Abstract
Matching meal insulin to carbohydrate intake, blood glucose, and activity level is recommended in type 1 diabetes management. Calculating an appropriate insulin bolus size several times per day is, however, challenging and resource demanding. Accordingly, there is a need for bolus calculators to support patients in insulin treatment decisions. Currently, bolus calculators are available integrated in insulin pumps, as stand-alone devices and in the form of software applications that can be downloaded to, for example, smartphones. Functionality and complexity of bolus calculators vary greatly, and the few handfuls of published bolus calculator studies are heterogeneous with regard to study design, intervention, duration, and outcome measures. Furthermore, many factors unrelated to the specific device affect outcomes from bolus calculator use and therefore bolus calculator study comparisons should be conducted cautiously. Despite these reservations, there seems to be increasing evidence that bolus calculators may improve glycemic control and treatment satisfaction in patients who use the devices actively and as intended.
Keywords: review, bolus calculator, bolus calculation, insulin dosing, type 1 diabetes
Background
The American Diabetes Association (ADA) recommends intensive insulin therapy for type 1 diabetes (T1D) with multiple daily injections (MDI) of insulin or continuous subcutaneous insulin infusion (CSII) and matching meal insulin to carbohydrate (CHO) intake, premeal blood glucose (BG) and activity level.1 These standards are based on the results of the landmark Diabetes Control and Complications Trial (DCCT) and the Epidemiology of Diabetes Interventions and Complications study which documented that intensive insulin therapy in T1D delays the onset and slows the progression of diabetic microvascular disease and reduces the risk of cardiovascular disease.2,3 Furthermore, DCCT results showed that patients who almost always adjusted their meal insulin dose to food intake achieved HbA1c values that were 0.5%-point lower than patients who never made adjustments.4
Carbohydrate Counting and Bolus Calculation
One method for matching meal insulin to CHO intake is called ‘carbohydrate counting’ (CC).5 It is a systematic approach for insulin bolus size calculation, and in addition to improving metabolic control, CC has been shown to improve quality of life, treatment satisfaction, and psychological well-being and to increase dietary freedom without concomitant deteriorations in cardiovascular risk factors in patients with T1D.6,7 Insulin dose calculations by CC concern only bolus insulin, but a prerequisite for success is a correct basal insulin dose in the form of either long-acting insulin or a basal rate. Basal insulin dosing can be evaluated by diabetes diary review or basal rate check.8
The correction factor (CF) and the insulin to carbohydrate ratio (ICR), are patient specific empirically estimated parameters included in the insulin bolus calculation.8 CF is the decrease in BG level caused by 1 unit of subcutaneously injected rapid-acting insulin. ICR is the amount of CHO needed to match the BG lowering effect of 1 unit of rapid-acting insulin. Guides to CF and ICR estimations have been published.9,10 The clinician should however note that there is often a need for further parameter adaptation and that CF and ICR values may vary during the day.
With basal insulin dosing, CF and ICR in place, the next step in the insulin bolus calculation procedure is to estimate the meal CHO content. To do this, knowledge about the CHO content of different foods is required. Furthermore, a BG measurement must be obtained and a BG target set. The BG target is patient specific depending on individual patient goals and may also vary according to time of day.
Now the patient is ready to calculate an insulin bolus. The insulin bolus equation consists of a meal insulin part and a correction insulin part:
If no food is to be consumed, the meal insulin part is eliminated and correspondingly the correction insulin part is eliminated if the BG is already in target.
