Abstract
As technology continues to develop rapidly, the incidence of obesity also continues to climb at an alarming rate. The increase in available technology is thought to be a contributor in the obesogenic environment, yet at the same time technology can also be used to intervene and improve health and health behaviors. This article reviews the components of effective weight management programs and the novel role that technology, such as SMS, websites, and smartphone apps, is playing to improve the success of such programs. Use of these modern technologies can now allow for individualized treatment recommendations to be delivered to individuals remotely, increased self-monitoring/tracking of health-related data, broader and more rapid dissemination of health information/recommendations, and increased patient–dietician/physician contact. The use of technology in weight management programs results in improved long-term weight management, and in most cases improved cost-effectiveness. Rather than blaming increased food intake and sedentary lifestyle on technology, rapidly developing and innovative technologies should be used to our advantage and deployed to combat the obesity epidemic.
Keywords: obesity, weight loss, Internet, smartphone
Phenotypically, the world’s population is the largest in history1 and children, unfortunately, are not spared in this epidemic as childhood obesity is of international concern.2 It was recently projected that without an attenuation of current weight gain trends, 1.35 billion people worldwide will be overweight and 573 million obese by 2030.3 Clearly there is a necessity to determine the most effective programs for treatment as well as prevention of weight gain and obesity.
Parallel to the increase in obesity, society is experiencing the development of huge technological advances. Individuals are more reliant than ever before on computers and computer technology to perform many tasks of daily living not only in the workplace but also in their home environments. While the technological boom might be to blame for increased access to calorie dense processed foods and sedentary behaviors, technology is also being swiftly developed to play a role in health management. In this growing technological age, there is revived hope that devices will be developed to provide real-time feedback on energy intake and energy expenditure. Many leading groups envisage that sophisticated, as well as scientifically tested, weight management interventions will be translated to technological platforms that allow dissemination to millions of individuals at the same time.4,5 In this review, we summarize the emerging field of electronic health (eHealth) and mobile health (mHealth) for weight management. First, we reflect on integral components of successful weight management programs and consider how these can be maintained or even more effectively delivered with current technology. Second, we review the current commercially available devices and technology platforms that might be useful for weight management and, where possible, review efficacy of these in scientific, peer-reviewed studies. Finally, we provide possible insights for translation of weight management programs through integrated devices and mobile technology.
Targets for Obesity treatment
Obesity is a result of long-term positive energy balance regardless of the macronutrient composition of the diet.6 As a result, countless weight management interventions have been developed to focus on lifestyle modifications that promote sustained reductions in energy intake, increased physical activity, or both.7 For the most part these interventions demonstrate variable efficacy which is primarily owed to fluctuations in adherence of individuals to the assigned program.8,9 Intensive lifestyle interventions that incorporate a behavior modification component are associated with higher weight loss and long-term success.10,11 A structured behavior modification program harnessed on social learning theories is considered the gold-standard approach for intensive inventions targeting weight loss.12 The hope is that throughout the course of the structured intervention, individuals will make permanent changes in behavior that will allow the renewed energy intake and energy expenditures to continue after the intervention is complete and ensure long-term maintenance of weight loss.
Hallmark, multicenter, and internationally reputable clinical trials for weight loss management in obese individuals include Pounds Lost,13 the Diabetes Prevention Program or DPP,14 and the Look AHEAD trial,15 all funded by the National Institutes of Health. The cornerstone features of these trials recognized alongside the weight loss and weight loss maintenance success were (1) establishment of individualized weight loss goals, (2) frequent contact with individuals in both a one-on-one setting as well as in a group situation, (3) frequent monitoring of body weight as well as activity and food intake data, (4) delivery of a structured behavior modification program by highly trained behaviorists or dietitians, and (5) monitoring of individual adherence with “toolbox” strategies to help individuals overcome specific barriers to achieve weight loss success (use of portion controlled foods, exercise videos, etc).16,17 While these studies were successful, they were highly intensive lifestyle interventions which equates to substantial burden in regard to both time and resources. While Herman et al reported long-term cost-effectiveness of the DPP intensive lifestyle intervention, the price per capita was estimated at US$4600.18 In the past 5 years, there have been several successful attempts by investigators and clinicians to modify intensive lifestyle interventions such as DPP to be more cost-effective.19-21 These studies have used varying degrees of technology from telephone calls, SMS, study-specific websites and most recently smartphone applications. Therefore, with the constant development of new technologies, researchers are trying to integrate technology into weight management programs. The overall goal is to deliver intensive lifestyle modification programs remotely without compromising weight loss efficacy, while at the same time significantly reducing burden to the individual.
