Abstract
We propose a transdisciplinary, life span framework for examining the underlying cause of the observed intergenerational decline in health among Hispanic Americans. We focus on acculturation, and we posit that acculturation-related processes in first-generation Hispanic immigrant mothers may affect the intrauterine development of an unborn child, via the process of fetal programming, to produce phenotypic effects that may alter the susceptibility for noncommunicable chronic diseases. In this manner, an intergenerational cascade of perpetuation may become established. Our framework may shed light on the biological, behavioral, and social causes of intergenerational cycles of vulnerability among immigrant minority groups, with public health and policy implications for primary prevention and intervention.
The public health significance of addressing the issue of health and health disparities in Hispanics, the largest ethnic minority in the United States1 and an especially disenfranchised segment of American society,2 is well established. The fact that the majority of Hispanic Americans are immigrants or the children of immigrants,3 coupled with the robust epidemiologic observation that Hispanic immigrants in the United States exhibit a progressive decline in health over time4–11 and across generations,5,12–20 has justified a particular focus on how postimmigration conditions affect health in this population. The negative consequences of acculturation have commonly been invoked to explain this phenomenon, and several studies in Hispanic Americans have established associations between measures of acculturation and adverse health outcomes.21–24 The prevailing paradigm posits the deleterious effect of acculturation on health is a consequence of the biological embedding of its psychological and behavioral sequelae, such as excess psychological stress,25–27 declining social ties,28,29 and adoption of unhealthy diets and other behaviors.30–36 This paradigm, as currently formulated, may account for the observed decline in first-generation immigrant health associated with length of residence in the United States. However, a major shortcoming is that it does not adequately explain the intergenerational aspect of the observed health decline. We sought to address this important limitation.
In this article, we articulate a novel framework that is grounded in principles from evolutionary and developmental biology, and we integrate the concepts of biological embedding of life experiences and fetal origins of health and disease risk. We propose that the origins of the observed intergenerational health decline among Hispanic Americans might be traced back to as early as the intrauterine period of life, at which time the effects of acculturation could be transmitted from a mother to her as-yet-unborn child via the process of fetal programming. This process might produce phenotypic alterations in the structure and function of cells, tissues, and organ systems that increase the offspring’s susceptibility for developing many of the health disorders that are disproportionately prevalent among Hispanic Americans. In this manner, an intergenerational cascade of perpetuation of the deleterious consequences of acculturation on health might become established. Our framework also addresses the proximate causal pathway by highlighting the tripartite role of maternal–placental–fetal endocrine, immune, and oxidative-state–related biological processes, such as sensors, transducers, and effectors of acculturation-related states and conditions on the developing fetus. The plausibility of our formulation was supported by empirical evidence in the general population that the same psychological and behavioral processes associated with acculturation (e.g., stress, diet) are also known to affect biological processes implicated in fetal programming.37 Moreover, studies in pregnant Hispanic women demonstrate that maternal acculturation is associated with the same psychological, behavioral, and biological processes during gestation that are implicated in the process of fetal programming.30,33,38–41 In this way, we suggest that the fetal programming perspective potentially offers a parsimonious explanation for the observed intergenerational decline in Hispanic American health, and also reconciles the apparent contradiction between the observations in this population that disease risk increases across generations despite improvements in life conditions.
SIGNIFICANCE OF HISPANIC AMERICAN HEALTH
The importance of addressing the issue of health and health disparities in minority and underserved populations is well recognized42,43 (Healthy People 202044; NIH Health Disparities Strategic Plan 2009–201345), and the need for investigating the social determinants of health disparities is well established.46–50 In this context, a particular focus on the Hispanic population in the United States is warranted. Hispanic Americans exhibit disproportionately high rates of many of the noncommunicable chronic disorders (NCDs) that confer the major national burden of disease, including obesity,51 diabetes,52 the metabolic syndrome,53 certain cancers,54 and dementia.55
Hispanics currently represent the largest minority group in the United States, and it is projected that by 2030, Hispanics will constitute one third of the United States population.1 Moreover, Hispanics are the most rapidly growing population in the United States,56 and the only ethnic group projected to maintain population growth above replacement level.57 The majority (70%) of Hispanics in the United States are immigrants or the children of immigrants.3 Hispanics exhibit the highest immigration rate to the United States of any ethnic group,58 making up 36% of all immigrants in the United States.58 Mexican Americans account for the majority (65%) of Hispanic Americans.56 Hispanics represent a disadvantaged segment of American society. According to the Census Bureau’s Supplemental Poverty Measure, Hispanics have the highest poverty rate (28.2%) of any ethnic group in the United States.59 Mexican immigrants are exceptionally disenfranchised, with the highest poverty rate (29%) of any immigrant group in the United States.60,61
EPIDEMIOLOGICAL TRENDS IN HISPANIC AMERICAN HEALTH OUTCOMES
Two major epidemiological trends have consistently been described in terms of health outcomes in the Hispanic American population: a health paradox, and an acculturation paradox. The Hispanic health paradox62 refers to the observation that despite lower socioeconomic status (SES) and less access to health care, Hispanic Americans appear to exhibit mortality rates63–67 and health outcomes68,69 that are similar to non-Hispanic White Americans, and are more favorable than those of other disadvantaged minorities, such as African Americans (although not all studies have demonstrated this effect70–73). This pattern does not appear to merely reflect data artifacts,74–78 although healthy migrant (selective migration) and salmon biases (selective return migration because of poor health) may contribute.77,79
A more nuanced trend is revealed upon closer inspection: the acculturation paradox. After immigrating and while acculturating to the mainstream US lifestyle, Hispanics appear to exhibit a progressive decline in health, in many instances despite concurrent improvement in SES and greater access to health care.8,17,18,69,80–91 First-generation (immigrant) Hispanics exhibit better physical5,12,13 and mental14–20 health outcomes, and lower mortality rates67 than second-generation (US-born) Hispanics. Also, among first-generation Hispanics, longer residence in the United States has been associated with diminished mental4 and physical health5–11 and higher mortality rates.67
The Construct of Acculturation
Of the myriad factors that influence health, the effects of postmigration sociocultural conditions in the Hispanic population may warrant particular consideration because, as discussed previously, the majority of Hispanics in the United States are immigrants or the children of immigrants.3 The rapid rate of Hispanic immigration is a major contributor to the growth of this population.58,92 Migration necessitates adjustment to life in the adoptive-host country, which may be substantially different from life in the origin country. This adjustment may involve changes in identity, values, beliefs, and behaviors. The term “acculturation” is commonly used to describe this process of postmigration adjustment, which involves the acquisition of the host-country cultural orientation, the loss of origin-country cultural orientation, or both.93–95 Some of the major aspects of cultural change measured in acculturation instruments are related to language, self-identification, attitudes, knowledge of customs and history, contact with media, and social interactions.96,97
The construct of acculturation was born more than 100 years ago in anthropology,94 subsequently adopted by psychology,95,98–100 and more recently, it has become a concept of interest in the biomedical community.101,102 Along the way, a variety of changes have been proposed and made to its conceptualization and operationalization. Acculturation was initially conceptualized to be a unidimensional process, with adoption of host country culture necessarily characterized by loss of heritage country culture.103–106 Thereafter, acculturation was considered a multidimensional process with cultural change occurring independently in various domains,105,107,108 or as a bidimensional process93,109 in which acquisition of the host culture and retention of the heritage culture represent independent, orthogonal processes.105,109–111 The conceptualization and operationalization of the construct has been critiqued for various reasons.112–114 For example, sociocultural changes occur at varying rates and time points, in multiple directions, with variation in the order and nature of these life changes,115 which is not sufficiently captured in many of the existing instruments. One ideology with respect to intercultural relations, often adopted in the United States, is guided by an assumption of assimilation, in which the terms acculturation and assimilation are equated and used synonymously. However, this may not represent an accurate depiction because acculturation can take many different paths.100,116 For example, certain acculturation strategies are more often associated than other strategies with health mediators (e.g., psychological distress). With regard to the widely used 4-category model of acculturation profiles by Berry,100,117 research has demonstrated that individuals who abandon heritage cultural identity alongside acquisition of host cultural identity (“assimilation”), or who retain heritage cultural identity and do not acquire host cultural identity (“separation”), may be at greater risk for poor mental health than those who exhibit a bicultural orientation (“integration”).108,109,118–121 However, biculturalism has also been associated with higher levels of stress attributed to one’s role as cultural translator in the family,32,122 and has been associated with poor health in some studies.111,123 Lastly, the effects of acculturation on health may be context-dependent and vary as a function of the underlying reason(s) for migration, relative changes between heritage and host cultures, the ethnic composition of the neighborhood of residence, and sociological features of the host country.112,116,124,125 It is important to note that many studies of the relationship between acculturation and health do not adequately address these issues. Moreover, for lack of access or ease of operationalization, several studies have relied on acculturation proxy variables, such as nativity, length of stay in the United States, and language preference or use instead of assessing acculturation directly.22,126–128
Evidence of the Acculturation Paradox
The Hispanic acculturation paradox refers to the observed decline in mental and physical health that is concurrent with duration of residence in the United States,5–11 and also occurs across generations in the United States.5,12–20 For example, higher degrees of acculturation (typically defined as greater adoption of Anglo cultural identity) and later generation status have been associated with overall more mental health problems,14–16 including higher rates of psychopathology,17,18 anxiety,129–131 depression,19,131,132 and fewer positive self-feelings.133 Degree of acculturation has been associated in many studies with decline in physical health for a range of chronic conditions,5,67,74 including poor overall physical health,74 hypertension,88 cardiovascular disease,13 and diabetes.12,134 It should be noted that some studies have failed to demonstrate a relationship between acculturation and health,36,85,135–146 and that a few studies have reported health advantages.80,84,86,147
The acculturation paradox is particularly apparent when considering birth outcomes and obesity. For example, a greater degree of acculturation33,82,148 and later generation status82,90,149–155 have been associated with adverse birth outcomes, including low birth weight and premature birth, as well as lower infant survival89,156–158 (see Lara et al.159 for review). Among Hispanic immigrants, English language preference160 and length of United States residence6,67,161–166 have been positively associated with body mass index and the likelihood of being overweight or obese. Generation status has also been positively associated with body mass index and obesity, such that second-generation Hispanics have higher rates of obesity than first-generation Hispanic immigrants.67,160,162,167–169 These trends have been observed among Hispanics across the entire age spectrum, including children and adolescents161,170 (see Yeh et al.171 for review).
Existing Paradigm Proposed to Explain the Acculturation Paradox
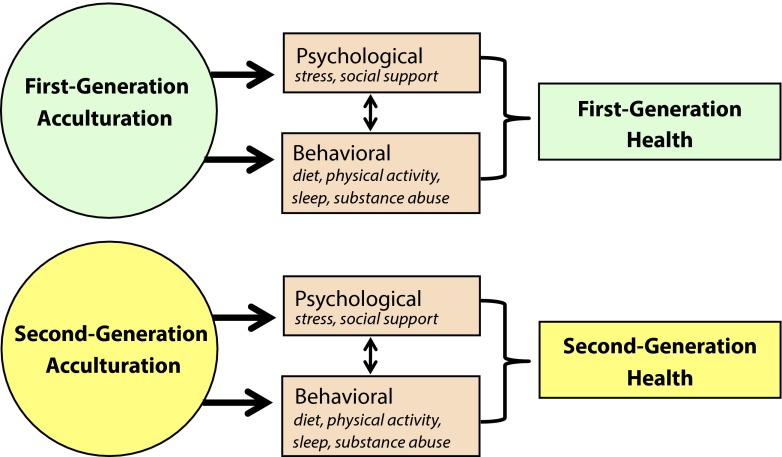
Change in an individual’s health after migration could hypothetically be attributable to change in ecological–environmental conditions or change in sociobehavioral conditions.172–174 Because the observed postmigration decline in Hispanic health has been shown to occur despite improvement in ecological–environmental conditions, such as higher SES, residence in neighborhoods with more health-promoting resources, and greater access to health care and education,8,17,18,69,80–91 previous authors have suggested changes in other factors as the likely pathway. The prevailing paradigm to explain the Hispanic acculturation paradox (Figure 1) posits that the effects of acculturation on health are mediated via the behavioral and psychological sequelae of acculturation, including (1) unhealthy behaviors, (2) loss of social support, and (3) acculturative stress, that, in turn, have impact on biology and health (i.e., the concept of biological embedding of life experience175,176). These pathways are not mutually exclusive. Here, we briefly summarize these processes (for reviews, see96,112,159).
FIGURE 1—
The prevailing paradigm, which suggests that the decline in health observed both within individuals and across generations of Hispanic Americans is explained by the degree of acculturation.
Unhealthy behaviors.
Acculturation appears to be associated with the adoption of unhealthy behaviors and the abandonment of healthy behaviors. Traditional Hispanic cultural values are generally associated with healthier behaviors that have been shown to deteriorate with acculturation. Acculturation has been associated with poor nutrition diets,81,161,177–181 fast food consumption,182,183 and less fruit and vegetable consumption.184,185 Acculturation has been positively associated with smoking,186,187 alcohol consumption,188,189 and illicit drug use,14,15,135,137,190–193 especially marijuana and cocaine.190,194,195 Subsequent-generation Hispanic immigrants are more likely to have insufficient sleep duration than first-generation Hispanics,196–198 and acculturation has been associated with poor sleep quality199,200 and insomnia.201 Contrary to expectations, acculturation among Hispanics appears to be associated with increasing amounts of time engaged in physical activity.202–206
Loss of social support.
The direct and indirect pathways linking social networks, relationships, and support with health are well established.207–209 A distinctive feature of Hispanic cultures is the quality of “familism,”28 which refers to strong attachment, identification, and loyalty toward one’s family132 and a high degree of social support.210–212 Immigration erodes ties between immigrants and family remaining in the home country, causing loss of social support and psychological distress.213 Maintaining contact with loved ones in the origin country can be more difficult with an increasing degree of acculturation because of linguistic and cultural barriers.214 Social isolation may accompany improvements in SES, as wealthier communities may also be characterized by fewer coethnics and more racism.215
Acculturative stress.