Often, the sum of the meal and correction insulin part should be multiplied by a proportion reflecting the current physiologic state (PS) of the patient. When insulin sensitivity is increased, for example, due to physical activity, the PS is < 1 and when insulin sensitivity is decreased, for example, during illness, the PS is > 1. The PS is subject to large intra- and interindividual variation and since there is no research supporting quantification of the proportion, the patient is left to a trial-and-error approach. Finally, if insulin from previously administered boluses is still active, insulin on board (IOB) should be subtracted. In pump patients, 65% of all insulin boluses are given within 4.5 hours of a prior bolus, that is, within the duration of insulin action (DIA), and thus inclusion of IOB in the bolus calculation is important to avoid insulin stacking.11 IOB is determined based on patient specific DIA and assumptions of insulin kinetics.11,12
The complete bolus insulin equation reads as follows:
Bolus insulin equations are complex and—for most people—difficult and time consuming to solve by mental calculations.13-15 To complicate bolus calculation even further, all equation parameters may vary from hour to hour. The complexity in itself fully justifies the use of a device that facilitates bolus calculation and the need for bolus calculators (BCs) is further substantiated by studies documenting a high frequency of poor numeracy skills among adults with T1D.16,17 Despite the fact that the exact amount of CHO in a meal was given to 201 adult T1D patients, 57% came to a false result by manual insulin dose calculation. However, when provided with an automated BC the proportion of false results was reduced to 7%. Some of the remaining false results were retrospectively identified by BC download which showed that the study subjects had deviated from protocol and logged insulin doses in the meter before study start and that these loggings affected the study results due to the IOB feature.15
All in all, to meet ADA recommendations, insulin BCs are needed in the treatment of most patients with T1D.
Fat and Protein Counting
CC is based on the assumption that CHO is the nutrient component with greatest impact on postprandial BG excursions and that the impact of protein and fat is minor and covered by the basal insulin. There is evidence, however, that dietary fat and protein increase BG levels by impairing insulin sensitivity and enhancing hepatic glucose production.18-20 Algorithms for insulin bolus calculation including all 3 components have been proposed but are not widely adopted in BCs and it remains to be fully clarified how the glycemic impact of fat and protein should be estimated.21 Furthermore, it is questionable whether all patients are able to perform these increasingly advanced meal composition evaluations. The ADA recommends that selected individuals who master CC are trained in including protein and fat estimations in their diabetes management.1
Different Bolus Calculators
Stand-Alone Bolus Calculators
The selection of stand-alone BCs ranges from simple sliding scales including only meal insulin and correction insulin in the bolus calculation to advanced automated calculators with IOB, time dependent patient specific parameters, and memory functions.14,22-27 The devices differentiate by look, ease of use, degree of automation, and not least by algorithms. Consequently, direct comparisons of studies of the various stand-alone BCs should be conducted with care. Currently, 2 stand-alone advanced automated BCs are approved by regulatory authorities in Europe but none in the United States.
HbA1c
One of the very first published reports on the use of a BC to support insulin dosage decision demonstrated that even a simple, plastic guide could improve HbA1c significantly in young T1D patients treated with human short-acting insulin.23 Almost 10 years later, a similar inexpensive bolus calculation card was developed to provide MDI users with the bolus calculation means enjoyed by users of the more expensive CSII therapy, and a retrospective database study showed that MDI-treated patients using the card achieved lower HbA1c levels compared with nonusers.28
A third manual BC in the form of a cardboard wheel named InsuCalc was presented more than a decade ago but is still available at low cost. The wheel comes in 12 different versions each with a fixed CF and ICR combination. The fixed combinations mean that a patient may need several wheels if CF and/or ICR changes during the day. Bolus calculations are based on BG in 72-mg/dl intervals and meal CHO content in 15-gram intervals. The use of intervals can potentially result in highly variable BG results (from 23 to 200 mg/dl!). A 6-month, randomized, controlled pediatric study including the device found significant improvements in HbA1c (from 9.7% to 8.8%) in 10 patients using the device consistently but not in the intention to treat group.14
A simple electronic pocket calculator with fixed CF (at 54 mg/dl/unit) and dose reduction for physical activity was also able to reduce HbA1c significantly in a 6-month, randomized trial. The mean HbA1c change in the calculator group was −0.8% compared with −0.1% in the group using mental calculations.24
A more advanced, PDA-based BC, a forerunner of an insulin pump BC, was studied in a 12-month randomized, controlled study of MDI users. At the end of the study period, HbA1c-levels were lower in the intervention group; however, there was also an increase in the number of severe hypoglycemic events in these patients.22 The authors concluded that the device did not handle hypoglycemia well and this might have been due to the lack of IOB function.
