Abstract
Identification of individuals is the mainstay of any forensic investigation especially in cases of mass disasters when mutilated remains are brought for examination. Dental examination helps in establishing the identity of an individual and thus, has played a vital role in forensic investigation process since long. In this regard, description on the role of enamel hypoplasia is limited in the literature. The present article reviews the literature on the enamel hypoplasia and discusses its utility in forensic identification. Enamel hypoplasia is a surface defect of the tooth crown caused by disturbance of enamel matrix secretion. Enamel defects can be congenital or acquired. In cases of mass disasters, or when the body is completely charred, putrefied and mutilated beyond recognition, the unique dental features can help in identification of the victims.
Keywords: Enamel hypoplasia, forensic odontology, mass disasters
INTRODUCTION
Human identification is one of the most challenging tasks one has been confronted with whenever a catastrophe strikes. Identification of the victims of the disaster is mandatory from a judicial point of view for settlement of wills, insurance payments and disposal of deceased estate as well as from a humanitarian point of view for the relatives to claim the body for last rites according to their religious beliefs.[1] In order to establish a positive identification, the available antemortem data is compared with the postmortem findings on the skeleton.[2] Procedures such as DNA fingerprinting, dental analysis, identification using scars, tattoos, recognition using clothes and belongings, autopsy findings, analysis of skeletal remains can all be used to identify an individual.[3] Dental identification remains one of the most reliable and widely applied parameter in identification.[4] Forensic odontology has played a pivotal role in identification of persons in various scenarios like in mass disasters, crime investigations, ethnic studies as well as in cases of decomposed, and disfigured remains in traffic accidents, fires, and bomb blasts.[4] The reason why dentition is used so often in identification is because dental tissue is amongst the hardest structures in the human body which is resistant to a number of adverse conditions such as incineration, immersion, trauma, mutilation, and putrefaction.[5] Due to its durability and ability to withstand very high temperatures without appreciable loss of microstructure, it can survive long after the soft and skeletal tissues have been destroyed.[6] Furthermore, because of their impervious nature, they serve as an excellent source of DNA, which can ascertain the identification in catastrophic conditions.[7] Teeth are conventionally used in the determination of age, sex, and ethnicity. Calcification and eruption are the two developmental factors that are considered while estimating the age from dentition, while a combination of odontometric dimensions can be used for estimation of sex accurately.[8] Apart from its application in anthropological studies, tooth can be a valuable source of toxicological information, for it is an imperative site of deposit of exogenous substances, which may be accumulated in the pulp or calcified tissues.[9] With an overview of the diverse applications of teeth in forensic medicine, the present report discusses the importance of enamel hypoplasia in identification. Enamel hypoplasia appears as scars on the teeth and can provide valuable information in identification of the deceased. However, description of this entity is limited in forensic literature. The present article reviews the literature on the enamel hypoplasia and discusses its utility in the identification of individuals in forensic examinations.
