Abstract
The Centers for Population Health and Health Disparities program promotes multilevel and multifactorial health equity research and the building of research teams that are transdisciplinary. We summarized 5 areas of scientific training for empowering the next generation of health disparities investigators with research methods and skills that are needed to solve disparities and inequalities in cancer and cardiovascular disease. These areas include social epidemiology, multilevel modeling, health care systems or health care delivery, community-based participatory research, and implementation science. We reviewed the acquisition of the skill sets described in the training components; these skill sets will position trainees to become leaders capable of effecting significant change because they provide tools that can be used to address the complexities of issues that promote health disparities.
The difficulty of reducing disparities has been largely attributed to the complex interaction among various determinants, including biological, genetic, behavioral, socioeconomic, and environmental factors. To a large extent, these factors have not been studied simultaneously to understand the complex interactions and pathways through which they influence health outcomes.1 One way to achieve this more comprehensive understanding is through transdisciplinary and multilevel research. The Centers for Population Health and Health Disparities (CPHHD) program, developed by the National Institutes of Health (NIH), promotes multilevel and multifactorial health equity research and promotes the building of research teams that are transdisciplinary.2
The current iteration of the CPHHD was launched by the National Cancer Institute and the National Heart, Lung, and Blood Institute, with funds for scientific sharing of progress provided by the NIH Office of Behavioral and Social Sciences Research. In recognition of the multifactorial causes of health disparities, the CPHHD program was designed to conduct
research involving social, behavioral, biological, and genetic research to improve knowledge of the causes of health disparities and devise effective methods of preventing, diagnosing and treating disease and promoting health.2(p1)
All of the 10 funded centers focus their research on populations that are experiencing health disparities. Four of the centers concentrate on research in African American communities, 1 focuses on American Indian/Alaska Native communities, 3 focus on Hispanic communities, and 2 conduct research in rural communities. An article that describes the current round of the CPHHD program is included in this issue.3
In addition to their efforts toward enhancing disease prevention, diagnosis, and treatment via research, each center is required to offer a training program directed toward fostering the next generation of health disparities researchers, including predoctoral students, postdoctoral fellows, and early stage investigators. In the first round of the CPHHD program, training cores were not included; however, in the second round, programs were required to include a training core. We outline these training efforts and describe the specific training goals shared across individual centers.
TRAINING A NEW GENERATION OF HEALTH DISPARITIES RESEARCHERS
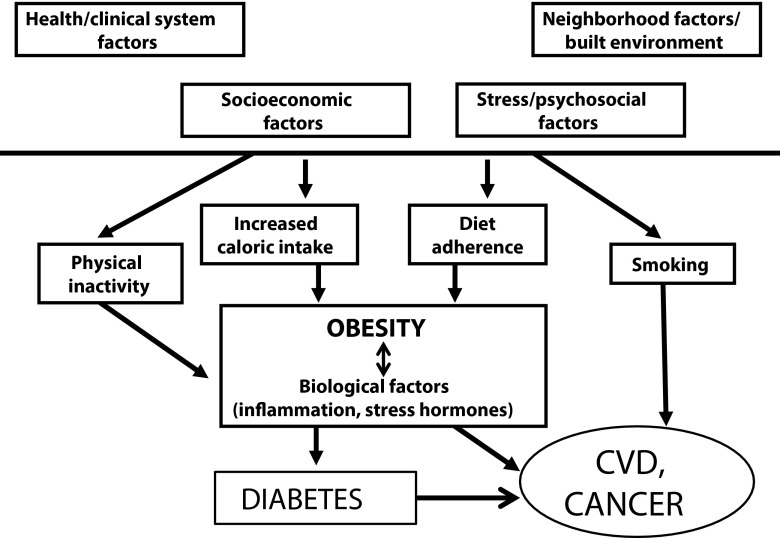
The next generation of health researchers confronting disparities in cancer and cardiovascular disease (CVD) require an extensive set of competencies because the disease pathways and interactions are complex. Although cancer and CVD are different diseases, they share some common risk factors (Figure 1). These include socioeconomic and psychosocial factors, both of which are associated with many individual risk behaviors. Some of these risk behaviors (e.g., smoking) are directly associated with CVD and cancer. Others, such as physical inactivity, are associated with obesity, which is a risk factor for both conditions, either directly, through activation of biological risk factors or through an elevated risk of diabetes. It is recognized widely that health system and neighborhood factors are also important for optimal health.4
FIGURE 1—
Effect of biological, behavioral, clinical, and nonclinical factors on disease pathways in cardiovascular disease (CVD) and cancer: Transdisciplinary Cardiovascular and Cancer Health Disparities Training.
