Abstract
Objectives. We estimated the effect of the ACA expansion of dependents’ coverage on health care expenditures and utilization for young adults by race/ethnicity.
Methods. We used difference-in-difference models to estimate the impact of the ACA expansion on health care expenditures, out-of-pocket payments (OOP) as a share of total health care expenditure, and utilization among young adults aged 19 to 26 years by race/ethnicity (White, African American, Latino, and other racial/ethnic groups), with adults aged 27 to 30 years as the control group.
Results. In 2011 and 2012, White and African American young adults aged 19 to 26 years had significantly lower total health care spending compared with the 27 to 30 years cohort. OOP, as a share of health care expenditure, remained the same after the ACA expansion for all race/ethnicity groups. Changes in utilization following the ACA expansion among all racial/ethnic groups for those aged 19 to 26 years were not significant.
Conclusions. Our study showed that the impact of the ACA expansion on health care expenditures differed by race/ethnicity.
In 2009, approximately 30% of the population aged 19 to 30 years, labeled the “young invincibles,” were uninsured.1 This group represented 1 in 5 uninsured individuals in the United States.2 In September 2010, the Affordable Care Act (ACA) extended eligibility for dependents’ coverage under family private health insurance up to age 26 years.3 Under the ACA expansion of dependents’ coverage, enrollment of employer-sponsored health insurance plans for young adult dependents significantly increased.3–8 Research showed that this ACA provision reduced the number of uninsured young adults by at least 3 million individuals.3 Recent studies that used nationally representative data also showed that this ACA expansion significantly reduced young adults’ out-of-pocket payments (OOP).9,10
Young adults’ health spending patterns with the rollout of the ACA may affect the nation’s aggregate health spending growth rate in the long term. Lack of health insurance may result in limited access to health care, and delaying or forgoing necessary treatment, potentially leading to health problems and greater health expenditures in mid-adulthood.11,12 Understanding the influence of the expansion specifically on young racial/ethnic minorities is critical, because inadequate access to health care is a major driver of racial/ethnic disparities in health.
More than 50% of Latino and one third of African American young adults aged 20 to 29 years were uninsured in 2008 and 2009, compared with 25% of non-Latino White (White) young adults.13 Lack of health insurance coverage across racial/ethnic groups has been associated with uncertainty over family health expenditures, potentially ruinous OOP, and lower health care access and use.14–17 Because racial/ethnic minorities had low rates of health insurance coverage before the ACA implementation, it is likely that racial/ethnic minorities would benefit from the ACA expansion on dependents’ coverage. By contrast, this ACA expansion of dependents’ coverage only focused on those whose parents had employer-sponsored health insurance. Compared with Whites, African Americans and Latinos were less likely to have employer-provided private coverage because of income and immigration status, and thus might be less likely to benefit from this expansion. Because of the differences in health insurance coverage, employment status, demographic characteristics, socioeconomic status, and clinical needs, health care expenditures and use patterns might differ by race/ethnicity under the ACA expansion of dependents’ coverage. It is critical to understand these differentiated responses to predict the racial/ethnic disparities in health care under overall ACA health care reform, and to design policies to improve efficiency and equity of the health care system. To our knowledge, this is the first study that examined the effect of the ACA expansion of dependents’ coverage on health care spending and use by race/ethnicity.
METHODS
We used the Medical Expenditure Panel Survey,18 which is a nationally representative survey of the civilian, noninstitutionalized population in the United States. This survey provides information of respondents’ health care spending, use, and insurance during the survey year, as well as demographic, socioeconomic, and health characteristics.
Variables
Outcome variables.
Our outcome variables were total health care spending, shares of patients’ OOP of their total health care spending, and the probabilities of using any health care during the survey year. Health care use and expenditures were self-reported and validated by respondents’ physicians and pharmacists. These outcome variables were used previously in the literature.19–21 All health care expenditures were adjusted to constant dollars using the 2012 Consumer Price Index medical component.
Key independent variables.
We had 3 groups of key independent variables: (1) the indicator of the timing of the survey with respect to the ACA expansion of dependents’ coverage (1 = survey year of 2011 or 2012, after the ACA implementation; 0 = survey year of 2008 or 2009, before the implementation), (2) respondents’ races/ethnicities matched by age (treatment group: White, African American, Latino, and other races/ethnicities, all aged 19–26 years; and the control group: White, African American, Latino, and other races/ethnicities, all aged 27–30 years), and (3) the interaction terms between the indicator of the ACA expansion and each race/ethnicity and age variable.
Other covariates.
We used the conceptual framework of Andersen social behavioral model22 to select the covariates. These covariates were also widely used in the literature to examine racial/ethnic disparities in health care expenditures and use.19–21,23,24 According to the Andersen model, health care expenditures and use varied by respondents’ predisposition, enabling, and need factors. Predisposition factors reflected respondents’ demographic characteristics and cultural background. In addition to race/ethnicity, we controlled for gender and marital status. As proxies for US acculturation, we also included interview language and whether the respondent was US-born, foreign-born with < 10 years residence in United States, and foreign-born with ≥ 10 years residence in the United States. Enabling factors controlled in our study were education (schooling years ≤ 12 years, 13–16 years, and > 16 years), family income (< 100% federal poverty level [FPL], 100%–199% FPL, and ≥ 200% FPL), employment status, health care access (having usual source of care), and insurance status (uninsured, private health insurance, and public health insurance). We considered contextual factors to be enabling factors that measured access to health care and exposure to different regional health policies.19,23 We thus controlled for urban/rural residence area and US Census region (Northeast, Midwest, South, and West) in our study. Need factors referred to respondents’ clinical need. We used self-reported physical and mental health as proxies for respondents’ health needs.