ENAMEL HYPOPLASIA
Ameloblasts are the cells that produce the enamel. Their life cycle is divided into six stages that include morphogenetic, organizing, formative, maturative, protective, and desmolytic. Amelogenesis that refers to the formation of enamel occurs during the formative and maturative stages of the ameloblasts. Enamel matrix is secreted in the formative stage where as mineralization of the enamel matrix occurs in the maturation stage. The principal expressions of pathologic amelogenesis are the hypoplasia, hypocalcification or hypomineralization. Enamel hypoplasia occurs if matrix formation is affected and may manifest as pitting, grooving or even total absence of enamel. Hypomineralization results when maturation is disturbed and is manifested in the form of opaque or chalky areas on normally contoured enamel surfaces. Thus, disturbance either in matrix formation or in calcification can occur depending chiefly on the stage of tooth formation at the time of injury.[10]
Development defects of enamel (DDE) comprise of mainly dental defects such as hypoplasia and diffuse and demarcated opacities; fluorosis and amelogenesis imperfecta. Enamel hypoplasia, thus, is a surface defect of the tooth crown that is caused by a disturbance of enamel matrix secretion, defective calcification or defective maturation.[11] Enamel hypoplasia or hypo mineralization may be caused by hereditary factors and environmental factors that include systemic factors such as nutritional factors, exanthematous diseases like measles and chicken pox, congenital syphilis, hypocalcemia, birth injury or premature birth, fluoride ingestion or idiopathic causes, and local factors such as infection or trauma from a deciduous tooth. Hereditary enamel hypoplasia/hypomineralization is known as amelogenesis imperfecta. It is transmitted in the family as a mendelian dominant trait which affects enamel of all the teeth, deciduous as well as permanent. Environmental enamel hypoplasia/hypo mineralization of systemic or local origin is also termed as “chronologic hypoplasia”. This lesion is found in areas of those teeth where the enamel was being formed during the systemic or local disturbance. Since the formation of enamel extends over a long period and the systemic or local disturbance, in most cases are of short duration, the defect is limited to a circumscribed area of the affected teeth or tooth. Thus knowing the chronologic development of deciduous and permanent teeth will make it possible to determine from the location of the defect, the approximate time at which the injury occurred.[12,13]
The basic pathology in DDE is the result of abrupt, short-term or long-term ameloblastic insults during the secretory or maturation phase of the development of tooth; any systemic illness, disturbance, deficiency or prematurity of neonate or local trauma can lead to DDE.[14] Enamel hypoplasia can also be seen in other pediatric conditions in which hypocalcemia is a major sign as in rickets, prematurity and neonatal tetany.[15] Furthermore, disturbances in the development of the enamel of permanent teeth can result from trauma to the primary teeth because of the close proximity of the root of the primary teeth to their permanent successors.[16] Enamel hypoplasia may be inherited or may result from an illness, malnutrition, trauma or due to fluorosis.[11] Although it can occur in any permanent tooth, the most commonly involved sites of hypoplasia are the permanent first molars and incisors with specific areas of defect and well-demarcated areas of hypomineralization.[17] The secretory phase for development of the permanent incisors and first molars begins in utero whereas the maturation process begins at birth and thus any trauma of inadequate mineralization can result in DDE.[14]
Molar incisor hypomineralization” (MIH), is a more specific form of DDE characterized by hypomineralization due to systemic illness, which can be seen as translucency in the enamel.[18] Environmental enamel hypoplasia/hypomineralization due to systemic factors are commonly manifested in the first permanent molars and incisors. Clinical studies indicate that enamel hypoplasia involve those teeth that form within the 1st year of birth. So, most frequently incisors and first permanent molars are affected. Hence, this condition is termed as “molar incisor hypomineralization.” When presented clinically these hypomineralized defects frequently break down because of the masticatory pressure and are seen as mixed areas of hypoplasias and hypomineralizations. Premolars and 2nd, 3rd molars are seldom affected, since their formation does not begin until age of 3 years or later.
Environmental enamel hypoplasia/hypomineralization due to local factors is also called as “turners hypoplasia/hypomineralization” seen most commonly in permanent maxillary incisors or upper lower premolars. Turner's hypoplasia usually manifests as a portion of missing or diminished enamel, which affects one or more than one permanent tooth in the oral cavity.[19] It commonly affects single permanent tooth because of infection of the corresponding deciduous tooth. Any degree of defects ranging from mild brownish discoloration of enamel (hypomineralization) to severe pitting and irregularity of tooth crown (hypoplasia) depending on severity of infection [Figure 1]. Similarly, when a deciduous tooth has been driven into the alveolus and has disturbed the permanent bud, it can manifest as a yellowish or brownish stain or pigmentation of the enamel usually on the labial surface or a true hypoplastic pitting defect or deformity.
Figure 1.