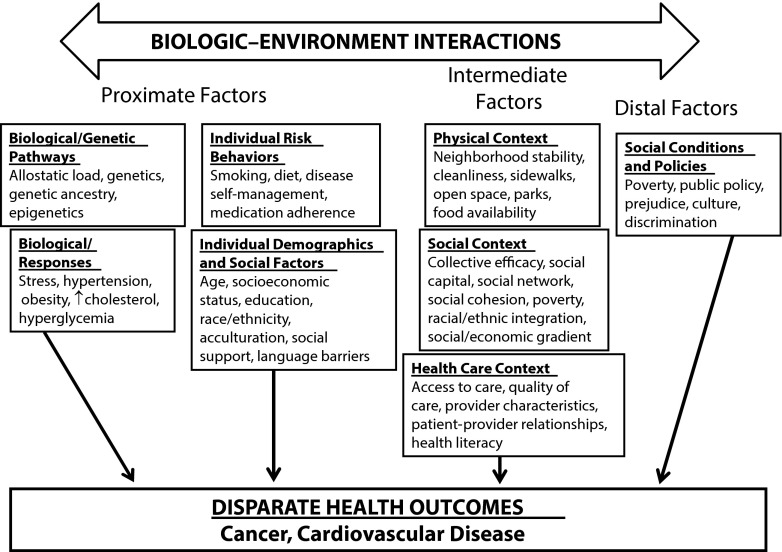
Disease pathways for CVD and cancer unfold within the constellation of contributory factors illustrated in Figure 2. These operate at multiple levels, ranging from factors proximal to the individual (genetics, individual behaviors) to intermediate factors (neighborhood stability, access to care) to distal factors (public policy, culture). To address the simultaneous complexity of disease pathways and of disease disparities, researchers in CVD and cancer disparities require public health expertise across several domains of knowledge and skill, including social epidemiology, health services research, health policy, community-based participatory research (CBPR), and implementation science, which we discuss in the following sections. Thus, a broad program of research training is needed to sustain the scientific workforce for effective research on the causes and elimination of health disparities. Training programs in multidisciplinary translational research focused on health disparities are not widely available at most universities. An example of such a training program targeting postdoctoral fellows enrolled in clinical research Masters of Science programs at 5 institutions focused on training minority researchers (e.g., Charles Drew University, Los Angeles, CA; Morehouse School of Medicine, Atlanta, GA; Meharry Medical College, Nashville, TN; University of Hawaii at Manoa; University of Puerto Rico Medical Science Campus, San Juan) is based in Puerto Rico.6 This program focuses on reducing health disparities in Hispanic populations, and the course content focuses on clinical research design and implementation, cultural diversity principles, and community engagement.
FIGURE 2—
Multilevel contributors to cancer and cardiovascular disease disparities: Transdisciplinary Cardiovascular and Cancer Health Disparities Training.
Note. Adapted from Warnecke et al.5
WORKING GROUP RECOMMENDATIONS
The Training and Career Development Work Group (TCDWG) is one of the working groups of the CPHHD. The main goal of the TCDWG is to share ideas about the diverse training and career development initiatives occurring within and across the centers, as well as to develop strategies for the cooperation and collaboration of training and career development across the centers. TCDWG members are expected to:
Identify training and career development strategies appropriate for training in health disparities research;
Identify opportunities for training and career development collaborations across centers;
Create events showcasing training and career development during CPHHD national meetings; and
Plan and coordinate courses on health disparities–related topics within and across the centers.
As the TCDWG pursued these goals, deliberations by its members yielded agreement on key domains that centers incorporated into their training programs. These included specific instruction in social epidemiology, multilevel data modeling, health care systems and their contributions to health disparities, CBPR, and implementation science. Each domain is discussed in the following, articulating a rationale for its importance. Table 1 summarizes these discussions, supplements them with examples of how particular centers have elected to address each domain, and includes references to studies conducted at and outside of our centers that are representative of each domain.