The direct and indirect pathways linking psychological stress with health are well established,216–218 including elucidation of their endocrine,219,220 immune,221,222 and oxidative223,224 pathways. Moreover, the effects of stress on health have been also demonstrated specifically in Mexican immigrants.225,226 The psychological distress associated with acculturation has been referred to as “acculturative stress,”26,227 and several authors have discussed the role of acculturative stress in negative health outcomes and as an important contributor to the acculturation paradox.130,131,228–231 Learning a new language, customs, dress, cuisine, and interpersonal relationship styles can induce a high degree of psychosocial stress.214,232 The loss of heritage identity may be its own source of psychological stress.18,233,234 Poor English language ability and the challenges of finding living arrangements and employment have been associated with a greater degree of acculturative stress.214,235 Fear of deportation can induce acculturative stress,236–238 and legal status can affect immigrants’ ability to incorporate into the mainstream culture.239 Documented and undocumented Hispanic immigrants have been shown to exhibit similar degrees of fear of deportation240 and no differences in health outcomes.155 Hispanics generally face considerable racism or discrimination,241 with studies suggesting that US-born Americans tend to regard Hispanic immigrants the most negatively of any migrant group in the United States.242 Immigrants may experience stress resulting from discrimination by Whites, other minorities, and later-generation Hispanic Americans.243,244
Acculturation and Biological Processes
A relatively small number of studies have examined the relationship of acculturation with biological pathways. In studies that used proxy measures of acculturation, nativity status (US-born Hispanics compared with foreign-born Hispanic immigrants) and longer duration of residence in the United States among Hispanic immigrants have been associated with higher blood pressure, metabolic risk biomarkers such as higher total cholesterol, low high-density lipoprotein to total cholesterol ratio, and glycosylated hemoglobin, inflammatory risk biomarkers such as circulating concentrations of proinflammatory cytokines, and higher levels of the stress hormone cortisol.78,245 In a study that used a multidimensional acculturation rating scale for Mexican Americans, greater Anglo cultural orientation was associated with an attenuated cortisol awakening response.246
Shortcomings of the Existing Paradigm and Unresolved Issues
The current paradigm linking acculturation with health in Hispanic Americans provides a plausible explanation, supported by empirical findings, for the within-individual health decline that is associated with length of residence in the United States. Previous authors have suggested that the intergenerational aspect of the observed health decline can also be explained using the same formulation (Figure 1), simply because US-born individuals are also likely to be more acculturated than foreign-born individuals.15,151,168,247 We, however, suggest that this explanation is not sufficient, and argue that its major shortcoming is its inability to adequately account for the observed intergenerational aspect of the health decline. Specifically, the existing paradigm (1) does not consider the biological continuity between generations, (2) fails to explain the observed decline in health outcomes between first-generation immigrants (foreign-born) and second- and subsequent generation native (US-born) individuals, and (3) does not appear to fully appreciate the potential implications of adverse birth outcomes in lifelong health.
Biological continuity between generations.
The acculturation paradox has been the subject of considerable interest in the academic, public health, and public policy sectors.68,69,150,248–250 However, until now, research has overlooked a crucial feature of the acculturation paradox: it includes an intergenerational component, and yet intergenerational transmission is unaddressed. It remains unknown whether effects associated with acculturation are biologically transmitted from one generation to the next. Rather, each generation has been considered as a biologically isolated entity, despite the fact that the generations are biologically linked. In other words, second-generation individuals are, by definition, the offspring of first-generation individuals, and yet the health effects of acculturation in first-generation Hispanics have not been included in previous efforts to understand health in second-generation Hispanics. The biological link between generations provides a basis for the possibility of intergenerational transmission, with pregnancy and fetal development representing an especially vulnerable period of time for the intergenerational transmission of the deleterious biobehavioral effects of acculturation from mothers to their children.
Nativity.
Among first-generation immigrants, acculturation status represents the change in cultural orientation that has occurred since immigration. Therefore, previous authors are justified in suggesting that acculturation may induce poor health both through adoption of unhealthy behaviors and through the psychosocial difficulties of cultural change. However, among subsequent-generation (US-born) individuals, acculturation status is not necessarily reflective of sociocultural change. US-born persons’ health status cannot be attributed to the experience or extent of the sociocultural adjustment associated with migration. Acculturation status may reflect a different construct for foreign-born and US-born individuals, and previous authors’ suggestions that acculturation’s relationship to health is similarly interpreted for foreign-born and native-born individuals15,151,168,247 may be unjustified (Figure 1). In accordance with this line of reasoning, several findings suggest that the acculturation status of first-generation and later-generation Hispanic individuals may not account for health differences between these 2 groups. For example, language preference did not explain the effect of nativity on birth outcomes in Mexican Americans.143 A multidimensional assessment of acculturation251 did not explain the effect of nativity on biological risk profiles.245 An acculturation variable encompassing language spoken at home and the proportion of foreign-born neighbors did not explain the effect of nativity on adolescent obesity.161
Existing frameworks are based on the premise that the health benefits of improvements in socioeconomic conditions that accompany longer duration of residence in the United States and acculturation are overshadowed by the more potent health detriments of the deleterious psychological and behavioral factors associated with acculturation. However, these deleterious psychological and behavioral factors, especially acculturative stress and loss of social support, may be less relevant for subsequent-generation individuals because they have not migrated. Also, Hispanic immigrants of different generational status do not experience different degrees of discrimination, which is an important contributor to acculturative stress.214,241,243
Birth outcomes.
Greater degree of acculturation33,82,148 and later generation status82,90,149–155 are associated with higher rates of adverse birth outcomes, including low birth weight, preterm birth, and lower infant survival.89,156–158 Existing frameworks suggest that acculturation’s deleterious health consequences may result in poor maternal condition during pregnancy, and thereby, contribute to adverse birth outcomes. However, these frameworks have not extended the logic of this phenomenon to consider whether maternal acculturation may affect the health of the offspring. We suggest that this effect of maternal acculturation on adverse birth outcomes should be considered in addressing the question of why subsequent-generation Hispanic individuals exhibit worse lifelong health than first-generation immigrants. The observation that maternal acculturation is associated with her child’s condition from as early as at the time of birth may be particularly relevant for interpreting intergenerational health patterns, because adverse birth outcomes are well-established predictors of increased risk for other adverse health conditions over the life course.252 In addition, many of the long-term health effects of intrauterine perturbations may not be evident at the time of birth, but may become apparent later in the life course.253–255 For example, even in the absence of adverse birth outcomes, the adult children of mothers who experience excessive psychological stress during pregnancy exhibit impaired endocrine stress reactivity,256 compromised immune function,257 insulin resistance,258 cognitive decline,259,260 and accelerated aging.261,262
A NEW PERSPECTIVE ON HISPANIC HEALTH DECLINE ACROSS GENERATIONS
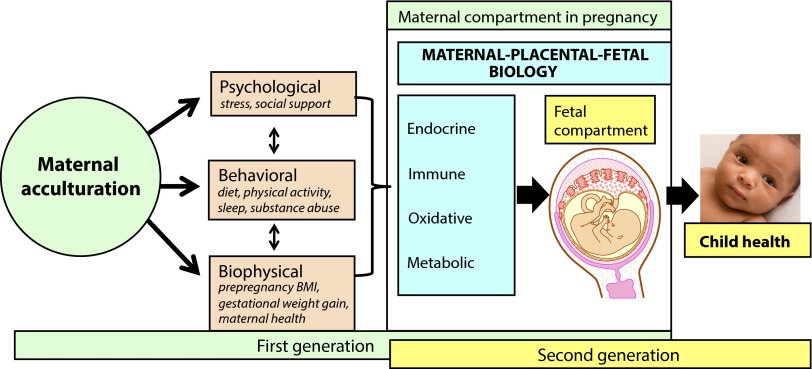
What, then, may account for the observed intergenerational decline in Hispanic health? There are 2 broad possibilities. First, the same exposures and processes whereby acculturation affects the health of first-generation individuals may operate independently in subsequent-generational individuals, somehow exerting a stronger effect on health status in subsequent generations (to account for escalation of poor health outcomes; Figure 1). Second, the health-related effects of acculturation that already have occurred in first-generation individuals may be transmitted to the next generation individuals in a way that perpetuates and possibly amplifies these effects (Figure 2). We argue in support of the latter possibility, because the former explanation has proven inadequate (see shortcomings of the existing paradigm, as previously described), and unfavorable health outcomes or their antecedent risk phenotypes in later-generation Hispanics may be already apparent during early stages of the life course, as indicated by patterns of adverse birth outcomes33,82,148 and childhood obesity.161,170
FIGURE 2—
New, proposed framework suggesting that maternal acculturation may influence fetal programming in ways that affect the offspring’s lifelong health, potentially accounting for the intergenerational decline in health observed in Hispanic Americans.
Note. BMI = body mass index.
Our framework integrates the concepts of biological embedding of life experiences and fetal origins of health and disease risk (Figure 2) to posit that the effects of acculturation can be transmitted across generations from mothers to their offspring. We suggest that intrauterine life represents a key time period when the effects of maternal acculturation may be transmitted to offspring, that the principal mode of transmission is biological, and that transmission occurs via the psychological and behavioral consequences of maternal acculturation on aspects of maternal–placental–fetal gestational biology that participate in the process of fetal programming of health and disease risk. There is extensive empirical evidence from human and animal-model studies that the same processes that have been associated in Hispanics with maternal acculturation (i.e., unfavorable psychological and behavioral states) exert pervasive effects on gestational processes implicated in fetal programming.37,253,263–265 There is also some evidence specifically in pregnant Hispanic women that links acculturation and acculturation-related processes with gestational biology,38,40,41,148,266,267 and with maternal psychological36,38,268,269 and behavioral30–36,161 states that are linked to gestational biology. Through the pathway of fetal programming, the acculturation experience of one generation may influence the health of subsequent generations. This pattern can account for and also reconcile unresolved issues in the acculturation paradox.
Fetal Programming and Lifelong Health
In the context of the intergenerational transmission of the effects of acculturation, our focus on fetal programming as the principal candidate mechanism of interest is justified by the fact that the origins of many health outcomes whose prevalence differs by generation status in Hispanics can be traced back to developmental processes in the fetal period of life. As described previously, the adult health outcomes most robustly implicated in the Hispanic acculturation paradox are obesity, diabetes, cardiovascular disease, and depression.159 Each of these conditions is a noncommunicable chronic disease or disorder. For any given individual, the likelihood of developing an NCD is a joint function of both cumulative exposures to risk factors (e.g., excess caloric intake, hyperglycemia, hyperlipidemia, antigen exposure, stressful life events) and susceptibility to these exposures, as reflected in the wide interindividual variation in the magnitude and duration of biological responses to these and other health-risk exposures in question.37,255,263 Contrary to the assertion that susceptibility is determined solely by genetic (DNA base-pair) variation,45 a growing and converging body of epidemiological, clinical, experimental, cellular, and molecular evidence supports the concept that susceptibility for NCDs is determined by the dynamic interplay between genetic makeup and environment, particularly during the embryonic and fetal periods of development.253,263,270,271 Development is a plastic process in which a range of different phenotypes can be expressed from a given genotype. The unfolding of developmental processes across the multicontoured landscape from genotype to phenotype is context-dependent, in which the developing embryo or fetus seeks, receives, and responds to, or is acted upon by, the intrauterine environment during sensitive periods of cellular proliferation, differentiation, and maturation, which results in structural and functional changes in cells, tissues, organ systems, and homeostatic set points (the process of phenotypic specification). These changes may, either independently or through interactions with subsequent developmental processes and environments, have short- or long-term consequences for health and disease susceptibility.253,263 These concepts have variously been referred to as the fetal or developmental origins of health and disease risk.270,272,273 It is important to emphasize that, except in extreme cases, this process of phenotypic specification does not, per se, cause disease, but, instead, determines propensity or susceptibility for the development of disease(s) in later life by shaping the individual’s responses to subsequent endogenous and exogenous conditions.273
Our framework also addresses the proximate causal pathway by emphasizing the tripartite role of metabolism- and stress-related maternal–placental–fetal biological processes as key sensors, transducers, and effectors of acculturation-related states and conditions on the developing fetus. Extrinsic (environmental) conditions related to energy availability and mortality risk represent key factors that determine the evolutionary adaptiveness of traits. We, therefore, propose that the biological systems most sensitive to these 2 classes of conditions would be expected to directly mediate phenotypic specification during development. Metabolism- and stress-related processes constitute an attractive underlying common candidate mechanism because of their sensitivity to these 2 types of environmental conditions. Metabolism- and stress-related maternal–placental–fetal endocrine, immune, and oxidative processes in gestation represent a plausible mediating pathway during fetal development because they are responsive to all classes of intrauterine perturbations (sensors), they mediate all communication between maternal and fetal compartments (transducers), and they play an essential and obligatory role in orchestrating key events and variations underlying cellular growth, replication, and differentiation in the brain and peripheral tissues (effectors).264,265,274–277
Maternal Acculturation and Fetal Programming of Health
The predominant, proximate pathway by which maternal environmental, psychological, behavioral, or other conditions influence offspring development in utero is ultimately biological in nature and involves maternal–placental–fetal gestational physiology. It follows, then, that a crucial component of our framework of intergenerational transmission of the effects of maternal acculturation on offspring health and disease risk (Figure 2) is the question of whether maternal acculturation can influence maternal–placental–fetal gestational biology, particularly those aspects of gestation biology that have been implicated in fetal programming of health and disease risk. Our model proposes that the effects of maternal acculturation on maternal–placental–fetal gestational biology are mediated by the same behavioral, psychosocial, and biophysical sequelae of acculturation that are linked to health and disease risk within the individual life span (Figure 1), because in the context of pregnancy, each of these domains has previously been shown to affect gestational biology.263,278–280 The plausibility of our model is supported by empirical evidence in the general population, and is also supported more specifically by study findings in pregnant Hispanic women that describe the effects of maternal acculturation on the same psychological, behavioral, and biological processes that have been implicated in the process of fetal programming.
Maternal acculturation and gestational biology.
