items that were relevant to our setting were included. The questionnaire consisted of 40 items related to satisfaction and challenges they faced during simulation teaching. All items were mixed to avoid any misunderstanding with the 2 concepts; satisfaction and challenge. In addition, space was provided for open-ended follow-up questions to generate qualitative data on the strengths and weaknesses of SBL.
The questionnaire was validated by expert reviewers; one senior researcher from the medical education department, a biostatician, and 2 faculty members involved in simulation teaching. The reliability was calculated for all the questionnaire items. The alpha coefficient for all items was 0.73, suggesting relatively high internal consistency of items.
Ethical approval was sought from the College of Medicine Research Committee for the current research project. Written consent was taken from the participants after being informed of the purpose of the study, and the right to withdraw from the study at any time. They were assured that the information they provide would remain confidential and their identity would not be disclosed. The questionnaire was distributed and collected manually by the investigator with the help of students’ leaders. Only those who volunteer were included in the study. No incentives or follow-ups were undertaken.
Data cleaning and assigning codes were carried out before the analysis. The analysis was based on the respondents who provided complete data. The data was entered and analyzed using IBM SPSS statistical package for windows (IBM Corp., Armonk, NY, USA) version 20. The data was analyzed on a group basis. Descriptive statistics was presented as frequencies and percentages for categorical variables (namely, gender, year of education). Basic descriptive statistical analysis of the Likert items was conducted by calculating frequencies, means, and standard deviations. The percentage of satisfaction of all students was calculated by combining frequency of levels of satisfaction (satisfied and very satisfied) for each item in the questionnaire. The responses on the Likert scale were totaled for each domain (from 1=very dissatisfied to 5=very satisfied). Then, inferential statistics using independent samples t-test was used to compare the difference between the satisfaction and challenges scores by year of study and gender. A p-value of less than 0.05 was considered as being statistically significant. Overall responses on open ended questions were coded, and themes were derived from the responses. Results were used to support the quantitative responses.
Results
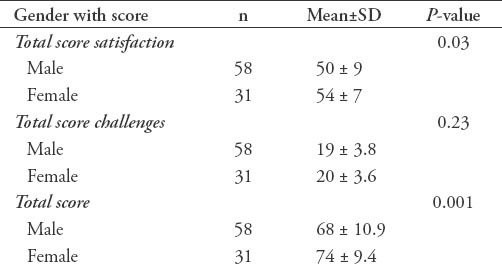
A questionnaire was distributed to 185 undergraduate medical students with a response rate of 62% (n=115). Ten students refused to participate and the remaining questionnaires were incomplete. The included sample was comprised of 89 third-year students and 26 fourth-year students. There were more males (n=84) than females (n=31). There was no accepting of female student in the fourth-year students. The overall satisfaction scores with SBL were high (85%), as most of them considered it a useful addition to learning, and felt the need for more training sessions with simulators (71%). Most of the students (67%) opined that they were familiar with the concept. Sixty percent reported SBL as a helpful modality to retain knowledge and to gain more communication skills. Furthermore, approximately 50% of the students reported that the use of simulation improved their clinical decision making ability and psychomotor skill competency, and difficult to treat the mannequin (Table 1). With regards to challenges, most of the students showed their dissatisfaction with the skills-laboratory facilities (13%), the time allocated for skills-laboratory (26%), and the cooperation between the students during the sessions (22%). On other hand, most of the students opined that they were given an opportunity to practice at the skills-laboratory (86%), and most had observed the high fidelity simulators (69%) (Table 2). While comparing the mean scores of the third year male and female students, a small difference, but significant difference between the satisfaction scores among the genders was found (p=0.001) (Table 3).
Table 1.
Students satisfaction with simulation based learning among 115 third and fourth year medical students.
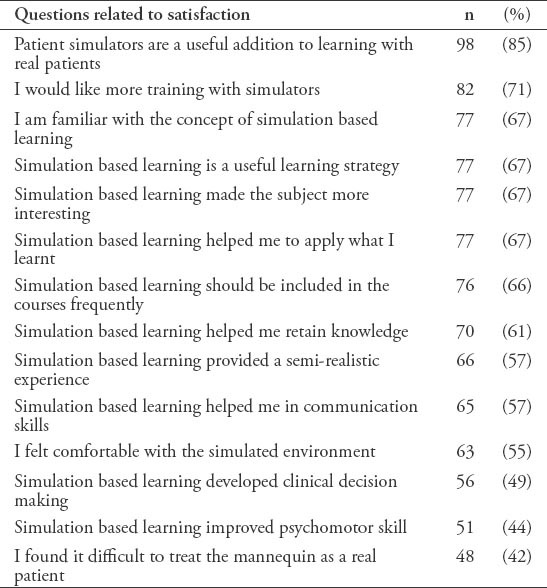
Table 2.
