Abstract
The ansa cervicalis is a loop of nerves that is usually formed by the union of ventral rami of spinal nerves C1, C2, and C3. It is located in the carotid triangle of the neck, lying superficial to the carotid sheath. During routine dissection, unilateral variation of the ansa cervicalis was observed. The superior root, arising from hypoglossal nerve, was initially bifurcated and later united to form a single superior root. IN addition, the inferior root consisted of fibres arising from the spinal accessory nerve, C1, C2 and C3 spinal nerves that joined separately. Fibres from the spinal accessory and C1 joined to form a single root. Thus, a ‘triple form’ of ansa cervicalis was observed. An interconnection was observed between the C2 and C3 fibres. Knowledge of such anatomical variations is important for surgery, clinical intervention or trauma involving the carotid triangle or the structures within or deep to this region.
Keywords: Ansa cervicalis, inferior root, spinal accessory nerve, superior root, spinal nerves
Implications for Practice:
-
What is known about this subject?
The common anatomy of the ansa cervicalis is well described in textbooks, however, variations are known to occur in some instances.
-
What new information is offered in this case study?
A novel anatomical variation of this nerve complex is described: a triple form of the ansa cervicalis with the inferior root formed by the fibres from the spinal accessory nerve, ventral rami of C1, C2, and C3 spinal nerves. The fibres from the spinal accessory nerve and C1 fibres joined to form a single root. The superior root had a bifurcated origin from the hypoglossal nerve.
-
What are the implications for research, policy, or practice?
Knowledge of anatomical variations of the ansa cervicalis is important for surgery, clinical intervention, and trauma involving the carotid region.
Background
The ansa cervicalis is a loop of nerves that originates from the upper cervical spinal nerves (C1, C2, and C3) that passes inferior and anterior to provide innervation to muscles involved with phonation and deglutition. It is formed by the union of the superior root (descendens hypoglossi) consisting of the C1 fibres that pass through the hypoglossal nerve, and the inferior root (descendens cervicalis) that is formed by the fibres of C2 and C3 spinal nerves. Nerves descend lateral to the internal jugular vein, and then pass anterior to it to join with the superior root in front of the common carotid artery embedded within the anterior layer of the carotid sheath.
The branches of the ansa cervicalis innervate the infrahyoid muscles, which are very important in maintaining phonation and deglutition.1 The infrahyoid muscles exert their action mainly on the larynx by supporting the laryngeal cartilages during phonation. Therefore, any injury to these muscles through their nerve supply would cause disturbance in phonation in professional voice users, where the pitch of their voice would change gradually.2
The ansa cervicalis is commonly used for nerve anastomosis with the recurrent laryngeal nerve due to its proximity to the larynx and because its sacrifice causes no serious functional or cosmetic sequelae.3–6 Because the ansa cervicalis is located in the vicinity of major nerves and vessels of the neck, knowledge of topography and morphology of this loop is very important. Any variation in its course, formation, or branching pattern could pose complications in neurorrhaphy and neck dissections.3,7
Variations in the formation, course, and branching pattern of the ansa cervicalis are likely asymptomatic and would only be made apparent during specific radiological investigation (e.g., local ultrasound) or surgery, with most variations coming to light as incidental findings. Knowledge of the variations of the ansa cervicalis is important during skull base surgery, thyroid surgeries, thyroplasty, arytemid adduction, Teflon injection, carotid endarterectomy to avoid iatrogenic injuries to the ansa cervicalis, and inadvertent injuries to great vessels of the neck region.3 Here we present a case that describes variation in the formation of the ansa cervcialis in a South Indian adult cadaver.
Case details
During the routine cadaveric dissection of the left carotid triangle of a 70-year-old male cadaver (Department of Anatomy, Kasturba Medical College, Manipal, India) a unilateral variation was observed in the formation of the ansa cervicalis. Dissection was undertaken in accordance with local ethical and institutional requirements. The inferior root was formed by the fibres arising from the spinal accessory nerve, and the C1, C2, and C3 spinal nerves. The fibres arising from C1 and spinal accessory nerve joined to form a common root (Figure 1). Thus, a triple form of the ansa cervicalis was observed. An intercommunicating branch was observed between the C2 and C3 fibres (Figure 1).
Figure 1: Triple form of the ansa cervicalis with variant inferior root fibres in the left carotid triangle.