The small number of studies that have addressed maternal acculturation’s effect on maternal–placental–fetal gestational biology have consistently reported that among pregnant Mexican American women, a greater degree of acculturation is associated with several indicators of gestational biology that are implicated in the process of fetal programming. These include higher concentrations of the stress hormones cortisol266 and placental corticotrophin-releasing factor,148 hypothalamic–pituitary–adrenal axis feedback dysregulation (blunted diurnal cortisol slope),267 a higher estriol-to-progesterone ratio,40,41 and higher concentrations of proinflammatory cytokines.38 Later generation status was associated with lower concentrations of the stress hormones cortisol and corticotropin-releasing hormone and a higher estriol-to-progesterone ratio in Mexican American pregnant women.39 Also, the evidence, reviewed in a preceding section,78,245 that acculturation is associated with biomarkers of health in nonpregnant Hispanic individuals provides further, but more tentative, support of the likelihood that acculturation may influence gestational biology.
Maternal acculturation and health-related behaviors in pregnancy.
Maternal health-related behaviors before or during pregnancy are known to influence maternal–placental–fetal biology directly via biological pathways or indirectly via psychological pathways.278,279,281 A greater degree of acculturation among Hispanic women has been associated during pregnancy with poorer diet,30,33 more alcohol,31,36 cigarette smoking,30–34 marijuana31 and other substance abuse,34–36 and inactivity.161 Another finding of note is that the effect of acculturation on health-related behaviors is strongest and most consistent for women (e.g., smoking,282,283 alcohol,179,180,189,284,285 drug use193,195) compared with men. Mexican American women with lower acculturation scores (as assessed by a combination of nativity, length of stay, and language preference) exhibited lower folic acid dietary intakes than more acculturated Mexican American women.286,287
Maternal acculturation and psychosocial processes in pregnancy.
Maternal psychosocial conditions before or during pregnancy are known to influence maternal–placental–fetal biology directly via endocrine, immune, and oxidative state-related pathways, and indirectly via effects on health-related behaviors.278,279,281,288,289 During pregnancy, second-generation Mexican American women are more likely than Mexican immigrant women to experience depression,38,39 anxiety,39,268 and prenatal stress.36,39 More acculturated Mexican American women compared with those less acculturated (as measured by language preference) exhibited higher rates of depression during pregnancy.269 With acculturation, women may lose an important source of social support during pregnancy.290 In traditional Hispanic cultures, women within a community are close-knit, receiving support not only from their own female relatives but also from other women in the community and “comadres” or godmothers.291 As acculturation progresses, the degree of community and family support may diminish. Hispanic immigrants to the United States who retain more traditional Hispanic values have been shown to benefit from more family support during pregnancy,30,292 have higher degrees of pregnancy wantedness,36,293 are more likely to be married or living with a partner,31 and have more family-centered views with regard to reproduction and parenting.293–295
Interaction between the effects of maternal acculturation during gestation and child acculturation after birth on subsequent child health outcomes.
As discussed previously, the likelihood of developing a complex, common NCD is a joint function of exposure to risk factors and the individual’s predisposition or susceptibility. Fetal programming plays a major role in shaping predisposition or susceptibility. Thus, maternal acculturation may affect fetal developmental processes that alter her child’s physiological or psychological susceptibility to potentially deleterious conditions encountered subsequently over the course of the child’s life. Some of these conditions may themselves be causally related to the child’s own acculturation status, such as an unhealthy diet. In this way, maternal acculturation during pregnancy could additionally affect child health by influencing the child’s susceptibility to environmental risk factors associated with the child’s own subsequent cultural orientation. For example, maternal acculturation may be associated with excess maternal stress or poor diet, which may alter maternal–placental–fetal glucocorticoid physiology during pregnancy. Exposure to inappropriate concentrations of glucocorticoids during sensitive periods of intrauterine development is known to produce alterations in the fetal brain and peripheral systems that have long-term consequences and can alter the offspring’s propensity for developing excessive adiposity and metabolic disorders in the face of obesogenic exposures. These changes include altered set points in hypothalamic circuits that regulate appetite and satiety,296,297 reduced β-cell mass,298 impaired adipocyte (peroxisome proliferator-activated receptor-γ) function,299,300 and decreased insulin sensitivity.301 Through this pathway, a mother’s acculturation could alter her offspring’s degree of susceptibility to obesity and metabolic disorders in the context of her offspring’s exposure to a typical US (as opposed to traditional Hispanic) diet. Similar suites of phenotypic changes in association with alterations in maternal–placental–fetal gestational biology have been described with respect to the propensity for developing the various other adverse health outcomes implicated in the Hispanic acculturation paradox.
Postnatal transmission of effects of maternal acculturation on child health.
Only a small number of studies have examined the link between maternal acculturation and children's health (e.g., physical illness,302 such as asthma,303,304 and risk of psychological disorders, such as internalizing behaviors305). These authors postulated postnatal pathways of transmission, but they did not investigate the underlying mechanisms. Although it is quite plausible that the process of fetal programming may account for these findings (in the manner discussed previously), we recognize and note that intrauterine life is not the only time period when acculturation may exert an intergenerational effect on health. Another time window and mode of parent-to-child transmission of the effects of acculturation may be during postnatal life, potentially through the effects of maternal acculturation on infant feeding practices (including duration of breast feeding and breast milk composition),306–308 parent–child interaction and parenting behaviors,309,310 or health care utilization.311,312 Further discussion of these postnatal pathways is beyond the scope of this article.
Reconciliation
We suggest that the fetal programming perspective potentially offers a parsimonious explanation to account for the observed intergenerational decline in Hispanic American health, and also to reconcile the apparent contradiction among the observations in this population that disease risk increases across generations despite improvements in life conditions.8,17,18,69,80–91
If the unfavorable psychological, behavioral, and biological sequelae of acculturation established in one generation of women are transmitted to the next generation particularly during the sensitive period of fetal life, the resulting consequences in the subsequent generation can include long-term alterations in the physiological sensitivity of endocrine, immune, vascular, metabolic, cognitive, and affective systems.253,313,314 These alterations may not only perpetuate the intergenerational cycle of poor health but may amplify it. The same conditions that produced poor health in the prior generation may persist and act on the second generation and produce even larger adverse effects because the second-generation individual is physiologically more reactive to these exposures than the parent-generation individual.313,315,316 If the magnitude of this amplification is greater than the salutary effects of improvements in socioeconomic conditions, the net effect is worse health in the second-generation individuals compared with the first-generation individuals despite improvements in SES. Exposure to unfavorable conditions during the prenatal period of life is known to have greater and longer term effects compared with exposure to the same or equivalent unfavorable conditions encountered later in the life course.253,263 Therefore, fetal exposure to the mother’s stresses and unhealthy behaviors associated with acculturation may have lifelong health consequences for the US-born child, regardless of the postnatal improvements in the child’s life conditions. This pattern may then enhance the likelihood of poor health among third-generation individuals, and so forth, across generations.
There is already evidence for this kind of intergenerational trend among underprivileged US minority groups. Among African Americans, low-birth weight and preterm birth persist across generations despite improvement in socioeconomic conditions.317–319 The authors of these studies have suggested that unfavorable life conditions in an initial generation of individuals could instigate a transgenerational cascade of adverse birth outcomes, regardless of the life conditions of subsequent generations.318
PUBLIC HEALTH RELEVANCE
The perspective that the effects of acculturation can be biologically transmitted across generations via the process of fetal programming to perpetuate intergenerational cycles of social disadvantage and poor health may have broad implications for public health and policy in the United States and elsewhere. The approach articulated in this article has implications for risk identification and the subsequent development of interventions directed toward primary prevention in not only the Hispanic American population but perhaps also has implications in other national and global minority, immigrant populations, and populations in transition.
Women’s Health
The fetal origins perspective places a particular emphasis on the health and well-being of girls and women of reproductive age. Attending to the health of Hispanic women could be of vital importance for stemming transgenerational cascades of poor health.
Although child- and adult-intervention approaches have dominated national and global efforts to diminish NCD incidence and health disparities,312,320,321 our framework points to the importance of interventions focused on the prenatal phase of life. Because of the abundance of evidence for NCD propensity being strongly influenced by prenatal conditions, along with the substantial and growing national and global threat of the NCD burden, primary prevention strategies aimed at girls and women are warranted.
Future Hispanic Demographics and Public Health
The fetal origins perspective is especially relevant for shedding light on the determinants of health in the offspring of individuals who experience adversity. Therefore, in the case of immigrants, this perspective offers specific insight into the determinants of health in second-generation individuals.
In terms of national disease burden, health in second-generation Hispanics is especially important to consider, because Hispanic demographic characteristic trends predict that over the next 20 years, the second generation is projected to emerge as the largest subset of Hispanic Americans, compared with the first-generation (immigrants) and subsequent generations.3 Thus, health decline in second-generation Hispanics poses a particularly urgent and growing threat. In addition, the health status of second-generation individuals would affect fetal development of third-generation individuals and thereby affect third-generation health, and so forth; therefore, these adverse health conditions may perpetuate across generations.
Public Policy and Global Health
Understanding the health consequences of the integration of Hispanic immigrants into American society has profound implications for public policy. There is a need to understand the potential downstream health effects of policies that influence postmigration life, such as immigration reform, child education, and neighborhood integration. In addition, a better understanding of acculturation’s transgenerational effects in Hispanic Americans could inform epidemiological and biomedical studies in other immigrant populations, especially because acculturation paradoxes have been observed in other immigrant groups, including African,322 Chinese,323,324 and Korean325 immigrants in the United States, as well as ethnic-minority immigrants in the United Kingdom,326,327 Canada,328,329 Sweden, Finland,330 and Israel.233
A better understanding of acculturation’s transgenerational effects would also inform issues of public health in rapidly developing countries, where dramatic environmental and cultural change may occur within an individual’s lifetime. In these populations in transition, the process of acculturation may be relevant for health among nonmigrant individuals who experience the change of sociocultural context that occurs with industrialization, urbanization, and globalization. Deciphering the mechanisms through which chronic disease risk varies by generation status in the United States will help in preparing for national disease and disability burden, and forecasting worldwide changes in health-related conditions as global migration continues to accelerate.
CONCLUSIONS
Existing frameworks on the effects of acculturation and acculturation-related processes in Hispanic Americans on health over time and across generations have not satisfactorily addressed important issues related to intergenerational transmission and nativity. In this context, we propose the adoption of a fetal programming perspective that takes into account the biological continuity between generations and considers each subsequent generation with regard to the cumulative effects of previous generations’ acculturation experiences. This perspective provides the opportunity to arrive at a parsimonious explanation that accounts for the observed intergenerational decline in Hispanic American health and also reconciles the apparent contradiction of disease risk increases across generations despite improvements in life conditions. This understanding has important implications for risk identification and the development of interventions aimed at primary prevention to break the cycle of perpetuation of suboptimal health in the disenfranchised and rapidly growing minority population of Hispanic Americans.
Acknowledgments
The preparation of the article was supported, in part, by United States Public Health Service (National Institutes of Health; grants RO1 HD-060628 to P. D. W., RO1 HD-065825 to S. E., and RO1 MH-091351 to C. B.).
Human Participant Protection
Institutional review board approval was not needed because no research with human participants was conducted.
References
- 1.Passel J, Cohn D. Population projections: 2005-2050. 2008. Available at: http://www.pewhispanic.org/2008/02/11/us-population-projections-2005-2050. Accessed December 18, 2013.
- 2.Lopez MH, Cohn D. Hispanic poverty rate highest in new supplemental census measure. 2011. Available at: http://www.pewhispanic.org/2011/11/08/hispanic-poverty-rate-highest-in-new-supplemental-census-measure. Accessed November 11, 2013.
- 3.Suro R, Passel JS. The rise of the second generation: changing patterns in Hispanic population growth. 2003: Available at: http://pewhispanic.org/files/reports/22.pdf. Accessed November 26, 2013.