Cardinal Features of Successful Weight Management Programs and Adaptation to eHealth
When evaluating the most efficacious weight management interventions such as DPP, Look AHEAD and Pounds Lost, 3 components are commonly represented.16,17,22 The intervention includes a behavioral component that addresses behavior change, encourages self-monitoring of individual data (weight, steps), and provides personalized recommendations and feedback. As researchers strive to translate traditional weight management interventions to eHealth, these 3 pillars of a successful intervention should be incorporated.23
Behavior Change Modification Therapy
Behavior therapy, when applied to weight control, is a goal-centered approach that provides techniques to help individuals modify eating, activity, and thinking habits that may be associated with excess weight.23 Many weight loss interventions will result in successful weight loss, at least for the short term. However, after a weight loss intervention concludes, many individuals will regain the weight lost even with subsequent therapeutic support24 though some will maintain their weight loss.25 To combat weight regain, various types of behavior therapy have been incorporated into weight loss interventions.26,27 The Look AHEAD study uses attenuated frequency, but continued interaction between the interventionist and participant to prevent or address weight regain with success well into the fourth year of the study.23
The use of wellness coaches is becoming more popular within health care settings to aid in behavioral modification. Whether this service is provided within the Veterans Affairs system or through a health insurance company, interaction with a wellness coach provides personalized attention to behavior change, and this approach has been shown to produce greater weight loss in comparison to traditional methods.28 The unique feature of individualized weight loss programs facilitated by a wellness coach is delivery of continuous and data-driven feedback to foster behavior change.29 While intensive programs employing frequent in-person contact are most efficacious, they are unable to reach the estimated 200 million U.S. adults who are overweight or obese as they are expensive and inefficient for widespread scalability. A review of diabetes prevention lifestyle interventions, though they are likely cost-effective, estimates average costs to be approximately $27 000 per quality-adjusted life-year.15,18
Self-monitoring of Individual Data
Self-monitoring or the systematic observation of one’s own behavior allows an individual to become more aware of the extent to which he or she is engaging in a particular activity. When self-monitoring, participants are able to quickly identify a behavior that may have positive or detrimental effects on the success or failure to meet set goals. Examples of self-monitoring behaviors in weight management interventions include weighing on a regular basis, frequent recording/tracking of food and/or exercise, and tracking television or computer use. Self-monitoring of behaviors during weight management programs has been shown to facilitate adherence and lead to increased effectiveness.30
Body Weight Tracking
Weighing every 1 to 3 days has been shown to result in improved weight loss. For example, individuals who weighed daily lost approximately 1 BMI unit (kg/m2) more than individuals who weighed only weekly and 3 BMI units more than individuals who did not weigh at all.31-33 In general, frequent monitoring (every 1 to 3 days) has been shown to be associated with the greatest efficacy in weight loss settings.
Self-monitoring Food Intake
Although individuals underestimate food intake by an average of 18%,34,35 monitoring food intake has been demonstrated as a successful self-monitoring tool leading to increased weight loss. Boutelle et al suggest that recording foods consumed at least 75% of the time is a reasonable goal for self-monitoring food intake and more likely to result in weight loss.36
Self-monitoring of Physical Activity
Although the use of activity self-monitoring has not been as widely studied as self-monitoring body weight, studies suggest, activity monitoring is associated with greater weight loss success.37 Furthermore, self-monitoring of physical activity also leads to improved adherence to physical activity goals and higher physical activity levels.37 Physical activity recorded as a diary entry tends to be overreported however the use of pedometers or accelerometers provides a more accurate estimate of daily activity and thereby better allows for goals and feedback to be more closely monitored and evaluated.38 Self-monitoring and reporting during a weight management intervention, when provided to an interventionist, allows for individualized feedback and recommendations.
Individualized Intervention Programs
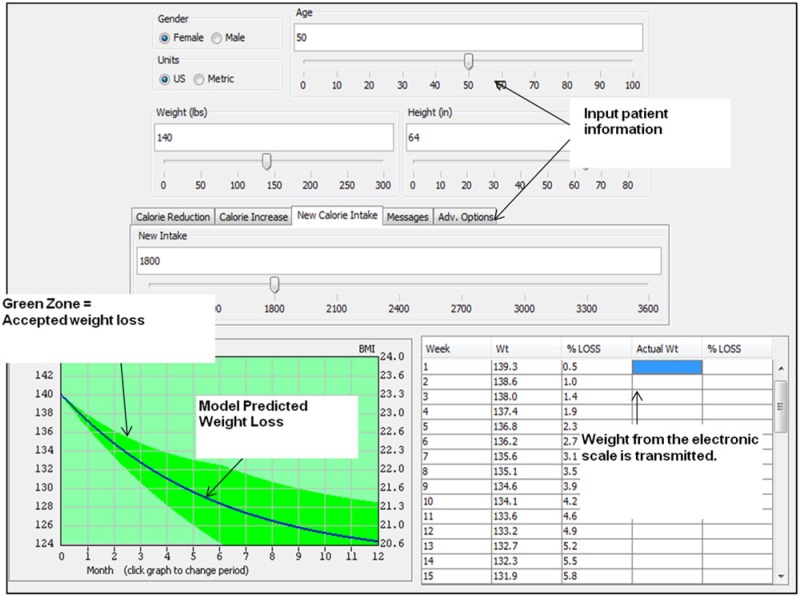
National dietary39 and physical activity40 recommendations serve as recommendations for the general public and are not based on the specific needs of an individual. However, when individualized recommendations are given, greater improvements in dietary quality are seen than with general messages.41 To make individual recommendations more personalized, applied mathematicians in collaboration with obesity researchers have recently modeled expected weight change, as well as food intake and energy expenditure changes in response to weight loss interventions. The mathematical models have been derived from the richest and most comprehensive datasets of individuals enrolled in lifestyle interventions. Importantly model predictions can be determined on the basis of individual parameters at the onset of the weight loss intervention. The models have been extrapolated into user-friendly software platforms on the web and are available for use by the public. Two examples include http://www.pbrc.edu/research-and-faculty/calculators/weight-loss-predictor/ and http://bwsimulator.niddk.nih.gov. As shown (Figure 1), by inputting demographic and physiological characteristics for an individual at the onset of a weight management program as well as the target level of calorie restriction, an estimated trajectory of weight change is computed from the model.4,42,43 The weight loss projection is then deployed in the intervention as a tool to guide adherence. It is anticipated that these kinds of models will become an integral feature of weight management interventions in the future. This approach has already been used in a large multicenter clinical trial of calorie restriction to drive and track weight loss.22 The benefit of using the models are 2-fold: (1) individuals are more likely to experience weight loss success since realistic levels of dietary intake can be set to achieve a target goal weight and (2) individuals can be easily trained on how to interpret the weight loss chart and by overlaying or plotting weight recorded during an intervention, self-monitoring of weight loss can be enhanced. Given that the underlying models are centered on the energy balance equation, the weight change at a given point in time can indicate compliance to the dietary intake goal. One of these online weight loss calculators44 allows for the weight loss trajectory to be stored on a local computer and actual body weight can be imputed and automatically overlaid onto the weight chart for long-term monitoring22,44 by individuals and interventionists.
Figure 1.
