Abstract
The Japanese Society for Dialysis Therapy (JSDT) collects the clinical data from all the facilities to create a nation-wide registry system named JSDT Renal Data Registry (JRDR). This survey was begun in 1966 as a form of facility survey. Patient survey started in 1983. More than 95% of facilities respond to the survey on the basis of voluntary work of facility staffs. Therefore, JRDR has the longest history and the most comprehensive coverage. As for the prevalent patients, 304,856 patients are treated by dialysis therapy in Japan as of the year 2011. The demographics of the Japanese dialysis population have been markedly changing in terms of age, primary diagnoses and dialysis vintage. The mean age of prevalent population reaches 66.55 years at the end of 2011. The increase in the numbers of dialysis population is due to the growth of those older than 65 years old. Patients with the vintage longer than 20 years account for 8% of the entire population. Around 38 thousands patients started their dialysis treatments, whereas 31 thousands deceased. The disease burden of cardiovascular diseases as well as infection is substantial due to the demographic changes. Many evidences have been reported from the data obtained from JRDR to date. These findings covers a wide range of dialysis practice and are utilized for the development of JSDT guidelines. Therefore, JRDR has provided indispensable and fundamental data of Japanese dialysis population.
Keywords: aging population, demographics, The Japanese Society for Dialysis Therapy Renal Data Registry (JRDR)
OVERVIEW OF JRDR
Japanese Society for Dialysis Therapy (JSDT) has been performing a survey of dialysis patients as well as dialysis facilities in Japan annually. JSDT develops a nation-wide registry system from thus collected data, named ‘JSDT Renal Data Registry (JRDR)'. In this article, we review the overview of JRDR, several important findings derived from the registry and significance of JRDR.
History of JRDR
In 1963, the first chronic hemodialysis (HD) therapy was performed in Japan.1 In 1966, 3 years after the first chronic HD therapy, annual survey as a form of facility survey was started. In 1983, 20 years after the first HD therapy in Japan, the current survey system designed for individual patient was implemented.1 Thereafter, although some modifications, mostly concerning items to be collected, were made, the overall system has remained the same.
Data collection methods
JSDT headquarters send questionnaires every November to all dialysis facilities where patients receive dialysis treatment. Thereafter, the staffs at each dialysis facility fill the questionnaires with the data of all patients at the end of every year on the basis of totally voluntary work of the staffs at each facility. And they send them back to the JSDT headquarters.
There are two forms of questionnaires: one is a paper version and the other is an electrical version, which was implemented in 1994. Both include facility survey and the critical data in patient survey in common; the latter contains patient demographics, outcomes, comorbidities, and important clinical conditions. The electrical version as a form of Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) collects more detailed data (Appendix indicates items that were collected at the end of 2013).2
Facility survey and patient survey
Questionnaires consist of facility survey and patient survey.
Facility survey comprises the data of each facility and includes such parameters as numbers of patients, modality, numbers of staffs in charge of dialysis patients, and status of water purification (Appendix).
Patient survey collects these data for individual patients. The patients to be investigated are all of the patients who are treated by dialysis at any moment during the year.
Patient survey includes data as follows: (1) demographic data such as anonymized name, sex, date of birth, month of initiation, primary diagnosis, and place of living; (2) modalities of therapies, such as HD, hemodiafiltration, or peritoneal dialysis (PD); (3) outcomes such as death, transplantation or withdrawal, and the occurrence of cardiovascular events and fracture; (4) outcome-relating factors such as body size, urea, creatinine, mineral bone disorder (MBD) markers, anemia, blood pressure, and pulse rate; (5) PD relating data including PD prescription, dialysis dose, the results of peritoneal equilibration test, and infection rate only for PD patients.
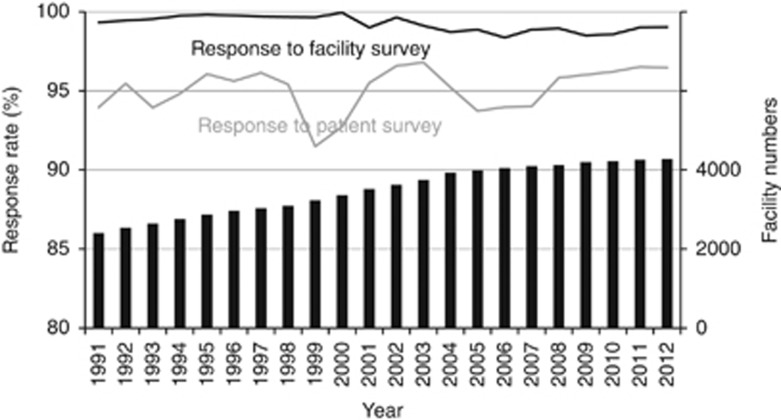
Figure 1 indicates the trend of response rate for facility survey and patient survey, as well as facility numbers. Facility numbers themselves are increasing steadily and exceeded 4000 past several years. The response rates have been around 95% for patient survey and more than 98% for facility survey. Therefore, JRDR a is comprehensive survey of the Japanese dialysis population.
Figure 1.
Trend of response rate and facility numbers. Facility numbers themselves are increasing steadily and exceeded 4000 in the past several years. About 95% of total facilities responded to patient survey. Moreover, more than 98% of facilities responded to facility survey. This figure was modified from the data that appeared in the preface of the Japanese version of the annual report of each year with permission of CRDR. CRDR, The Committee of Renal Data Registry of the Japanese Society for Dialysis Therapy.