- 4.Cook B, Alegría M, Lin JY, Guo J. Pathways and correlates connecting Latinos’ mental health with exposure to the United States. Am J Public Health. 2009;99(12):2247–2254. doi: 10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho Y, Frisbie WP, Hummer RA, Rogers RG. Nativity, duration of residence, and the health of Hispanic adults in the United States. Int Migr Rev. 2004;38(1):184–211. [Google Scholar]
- 6.Kaplan MS, Huguet N, Newsom JT, McFarland BH. The association between length of residence and obesity among Hispanic immigrants. Am J Prev Med. 2004;27(4):323–326. doi: 10.1016/j.amepre.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Fuentes-Afflick E, Hessol NA. Acculturation and body mass among Latina women. J Womens Health (Larchmt) 2008;17(1):67–73. doi: 10.1089/jwh.2007.0389. [DOI] [PubMed] [Google Scholar]
- 8.Abraído-Lanza AF, Chao MT, Florez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc Sci Med. 2005;61(6):1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oza-Frank R, Venkat Narayan K. Effect of length of residence on overweight by region of birth and age at arrival among US immigrants. Public Health Nutr. 2010;13(6):868–875. doi: 10.1017/S1368980009992084. [DOI] [PubMed] [Google Scholar]
- 10.Koya DL, Egede LE. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007;22(6):841–846. doi: 10.1007/s11606-007-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goel MS, McCarthy EP, Phillips RS, Wee CC. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292(23):2860–2867. doi: 10.1001/jama.292.23.2860. [DOI] [PubMed] [Google Scholar]
- 12.Stern MP, Gonzalez C, Mitchell BD, Villalpando E, Haffner SM, Hazuda HP. Genetic and environmental determinants of type II diabetes in Mexico City and San Antonio. Diabetes. 1992;41(4):484–492. doi: 10.2337/diab.41.4.484. [DOI] [PubMed] [Google Scholar]
- 13.Sundquist J, Winkleby MA. Cardiovascular risk factors in Mexican American adults: a transcultural analysis of NHANES III, 1988-1994. Am J Public Health. 1999;89(5):723–730. doi: 10.2105/ajph.89.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ortega AN, Rosenheck R, Alegria M, Desai RA. Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. J Nerv Ment Dis. 2000;188(11):728–735. doi: 10.1097/00005053-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Vega WA, Sribney WM, Achara-Abrahams I. Co-occurring alcohol, drug, and other psychiatric disorders among Mexican-origin people in the United States. Am J Public Health. 2003;93(7):1057–1064. doi: 10.2105/ajph.93.7.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vega WA, Sribney WM, Miskimen TM, Escobar JI, Aguilar-Gaxiola S. Putative psychotic symptoms in the Mexican American population: prevalence and co-occurrence with psychiatric disorders. J Nerv Ment Dis. 2006;194(7):471–477. doi: 10.1097/01.nmd.0000228500.01915.ae. [DOI] [PubMed] [Google Scholar]
- 17.Alegría M, Canino G, Shrout PE et al. Prevalence of mental illness in immigrant and non-immigrant US Latino groups. Am J Psychiatry. 2008;165(3):359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Arch Gen Psychiatry. 1998;55(9):771–778. doi: 10.1001/archpsyc.55.9.771. [DOI] [PubMed] [Google Scholar]
- 19.Mościcki EK, Locke BZ, Rae DS, Boyd JH. Depressive symptoms among Mexican Americans: the Hispanic Health and Nutrition Examination Survey. Am J Epidemiol. 1989;130(2):348–360. doi: 10.1093/oxfordjournals.aje.a115341. [DOI] [PubMed] [Google Scholar]
- 20.Swanson JW, Linskey AO, Quintero-Salinas R, Pumariega AJ, Holzer CE., III A binational school survey of depressive symptoms, drug use, and suicidal ideation. J Am Acad Child Adolesc Psychiatry. 1992;31(4):669–678. doi: 10.1097/00004583-199207000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Slattery ML, Sweeney C, Edwards S et al. Physical activity patterns and obesity in Hispanic and non-Hispanic white women. Med Sci Sports Exerc. 2006;38(1):33–41. doi: 10.1249/01.mss.0000183202.09681.2a. [DOI] [PubMed] [Google Scholar]
- 22.Corral I, Landrine H. Acculturation and ethnic-minority health behavior: a test of the operant model. Health Psychol. 2008;27(6):737–745. doi: 10.1037/0278-6133.27.6.737. [DOI] [PubMed] [Google Scholar]
- 23.Fitzgerald N, Himmelgreen D, Damio G, Segura-Pérez S, Peng Y-K, Pérez-Escamilla R. Acculturation, socioeconomic status, obesity and lifestyle factors among low-income Puerto Rican women in Connecticut, US, 1998–1999. Rev Panam Salud Publica. 2006;19(5):306–313. doi: 10.1590/s1020-49892006000500003. [DOI] [PubMed] [Google Scholar]
- 24.Kasirye OC, Walsh JA, Romano PS et al. Acculturation and its association with health-risk behaviors in a rural Latina population. Ethn Dis. 2005;15(4):733–739. [PubMed] [Google Scholar]
- 25.Torres L, Driscoll MW, Voell M. Discrimination, acculturation, acculturative stress, and Latino psychological distress: a moderated mediational model. Cultur Divers Ethnic Minor Psychol. 2012;18(1):17–25. doi: 10.1037/a0026710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berry JW. Acculturative stress. In: Wong P, Wong L, editors. Handbook of Multicultural Perspectives on Stress and Coping. Langley, BC, Canada: Springer; 2006. pp. 287–298. [Google Scholar]
- 27.Finch BK, Hummer RA, Kol B, Vega WA. The role of discrimination and acculturative stress in the physical health of Mexican-origin adults. Hisp J Behav Sci. 2001;23(4):399–429. [Google Scholar]
- 28.Ayón C, Marsiglia FF, Bermudez-Parsai M. Latino family mental health: exploring the role of discrimination and familismo. J Community Psychol. 2010;38(6):742–756. doi: 10.1002/jcop.20392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gil AG, Wagner EF, Vega WA. Acculturation, familism, and alcohol use among Latino adolescent males: longitudinal relations. J Community Psychol. 2000;28(4):443–458. [Google Scholar]
- 30.Page RL. Positive pregnancy outcomes in Mexican immigrants: what can we learn? J Obstet Gynecol Neonatal Nurs. 2004;33(6):783–790. doi: 10.1177/0884217504270595. [DOI] [PubMed] [Google Scholar]
- 31.Page RL. Differences in health behaviors of Hispanic, White, and Black childbearing women: focus on the Hispanic paradox. Hisp J Behav Sci. 2007;29(3):300–312. [Google Scholar]
- 32.Acevedo MC. The role of acculturation in explaining ethnic differences in the prenatal health-risk behaviors, mental health, and parenting beliefs of Mexican American and European American at-risk women. Child Abuse Negl. 2000;24(1):111–127. doi: 10.1016/s0145-2134(99)00121-0. [DOI] [PubMed] [Google Scholar]
- 33.Cobas JA, Balcazar H, Benin MB, Keith VM, Chong Y. Acculturation and low-birthweight infants among Latino women: a reanalysis of HHANES data with structural equation models. Am J Public Health. 1996;86(3):394–396. doi: 10.2105/ajph.86.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heilemann MV, Lee KA, Stinson J, Koshar JH, Goss G. Acculturation and perinatal health outcomes among rural women of Mexican descent. Res Nurs Health. 2000;23(2):118–125. doi: 10.1002/(sici)1098-240x(200004)23:2<118::aid-nur4>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 35.Coonrod DV, Bay RC, Balcazar H. Ethnicity, acculturation and obstetric outcomes: different risk factor profiles in low-and high-acculturation Hispanics and in white non-Hispanics. J Reprod Med. 2004;49(1):17–22. [PubMed] [Google Scholar]
- 36.Zambrana RE, Scrimshaw S, Collins N, Dunkel-Schetter C. Prenatal health behaviors and psychosocial risk factors in pregnant women of Mexican origin: the role of acculturation. Am J Public Health. 1997;87(6):1022–1026. doi: 10.2105/ajph.87.6.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Entringer S, Buss C, Wadhwa PD. Prenatal stress and developmental programming of human health and disease risk: concepts and integration of empirical findings. Curr Opin Endocrinol Diabetes Obes. 2010;17(6):507–516. doi: 10.1097/MED.0b013e3283405921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ruiz RJ, Stowe RP, Goluszko E, Clark MC, Tan A. The relationships among acculturation, body mass index, depression, and interleukin 1-receptor antagonist in Hispanic pregnant women. Ethn Dis. 2007;17:338–343. [PubMed] [Google Scholar]
- 39.Ruiz RJ, Stowe RP, Brown A, Wommack J. Acculturation and biobehavioral profiles in pregnant women of Hispanic origin: generational differences. ANS Adv Nurs Sci. 2012;35(3):E1–E10. doi: 10.1097/ANS.0b013e3182626199. [DOI] [PubMed] [Google Scholar]
- 40.Ruiz RJ, Marti CN, Pickler R, Murphey C, Wommack J, Brown CE. Acculturation, depressive symptoms, estriol, progesterone, and preterm birth in Hispanic women. Arch Womens Ment Health. 2012;15(1):57–67. doi: 10.1007/s00737-012-0258-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ruiz RJ, Saade GR, Brown CE et al. The effect of acculturation on progesterone/estriol ratios and preterm birth in Hispanics. Obstet Gynecol. 2008;111(2 pt 1):309–316. doi: 10.1097/01.AOG.0000297896.00491.2c. [DOI] [PubMed] [Google Scholar]
- 42.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- 43.Dankwa-Mullan I, Rhee KB, Williams K et al. The science of eliminating health disparities: summary and analysis of the NIH summit recommendations. Am J Public Health. 2010;100(suppl 1):S12–S18. doi: 10.2105/AJPH.2010.191619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.US Department of Health and Human Services. Healthy People 2020. 2011. Available at: http://www.healthypeople.gov/2020. Accessed November 12, 2013. [DOI] [PubMed]
- 45.National Institutes of Health. NIH health disparities strategic plan and budget, fiscal years 2009-2013. Available at: http://www.nimhd.nih.gov/documents/NIH%20Health%20Disparities%20Strategic%20Plan%20and%20Budget%202009-2013.pdf. Accessed October 18, 2013.
- 46.Adler NE, Rehkopf DH. US disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 47.Wise PH. Confronting social disparities in child health: a critical appraisal of life-course science and research. Pediatrics. 2009;124(suppl 3):S203–S211. doi: 10.1542/peds.2009-1100H. [DOI] [PubMed] [Google Scholar]
- 48.Dankwa-Mullan I, Rhee KB, Stoff DM et al. Moving toward paradigm-shifting research in health disparities through translational, transformational, and transdisciplinary approaches. Am J Public Health. 2010;100(suppl 1):S19–S24. doi: 10.2105/AJPH.2009.189167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ruffin J. The science of eliminating health disparities: embracing a new paradigm. Am J Public Health. 2010;100(suppl 1):S8–S9. doi: 10.2105/AJPH.2010.191957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Adler N, Bush NR, Pantell MS. Rigor, vigor, and the study of health disparities. Proc Natl Acad Sci U S A. 2012;109(suppl 2):17154–17159. doi: 10.1073/pnas.1121399109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fontaine KR, McCubrey R, Mehta T et al. Body mass index and mortality rate among Hispanic adults: a pooled analysis of multiple epidemiologic data sets. Int J Obes (Lond) 2012;36(8):1121–1126. doi: 10.1038/ijo.2011.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 53.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults. JAMA. 2002;287(3):356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 54.Siegel R, Naishadham D, Jemal A. Cancer statistics for Hispanics/Latinos, 2012. CA Cancer J Clin. 2012;62(5):283–298. doi: 10.3322/caac.21153. [DOI] [PubMed] [Google Scholar]
- 55.Tang M-X, Cross P, Andrews H et al. Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology. 2001;56(1):49–56. doi: 10.1212/wnl.56.1.49. [DOI] [PubMed] [Google Scholar]
- 56.US Census Bureau. National characteristics: population by sex, race, and Hispanic origin. Estimates of the components of resident population change by race and Hispanic origin for the United States. Population division. 2012. Available at: http://factfinder2.census.gov. Accessed January 1, 2014.
- 57.US Census Bureau. Supplemental US population projections: 2000-2050. 2009. Available at: http://www.census.gov/newsroom/releases/archives/population/2009-12-16_population.html. Accessed December 24, 2013.
- 58.Motel S, Patten E. Statistical portrait of the foreign-born population in the United States, 2011. 2013. Available at: http://www.pewhispanic.org/2013/01/29/statistical-portrait-of-the-foreign-born-population-in-the-united-states-2011. Accessed June 24, 2013.
- 59.US Census Bureau. Selected characteristics of the foreign-born population by region of birth: Latin America: 2012 American Community Survey 1-year estimates. 2012. Available at: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_12_1YR_S0506&prodType=table. Accessed December 24, 2013.
- 60.US Census Bureau. Selected social characteristics in the United States: 2012 American Community Survey 1-year estimates. 2012. Available at: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_12_1YR_DP02&prodType=table. Accessed December 24, 2013.
- 61.US Census Bureau. ACS demographic and housing estimates: 2012 American Community Survey 1-year estimates. 2012. Available at: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_12_1YR_DP05&prodType=table. Accessed January 1, 2014.
- 62.Acevedo-Garcia D, Bates L. Latino health paradoxes: empirical evidence, explanations, future research, and implications. In: Rodríguez H, Sáenz R, Menjívar C, editors. Latinas/os in the United States: Changing the Face of América. New York, NY: Springer; 2008. pp. 101–113. [Google Scholar]
- 63.Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic status in the United States. JAMA. 1993;270(20):2464–2468. [PubMed] [Google Scholar]
- 64.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- 65.Hummer RA, Rogers R, Amir S, Forbes D, Frisbie W. Adult mortality differentials among Hispanic subgroups and non-Hispanic whites. Soc Sci Q. 2000;81(1):459–476. [PubMed] [Google Scholar]
- 66.Lin CC, Rogot E, Johnson NJ, Sorlie PD, Arias E. A further study of life expectancy by socioeconomic factors in the National Longitudinal Mortality Study. Ethn Dis. 2003;13(2):240–247. [PubMed] [Google Scholar]
- 67.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol. 2002;74(1):83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- 68.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11(3):496–518. [PubMed] [Google Scholar]
- 69.Scribner R. Paradox as paradigm–the health outcomes of Mexican Americans. Am J Public Health. 1996;86(3):303–305. doi: 10.2105/ajph.86.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ford ES, Giles WH, Mokdad AH, Myers GL. Distribution and correlates of C-reactive protein concentrations among adult US women. Clin Chem. 2004;50(3):574–581. doi: 10.1373/clinchem.2003.027359. [DOI] [PubMed] [Google Scholar]
- 71.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 72.Mitchell BD, Stern MP, Haffner SM, Hazuda HP, Patterson JK. Risk factors for cardiovascular mortality in Mexican Americans and non-Hispanic whites. San Antonio Heart Study. Am J Epidemiol. 1990;131(3):423–433. doi: 10.1093/oxfordjournals.aje.a115517. [DOI] [PubMed] [Google Scholar]
- 73.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 74.Riosmena F, Wong R, Palloni A. Migration selection, protection, and acculturation in health: a binational perspective on older adults. Demography. 2013;50(3):1039–1064. doi: 10.1007/s13524-012-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Elo IT, Turra CM, Kestenbaum B, Ferguson BR. Mortality among elderly Hispanics in the United States: past evidence and new results. Demography. 2004;41(1):109–128. doi: 10.1353/dem.2004.0001. [DOI] [PubMed] [Google Scholar]
- 76.Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60(spec no. 2):S68–S75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- 77.Barquera S, Durazo-Arvizu R, Luke A, Cao G, Cooper R. Hypertension in Mexico and among Mexican Americans: prevalence and treatment patterns. J Hum Hypertens. 2008;22(9):617–626. doi: 10.1038/jhh.2008.9. [DOI] [PubMed] [Google Scholar]
- 78.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97(7):1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Crimmins EM, Soldo BJ, Ki Kim J, Alley DE. Using anthropometric indicators for Mexicans in the United States and Mexico to understand the selection of migrants and the “Hispanic paradox.”. Soc Biol. 2005;52(3-4):164–177. doi: 10.1080/19485565.2005.9989107. [DOI] [PubMed] [Google Scholar]
- 80.Hazuda HP, Haffner SM, Stern MP, Eifler CW. Effects of acculturation and socioeconomic status on obesity and diabetes in Mexican Americans. The San Antonio Heart Study. Am J Epidemiol. 1988;128(6):1289–1301. doi: 10.1093/oxfordjournals.aje.a115082. [DOI] [PubMed] [Google Scholar]
- 81.Guendelman S, Abrams B. Dietary intake among Mexican-American women: generational differences and a comparison with white non-Hispanic women. Am J Public Health. 1995;85(1):20–25. doi: 10.2105/ajph.85.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Scribner R, Dwyer JH. Acculturation and low birthweight among Latinos in the Hispanic HANES. Am J Public Health. 1989;79(9):1263–1267. doi: 10.2105/ajph.79.9.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002;13(4):477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cuellar I, Roberts RE. Relations of depression, acculturation, and socioeconomic status in a Latino sample. Hisp J Behav Sci. 1997;19(2):230–238. [Google Scholar]
- 85.Beard HA, Al Ghatrif M, Samper-Ternent R, Gerst K, Markides KS. Trends in diabetes prevalence and diabetes-related complications in older Mexican Americans from 1993–1994 to 2004–2005. Diabetes Care. 2009;32(12):2212–2217. doi: 10.2337/dc09-0938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mainous AG, III, Majeed A, Koopman RJ et al. Acculturation and diabetes among Hispanics: evidence from the 1999–2002 National Health and Nutrition Examination Survey. Public Health Rep. 2006;121(1):60–66. doi: 10.1177/003335490612100112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Crump C, Lipsky S, Mueller BA. Adverse birth outcomes among Mexican-Americans: are US-born women at greater risk than Mexico-born women? Ethn Health. 1999;4(1-2):29–34. doi: 10.1080/13557859998164. [DOI] [PubMed] [Google Scholar]
- 88.Espino DV, Maldonado D. Hypertension and acculturation in elderly Mexican Americans: results from 1982–84 Hispanic HANES. J Gerontol. 1990;45(6):M209–M213. doi: 10.1093/geronj/45.6.m209. [DOI] [PubMed] [Google Scholar]
- 89.Singh GK, Yu SM. Adverse pregnancy outcomes: differences between US-and foreign-born women in major US racial and ethnic groups. Am J Public Health. 1996;86(6):837–843. doi: 10.2105/ajph.86.6.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Collins JW, Shay DK. Prevalence of low birth weight among Hispanic infants with United States-born and foreign-born mothers: the effect of urban poverty. Am J Epidemiol. 1994;139(2):184–192. doi: 10.1093/oxfordjournals.aje.a116980. [DOI] [PubMed] [Google Scholar]
- 91.Zsembik BA, Fennell D. Ethnic variation in health and the determinants of health among Latinos. Soc Sci Med. 2005;61(1):53–63. doi: 10.1016/j.socscimed.2004.11.040. [DOI] [PubMed] [Google Scholar]
- 92.Passel J, Cohn D, Gonzalez-Barrera A. Net migration from Mexico fall to zero—and perhaps less: II. Migration between the US and Mexico. 2012. Available at: http://www.pewhispanic.org/2012/04/23/ii-migration-between-the-u-s-and-mexico. Accessed December 16, 2013.
