Abstract
Adolescents and young adults use text messaging as their primary mode of communication, thus providing an opportunity to use this mode of communication for mobile health (mHealth) interventions. Youth with diabetes are an important group for these mHealth initiatives, as diabetes management requires an enormous amount of daily effort and this population has difficulty achieving optimal diabetes management. Goal setting and self-efficacy are 2 factors in the management of diabetes. We examined the feasibility of a healthy lifestyle text messaging program targeting self-efficacy and goal setting among adolescents and young adults with diabetes. Participants, ages 16-21, were assigned to either a text messaging group, which received daily motivational messages about nutrition and physical activity, or a control group, which received paper-based information about healthy lifestyle. Both groups set goals for nutrition and physical activity and completed a measure of self-efficacy. Participants’ mean age was 18.7 ± 1.6 years old, with diabetes duration of 10.0 ± 4.6 years, and A1c of 8.7 ± 1.7%. The text messaging intervention was rated highly and proved to be acceptable to participants. Self-efficacy, glycemic control, and body mass index did not change over the course of the short, 1-month pilot study. Positive, daily, motivational text messages may be effective in increasing motivation for small goal changes in the areas of nutrition and physical activity. These interventions may be used in the future in youth with diabetes to improve diabetes care. Utilizing more targeted text messages is an area for future research.
Keywords: adolescents, diabetes, goal setting, mHealth, text messaging, young adults
Text messaging is the primary mode of communication among adolescents and young adults. According to recent survey data, the majority of teenagers (78%) have a cell phone, with almost half of those (47%) owning a smartphone.1 Adolescents “out-text” any other age group, with an average of 3364 texts per month, followed by young adults in the amount of texts sent per month.2 There is an enormous opportunity in health education, prevention, and intervention research to capitalize on this activity and to assess the feasibility and benefits of mobile health (mHealth) programs among adolescents.3,4
Adolescents and young adults with diabetes represent an important group for mHealth initiatives. Diabetes self-care behaviors are aimed at normalizing blood glucose levels in efforts to prevent the development of both acute and chronic complications. However, despite the need to optimize blood glucose levels to preserve health, and with many new treatment technologies that assist in this, many adolescents and young adults fail to achieve the recommended glycemic outcomes.5-7 Furthermore, overweight and obesity are particular challenges for adolescents and young adults in general and for those with diabetes, both type 1 and type 2.8,9
Diabetes management is particularly difficult during adolescence and emerging adulthood due to many reasons, including the effect of puberty during adolescence on glycemic control,10 and many behavioral and psychological factors that contribute to deterioration of blood glucose levels.11,12 Challenges facing adolescents include difficulties adhering to the numerous aspects of diabetes self-care including frequent glucose monitoring, insulin administration, diet, and exercise,13-15 peer-related concerns (eg, worry about what friends think about diabetes, avoidance of diabetes self-care tasks in the presence of peers and coworkers),16-18 and depression.19-21
To maximize diabetes self-care, it is important for adolescents and young adults to perceive self-efficacy around self-care tasks. Self-efficacy refers to a person’s belief in their ability for a specific behavior.22 A recent study examining the relationship between self-efficacy and self-care in older adolescents with type 1 diabetes found that greater self-efficacy was significantly related to greater diabetes self-management.23 Understanding the importance of goals and goal setting may increase the likelihood of succeeding with diabetes self-management.24
Due to the pervasive challenges that face adolescents and young adults, frequent support for healthy lifestyle management is needed to supplement quarterly diabetes visits. mHealth interventions may offer such an opportunity. These modalities can address lifestyle issues related to healthy eating and exercise, as well as reminders to perform diabetes-related medical tasks.
