Abstract
Diabetes, with its acute and long-term complications, has become a major health hazard in developing countries. An estimated 62.4 million people in India have diabetes. With increasing urbanization and industrialization, we can expect huge numbers of people with diabetes in India in the future. Moreover, all diabetes efforts in India are currently focused in urban areas while 70% of India’s population actually lives in rural areas. The current statistics demonstrates that urgent interventions are mandatory to curb the epidemic of diabetes and its complications at the grassroots level. This gap in providing diabetes care can be nullified by the use of tele-diabetology. This holds great potential to overcome barriers and improve quality and access to diabetes care to remote, underserved areas of developing counties. The Chunampet Rural Diabetes Prevention Project (CRDPP) has been developed and tested as a successful model for screening and delivering diabetes care to rural areas in developing countries. Using a tele-diabetology mobile van loaded with appropriate equipment, trained technicians, and satellite technology helped us to screen for diabetes and its complications and deliver diabetes care to remote villages in southern India. The Chunampet model can be applied in reaching out to remote areas where specialized diabetes care facilities may not be available.
Keywords: complications, CRDPP, diabetes, tele-diabetology, screening, telemedicine
In developing countries like India, noncommunicable diseases such as diabetes have already replaced communicable diseases as the major cause of death.1 The International Diabetes Federation (IDF) estimates that diabetes will affect over 552 million individuals worldwide by 2030.2 According to the recent national Indian Council of Medical Research—India Diabetes (ICMR-INDIAB) study, there are 62.4 million people with type 2 diabetes in India in 2011.3 With increasing urbanization and growing affluence and its consequent changes in lifestyle coupled with increasing life expectation, we can expect huge numbers of people with diabetes in India in the future.
Individuals who are known to have diabetes represent the tip of the iceberg as an equal or even larger number of patients have undiagnosed diabetes. They are at an even greater risk of adverse clinical outcomes as they are unaware of their condition. The ICMR-INDIAB study reported that the ratio of undiagnosed to diagnosed diabetes is higher in rural areas compared to the urban areas.3 Thus, if diabetes is not detected early and treated adequately, there is a high risk of developing both macrovascular disease (coronary artery disease and cerebrovascular disease or stroke, and peripheral vascular disease) and microvascular disease (retinopathy, nephropathy, and neuropathy).4 Even among self-reported diabetic individuals, fewer than one-third have their diabetes under good control.5 Population data on micro and macro vascular complications of diabetes are available in urban India.6-10 However, such data were not available in rural India. This is largely because in rural areas, diabetes remains a neglected field, as awareness levels and accessibility to diabetes health care remains woefully inadequate. Although the prevalence of diabetes is lower in rural India, the total number of diabetic subjects in rural areas is much higher, since over 70% of the population in India live in rural areas, half of whom are below the poverty line and continue to fight for survival and health, although all this is rapidly changing due to economic development.5 In rural population, the main challenges for screening for diabetes and its complications are inadequate health care resources, poor infrastructure, lack of awareness and illiteracy, limited of physicians and paramedical staff trained in diabetes, limited access to health care due to problems with transport, and unaffordability due poverty.11 It is necessary to develop models of care tailored to rural areas to provide better access to screening for diabetes and its complications leading to better treatment. To reach remote and medically underserved communities in rural areas, telecommunication technologies can be used to facilitate the delivery of health care to patients and provide access to health care professionals located in specialized centers in cities.12
Tele-diabetology in Screening Diabetes and Associated Complications
What is telemedicine? Telemedicine is defined as a tool that uses telecommunication to support health care in remote areas and its main purpose is to facilitate a beneficial interaction between the patient and the health care provider to achieve improved treatment and lower treatment costs.13 Telemedicine helps to reduce the burden for health care personnel so that only those patients with more advanced disease requiring tertiary-level treatment need to be brought to the specialist hospitals in cities for management.