Mathematical models are used to generate personalized caloric prescriptions for weight loss. Individual parameters (sex, age, weight, height) are imputed to generate personalized weight graphs that show the expected trajectory of weight change as well as upper and lower limits for a given caloric prescription.
Use of Modern Technology for Delivery of Obesity Management
In an attempt to increase access to health care, increase intervention cost-effectiveness, reduce barriers for participation, improve treatment compliance, and decrease dropout rates, adopting many modern technologies into weight management interventions has been investigated. Ideally an eHealth intervention would incorporate each of the cornerstone features of successful obesity treatments reviewed above. Given that an estimated 56% of Americans have access to the Internet by way of a smartphone45 development of web-based applications or “apps” for delivery through mobile devices are at the forefront of several health conditions including diabetes, obesity/overweight, mental health, tobacco use, and many others.46 For instance, at the time of writing (May 2013), the search terms “eHealth” and “mHealth” returned 154 and 23 studies on clinicaltrials.gov, respectively, indicating that electronic and mobile technologies have a large presence in current research. These studies are incorporating devices to aid in self-monitoring of weight, food intake, and physical activity, and client–counselor interactions through SMS, email, and/or study-specific websites. A summary of commercially available apps for diet, activity or weight monitoring is provided in Table 1. Very few of these apps have been validated against gold-standard measures of dietary intake and physical activity, and thus further research is required.
Table 1.
Commercially Available Internet Applications or “Apps” Used for Diet, Lifestyle, and Physical Wellness.
| App name | App platform | Type of app | App features | Additional devices needed | Cost | Efficacy |
|---|---|---|---|---|---|---|
Couch to 5K
|
iPhone | Exercise | Weight loss, physical activity, builds up your endurance to run a 5K, timer | None | Free | No data available |
Eat Local
|
iPhone | Diet | Local produce locator and recipe suggestions | None | Free | No data available |
Endomondo
|
iPhone, Android, Blackberry | Exercise | Can be used for a variety of sports: running, cycling, and walking, showing GPS tracking route, distance, duration, and calories burned | None | Free version and a Pro version for less than $3 | No data available |
FitBit
|
iPhone, Android, PC | Exercise, diet, and sleep log | Main function as an accelerometer; able to act as a food and activity diary or sync to other apps (MyFitnessPal); some devices also monitor sleep | One of the FitBit devices | Free | FitBit One counts steps reliably73 |
Fitness Buddy
|
iPhone, Android | Exercise | Weight loss, physical activity, workouts utilizing gym equipment; excellent app for strength training | None | Free version and paid version for $1.99 | No data available |
FitnessFast
|
iPhone | Exercise | Users can log workouts, body stats, sleep, etc | None | $1.99 | No data available |
Fitocracy
|
iPhone, Android | Exercise | Used like a video game to play against others and gain points and levels based on frequency, duration, and difficulty of workouts | None | Free | No data available |
Fooducate
|
iPhone, Android | Diet | Barcode scanner, tracks your weight, clues into the nutritional quality of food | None | Free | No data available |
GAINFitness
|
iPhone | Exercise | Free workout; in-app purchase “packs” feature options like basketball training, yoga, or circuit strength | None | Free in iTunes; in-app purchases range from $3 up to $30 | No data available |
iStepLog
|
iPhone | Exercise | Records your steps and daily physical activity; synchronization with Step Log on the 10,000 Steps website | Steps website | Free | Use was associated with increased likely hood to log steps71 |
iTrackBites
|
iPhone, Android | Diet and exercise | Assigns food scores and points to each food; food diary similar to weight watchers | None | $1.99 for iPhone and $2.99 for Android | No data available |
Map My Run
|
iPhone, Android, BlackBerry | Exercise | Allows users to map their runs through the phone’s GPS | None | Free, $2.99 for Plus | No data available |
Moves
|
iPhone | Exercise | Smart pedometer that records everything from steps taken in a day to miles cycled | None | Free | No data available |
MyFitnessCompanion
|
Android | Diet and Exercise | Personalized exercise tracking; weight monitoring, blood pressure, food intake, asthma, blood glucose, insulin, HbA1c, cholesterol, temp, respiration, oxygen, intraocular pressure, bowel movements, heart rate using Bluetooth sensors or manual input | Microsoft HealthVault | Free with different levels of paid versions | No data available |
MyFitnessPal
|
Android, BlackBerry, Windows, iPhone | Diet and exercise | Barcode scanner, database of foods, food diary. | None | Free | No data available |
My Meal Mate (MMM)
|
Android | Diet | Allows users to map their eating habits by selecting the products they consume; first free app to contain a large UK-based food database | None | Free | Accuracy of food diary equal to that of 24 hour food recall; more adherent to app than website or paper methods; overall weight loss of 4.6 kg over 6 months64 |
Nike Training Club
|
iPhone, Android | Diet and Exercise | Weight loss, physical activity, select a goal and fitness level then the app creates several 30-45 min workout options; pictures; timer | None | Free | No data available |
Nike+ Running
|
iPhone, Android | Exercise | Allows users to map their runs through the phone’s GPS | None | Free | No data available |
UP by Jawbone
|
iPhone, Android | Exercise | Wristband that tracks movement and sleep; displays data and allows users to input meals and mood | Wristband | Free | No data available |
Weightbot
|
iPhone | Diet | Tracks self-entered weights and calculates BMI | None | $1.99 | No data available |
WellnessFX
|
iPhone | Overall wellness | Platform for developing, maintaining, and sharing personal health goals; vitamin shop | None | Free | No data available |
Weight Watchers Mobile
|
iPhone, Android | Diet and Exercise | Tracks dietary intake, activity, and weight | Can be used with or without Weight Watchers subscription | Free | When used in conjunction with the comprehensive Weight Watchers program, subjects were 8 times more likely to reach their goal of 5-10% weight loss than those in the self-help group74 |
There have been significant technological advances in all areas of self-monitoring tools. Wireless scales such as those by BodyTrace, FitBit Aria, and Withings transmit body weight in real-time via Bluetooth to the product website. The product website tracks weight history which can be viewed and monitored by the individual or an interventionist/clinician. This is also evident for physical activity monitors. Monitors such as those by Nike+, FitBit, and BodyMedia Fit can collect and transmit activity data to a website or app through the use of Bluetooth technology.