To explore the mHealth modalities, the current study examined the feasibility of a healthy lifestyle text messaging program targeting goal-setting and self-efficacy among adolescents and young adults with diabetes. The aims of the study were (1) to conduct a 1-month pilot and feasibility randomized clinical trial comparing a text messaging intervention with a control condition; (2) to evaluate usability, acceptability, and satisfaction of the text messaging intervention; (3) to evaluate self-efficacy before and after the 1-month study related to achieving health goals; and (4) to describe glycemic control (A1c) and body mass index (BMI) before and 3 months after enrollment. We hypothesized that the mHealth intervention would have near universal uptake and acceptance among adolescents and young adults with diabetes. However, we did not expect significant changes in health outcomes due to the short duration of this pilot study.
Methods
Potential participants were approached by a research assistant at the time of a routine clinic visit at a tertiary diabetes outpatient center; if under 18, the child and parent were approached together. Inclusion criteria were (1) clinician diagnosis of type 1 or type 2 diabetes, according to American Diabetes Association criteria; (2) ages 16-21; (3) possession of a cell phone with text messaging capability; and (4) fluency in English. Eligibility was assessed by review of potential participants’ medical charts and confirmed with the patient/family prior to enrollment. Participants and a parent (if youth < 18) completed consent/assent procedures. The study was approved by the Institutional Review Board at the Joslin Diabetes Center.
Participants were randomized to receive 1 month of daily text messages (text group) with healthy lifestyle tips, or to receive a pamphlet (control group) about healthy eating and physical activity created and disseminated by the NIH/NIDDK (http://win.niddk.nih.gov/publications/take_charge.htm). At enrollment and after informed consent/assent, participants met with a research assistant to complete questionnaires. In addition, both the text and control groups set personal goals specifically related to nutrition and physical activity. Participants received a list of 8 nutrition goals and 8 physical activity goals and chose 1-3 for each area (see Results). Participants in the text messaging group selected goals electronically on a health promotion website related to the text messaging platform (www.bodimojo.com); participants in the control group selected goals on paper and had no further follow-up regarding goal attainment.
The text messaging intervention included 3 components and were sent automatically to participants: (1) daily motivational messages, (2) goal check-ins (2 times per week), and (3) logistical check-ins (bimonthly). The daily motivational text messages focused on healthy eating and physical activity (Figure 1) and some included links to health quizzes and articles on bodimojo.com which participants could access from their smart phones or from a computer, if they chose to do so. In addition to reading information on the website, users were able to set and track their health goals. “Goal check-ins” asked participants by text to respond with a text message regarding whether they were meeting their goals. “Logistical check-in” messages asked participants by text to identify any difficulties with the text messaging (Figure 2). Participants responded to the text messages via their cell phones and were able to access the additional content on bodimojo.com via their smart phones or using a computer.
Figure 1.
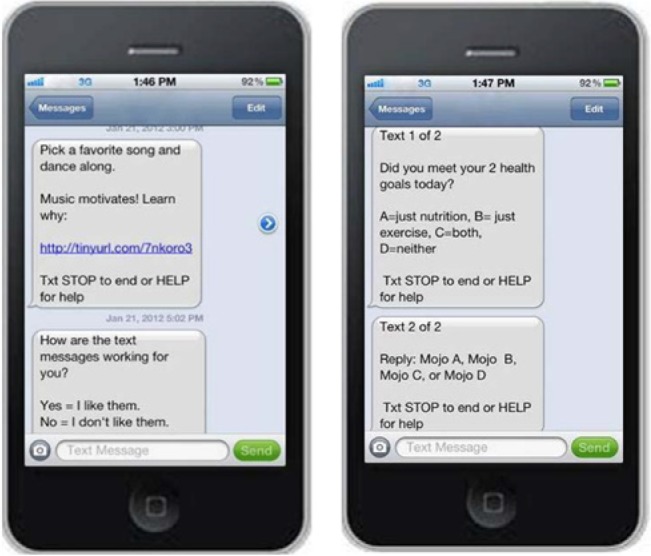
Text message examples.
Figure 2.