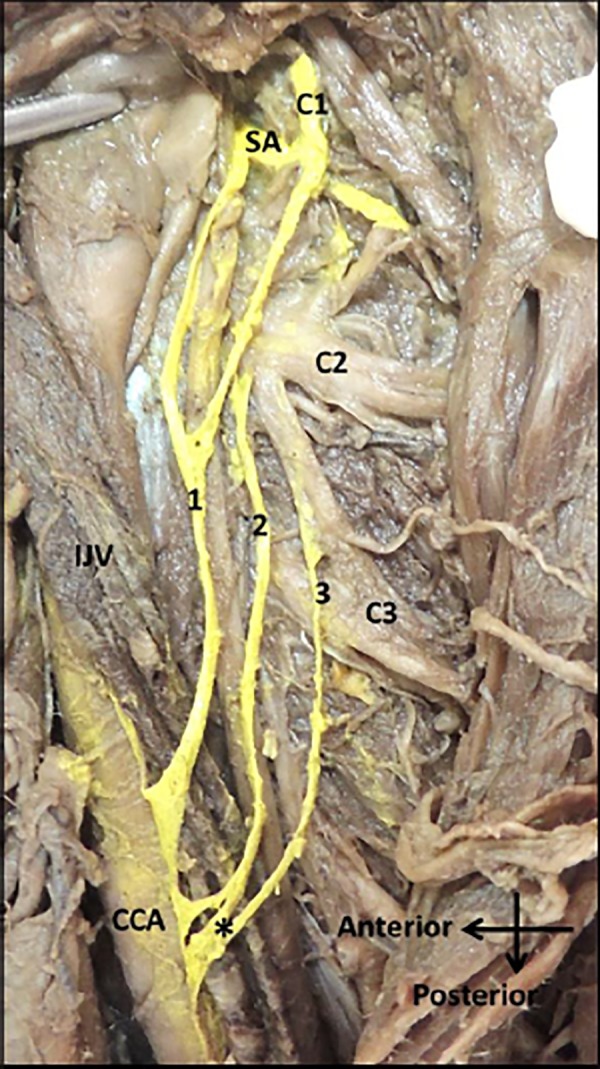
CCA: common carotid artery, IJV: internal jugular vein, SA: spinal accessory nerve, C1: first cervical spinal nerve, C2: second cervical spinal nerve, C3: third cervical spinal nerve, SR: superior root, 1: fibres from SA and C1, 2: fibres from C2, 3: fibres from C3, *: intercommunicating branch between C2 and C3 fibres. Nerves have been highlighted using digital imaging to indicate their location.
All nerve fibres passed superficial to the internal jugular vein to join with the superior root independently. The superior root arising from hypoglossal nerve was initially bifurcated, which later united to form a single superior root (Figure 2). The superior root was located medial to the posterior belly of the digastric muscle and lateral to the bifurcation of the common carotid artery. The superior root descended posterior to the common carotid artery and joined with the fibres of the inferior root deep to the inferior belly of the omohyoid muscle (Figure 2). A common trunk aroused from the loop that innervated the infrahyoid muscles. No other associated variations were observed.
Figure 2: Bifurcated superior root of the ansa cervicalis in the left carotid triangle.