DEMOGRAPHICS OF THE JAPANESE DIALYSIS POPULATION AND THEIR CHANGE
Overview of the Japanese dialysis population. As of 2011, 304,856 patients were receiving dialysis therapies.2 This figure corresponds to 2385.4 patients per million of general population. The numbers of facilities that responded to the survey was 4213. More than 125 thousands of dialysis machines existed in Japan.
During the year 2011, 38,613 patients started their dialysis and 30,743 patients deceased. The number of deceased patients has been continuously increasing, whereas the number of incident patients almost remains the same during the past several years. The differences of these two figures correspond to the annual increase in dialysis population. Therefore, the increase in the dialysis population becomes dull.
Most of patients as much as 97% of total dialysis population receive HD, whereas the remaining 3.2% (9642 patients) are treated by PD. Although only 0.1% (327 patients) receives home-based HD, the population treated by home-based HD is growing sharply during the past several years.
The male patients are more predominant (62.6% of total population) than female patients for all vintage groups. However, the differences become smaller for the patients with longer vintage, e.g., male patients account for 54.2% of those who have been treated for more than 25 years. The fact might indicate that the survival is better among female patients.
Dialysis population is rapidly aging. The average ages of dialysis patients were 46.23 years for prevalent patients and 50.05 years for incident patients in 1981.3 The average age of the incident population was 67.84 years, and prevalent population was 66.55 years as of 2011.
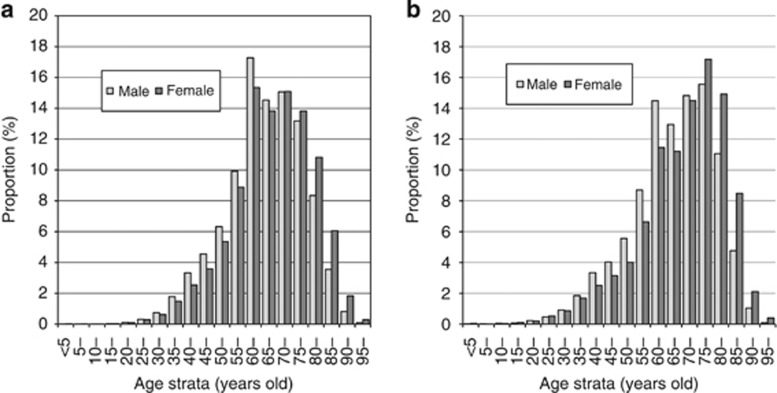
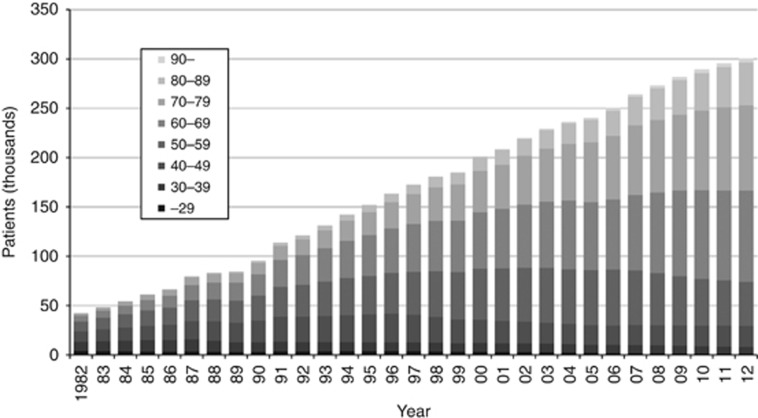
The most prevalent age group is 60–64 years for male and female prevalent patients (Figure 2a). The former is the reflection of baby boomers. The proportion of elderly over 75 was larger for female (32.8%) than male (26.0%). On the other hand, for both male and female the mode age stratum of incident population was 75–79 years (Figure 2b). Figure 3 shows the trend of population by age. The population under 60 years has remained unchanged during the past 20 years. The increase of the total population is due to the increase of the patients over 60 years of age (Figure 3).4
Figure 2.
Distribution of the patients by age strata. (a) For prevalent patients, the mode of age strata is 60–64 years both for male and and female patients. The proportion was larger for female patients over 75 years of age. (b) For incident population, 75–79 years old strata are the most populous for both male and female patients. Pale bar and filled bar represent male and female patients, respectively.
Figure 3.
Trend of population by age. Numbers of the prevalent dialysis patients are increasing. Trend of age distribution demonstrates that the increase of the total population is due to the increase of the patients over 60 years of age.
Patients with a long history of dialysis are increasing in their numbers. The percentage of the patients with more than 20 years on renal replacement thrapies is increasing and as much as 7.6% as of 2011. The patient with the longest vintage receives dialysis treatment for more than 43 years.