Similarly, analysis of diet records was reliant on a dietician or dietary clinic to access to corporate nutrition databases. Now there are countless nutrition databases available to the public free of charge including the USDA Nutrient Database, http://ndb.nal.usda.gov/. Individual users are now able to self-enter the foods consumed and receive immediate nutritional analysis. These databases can also be readily accessed from almost anywhere through smartphone-based applications.
Web-based Interventions
Web-based interventions, as the name suggests, are interventions hosted on the Internet. Web-based interventions may be used to distribute nutrition, lifestyle, and behavior education material, may aid in self-monitoring, and may provide a medium for participant-participant interaction or personalized feedback from a health care provider. Web-based interventions have the ability to deliver standardized, tailored information to a large number of people simultaneously. Web-based interventions, like many eHealth interventions, can easily involve family members. Chen et al developed a web-based intervention to deliver behavior, dietary, and physical activity information to adolescents and their parents. Intervention compliance was ~70% and significantly decreased the adolescents’ waist-hip ratio.47 Van Genugten et al developed a modest website based intervention to prevent weight gain in obese adults through decreasing caloric intake by 100 kcal/day and increasing physical activity. Though the randomized participants were asked to view only 3 to 4 online modules, compliance to the intervention was poor and decreased with time. The authors suspect, due to poor intervention compliance, no significant changes were seen in BMI.48 Web-based intervention can also be used for long-term weight loss or maintenance after intensive weight loss intervention. As seen with increased self-monitoring, the amount of website interaction was proportional to success.49-53 Web-based interventions can serve as the sole intervention or as support to a more intensive intervention. It can be isolated to an individual, encourage family participation, or be connected to a larger social network. Bennett et al reported greater weight loss with a web-based intervention than when compared to traditional care and suggested that web-based care could be integrated into traditional care plans to increase treatment effectiveness.52 When behavior modification therapy is integrated into the web-based intervention with personalized feedback, Tate et al observed greater weight loss and decreases in waist circumference.54 Regardless of function, eHealth/mHealth interventions must be used frequently by the participant to be a useful tool and aid in success. Because successful web-based interventions require consistent interaction from their participants, they must have the ability to keep the participants engaged and avoid becoming a passive educational tool. Intensive, interactive web-based interventions can be quite costly and time consuming to develop. It takes a large amount of time to assess the desires of a population, develop a web-based intervention, and test that intervention. Riiser et al fear that preferences and public demands will have changed by the time a web-based intervention becomes available to the public making it less effective.55 Though developmental costs of web-based interventions are high, Meenan et al found the web-based intervention in the Weight Loss Maintenance Trial cost substantially less than standard phone and in-person treatment programs.21
SMS
With the popularity and reliance on cell phones, short message service as a way to communicate quickly and easily with people has also gained popularity. SMS is accessible almost relentlessly by most individuals and proves to be a fast, interactive medium while being inexpensive. SMS was first utilized as an intervention tool in developed countries, although as time progresses, SMS is becoming more widely used in developing and developed countries alike.56 Tailored automated SMS containing diet, lifestyle, and behavior information has been widely used and well received in adolescents.57 Though well accepted by participants, SMS diet, physical activity, and behavior change intervention effectiveness varies.58-60 While SMS is a quick, easy, and inexpensive way to communicate with study participants and provides personalized feedback, SMS can provide only a limited amount of information in a 160-character-limit message. SMS may be more beneficial as a communication tool within a larger intervention rather than being the sole intervention delivery system.
Internet-based Applications
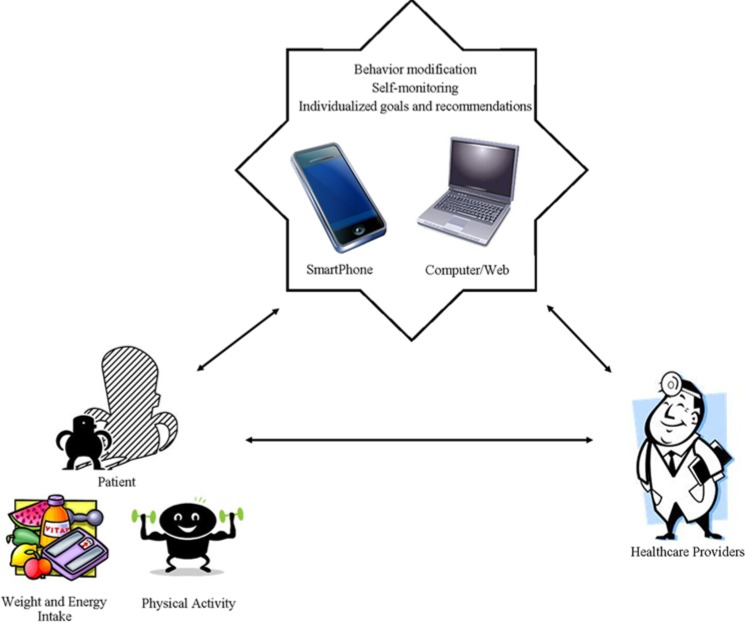
The rising popularity of smartphone applications provides a unique opportunity to influence health behavior.61 There are countless health care and fitness apps available on various operating systems (eg, iPhone, Android; Figure 2).62 Many of these apps are free or inexpensive allowing them to be readily available to the general public which contributes to their potential to be used in weight loss and management. Advantages of utilizing apps for weight management include low cost, low burden, ease in delivery, and capability of wide dissemination.61 While there are thousands of commercially available health and fitness apps, there is little research (validation, efficacy, usability, or otherwise) done using commercially available apps. For this reason, we do not intend for this to be a systematic review, but a discussion of commercially available apps. When looking at which apps to discuss, we focused on those apps listed as most popular (both free and paid) in iTunes and the Android Market. We then used the app name, “app,” “eHealth,” and/or “mHealth” to review the literature for research using these apps and others.