- 93.Berry JW. Acculturation and adaptation in a new society. Int Migr. 1992;30(suppl s1):69–85. [Google Scholar]
- 94.Boas F. The aims of ethnology. In: Boas F, editor. Race, Language, and Culture. New York, NY: Macmillan; 1888. pp. 628–638. [Google Scholar]
- 95.Olmedo EL. Acculturation: a psychometric perspective. Am Psychol. 1979;34(11):1061–1070. [Google Scholar]
- 96.Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. Soc Sci Med. 2009;69(7):983–991. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 97.Wallace PM, Pomery EA, Latimer AE, Martinez JL, Salovey P. A review of acculturation measures and their utility in studies promoting Latino health. Hisp J Behav Sci. 2010;32(1):37–54. doi: 10.1177/0739986309352341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Graves TD. Psychological acculturation in a tri-ethnic community. Southwest J Anthropol. 1967;23(4):337–350. [Google Scholar]
- 99.Thurnwald R. The psychology of acculturation. Am Anthropol. 1932;34(4):557–569. [Google Scholar]
- 100.Berry JW. Psychology of acculturation. In: Brislin RW, editor. Applied Cross-Cultural Psychology. Vol. 14. Newbury Park, CA: SAGE Publications; 1990. pp. 232–253. [Google Scholar]
- 101.Abraído-Lanza AF, Armbrister AN, Flórez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. Am J Public Health. 2006;96(8):1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Berry JW. Acculturation and Health: Theory and Research. New York, NY: Oxford University Press; 1998. [Google Scholar]
- 103.Yoon E, Chang C-T, Kim S et al. A meta-analysis of acculturation/enculturation and mental health. J Couns Psychol. 2013;60(1):15–30. doi: 10.1037/a0030652. [DOI] [PubMed] [Google Scholar]
- 104.Cuéllar I, Arnold B, Gonzalez G. Cognitive referents of acculturation: assessment of cultural constructs in Mexican Americans. J Community Psychol. 1995;23(4):339–356. [Google Scholar]
- 105.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9(2):183–205. [Google Scholar]
- 106.Barona A, Miller JA. Short Acculturation Scale for Hispanic Youth (SASH-Y): a preliminary report. Hisp J Behav Sci. 1994;16(2):155–162. [Google Scholar]
- 107.Cuellar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans-II: a revision of the original ARSMA scale. Hisp J Behav Sci. 1995;17(3):275–304. [Google Scholar]
- 108.Szapocznik J, Kurtines WM, Fernandez T. Bicultural involvement and adjustment in Hispanic-American youths. Int J Intercult Relat. 1980;4(3–4):353–365. [Google Scholar]
- 109.Berry JW. Immigration, acculturation, and adaptation. Appl Psychol. 1997;46(1):5–34. [Google Scholar]
- 110.Oetting ER, Beauvais F. Orthogonal cultural identification theory: the cultural identification of minority adolescents. Int J Addict. 1990–1991;25(5A–6A):655–685. doi: 10.3109/10826089109077265. [DOI] [PubMed] [Google Scholar]
- 111.Burnam MA, Telles CA, Karno M, Hough RL, Escobar JI. Measurement of acculturation in a community population of Mexican Americans. Hisp J Behav Sci. 1987;9(2):105–130. [Google Scholar]
- 112.Hunt LM, Schneider S, Comer B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Soc Sci Med. 2004;59(5):973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 113.Ward C, Kus L. Back to and beyond Berry’s basics: the conceptualization, operationalization and classification of acculturation. Int J Intercult Relat. 2012;36(4):472–485. [Google Scholar]
- 114.Rudmin F. Constructs, measurements and models of acculturation and acculturative stress. Int J Intercult Relat. 2009;33(2):106–123. [Google Scholar]
- 115.Lopez-Class M, Castro FG, Ramirez AG. Conceptions of acculturation: a review and statement of critical issues. Soc Sci Med. 2011;72(9):1555–1562. doi: 10.1016/j.socscimed.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 116.Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. Am Psychol. 2010;65(4):237–251. doi: 10.1037/a0019330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Berry JW. Conceptual approaches to acculturation. In: Chun KM, Balls Organista P, Marín G, editors. Acculturation: Advances in Theory, Measurement, and Applied Research. Washington, DC: American Psychological Association; 2003. pp. 17–37. [Google Scholar]
- 118.Smokowski PR, Bacallao ML. Acculturation, internalizing mental health symptoms, and self-esteem: cultural experiences of Latino adolescents in North Carolina. Child Psychiatry Hum Dev. 2007;37(3):273–292. doi: 10.1007/s10578-006-0035-4. [DOI] [PubMed] [Google Scholar]
- 119.Torres L, Rollock D. Psychological impact of negotiating two cultures: Latino coping and self-esteem. J Multicult Couns Devel. 2009;37(4):219–228. [Google Scholar]
- 120.Bacallao ML, Smokowski PR. Entre dos mundos/between two worlds: bicultural development in context. J Prim Prev. 2009;30(3–4):421–451. doi: 10.1007/s10935-009-0176-x. [DOI] [PubMed] [Google Scholar]
- 121.Phinney JS, Horenczyk G, Liebkind K, Vedder P. Ethnic identity, immigration, and well-being: an interactional perspective. J Soc Issues. 2001;57(3):493–510. [Google Scholar]
- 122.Romero AJ, Roberts RE. Stress within a bicultural context for adolescents of Mexican descent. Cultur Divers Ethnic Minor Psychol. 2003;9(2):171–184. doi: 10.1037/1099-9809.9.2.171. [DOI] [PubMed] [Google Scholar]
- 123.Rotheram-Borus MJ. Adolescents’ reference-group choices, self-esteem, and adjustment. J Pers Soc Psychol. 1990;59(5):1075–1081. doi: 10.1037//0022-3514.59.5.1075. [DOI] [PubMed] [Google Scholar]
- 124.Acevedo-Garcia D, Bates LM. Latino health paradoxes: empirical evidence, explanations, future research, and implications. In: Rodriguez H, Saenz R, Menjivar C, editors. Latinas/os in the United States: Changing the Face of America. New York, NY: Springer; 2008. pp. 101–113. [Google Scholar]
- 125.Cabassa LJ. Measuring acculturation: where we are and where we need to go. Hisp J Behav Sci. 2003;25(2):127–146. [Google Scholar]
- 126.Alegria M, Shrout PE, Woo M et al. Understanding differences in past year psychiatric disorders for Latinos living in the US. Soc Sci Med. 2007;65(2):214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Allen ML, Elliott MN, Fuligni AJ, Morales LS, Hambarsoomian K, Schuster MA. The relationship between Spanish language use and substance use behaviors among Latino youth: a social network approach. J Adolesc Health. 2008;43(4):372–379. doi: 10.1016/j.jadohealth.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Caetano R, Ramisetty-Mikler S, Wallisch LS, McGrath C, Spence RT. Acculturation, drinking, and alcohol abuse and dependence among Hispanics in the Texas–Mexico border. Alcohol Clin Exp Res. 2008;32(2):314–321. doi: 10.1111/j.1530-0277.2007.00576.x. [DOI] [PubMed] [Google Scholar]
- 129.Hiott A, Grzywacz JG, Arcury TA, Quandt SA. Gender differences in anxiety and depression among immigrant Latinos. Fam Syst Health. 2006;24(2):137–146. doi: 10.1037/1091-7527.24.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hovey JD, Magaña CG. Psychosocial predictors of anxiety among immigrant Mexican migrant farmworkers: implications for prevention and treatment. Cultur Divers Ethnic Minor Psychol. 2002;8(3):274–289. doi: 10.1037/1099-9809.8.3.274. [DOI] [PubMed] [Google Scholar]
- 131.Hovey JD, Magaña C. Acculturative stress, anxiety, and depression among Mexican immigrant farmworkers in the Midwest United States. J Immigr Health. 2000;2(3):119–131. doi: 10.1023/A:1009556802759. [DOI] [PubMed] [Google Scholar]
- 132.Hovey JD, King CA. Acculturative stress, depression, and suicidal ideation among immigrant and second-generation Latino adolescents. J Am Acad Child Adolesc Psychiatry. 1996;35(9):1183–1192. doi: 10.1097/00004583-199609000-00016. [DOI] [PubMed] [Google Scholar]
- 133.Krause N, Goldenhar LM. Acculturation and psychological distress in three groups of elderly Hispanics. J Gerontol. 1992;47(6):S279–S288. doi: 10.1093/geronj/47.6.s279. [DOI] [PubMed] [Google Scholar]
- 134.West SK, Munoz B, Klein R et al. Risk factors for type II diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Am J Ophthalmol. 2002;134(3):390–398. doi: 10.1016/s0002-9394(02)01595-7. [DOI] [PubMed] [Google Scholar]
- 135.Burnam MA, Hough RL, Karno M, Escobar JI, Telles CA. Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. J Health Soc Behav. 1987;28(1):89–102. [PubMed] [Google Scholar]
- 136.Kaplan MS, Marks G. Adverse effects of acculturation: psychological distress among Mexican American young adults. Soc Sci Med. 1990;31(12):1313–1319. doi: 10.1016/0277-9536(90)90070-9. [DOI] [PubMed] [Google Scholar]
- 137.Turner RJ, Gil AG. Psychiatric and substance use disorders in South Florida: racial/ethnic and gender contrasts in a young adult cohort. Arch Gen Psychiatry. 2002;59(1):43–50. doi: 10.1001/archpsyc.59.1.43. [DOI] [PubMed] [Google Scholar]
- 138.Harris MI. Epidemiological correlates of NIDDM in Hispanics, whites, and blacks in the US population. Diabetes Care. 1991;14(7):639–648. doi: 10.2337/diacare.14.7.639. [DOI] [PubMed] [Google Scholar]
- 139.Kieffer EC, Martin JA, Herman WH. Impact of maternal nativity on the prevalence of diabetes during pregnancy among US ethnic groups. Diabetes Care. 1999;22(5):729–735. doi: 10.2337/diacare.22.5.729. [DOI] [PubMed] [Google Scholar]
- 140.Markides KS, Coreil J, Ray LA. Smoking among Mexican Americans: a three-generation study. Am J Public Health. 1987;77(6):708–711. doi: 10.2105/ajph.77.6.708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kelaher M, Jessop DJ. Differences in low-birthweight among documented and undocumented foreign-born and US-born Latinas. Soc Sci Med. 2002;55(12):2171–2175. doi: 10.1016/s0277-9536(01)00360-4. [DOI] [PubMed] [Google Scholar]
- 142.Balcazar H, Krull J. Determinants of birth-weight outcomes among Mexican-American women: examining conflicting results about acculturation. Ethn Dis. 1999;9(3):410–422. [PubMed] [Google Scholar]
- 143.English PB, Kharrazi M, Guendelman S. Pregnancy outcomes and risk factors in Mexican Americans: the effect of language use and mother’s birthplace. Ethn Dis. 1997;7(3):229–240. [PubMed] [Google Scholar]
- 144.Wolff CB, Portis M. Smoking, acculturation, and pregnancy outcome among Mexican Americans. Health Care Women Int. 1996;17(6):563–573. [PubMed] [Google Scholar]
- 145.Epstein JA, Doyle M, Botvin GJ. A mediational model of the relationship between linguistic acculturation and polydrug use among Hispanic adolescents. Psychol Rep. 2003;93(3 pt 1):859–866. doi: 10.2466/pr0.2003.93.3.859. [DOI] [PubMed] [Google Scholar]
- 146.Campos B, Schetter CD, Abdou CM, Hobel CJ, Glynn LM, Sandman CA. Familialism, social support, and stress: positive implications for pregnant Latinas. Cultur Divers Ethnic Minor Psychol. 2008;14(2):155–162. doi: 10.1037/1099-9809.14.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.González HM, Haan MN, Hinton L. Acculturation and the prevalence of depression in older Mexican Americans: baseline results of the Sacramento Area Latino Study on Aging. J Am Geriatr Soc. 2001;49(7):948–953. doi: 10.1046/j.1532-5415.2001.49186.x. [DOI] [PubMed] [Google Scholar]
- 148.Ruiz RJ, Dolbier CL, Fleschler R. The relationships among acculturation, biobehavioral risk, stress, corticotropin-releasing hormone, and poor birth outcomes in Hispanic women. Ethn Dis. 2006;16(4):926–932. [PubMed] [Google Scholar]
- 149.Ventura SJ, Taffel SM. Childbearing characteristics of US- and foreign-born Hispanic mothers. Public Health Rep. 1985;100(6):647–652. [PMC free article] [PubMed] [Google Scholar]
- 150.Brown HL, Chireau MV, Jallah Y, Howard D. The “Hispanic paradox”: an investigation of racial disparity in pregnancy outcomes at a tertiary care medical center. Am J Obstet Gynecol. 2007;197(2):197.e1–197.e7. doi: 10.1016/j.ajog.2007.04.036. [DOI] [PubMed] [Google Scholar]
- 151.Cervantes A, Keith L, Wyshak G. Adverse birth outcomes among native-born and immigrant women: replicating national evidence regarding Mexicans at the local level. Matern Child Health J. 1999;3(2):99–109. doi: 10.1023/a:1021805427469. [DOI] [PubMed] [Google Scholar]
- 152.Rosenberg TJ, Raggio TP, Chiasson MA. A further examination of the “epidemiologic paradox”: birth outcomes among Latinas. J Natl Med Assoc. 2005;97(4):550–556. [PMC free article] [PubMed] [Google Scholar]
- 153.Engel T, Alexander GR, Leland NL. Pregnancy outcomes of US-born Puerto Ricans: the role of maternal nativity status. Am J Prev Med. 1995;11(1):34–39. [PubMed] [Google Scholar]
- 154.Acevedo-Garcia D, Soobader M-J, Berkman LF. Low birthweight among US Hispanic/Latino subgroups: the effect of maternal foreign-born status and education. Soc Sci Med. 2007;65(12):2503–2516. doi: 10.1016/j.socscimed.2007.06.033. [DOI] [PubMed] [Google Scholar]