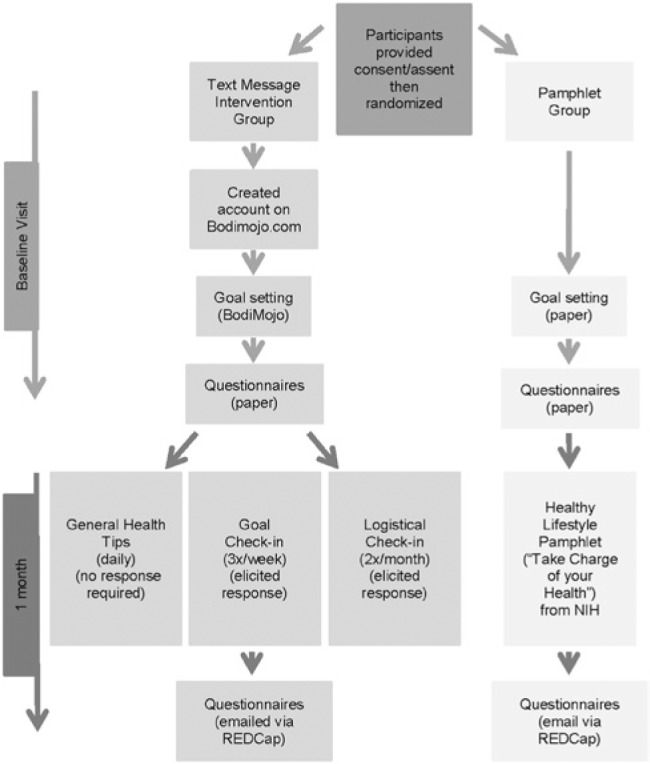
Study procedures.
After 1 month, all participants received an email with a link to complete online questionnaires using REDCap survey.25 Once completed, all participants (regardless of study group) received a $25 gift card; control participants were invited by letter to receive the text messaging intervention for 1 month.
Measures
Demographic Information
At baseline, participants completed a demographic questionnaire to gather data on educational level, race/ethnicity, physical activity level, team sport participation, type of cell phone, and computer use. Medical chart review was conducted to collect height and weight, A1c, sex, type of diabetes, and diabetes duration.
Physical Activity and Healthy Food Efficacy Scale for Children (PAHFE-C)
At baseline and 1-month follow-up participants completed the PAHFE-C,26 a 20-item instrument designed to assess efficacy related to personal goal setting and decision making for healthy food choices and physical activity. Response options included a 5-point Likert-type scale ranging from not sure to completely sure. The 4 subscales (healthy eating goal setting, healthy eating decision making, physical activity goal setting, physical activity decision making) have moderate to high internal consistency in previously reported research (0.59 ≤ α ≤ 0.87). A sample question is, “How sure are you that you can set goals for yourself to eat healthy foods (like fruit & vegetables)?”
Satisfaction Survey
Participants in the text group completed the 21-item satisfaction survey at the 1-month follow-up, with response ratings on a 1-9 Likert scale. A sample question is, “Do you think the text messages helped you feel motivated about having healthy/healthier habits?”
Statistical Analyses
Data were analyzed using SAS (version 9.2 for Windows; SAS Institute Inc, Cary, NC). Analyses included univariate analyses for obtaining descriptive statistics, as well as t tests and chi-square analyses. A P value of <.05 was considered significant.
Results
Recruitment and participation
Recruitment was accomplished within 2 months; 90 of 136 patients (66%) approached agreed to participate in the study. There was no difference between those who chose to participate and those who declined based on age, diabetes duration, or sex. None of the patients with type 2 diabetes who were approached declined (n = 8), while 34% of those with type 1 diabetes declined (P = .04). One potential participant was deemed ineligible because he or she did not have a cell phone. We do not have data regarding whether participants had unlimited text messaging or not. None of the participants expressed concerns about the cost of participating in the intervention. At the end of the study, 11 of the 45 participants in the control group considered participation in the text intervention; only 6 opted to receive the intervention.
Participant Characteristics
Participants’ mean age was 18.7 ± 1.6 years old, with diabetes duration of 10.0 ± 4.6 years and A1c of 8.7 ± 1.7% (see Table 1). Almost half of the participants were male (47%), and 91% had type 1 diabetes. The majority of participants were college students (66%), were white (86%), and reported participating on a sports team or in regular physical activity (79%).