Figure 2.
Mobile phone and Internet program can be used to enhance communication and weight management interventions between a patient and his or her health care providers. We are currently working with our graphic designer on a high-definition image.
Many health care and fitness apps use self-monitoring to promote use and behavior change. Weight management apps use many strategies to incorporate self-monitoring mainly through tracking each food that is consumed and its respective portion size. Typically, these apps include comprehensive databases of foods, barcode scanners with the ability to identify packaged products, and the option for manual entry of unknown foods or favorite recipes. Many of these apps focus on calorie counting to achieve energy balance or deficit (for weight loss). MyFitnessPal, Lose it!, FatSecret’s Calorie Counter, SparkPeople, and Fooducate are popular apps that use these strategies for recording intake. MyFitnessPal, Lose it!, FatSecret’s Calorie Counter, and SparkPeople feature both diet and physical activity tracking through calorie counting, while Fooducate focuses solely on diet by providing a database of foods, offering nutritional quality information, and grading foods in the database. In addition, some apps include recipe builders and forums for support, questions, and recipe sharing (iTunes App Store, Android Market). Turner-McGrievy et al conducted a behavioral weight loss intervention in overweight adults investigating the effect of self-monitoring food intake by traditional pen-and-paper method compared to use of a web-based app. Fat Secret’s Calorie Counter, MyFitnessPal, and Lose it! were the most popular apps used for recording food intake.63 Other work suggests that individuals using an app to monitor dietary intake compared to those using traditional pen-and-paper methods have significantly more weight loss.64
Several research groups have developed their own smartphone apps for intervention studies focusing on nutrition education, recording energy intake, and support. Brindal et al developed static and support versions of an app focusing on a commercial meal replacement program, Celebrity Slim MRP. The Celebrity Slim MRP recommends replacing 2 meals a day with meal replacement shakes, 1 well-balanced meal, and up to 3 snacks (Celebrity Slim MRP http://celebrityslim.com.au/). The static version of the intervention app included a guide to the Celebrity Slim MRP. The Support app version included the static guide to the Celebrity Slim MRP as well as other support features including a meal calendar, a weight tracker, tasks log, and prompts for weighing and tracking food intake 3 times daily. Usage data showed that the Support app users were more engaged in the app throughout the study period, and the Support app users perceived that they weighed themselves more frequently than the static app users. The mean difference in weight loss between the Support (3.2%) and static app (2.2%) users was not significant (P = .08).65 Carter et al developed the My Meal Mate smartphone app designed to promote weight loss. The My Meal Mate smartphone app was developed using an evidence-based approach of goal setting, self-monitoring, and feedback using text messaging.64 In a validation study to assess the correlation between using the smartphone app to track food and beverage consumption and the 24-hour recall method, energy intake recorded on the My Meal Mate smartphone app correlated well with 24-hour dietary recalls from 2 study days.66 Carter et al compared the My Meal Mate smartphone app to website and paper diaries for promoting weight loss in a pilot study. In the pilot study, all groups included a similar intervention using 3 different delivery methods. Results showed that retention was highest in the smartphone app group (93%) as compared to the website (55%) and paper diary (53%) groups. In addition, adherence was higher in the smartphone app group as compared to the website and paper diary groups (P < .001). Mean weight change was significantly greater in the smartphone app group (–4.6 kg) as compared to the website group (–1.3 kg) and to the paper diary group (–2.9 kg) at 6 months of the intervention (P = .004).64 Well-established companies that specialize in weight management programs, such as Weight Watchers, Atkins, South Beach, and so on, have also developed apps to support their weight management programs, and to our knowledge efficacy data are not available.
The apps described thus far are helpful in weight management as a self-monitoring tool, but they remain subjected to an underestimation of actual energy intake due to self-report. Research has been focused on using mobile technology to develop objective methods for assessing dietary intake. For instance, researchers and app developers have recently developed technology that uses the camera function of the smartphone to capture images of foods.67-70 The most advanced food photography programs have partnered with computer science engineers to analyze the food photos before and after meals to derive estimates of calorie and nutritional information. In a much simpler approach than recording food intake in an app or on paper, an individual is instructed to capture a before meal photo. About 15 minutes later, a text message is received prompting a photo of the after meal photo. Users are also prompted to report a description of the meal and can either text or voice record the details, scan a barcode of a commercially available product, or enter a PLU (price look-up code) for fruits or vegetables. A semiautomated computer program then assesses portion size of the individual meal components and amount consumed. With the use of the USDA Nutrient Database (http://ndb.nal.usda.gov/), nutrient analysis of each item can be completed resulting in a more objective assessment of total energy intake. These food photography programs have been validated against doubly labeled water and have been shown to be an accurate and precise measure of energy intake.67,69 Like all interventions, user burnout can be a barrier to success. To combat this problem, messages are sent to remind the participant to reengage in the app and continue to send photos of his or her food. This prompting system can be used in a variety of ways in various eHealth and mHealth interventions to reduce user burnout and increase overall participation and compliance. Several large clinical trials are now under way using the remote food photography method to capture food intake in free-living individuals.