Sample
We categorized the US young adult population into 2 groups: (1) the ACA expansion of dependents’ coverage target population (adults aged 19–26 years), and (2) the nontarget population (adults aged 27–30 years). To be consistent with previous research, we used those aged 27 to 30 years as the reference group.2,10
Under the ACA, since September 23, 2010, young adults have been able to join or remain in their parents’ private health insurance plans.2 Some large employers claimed that they expanded coverage in early 2010. To precisely examine the trends of health care expenditures and use caused by the ACA expansion, we used 2008 to 2009 and 2011 to 2012 as the pre- and postimplementation periods. Our sample size of young adults aged 19 to 30 years in the 4 survey years was 15 212. After we dropped the observations with missing variables and respondents who reported multiple races, 14 328 observations remained. The total health care expenditures were highly skewed to the right. We dropped the observations with extreme high expenditures (i.e., the outliers). An outlier was defined as an expenditure more than 3 SDs above the average expenditure. Specifically, we dropped 19 observations with total health care expenditures more than $72 355. Our final sample had 14 309 observations in total, including 9327 young adults aged 19 to 26 years and 4982 young adults aged 27 to 30 years.
Analysis
We first summarized health care spending and use for young adults aged 19 to 26 years and aged 27 to 30 years from 2008 to 2009 (before the ACA expansion) and from 2011 to 2012 (after the full implementation of the ACA expansion). We used the difference-in-difference approach to capture the differentiated impact of this natural experiment of the ACA early implementation on different racial/ethnic groups. We used a general linear model with log link and gamma distribution to estimate overall health care expenditures,25,26 multivariate linear regression to estimate OOP as a share of total health care expenditure, and multivariate logistic regression to estimate the likelihood of receiving any health care services. We used stepwise regression models to estimate the impact of the ACA expansion, controlling for different groups of covariates following our conceptual framework. Specifically, in model 1, we controlled for gender, marital status, US-born versus foreign-born, and interview language (i.e., predisposition variables of the Andersen model). In model 2, we controlled for enabling factors, including education, family income, health care access, employment status, urban, and US Census region, in addition to the predisposition factors controlled in model 1. In model 3, we controlled for clinical needs factors, including self-reported physical and mental outcomes, in addition to the predisposition and enabling factors controlled in model 2. Finally, we conducted sensitivity analyses to test the robustness of our results. Our findings were nationally representative using the survey weights provided by the Medical Expenditure Panel Survey. We used Stata version 12 MP (StataCorp, College Station, TX) to conduct the analysis.
RESULTS
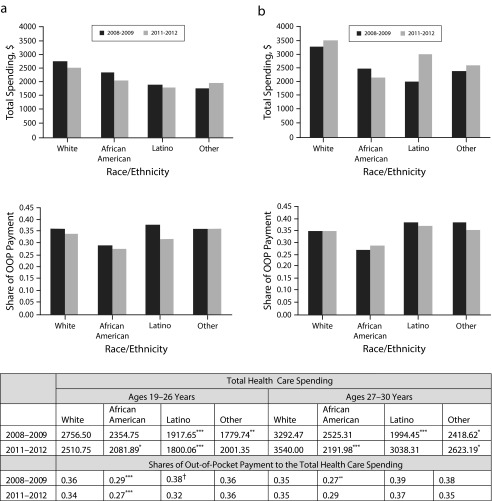
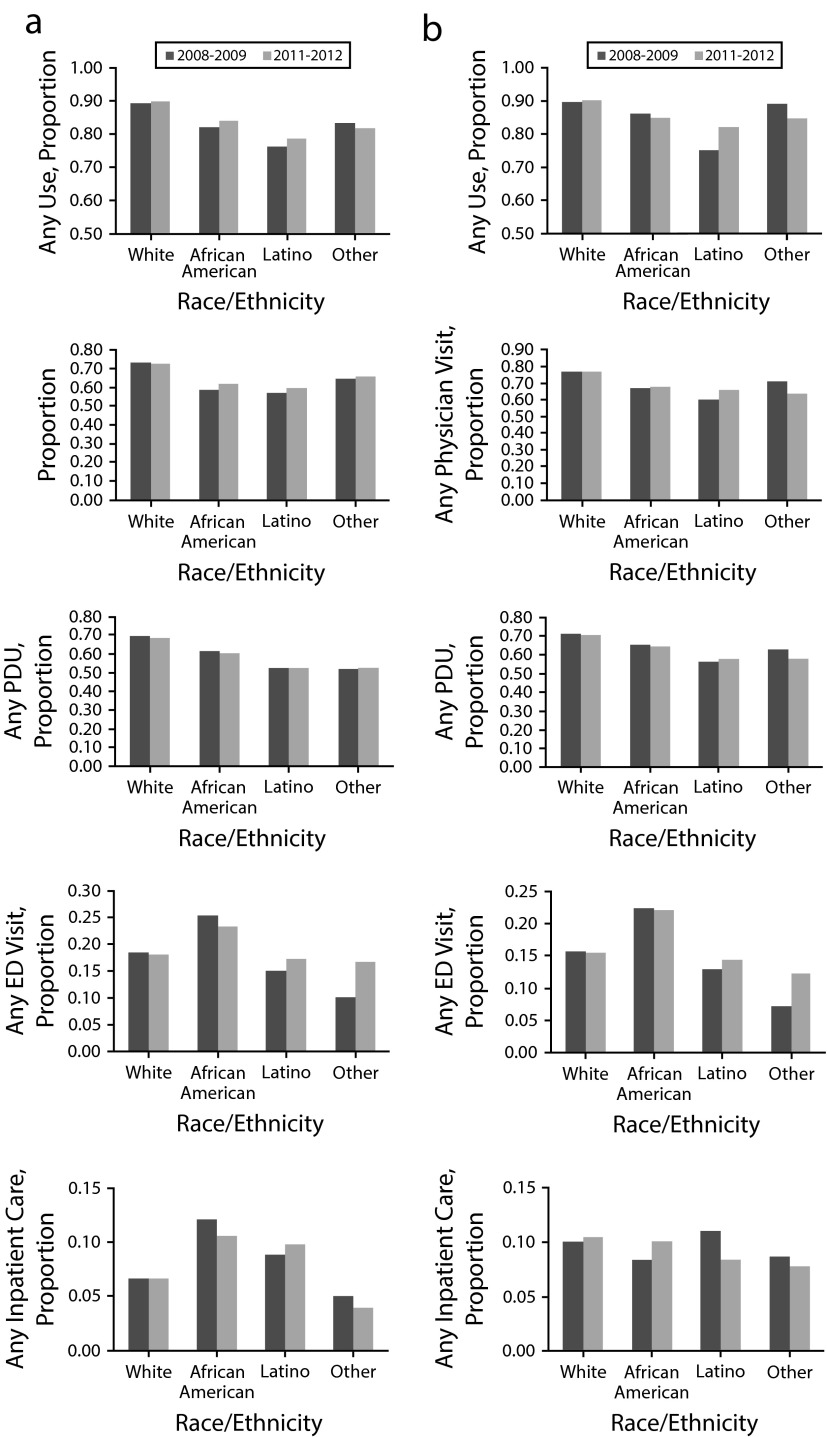
Figure 1 shows that White, African American, and Latino young adults aged 19 to 26 years had reduced total health care spending and OOP as a share of health care spending in 2011 and 2012 compared with 2008 and 2009. The opposite spending trends were observed among adults aged 27 to 30 years, for whom total health care expenditures of Whites and Latinos aged 27 to 30 years were higher in 2011 and 2012, and OOP as a share of health care spending of African Americans aged 27 to 30 years were higher in 2011 and 2012. Figure 2 shows that health care use rates by race/ethnicity were generally similar across all racial/ethnic age cohorts before and after the ACA expansion in 2010.