TABLE 1—
Summary of Centers for Population Health and Health Disparities (CPHHD) Training Program Components to Address Key Scientific Elements for Health Disparities Research: Transdisciplinary Cardiovascular and Cancer Health Disparities Training
| Scientific Area/CPHHD Training | Selected References of Research Studies in Each Area |
| Social epidemiology | Diez Roux and Mair7 Vargas Bustamante et al.8 Thompson et al.9 |
| Introductory and advanced public health coursework on principles of social epidemiology | |
| Seminars on the science of social epidemiology | |
| Multilevel modeling | Holmes et al.10 Plascak et al.11 |
| Formal coursework on multilevel modeling | |
| Individual mentoring provided by statisticians with expertise in multilevel modeling | |
| Health care systems/health care delivery | Institute of Medicine12 Jones et al.13 Adams et al.14 |
| Formal coursework and degree programs in health services research | |
| Seminars, readings | |
| Community-based participatory research (CBPR) | De Marco et al.15 Gehlert and Coleman16 |
| Introductory and advanced public health coursework and seminars on CBPR | |
| Design of and participation in projects utilizing CBPR | |
| Participation in community advisory board activities and interfacing with the centers’ community advisory boards in designing and implementing their projects | |
| Implementation science | Jean-Jacques et al.17 Cooper et al.18 Ephraim et al.19 |
| Seminars and roundtable discussions to highlight and address health system factors and health policy factors influencing successful implementation of interventions | |
| Shadowing opportunities to meet with key community stakeholders to expose trainees to existing policy programs administered on a population scale and to provide diverse stakeholder perspectives to sustain and disseminate findings |
Social Epidemiology
Social epidemiologists study the frequency, distribution, and social determinants of health outcomes in a population.20 It goes beyond analyzing individual risk factors to studying contexts in which health–disease phenomena occur.21 This perspective has encouraged researchers to examine characteristics of the physical, social, and structural contexts of disease. The physical factors commonly observed among vulnerable population subgroups include neighborhood disorder, poor accessibility of recreational facilities and healthy foods, or residential segregation by race, ethnicity, and income.
Social epidemiologists also study the social contexts of minority and disadvantaged or underserved populations. These include, for example, organizational and interpersonal relationships, social networks, and early life influences on health. It includes health norms distinctive to specific subpopulations, such as when the concentration of individuals within a neighborhood who have high body mass indexes encourages dismissive attitudes toward the risks of obesity.22 In this way, researchers in the field of social epidemiology provide insight into ways that environmental factors can contribute to established risk factors (e.g., obesity or diets low in fruits and vegetables) for cancer and CVD.7,23–26 Because of the emphasis on rigorously measuring health exposures originating in physical and social environments and on analytically relating them to disease outcomes, most centers provide training in social epidemiology, which can occur through formal coursework and hands-on research experience (Table 1).
Multilevel Modeling
Multilevel statistical models allow investigators to examine the influence of a factor at one level (e.g., an individual behavior such as smoking) while controlling for a factor at another level (e.g., a policy such as a clean indoor air ordinance). For this reason, they are especially suited to the analysis of multifactorial influences on health disparities. Such models have posed special challenges for health disparities researchers. Issues related to sample size (small number of study participants or clusters), data (census and secondary data, correlated data), and statistical models (fully modeling theoretical frameworks, low statistical power for examining variables involving small number of clusters, such as neighborhood effects) have all been reported.10 The TCDWG strongly supports efforts at individual centers to address these challenges by recruiting and collaborating with statisticians who specialize in designing multilevel studies, and analyzing data from multilevel interventions or observational studies and training the next generation of methodologically sophisticated researchers (Table 1).
Health Care Systems and Their Contribution to Health Disparities
The Institute of Medicine report Unequal Treatment provided the most comprehensive study of racial/ethnic disparities in health care in the United States.27 It identified contributors to disparities at the level of providers, patients, and health systems, with specific focus on the need to train researchers and the health care workforce as essential tools for reducing health care disparities.
Minority and disadvantaged populations have a range of health challenges that reflect issues relevant to health care systems, including access to and quality of care and patient–provider relationships.4 Some patient subgroups struggle with language barriers and low health literacy, less participatory medical visits, and low quality patient–provider communication. Financial and organizational arrangements may pose exceptional obstacles, whereas discrimination and distrust of health care providers adversely affect the patient–physician interaction.4
Because of the centers’ shared focus on creating effective strategies for reducing disparities, the TCDWG recommended training opportunities that allow researchers to examine and design interventions in health care systems at multiple levels—patients, providers, microsystems (immediate health care environment and delivery team), and the entire health care organization.4,28 Table 1 presents examples of how individual centers have responded to this recommendation.