In addition to apps developed to track food intake or promote positive health behavior, various physical activity apps have been developed as well. Some use self-monitoring, similarly to diet strategies, by tracking physical activity and exercise occurrences including MyFitnessPal, Lose it!, FatSecret’s Calorie Counter, and SparkPeople (iTunes App Store, Android Market).61-63 These apps include databases of numerous activities (eg, dancing, aerobics, housework, gardening, swimming and running) that can be added to a daily energy tracker. Typically, calories burned from these activities are subtracted from the daily calorie goal. Other apps like Fitocracy and RunKeeper include physical activity tracking databases without recording food intake. Recent advancements in GPS capability in smartphones have allowed for the development of physical activity apps that can track activities (eg, running, biking, walking) accurately through GPS rather than relying on self-report methods. Some GPS capable apps that can track physical activity, utilizing GPS for tracking route, distance, duration, and calories burned include RunKeeper, Endomondo, and Map my Run (iTunes App Store, Android Market). There are some free pedometer apps available that use GPS capabilities to count and log steps including Pedometer Free, Pedometer Ultimate, and Pedometer Step Counter (iTunes App Store, Android Market). At a cost of $1.99, the Couch to 5K app provides a 5K training guide for people who want to train for a 5K gradually from low physical activity levels. Another unique app, Fitness Buddy, provides a catalog of exercises with step by step directions. Fitness buddy is especially useful for strength training exercises, and it also includes built-in workouts (iTunes App Store, Android Market). Turner-McGrievy et al found that RunKeeper, Fat Secret’s Calorie counter, and MyFitnessPal were the most commonly used self-monitoring physical activity apps in their intervention study.63 Kirwan et al evaluated the effect of the iStepLog smartphone app use in their website-delivered physical activity program and the perceived usefulness of the iStepLog smartphone app. The iStepLog app was developed to allow the recording of daily physical activity with automatic synchronization to the website-delivered physical activity program log. Findings from the study showed that iStepLog app use was associated with increased likelihood to log steps.71 Cowan et al evaluated the content of several physical activity iPhone apps for the presence of behavior change theories and strategies. They concluded that the majority of the apps comprised of minimal behavior change content and that price was correlated with the quality of the content.72
There is little scientific evidence to support the use of many of the available devices and technologies for therapeutics. This makes it difficult to recommend one app over another, and this leaves a great area for future research for clinicians, laboratory researchers, and industry alike. Studies that involve head to head comparisons of the usability and efficacy of the apps along with studies that validate the technologies against gold-standard research methods are warranted. Literature suggests that diet and physical activity apps that incorporate self-monitoring, education, and support strategies have the potential for success; however, for apps to be most successful, they should be appropriately validated against standard objective assessments of energy intake and expenditure (eg, doubly labeled water, accelerometry, directly weighed foods, etc). Validating existing apps against standard methods could determine if the app is evidence-based, accurate, and clinically relevant. A novel approach however would be to incorporate mathematical models of energy balance that were derived from these kinds of objective data into the app framework. This would allow for weight loss programs to be customized to individual users and, when partnered with devices for wireless measurement of weight, food, and activity data, can deliver data-driven feedback to facilitate self-monitoring and improve weight loss efficacy.
Conclusions
While the obesity epidemic may be blamed on the increase in food intake and sedentary behavior associated with the current technology boom, the wide use of modern devices and frequent access to the Internet provides a unique opportunity to direct the management of obesity through eHealth platforms. Current studies have used SMS messaging, chat rooms, study-specific websites, and telephone calls to deliver weight management programs with equal if not better efficacy than traditional in-person approaches. With the rapidly growing number of devices for remote collection of body weight as well as food intake and activity data, the next era of obesity management will include development of a virtual obesity management clinic. More than likely housed in an app designed for mobile devices, the virtual clinic will transmit data from individuals remotely in their own home to the clinical team. Ideally, mathematical models will underlie these apps so that patients and clinicians, with reasonable accuracy, can gauge the level of adherence against goals established for weight loss (absolute as well as rate), daily food intake, and levels of activity. This new era of research currently under way serves to indicate if complex behavioral interventions for weight loss can be disseminated remotely with modern technology and with similar if not better efficacy than those gold-standard interventions performed only in expensive clinical trials.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by NIH grants (U01DK094418, R00HD060762, R01DK099175) to Leanne Redman.
References
- 1. World Health Organization. Overweight and Obesity: Fact sheet N°311. Available at: http://www.who.int/gho/ncd/risk_factors/obesity_text/en/index.html. Accessed May 28, 2013.
- 2. Arroyo K, Herron D. The epidemiology of obesity. In: Thompson CC.ed. Bariatric Endoscopy. New York, NY: Springer; 2013:1-9. [Google Scholar]
- 3. Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008;32(9):1431-1437. [DOI] [PubMed] [Google Scholar]
- 4. Thomas DM, Schoeller DA, Redman LA, Martin CK, Levine JA, Heymsfield SB. A computational model to determine energy intake during weight loss. Am J Clin Nutr. 2010;92(6):1326-1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thomas DM, Navarro-Barrientos JE, Rivera DE, et al. Dynamic energy-balance model predicting gestational weight gain. Am J Clin Nutr. 2012;95(1):115-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McAllister EJ, Dhurandhar NV, Keith SW, et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr. 2009;49(10):868-913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Miller WC, Koceja DM, Hamilton EJ. A meta-analysis of the past 25 years of weight loss research using diet, exercise or diet plus exercise intervention. Int J Obes Related Metab Disord. 1997;21(10):941-947. [DOI] [PubMed] [Google Scholar]