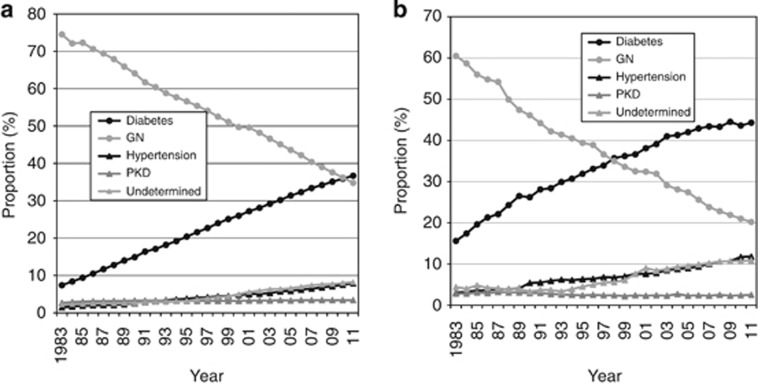
The most common primary diagnosis of end-stage renal disease (ESRD) had been glomerulonephritis before 1997 for incident patients. However, numbers of patients who started dialysis therapies due to diabetes exceeded those of glomerulonephritis in 1997. The proportions of diabetes and hypertension as primary diagnoses of ESRD have steadily been increasing thereafter (Figure 4a). The same trend is observed also for prevalent patients. Diabetes has overtaken glomerulonephritis as of the year 2011 and diabetes has become the most common primary diagnosis also among the prevalent population (Figure 4b).
Figure 4.
Proportion of primary diagnoses of ESRD. Diabetes is most predominant in primary diagnosis of end-stage renal disease (ESRD) both for (a) the incident population as well as (b) the prevalent population. Patients with ESRD due to hypertension are also increasing. GN, glomerulonephritis; PKD, polycystic kidney disease.
Statistics of deceased patients
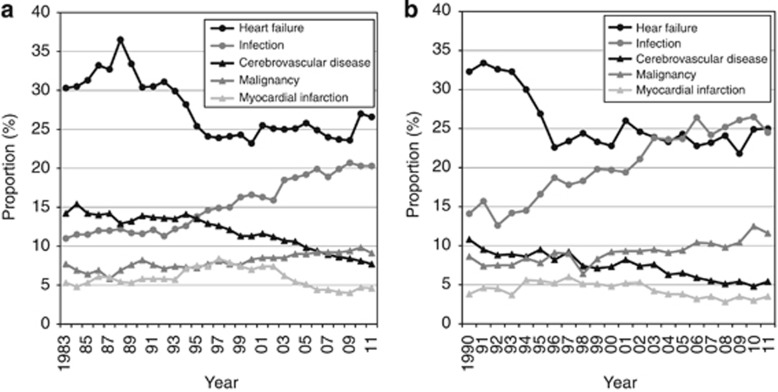
The trend of causes of death among the dialysis population indicates that cardiovascular mortality including heart failure, stroke, and myocardial infarction are most prevalent and accounts for almost 40% of all causes of mortality. The proportion of those who die from infection is also growing (Figure 5a). A similar trend can be found among the incident population, whereas the burden of infection on causes of death is larger than that of the prevalent population (Figure 5b).
Figure 5.
Trend of causes of death. (a) Heart failure is the leading cause of death in prevalent patients, whereas the population who die from infection is also growing. (b) For incident patients, the proportion of patients that died from infection is larger than that of prevalent patients, and is almost the same as that of heart failure.
Crude mortality rate is increasing, probably due to aging and the changes in primary diagnoses. The cured mortality rate exceeded 10% in the year 2011 for the first time.
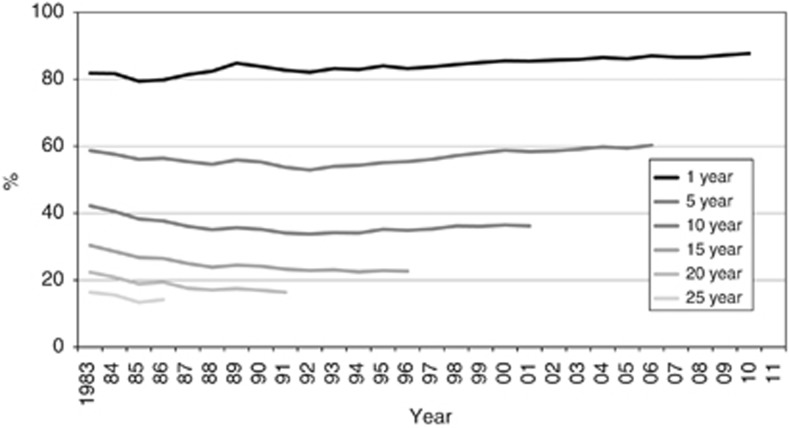
The trends of crude cumulative survival rates show that the survival rates less than 15 years are improving. However, those of the longer than 15 years are declining, probably due to the fact that the population is aging (Figure 6).
Figure 6.
Trends of crude cumulative survival rates by the year of initiation. The survival rates during the shorter period less than 15 years are improving. However, those of the longer than 15 years are declining, probably due to the fact that the population is aging.
Thus trend in epidemiology of Japanese dialysis patients can be summarized as increase in numbers of total population, elderly patients, or ESRD due to diabetes or hypertension, and patients with long ESRD history. Similar trends were also reported in the United States Renal Data System5 and ANZDATA.6 Cardiovascular disease as well as infection are predominant causes of death among the Japanese dialysis population, probably due to the changes of demographics.
PERIODICALLY PUBLISHED REPORTS OF JRDR
JRDR has published its summary as four types of publications. These are (1) an illustrated and draft version of the annual report, (2) integrated tables as a form of CD-ROM, (3) Japanese version of the annual report, and (4) English version of the annual report.