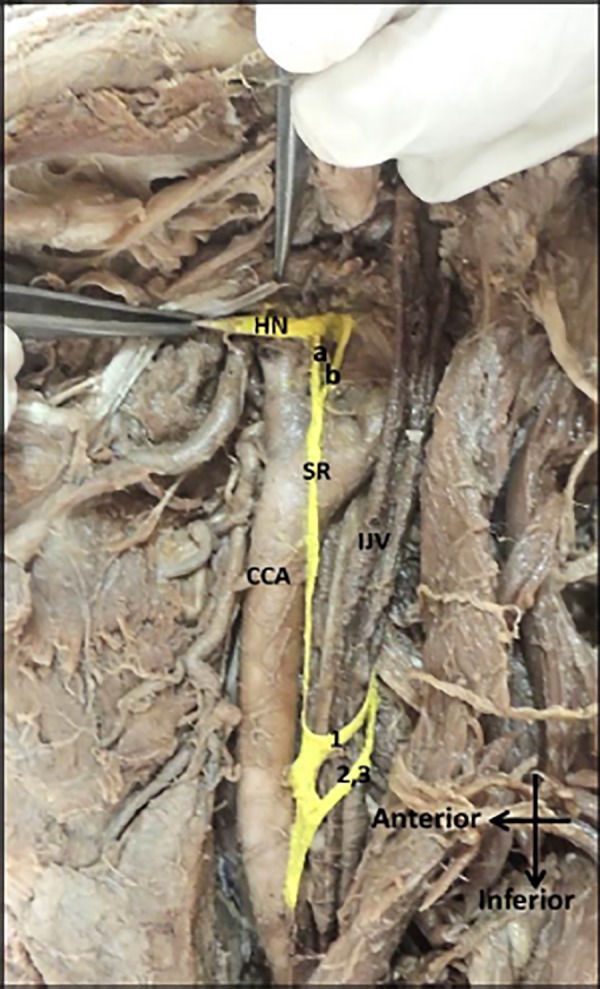
CCA: common carotid artery, IJV: internal jugular vein, HN: Hypoglossal nerve, a&b: bifurcated superior root from hypoglossal nerve, C2: second cervical spinal nerve, C3: third cervical spinal nerve, SR: superior root, 1: fibres from SA and C1, 2: fibres from C2, 3: fibres from C3. Nerves have been highlighted using digital imaging to indicate their location.
Discussion
Formation of the ansa cervicalis is normally from the descending branch of hypoglossal nerve and the descending branch of the cervical plexus.8 In human specimens the ansa cervicalis shows a great degree of variation in its origin and also distribution.9 The bifurcated origin of the superior root from the hypoglossal nerve, and multiple origins of inferior root fibres from the spinal accessory nerve, C1, C2, and C3 spinal nerves are an unusual finding reported in this case, and therefore accounts as a new variation of the ansa cervicalis.
The formation of inferior root varies considerably when compared to that of the superior root owing to the various cervical root contributions possible. In a study conducted by Poviraev and Chernikov on 160 cadavers, the inferior root was derived from the fibres of the C1–C4 spinal nerves, among which the C3 spinal nerve was the most important contributor.10 In 15 per cent of cases, formation of the inferior root is completed over the internal jugular vein.6
An absent inferior root has been described by Babu, where the fibres derived from the C2 and C3 spinal nerves joined the superior root independently.11 In the present case, the inferior root was absent with the fibres derived from the spinal accessory nerve, and the C1, C2, and C3 spinal nerves. Our finding partially corresponds with the findings of Babu and Khakhi et al.3,11
The ventral rami of the C2 and C3 spinal nerves joined the vagus nerve separately at different levels and the infrahyoid muscles were supplied directly from the vagus.12 An unusual origin of the inferior root from the sympathetic chain has been described by Chhetri and Berke,4 In a study conducted on 40 hemi-necks, two hemi-necks showed intercommunicating nerves between the C2 and C3 fibres.12 These intercommunicating branches may not pose any serious complications but is of academic interest for anatomists. Of the seven morphological variations of the ansa cervicalis, the variation presented in this case belongs to the triple form, where the fibres of the inferior root join the superior root independently.13 The morphology observed in this case report also highlights the fact that variations in this morphology are possible, however, the prevalence of such variations in or across different ethnic populations has not been described.
Although formation of the inferior root from the spinal accessory nerve is very rare, one case in the available literature has mentioned the formation of inferior root of the ansa cervicalis by the joining of two rootlets: one originating from the spinal accessory nerve and the other from a branch of the cervical plexus to the sternocleidomastoid has been reported. The fibres traversing the branch of the spinal accessory nerve was derived from the first segments of the cervical spinal cord.3
In relation to the internal jugular vein, the inferior root may either descend posterolateral or anterolateral to join the superior root. However, the dangers of an inadvertent injury to the great vessels are significant and it would be prudent to initially locate the individual nerve branches or to use a nerve stimulator to find the ansa cervicalis over the carotid sheath.4
The superior root usually is derived from the C1 fibres leaving the hypoglossal nerve. However, the superior root, although apparently coming out of the vagus nerve, in fact had its true origin in the cervical plexus.3,9 Dual superior roots arising from hypoglossal nerve have been reported.14,15 In the present case, dual superior roots were observed, however, both these roots later united to form a single superior root. Therefore, the term “bifurcated” superior root was preferred. This bifurcated superior root united before the bifurcation of the common carotid artery. It is important to be aware of such bifurcated roots since it lies in close proximity to the ascending pharyngeal artery. Very likely, this bifurcated root would enclose the ascending pharyngeal artery leading to further complication in furnishing arterial supply to the pharynx.