- 8. Del Corral P, Chandler-Laney PC, Casazza K, Gower BA, Hunter GR. Effect of dietary adherence with or without exercise on weight loss: a mechanistic approach to a global problem. J Clin Endocrinol Metab. 2009;94(5):1602-1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Delany JP, Kelley DE, Hames KC, Jakicic JM, Goodpaster BH. Effect of physical activity on weight loss, energy expenditure and energy intake during diet induced weight loss. Obesity. 2014;22:363-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cowburn G, Hillsdon M, Hankey CR. Obesity management by life-style strategies. Brit Med Bull. 1997;53(2):389-408. [DOI] [PubMed] [Google Scholar]
- 11. Unick JL, Beavers D, Bond DS, et al. The long-term effectiveness of a lifestyle intervention in severely obese individuals. Am J Med. 2013;126(3):236-242, 42 e1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation. 2012;125(9):1157-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Eng J Med. 2009;360(9):859-873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Eng J Med. 2002;346(6):393-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Look ARG, Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Eng J Med. 2013;369(2):145-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165-2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Anton SD, LeBlanc E, Allen HR, et al. Use of a computerized tracking system to monitor and provide feedback on dietary goals for calorie-restricted diets: the POUNDS LOST study. J Diabetes Sci Technol. 2012;6(5):1216-1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Herman WH, Edelstein SL, Ratner RE, et al. Effectiveness and cost-effectiveness of diabetes prevention among adherent participants. Am J Managed Care. 2013;19(3):194-202. [PMC free article] [PubMed] [Google Scholar]
- 19. Vadheim LM, McPherson C, Kassner DR, et al. Adapted diabetes prevention program lifestyle intervention can be effectively delivered through telehealth. Diabetes Educator. 2010;36(4):651-656. [DOI] [PubMed] [Google Scholar]
- 20. Hunter CM, Peterson AL, Alvarez LM, et al. Weight management using the Internet a randomized controlled trial. Am J Prev Med. 2008;34(2):119-126. [DOI] [PubMed] [Google Scholar]
- 21. Meenan RT, Stevens VJ, Funk K, et al. Development and implementation cost analysis of telephone- and Internet-based interventions for the maintenance of weight loss. Int J Technol Assess Health Care. 2009;25(3):400-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rickman AD, Williamson DA, Martin CK, et al. The CALERIE Study: design and methods of an innovative 25% caloric restriction intervention. Contemp Clin Trials. 2011;32(6):874-881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wadden TA, Neiberg RH, Wing RR, et al. Four-year weight losses in the Look AHEAD study: factors associated with long-term success. Obesity. 2011;19(10):1987-1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299(10):1139-1148. [DOI] [PubMed] [Google Scholar]
- 25. Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 suppl):222S-225S. [DOI] [PubMed] [Google Scholar]
- 26. Cooper Z, Doll HA, Hawker DM, et al. Testing a new cognitive behavioural treatment for obesity: a randomized controlled trial with three-year follow-up. Behav Res Ther. 2010;48(8):706-713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Paxman JR, Hall AC, Harden CJ, O’Keeffe J, Simper TN. Weight loss is coupled with improvements to affective state in obese participants engaged in behavior change therapy based on incremental, self-selected “small changes.” Nutr Res. 2011;31(5):327-337. [DOI] [PubMed] [Google Scholar]
- 28. Shahnazari M, Ceresa C, Foley S, Fong A, Zidaru E, Moody S. Nutrition-focused wellness coaching promotes a reduction in body weight in overweight US veterans. J Acad Nutr Dietetics. 2013;113:928-935. [DOI] [PubMed] [Google Scholar]
- 29. Matteson M, Russell C. Systematic review of continuous self-improvement interventions. Clin Nurs Stud. 2013;1(1):10-25. [Google Scholar]
- 30. Reyes NR, Oliver TL, Klotz AA, et al. Similarities and differences between weight loss maintainers and regainers: a qualitative analysis. J Acad Nutr Dietetics. 2012;112(4):499-505. [DOI] [PubMed] [Google Scholar]
- 31. Jeffery RW, Sherwood NE, Brelje K, et al. Mail and phone interventions for weight loss in a managed-care setting: Weigh-To-Be one-year outcomes. Int J Obes Related Metab Disord. 2003;27(12):1584-1592. [DOI] [PubMed] [Google Scholar]
- 32. Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. 2005;30(3):210-216. [DOI] [PubMed] [Google Scholar]
- 33. Butryn ML, Phelan S, Hill JO, Wing RR. Consistent self-monitoring of weight: a key component of successful weight loss maintenance. Obesity. 2007;15(12):3091-3096. [DOI] [PubMed] [Google Scholar]
- 34. Hill RJ, Davies PS. The validity of self-reported energy intake as determined using the doubly labelled water technique. Br J Nutr. 2001;85(4):415-430. [DOI] [PubMed] [Google Scholar]
- 35. Trabulsi J, Schoeller DA. Evaluation of dietary assessment instruments against doubly labeled water, a biomarker of habitual energy intake. Am J Physiol Endocrinol Metab. 2001;281(5):E891-E899. [DOI] [PubMed] [Google Scholar]
- 36. Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obes Res. 1998;6(3):219-224. [DOI] [PubMed] [Google Scholar]
- 37. Conroy MB, Yang K, Elci OU, et al. Physical activity self-monitoring and weight loss: 6-month results of the SMART trial. Med Sci Sports Exerc. 2011;43(8):1568-1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Andre D, Wolf DL. Recent advances in free-living physical activity monitoring: a review. J Diabetes Sci Technol. 2007;1(5):760-767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. USDA DHHS. Dietary Guidelines for Americans. 2010. [Google Scholar]
- 40. DHHS. 2008 Physical Activity Guidelines for Americans. 2008.
- 41. Campbell MK, DeVellis BM, Strecher VJ, Ammerman AS, DeVellis RF, Sandler RS. Improving dietary behavior: the effectiveness of tailored messages in primary care settings. Am J Pub Health. 1994;84(5):783-787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hall KD, Jordan PN. Modeling weight-loss maintenance to help prevent body weight regain. Am J Clin Nutr. 2008;88(6):1495-1503. [DOI] [PubMed] [Google Scholar]
- 43. Pieper C, Redman L, Racette S, et al. Development of adherence metrics for caloric restriction interventions. Clin Trials. 2011;8(2):155-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Thomas DM, Martin CK, Heymsfield SB, Redman LM, Schoeller DA, Levine JA. A simple model predicting individual weight change in humans. J Biol Dynamics. 2011;5(6):579-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Smith A. Smartphone ownership 2013. Pew Internet; 2013; Available at: http://www.pewinternet.org/2013/06/05/smartphone-ownership-2013/. Accessed June 11, 2013.