FIGURE 1—
Total health care spending and out-of-pocket (OOP) payment as shares of OOP payment to the total health care spending among young adults aged (a) 19–26 years and (b) 27–30 years: United States, 2008–2012.
Source. The data source is Medical Expenditure Panel Survey. Statistics are nationally representative (representing approximately 23 million White, 4.2 million African American, 6.2 million Latino, and 2 million other racial/ethnic young adults aged 19–30 years).
*P < .05; **P < .01; ***P < .001; Ref = White in the same survey year.
†P < .01; Ref = according to race/ethnicity age cohort in 2011–2012.
FIGURE 2—
Health care utilization by race/ethnicity among young adults aged (a) 19–26 years and (b) 27–30 years: United States, 2008–2012.
Note. ED = emergency department; PDU = prescription drug use.
Source. The data source is Medical Expenditure Panel Survey. Statistics are nationally representative (representing approximately 23 million White, 4.2 million African American, 6.2 million Latino, and 2 million other racial/ethnic young adults aged 19–30 years).
Table 1 presents sample characteristics by race/ethnicity among young adults before and after the implementation of the ACA expansion of dependents' coverage. Compared with White adults aged 19 to 26 years, African American, Latino, and individuals of other races/ethnicities in the same age cohort were less likely to be US-born, have usual source of care, or be employed. Latinos and other races/ethnicities were more likely to live in the West. Compared with Whites, Africans Americans and Latinos had fewer schooling years and lower family income, whereas other races/ethnicities group had more schooling years and equivalent family income. Similar trends were observed among the comparison age cohort, adults aged 27 to 30 years.
TABLE 1—
Weighted Sample Characteristics of Young Adults Aged 19–26 Years and 27–30 Years by Race/Ethnicity: Health Care Spending and Use Under the Affordable Care Act Expansion, United States, 2011–2012
| White |
African American |
Latino |
Other Races/Ethnicities |
|||||
| Characteristics | 19–26 Years (n = 4007), Mean (95% CI) | 27–30 Years (n = 2318), Mean (95% CI) | 19–26 Years (n = 1943), Mean (95% CI) | 27–30 Years (n = 863), Mean (95% CI) | 19–26 Years (n = 2745), Mean (95% CI) | 27–30 Years (n = 1401), Mean (95% CI) | 19–26 Years (n = 632), Mean (95% CI) | 27–30 Years (n = 400), Mean (95% CI) |
| Predisposition factors | ||||||||
| Female gender | 0.54 (0.52, 0.56) | 0.57 (0.54, 0.59) | 0.58* (0.55, 0.61) | 0.64*** (0.60, 0.68) | 0.55 (0.53, 0.58) | 0.54 (0.50, 0.58) | 0.51 (0.46, 0.57) | 0.61 (0.54, 0.68) |
| Married | 0.12 (0.11, 0.14) | 0.44 (0.41, 0.47) | 0.06***(0.04, 0.07) | 0.22*** (0.19, 0.26) | 0.15 (0.12, 0.18) | 0.40 (0.36, 0.44) | 0.11 (0.08, 0.14) | 0.43 (0.36, 0.50) |
| Residence status | ||||||||
| US-born | 0.97 (0.96, 0.98) | 0.96 (0.95, 0.98) | 0.93*** (0.91, 0.94) | 0.92* (0.89, 0.95) | 0.67*** (0.64, 0.70) | 0.52*** (0.48, 0.56) | 0.55*** (0.47, 0.63) | 0.35*** (0.26, 0.44) |
| Foreign-born and < 10 y US residence | 0.01 (0.01, 0.02) | 0.02 (0.01, 0.04) | 0.04*** (0.03, 0.06) | 0.04 (0.02, 0.06) | 0.19*** (0.16, 0.21) | 0.25*** (0.22, 0.28) | 0.25*** (0.18, 0.32) | 0.42*** (0.34, 0.50) |
| Foreign-born and ≥ 10 y US residence | 0.02 (0.01, 0.02) | 0.01 (0.01, 0.02) | 0.03* (0.02, 0.04) | 0.04** (0.02, 0.06) | 0.14*** (0.12, 0.16) | 0.23*** (0.20, 0.26) | 0.20*** (0.15, 0.26) | 0.23*** (0.15, 0.30) |
| Interviewed in English | 1.00 (0.99, 1.00) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) | 1.00 (0.99, 1.00) | 0.63*** (0.59, 0.67) | 0.63*** (0.59, 0.67) | 0.98*** (0.96, 0.99) | 0.99 (0.97, 1.00) |
| Enabling factors | ||||||||
| Education | ||||||||
| Schooling years < 12 y | 0.47 (0.45, 0.49) | 0.28 (0.25, 0.31) | 0.59*** (0.55, 0.63) | 0.45*** (0.40, 0.50) | 0.64*** (0.61, 0.68) | 0.57*** (0.52, 0.61) | 0.33*** (0.26, 0.41) | 0.15*** (0.09, 0.21) |
| Schooling years 12–16 y | 0.50 (0.48, 0.52) | 0.59 (0.56, 0.62) | 0.40*** (0.36, 0.44) | 0.49*** (0.44, 0.54) | 0.34**** (0.31, 0.38) | 0.36*** (0.32, 0.40) | 0.59** (0.53, 0.66) | 0.61 (0.54, 0.68) |