Two studies of an advanced automated BC with integrated BG meter have been published within the last 2 years and more large-scale studies of this particular device are on their way (clinicaltrials.gov registry number NCT02084498; Danish National Committee on Health Research Ethics H-4-2013-035). The first publication was a 16-week randomized, controlled pilot study, the BolusCal Study, of 51 CC-naïve adults with T1D.25 The study demonstrated a change in HbA1c from 8.9% to 8.1% in patients using the BC and this improvement was maintained 1 year after the device was implemented in their therapy.29 However, metabolic control after 16 weeks in the BC group was not different from metabolic control in the study group trained in CC by mental calculations, that is, there was no additional effect of BC use on metabolic control.
The second clinical study investigating the same automated BC, the ABACUS trial, was larger (N = 193), longer (26 weeks), and included both T1D (mostly 92.7%) and type 2 diabetes patients who were experienced in CC.27 Patients were randomized into 2 groups, 1 using the BC and 1 using mental calculations. Significantly more patients in the BC group achieved an HbA1c reduction >0.5% (56.0% vs 34.4%).
Glycemic Variability
Another PDA-based BC than the 1 described above but also a forerunner of an insulin pump BC was studied in a short-term randomized crossover study in CSII-treated patients.30 The study showed that users of the BC needed less supplemental CHO for hypoglycemia treatment and fewer correction boluses due to more accurate insulin dosing.
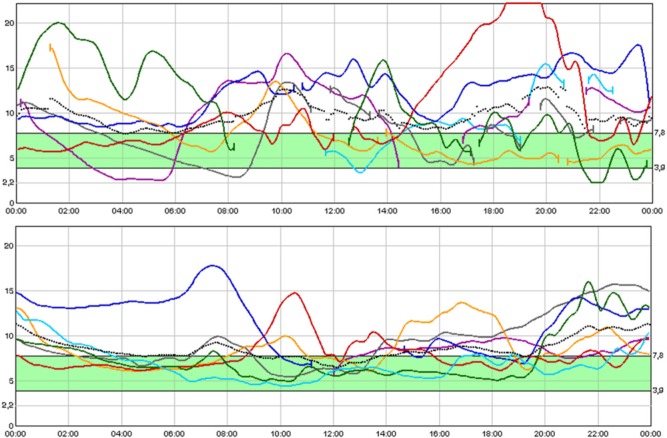
Continuous glucose monitoring was used in the BolusCal study to observe glucose fluctuations.25 Although the numbers did not reach statistical significance, perhaps because of lack of power, BC use was associated with improved distribution of glucose values with less time in hypo- and hyperglycemia. An example of the changes observed after introduction of the BC is depicted in Figure 1.
Figure 1.
Six days of blinded continuous glucose monitoring before (upper panel) and after (lower panel) introduction of carbohydrate counting and an automated bolus calculator.
Treatment Satisfaction
One important function of a BC is to ease the burden of insulin dosing decisions, however, only very few studies have included treatment satisfaction as an outcome parameter. In the InsuCalc wheel study, treatment satisfaction measured by the Diabetes Treatment Satisfaction Questionnaire (DTSQ) improved in the intervention group during the study, but the improvements were not different from the improvements obtained in the control group.14 In the BolusCal Study on the other hand, changes in DTSQ scores were significantly greater in patients using the automated BC compared with patients performing mental calculations and the same was the case in the ABACUS trial.25,27
Applications for Smartphones
The launch of software applications for smartphones to assist the diabetes patient in CC and bolus calculation has long since surpassed the realization of studies testing application safety, reliability and clinical efficacy. Patients can download applications, either free or at very low cost, that provide insulin dosing advice even though they have not been approved by the FDA or corresponding regulatory authority. This leaves the health care provider with the challenge of maneuvering in a field of black boxes that may potentially cause harm to patients.31
Only recently, in 2013, the first smartphone application received approval (CE marking) for insulin dose management.32 The software program includes a BC plus a telemedicine component which allows for communication between patient and health care provider. Prior to approval, the application had gone through clinical testing. A randomized, controlled study of 162 type 1 diabetes patients documented that the bolus calculator decreased HbA1c significantly, but there was no additional effect of the telemedicine component.33
Another telemedicine system for smartphones including an advanced bolus calculator was studied in 130 T1D patients randomized to 26 weeks of CC with either mental calculations or use of the new system. Significant improvements in HbA1c were found within but not between groups; however, DTSQ scores increased more in users of the BC compared with those using mental calculations.34
Bolus Calculators Integrated in Pumps
All insulin pumps targeted T1D patients sold today have built-in advanced automated BCs. There are subtle differences between the BC algorithms with respect to the way they handle IOB and correction of hyperglycemia but health care professionals should be aware of these manufacturer-specific differences to be able to set the pump optimally for each patient.12 Although BCs integrated in pumps have been on the market for some years now, studies of their effectiveness are still few.