The telemedicine concept has been used in developed countries for a number of years, especially in North America, Australia, and Europe, where a substantial body of literature has emerged about their successes and short comings.14 In India, the telemedicine concept was introduced in 2000, in Andhra Pradesh by the Apollo Aragonda Hospital, which was inaugurated by then US president Bill Clinton. This became the world’s first very small aperture terminal (VSAT)-enabled village hospital. Today, with 115 centers including 9 overseas, the Apollo Telemedicine Networking Foundation (ATNF) is the oldest and largest multispecialty telemedicine network.15 The Sankara Nethralaya and the Aravind Eye Hospitals in Tamilnadu and the Tripura Vision Centre in Tripura also have successfully used telemedicine to screen for eye diseases (Tele-Ophthalmology) in rural regions of India in the general population.16-19 In the study conducted by Sankara Nethralaya between April 2009 and September 2010, 54 751 patients underwent evaluation at 872 camps across 4 states in India. During this period, uncorrected refractive error was found to be the commonest cause of avoidable blindness (59%), followed by cataract (30%). Retinal diseases, mainly diabetic retinopathy, contributed 3.3% of avoidable blindness, and corneal diseases accounted for 1%. When they assessed patient satisfaction levels during teleophthalmology consultation, it was reported that patients who asked questions during the screening were 2.18 times more likely to be satisfied with teleophthalmology than those who did not.20 The Sankara Nethralaya experience is described in greater detail in another article in this symposium. The Aravind Comprehensive Eye Survey Research Group Study18 showed that the prevalence of diabetic retinopathy in rural south Indian population using tele-ophthalmology was 10.5%. Only 6.7% of individuals with diabetic retinopathy had previous eye examinations.
Telemedicine is currently being used in the field of diabetes at many medical centers in the United States including Harvard Medical School, Joslin Diabetes Center, and Massachusetts Institute of Technology. In addition, tele-consultation for diabetes is also now being used worldwide.21-23 Tele- diabetology may be beneficial in improving access, care, and outcome in diabetic patients. In Native Hawaiian and Alaskan population,24 the use of telemedicine in chronic disease management such as diabetes, was found to have potential to improve patient care in remote indigenous populations and may supplement patient-provider relationships. In 2006, telemedicine was initiated by us at the Madras Diabetes Research Foundation (MDRF) for screening of diabetes and its complications and to provide diabetes health care and prevention to a rural south Indian population in the south eastern state of Tamil Nadu in collaboration with the World Diabetes Foundation, Denmark and the Indian Space Research Organization (ISRO) in Bangalore, India, through the Chunampet Rural Diabetes Prevention Project (CRDPP).25 The rest of the article focuses on the CRDPP Model.
The Chunampet Rural Diabetes Prevention Project Model
The CRDPP is a rural community outreach program undertaken in a cluster of 42 villages in and around Chunampet in the Chithamur block in the Kancheepuram district of Tamil Nadu state in southern India, with an adult population of 27 014 (refer to http://www.mdrf.in/telemedicine.html for a map of the study area). The main goals of the CRDPP were to increase awareness, screen and provide treatment plan of diabetes in the underserved regions. A door-to-door survey was carried out to screen for diabetes (a fasting capillary blood glucose test using a handheld glucose monitor [One Touch® Ultra,® LifeScan, Milpitas, CA, USA] and self-reported diabetes) in subjects aged ≥ 20 years in all selected villages and details on demographic and socioeconomic characteristics, health behavior, knowledge of diabetes and its complications, health status and medical history of the subjects and their families, and their perception of health, diet, and physical activity was collected using a structured questionnaire. In addition, anthropometric and clinical measurements including weight, height, waist circumference, and blood pressure were obtained. An oral glucose tolerance test (OGTT) was done to confirm diabetes status (using venous blood) in those who had fasting capillary blood glucose (CBG) ≥ 126 mg/dl (≥7 mmol/liter). Those confirmed to have diabetes by OGTT, and all self-reported diabetes subjects, underwent screening for diabetes-related complications in a fully equipped mobile tele-diabetology van with satellite connectivity.
The infrastructure for screening diabetes and associated complications diabetes in the tele-diabetology van includes facilities for blood sampling, a digital retinal camera, a slit lamp, computerized electrocardiogram (ECG), Doppler imaging, and biothesiometry (Figure 1). The mobile van also has other facilities like videoconferencing equipment with a television screen, air conditioning, a generator for uninterrupted power supply, computers, a laser printer, and basic furniture. The mobile van is linked to the tertiary care center—Dr Mohan’s Diabetes Specialties Center (DMDSC) in Chennai through the VSAT satellite connectivity provided by ISRO.