Illustrated and draft version
The illustrated version of the annual report has been delivered for every member facility and all Councilors of JSDT during the period of the annual meeting of JSDT held every June. This version includes the summaries of patient demographics and the newly surveyed items. These data depend on the data collected before April of the same year, only 4 months after the date of survey. Therefore, the data are subjected to be modified by further inquiry made by JSDT headquarters for each facility about missing or erroneous data. However, its graphically presentable nature made this version useful and a PowerPoint (Microsoft Corporation) file can be downloaded through JSDT web page.
CD-ROM version of annual reports
This version is made until every November, when the questionnaires of the year are sent to all facilities and the CD-ROM version of annual report is also sent together with the questionnaires.
The data used for this version have been cleaned through the inquiry for the facility. Therefore, we consider the data used in this version or thereafter as fixed ones. These ‘fixed' data are also used for Japanese and English versions of annual reports, which depend on the data appearing in the CD-ROM version.
The CD-ROM includes thousands of tables (6431 tables in the CD-ROM for the year 2012). Most of them have the structure of a summarized sheet in which both columns and rows are designed for all items that were collected. Some of them are stratified by therapeutic modalities (such as HD, hemodiafiltration, or PD), patient background (those who have their vintage more than 2 years), or therapeutic conditions (those receiving dialysis three times a week). Therefore, this version is a very comprehensive summary of the collected data.
The member of JSDT can refer to this version through the web page of JSDT.
Japanese version of the annual report
This version depends on the data that appeared in the CD-ROM version and is published in the January issue of the Journal of Japanese Society for Dialysis Therapy, an official journal of JSDT. The essential tables are selected and reviewed in this article. The modifications of the questionnaires used for data collection of the year are also described, if any. We recommend for the users to cite this or the English version described below, because the data on which this article depends are the fixed one as mentioned above.
English version of the annual report
The last version of the report is the English version of the annual report, entitled ‘Overview of regular dialysis treatment in Japan (as of 31 December ****)', **** indicates the year when the data were surveyed. This version of the annual report is published in Therapeutic Apheresis and Dialysis, the other official journal of JSDT, usually in the December issue, when almost 2 years after the survey was performed.
IMPACT OF JRDR
JSDT guidelines that depend on JRDR data
JSDT has published 19 guidelines and statements to date including the revised version of the previous one. More than half of them were translated into English and appeared in Therapeutic Apheresis and Dialysis.7, 8, 9, 10, 11, 12, 13, 14, 15, 16 Almost all of these guidelines and statements cited the results of the annual reports or utilized the data of JRDR themselves. Therefore, JRDR has contributed to the improvement of the management of Japanese dialysis population. We also believe in the significance and impact of JRDR in improving the prognoses of the Japanese dialysis population.
Evidences and their publications obtained through JRDR
More than 20 articles except for the annual reports have been published to date. The themes of the articles are diverse: therapeutic conditions of HD, cardiovascular complications, MBDs, dialysis initiation, and others.
Since the year 2008, the registry database was opened for members of JSDT and the studies on JRDR have been invited. Some of them had already been published and some others are under preparation.
Here we introduce some principal findings obtained from JRDR.
Therapeutic conditions and survival in an early study
Shinzato et al.17 investigated the factors that affect mortality of dialysis population in 1997, and demonstrated that age, diabetes, male, Kt/V<1.8, duration of treatment <5 h, protein catabolic rate <0.9 g/kg/day, and body weight reduction <4% or >8% during a session all related to the worse outcome, which can be applicable for the contemporary dialysis population.
Cardiovascular complications
In the field of cardiovascular complications, several findings are obtained. The study on the prevalence of hypertension among the dialysis population indicated that the proportion of the patients with hypertension was high, although many patients took anti-hypertensive drugs.18 On the other hand, the patients on anti-hypertensive medication, especially renin–angiotensin system inhibitors, experienced better survival compared with those who are not.19 A novel finding that elevated pulse rate is related to worse outcome is also demonstrated by JRDR data.20
Mineral bone disorders
MBD is another field where many evidences are reported from JRDR. The relation of MBD markers including phosphate, calcium, and parathyroid hormone to survival are investigated. The study published in 200821 was cited in the previous version of the MBD guideline,9 whereas the article published in 2013 (ref. 22) investigated 3 years mortality and was adopted by the revised version of the CKD-MBD guideline.15 Magnesium is one of the important minerals but is poorly investigated under the light of survival. Sakaguchi et al.23 demonstrated elegantly that hypomagnesemia can be related to both cardiovascular and non-cardiovascular mortality. This is one of the first reports that showed the relationship between magnesium and mortality. Hip fracture is a common consequence of CKD-MBD. Wakasugi et al.24 intensively investigated the incidence of hip fracture among the dialysis population and found interesting findings including regional variation of its incidence.25 Maruyama et al.26 found that higher alkaline phosphatase can be associated with the incidence of hip fracture among prevalent patients, as well as all-cause and cardiovascular mortality. Dialysis-related amyloidosis was also investigated as the history of CTS as its proxy. Numbers of patients with carpal tunnel syndrome history increased along with dialysis vintage. Age, albumin, diabetes, and β2 microglobulin clearance are also related to carpal tunnel syndrome incidence.27
Incident dialysis population
The timing of initiation of dialysis is one of the fields that have evoked much discussion. JSDT28 as well as the Japanese Society of Nephrology29 published guidelines of dialysis initiation in 2013. Both guidelines cited the evidences derived from JRDR, which demonstrated that estimated glomerular filtration rate <2 ml/min/1.73 m2 or >8 ml/min/1.73 m2 were related to worse outcome.30 Ogata et al.31 investigated the relationship between as much as 81 factors and incidence of dialysis patients, which shed light on the factors to be modified in reducing the burden of the dialysis population.