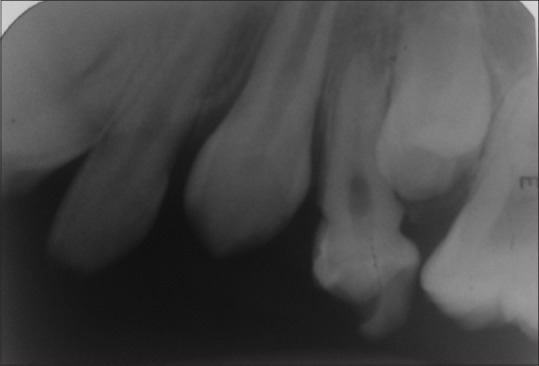
Radiograph showing turner's hypoplasia of upper first premolar
Different types of enamel hypoplasia have been identified such as pit type, plane type, and linear enamel type.[11] In MIH, there is a definite correlation between the color, histology, porosity and mineral content. Yellow-brown defects are deeper, extending from the dento-enamel junction to the enamel surface, whereas white creamy defects are usually less porous and vary in depth and are typically limited to the inner enamel.[18] Biochemically, it is found that, hypomineralized enamel had a higher content of carbon and lower levels of calcium and phosphorous as compared to the normal enamel.[20]
FORENSIC ODONTOLOGY, IDENTIFICATION AND SIGNIFICANCE OF DOCUMENTATION OF DENTAL DEFECTS
Forensic odontology has been playing a significant role in the identification of unknown, dismembered and commingled human remains. Dental restorations, diseased conditions, disorders, prostheses and radiological examinations of the teeth may help in identification of the victims of mass disasters.[21] The reports suggest that various kinds of dental characteristics helped in identification process in the recently experienced disasters. According to a communication,[22] about 80% of the non-Thai victims were identified by dental characteristics in Phuket, Thailand when a powerful tsunami hit South-East Asia in December 2004. All the dental characteristics including the information pertaining to the conditions of the teeth are entered in a standardized dental disaster victim identification (DVI) protocol[23](DVI form of the Interpol) and then matched with the available antemortem data. The process of comparison involves certain important features of the teeth which are individualistic to a person,[24] and include dental fillings, dental enamel hypoplasia, extractions, missing teeth, extra teeth, rotations, supernumerary cusps, features of the occlusal aspect of the teeth, various other dental anomalies and special characteristics as the taurodontism and carabelli cusps, etc.
CONCLUSIONS
Enamel defects have been widely used by anthropologists for the investigation of growth disruptions in the past populations as they provide a permanent record for disturbances during much of a child's developmental period.[25] To the best of our knowledge, there is no reported case of enamel hypoplasia being used for identification in forensic investigation. The fact that these defects are a reflection of the events in utero as well as after birth means that their unique profile can help in identification of victims of mass disasters as well as the bodies of those which are completely charred, putrefied and mutilated and thus, revolutionize the face of forensic identification. It is suggested that dental practitioners make a note of these defects in their routine practice so that the information is available for matching dental records during forensic investigations.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Martin-de las Heras S, Valenzuela A, Villanueva E, Marques T, Exposito N, Bohoyo JM. Methods for identification of 28 burn victims following a 1996 bus accident in Spain. J Forensic Sci. 1999;44:428–31. [PubMed] [Google Scholar]
- 2.Definis Gojanovic M, Sutlovic D. Skeletal remains from World War II mass grave: From discovery to identification. Croat Med J. 2007;48:520–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Marjanovic D, Durmic-Pasic A, Bakal N, Haveric S, Kalamujic B, Kovacevic L, et al. DNA identification of skeletal remains from the World War II mass graves uncovered in Slovenia. Croat Med J. 2007;48:513–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Saxena S, Sharma P, Gupta N. Experimental studies of forensic odontology to aid in the identification process. J Forensic Dent Sci. 2010;2:69–76. doi: 10.4103/0975-1475.81285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manjunath BC, Chandrashekar BR, Mahesh M, Vatchala Rani RM. DNA profiling and forensic dentistry – A review of the recent concepts and trends. J Forensic Leg Med. 2011;18:191–7. doi: 10.1016/j.jflm.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Shetty M, Premalatha K. ABO Blood Grouping from Tooth Material. J Indian Acad Forensic Med. 2012;32:336–8. [Google Scholar]