The triple form of the ansa cervicalis presented in this case informs physicians of another important contribution of the spinal accessory nerve and ventral rami of the C1 nerve to the formation of the inferior root of the ansa cervicalis. Such information is of relevance to interventions that directly involve the ansa cervicalis and the adjacent anatomical region.
ACKNOWLEDGEMENTS
The authors are grateful to the teaching and non-teaching staff for their help and support.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
Please cite this paper as: Quadros LS, Prasanna LC, D’souza AS, Singh A, Kalthur SG. Unilateral anatomical variation of the ansa cervicalis. AMJ 2015;8(5): 170–173. http//dx.doi.org/10.4066/AMJ.2015.2371
References
- 1.Nayak SR, Rai R, Krishnamurthy A, Prabhu LV, Potu BK. An anomalous belly of sternothryoid muscle and its significance. Rom J Morphol Embryol. 2009;50(2):307–8. [PubMed] [Google Scholar]
- 2.Ayyoubian M, Koruji M. A rare anatomical variant of ansa cervicalis: case report. Med J Islam Repub Iran. 2011;24(4):238–40. [Google Scholar]
- 3.Khaki AA, Shokouhi G, Shoja MM, Farahani RM, Zarrintan S, Khaki A. et al. Ansa cervicalis as a variant of spinal accessory nerve plexus: a case report. Clin Anat. 2006;19:540–3. doi: 10.1002/ca.20299. [DOI] [PubMed] [Google Scholar]
- 4.Chhetri DK, Berke GS. Ansa cervicalis nerve: review of the topographic anatomy and morphology. Laryngoscope. 1997;107(10):1366–72. doi: 10.1097/00005537-199710000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Vollala VR, Bhat SM, Nayak S, Raghunathan D, Samuel VP, Rodrigues V. et al. A rare origin of upper root of ansa cervicalis from vagus nerve: a case report. Neuroanatomy. 2005;4:8–9. [Google Scholar]
- 6.Rao TR, Shetty P, Rao SR. A rare case of formation of double ansa cervicalis: a case report. Neuroanatomy. 2007;6:26–7. [Google Scholar]
- 7.Verma R, Das S, Suri R. Unusual organization of the ansa cervicalis: A case report. Braz J Morphol Sci. 2005;22:175–7. [Google Scholar]
- 8.Caliot P, Dumont D, Bousquet V, Midy D. A note on the anastomoses between the hypoglossal nerve and the cervical plexus. Surg Radiol Anat. 1968;8:75–9. doi: 10.1007/BF02539711. [DOI] [PubMed] [Google Scholar]
- 9.Loukas M, Thorsell A, Tubbs RS, Kapos T, Louis Jr RG, Vulis M. et al. The ansa cervicalis revisited. Folia Morphol (Warsz) 2007;66:120–5. [PubMed] [Google Scholar]
- 10.Poviraev NP, Chernikov YF. Anatomy of the ansa cervicalis. Exerpta Medicu. 1967;21:219. [Google Scholar]
- 11.Babu PB. Variant inferior root of ansa cervicalis. Int J Morphol. 2011;29(1):240–3. [Google Scholar]
- 12.D’souza AS. Ray Biswabina. Study of the formation and distribution of the ansa cervicalis and its clinical significance. Eur J Anat. 2010;14(3):143–8. [Google Scholar]
- 13.Kuniak B, Klacansky J. A contribution to topographic anatomy of ansa cervicalis with reference to reinnervation of the larynx. Cesk Otolaryngol. 1982;31:170–5. [PubMed] [Google Scholar]
- 14.Pillay P, Partab L, Lazarus, Satyapal KS. The ansa cervicalis in fetuses. The ansa cervicalis in fetuses. 2012;30(4):1321–6. [Google Scholar]
- 15.Quadros LS, Bhat N, Babu A, D’souza AS. Anatomical variations in the ansa cervicalis and innervation of infrahyoid muscles. Int J Anat Res. 2013;1(2):69–74. [Google Scholar]