| Schooling years > 16 y | 0.03 (0.02, 0.04) | 0.13 (0.10, 0.15) | 0.01** (0.01, 0.02) | 0.06*** (0.04, 0.09) | 0.02* (0.01, 0.02) | 0.07*** (0.05, 0.09) | 0.07* (0.04, 0.11) | 0.25*** (0.18, 0.32) |
| Family income | ||||||||
| Family income < 100% FPL | 0.16 (0.14, 0.18) | 0.10 (0.08, 0.11) | 0.32*** (0.28, 0.35) | 0.28*** (0.24, 0.32) | 0.24*** (0.22, 0.27) | 0.19*** (0.16, 0.22) | 0.19 (0.14, 0.23) | 0.10 (0.04, 0.15) |
| Family income 100%−199% FPL | 0.19 (0.17, 0.20) | 0.16 (0.14, 0.18) | 0.25*** (0.22, 0.27) | 0.22*** (0.18, 0.25) | 0.28*** (0.26, 0.30) | 0.29*** (0.26, 0.32) | 0.19 (0.14, 0.24) | 0.14 (0.10, 0.19) |
| Family income ≥ 200% FPL | 0.65 (0.63, 0.67) | 0.74 (0.72, 0.76) | 0.44*** (0.40, 0.47) | 0.50*** (0.45, 0.55) | 0.48*** (0.44, 0.52) | 0.53*** (0.49, 0.57) | 0.62 (0.55, 0.69) | 0.76 (0.70, 0.83) |
| Access | ||||||||
| Have usual source of care | 0.68 (0.66, 0.70) | 0.66 (0.63, 0.69) | 0.60*** (0.57, 0.63) | 0.63 (0.59, 0.67) | 0.53*** (0.51, 0.56) | 0.57*** (0.53, 0.61) | 0.58** (0.51, 0.65) | 0.61 (0.54, 0.69) |
| Uninsured | 0.15 (0.14, 0.17) | 0.16 (0.14, 0.18) | 0.22*** (0.19, 0.24) | 0.22*** (0.19, 0.26) | 0.32*** (0.29, 0.35) | 0.37*** (0.33, 0.41) | 0.21* (0.15, 0.28) | 0.17 (0.11, 0.22) |
| Private health insurance | 0.74 (0.72, 0.77) | 0.76 (0.73, 0.78) | 0.48*** (0.45, 0.52) | 0.52*** (0.45, 0.57) | 0.46*** (0.42, 0.49) | 0.49*** (0.44, 0.53) | 0.69 (0.63, 0.76) | 0.76 (0.68, 0.83) |
| Public health insurance | 0.10 (0.09, 0.12) | 0.08 (0.07, 0.10) | 0.30*** (0.26, 0.33) | 0.25*** (0.21, 0.29) | 0.22*** (0.19, 0.25) | 0.15*** (0.12, 0.17) | 0.09 (0.06, 0.12) | 0.07 (0.03, 0.12) |
| Unemployed | 0.18 (0.16, 0.20) | 0.11 (0.09, 0.12) | 0.27*** (0.24, 0.30) | 0.14 (0.11, 0.18) | 0.24*** (0.21, 0.26) | 0.18*** (0.15, 0.20) | 0.24** (0.20, 0.29) | 0.18* (0.12, 0.24) |
| Urban | 0.82 (0.78, 0.86) | 0.85 (0.81, 0.88) | 0.92*** (0.90, 0.94) | 0.89* (0.86, 0.92) | 0.92*** (0.88, 0.96) | 0.91*** (0.88, 0.95) | 0.93* (0.84, 1.02) | 0.96*** (0.89, 1.02) |
| US Census region | ||||||||
| Northeast | 0.19 (0.16, 0.22) | 0.18 (0.15, 0.21) | 0.14 (0.11, 0.18) | 0.16 (0.12, 0.20) | 0.13** (0.10, 0.16) | 0.15 (0.11, 0.19) | 0.17 (0.11, 0.23) | 0.15 (0.08, 0.21) |
| Midwest | 0.28 (0.25, 0.31) | 0.28 (0.25, 0.32) | 0.21* (0.17, 0.26) | 0.20** (0.15, 0.25) | 0.10*** (0.07, 0.12) | 0.11*** (0.08, 0.13) | 0.17*** (0.11, 0.22) | 0.17*** (0.11, 0.23) |
| South | 0.33 (0.30, 0.37) | 0.32 (0.27, 0.36) | 0.55*** (0.49, 0.60) | 0.55*** (0.49, 0.61) | 0.34*** (0.27, 0.40) | 0.34 (0.28, 0.40) | 0.29 (0.18, 0.39) | 0.29 (0.19, 0.39) |
| West | 0.20 (0.17, 0.23) | 0.22 (0.19, 0.25) | 0.10*** (0.07, 0.12) | 0.09*** (0.05, 0.12) | 0.44 (0.38, 0.49) | 0.40*** (0.35, 0.46) | 0.37*** (0.27, 0.48) | 0.39*** (0.30, 0.49) |
| Need factors | ||||||||
| Self-reported health | ||||||||
| Poor or fair | 0.06 (0.05, 0.08) | 0.07 (0.06, 0.09) | 0.08 (0.06, 0.10) | 0.11** (0.09, 0.13) | 0.10*** (0.08, 0.11) | 0.10* (0.08, 0.11) | 0.08 (0.04, 0.12) | 0.05 (0.03, 0.08) |
| Good | 0.20 (0.18, 0.21) | 0.22 (0.20, 0.24) | 0.24** (0.22, 0.27) | 0.28*** (0.25, 0.31) | 0.27*** (0.25, 0.29) | 0.29*** (0.25, 0.32) | 0.22 (0.18, 0.27) | 0.26 (0.19, 0.33) |
| Very good or excellent | 0.74 (0.72, 0.76) | 0.71 (0.68, 0.73) | 0.68*** (0.65, 0.70) | 0.61*** (0.58, 0.65) | 0.63*** (0.60, 0.66) | 0.62* (0.57, 0.66) | 0.70 (0.64, 0.75) | 0.68 (0.60, 0.76) |
| Self-reported mental health | ||||||||
| Poor or fair | 0.05 (0.04, 0.06) | 0.05 (0.04, 0.06) | 0.05 (0.04, 0.07) | 0.06 (0.04, 0.08) | 0.06 (0.04, 0.07) | 0.05 (0.04, 0.07) | 0.04 (0.02, 0.07) | 0.03** (0.01, 0.04) |
| Good | 0.17 (0.16, 0.19) | 0.19 (0.17, 0.20) | 0.18 (0.16, 0.20) | 0.20 (0.17, 0.24) | 0.21** (0.19, 0.23) | 0.22 (0.19, 0.25) | 0.20 (0.15, 0.25) | 0.15 (0.09, 0.20) |
| Very good or excellent | 0.77 (0.75, 0.79) | 0.76 (0.75, 0.78) | 0.77 (0.75, 0.79) | 0.74 (0.70, 0.77) | 0.74** (0.71, 0.76) | 0.73 (0.69, 0.76) | 0.75 (0.70, 0.81) | 0.82 (0.77, 0.88) |
Note. CI = confidence interval; FPL = federal poverty level. Sample characteristics are weighted by the survey sampling weights provided by the Medical Expenditure Panel Survey.