Trends of dialysis population were also investigated. Wakai et al. showed that diabetic and aged incident dialysis patients are increasing in their numbers.32 Iseki et al.33 also demonstrated that male is becoming more predominant than female gender among the incident dialysis population.
Other findings
Other many important findings are also demonstrated. Shoji et al.34 showed that elevated non-high-density lipoprotein related to incidence of myocardial infarction or cerebral infarction, although not related to mortality due to these diseases. This fact reinforces the importance of controlling dyslipidemia, even though randomized trials did not show much benefits on the dialysis population.35, 36 Fukuma et al.37 demonstrated erythropoiesis-stimulating agent responsiveness can affect mortality by examining the relation between erythropoiesis-stimulating agent dose and mortality stratified by hemoglobin level. They found that higher a erythropoiesis-stimulating agent dose related to worse outcome, especially in lower hemoglobin strata. Water purification is also the field to draw much attention. It is unique that most of the facility in Japan adopts central dialysate delivery system, in which dialysate made by a central machine is delivered to each bedside dialysis machine. Masakane et al.38, 39 demonstrated that more than 90% of facilities meet the standard of the JSDT guideline and maintain high levels of dialysate purity, which might be related to good survival among dialysis population in Japan.
As described here, wide variety of findings are reported from JRDR. Some other findings are also supposed to be published in the near future. These evidences do not only contribute to the development of clinical guidelines of JSDT, but also to the daily clinical practice that is taken for dialysis patients.
LIMITATIONS OF JRDR
Thus described JRDR also has several limitations.
The first is its observational nature. Heterogeneity of the background cannot be removed. The cause and effect relationship is also difficult to be drawn. However, several statistical techniques, such as propensity score matching, or long-term follow-up time, can circumvent these disadvantages, because JRDR collects many kinds of clinical data. These quasi-randomization methods had been utilized to produce the models in reported publications. Moreover, it is important that the results themselves were drawn from the actual entire dialysis population, while clinical trials define and set the criteria of the patients to be included.
The second is the existence of missing values. There certainly exist missing values within the database. However, the statistical powers retained even after either excluding or imputing the missing values, because the numbers of patients investigate are enormous. Moreover, staffs at the headquarters of JSDT asks facilities for the actual data instead of missing values for critical items such as demographics or outcomes.
The third is the aims of this database; the database had been intended to capture the cross-sectional summary of the dialysis population at first. Therefore, the matching system of the patients is indispensable. During the procedures some patients become lost for follow-up or duplicated. However, the numbers of such patients are minimal and actually about 95% of patients were matched longitudinally (data not shown).
The fourth is the fact that more detailed data cannot be obtained. Because the survey is conducted on the basis of totally voluntary work of each facility, not so many items can be collected in the questionnaires. The definition of clinical conditions is also not necessarily standardized. However, detailed manuals are sent every year that indicate how to fill the questionnaires with data. Questions about the survey themselves are also welcomed by JSDT headquarters. Therefore, we believe in the preciseness and comprehensiveness of the database as much as we can attain.
The last is the items are not necessarily surveyed in consecutive years. Because the total numbers of items to be collected are limited, all of clinical parameters are not surveyed every year. However, critical data such as demographics or outcome-relating ones are investigated every year by both paper and the electrical version to capture all outcomes and to adjust important confounders.
STRENGTHS OF JRDR
Although actually are several limitations in JRDR, the wide coverage of the dialysis population is a very important advantage of JRDR in terms of population, items to be collected, and chronological continuity.
The first is the coverage of population. As described above, JRDR is a nation-wide registry and covers almost all of the dialysis population treated in Japan, irrespective of treatment modalities of dialysis, health insurance states, or types of facilities where the patients receive their dialysis treatments.
The second is items to be investigated. Clinical data such as physiques, laboratory data, and clinical history that potentially relates to the outcomes of the patients are also collected besides demographics or outcomes themselves. These data reinforce the robustness of the relationship between some clinical exposures to be investigated and outcomes.
The third is chronological continuity. The facility survey started in 1966 and has the history of almost 50 years. The patient survey was begun in 1983, which is 30 years ago. More than 700 thousands of patients were at least once treated in Japan by dialysis to date, therefore such large numbers of population was enrolled in JRDR. Although not all of the data are readily available, long-term survival can be analyzed potentially.
CONCLUSIONS
JRDR is the nation-wide registry system with the longest history and the most comprehensive coverage. These surveys have been maintained on the basis of totally voluntary work. The data and evidences obtained from JRDR have been utilized for many guidelines such as anemia,11 chronic kidney disease MBD,15 and cardiovascular disease14 guidelines. Therefore, the patients and staffs in charge of the patients can benefit from the results of JRDR.
Moreover, JRDR tells us that the demographics of the Japanese dialysis population are markedly changing in terms of age, primary diagnoses, and dialysis vintage. The disease burden of cardiovascular diseases as well as infection is substantial among the dialysis population. We must take these facts into account in the daily management of dialysis patients.
In this respect, JRDR has provided indispensable and fundamental data of the Japanese dialysis population and will continue to offer the most appropriate way to go in dialysis patients' management.