Table 1.
Participant Characteristics.
| Characteristic | mHealth (n = 45) | Pamphlet (n = 45) | P value |
|---|---|---|---|
| Mean age (years) | 18.8 ± 1.6 | 18.6 ± 1.6 | .65 |
| Sex (% male) | 47 | 47 | 1 |
| Race (% white) | 84 | 87 | .76 |
| College students (%) | 70 | 63 | .49 |
| Participates in sports/regular physical activity (%) | 73 | 84 | .2 |
| Diabetes duration (years) | 9.7 ± 4.4 | 10.2 ± 4.9 | .66 |
| Type of diabetes (% T1D) | 89 | 93 | .46 |
| % pump treated (at baseline) | 53 | 42 | .29 |
| Baseline A1c (%) | 8.7 ± 1.8 | 8.7 ± 1.6 | .94 |
| BMI (kg/m2) | 26.8 ± 5.5 | 26.4 ± 5.2 | .74 |
| Smartphone/phone with internet (%) | 67 | 73 | .49 |
N = 90 patients. Values are mean ± SD or percentage, as indicated.
Nutrition and Physical Activity Goals
Table 2 indicates the frequency with which each goal was chosen. For nutrition goals, the majority (52%) chose 1 goal, 24% chose 2 goals, and 23% chose 3 goals. For physical activity goals, 47% chose 1 goal, 24% chose 2 goals, and 28% chose 3 goals. The most frequently chosen nutrition goal was “eat breakfast every day.” The most frequently chosen physical activity goal was “go to the gym or be physically active at least 3 times a week.” Male and female participants chose similar nutrition and physical activity goals, with 2 exceptions. Males were more likely than females (55% vs 29%, respectively; P = .01) to choose the goal “Go to the gym or be physically active at least 3x/week” and females were more likely than males (33% vs 14%, respectively; P = .04) to choose the goal “Eat one piece/serving of fruit with every meal.”
Table 2.
Nutrition and Physical Activity Goals by Percentage of Participants Who Chose the Goal.
| Nutrition goal | % | Physical activity goals | % |
|---|---|---|---|
| Eat breakfast every day | 17 | Go to the gym or be physically active at least 3 times a week | 24 |
| Choose whole wheat bread instead of white bread | 15 | Exercise for 60 minutes a day | 16 |
| Drink 2-3 glasses (8 oz) of milk each day | 14 | Do morning or evening stretches | 12 |
| Eat one piece/serving of fruit with every meal | 14 | Work out with an exercise buddy twice a week | 12 |
| Eat a salad every day | 13 | Do 20 sit-ups first thing in the morning to get yourself energized | 11 |
| Make one of your veggie choices green each day | 11 | Exercise for 30 minutes a day | 10 |
| Avoid drinks with carbs or calories (except milk) | 9 | Walk every day for at least 30 minutes | 9 |
| Bring a homemade lunch to school | 7 | Ride a bike (or stationary bike) 2-3 times a week | 5 |
Participants were instructed to choose between 1 and 3 nutrition goals and between 1 and 3 physical activity goals. All participants (N = 90) chose goals.
Text Messaging
During the 1-month study period, participants received a motivation message daily and also 14 text messages eliciting responses were sent to participants (12 goal check-ins; 2 logistical check-ins). Of the 45 participants receiving text messages, 40 responded at least once (see Figure 3 for the distribution of responses). The mean lapse between receiving a text message and writing back was 2.1 ± 1.6 days. Of the 40 participants who responded to the texts at least once, the average number of responses was 10.3 ± 3.5, with a median response rate of 11. When participants were asked “Did you meet your nutrition goal today?,” 70% replied yes. When asked “Did you meet your physical activity goal today,” 66% replied yes. When answering the question “Did you meet your 2 health goals today?,” 49% answered yes, 12% answered no, and 39% answered yes to 1 of the goals.
Figure 3.