A cross-sectional study of 88 adult T1D insulin pump users with a mean HbA1c of 6.8% found that patients who used the insulin pump BC for ≥ 50% of bolus calculations had HbA1c, mean BG and mean BG standard deviation that were significantly lower than patients who used the BC less (0.6%, 25.45 mg/dl, and 9.1 mg/dl, respectively).35
In a prospective study of 30 patients who switched from an insulin pump without to a pump with a BC and used the BC for 80% of bolus calculations, HbA1c levels decreased significantly by 0.2%-points after the switch.36 The study further reported that postprandial BG values improved significantly. This observation has been confirmed by other small studies in CSII-treated patients.37,38
On the contrary, a 12-month randomized, controlled pediatric study (N = 45) was not able to demonstrate any additional effect of BC use with regard to HbA1c, postprandial BG values or other study outcomes.39
Factors Affecting Outcomes of Bolus Calculator Use
When evaluating the outcomes of BC use, one should keep in mind that the effectiveness of a BC is limited by the manner in which it is used. A BC must be used actively to serve its purpose and the input to the BC must be correct if the output should be equally so.
First, the constants of the bolus insulin equation need to be fairly accurate. If CF or ICR are set too low, the patient gets recurring hypos and vice versa. The BC BG target should be set according to the glycemic goals of the individual patient and will be reflected in the HbA1c over time. For BCs including IOB in the bolus calculation, DIA accuracy is equally important, because a DIA set too short leads to insulin stacking and if DIA is set too long, it may lead to a compensatory increase in basal rate. Recommendations that can guide the clinician in adjusting BC DIA settings are available.11
Second, successful outcomes from BC use depend on user skills. To provide relevant input to the BC, the patient needs to be able to adequately determine the CHO content of a meal, apply correct BG monitoring technique and have general insights into the diabetes disease and factors affecting the patient’s PS.
Third, the skills of the health care team may also affect BC outcomes. The team needs to be familiar with CC as well as the particular device and be trained in continuous adjustments of device settings since the constants of the bolus insulin equation typically change over time.
If the requirements mentioned above are not met, the BC output is likely to be false and as a consequence, the patient might lose confidence in the device and stop using it. One should not expect any effect from a BC, if it is not in use. Therefore, to get the greatest possible benefit from BC use it is important to train patients and their potential caretakers in general diabetes management as well as in the use of the device. To further stimulate treatment adherence, BC use should be addressed and BC settings should be evaluated routinely during consultations to emphasize their importance and make continuous use of the device meaningful to the patient.
Factors Affecting Outcomes of Bolus Calculator Studies
All factors affecting outcomes of BC use discussed so far also affect outcomes of BC studies and this should be taken into consideration when evaluating and comparing study results. Furthermore, BCs are often introduced coincident with CC or a CC refresher course and some amount of diabetes self-management training. This makes changes in glycemic control difficult to attribute to BC use only. In addition, the baseline HbA1c level of the study population is likely to determine the magnitude of the achievable change in HbA1c. Last, as is often the case with clinical studies, the patients included are typically particularly motivated, at least at study start, and may not represent the general T1D population.