Community-Based Participatory Research
The philosophy of CBPR has gained increasing attention among contemporary health disparities researchers. Research consistent with this model targets a system of care and its providers, the patient population, and the neighboring geographic community. It offers opportunities to reduce health disparities through interventions and relevant policy designed cooperatively by researchers and community, thus resulting in more effective and sustainable outcomes. CBPR encourages partnerships of academic health investigators with community organizations and leaders, with community representatives often serving as an advisory board for research projects. Researchers and community partners then work together to plan, develop, and implement interventions; to evaluate and disseminate results; and, perhaps, to craft new policy.
Collaborations undertaken through the principles of CBPR prioritize culturally sensitive, effective and sustainable methods, and results.29 Ideally, such efforts can bridge the cultural gap between researchers and communities. For instance, these partnerships can provide guidance and infrastructure for adapting recruitment and intervention materials to the cultural and literacy needs of a community; the result serves the researchers’ need to collect information efficiently and the participants’ need to understand their rights and responsibilities. Genuine research collaborations guided by CPBR principles provide vehicles through which traditionally marginalized communities may gain power through the acquisition of new knowledge.30
For such reasons, the TCDWG agrees that well-trained disparities researchers will recognize the role of community-based advisory boards and other aspects of successful CBPR. The trainees at all CPHHD centers currently draw on CBPR principles and community engagement through the examples shown in Table 1.
Implementation Science
Implementation science is the study of methods to promote the integration of research findings and evidence into health care policy and practice.31 As indicated in Table 1, the centers provide trainees with theoretical and practical training in the methodology for promoting integration of research findings into health policy and health system decision-making. Trainees are provided opportunities to interact with leading experts within their institutions and other centers to learn communication skills needed to advocate for less powerful social groups to enhance the impact of research on population health.
SPECIFIC TRAINING NEEDS FOR DIFFERENT GROUPS OF RESEARCHERS
In light of abundant evidence that the causes of health disparities are multifactorial, the CPHHD program is explicitly committed to transdisciplinary research. This calls for collaborations not only among different clinical areas in biomedical research, but across seemingly distant academic disciplines from bench to social sciences.
As a result, enhancing a research professional’s existing specialty experience effectively poses special challenges to training programs. In particular, programs committed to transdisciplinary collaboration will recruit individuals who desire experiences to augment their existing specializations and skills in ways that allow them to interact more effectively with colleagues from other disciplines. In the following, we share the experience of the TCDWG with regard to the needs common to 2 groups of trainees who are typical at our centers, namely physicians without a public health background and scientists without a clinical background.
Needs of Physicians Without a Public Health Background
Developing a successful career as a physician–scientist focused on health disparities research requires formal training at the master’s level (e.g., Masters of Public Health [MPH], Masters of Health Science [MHS], Masters of Science [MSc]) or PhD level in a public health discipline (e.g., epidemiology, health behavior, biostatistics, health services research, health policy). The goal is to equip clinically trained physicians with the research skills necessary to become successful, independent health disparities researchers.
Advanced degree training can be incorporated into a postdoctoral clinical fellowship program, supported by an institutional (T32) or individual (F32) NIH training grant, diversity supplement grant, or incorporated into junior faculty career development through NIH Mentored Patient Oriented Career Development (K23) or foundation career development awards.
Needs of Doctoral-Level Scientists Without a Clinical Background
Trainees with a nonclinical background benefit from exposure to clinical problems and settings that apply public health theories and methods. In addition to providing nonclinical trainees with opportunities to collaborate with medical trainees on clinically oriented research projects, centers facilitate roundtable discussions that highlight important medical and ethical considerations (e.g., how to address adverse medical events) when dealing with patient-oriented research. Trainees with nonclinical backgrounds are also encouraged to complete clinically oriented public health coursework (e.g., diabetes or obesity epidemiology, CVD epidemiology, cancer epidemiology, and clinical trials) and advanced courses in biological disciplines (e.g., physiology, pathology, and pharmacology), to attend clinically oriented grand rounds and seminar series, and to participate in clinical shadowing opportunities with medical professionals (e.g., preventive cardiologists, endocrinologists, oncologists, nurse practitioners) to provide valuable exposure to relevant clinical issues that contribute to CVD and cancer disparities. Disease-specific training can also be incorporated into the training component of NIH career development awards (e.g., Cancer Prevention and Control, Behavioral Sciences, and Population Sciences Career Development Award [K07]).