Overall response of 115 third and fourth year medical students to the challenges associated with simulation based learning.
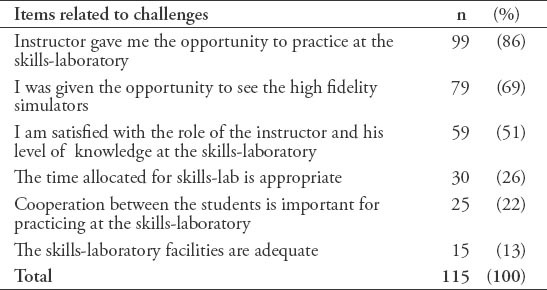
Table 3.
Comparison of satisfaction and challenges with simulated based learning by gender of 89 third year medical students.
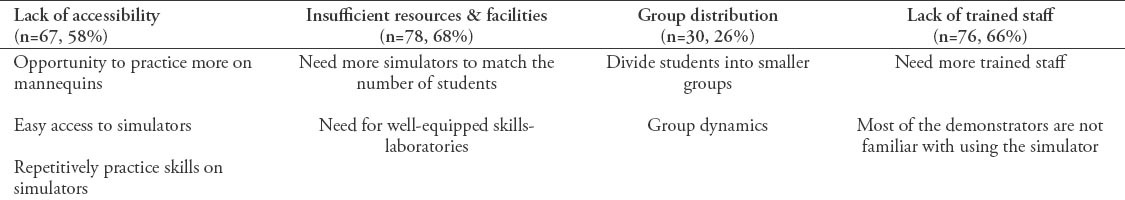
We compared the overall differences between the male participants’ scores on the satisfaction with SBL by year of education. No significant differences were identified in the case of satisfaction (p=0.62) and challenges (p=0.99). All males from both batches obtained almost the same mean scores (Table 4). For the qualitative part of the questionnaire, students mentioned the main traits of the SBL such as exposure to semi realistic environment (73%), protected learning environment (77%), knowledge retention (75%), and opportunity to practice more (86%) (Table 5). Whereas areas that require improvement identified by the students were: lack of accessibility (58%), insufficient resources and facilities (68%), group distribution (26%), and lack of trained staff (66%) (Table 6).
Table 4.
Comparison of satisfaction and challenges of simulation based learning by year of education among 84 third and fourth year medical students.
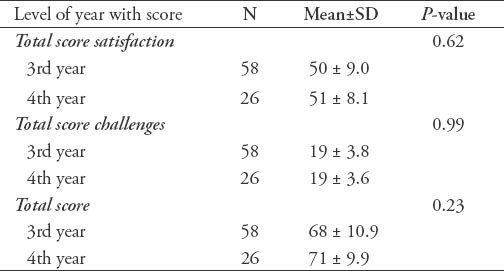
Table 5.
Overall response to the strengths of simulated based learning among 115 among third and fourth year medical students.
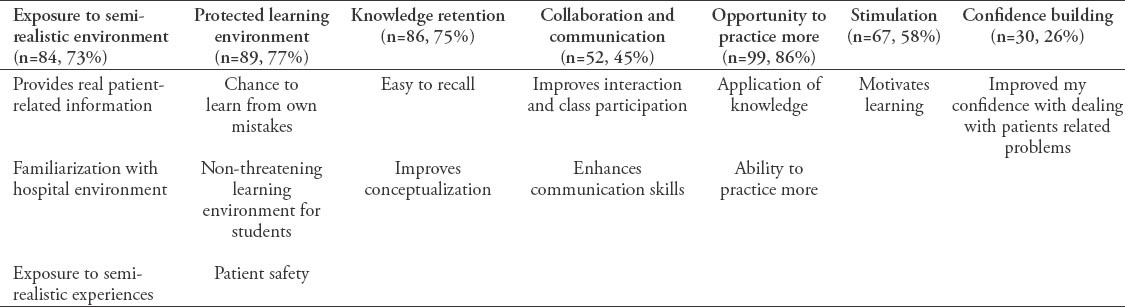
Table 6.
Overall response to the weaknesses of the simulated based learning among 115 among third and fourth year medical students.