Acknowledgments
Data shown in this review were adopted from the annual reports of JRDR with permission of the publisher and the Committee of Renal Data Registry of the JSDT. The opinions reflected in this manuscript are those of the authors alone and do not reflect an official position of the JSDT. This supplement was supported by a grant from the 59th Annual Meeting of the JSDT. We are also grateful to all of the staffs and doctors in charge of dialysis patients and responded questionnaires for all the time and attention they have devoted to JRDR.
Appendix
Appendix Table 1: Items Collected Through Facility or Patient Survey
Facility survey
Basic data of each facility: name, address, time of starting offering dialysis service, total number of patients who can simultaneously receive dialysis, maximum capacity, and bedside consoles.
Staffs: number of workers engaged in dialysis treatment by their speciality (e.g., doctors, nurses, clinical engineers, dietitians, and social workers).
Patients: numbers prevalent patients by dialysis modalities (daytime dialysis, nighttime dialysis, home-based hemodialysis (HD), peritoneal dialysis (PD)) including more detailed conditions for patients that ever experienced PD such as peritoneal catheter status, and combined therapies of PD and HD; numbers of hospitalized patients, incident patients, and deceased patients.
Water purification system: number of bedside consoles equipped with an endotoxin retentive filter, use or non-use of endotoxin retentive filters for dialysate sampling as well as the site of sampling; frequency of measurement of dialysate endotoxin level and its results; frequency of measurement of bacterial count in dialysate and its results together with medium used for cultivation in detecting bacteria in dialysate.
Patient survey
Data collected through both the electrical and paper version
Basic data for each patient: anonymized name, gender, date of birth, year and month of start of dialysis, primary diagnoses of ESRD, prefecture of living, and treatment modality.
Data for moving if the patient moved during the year: year and month of transfer to another facility, month of transfer (code of facility to and from which the patient is transferred).
Outcome data: month and cause of death for deceased patient, month and the evidence for transplanted or withdrawn patients, and year and month of change and its modality for the patient who changed the modality during the year.
History of certain critical conditions: diabetes, myocardial infarction, cerebral hemorrhage, cerebral infarction, limb amputation, femoral neck fracture, encapsulating peritoneal sclerosis, PD and kidney transplantation; anti-hypertensive drug use and smoking status.
Modality of therapy: modality of dialysis therapy, and status of combination of PD and other blood purification therapies.
Therapeutic conditions of HD or hemodiafiltration (HDF): treatment times per week and per session, and blood flow rate; mode of infusion and volume of supplementary fluid, and reasons for receiving HDF only for a HDF patient.
Physiques of patient: body height, and body weight both before and after each session.
Laboratory data: blood urea nitrogen and creatinine both before and after dialysis, predialytic albumin, C-reactive protein, calcium, phosphate, parathyroid hormone (including method for measurement), and hemoglobin level.
Data only collected by the electrical version
Other laboratory data: glycated hemoglobin, glycated albumin, total cholesterol, and high-density cholesterol.
Blood pressure: predialytic systolic and diastolic blood pressure, and pulse rate.
Therapy for diabetes: use of insulin, dipeptidyl peptidase-4 inhibitors, and other oral hypoglycemic agents.
PD relating data—only for PD patients
Months on PD in total and during the year 2013, peritoneal equilibration test and its result in terms of creatinine dialysate/plasma ratio, type and volume of PD solution used, residual renal function by urinary volume per day and by Kt/V, averaged amount of water removal per day, Kt/V by PD, automated PD machine use, hours on PD per day, methods of exchange, and frequency of peritonitis and exit site infection per year.
NH received research consulting fee from Kyowa Hakko Kirin Co. Ltd; lecture fee from Bayer Yakuhin Ltd, Chugai Pharmaceutical Co. Ltd, Kyowa Hakko Kirin Co. Ltd, and Nikkiso Co. Ltd; grant support from Chugai Pharmaceutical Co. Ltd and Kyowa Hakko Kirin Co. Ltd. NH is also a member of a division that is funded by Terumo Corporation. KI received consulting fee from Kyowa Hakko Kirin Co. Ltd; lecture fees from Bayer Yakuhin Ltd, Chugai Pharmaceutical Co. Ltd, Kyowa Hakko Kirin Co. Ltd, Merck Sharp & Dohme Corp., Teijin Pharma Limited, Astellas, Daiichi-Sankyo, Mochida, and Torii Pharmaceutical Co. Ltd. YT received consulting fees from Chugai Pharmaceutical Co. Ltd, GlaxoSmithKline K.K., Kyowa Hakko Kirin Co. Ltd, and Taisho Pharmaceutical Co. Ltd; lecture fees from Bayer Yakuhin Ltd, Chugai Pharmaceutical Co. Ltd, Kissei Pharmaceutical Co. Ltd, Kyowa Hakko Kirin Co. Ltd, Otsuka Pharmaceutical Co. Ltd, and Torii Pharmaceutical Co. Ltd; grant support from Asahi Kasei Corporation, Baxter Limited, Bayer Yakuhin Ltd, Chugai Pharmaceutical Co. Ltd, Eisai Co. Ltd, and Otsuka Pharmaceutical Co. Ltd. SN declared no competing interests.