*P < .05; **P < .01; ***P < .001; Ref = according White age cohort in 2011–2012.
Table 2 shows the results of the difference-in-difference estimation, controlling for respondents’ predisposition, clinical needs, and enabling factors. Results showed significant variation in race/ethnicity age groups in total health care expenditures in model 1. After controlling for enabling factors (model 2), our results showed significant variation of the interaction terms between race/ethnicity age groups and the year indicator. Model 3 was our full model. Compared with White young adults aged 27 to 30 years, African American (coefficient = −0.33; P < .05), Latino young adults (coefficient = −0.45; P < .001), and other races/ethnicities (coefficient = −0.42; P < .01) in the same age group had significantly lower total health spending. Younger cohorts of other races/ethnicities (coefficient = −0.58; P < .001) had lower total health spending compared with Whites aged 27 to 30 years. The interaction terms of race/ethnicity age group and year indicator showed that White (coefficient = −0.25; P < .05) and African American (coefficient = −0.33; P < .05) adults aged 19 to 26 years had significantly lower total health care expenditures in 2011 and 2012 compared with White young adults aged 27 to 30 years in 2011 and 2012.
TABLE 2—
Results of Difference-in-Difference Estimation of Healthcare Expenditures and Utilization: Health Care Spending and Use Under the Affordable Care Act Expansion, United States, 2011–2012
| Total Health Care Spending |
Share of Out-of-Pocket Payment |
Any Use |
|||||||
| Model 1, Coef (95% CI) | Model 2, Coef (95% CI) | Model 3, Coef (95% CI) | Model 1, Coef (95% CI) | Model 2, Coef (95% CI) | Model 3, Coef (95% CI) | Model 1, OR (95% CI) | Model 2, OR (95% CI) | Model 3, OR (95% CI) | |
| Year 2008–2009 (before the ACA expansion; Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Year 2011–2012 (after the ACA expansion) | 0.09 (–0.09, 0.28) | 0.14 (–0.05, 0.33) | 0.14 (–0.04, 0.33) | 0.00 (–0.03, 0.03) | 0.00 (–0.03, 0.03) | 0.00 (–0.03, 0.03) | 1.10 (0.81, 1.51) | 1.09 (0.78, 1.53) | 1.09 (0.77, 1.53) |
| White, aged 27–30 y (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| African American, aged 27–30 y | −0.18 (–0.54, 0.18) | −0.37** (–0.65, –0.10) | −0.33* (–0.62, –0.04) | −0.08** (–0.13, –0.03) | −0.06** (–0.1, –0.02) | −0.06** (–0.10, –0.02) | 0.71 (0.47, 1.10) | 0.84 (0.51, 1.38) | 0.83 (0.51, 1.37) |
| Latino, aged 27–30 y | −0.41** (–0.67, −0.15) | −0.44*** (–0.71, –0.18) | −0.45*** (–0.70, –0.19) | 0.01 (–0.04, 0.05) | 0.00 (–0.04, 0.04) | 0.00 (–0.04, 0.04) | 0.51*** (0.36, 0.73) | 0.63* (0.43, 0.92) | 0.63 (0.43, 0.91) |
| Other races/ethnicities, aged 27–30 y | −0.31 (–0.66, 0.05) | −0.45* (–0.79, –0.12) | −0.42** (–0.75, –0.08) | 0.01 (–0.08, 0.10) | 0.01 (–0.07, 0.09) | 0.01 (–0.07, 0.09) | 1.04 (0.58, 1.88) | 0.82 (0.44, 1.53) | 0.81 (0.43, 1.51) |
| White, aged 19–26 y | 0.00 (–0.19, 0.19) | −0.03 (–0.19, 0.14) | 0.00 (–0.16, 0.16) | 0.00 (–0.03, 0.03) | 0.01 (–0.02, 0.04) | 0.01 (–0.02, 0.04) | 1.20 (0.86, 1.68) | 1.17 (0.83, 1.65) | 1.20 (0.85, 1.69) |
| African American, aged 19–26 y | −0.17 (0.42, 0.09) | −0.25* (–0.48, –0.02) | −0.18 (–0.41, 0.04) | −0.08*** (–0.12, –0.03) | −0.05 (–0.08, –0.01) | −0.05** (–0.09, –0.01) | 0.62** (0.43, 0.87) | 0.68* (0.47, 1.00) | 0.70 (0.48, 1.03) |
| Latino, aged 19–26 y | −0.23 (–0.49, 0.03) | −0.20 (–0.50, 0.11) | −0.17 (–0.46, 0.13) | −0.01 (–0.05, 0.03) | −0.00 (–0.04, 0.04) | −0.00 (–0.04, 0.04) | 0.61** (0.44, 0.84) | 0.75 (0.53, 1.06) | 0.75 (0.53, 1.06) |
| Other races/ethnicities, aged 19–26 y | −0.46* (–0.83, –0.10) | −0.50* (–0.92, –0.09) | −0.58*** (–0.93, –0.24) | −0.02 (–0.08, 0.04) | −0.01 (–0.07, 0.06) | −0.01 (–0.07, 0.06) | 0.82 (0.49, 1.37) | 0.82 (0.5, 1.34) | 0.81 (0.50, 1.32) |
| Interaction terms | |||||||||
| White, aged 19–26 y × year 2011–2012 | −0.19 (–0.45, 0.08) | −0.27* (–0.51, –0.02) | −0.25* (–0.49, –0.01) | −0.02 (–0.07, 0.02) | −0.01 (–0.05, 0.02) | −0.01 (–0.05, 0.02) | 0.93 (0.62, 1.41) | 0.88 (0.57, 1.36) | 0.88 (0.57, 1.36) |
| African American, aged 19–26 y × year 2011–2012 | −0.25 (–0.57, 0.08) | −0.35* (–0.65, –0.05) | −0.33* (–0.63, –0.03) | −0.02 (–0.07, 0.04) | −0.01 (–0.05, 0.04) | −0.01 (–0.05, 0.04) | 1.06 (0.66, 1.70) | 1.02 (0.61, 1.71) | 1.02 (0.61, 1.71) |
| Latino, aged 19–26 y × year 2011–2012 | −0.23 (–0.6, 0.14) | −0.33 (–0.75, 0.10) | −0.33 (–0.74, 0.09) | −0.05* (–0.11, 0.00) | −0.04 (–0.09, 0.01) | −0.04 (–0.09, 0.01) | 0.96 (0.64, 1.44) | 0.86 (0.56, 1.30) | 0.87 (0.57, 1.32) |