Figure 1.
Tele-diabetology van and facilities to screen for diabetic complications.
Screening for all complications in the identified diabetic subjects (self-reported and newly detected diabetes) was being done by trained technicians/optometrists and unemployed youth recruited from the local area who were trained at our the tertiary care center at Gopalapuram in Chennai. Retinopathy screening was done using 7-field color retinal photography in the mobile tele-diabetology van by trained optometrist. The retinal photographs were then sent by satellite network to our center in Chennai. The ophthalmologists then graded the photographs by the Modified Early Treatment Diabetic Retinopathy Study Grading System.26 Using video conferencing, the consultants then interacted with patients, explained about the present condition and formulated the treatment and follow-up plans (Figure 2). The consultant also used the opportunity to educate the patient about diabetes. In addition, also photographs of foot lesions (Figure 3) were also transmitted to the center for further opinion on follow-up. This figure shows a typical neuropathic (tropic) ulcer diagnosed during the screening in a long-standing patient with type 2 diabetes. Chiropody was done at the rural center and special diabetic foot wear was also provided to offload the pressures. The patient has done well and could avoid the trip to the city for this treatment.
Figure 2.

Tele-consultation under way between the mobile van (Chunampet) and tertiary care hospital (DMDSC, Chennai).
Figure 3.

Photographs of a foot lesion taken in mobile van show a typical neuropathic (tropic) ulcer diagnosed during the screening in a long-standing patient with type 2 diabetes. Chiropody was done at the rural centre and special diabetic foot wear was also provided to offload the pressures.
Glycemic control of self-reported diabetes subjects was assessed by measuring Hemoglobin A1c (HbA1c) levels. The entire screening in the van was offered free to cost to all individuals.
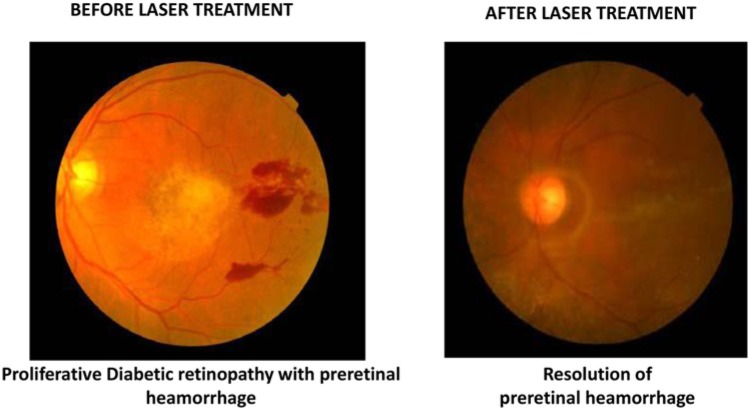
Individuals, identified through screening, with diabetes and early complications were then offered follow-up care at the Sai Rural Diabetes Specialties Centre, our rural diabetes center established at Illedu near Chunampet in Kancheepuram districts to provide regular follow-up care (Figure 4). Those who could not afford to pay were given free treatment while others were treated at heavily subsidized costs. This center is manned by physicians and paramedical staff who were all recruited locally but trained at the main hospital in Chennai. Individuals identified through tele-diabetology screening to have sight threatening retinopathy requiring laser treatment or cataract surgery or patients with more advanced diabetic foot, heart, or kidney complications requiring surgical treatment or hospitalization were referred to the main center at Chennai. All surgeries were offered free of cost or at subsidized rates and in addition free transport was also provided. Figure 5 shows the retinal photographs taken before and after laser treatment in a diabetic individual identified through the CRDPP. This patient had proliferative diabetic retinopathy (PDR) with preretinal hemorrhage (sight-threatening diabetic retinopathy) picked up during screening by telemedicine. Patient was advised to undergo fundus fluorescein angiography (FFA) and panretinal photocoagulation at the Chennai center. Using telemedicine, vision loss was prevented in this patient, as PDR can lead to vitreous hemorrhage and permanent blindness.
Figure 4.