- 7.Pretty IA, Sweet D. A look at forensic dentistry – Part 1: The role of teeth in the determination of human identity. Br Dent J. 2001;190:359–66. doi: 10.1038/sj.bdj.4800972. [DOI] [PubMed] [Google Scholar]
- 8.Krogman WM, Iscan YM. 2nd ed. Springfield, Illinois, USA: Charles C; 1986. The Human Skeleton in Forensic Medicine. [Google Scholar]
- 9.Cattaneo C, Gigli F, Lodi F, Grandi M. The detection of morphine and codeine in human teeth: An aid in the identification and study of human skeletal remains. J Forensic Odontostomatol. 2003;21:1–5. [PubMed] [Google Scholar]
- 10.Via WF., Jr Enamel defects induced by trauma during tooth formation. Oral Surg Oral Med Oral Pathol. 1968;25:49–54. doi: 10.1016/0030-4220(68)90196-5. [DOI] [PubMed] [Google Scholar]
- 11.Lv P, Gao XJ. Phenotype analysis and the molecular mechanism of enamel hypoplasia. Beijing Da Xue Xue Bao. 2009;41:121–3. [PubMed] [Google Scholar]
- 12.Rajendran R, Sundaram S, editors. In: Shafer's Textbook of Oral Pathology. 7th ed. India: Elsevier; 2012. Developmental disturbances of oral and para oral structures; pp. 49–55. [Google Scholar]
- 13.Kumar G. 13th ed. India: Elsevier; 2011. Orban's Oral Histology and Embryology; pp. 72–87. [Google Scholar]
- 14.Nelson S, Albert JM, Lombardi G, Wishnek S, Asaad G, Kirchner HL, et al. Dental caries and enamel defects in very low birth weight adolescents. Caries Res. 2010;44:509–18. doi: 10.1159/000320160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nikiforuk G, Fraser D. The etiology of enamel hypoplasia: A unifying concept. J Pediatr. 1981;98:888–93. doi: 10.1016/s0022-3476(81)80580-x. [DOI] [PubMed] [Google Scholar]
- 16.Gomes AC, Messias LP, Delbem AC, Cunha RF. Developmental disturbance of an unerupted permanent incisor due to trauma to its predecessor. J Can Dent Assoc. 2010;76:a57. [PubMed] [Google Scholar]
- 17.Fagrell TG, Ludvigsson J, Ullbro C, Lundin SA, Koch G. Aetiology of severe demarcated enamel opacities – An evaluation based on prospective medical and social data from 17,000 children. Swed Dent J. 2011;35:57–67. [PubMed] [Google Scholar]
- 18.Sapir S, Shapira J. Clinical solutions for developmental defects of enamel and dentin in children. Pediatr Dent. 2007;29:330–6. [PubMed] [Google Scholar]
- 19.Bhushan BA, Garg S, Sharma D, Jain M. Esthetic and endosurgical management of Turner's hypoplasia; a sequlae of trauma to developing tooth germ. J Indian Soc Pedod Prev Dent. 2008;26(Suppl 3):S121–4. [PubMed] [Google Scholar]
- 20.Jälevik B. Enamel hypomineralization in permanent first molars. A clinical, histo-morphological and biochemical study. Swed Dent J Suppl. 2001;149:1–86. [PubMed] [Google Scholar]
- 21.Girish KL, Rahman FS, Tippu SR. Dental DNA fingerprinting in identification of human remains. J Forensic Dent Sci. 2010;2:63–8. doi: 10.4103/0975-1475.81284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schuller-Götzburg P, Suchanek J. Forensic odontologists successfully identify tsunami victims in Phuket, Thailand. Forensic Sci Int. 2007;171:204–7. doi: 10.1016/j.forsciint.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 23.DVI form of the Interpol. [Last accessed on 2014 Oct 09]. Available from: http://www.interpol.int/content/download/10801/76833//10//PMForm.pdf .
- 24.Kaur S, Krishan K, Chatterjee PM, Kanchan T. Analysis and identification of bite marks in forensic casework. Oral Health Dent Manag. 2013;12:127–31. [PubMed] [Google Scholar]
- 25.King T, Hillson S, Humphrey LT. A detailed study of enamel hypoplasia in a post-medieval adolescent of known age and sex. Arch Oral Biol. 2002;47:29–39. doi: 10.1016/s0003-9969(01)00091-7. [DOI] [PubMed] [Google Scholar]