| Other races/ethnicities, aged 19–26 y × year 2011–2012 | 0.07 (–0.41, 0.56) | 0.21 (–0.45, 0.88) | 0.36 (–0.28, 1.00) | 0.00 (–0.08, 0.08) | 0.00 (–0.07, 0.07) | 0.00 (–0.07, 0.07) | 0.80 (0.41, 1.56) | 0.70 (0.37, 1.35) | 0.73 (0.38, 1.41) |
| African American, aged 27–30 y × year 2011–2012 | −0.25 (–0.68, 0.19) | −0.14 (–0.53, 0.24) | −0.17 (–0.57, 0.24) | 0.01 (–0.05, 0.07) | −0.01 (–0.06, 0.05) | −0.01 (–0.06, 0.05) | 0.88 (0.51, 1.52) | 0.84 (0.45, 1.58) | 0.83 (0.44, 1.55) |
| Latino, aged 27–30 y × year 2011–2012 | 0.40 (–0.03, 0.84) | 0.37 (–0.03, 0.77) | 0.36 (–0.02, 0.75) | −0.01 (–0.08, 0.05) | 0.00 (–0.06, 0.05) | 0.00 (–0.06, 0.05) | 1.38 (0.84, 2.25) | 1.32 (0.78, 2.22) | 1.33 (0.79, 2.24) |
| Other races/ethnicities, aged 27–30 y × year 2011–2012 | 0.10 (–0.31, 0.50) | 0.12 (–0.30, 0.54) | 0.14 (–0.29, 0.58) | −0.03 (–0.13, 0.07) | −0.02 (–0.09, 0.08) | −0.02 (–0.09, 0.08) | 0.64 (0.32, 1.27) | 0.69 (0.33, 1.46) | 0.70 (0.33, 1.50) |
Note. ACA = Affordable Care Act; CI = confidence interval; Coef = coefficient; OR = odds ratio. We used the conceptual framework of Andersen social behavioral model to select the covariates that were associated with health care expenditures. Model 1 = covariates included predisposition factors (i.e., race/ethnicity, gender, marital status, US-born, and interview language); model 2 = model 1 + enabling factors (i.e., education, family income, health care access, urban/rural, and US Census region); model 3 = model 2 + clinical need factors (i.e., self-reported physical and mental health). Full sets of results are omitted for brevity but are available upon request. Multivariate logistic regressions were estimated for any use of physician visit, prescription drug, emergency department visit, and hospital inpatient use. The coefficients of interaction terms of race/ethnicity or age with year indicator were not significant. Results of these regressions are omitted for brevity but are available upon request. All the estimates are nationally representative.
*P < .05; **P < .01; ***P < .001.
Table 2 also presents the estimation results of OOP as a share of total health care expenditures. Compared with White adults aged 27 to 30 years, African Americans had significantly lower OOP shares. OOP shares were similar among Latinos, other races/ethnicities, and Whites. The interaction term of the Latino aged 19 to 26 years group with the year indicator was significantly negative (coefficient = −0.05; P < .05) in model 1. The interaction terms of race/ethnicity age group and the 2011 and 2012 year indicator were not significant for all race/ethnicity groups in model 3.
Our results did not show significant differences in the probability of having any type of health care services among young adults aged 19 to 26 years in 2011 and 2012 compared with those aged 27 to 30 years for any race/ethnicity group. We estimated multivariate logistic regressions for any use of physician visit, prescription drug, emergency department visit, and hospital inpatient use. The coefficients of interaction terms of race/ethnicity or age with year indicator were not significant. We omitted the results of these regressions for brevity, but they are available upon request.
We conducted several sensitivity tests on refinement of treatment groups, model specifications, and robustness. Specifically, in the sensitivity analyses, we also compared other age groups, such as 19 to 25 years versus 26 to 30 years. We excluded individuals who were 26 years old because of a lack of accurate information to determine their eligibility when the ACA was implemented in 2010.2 We also excluded full-time students aged 19 to 23 years from the targeted group because they were already eligible to enroll in their parents’ health insurance before the ACA implementation. Our findings were similar using this refined treatment group. We also used different ways to define outliers, tested different model specifications (e.g., we added comprehensive health need factors, including diabetes, asthma, heart diseases, depressive and anxiety disorders, used 2-part model, etc.), and estimated the model adjusting for the robustness of SEs using the clustered survey design.27 Our results were similar as those presented in Table 2.
DISCUSSION
Racial/ethnic health disparities have been well defined.28 Health care access and insurance coverage were the 2 major factors associated with these disparities.19,23,24,28 The ACA early implementation expansion of dependent’s coverage provided the first evidence of racial/ethnic disparities in health care expenditures under the emerging ACA provisions.