Sai Rural Diabetes Specialties Centre, Chunampet for follow-up care.
Figure 5.
Retinal photographs taken before and after laser treatment in patient identified through this program. This patient had proliferative diabetic retinopathy (PDR) with preretinal hemorrhage (sight-threatening diabetic retinopathy) picked up during screening by telemedicine. Patient was advised to undergo fundus fluorescein angiography (FFA) and panretinal photocoagulation at the Chennai center.
Figure 6 provides the schematic flow of activities undertaken in CRDPP. Overall, using the CRDPP tele-diabetology model 23 380 individuals were screened for diabetes, of whom 1138 (4.9%) had diabetes. Of the 1001 diabetes subjects who were screened for complications, diabetic retinopathy was detected in 18.2%, neuropathy in 30.9%, microalbuminuria in 24.3%, peripheral vascular disease in 7.3%, and coronary artery disease in 10.8%.25 On 1-year follow-up of the glycemic control of the diabetic subjects, it was observed that the mean HbA1c levels decreased from 9.3 ± 2.6% to 8.5 ± 2.4%. Of the diabetic subjects screened for complications, 4.9% (49/1001) had severe diabetic retinopathy and 3.2% (32/1001) had severe foot complications requiring referral to the hospital in Chennai for laser photo-coagulation and hospitalization respectively.25
Figure 6.
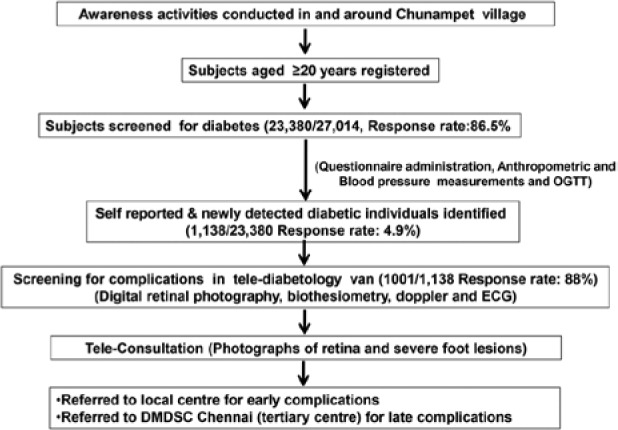
Flow of activities in CRDPP.
The CRDPP model has been highly successful and was well received by the local community. According to Klonoff,27 a telemedicine program can be judged as successful if it meets 4 criteria by being sound, effective, cost-effective, and practical. The CRDPP model is reproducible and can be scaled up as the screening was mostly done by people without formal education who were given hands on training. As technicians were recruited from the local rural population, were able to provide employment to the rural people. Tele-diabetology model is found to be specifically useful as the patients do not need to travel substantial distances to visit a specialist to get a proper diagnosis and treatment for diabetes. From a health provider perspective, this program is feasible compared as it does not need the full time services of highly qualified specialists. In addition, education about diabetes and its complications to the rural population helps to increase awareness about diabetes. However, more data are needed on the cost-effectiveness of the CRDPP Model.
The advantages of tele-diabetology are summarized in Figure 7. One of the main advantages is that, it helps detection and management of diabetes and its complications in remote areas of countries where such medical facilities are nonexistent. Employment opportunities have also been provided to many of the local youth, thus providing a source of livelihood to the villagers. This successful rural health care model can be scaled up and made available in other parts of our country provided infrastructural support, adequate training, and capacity building is done. The CRDPP has been recognized as a model for screening and delivering diabetes care to rural areas in developing countries.28
Figure 7.
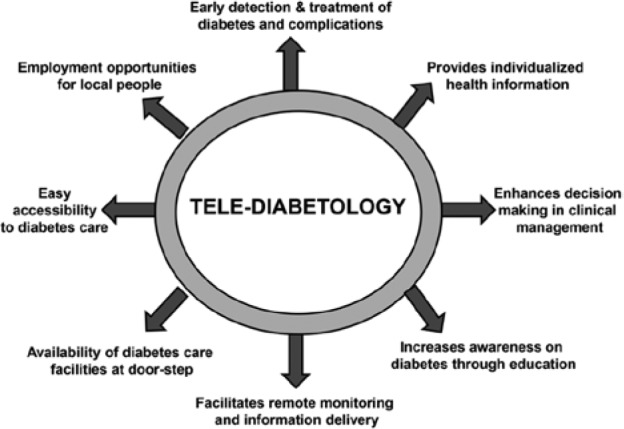
Advantages of tele-diabetology.