Discussion
In this study, student satisfaction score with the SBL showed overall satisfaction (mean score=7). These results are in accordance with the findings of Franc-Law’s et al’s study at 2010,12 where the overall medical students’ satisfaction a with simulated based curriculum was high (8 of 10 on a Likert scale). Our findings demonstrated students’ perception on patient simulators and its usefulness, and reported SBL as an addition to learning with real patients, improve retention of learning material, enhance decision making skill, and provide conducive learning environment. This is similar to the studies carried out by Traynor et al13 and Ennen & Satin,14 who reported that students gain knowledge and confidence during simulation sessions for clinical practice and improves communication and team work in emergency situations. Moreover, in 200915 a study is conducted at Loma Linda University incorporated simulation into resuscitation training sessions, and reported that it provided student confidence to manage similar cases in the future. Another study carried out by Chakravarthy et al in 201116 showed significant improvement in medical student knowledge, confidence, management skills, and level of satisfaction with the emergency rotation. A comparative study conducted at the University of California, Los Angeles in 2006,17 showed better transfer of knowledge in the simulator-educated students compared with the PBL students. While other studies18-20 demonstrated high student satisfaction scores for material taught with simulation compared with more traditional modalities such as Power Point lecture,18 self-study session,19 and group discussion.
In addition to this study, we also compared the satisfaction scores with gender and year of study. There was no significant difference except for the gender, which suggests that the satisfaction of the female group was higher compared with their counterpart. Further, different themes were derived from open-ended follow-up questions such as exposure to semi-realistic environment including real patient-related information, familiarization of hospital environment, knowledge retention, stimulation, collaboration and communication, protected learning environment including chance to learn from own mistakes, non-threatening learning environment for students, patient safety, confidence building, and opportunity to practice more. However, students’ responses on the weaknesses identified some very important aspects of SBL that need to be considered while using it for teaching clinical skills. These aspects were: insufficient resources and facilities, lack of trained staff, group distribution, and accessibility of simulators. A survey conducted among clerkship directors in emergency medicine on simulation in medical education highlighted limited faculty time and clerkship hours as barriers associated with this type of teaching and learning activities. They also found that financial resources, faculty time, and the number of students are the main barriers in preclinical years.21
Study limitations
Although the findings of this study suggest satisfaction with the learning method, but still this study has certain limitations. The study population was very small, and the findings cannot be used for generalization. Secondly, it was conducted within one institution. Third, there was a lack of psychometric testing of the instrument. However, it is recommended that for generalization of the results inclusion of a larger sample with mixed methods and a multicenter approach can provide better results. Despite certain limitations, the results of this study will help the stakeholders to identify the areas where students’ learning needs were not addressed. They can accordingly plan, develop, and evaluate the SBL in education.
This study concludes that students found SBL an effective instructional technique. The use of simulation in teaching helps students to improve 3 domains of learning; knowledge, skills, and attitude. The results indicate that SBL was considered beneficial by the students. Lack of instructor knowledge and resources was reported as the main challenges. There is a serious need for a simulation-based training program for faculty members and students.
Footnotes
Related Articles.
Al-Drees AA, Khalil MS, Irshad M, Abdulghani HM. Students’ perception towards the problem based learning tutorial session in a system-based hybrid curriculum. Saudi Med J 2015; 36: 341-348.
Albarrak AI, Mohammed R, Abalhassan MF, Almutairi NK. Academic satisfaction among traditional and problem based learning medical students. A comparative study. Saudi Med J 2013; 34: 1179-1188.
Al-Yousuf NH. The clinical skills laboratory as a learning tool for medical students and health professionals. Saudi Med J 2004; 25: 549-551.