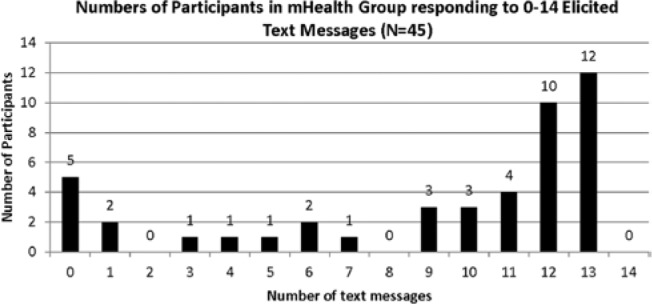
Distribution of text responses.
Of the 45 text participants, 23 (51%) responded to at least 1 of the logistical check-in messages. When asked to provide feedback via text to the questions “How are the text messages working for you?” or “Hey! We’re checking in. Text us your feedback or any problems u have encountered,” the overwhelming majority of comments (85%) were positive. Of these 23 participants, only 3 responded with negative comments.
Satisfaction with Text Messaging Intervention
Participants were positive about the intervention, with 93% reporting that they worked toward their health goal during the study duration and 71% stating that BodiMojo helped them follow their health goals. The majority of the adolescents and young adults (67%) stated the text messages helped them feel motivated about having healthy/healthier habits and would recommend the text messaging to friends.
The majority of feedback about participation in the text messaging intervention was positive. Participants offered positive feedback, such as: “The facts are helpful and are a reminder of ways to stay healthy.” “This has been an easy and nice way of reminding me to stay on track with my health goals!” One participant commented on the positive nature of the messages: “I had a problem with this service when I broke my phone and couldn’t get a new one for a week that resulted in my having about 10 texts from you guys. I missed having the cheerful texts!” An example of a negative comment was: “[The texts] just make me feel guilty because I know I need to focus on nutrition and it’s just harder this time of year.”
For those participants in the text messaging group, 51% reported accessing BodiMojo on the computer and 39% of those with smartphones reported accessing BodiMojo on their phone.
Self-efficacy
Internal consistency of all 4 subscales were good to excellent in our sample (Cronbach’s α = .80-.90). At baseline, there was no difference in self-efficacy between participants in the control and intervention groups on any subscale (P > .53 for all subscales). In addition, there was no difference in change score from baseline to follow-up between the 2 groups (P > .21 for all subscales).
Glycemic control and body mass index
At baseline, the 2 groups did not differ in A1c (control group: 8.7 ± 1.6; text group: 8.7 ± 1.8, P = .94) or BMI (control group: 26.4 ± 5.2; text group: 26.8 ± 5.5, P = .74). Both groups showed a small, nonsignificant improvement in A1c from baseline to their next follow-up diabetes visit, approximately 3 months later. Average change score was –.06 in the control group and –.2 in the intervention group (P = .50). BMI did not change from baseline to follow-up diabetes visits.
Discussion
This brief pilot intervention focused on comparing a text messaging intervention with information provided in a more traditional pamphlet format about healthy lifestyle in older adolescents and emerging adults with diabetes. This intervention appeared to be desirable to this population, as evidenced by the rapid recruitment and high participation rates and positive feedback from participants in the text group. Previous studies also demonstrated high acceptance with text messaging interventions among children/teens and adults.27,28 Many participants in the text arm of the current study appeared to achieve both their physical activity and nutrition goals as reported by their responses to the text queries. On the other hand, there was no demonstrable change in reported self-efficacy for healthy lifestyle behaviors.
There are several possible explanations for the lack of significant differences between the groups on the self-efficacy measure. First, participants’ baseline self-efficacy ratings were high for both physical activity and nutrition domains, suggesting a potential ceiling effect. Second, this measure may not be sensitive enough for this demographic group, as the PAHFE has only been validated in elementary school children.26 Third, although participants indicated that they had achieved their goals and liked the text messaging system, the texts were not specifically designed to increase self-efficacy. Future studies should attend to developing text messaging that targets individuals’ self-efficacy in improving health behaviors.