Conclusions
Tele-diabetology holds great potential to overcome barriers and improve quality, access to diabetes care to remote underserved areas of developing counties. It has special significance to India considering its vast geographical spread and predominant rural population where diabetes care is currently not available accessible or affordable using a mobile van with appropriate equipment, trained technicians, and satellite technology helped us to screen for diabetes and its complications and also bridge the gap between patient and diabetes care providers. We also increased awareness through mass diabetes education regarding the importance of strict glycemic control and diabetic complications and their prevention and ensured accessibility to diabetes health services in a large number of villages in southern India. There is ample scope for tele-diabetology to improve diabetes care outcomes, in terms of reducing the rate of secondary complications in both developed and developing nations, but obviously more data are needed especially on its cost-effectiveness.
Footnotes
Abbreviations: ATNF, Apollo Telemedicine Networking Foundation; CBG, capillary blood glucose; CRDPP, Chunampet Rural Diabetes Prevention Project; DMDSC, Dr Mohan’s Diabetes Specialties Centre; ECG, Electrocardiogram; ICMR-INDIAB, Indian Council of Medical Research, India Diabetes Study; IDF, International Diabetes Federation; ISRO, Indian Space Research Organization; MDRF, Madras Diabetes Research Foundation; OGTT, oral glucose tolerance test; VSAT, very small aperture terminal.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The CRDPP was supported by a grant from the World Diabetes Foundation, Denmark, and the satellite link for telemedicine services was donated by the Indian Space Research Organization, Bangalore, India. Land was donated by Mr. C. Ramakrishna to establish a rural center for diabetes in Chunampet, India.
References
- 1. World Health Organization. Preventing Chronic Diseases: A Vital Investment. WHO global report. Geneva, Switzerland; 2005. [Google Scholar]
- 2. World Health Organization, International Diabetes Federation. Diabetes Atlas. Unwin N, Whiting D, Guariguata L, Ghyoot G, Gan D, eds. 5th ed. Brussels, Belgium: International Diabetes Federation; 2011. [Google Scholar]
- 3. Anjana RM, Pradeepa R, Deepa M, et al. ICMR-INDIAB Collaborative Study Group: prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research—INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022-3027. [DOI] [PubMed] [Google Scholar]
- 4. Donnelly R, Emslie-Smith AM, Gardner ID, Morris AD. ABC of arterial and venous disease: vascular complications of diabetes. BMJ. 2000;320:1062-1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Census of India. Rural Urban Distribution of Population. Office of the Registrar General and Census Commissioner, India. Available at: http://censusindia.gov.in/2011-prov-results/paper2/data_files/india/Rural_Urban_2011.pdf. Accessed October 31, 2013.