- 155.Flores ME, Simonsen SE, Manuck TA, Dyer JM, Turok DK. The “Latina epidemiologic paradox”: contrasting patterns of adverse birth outcomes in US-born and foreign-born Latinas. Womens Health Issues. 2012;22(5):e501–e507. doi: 10.1016/j.whi.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 156.Powers DA. Paradox revisited: a further investigation of racial/ethnic differences in infant mortality by maternal age. Demography. 2013;50(2):495–520. doi: 10.1007/s13524-012-0152-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Frisbie WP, Forbes D, Hummer RA. Hispanic pregnancy outcomes: additional evidence. Soc Sci Q. 1998;79(1):149–169. [Google Scholar]
- 158.Hummer RA, Biegler M, De Turk PB et al. Race/ethnicity, nativity, and infant mortality in the United States. Soc Forces. 1999;77(3):1083–1117. [Google Scholar]
- 159.Lara M, Gamboa C, Kahramanian MI, Morales LS, Hayes Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Khan LK, Sobal J, Martorell R. Acculturation, socioeconomic status, and obesity in Mexican Americans, Cuban Americans, and Puerto Ricans. Int J Obes Relat Metab Disord. 1997;21(2):91–96. doi: 10.1038/sj.ijo.0800367. [DOI] [PubMed] [Google Scholar]
- 161.Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc Sci Med. 2003;57(11):2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 162.Krueger PM, Coleman-Minahan K, Rooks RN. Race/ethnicity, nativity and trends in BMI among US adults. Obesity. 2014;22(7):1739–1746. doi: 10.1002/oby.20744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Antecol H, Bedard K. Unhealthy assimilation: why do immigrants converge to American health status levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- 164.Kaushal N. Adversities of acculturation? Prevalence of obesity among immigrants. Health Econ. 2009;18(3):291–303. doi: 10.1002/hec.1368. [DOI] [PubMed] [Google Scholar]
- 165.Park Y, Neckerman KM, Quinn J, Weiss C, Rundle A. Place of birth, duration of residence, neighborhood immigrant composition and body mass index in New York City. Int J Behav Nutr Phys Act. 2008;5(1):19. doi: 10.1186/1479-5868-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sanchez-Vaznaugh EV, Kawachi I, Subramanian S, Sánchez BN, Acevedo-Garcia D. Differential effect of birthplace and length of residence on body mass index (BMI) by education, gender and race/ethnicity. Soc Sci Med. 2008;67(8):1300–1310. doi: 10.1016/j.socscimed.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 167.Bates LM, Acevedo-Garcia D, Alegria M, Krieger N. Immigration and generational trends in body mass index and obesity in the United States: results of the National Latino and Asian American Survey, 2002–2003. Am J Public Health. 2008;98(1):70–77. doi: 10.2105/AJPH.2006.102814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Popkin BM, Udry JR. Adolescent obesity increases significantly in second and third generation US immigrants: the National Longitudinal Study of Adolescent Health. J Nutr. 1998;128(4):701–706. doi: 10.1093/jn/128.4.701. [DOI] [PubMed] [Google Scholar]
- 169.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican–American women and men. Int J Epidemiol. 2000;29(3):470–477. [PubMed] [Google Scholar]
- 170.Liu J, Probst JC, Harun N, Bennett KJ, Torres ME. Acculturation, physical activity, and obesity among Hispanic adolescents. Ethn Health. 2009;14(5):509–525. doi: 10.1080/13557850902890209. [DOI] [PubMed] [Google Scholar]
- 171.Yeh M-C, Viladrich A, Bruning N, Roye C. Determinants of Latina obesity in the United States: the role of selective acculturation. J Transcult Nurs. 2009;20(1):105–115. doi: 10.1177/1043659608325846. [DOI] [PubMed] [Google Scholar]
- 172.Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009;124(suppl 3):S163–S175. doi: 10.1542/peds.2009-1100D. [DOI] [PubMed] [Google Scholar]
- 173.Braveman PA, Egerter SA, Mockenhaupt RE. Broadening the focus: the need to address the social determinants of health. Am J Prev Med. 2011;40(1):S4–S18. doi: 10.1016/j.amepre.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 174.Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1186(1):69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Hertzman C. The biological embedding of early experience and its effects on health in adulthood. Ann N Y Acad Sci. 1999;896(1):85–95. doi: 10.1111/j.1749-6632.1999.tb08107.x. [DOI] [PubMed] [Google Scholar]
- 176.Adler NE, Stewart J. Preface to the biology of disadvantage: socioeconomic status and health. Ann N Y Acad Sci. 2010;1186(1):1–4. doi: 10.1111/j.1749-6632.2009.05385.x. [DOI] [PubMed] [Google Scholar]
- 177.Aldrich L, Variyam JN. Acculturation erodes the diet quality of US Hispanics. Food Review. 2000;23(1):51–55. [Google Scholar]
- 178.Bermúdez OI, Falcón L, Tucker K. Intake and food sources of macronutrients among older Hispanic adults: association with ethnicity, acculturation, and length of residence in the United States. J Am Diet Assoc. 2000;100(6):665–673. doi: 10.1016/s0002-8223(00)00195-4. [DOI] [PubMed] [Google Scholar]
- 179.Marks G, Garcia M, Solis JM. Health risk behaviors of Hispanics in the United States: findings from HHANES, 1982-84. Am J Public Health. 1990;80(suppl):20–26. doi: 10.2105/ajph.80.suppl.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Otero-Sabogal R, Sabogal F, Perez-Stable EJ, Hiatt RA. Dietary practices, alcohol consumption, and smoking behavior: ethnic, sex, and acculturation differences. J Natl Cancer Inst Monogr. 1995;(18):73–82. [PubMed] [Google Scholar]
- 181.Dixon LB, Sundquist J, Winkleby M. Differences in energy, nutrient, and food intakes in a US sample of Mexican-American women and men: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol. 2000;152(6):548–557. doi: 10.1093/aje/152.6.548. [DOI] [PubMed] [Google Scholar]
- 182.Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22(1):23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 183.MacDonald JM, Nelson PE., Jr Do the poor still pay more? Food price variations in large metropolitan areas. J Urban Econ. 1991;30(3):344–359. [Google Scholar]
- 184.Neuhouser ML, Thompson B, Coronado GD, Solomon CC. Higher fat intake and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington state. J Am Diet Assoc. 2004;104(1):51–57. doi: 10.1016/j.jada.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 185.Mazur RE, Marquis GS, Jensen HH. Diet and food insufficiency among Hispanic youths: acculturation and socioeconomic factors in the Third National Health and Nutrition Examination Survey. Am J Clin Nutr. 2003;78(6):1120–1127. doi: 10.1093/ajcn/78.6.1120. [DOI] [PubMed] [Google Scholar]
- 186.Coonrod DV, Balcazar H, Brady J, Garcia S, Van Tine M. Smoking, acculturation and family cohesion in Mexican-American women. Ethn Dis. 1999;9(3):434–440. [PubMed] [Google Scholar]
- 187.Coreil J, Ray LA, Markides KS. Predictors of smoking among Mexican-Americans: findings from the Hispanic HANES. Prev Med. 1991;20(4):508–517. doi: 10.1016/0091-7435(91)90048-9. [DOI] [PubMed] [Google Scholar]
- 188.Marín G, Posner SF. The role of gender and acculturation on determining the consumption of alcoholic beverages among Mexican-Americans and Central Americans in the United States. Int J Addict. 1995;30(7):779–794. doi: 10.3109/10826089509067007. [DOI] [PubMed] [Google Scholar]
- 189.Markides KS, Ray LA, Stroup-Benham CA, Treviño F. Acculturation and alcohol consumption in the Mexican American population of the southwestern United States: findings from HHANES 1982-84. Am J Public Health. 1990;80(suppl):42–46. doi: 10.2105/ajph.80.suppl.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Cherpitel CJ, Borges G. Substance use among emergency room patients: an exploratory analysis by ethnicity and acculturation. Am J Drug Alcohol Abuse. 2002;28(2):287–305. doi: 10.1081/ada-120002975. [DOI] [PubMed] [Google Scholar]
- 191.Gfroerer J, De La Rosa M. Protective and risk factors associated with drug use among Hispanic youth. J Addict Dis. 1993;12(2):87–107. doi: 10.1300/J069v12n02_07. [DOI] [PubMed] [Google Scholar]
- 192.Gfroerer JC, Tan LL. Substance use among foreign-born youths in the United States: does the length of residence matter? Am J Public Health. 2003;93(11):1892–1895. doi: 10.2105/ajph.93.11.1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Velez CN, Ungemack JA. Drug use among Puerto Rican youth: an exploration of generational status differences. Soc Sci Med. 1989;29(6):779–789. doi: 10.1016/0277-9536(89)90158-5. [DOI] [PubMed] [Google Scholar]
- 194.Amaro H, Whitaker R, Coffman G, Heeren T. Acculturation and marijuana and cocaine use: findings from HHANES 1982-84. Am J Public Health. 1990;80(suppl):54–60. doi: 10.2105/ajph.80.suppl.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Vega WA, Alderete E, Kolody B, Aguilar-Gaxiola S. Illicit drug use among Mexicans and Mexican Americans in California: the effects of gender and acculturation. Addiction. 1998;93(12):1839–1850. doi: 10.1046/j.1360-0443.1998.931218399.x. [DOI] [PubMed] [Google Scholar]
- 196.Hale L, Rivero-Fuentes E. Negative acculturation in sleep duration among Mexican immigrants and Mexican Americans. J Immigr Minor Health. 2011;13(2):402–407. doi: 10.1007/s10903-009-9284-1. [DOI] [PubMed] [Google Scholar]
- 197.Kachikis AB, Breitkopf CR. Predictors of sleep characteristics among women in southeast Texas. Womens Health Issues. 2012;22(1):e99–e109. doi: 10.1016/j.whi.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Ebin VJ, Sneed CD, Morisky DE, Rotheram-Borus MJ, Magnusson AM, Malotte CK. Acculturation and interrelationships between problem and health-promoting behaviors among Latino adolescents. J Adolesc Health. 2001;28(1):62–72. doi: 10.1016/s1054-139x(00)00162-2. [DOI] [PubMed] [Google Scholar]
- 199.Ehlers CL, Gilder DA, Criado JR, Caetano R. Sleep quality and alcohol-use disorders in a select population of young-adult Mexican Americans. J Stud Alcohol Drugs. 2010;71(6):879–884. doi: 10.15288/jsad.2010.71.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethn Dis. 2006;16(1):16–21. [PubMed] [Google Scholar]
- 201.Roberts RE, Lee E, Hemandez M, Solari AC. Symptoms of insomnia among adolescents in the lower Rio Grande Valley of Texas. Sleep. 2004;27(4):751–760. doi: 10.1093/sleep/27.4.751. [DOI] [PubMed] [Google Scholar]
- 202.Barcenas CH, Wilkinson AV, Strom SS et al. Birthplace, years of residence in the United States, and obesity among Mexican-American adults. Obesity (Silver Spring) 2007;15(4):1043–1052. doi: 10.1038/oby.2007.537. [DOI] [PubMed] [Google Scholar]
- 203.Crespo CJ, Smit E, Carter-Pokras O, Andersen R. Acculturation and leisure-time physical inactivity in Mexican American adults: results from NHANES III, 1988–1994. Am J Public Health. 2001;91(8):1254–1257. doi: 10.2105/ajph.91.8.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Evenson KR, Sarmiento OL, Ayala GX. Acculturation and physical activity among North Carolina Latina immigrants. Soc Sci Med. 2004;59(12):2509–2522. doi: 10.1016/j.socscimed.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 205.Cantero PJ, Richardson JL, Baezconde-Garbanati L, Marks G. The association between acculturation and health practices among middle-aged and elderly Latinas. Ethn Dis. 1999;9(2):166–180. [PubMed] [Google Scholar]
- 206.Pérez-Stable EJ, Marín G, Marín BV. Behavioral risk factors: a comparison of Latinos and non-Latino Whites in San Francisco. Am J Public Health. 1994;84(6):971–976. doi: 10.2105/ajph.84.6.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 208.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119(3):488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 209.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 210.Finch BK, Vega WA. Acculturation stress, social support, and self-rated health among Latinos in California. J Immigr Health. 2003;5(3):109–117. doi: 10.1023/a:1023987717921. [DOI] [PubMed] [Google Scholar]
- 211.Griffith J, Villavicencio S. Relationships among acculturation, sociodemographic characteristics and social supports in Mexican American adults. Hisp J Behav Sci. 1985;7(1):75–92. [Google Scholar]
- 212.Sabogal F, Marín G, Otero-Sabogal R, Marín BV, Perez-Stable EJ. Hispanic familism and acculturation: what changes and what doesn’t? Hisp J Behav Sci. 1987;9(4):397–412. [Google Scholar]
- 213.Rivera FI, Guarnaccia PJ, Mulvaney-Day N, Lin JY, Torres M, Alegria M. Family cohesion and its relationship to psychological distress among Latino groups. Hisp J Behav Sci. 2008;30(3):357–378. doi: 10.1177/0739986308318713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Cervantes RC, Padilla AM, Napper LE, Goldbach JT. Acculturation-related stress and mental health outcomes among three generations of Hispanic adolescents. Hisp J Behav Sci. 2013;35(4):451–468. [Google Scholar]
- 215.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896(1):173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 216.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 217.Chrousos GP, Gold PW. The concepts of stress and stress system disorders: overview of physical and behavioral homeostasis. JAMA. 1992;267(9):1244–1252. [PubMed] [Google Scholar]