Youth with diabetes attend to multiple daily tasks for their diabetes management. The current intervention focused not on diabetes management, but on lifestyle issues. Because youth with diabetes may not want reminders about specific diabetes tasks, interventions that focus on general healthy lifestyle issues may be more acceptable to this cohort. In turn, this may result in higher motivation for health behaviors which ultimately may lead to more optimal diabetes self-management. A review of public health campaigns in the related area of lifestyle change and obesity prevention supports this, showing that health messages that are perceived as most positive and motivating make no reference to any health condition.29 This finding likely applies to text messages as well; however, this is a topic that requires further study
Limitations of this study include the lack of data for participants in the control group with respect to their goal achievement. Because this was a small feasibility study, the study duration was likely too short to observe changes in glycemic control or BMI. Generalizability is limited to adolescents and young adults who have access to text messaging. In addition, this sample was primarily white college students who were physically active. It is not representative of youth in general, nor is it representative of youth with type 2 diabetes. Future research should include greater heterogeneity of participants.
Conclusions
Longer term studies evaluating the impact of text messaging and mHealth initiatives are needed in this population to assess the effects on glycemic control and other health outcomes. Asking adolescents and young adults how they would like to use text messaging for health initiatives would be important information to gather to better tailor future interventions. In addition, the focus on healthy lifestyle, as opposed to specific diabetes management tasks, may be an effective use of text messaging in this population, with potential to positively impact future health outcomes.
Footnotes
Abbreviations: A1c, hemoglobin A1c; mHealth, mobile health.
Authors’ Note: Previous poster presentations include a poster at the American Diabetes Association Scientific Sessions in June 2013 and a poster at the Med 2.0 conference in 2012.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded in part by National Institute of Diabetes and Digestive and Kidney Diseases Grant 1K23DK092335, National Institute of Diabetes & Digestive & Kidney Diseases Grant 1R43DK85748-11A1, Charles H. Hood Foundation, Katherine Adler Astrove Youth Education Fund, Maria Griffin Drury Pediatric Fund, Eleanor Chesterman Beatson Fund.
References
- 1. Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Pew Internet, teens and technology. 2013. http://www.pewinternet.org/Reports/2013/Teens-and-Tech.aspx. Accessed March 13, 2013.
- 2. Nielsen. Kids today: how the class of 2011 engages with media. 2011. http://www.nielsen.com/us/en/newswire/2011/kids-today-how-the-class-of-2011-engages-with-media.html
- 3. Sarasohn-Kahn J. How smartphones are changing health care for consumers and providers. April 2010. http://www.chcf.org/publications/2010/04/how-smartphones-are-changing-health-care-for-consumers-and-providers#ixzz27EE0W4kL
- 4. Patrick K, Griswold WG, Raab F, Intille SS. Health and the mobile phone. Am J Prev Med. 2008;35(2):177-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Beck RW, Tamborlane WV, Bergenstal RM, Miller KM, Dubose SN, Hall CA. The T1D dxchange clinic registry. J Clin Endocrinol Metab. 2012;97(12):4383-4389. [DOI] [PubMed] [Google Scholar]
- 6. Wood JR, Miller KM, Maahs DM, et al. Most youth with type 1 diabetes in the T1D exchange clinic registry do not meet American Diabetes Association or International Society for pediatric and adolescent diabetes clinical guidelines. Diabetes Care. 2013;36(7):2035-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Markowitz JT, Harrington KR, Laffel LM. Technology to optimize pediatric diabetes management and outcomes. Curr Diabetes Rep. 2013;13(6):877-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lawrence JM, Liese AD, Liu L, et al. Weight-loss practices and weight-related issues among youth with type 1 or type 2 diabetes. Diabetes Care. 2008;31(12):2251-2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sands AL, Higgins LA, Mehta SN, Nansel TR, Lipsky LM, Laffel LM. Associations of youth and parent weight status with reported versus predicted daily energy intake and hemoglobin A1c in youth with type 1 diabetes mellitus. J Diabetes Sci Technol. 2013;7(1):263-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Amiel SA, Sherwin RS, Simonson DC, Lauritano AA, Tamborlane WV. Impaired insulin action in puberty. A contributing factor to poor glycemic control in adolescents with diabetes. N Engl J Med. 1986;315(4):215-219. [DOI] [PubMed] [Google Scholar]