References
- Nakai S. History of annual survey of the Japanese Society for Dialysis Therapy (in Japanese) J Jpn Soc Dial Ther. 2010;43:119–152. [Google Scholar]
- Nakai S, Watanabe Y, Masakane I, et al. Overview of regular dialysis treatment in Japan (as of 31 December 2011) Ther Apher Dial. 2013;17:567–611. doi: 10.1111/1744-9987.12147. [DOI] [PubMed] [Google Scholar]
- Odaka M. An overview of dialysis treatment in Japan (in Japanese) J Jpn Soc Dial Ther. 1982;14:295–303. [Google Scholar]
- The Illustrated, an Overview of Regular Dialysis Treatment in Japan (as of Dec. 31, 2012) (in Japanese) Japanese Society for Dialysis Therapy: Tokyo, Japan; 2013. [Google Scholar]
- Collins AJ, Foley RN, Chavers B, et al. US Renal Data System 2013 Annual Data Report. Am J Kidney Dis. 2014;63:e1–478. doi: 10.1053/j.ajkd.2013.11.001. [DOI] [PubMed] [Google Scholar]
- Clayton P, McDonald S, Hurst K.(eds). The 36th Annual ANZDATA Report (2013). Australia & New Zealand Dialysis & Transplant Registry: Adelaide, South Australia, 2013.
- Gejyo F, Saito A, Akizawa T, et al. 2004 Japanese Society for Dialysis Therapy guidelines for renal anemia in chronic hemodialysis patients. Ther Apher Dial. 2004;8:443–459. doi: 10.1111/j.1774-9987.2004.00199.x. [DOI] [PubMed] [Google Scholar]
- Ohira S, Naito H, Amano I, et al. 2005 Japanese Society for Dialysis Therapy guidelines for vascular access construction and repair for chronic hemodialysis. Ther Apher Dial. 2006;10:449–462. doi: 10.1111/j.1744-9987.2006.00410.x. [DOI] [PubMed] [Google Scholar]
- Guideline Working Group JSfDT Clinical practice guideline for the management of secondary hyperparathyroidism in chronic dialysis patients. Ther Apher Dial. 2008;12:514–525. doi: 10.1111/j.1744-9987.2008.00648.x. [DOI] [PubMed] [Google Scholar]
- Kawanishi H, Akiba T, Masakane I, et al. Standard on microbiological management of fluids for hemodialysis and related therapies by the Japanese Society for Dialysis Therapy 2008. Ther Apher Dial. 2009;13:161–166. doi: 10.1111/j.1744-9987.2009.00674.x. [DOI] [PubMed] [Google Scholar]
- Tsubakihara Y, Nishi S, Akiba T, et al. 2008 Japanese Society for Dialysis Therapy: guidelines for renal anemia in chronic kidney disease. Ther Apher Dial. 2010;14:240–275. doi: 10.1111/j.1744-9987.2010.00836.x. [DOI] [PubMed] [Google Scholar]
- Working Group Committee for Preparation of Guidelines for Peritoneal Dialysis JSfDT. Japanese Society for Dialysis Therapy 2009 Japanese Society for Dialysis Therapy guidelines for peritoneal dialysis. Ther Apher Dial. 2010;14:489–504. doi: 10.1111/j.1744-9987.2010.00901.x. [DOI] [PubMed] [Google Scholar]
- Akiba T, Hora K, Imawari M, et al. 2011 Japanese Society for Dialysis Therapy guidelines for the treatment of hepatitis C virus infection in dialysis patients. Ther Apher Dial. 2012;16:289–310. doi: 10.1111/j.1744-9987.2012.01078.x. [DOI] [PubMed] [Google Scholar]
- Hirakata H, Nitta K, Inaba M, et al. Japanese Society for Dialysis Therapy guidelines for management of cardiovascular diseases in patients on chronic hemodialysis. Ther Apher Dial. 2012;16:387–435. doi: 10.1111/j.1744-9987.2012.01088.x. [DOI] [PubMed] [Google Scholar]
- Fukagawa M, Yokoyama K, Koiwa F, et al. Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Ther Apher Dial. 2013;17:247–288. doi: 10.1111/1744-9987.12058. [DOI] [PubMed] [Google Scholar]
- Masakane I, Kawanishi H, Mineshima M, et al. 2011 JSDT standard on the management of endotoxin retentive filter for dialysis and related therapies. Ther Apher Dial. 2013;17:229–240. doi: 10.1111/1744-9987.12031. [DOI] [PubMed] [Google Scholar]
- Shinzato T, Nakai S, Akiba T, et al. Survival in long-term haemodialysis patients: results from the annual survey of the Japanese Society for Dialysis Therapy. Nephrol Dial Transplant. 1997;12:884–888. doi: 10.1093/ndt/12.5.884. [DOI] [PubMed] [Google Scholar]
- Iseki K, Nakai S, Shinzato T, et al. Prevalence and determinants of hypertension in chronic hemodialysis patients in Japan. Ther Apher Dial. 2007;11:183–188. doi: 10.1111/j.1744-9987.2007.00479.x. [DOI] [PubMed] [Google Scholar]
- Iseki K, Shoji T, Nakai S, et al. Higher survival rates of chronic hemodialysis patients on anti-hypertensive drugs. Nephron Clin Pract. 2009;113:c183–c190. doi: 10.1159/000232600. [DOI] [PubMed] [Google Scholar]
- Iseki K, Nakai S, Yamagata K, et al. Tachycardia as a predictor of poor survival in chronic haemodialysis patients. Nephrol Dial Transplant. 2011;26:963–969. doi: 10.1093/ndt/gfq507. [DOI] [PubMed] [Google Scholar]