References
- 1.Cleland JA, Abe K, Rethans JJ. AMEE Guide No. 42: The use of simulated patients in medical education. Med Teach. 2009;31:477–486. doi: 10.1080/01421590903002821. [DOI] [PubMed] [Google Scholar]
- 2.Alinier G, Hunt G, Gordon R. Determining the value of simulation in nurse education: Study design and initial results. Nurse Educ Prac. 2004;4:200–207. doi: 10.1016/S1471-5953(03)00066-0. [DOI] [PubMed] [Google Scholar]
- 3.Al-Elq AB. Simulation-based medical teaching and learning. J Family Community Med. 2010;17:35–40. doi: 10.4103/1319-1683.68787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weinberg ER, Auerbach MA, Shah NB. The use of simulation for pediatric training and assessment. Curr Opin Pediatr. 2009;21:282–287. doi: 10.1097/MOP.0b013e32832b32dc. [DOI] [PubMed] [Google Scholar]
- 5.Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Technology-enhanced simulation for health professions education: A systematic review and meta-analysis. JAMA. 2011;306:978–988. doi: 10.1001/jama.2011.1234. [DOI] [PubMed] [Google Scholar]
- 6.Okuda Y, Bryson EO, DeMaria S, Jr, Jacobson L, Quinones J, Shen B, et al. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med. 2009;76:330–343. doi: 10.1002/msj.20127. [DOI] [PubMed] [Google Scholar]
- 7.Weller JM, Nestel D, Marshall SD, Brooks PM, Conn JJ. Simulation in clinical teaching and learning. Med J Aust. 2012;196:594. doi: 10.5694/mja10.11474. [DOI] [PubMed] [Google Scholar]
- 8.Marei HF, Al-Jandan BA. Simulation-based local anaesthesia teaching enhances learning outcomes. Eur J Dent Educ. 2013;17:44–48. doi: 10.1111/j.1600-0579.2012.00760.x. [DOI] [PubMed] [Google Scholar]
- 9.Al-Kadi AS, Donnon T. Using simulation to improve the cognitive and psychomotor skills of novice students in advanced laparoscopic surgery: a meta-analysis. Med Teach. 2013;35:47–55. doi: 10.3109/0142159X.2013.765549. [DOI] [PubMed] [Google Scholar]
- 10.Cherry RA, Ali J. Current concepts in simulation-based trauma education. J Trauma. 2008;65:1186–1193. doi: 10.1097/TA.0b013e318170a75e. [DOI] [PubMed] [Google Scholar]
- 11.McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86:706–711. doi: 10.1097/ACM.0b013e318217e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Franc-Law J, Ingrassia P, Ragazzoni L, Corte F. The effectiveness of training with an emergency department simulator on medical student performance in a simulated disaster. Canadian J Emerg Med. 2010;12:27–32. doi: 10.1017/s1481803500011982. [DOI] [PubMed] [Google Scholar]
- 13.Traynor M, Gallagher A, Martin L, Smyth S. From novice to expert: Using simulators to enhance practical skill. Br J Nurs. 2010;19:1422–1426. doi: 10.12968/bjon.2010.19.22.1422. [DOI] [PubMed] [Google Scholar]
- 14.Ennen CS, Satin AJ. Training and assessment in obstetrics: The role of simulation. Best Pract Res Clin Obstet Gynaecol. 2010;24:747–758. doi: 10.1016/j.bpobgyn.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen HB, Daniel-Underwood L, Van Ginkel C, Wong M, Lee D, Lucas AS, et al. An educational course including medical simulation for early goal-directed therapy and the severe sepsis resuscitation bundle: an evaluation for medical student training. Resuscitation. 2009;80:674–679. doi: 10.1016/j.resuscitation.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 16.Chakravarthy B, Ter Haar E, Bhat SS, McCoy CE, Denmark TK, Lotfipour S. Simulation in medical school education: review for emergency medicine. West J Emerg Med. 2011;12:461–466. doi: 10.5811/westjem.2010.10.1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steadman RH, Coates WC, Huang YM, Matevosian R, Larmon BR, McCullough L, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34:151–157. doi: 10.1097/01.ccm.0000190619.42013.94. [DOI] [PubMed] [Google Scholar]
- 18.McCoy CE, Menchine M, Anderson C, Kollen R, Langdorf MI, Lotfipour S. Prospective randomized crossover study of simulation vs. didactics for teaching medical students the assessment and management of critically ill patients. J Emerg Med. 2010;40:448–455. doi: 10.1016/j.jemermed.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 19.Reynolds A, Ayres-de-Campos D, Bastos LF, van Meurs WL, Bernardes J. Impact of labor and delivery simulation classes in undergraduate medical learning. Med Educ. 2008;13:14. doi: 10.3885/meo.2008.Res00285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ten Eyck RP, Tews M, Ballester JM. Improved medical student satisfaction and test performance with a simulation-based emergency medicine curriculum: a randomized controlled trial. Ann Emerg Med. 2009;54:684–691. doi: 10.1016/j.annemergmed.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 21.Heitz C, Ten Eyck R, Smith M, Fitch M. Simulation in Medical Student Education: Survey of Clerkship Directors in Emergency Medicine. West J Emerg Med. 2011;12:455–460. doi: 10.5811/westjem.2011.3.2107. [DOI] [PMC free article] [PubMed] [Google Scholar]