- 218.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 219.Heinrichs M, Baumgartner T, Kirschbaum C, Ehlert U. Social support and oxytocin interact to suppress cortisol and subjective responses to psychosocial stress. Biol Psychiatry. 2003;54(12):1389–1398. doi: 10.1016/s0006-3223(03)00465-7. [DOI] [PubMed] [Google Scholar]
- 220.Kudielka BM, Buske-Kirschbaum A, Hellhammer DH, Kirschbaum C. HPA axis responses to laboratory psychosocial stress in healthy elderly adults, younger adults, and children: impact of age and gender. Psychoneuroendocrinology. 2004;29(1):83–98. doi: 10.1016/s0306-4530(02)00146-4. [DOI] [PubMed] [Google Scholar]
- 221.Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5(3):243–251. doi: 10.1038/nri1571. [DOI] [PubMed] [Google Scholar]
- 222.Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130(4):601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Epel ES, Blackburn EH, Lin J et al. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci U S A. 2004;101(49):17312–17315. doi: 10.1073/pnas.0407162101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Irie M, Asami S, Nagata S, Miyata M, Kasai H. Relationships between perceived workload, stress and oxidative DNA damage. Int Arch Occup Environ Health. 2001;74(2):153–157. doi: 10.1007/s004200000209. [DOI] [PubMed] [Google Scholar]
- 225.Farley T, Galves A, Dickinson LM, Perez Mde J. Stress, coping, and health: a comparison of Mexican immigrants, Mexican-Americans, and non-Hispanic whites. J Immigr Health. 2005;7(3):213–220. doi: 10.1007/s10903-005-3678-5. [DOI] [PubMed] [Google Scholar]
- 226.Mangold D, Mintz J, Javors M, Marino E. Neuroticism, acculturation and the cortisol awakening response in Mexican American adults. Horm Behav. 2012;61(1):23–30. doi: 10.1016/j.yhbeh.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Berry JW, Kim U, Minde T, Mok D. Comparative studies of acculturative stress. Int Migr Rev. 1987;21(3):491–511. [Google Scholar]
- 228.Cervantes RC, Padilla AM, Salgado de Snyder N. The Hispanic Stress Inventory: a culturally relevant approach to psychosocial assessment. Psychol Assess. 1991;3(3):438–447. [Google Scholar]
- 229.Thoman LV, Surís A. Acculturation and acculturative stress as predictors of psychological distress and quality-of-life functioning in Hispanic psychiatric patients. Hisp J Behav Sci. 2004;26(3):293–311. [Google Scholar]
- 230.Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. J Health Soc Behav. 2000;41(3):295–313. [PubMed] [Google Scholar]
- 231.Salgado de Snyder VN, Cervantes RC, Padilla AM. Gender and ethnic differences in psychosocial stress and generalized distress among Hispanics. Sex Roles. 1990;22(7–8):441–453. [Google Scholar]
- 232.Flores E, Tschann JM, Dimas JM, Bachen EA, Pasch LA, de Groat CL. Perceived discrimination, perceived stress, and mental and physical health among Mexican-origin adults. Hisp J Behav Sci. 2008;30(4):401–424. [Google Scholar]
- 233.Nakash O, Nagar M, Shoshani A, Zubida H, Harper RA. The effect of acculturation and discrimination on mental health symptoms and risk behaviors among adolescent migrants in Israel. Cultur Divers Ethnic Minor Psychol. 2012;18(3):228–238. doi: 10.1037/a0027659. [DOI] [PubMed] [Google Scholar]
- 234.Escobar JI. Immigration and mental health: why are immigrants better off? Arch Gen Psychiatry. 1998;55(9):781–782. doi: 10.1001/archpsyc.55.9.781. [DOI] [PubMed] [Google Scholar]
- 235.Concha M, Sanchez M, de La Rosa M, Villar ME. A longitudinal study of social capital and acculturation-related stress among recent Latino immigrants in south Florida. Hisp J Behav Sci. 2013;35(4):469–485. doi: 10.1177/0739986313499005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Pérez MC, Fortuna L. Psychosocial stressors, psychiatric diagnoses and utilization of mental health services among undocumented immigrant Latinos. J Immigr Refugee Serv. 2005;3(1–2):107–123. [Google Scholar]
- 237.Rodriguez R, DeWolfe A. Psychological distress among Mexican-American and Mexican women as related to status on the new immigration law. J Consult Clin Psychol. 1990;58(5):548–553. doi: 10.1037//0022-006x.58.5.548. [DOI] [PubMed] [Google Scholar]
- 238.Sullivan MM, Rehm R. Mental health of undocumented Mexican immigrants: a review of the literature. ANS Adv Nurs Sci. 2005;28(3):240–251. doi: 10.1097/00012272-200507000-00006. [DOI] [PubMed] [Google Scholar]
- 239.Gonzales RG. Learning to be illegal: undocumented youth and shifting legal contexts in the transition to adulthood. Am Sociol Rev. 2011;76(4):602–619. [Google Scholar]
- 240.Arbona C, Olvera N, Rodriguez N, Hagan J, Linares A, Wiesner M. Acculturative stress among documented and undocumented Latino immigrants in the United States. Hisp J Behav Sci. 2010;32(3):362–384. doi: 10.1177/0739986310373210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Umaña-Taylor AJ, Updegraff KA. Latino adolescents’ mental health: exploring the interrelations among discrimination, ethnic identity, cultural orientation, self-esteem, and depressive symptoms. J Adolesc. 2007;30(4):549–567. doi: 10.1016/j.adolescence.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 242.Cornelius WA. Ambivalent reception: mass public responses to the “new” Latino immigration to the United States. In: Suárez-Orozco M, Páez M, editors. Latinos: Remaking America. Berkeley, CA: University of California Press; 2002. pp. 165–189. [Google Scholar]
- 243.Benner AD, Graham S. Latino adolescents’ experiences of discrimination across the first 2 years of high school: correlates and influences on educational outcomes. Child Dev. 2011;82(2):508–519. doi: 10.1111/j.1467-8624.2010.01524.x. [DOI] [PubMed] [Google Scholar]
- 244.Córdova D, Jr, Cervantes RC. Intergroup and within-group perceived discrimination among US-born and foreign-born Latino youth. Hisp J Behav Sci. 2010;32(2):259–274. [Google Scholar]
- 245.Peek MK, Cutchin MP, Salinas JJ et al. Allostatic load among non-Hispanic Whites, non-Hispanic Blacks, and people of Mexican origin: effects of ethnicity, nativity, and acculturation. Am J Public Health. 2010;100(5):940–946. doi: 10.2105/AJPH.2007.129312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Mangold D, Wand G, Javors M, Mintz J. Acculturation, childhood trauma and the cortisol awakening response in Mexican–American adults. Horm Behav. 2010;58(4):637–646. doi: 10.1016/j.yhbeh.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117(1):43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 248.Abraído-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89(10):1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): infant mortality among the Mexican-origin population in the United States. Demography. 2007;44(3):441–457. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.McGlade MS, Saha S, Dahlstrom ME. The Latina paradox: an opportunity for restructuring prenatal care delivery. Am J Public Health. 2004;94(12):2062–2065. doi: 10.2105/ajph.94.12.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Hazuda HP, Stern MP, Haffner SM. Acculturation and assimilation among Mexican Americans: scales and population-based data. Soc Sci Q. 1988;69(3):687–706. [Google Scholar]
- 252.Barker DJ, Eriksson JG, Forsen T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol. 2002;31(6):1235–1239. doi: 10.1093/ije/31.6.1235. [DOI] [PubMed] [Google Scholar]
- 253.Wadhwa PD, Buss C, Entringer S, Swanson JM. Developmental origins of health and disease: brief history of the approach and current focus on epigenetic mechanisms. Semin Reprod Med. 2009;27(5):358–368. doi: 10.1055/s-0029-1237424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Shalev I, Entringer S, Wadhwa PD et al. Stress and telomere biology: a lifespan perspective. Psychoneuroendocrinology. 2013;38(9):1835–1842. doi: 10.1016/j.psyneuen.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Swanson JM, Entringer S, Buss C, Wadhwa PD. Developmental origins of health and disease: environmental exposures. Semin Reprod Med. 2009;27(5):391–402. doi: 10.1055/s-0029-1237427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Entringer S, Kumsta R, Hellhammer DH, Wadhwa PD, Wüst S. Prenatal exposure to maternal psychosocial stress and HPA axis regulation in young adults. Horm Behav. 2009;55(2):292–298. doi: 10.1016/j.yhbeh.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 257.Entringer S, Kumsta R, Nelson EL, Hellhammer DH, Wadhwa PD, Wüst S. Influence of prenatal psychosocial stress on cytokine production in adult women. Dev Psychobiol. 2008;50(6):579–587. doi: 10.1002/dev.20316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Entringer S, Wüst S, Kumsta R et al. Prenatal psychosocial stress exposure is associated with insulin resistance in young adults. Am J Obstet Gynecol. 2008;199(5):498.e1–498.e7. doi: 10.1016/j.ajog.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Buss C, Entringer S, Wadhwa PD. Fetal programming of brain development: intrauterine stress and susceptibility to psychopathology. Sci Signal. 2012;5(245) doi: 10.1126/scisignal.2003406. pt7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Entringer S, Buss C, Kumsta R, Hellhammer DH, Wadhwa PD, Wüst S. Prenatal psychosocial stress exposure is associated with subsequent working memory performance in young women. Behav Neurosci. 2009;123(4):886–893. doi: 10.1037/a0016265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Entringer S, Buss C, Wadhwa PD. Prenatal stress, telomere biology, and fetal programming of health and disease risk. Sci Signal. 2012;5(248) doi: 10.1126/scisignal.2003580. pt12. [DOI] [PubMed] [Google Scholar]
- 262.Entringer S, Epel ES, Kumsta R et al. Stress exposure in intrauterine life is associated with shorter telomere length in young adulthood. Proc Natl Acad Sci U S A. 2011;108(33):E513–E518. doi: 10.1073/pnas.1107759108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Entringer S, Buss C, Swanson JM et al. Fetal programming of body composition, obesity, and metabolic function: the role of intrauterine stress and stress biology. J Nutr Metab. 2012:632548. doi: 10.1155/2012/632548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Matthews SG. Antenatal glucocorticoids and programming of the developing CNS. Pediatr Res. 2000;47(3):291–300. doi: 10.1203/00006450-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 265.Trejo JL, Cuchillo I, Machín C, Rúa C. Maternal adrenalectomy at the early onset of gestation impairs the postnatal development of the rat hippocampal formation: effects on cell numbers and differentiation, connectivity and calbindin-D28k immunoreactivity. J Neurosci Res. 2000;62(5):644–667. doi: 10.1002/1097-4547(20001201)62:5<644::AID-JNR4>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 266.Ruiz RJ, Pickler RH, Marti CN, Jallo N. Family cohesion, acculturation, maternal cortisol, and preterm birth in Mexican-American women. Int J Womens Health. 2013;5:243–252. doi: 10.2147/IJWH.S42268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.D’Anna-Hernandez KL, Hoffman MC, Zerbe GO, Coussons-Read M, Ross RG, Laudenslager ML. Acculturation, maternal cortisol, and birth outcomes in women of Mexican descent. Psychosom Med. 2012;74(3):296–304. doi: 10.1097/PSY.0b013e318244fbde. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Fleuriet KJ, Sunil T. Perceived social stress, pregnancy-related anxiety, depression and subjective social status among pregnant Mexican and Mexican American women in south Texas. J Health Care Poor Underserved. 2014;25(2):546–561. doi: 10.1353/hpu.2014.0092. [DOI] [PubMed] [Google Scholar]
- 269.Nguyen HT, Clark M, Ruiz RJ. Effects of acculturation on the reporting of depressive symptoms among Hispanic pregnant women. Nurs Res. 2007;56(3):217–223. doi: 10.1097/01.NNR.0000270027.97983.96. [DOI] [PubMed] [Google Scholar]
- 270.Gluckman PD, Hanson MA. Living with the past: evolution, development, and patterns of disease. Science. 2004;305(5691):1733–1736. doi: 10.1126/science.1095292. [DOI] [PubMed] [Google Scholar]
- 271.Gluckman PD, Hanson MA. The developmental origins of health and disease. In: Wintour EM, Owens JA, editors. Early Life Origins of Health and Disease. New York, NY: Springer; 2006. pp. 1–5. [Google Scholar]
- 272.Gluckman PD, Low FM, Buklijas T, Hanson MA, Beedle AS. How evolutionary principles improve the understanding of human health and disease. Evol Appl. 2011;4(2):249–263. doi: 10.1111/j.1752-4571.2010.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Hanson M, Godfrey KM, Lillycrop KA, Burdge GC, Gluckman PD. Developmental plasticity and developmental origins of non-communicable disease: theoretical considerations and epigenetic mechanisms. Prog Biophys Mol Biol. 2011;106(1):272–280. doi: 10.1016/j.pbiomolbio.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 274.Merrill JE. Tumor necrosis factor alpha, interleukin 1 and related cytokines in brain development: normal and pathological. Dev Neurosci. 1992;14(1):1–10. doi: 10.1159/000111642. [DOI] [PubMed] [Google Scholar]