- Nakai S, Akiba T, Kazama J, et al. Effects of serum calcium, phosphorous, and intact parathyroid hormone levels on survival in chronic hemodialysis patients in Japan. Ther Apher Dial. 2008;12:49–54. doi: 10.1111/j.1744-9987.2007.00540.x. [DOI] [PubMed] [Google Scholar]
- Taniguchi M, Fukagawa M, Fujii N, et al. Serum phosphate and calcium should be primarily and consistently controlled in prevalent hemodialysis patients. Ther Apher Dial. 2013;17:221–228. doi: 10.1111/1744-9987.12030. [DOI] [PubMed] [Google Scholar]
- Sakaguchi Y, Fujii N, Shoji T, et al. Hypomagnesemia is a significant predictor of cardiovascular and non-cardiovascular mortality in patients undergoing hemodialysis. Kidney Int. 2014;85:174–181. doi: 10.1038/ki.2013.327. [DOI] [PubMed] [Google Scholar]
- Wakasugi M, Kazama JJ, Taniguchi M, et al. Increased risk of hip fracture among Japanese hemodialysis patients. J Bone Miner Metab. 2013;31:315–321. doi: 10.1007/s00774-012-0411-z. [DOI] [PubMed] [Google Scholar]
- Wakasugi M, Kazama JJ, Wada A, et al. Regional variation in hip fracture incidence among Japanese hemodialysis patients. Ther Apher Dial. 2014;18:162–166. doi: 10.1111/1744-9987.12074. [DOI] [PubMed] [Google Scholar]
- Maruyama Y, Taniguchi M, Kazama JJ, et al. A higher serum alkaline phosphatase is associated with the incidence of hip fracture and mortality among patients receiving hemodialysis in Japan. Nephrol Dial Transplant. 2014;29:1532–1538. doi: 10.1093/ndt/gfu055. [DOI] [PubMed] [Google Scholar]
- Hoshino J, Yamagata K, Nishi S, et al. Carpal tunnel surgery as proxy for dialysis-related amyloidosis: results from the Japanese society for dialysis therapy. Am J Nephrol. 2014;39:449–458. doi: 10.1159/000362567. [DOI] [PubMed] [Google Scholar]
- Akizawa T, Minakuchi J, Tomo T, et al. JSDT "Guidelines for maintenance hemodialysis: hemodialysis initiation" [in Japanese] J Jpn Soc Dial Ther. 2013;46:1107–1155. [Google Scholar]
- Kimura K, Okada H, Imai Y, et al. Evidence-based Clinical Pracice Guideline for CKD [in Japanese] Jpn J Nephrol. 2013;55:585–860. [Google Scholar]
- Yamagata K, Nakai S, Masakane I, et al. Ideal timing and predialysis nephrology care duration for dialysis initiation: from analysis of Japanese dialysis initiation survey. Ther Apher Dial. 2012;16:54–62. doi: 10.1111/j.1744-9987.2011.01005.x. [DOI] [PubMed] [Google Scholar]
- Ogata S, Nishi S, Wakai K, et al. Factors associated with the incidence of dialysis. Clin Exp Nephrol. 2013;17:890–898. doi: 10.1007/s10157-013-0786-8. [DOI] [PubMed] [Google Scholar]
- Wakai K, Nakai S, Kikuchi K, et al. Trends in incidence of end-stage renal disease in Japan, 1983-2000: age-adjusted and age-specific rates by gender and cause. Nephrol Dial Transplant. 2004;19:2044–2052. doi: 10.1093/ndt/gfh317. [DOI] [PubMed] [Google Scholar]
- Iseki K, Nakai S, Shinzato T, et al. Increasing gender difference in the incidence of chronic dialysis therapy in Japan. Ther Apher Dial. 2005;9:407–411. doi: 10.1111/j.1744-9987.2005.00318.x. [DOI] [PubMed] [Google Scholar]
- Shoji T, Masakane I, Watanabe Y, et al. Elevated non-high-density lipoprotein cholesterol (non-HDL-C) predicts atherosclerotic cardiovascular events in hemodialysis patients. Clin J Am Soc Nephrol. 2011;6:1112–1120. doi: 10.2215/CJN.09961110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellstrom BC, Jardine AG, Schmieder RE, et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med. 2009;360:1395–1407. doi: 10.1056/NEJMoa0810177. [DOI] [PubMed] [Google Scholar]
- Wanner C, Krane V, Marz W, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;353:238–248. doi: 10.1056/NEJMoa043545. [DOI] [PubMed] [Google Scholar]
- Fukuma S, Yamaguchi T, Hashimoto S, et al. Erythropoiesis-stimulating agent responsiveness and mortality in hemodialysis patients: results from a cohort study from the dialysis registry in Japan. Am J Kidney Dis. 2012;59:108–116. doi: 10.1053/j.ajkd.2011.07.014. [DOI] [PubMed] [Google Scholar]
- Masakane I, Takemoto Y, Nakai S, et al. Bacteriological water quality in the central dialysis fluid delivery system from the survey of the Japanese Society for Dialysis Therapy. Blood Purif. 2009;27 (Suppl 1):11–16. doi: 10.1159/000213491. [DOI] [PubMed] [Google Scholar]
- Masakane I, Tsubakihara Y, Akiba T, et al. Bacteriological qualities of dialysis fluid in Japan as of 31 December 2006. Ther Apher Dial. 2008;12:457–463. doi: 10.1111/j.1744-9987.2008.00635.x. [DOI] [PubMed] [Google Scholar]