Only 1 of the 14 studies reviewed above reported increased frequency of adverse events in users of BCs and that was an increase in the incidence of hypoglycemia in users of a PDA-based BC without IOB function.22 Six other publications included BCs without IOB function, all stand-alone BCs, but none of these reported increased hypoglycemia frequency. At least theoretically, IOB-estimations are important to prevent insulin stacking. Reasons for the absence of hypoglycemia could be related to high BG targets or other conservative BC settings, but it could also be due to low treatment adherence, for example, that the patient did not used the device consistently or made changes to the advice given by the BC. It may also be that MDI-users bolus less often than insulin pump users and therefore they generally do not encounter the problem of stacking. It should be noted, however, that although there were no reports of increased hypoglycemia frequency in studies of advanced BCs with IOB functions, the users of these devices may still stack insulin in specific situations. For instance, no advanced BC subtracts excess IOB from a meal bolus when the current BG is above the BG target, that is, they do not follow the logic of equation 3 and thereby the patients run the risk of insulin overdosing.
Conclusion
Bolus calculation is a demanding procedure and many patients can profit from BC assistance. BCs increase insulin bolus accuracy and shift the burden of calculations from the patient.
Clinical studies of BC use are still relatively few and study comparisons are complicated by heterogeneity across studies with regard to the actual BC, study design, intervention, duration, patient population, and outcome measures. Furthermore, many factors—besides BC use—may affect study outcomes as discussed in this review and this further complicates study interpretation. Nevertheless, there seems to be an increasing load of evidence that BCs may improve glycemic control and treatment satisfaction in some patients who use them actively. More studies of advanced automated BCs are in the pipeline and the results are eagerly awaited.
Some years ago, the BC and the insulin pump became combined together in 1 device. Perhaps the future holds more attractive combinations of diabetes technologies—1 obvious possibility would be a sensor-augmented BC.
Footnotes
Abbreviations: ADA, American Diabetes Association; BC, bolus calculator; BG, blood glucose; CC, carbohydrate counting; CF, correction factor; CHO, carbohydrate; CSII, continuous subcutaneous insulin infusion; DCCT, Diabetes Control and Complications Trial; DIA, duration of insulin action; DTSQ, Diabetes Treatment Satisfaction Questionnaire; ICR, insulin to carbohydrate ratio; IOB, insulin on board; MDI, multiple daily injections; PS, physiologic state; T1D, type 1 diabetes.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: SS has received speaker honoraria from Roche Diagnostics and serves on the advisory board of the same company. KN has received speaker honoraria from Roche Diagnostics, Animas, and Medtronic and serves on the advisory board of Medtronic.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a research grant from the Danish Diabetes Academy supported by the Novo Nordisk Foundation.
References
- 1. American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care. 2014;37(suppl 1):S14-S80. [DOI] [PubMed] [Google Scholar]
- 2. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977-986. [DOI] [PubMed] [Google Scholar]
- 3. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353(25):2643-2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Delahanty LM, Halford BN. The role of diet behaviors in achieving improved glycemic control in intensively treated patients in the Diabetes Control and Complications Trial. Diabetes Care. 1993;16(11):1453-1458. [DOI] [PubMed] [Google Scholar]
- 5. Gillespie SJ, Kulkarni KD, Daly AE. Using carbohydrate counting in diabetes clinical practice. J Am Diet Assoc. 1998;98(8):897-905. [DOI] [PubMed] [Google Scholar]