Cross-Training Between Centers
The centers have promoted students who are interested in studying the common underlying causes of and prevention strategies for both cancer and CVD and students who desire to obtain additional research skills or work with other underserved populations not available at their home centers. To this end, they have sponsored trainees to participate in CPHHD cross-center exchanges to expand their research skills and develop new collaborations through mentorship by researchers from a variety of disciplines.
TRAINING PROGRAMS SPECIFICS
In Table 2, we present an overview of the training programs at the CPHHD sites. To evaluate how well this transdisciplinary model is working within and across the centers, the TCDWG has developed a set of common metrics to monitor the progress of its predoctoral and postdoctoral trainees.
TABLE 2—
Training Components of the 10 Centers for Population Health and Health Disparities: Transdisciplinary Cardiovascular and Cancer Health Disparities Training
| Centers | Disparity Population | Predoctorate Program | Postdoctorate Program | Faculty Program |
| Cancer centers | ||||
| University of Washington | Native American | X | ||
| Fred Hutchinson Cancer Research Center | Latino | X | X | |
| Ohio State University | Appalachia | X | X | X |
| Harvard University | Low socioeconomic status and minority | X | ||
| University of Illinois at Chicago | African American | X | X | |
| Cardiovascular disease centers | ||||
| Johns Hopkins University | African American | X | X | X |
| University of California, Los Angeles | Latino | X | X | X |
| Rush University | African American and Puerto Rican | X | X | |
| University of North Carolina at Chapel Hill | Low-income, rural | X | X | X |
| University of Massachusetts, Lowell | Puerto Rican | X | X |
Predoctoral Trainees
The predoctoral fellow training programs in cancer and CVD vary. Some centers specify the required majors and require applicants to pursue an advanced degree, whereas other centers open eligibility to any undergraduate or graduate student interested in health disparities. Training can range from a multiweek summer undergraduate internship program held at the University of California, Los Angeles (UCLA), The Ohio State University (OSU; Cleveland, OH), Rush University (Chicago, IL), and Johns Hopkins University (JHU; Baltimore, MD) to a multiple-year program, such as those supported at Fred Hutchinson Cancer Research Center, Seattle, Washington; University of Washington, Seattle; University of Illinois at Chicago (UIC); University of North Carolina at Chapel Hill (UNC); Harvard University, Boston, Massachusetts; and JHU.
Training strategies are similar among the cancer and CVD centers, and they include journal clubs, individual mentoring, weekly meetings, health disparities seminars, and statistical training. Some programs, such as those at the University of Washington and UCLA, require students to conduct primary data collection in community-based settings. Other centers, like OSU, Rush University, and JHU, encourage the students to work on secondary data analysis projects from the center. The majority of the training programs expect the trainees to conceptualize research questions, analyze data, and present their research projects at the end of the training period. At JHU, predoctoral students have the option of obtaining a Health Disparities and Inequality Certificate through the School of Public Health during their formal degree program. UIC also offers a certificate in Health Disparities Research. Centers also encourage conference attendance, conference presentations, or manuscript submission before finishing the predoctoral program. The predoctoral student training program at UCLA also includes a writing assignment on the book The Immortal Life of Henrietta Lacks to prepare trainees for the responsible conduct of research.
Postdoctoral Trainees
The postdoctoral training programs in cancer and CVD are more uniform in their training objectives, duration, and expectations. Postdoctoral fellowships average 2 years at most of the CPHHD. Most require attendance at monthly seminars and disparities didactic sessions, and encourage their trainees to attend the annual CPHHD and other relevant scientific meetings. Additional educational opportunities are available to postdoctoral trainees, ranging from 2 courses at Harvard University, to an optional MPH at OSU. JHU also offers public health Masters’ degree programs (MPH, MHS, MSc), an optional Health Disparities and Inequality certificate program, and a course in CBPR through their School of Public Health.