Our study showed that the impact of the ACA expansion on health care expenditures differed by race/ethnicity. Specifically, our findings pointed out a significant reduction of health expenditures among White and African American young adults in the 19 to 26 years cohort. These population groups significantly reduced total health care expenditures in 2011 and 2012 compared with the corresponding comparison category of aged 27 to 30 years. Lack of health insurance coverage was more prevalent among African American young adults compared with Whites before the ACA implementation in 2010.29
OOP as a share of total health care expenditures remained the same under the expansion of dependents’ coverage. Because the total health care expenditures declined for White and African American young adults aged 19 to 26 years, lower OOP shares might translate to lower OOP. By combining our findings of the similar health care use pattern after the ACA implementation, lower OOP could reflect the lower price of health care. These findings suggested that White and African American young adults benefited from the ACA expansion, because they had better insurance coverage and paid less OOP.
The reduction of total health care spending among Latino young adults aged 19 to 26 years, after the ACA expansion was not statistically significant. OOP as a share of health care expenditures fell among the Latino young cohort aged 19 to 26 years from 38% to 32%, but this reduction was no longer statistically significant after controlling for respondents’ demographic and socioeconomic characteristics, and health status. Health spending among Latinos was found to be consistently lower compared with Whites and African Americans.19,24,30 The ACA expansion was designed to expand the health insurance coverage and improve health care access. However, our results showed that Latino young adults have not benefited from the ACA expansion of dependents’ coverage. We speculated that the employment and immigration status of their parents might be the major reasons associated with the stable health care expenditures.
Compared with Whites, Latinos were less likely to have employer-provided private coverage because of income and immigration status.31 Latinos, for instance, were more likely to have jobs, such as part-time or seasonal work, with no insurance provided by employers.32 Detailed information on health insurance would be needed to examine whether the relatively insignificant reduction in total health care expenditures and OOP shares among young adult Latinos and other races/ethnicities were because of the restricted coverage or the higher cost sharing of their health insurance plans.
Another possible explanation of this difference could be related to the “healthy immigrant” effect,33,34 as immigrants, on average, have better health outcomes compared with the US-born population. Our data showed that Latinos and individuals of other race/ethnic groups were 30% to 50% more likely to be foreign-born. Better health outcomes among these immigrant populations might explain why a higher share of Latino young adults and individuals of other race/ethnicity did not benefit from their parents’ private health insurance even when coverage was available.
Future research to explore the ACA impact on health care of individuals of other race/ethnicity group is needed. Compared with African American and Latino young adults, young adults of other races/ethnicities had higher socioeconomic status compared with Whites. Rates of being foreign-born were the highest among other race/ethnicity groups. Previous research showed that immigration status and limited English proficiency, rather than health insurance, were major barriers for Chinese to access health care.23 Because of the data limitations, we were not able to further identify the heterogeneities among other race/ethnicity groups. Our study, however, suggested that future research should examine the specific groups under the other race/ethnicity category separately. It was likely that policies targeted at improving insurance might not work effectively for all the other race/ethnicity groups.
It was worth noting that the ACA expansion of dependents’ coverage is mainly targeted at families with employer-sponsored insurance. Individuals who remained uninsured were more likely to be young adults with parents who lacked employer-provided health insurance coverage, who were ineligible for public health insurance, and those who selected to remain uninsured because of the high cost of premiums. This remaining cohort was more likely to have discretionary spending decisions in favor of other social priorities (e.g., food, student debt) rather than paying for large premiums and deductibles. Further exploration of our data showed that respondents who were Latino, did not speak English, and who lived in the South were more likely to be uninsured in 2011 and 2012 compared with 2008 and 2009 (results not shown, but available upon request). Further research should characterize the remaining uninsured young invincible pool and the main reasons for remaining uninsured.
Limitations
Our study had some limitations. First, the other race/ethnicity group was highly heterogeneous. Studies that used alternative data sources should investigate how the ACA expansion would affect the benefit of Asian Americans, Native/Indian Americans, and other racial/ethnic groups separately. Second, we chose a threshold of 26 years old because we lacked information of respondents' date of birth and we were unable to precisely determine whether individuals were 25 or 26 years old. Third, we controlled for a number of covariates that were associated with health care expenditures and use. However, it was likely that some important factors might have been excluded because of data limitations. Market aggregated impact, such as the economic recession from 2007 to 2009,21 might have influenced the patterns of health care expenditures and use. Policy variation might exist regionally. Although we controlled for Census region, future research should examine policy variation by state. In addition, our data only provided information on respondents’ US-born and foreign-born status. Specific information on respondents’ US citizenship and immigrant authorization status would be needed to examine health care expenditure patterns of Latinos and those of other races/ethnicities who were eligible for the expansion. Although the difference-in-difference estimation we used in our study could be helpful to identify the treatment effect of the ACA expansion, longitudinal data would be needed to study the causality of the ACA coverage expansion on health care spending. Future research on racial/ethnic disparities in health expenditure and utilization is essential when data are available.
Conclusions
Our study showed that the impact of the ACA expansion on health care expenditures differed by race/ethnicity. White and African American young adults aged 19 to 26 years had more pronounced reductions in health care spending after the implementation of this ACA provision came into effect, whereas Latino and other racial/ethnic young adults’ health spending did not decline significantly. The overall health care reform extends health insurance coverage to the majority of all uninsured individuals, not just those with employer-sponsored health insurance. Hence, we expect to see that minorities will receive more health benefits and greater consistency of care, and observe significant reduction in racial/ethnic disparities in health care.
Human Participant Protection
This study was exempt from review because it involved the collection and study of existing, publicly available data in which individuals could not be identified directly or through identifiers linked to the individuals.
References
- 1.Smith S. CDC: “Young invincibles” have significant health concerns. CNN. 2009. Available at: http://www.cnn.com/2009/HEALTH/02/17/cdc.young.people. Accessed September 1, 2014.
- 2.Centers for Medicare & Medicaid Services. Young Adults and the Affordable Care Act: Protecting Young Adults and Eliminating Burdens on Families and Businesses. Washington, DC: Department of Health and Human Services; 2010. [Google Scholar]
- 3. Kaiser Commission on Medicaid and the Uninsured. The uninsured: an interactive tool. 2014. Available at: http://kff.org/interactive/the-uninsured-an-interactive-tool. Accessed September 1, 2014.