- 11. Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care. 2001;24(9):1536-1540. [DOI] [PubMed] [Google Scholar]
- 12. Moreland EC, Tovar A, Zuehlke JB, Butler DA, Milaszewski K, Laffel LM. The impact of physiological, therapeutic and psychosocial variables on glycemic control in youth with type 1 diabetes mellitus. J Pediatr Endocrinol Metab. 2004;17(11):1533-1544. [DOI] [PubMed] [Google Scholar]
- 13. Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010;22(4):405-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Borus JS, Blood E, Volkening LK, Laffel L, Shrier LA. Momentary assessment of social context and glucose monitoring adherence in adolescents with type 1 diabetes. J Adolesc Health. 2013;52(5):578-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rasbach LE, Atkins AE, Milaszewski KM, et al. Treatment recommendations following 3-day masked continuous glucose monitoring (CGM) in youth with type 1 diabetes. J Diabetes Sci Technol. 2014;8(3):494-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hains AA, Berlin KS, Davies WH, Parton EA, Alemzadeh R. Attributions of adolescents with type 1 diabetes in social situations: relationship with expected adherence, diabetes stress, and metabolic control. Diabetes Care. 2006;29(4):818-822. [DOI] [PubMed] [Google Scholar]
- 17. Helgeson VS, Siminerio L, Escobar O, Becker D. Predictors of metabolic control among adolescents with diabetes: a 4-year longitudinal study. J Pediatr Psychol. 2009;34(3):254-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Markowitz JT, Laffel LM. Transitions in care: support group for young adults with type 1 diabetes. Diabetes Med. 2012;29(4):522-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hood KK, Huestis S, Maher A, Butler D, Volkening L, Laffel LM. Depressive symptoms in children and adolescents with type 1 diabetes: association with diabetes-specific characteristics. Diabetes Care. 2006;29(6):1389-1391. [DOI] [PubMed] [Google Scholar]
- 20. McGrady ME, Laffel L, Drotar D, Repaske D, Hood KK. Depressive symptoms and glycemic control in adolescents with type 1 diabetes: mediational role of blood glucose monitoring. Diabetes Care. 2009;32(5):804-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bryden KS, Dunger DB, Mayou RA, Peveler RC, Neil HA. Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care. 2003;26(4):1052-1057. [DOI] [PubMed] [Google Scholar]
- 22. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191-215. [DOI] [PubMed] [Google Scholar]
- 23. Hanna KM, Weaver MT, Stump TE, Slaven JE, Fortenberry JD, DiMeglio LA. Readiness for living independently among emerging adults with type 1 diabetes. Diabetes Educ. 2013;39(1):92-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Boot M, Volkening LK, Butler DA, Laffel LM. The impact of blood glucose and HbA(1c) goals on glycaemic control in children and adolescents with Type 1 diabetes. Diabetes Med. 2013;30(3):333-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Perry CM, De Ayala RJ, Lebow R, Hayden E. A validation and reliability study of the Physical Activity and Healthy Food Efficacy Scale for Children (PAHFE). Health Educ Behav. 2008;35(3):346-360. [DOI] [PubMed] [Google Scholar]
- 27. Rodgers A, Corbett T, Bramley D, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control. 2005;14(4):255-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shapiro JR, Bauer S, Hamer RM, Kordy H, Ward D, Bulik CM. Use of text messaging for monitoring sugar-sweetened beverages, physical activity, and screen time in children: a pilot study. J Nutr Educ Behav. 2008;40(6):385-391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Puhl R, Peterson JL, Luedicke J. Fighting obesity or obese persons? Public perceptions of obesity-related health messages. Int J Obes (Lond). 2013;37(6):774-782. [DOI] [PubMed] [Google Scholar]