- 46. Fiordelli M, Diviani N, Schulz PJ. Mapping mhealth research: a decade of evolution. J Med Internet Res. 2013;15(5):e95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chen JL, Weiss S, Heyman MB, Cooper B, Lustig RH. The efficacy of the web-based childhood obesity prevention program in Chinese American adolescents (Web ABC study). J Adolesc Health. 2011;49(2):148-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. van Genugten L, van Empelen P, Boon B, Borsboom G, Visscher T, Oenema A. Results from an online computer-tailored weight management intervention for overweight adults: randomized controlled trial. J Med Internet Res. 2012;14(2):e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Funk KL, Stevens VJ, Appel LJ, et al. Associations of Internet website use with weight change in a long-term weight loss maintenance program. J Med Internet Res. 2010;12(3):e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hansen AW, Gronbaek M, Helge JW, Severin M, Curtis T, Tolstrup JS. Effect of a web-based intervention to promote physical activity and improve health among physically inactive adults: a population-based randomized controlled trial. J Med Internet Res. 2012;14(5):e145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Brindal E, Freyne J, Saunders I, Berkovsky S, Smith G, Noakes M. Features predicting weight loss in overweight or obese participants in a web-based intervention: randomized trial. J Med Internet Res. 2012;14(6):e173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Bennett GG, Herring SJ, Puleo E, Stein EK, Emmons KM, Gillman MW. Web-based weight loss in primary care: a randomized controlled trial. Obesity. 2010;18(2):308-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sarwer DB, von Sydow Green A, Vetter ML, Wadden TA. Behavior therapy for obesity: where are we now? Curr Opinion Endocrinol Diabetes Obes. 2009;16(5):347-352. [DOI] [PubMed] [Google Scholar]
- 54. Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285(9):1172-1177. [DOI] [PubMed] [Google Scholar]
- 55. Riiser K, Londal K, Ommundsen Y, Sundar T, Helseth S. Development and usability testing of an Internet intervention to increase physical activity in overweight adolescents. JMIR Res Protocols. 2013;2(1):e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Deglise C, Suggs LS, Odermatt P. Short message service (SMS) applications for disease prevention in developing countries. J Med Internet Res. 2012;14(1):e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Woolford SJ, Clark SJ, Strecher VJ, Resnicow K. Tailored mobile phone text messages as an adjunct to obesity treatment for adolescents. J Telemed Telecare. 2010;16(8):458-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Bauer S, de Niet J, Timman R, Kordy H. Enhancement of care through self-monitoring and tailored feedback via text messaging and their use in the treatment of childhood overweight. Patient Educ Counseling. 2010;79(3):315-319. [DOI] [PubMed] [Google Scholar]
- 59. Patrick K, Raab F, Adams MA, et al. A text message-based intervention for weight loss: randomized controlled trial. J Med Internet Res. 2009;11(1):e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Shaw R, Bosworth H. Short message service (SMS) text messaging as an intervention medium for weight loss: a literature review. Health Inform J. 2012;18(4):235-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Hebden L, Cook A, van der Ploeg HP, Allman-Farinelli M. Development of smartphone applications for nutrition and physical activity behavior change. JMIR Res Protocols. 2012;1(2):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Vandewater EA, Denis LM. Media, social networking, and pediatric obesity. Pediatr Clin N Am. 2011;58(6):1509-1519, xii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Turner-McGrievy GM, Beets MW, Moore JB, Kaczynski AT, Barr-Anderson DJ, Tate DF. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J Am Med Inform Assoc. 2013;20(3):513-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Carter MC, Burley VJ, Nykjaer C, Cade JE. Adherence to a smartphone application for weight loss compared to website and paper diary: pilot randomized controlled trial. J Med Internet Res. 2013;15(4):e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Brindal E, Hendrie G, Freyne J, Coombe M, Berkovsky S, Noakes M. Design and pilot results of a mobile phone weight-loss application for women starting a meal replacement programme [published online ahead of print March 21, 2013]. J Telemed Telecare. [DOI] [PubMed] [Google Scholar]
- 66. Carter MC, Burley VJ, Nykjaer C, Cade JE. “My Meal Mate” (MMM): validation of the diet measures captured on a smartphone application to facilitate weight loss. Br J Nutr. 2012:1-8. [DOI] [PubMed] [Google Scholar]
- 67. Martin CK, Correa JB, Han H, et al. Validity of the Remote Food Photography Method (RFPM) for estimating energy and nutrient intake in near real-time. Obesity. 2012;20(4):891-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Daugherty BL, Schap TE, Ettienne-Gittens R, et al. Novel technologies for assessing dietary intake: evaluating the usability of a mobile telephone food record among adults and adolescents. J Med Internet Res. 2012;14(2):e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Zhu F, Bosch M, Woo I, et al. The use of mobile devices in aiding dietary assessment and evaluation. IEEE J Selected Top Signal Processing. 2010;4(4):756-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Lieffers JR, Hanning RM. Dietary assessment and self-monitoring with nutrition applications for mobile devices. Can J Diet Pract Res. 2012;73(3):e253-e260. [DOI] [PubMed] [Google Scholar]
- 71. Kirwan M, Duncan MJ, Vandelanotte C, Mummery WK. Using smartphone technology to monitor physical activity in the 10,000 Steps program: a matched case-control trial. J Med Internet Res. 2012;14(2):e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Cowan LT, Van Wagenen SA, Brown BA, et al. Apps of steel: are exercise apps providing consumers with realistic expectations?: a content analysis of exercise apps for presence of behavior change theory. Health Educ Behav. 2013;40(2):133-139. [DOI] [PubMed] [Google Scholar]
- 73. Takacs J, Pollock CL, Guenther JR, Bahar M, Napier C, Hunt MA. Validation of the FitBit One activity monitor device during treadmill walking [published online ahead of print October 31, 2013]. J Sci Med Sport. [DOI] [PubMed] [Google Scholar]
- 74. Johnston CA, Rost S, Miller-Kovach K, Moreno JP, Foreyt JP. A randomized controlled trial of a community-based behavioral counseling program. Am J Med. 2013;126(12):1143 e19-e24. [DOI] [PubMed] [Google Scholar]