- 6. DAFNE Study Group. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: Dose Adjustment for Normal Eating (DAFNE) randomised controlled trial. BMJ. 2002;325(7367):746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Speight J, Amiel SA, Bradley C, et al. Long-term biomedical and psychosocial outcomes following DAFNE (Dose Adjustment for Normal Eating) structured education to promote intensive insulin therapy in adults with sub-optimally controlled Type 1 diabetes. Diabetes Res Clin Pract. 2010;89(1):22-29. [DOI] [PubMed] [Google Scholar]
- 8. Walsh PA, Roberts R. Pumping Insulin. 4th ed. San Diego, CA: Torrey Pines Press; 2006. [Google Scholar]
- 9. Davidson PC, Hebblewhite HR, Steed RD, et al. Analysis of guidelines for basal-bolus insulin dosing: basal insulin, correction factor, and carbohydrate-to-insulin ratio. Endocr Pract. 2008;14(9):1095-1101. [DOI] [PubMed] [Google Scholar]
- 10. Walsh J, Roberts R, Bailey T. Guidelines for insulin dosing in continuous subcutaneous insulin infusion using new formulas from a retrospective study of individuals with optimal glucose levels. J Diabetes Sci Technol. 2010;4(5):1174-1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Walsh J, Roberts R, Heinemann L. Confusion regarding duration of insulin action: a potential source for major insulin dose errors by bolus calculators. J Diabetes Sci Technol. 2014;8(1):170-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zisser H, Robinson L, Bevier W, et al. Bolus calculator: a review of four “smart” insulin pumps. Diabetes Technol Ther. 2008;10(6):441-444. [DOI] [PubMed] [Google Scholar]
- 13. Ahola AJ, Makimattila S, Saraheimo M, et al. Many patients with Type 1 diabetes estimate their prandial insulin need inappropriately. J Diabetes. 2010;2(3):194-202. [DOI] [PubMed] [Google Scholar]
- 14. Glaser NS, Iden SB, Green-Burgeson D, et al. Benefits of an insulin dosage calculation device for adolescents with type 1 diabetes mellitus. J Pediatr Endocrinol Metab. 2004;17(12):1641-1651. [DOI] [PubMed] [Google Scholar]
- 15. Sussman A, Taylor EJ, Patel M, et al. Performance of a glucose meter with a built-in automated bolus calculator versus manual bolus calculation in insulin-using subjects. J Diabetes Sci Technol. 2012;6(2):339-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cavanaugh K, Huizinga MM, Wallston KA, et al. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737-746. [DOI] [PubMed] [Google Scholar]
- 17. Marden S, Thomas PW, Sheppard ZA, et al. Poor numeracy skills are associated with glycaemic control in Type 1 diabetes. Diabet Med. 2012;29(5):662-669. [DOI] [PubMed] [Google Scholar]
- 18. Kordonouri O, Hartmann R, Remus K, et al. Benefit of supplementary fat plus protein counting as compared with conventional carbohydrate counting for insulin bolus calculation in children with pump therapy. Pediatr Diabetes. 2012;13(7):540-544. [DOI] [PubMed] [Google Scholar]
- 19. Smart CE, Evans M, O’Connell SM, et al. Both dietary protein and fat increase postprandial glucose excursions in children with type 1 diabetes, and the effect is additive. Diabetes Care. 2013;36(12):3897-3902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wolpert HA, Atakov-Castillo A, Smith SA, et al. Dietary fat acutely increases glucose concentrations and insulin requirements in patients with type 1 diabetes: implications for carbohydrate-based bolus dose calculation and intensive diabetes management. Diabetes Care. 2013;36(4):810-816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blazik M, Pankowska E. The effect of bolus and food calculator Diabetics on glucose variability in children with type 1 diabetes treated with insulin pump: the results of RCT. Pediatr Diabetes. 2012;13(7):534-539. [DOI] [PubMed] [Google Scholar]
- 22. Garg SK, Bookout TR, McFann KK, et al. Improved glycemic control in intensively treated adult subjects with type 1 diabetes using insulin guidance software. Diabetes Technol Ther. 2008;10(5):369-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kaufman FR, Halvorson M, Carpenter S. Use of a plastic insulin dosage guide to correct blood glucose levels out of the target range and for carbohydrate counting in subjects with type 1 diabetes. Diabetes Care. 1999;22(8):1252-1257. [DOI] [PubMed] [Google Scholar]