- 4.Cantor JC, Monheit AC, DeLia D, Lloyd K. Early impact of the Affordable Care Act on health insurance coverage of young adults. Health Serv Res. 2012;47:1773–1790. doi: 10.1111/j.1475-6773.2012.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sommers BD, Buchmueller T, Decker SL et al. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Aff (Millwood) 2013;32(1):165–174. doi: 10.1377/hlthaff.2012.0552. [DOI] [PubMed] [Google Scholar]
- 6.The Kaiser Family Foundation. Employer health benefits: 2013 annual survey. 2013. Available at: http://ehbs.kff.org/pdf/2011/8225.pdf. Accessed September 1, 2014.
- 7.Mulcahy A, Harris K, Finegold K et al. Insurance coverage of emergency care for young adults under health reform. N Engl J Med. 2013;368(22):2105–2112. doi: 10.1056/NEJMsa1212779. [DOI] [PubMed] [Google Scholar]
- 8.Cantor JC, Belloff D, Monheit AC et al. Expanding dependent coverage for young adults: lessons from state initiatives. J Health Polit Policy Law. 2012;37(1):99–128. doi: 10.1215/03616878-1496056. [DOI] [PubMed] [Google Scholar]
- 9.Chua KP, Sommers BD. Changes in health and medical spending among young adults under health reform. JAMA. 2014;311(23):2437–2439. doi: 10.1001/jama.2014.2202. [DOI] [PubMed] [Google Scholar]
- 10.Busch SH, Golberstein E, Meara E. ACA dependent coverage provision reduced high out-of-pocket health care spending for young adults. Health Aff (Millwood) 2014;33(8):1361–1366. doi: 10.1377/hlthaff.2014.0155. [DOI] [PubMed] [Google Scholar]
- 11.Merluzzi TV, Nairn RC. Adulthood and aging: transitions in health and health cognition. In: Whitman TL, Merluzzi TV, White RD, editors. Life-Span Perspective on Health and Illness. Mahwah, NJ: Erlbaum; 1999. pp. 189–206. [Google Scholar]
- 12.Callahan ST, Cooper WO. Uninsurance and health care access among young adults in the United States. Pediatrics. 2005;116(1):88–95. doi: 10.1542/peds.2004-1449. [DOI] [PubMed] [Google Scholar]
- 13.Bloom B, Cohen RA. Young adults seeking medical care: do race and ethnicity matter? NCHS Data Brief. 2011;55:1–8. [PubMed] [Google Scholar]
- 14.Hadley J. Sicker and poorer–the consequences of being uninsured: a review of the research on the relationship between health insurance, medical care use, health, work, and income. Med Care Res Rev. 2003;60(2 suppl):3S–75S. doi: 10.1177/1077558703254101. discussion 76S–112S. [DOI] [PubMed] [Google Scholar]
- 15.Zuvekas SH, Taliaferro GS. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996–1999. Health Aff (Millwood) 2003;22(2):139–153. doi: 10.1377/hlthaff.22.2.139. [DOI] [PubMed] [Google Scholar]
- 16.Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res. 2003;38(3):809–829. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monheit AC, Vistnes JP. Race/ethnicity and health insurance status: 1987 and 1996. Med Care Res Rev. 2000;57(suppl 1):11–35. doi: 10.1177/1077558700057001S02. [DOI] [PubMed] [Google Scholar]
- 18.Cohen JW, Cohen SB, Banthin JS. The Medical Expenditure Panel Survey: a national information resource to support health care cost research and inform policy and practice. Med Care. 2009;47(7 suppl 1):S44–S50. doi: 10.1097/MLR.0b013e3181a23e3a. [DOI] [PubMed] [Google Scholar]
- 19.Cook BL, Manning WG. Measuring racial/ethnic disparities across the distribution of health care expenditures. Health Serv Res. 2009;44(5 pt 1):1603–1621. doi: 10.1111/j.1475-6773.2009.01004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ku L. Health insurance coverage and medical expenditures of immigrants and native-born citizens in the United States. Am J Public Health. 2009;99(7):1322–1328. doi: 10.2105/AJPH.2008.144733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen J, Bustamante AV, Mortensen K, Thomas S. Using quantile regression to examine health care expenditures during the Great Recession. Health Serv Res. 2014;49(2):705–730. doi: 10.1111/1475-6773.12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 23.Chen J, Bustamante AV, Ortega AN. Healthcare expenditures among Asian American subgroups. Med Care Res Rev. 2013;70(3):310–329. doi: 10.1177/1077558712465773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bustamante AV, Chen J. Health expenditure dynamics and years of US residence: analyzing spending disparities among Latinos by citizenship/nativity status. Health Serv Res. 2012;47(2):794–818. doi: 10.1111/j.1475-6773.2011.01278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465–488. doi: 10.1016/j.jhealeco.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 26.Wooldridge J. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2002. [Google Scholar]
- 27.Bertrand M, Duflo E, Mullainathan S. How much should we trust differences-in-differences estimates? Q J Econ. 2004;119(1):249–275. [Google Scholar]
- 28.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 29. Kaiser State Health Facts. Employer-Sponsored Coverage Rates for the Nonelderly by Race/Ethnicity 2011-2012. Available at: http://kff.org/other/state-indicator/rate-by-raceethnicity-2. Accessed September 1, 2014.
- 30.Lê Cook B, McGuire TG, Zuvekas SH. Measuring trends in racial/ethnic health care disparities. Med Care Res Rev. 2009;66(1):23–48. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Census US. The Hispanic Population: 2010. 2010 Census Brief. Washington, DC: US Department of Commerce; 2013. [Google Scholar]
- 32.US Census Bureau. 2010 American Community Survey. 2012. Available at: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_10_1YR_S0201&prodType=table. Accessed September 1, 2014.
- 33.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiological paradox. Public Health Rep. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- 34.McDonald JT, Kennedy S. Insights into the “healthy immigrant effect”: health status and health service use of immigrants to Canada. Soc Sci Med. 2004;59(8):1613–1627. doi: 10.1016/j.socscimed.2004.02.004. [DOI] [PubMed] [Google Scholar]