- 275.Cole TJ, Blendy JA, Monaghan AP et al. Targeted disruption of the glucocorticoid receptor gene blocks adrenergic chromaffin cell development and severely retards lung maturation. Genes Dev. 1995;9(13):1608–1621. doi: 10.1101/gad.9.13.1608. [DOI] [PubMed] [Google Scholar]
- 276.Zhao B, Schwartz JP. Involvement of cytokines in normal CNS development and neurological diseases: recent progress and perspectives. J Neurosci Res. 1998;52(1):7–16. doi: 10.1002/(SICI)1097-4547(19980401)52:1<7::AID-JNR2>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 277.Garbrecht MR, Klein JM, Schmidt TJ, Snyder JM. Glucocorticoid metabolism in the human fetal lung: implications for lung development and the pulmonary surfactant system. Biol Neonate. 2006;89(2):109–119. doi: 10.1159/000088653. [DOI] [PubMed] [Google Scholar]
- 278.Wadhwa PD. Psychoneuroendocrine processes in human pregnancy influence fetal development and health. Psychoneuroendocrinology. 2005;30(8):724–743. doi: 10.1016/j.psyneuen.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 279.Wadhwa PD, Entringer S, Buss C, Lu MC. The contribution of maternal stress to preterm birth: issues and considerations. Clin Perinatol. 2011;38(3):351–384. doi: 10.1016/j.clp.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Godfrey KM, Barker DJ. Fetal programming and adult health. Public Health Nutr. 2001;4(2B):611–624. doi: 10.1079/phn2001145. [DOI] [PubMed] [Google Scholar]
- 281.Wadhwa PD, Culhane JF, Rauh V, Barve SS. Stress and preterm birth: neuroendocrine, immune/inflammatory, and vascular mechanisms. Matern Child Health J. 2001;5(2):119–125. doi: 10.1023/a:1011353216619. [DOI] [PubMed] [Google Scholar]
- 282.Haynes SG, Harvey C, Montes H, Nickens H, Cohen BH. Patterns of cigarette smoking among Hispanics in the United States: results from HHANES 1982-84. Am J Public Health. 1990;80(suppl):47–53. doi: 10.2105/ajph.80.suppl.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Marin G, Perez-Stable EJ, Marin BV. Cigarette smoking among San Francisco Hispanics: the role of acculturation and gender. Am J Public Health. 1989;79(2):196–198. doi: 10.2105/ajph.79.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Black SA, Markides KS. Acculturation and alcohol consumption in Puerto Rican, Cuban-American, and Mexican-American women in the United States. Am J Public Health. 1993;83(6):890–893. doi: 10.2105/ajph.83.6.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Polednak AP. Gender and acculturation in relation to alcohol use among Hispanic (Latino) adults in two areas of the northeastern United States. Subst Use Misuse. 1997;32(11):1513–1524. doi: 10.3109/10826089709055875. [DOI] [PubMed] [Google Scholar]
- 286.Hamner HC, Cogswell ME, Johnson MA. Acculturation factors are associated with folate intakes among Mexican American women. J Nutr. 2011;141(10):1889–1897. doi: 10.3945/jn.111.143412. [DOI] [PubMed] [Google Scholar]
- 287.Marchetta CM, Hamner HC. Blood folate concentrations among women of childbearing age by race/ethnicity and acculturation, NHANES 2001-2010. Matern Child Nutr. 2014;28(1 suppl) doi: 10.1111/mcn.12134. 130.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Entringer S, Buss C, Andersen J, Chicz-DeMet A, Wadhwa PD. Ecological momentary assessment of maternal cortisol profiles over a multiple-day period predicts the length of human gestation. Psychosom Med. 2011;73(6):469–474. doi: 10.1097/PSY.0b013e31821fbf9a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Entringer S, Wadhwa PD. Developmental programming of obesity and metabolic dysfunction: role of prenatal stress and stress biology. Nestle Nutr Inst Workshop Ser. 2013;74:107–120. doi: 10.1159/000348454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Ceballos M, Palloni A. Maternal and infant health of Mexican immigrants in the USA: the effects of acculturation, duration, and selective return migration. Ethn Health. 2010;15(4):377–396. doi: 10.1080/13557858.2010.481329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Knickmeyer N, Sexton K, Nishimura N. The impact of same-sex friendships on the well-being of women: a review of the literature. Women Ther. 2002;25(1):37–59. [Google Scholar]
- 292.Sherraden MS, Barrera RE. Maternal support and cultural influences among Mexican immigrant mothers. Fam Soc. 1996;77(5):298–312. [Google Scholar]
- 293.Jones ME, Hughes ST, Jr, Bond ML. Predictors of birth outcome among Hispanic immigrant women. J Nurs Care Qual. 1999;14(1):56–62. doi: 10.1097/00001786-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 294.Callister LC, Birkhead A. Acculturation and perinatal outcomes in Mexican immigrant childbearing women: an integrative review. J Perinat Neonatal Nurs. 2002;16(3):22–38. doi: 10.1097/00005237-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 295.Laganá K. Come bien, camina y no se preocupe—eat right, walk, and do not worry: selective biculturalism during pregnancy in a Mexican American community. J Transcult Nurs. 2003;14(2):117–124. doi: 10.1177/1043659602250629. [DOI] [PubMed] [Google Scholar]
- 296.Breier BH, Vickers MH, Ikenasio BA, Chan KY, Wong WP. Fetal programming of appetite and obesity. Mol Cell Endocrinol. 2001;185(1–2):73–79. doi: 10.1016/s0303-7207(01)00634-7. [DOI] [PubMed] [Google Scholar]
- 297.Cripps RL, Martin-Gronert MS, Ozanne SE. Fetal and perinatal programming of appetite. Clin Sci (Lond) 2005;109(1):1–11. doi: 10.1042/CS20040367. [DOI] [PubMed] [Google Scholar]
- 298.Portha B, Chavey A, Movassat J. Early-life origins of type 2 diabetes: fetal programming of the beta-cell mass. Exp Diabetes Res. 2011;2011:105076. doi: 10.1155/2011/105076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Rees WD, McNeil CJ, Maloney CA. The roles of PPARs in the fetal origins of metabolic health and disease. PPAR Res. 2008;2008:459030. doi: 10.1155/2008/459030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Desai M, Ross MG. Fetal programming of adipose tissue: effects of IUGR and maternal obesity/high fat diet. Semin Reprod Med. 2011;29(3):237–245. doi: 10.1055/s-0031-1275517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Catalano PM, Presley L, Minium J, Hauguel-de Mouzon S. Fetuses of obese mothers develop insulin resistance in utero. Diabetes Care. 2009;32(6):1076–1080. doi: 10.2337/dc08-2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Guendelman S, English P, Chavez G. Infants of Mexican immigrants: health status of an emerging population. Med Care. 1995;33(1):41–52. doi: 10.1097/00005650-199501000-00004. [DOI] [PubMed] [Google Scholar]
- 303.Klinnert MD, Price MR, Liu AH, Robinson JL. Unraveling the ecology of risks for early childhood asthma among ethnically diverse families in the southwest. Am J Public Health. 2002;92(5):792–798. doi: 10.2105/ajph.92.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Mendoza F. Health risk profiles and race, culture and socioeconomic status. In: Pachter L, editor. Child Health in the Multicultural Environment. Report of the Thirty-First Ross Roundtable on Critical Approaches to Common Pediatric Problems. Columbus, OH: Ross Products Division, Abbott Labs; 2000. pp. 5–18. [Google Scholar]
- 305.Leidy MS, Parke RD, Cladis M, Coltrane S, Duffy S. Positive marital quality, acculturative stress, and child outcomes among Mexican Americans. J Marriage Fam. 2009;71(4):833–847. [Google Scholar]
- 306. Kimbro RT, Lynch SM, McLanahan S. The Hispanic Paradox and Breastfeeding: Does Acculturation Matter? Evidence From the Fragile Families Study. Working Paper 949. Princeton, NJ: Princeton University; 2004.
- 307.Romero-Gwynn E, Carias L. Breast-feeding intentions and practice among Hispanic mothers in southern California. Pediatrics. 1989;84(4):626–632. [PubMed] [Google Scholar]
- 308.de la Torre A, Rush L. The determinants of breastfeeding for Mexican migrant women. Int Migr Rev. 1987;21(3):728–742. [PubMed] [Google Scholar]
- 309.Umaña-Taylor AJ, Guimond AB. A longitudinal examination of parenting behaviors and perceived discrimination predicting Latino adolescents’ ethnic identity. Dev Psychol. 2010;46(3):636–650. doi: 10.1037/a0019376. [DOI] [PubMed] [Google Scholar]
- 310.Umaña-Taylor AJ, Zeiders KH, Updegraff KA. Family ethnic socialization and ethnic identity: a family-driven, youth-driven, or reciprocal process? J Fam Psychol. 2013;27(1):137–146. doi: 10.1037/a0031105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Anderson LM, Wood DL, Sherbourne CD. Maternal acculturation and childhood immunization levels among children in Latino families in Los Angeles. Am J Public Health. 1997;87(12):2018–2021. doi: 10.2105/ajph.87.12.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Busse R, Blumel M, Scheller-Kreinsen D, Zentner A. Tackling Chronic Disease in Europe: Strategies, Interventions and Challenges. London, UK: WHO Regional Office Europe; 2010. [Google Scholar]
- 313.Meaney MJ. Maternal care, gene expression, and the transmission of individual differences in stress reactivity across generations. Annu Rev Neurosci. 2001;24(1):1161–1192. doi: 10.1146/annurev.neuro.24.1.1161. [DOI] [PubMed] [Google Scholar]
- 314.Talge NM, Neal C, Glover V. Antenatal maternal stress and long-term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry. 2007;48(3–4):245–261. doi: 10.1111/j.1469-7610.2006.01714.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Kapoor A, Dunn E, Kostaki A, Andrews MH, Matthews SG. Fetal programming of hypothalamo-pituitary-adrenal function: prenatal stress and glucocorticoids. J Physiol. 2006;572(Pt 1):31–44. doi: 10.1113/jphysiol.2006.105254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Oberlander TF, Weinberg J, Papsdorf M, Grunau R, Misri S, Devlin AM. Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses. Epigenetics. 2008;3(2):97–106. doi: 10.4161/epi.3.2.6034. [DOI] [PubMed] [Google Scholar]
- 317.Coutinho R, David RJ, Collins JW. Relation of parental birth weights to infant birth weight among African Americans and Whites in Illinois: a transgenerational study. Am J Epidemiol. 1997;146(10):804–809. doi: 10.1093/oxfordjournals.aje.a009197. [DOI] [PubMed] [Google Scholar]
- 318.Jasienska G. Low birth weight of contemporary African Americans: an intergenerational effect of slavery? Am J Hum Biol. 2009;21(1):16–24. doi: 10.1002/ajhb.20824. [DOI] [PubMed] [Google Scholar]
- 319.Foster HW, Wu L, Bracken MB, Semenya K, Thomas J. Intergenerational effects of high socioeconomic status on low birthweight and preterm birth in African Americans. J Natl Med Assoc. 2000;92(5):213–221. [PMC free article] [PubMed] [Google Scholar]
- 320.Unwin N, Mugusi F, Aspray T et al. Tackling the emerging pandemic of non-communicable diseases in sub-Saharan Africa: the essential NCD health intervention project. Public Health. 1999;113(3):141–146. [PubMed] [Google Scholar]
- 321.Remington P, Brownson RC, Wegner MV. Chronic Disease Epidemiology and Control. Washington, DC: American Public Health Association; 2010. [Google Scholar]
- 322.Obasi EM, Leong FTL. Psychological distress, acculturation, and mental health-seeking attitudes among people of African descent in the United States: a preliminary investigation. J Couns Psychol. 2009;56(2):227–238. [Google Scholar]
- 323.Shen B-J, Takeuchi DT. A structural model of acculturation and mental health status among Chinese Americans. Am J Community Psychol. 2001;29(3):387–418. doi: 10.1023/A:1010338413293. [DOI] [PubMed] [Google Scholar]
- 324.Juang LP, Cookston JT. Acculturation, discrimination, and depressive symptoms among Chinese American adolescents: a longitudinal study. J Prim Prev. 2009;30(3-4):475–496. doi: 10.1007/s10935-009-0177-9. [DOI] [PubMed] [Google Scholar]
- 325.Jang Y, Chiriboga DA. Living in a different world: acculturative stress among Korean American elders. J Gerontol B Psychol Sci Soc Sci. 2010;65B(1):14–21. doi: 10.1093/geronb/gbp019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Harding S. Mortality of migrants from the Caribbean to England and Wales: effect of duration of residence. Int J Epidemiol. 2004;33(2):382–386. doi: 10.1093/ije/dyh059. [DOI] [PubMed] [Google Scholar]
- 327.Williams R. Health and length of residence among South Asians in Glasgow: a study controlling for age. J Public Health Med. 1993;15(1):52–60. doi: 10.1093/oxfordjournals.pubmed.a042820. [DOI] [PubMed] [Google Scholar]
- 328.Urquia ML, O’Campo PJ, Heaman MI. Revisiting the immigrant paradox in reproductive health: the roles of duration of residence and ethnicity. Soc Sci Med. 2012;74(10):1610–1621. doi: 10.1016/j.socscimed.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 329.Sanou D, O’Reilly E, Ngnie-Teta I et al. Acculturation and nutritional health of immigrants in Canada: a scoping review. J Immigr Minor Health. 2013;15(2):1–11. doi: 10.1007/s10903-013-9823-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Sam DL, Vedder P, Liebkind K, Neto F, Virta E. Immigration, acculturation and the paradox of adaptation in Europe. Eur J Dev Psychol. 2008;5(2):138–158. [Google Scholar]