- 24. Maurizi AR, Lauria A, Maggi D, et al. A novel insulin unit calculator for the management of type 1 diabetes. Diabetes Technol Ther. 2011;13(4):425-428. [DOI] [PubMed] [Google Scholar]
- 25. Schmidt S, Meldgaard M, Serifovski N, et al. Use of an automated bolus calculator in MDI-treated type 1 diabetes: the BolusCal Study, a randomized controlled pilot study. Diabetes Care. 2012;35(5):984-990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. van Niel J, Geelhoed-Duijvestijn PH. Use of a smart glucose monitoring system to guide insulin dosing in patients with diabetes in regular clinical practice. J Diabetes Sci Technol. 2014;8(1):188-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ziegler R, Cavan DA, Cranston I, et al. Use of an insulin bolus advisor improves glycemic control in multiple daily insulin injection (MDI) therapy patients with suboptimal glycemic control: first results from the ABACUS trial. Diabetes Care. 2013;36(11):3613-3619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Anderson DG. Multiple daily injections in young patients using the ezy-BICC bolus insulin calculation card, compared to mixed insulin and CSII. Pediatr Diabetes. 2009;10(5):304-309. [DOI] [PubMed] [Google Scholar]
- 29. Schmidt S, Meldgaard M, Serifovski N, et al. Long-term use of an automated bolus calculator in type 1 diabetes. Diabetes Technol Ther. 2014;15(S1):A-1-A-154. [Google Scholar]
- 30. Gross TM, Kayne D, King A, et al. A bolus calculator is an effective means of controlling postprandial glycemia in patients on insulin pump therapy. Diabetes Technol Ther. 2003;5(3):365-369. [DOI] [PubMed] [Google Scholar]
- 31. Klonoff DC. The current status of bolus calculator decision-support software. J Diabetes Sci Technol. 2012;6(5):990-994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Voluntis Insulin Therapy Manager Receives CE Mark. 2013. Available at: http://www.voluntis.com/en/news/275-voluntis-insulin-therapy-manager-receives-ce-mark.html.
- 33. Charpentier G, Benhamou PY, Dardari D, et al. The Diabeo software enabling individualized insulin dose adjustments combined with telemedicine support improves HbA1c in poorly controlled type 1 diabetic patients: a 6-month, randomized, open-label, parallel-group, multicenter trial (TeleDiab 1 Study). Diabetes Care. 2011;34(3):533-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rossi MC, Nicolucci A, Pellegrini F, et al. Interactive diary for diabetes: a useful and easy-to-use new telemedicine system to support the decision-making process in type 1 diabetes. Diabetes Technol Ther. 2009;11(1):19-24. [DOI] [PubMed] [Google Scholar]
- 35. Cukierman-Yaffe T, Konvalina N, Cohen O. Key elements for successful intensive insulin pump therapy in individuals with type 1 diabetes. Diabetes Res Clin Pract. 2011;92(1):69-73. [DOI] [PubMed] [Google Scholar]
- 36. Lepore G, Dodesini AR, Nosari I, et al. Bolus calculator improves long-term metabolic control and reduces glucose variability in pump-treated patients with Type 1 diabetes. Nutr Metab Cardiovasc Dis. 2012;22(8):e15-e16. [DOI] [PubMed] [Google Scholar]
- 37. Klupa T, Benbenek-Klupa T, Malecki M, et al. Clinical usefulness of a bolus calculator in maintaining normoglycaemia in active professional patients with type 1 diabetes treated with continuous subcutaneous insulin infusion. J Int Med Res. 2008;36(5):1112-1116. [DOI] [PubMed] [Google Scholar]
- 38. Shashaj B, Busetto E, Sulli N. Benefits of a bolus calculator in pre- and postprandial glycaemic control and meal flexibility of paediatric patients using continuous subcutaneous insulin infusion (CSII). Diabet Med. 2008;25(9):1036-1042. [DOI] [PubMed] [Google Scholar]
- 39. Enander R, Gundevall C, Stromgren A, et al. Carbohydrate counting with a bolus calculator improves post-prandial blood glucose levels in children and adolescents with type 1 diabetes using insulin pumps. Pediatr Diabetes. 2012;13(7):545-551. [DOI] [PubMed] [Google Scholar]