- 6. Rema M, Premkumar S, Anitha B, Deepa R, Pradeepa R, Mohan V. Prevalence of diabetic retinopathy in urban India: the Chennai Urban Rural Epidemiology Study (CURES) Eye Study I. Invest Ophthalmol Vis Sci. 2005;46:2328-2333. [DOI] [PubMed] [Google Scholar]
- 7. Unnikrishnan RI, Rema M, Pradeep R, et al. Prevalence and risk factor of diabetic nephropathy in an urban south Indian population; the Chennai Urban Rural Epidemiology study (CURES-45). Diabetes Care. 2007;30:2019-2024. [DOI] [PubMed] [Google Scholar]
- 8. Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban south Indian population: the Chennai Urban Rural Epidemiology Study (CURES-55). Diabetes Med. 2008;25:407-412. [DOI] [PubMed] [Google Scholar]
- 9. Premalatha G, Shanthi Rani CS, Deepa R, Markovitz J, Mohan V. Prevalence and risk factors of peripheral vascular disease in a selected south Indian population—the Chennai Urban Population Study (CUPS). Diabetes Care. 2000;23:295-1300. [DOI] [PubMed] [Google Scholar]
- 10. Mohan V, Deepa R, Shanthi Rani S, Premalatha G. Prevalence of coronary artery disease and its relationship to lipids in a selected population in south India. J Am Coll Cardiol. 2001;38:682-687. [DOI] [PubMed] [Google Scholar]
- 11. Joshi SR, Das AK, Vijay VJ, Mohan V. Challenges in diabetes care in India: sheer numbers, lack of awareness and inadequate control. J Assoc Physicians India. 2008;56:443-450. [PubMed] [Google Scholar]
- 12. Maheu MM, Whitten P, Allen A, eds. E-Health, Telehealth, and Telemedicine: A Guide to Start Up and Success. New York, NY: Jossey-Bass; 2001. [Google Scholar]
- 13. Klonoff DC. Using telemedicine to improve outcomes in diabetes—an emerging technology. J Diabetes Sci Technol. 2009;3:624-628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Demiris G, Tao D. An analysis of the specialized literature in the field of telemedicine. J Telemed Telecare. 2005;11:316-319. [DOI] [PubMed] [Google Scholar]
- 15. Ganapathy K, Ravindra A. Telemedicine in India: the Apollo story. Telemed J E Health. 2009;15:576-585. [DOI] [PubMed] [Google Scholar]
- 16. John S, Sengupta S, Reddy SJ, Prabhu P, Kirubanandan K, Badrinath SS. Sankara Nethralaya mobile teleophthalmology model for comprehensive eye care delivery in rural India. Telemed J E Health. 2012;18:382-387. [DOI] [PubMed] [Google Scholar]
- 17. Aravind Tele-Ophthalmology. Available at http://www.aravind.org/telemedicine/mobilevan.htm. Accessed October 31, 2013.
- 18. Bai VT, Murali V, Kim R, Srivatsa SK. Teleophthalmology-based rural eye care in India. Telemed J E Health. 2007;13:313-321. [DOI] [PubMed] [Google Scholar]
- 19. Tripura Vision Care Tele-ophthalmology. Available at: http://www.cips.org.in/public-sector-systems-government-innovations/documents/best-practices-in-health-care-tripura-vision-centre-project.pdf. Accessed October 31, 2013.
- 20. Paul PG, Raman R, Rani PK, Deshmukh H, Sharma T. Patient satisfaction levels during teleophthalmology consultation in rural South India. Telemed J E Health. 2006;12:571-580. [DOI] [PubMed] [Google Scholar]
- 21. Fatehi F, Gray LC, Russell AW. A clinimetric study of outpatient diabetes consultations: the potential for telemedicine substitution. Diabetes Technol Ther. 2014;16:8-14. [DOI] [PubMed] [Google Scholar]
- 22. Franc S, Borot S, Ronsin O, et al. Telemedicine and type 1 diabetes: is technology per se sufficient to improve glycaemic control? Diabetes Metab. 2014;40:61-66. [DOI] [PubMed] [Google Scholar]
- 23. Dy P, Morin PC, Weinstock RS. Use of telemedicine to improve glycemic management in a skilled nursing facility: a pilot study. Telemed J E Health. 2013;19:643-645. [DOI] [PubMed] [Google Scholar]
- 24. Hiratsuka V, Delafield R, Starks H, Ambrose AJ, Mau MM. Patient and provider perspectives on using telemedicine for chronic disease management among Native Hawaiian and Alaska Native people. Int J Circumpolar Health. 2013:5;72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mohan V, Deepa M, Pradeepa R, et al. Chunampet. Prevention of diabetes in rural India with a telemedicine intervention. J Diabetes Sci Technol. 2012;6:1355-1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Early Treatment of Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology. 1991;98:786-806. [PubMed] [Google Scholar]
- 27. Klonoff DC. Diabetes and telemedicine: is the technology sound, effective, cost-effective, and practical? Diabetes Care. 2003;26:162-168. [DOI] [PubMed] [Google Scholar]
- 28. Patel V, Chatterji S, Chisholm D, et al. India: Towards universal health coverage 3—chronic diseases and injuries in India. Lancet. 2011;377:413-428. [DOI] [PubMed] [Google Scholar]