Faculty Programs
Some of the CPHHDs include formal training programs for junior faculty. For example, the University of Washington, in partnership with the University of Colorado, Denver, supports American Indian/Alaskan Native junior faculty for 2 years to conduct research pertinent to cancer disparities. Specifically, they receive financial support to conduct secondary data analysis and primary data collection pilot studies, write grants, and publish articles to prepare them for independent investigator-initiated grant applications. JHU also has a 2-year faculty disparities fellowship focused on research training in CVD disparities in urban African Americans. Fellows are expected to attend monthly disparities curriculum didactic sessions and seminars, to present their preliminary research findings at twice yearly Research in Progress meetings, participate in community engagement experiences, attend the CBPR seminar course offered through the School of Public Health, and meet weekly with their research mentors. By the end of the fellowship, faculty fellows are expected to publish at least 1 peer-reviewed article. Several fellows have successfully competed for additional grant funding, including K awards and foundation grants.
Other Training Programs
Investigators at Rush University have developed and implemented a culturally sensitive community health worker curriculum in heart failure, pediatric asthma, and pediatric obesity. This training program includes the topics of health behavior, addiction, caregiver burden and burnout, and self-care, among others. Investigators at JHU are also developing a community health worker curriculum in collaboration with community partners. The topics include high blood pressure, heart attack, stroke, heart failure, healthy eating and weight control, and stress and depression.
TRAINING METRICS AND EVALUATIONS OF POSTDOCTORAL TRAINEES
A common metrics tool is being utilized by the CPHHD Training Cores to track the progress of our postdoctoral trainees. To assess the impact of our training programs on research productivity, the number of published articles (first authored and coauthored), oral abstract, poster, and symposium presentations at local and national meetings, awards received, and grants submitted and funded is being documented. To assess posttraining employment, data are collected on the position obtained (title, location, tenured or nontenured track), and whether the position focuses on health disparities research. Finally, trainees evaluate their mentors so that each center can ensure that future trainees are connected with the strongest mentors to facilitate individual success.
EARLY INDICATORS OF PROGRAM IMPACT
To date, the 10 centers have engaged 140 undergraduate and graduate students, 31 postdoctoral fellows, and 21 faculty in their training programs. Although still in the early years of training activities, the centers are currently coordinating plans to evaluate their impact on trainee outcomes, including their success in launching disparities research and public health careers, publishing peer-reviewed articles, and obtaining research funding to advance these important areas of science. At JHU, postdoctoral fellows have published several articles based on their participation in the center’s projects,32–35 5 research grant awards (institutional, foundation, and NIH grants) have been received by faculty fellows, 2 of 3 former predoctoral students completed their PhD degrees and now hold tenure-track faculty positions, and 1 former faculty fellow was promoted from assistant to associate professor and had a manuscript selected as article of the year by The Obesity Society.36,37 At OSU, the undergraduate training program has been particularly successful. Two students have published their summer independent research projects in peer-reviewed journals,38,39 4 students are finalizing their articles with their mentors for journal submission, and numerous students presented their research at national and local conferences. Moreover, of the students who graduated with a bachelor’s degree, 33% completed a health disparities thesis, and 50% are working in public health. Finally, at UCLA, there have been 14 peer-reviewed publications in press or print coauthored with trainees, and 2 postdoctoral fellows and 2 PhD students have obtained tenure track positions.
CONCLUSIONS
This article summarizes 5 areas of scientific training for empowering the next generation of health disparities researchers with research methods and skills that are needed to solve disparities and inequalities in cancer and CVD. The acquisition of the skill sets described in the training components reviewed here will position trainees to become leaders capable of effecting significant change because they provide tools that can be employed to address the complexities of issues that promote health disparities. These skills are applicable to disparities research on other chronic conditions. We believe that all persons entering the fields of public health or health policy, to the extent that their professional responsibilities require significant attention to health disparities, will benefit from training that emphasizes the elements that we have outlined.
In many ways, the multitude of approaches to training for research in health disparities provides a cadre of investigators with diverse skills. However, it is not clear whether these ad hoc methods can fill the need for sophisticated investigators well grounded in a critical core of skills and rigorous methodologies necessary to advance the knowledge needed to eliminate health disparities. Although every effort must be made to eliminate health disparities as quickly as possible, it is likely that they will persist at some level for many years to come, both nationally and internationally. Therefore, educational institutions with expertise in health disparities might consider creating a specialized curriculum or degree program to provide advanced training (e.g., MS in Health Disparities or doctorate in Health Psychology with concentration in health disparities). The CPHHD community is preparing to create a model draft curriculum and invites other organizations with similar interest to join the effort.
Acknowledgments
Funding sources: P50CA148143-01, Principal investigator (PI): Beti Thompson, Understanding and Preventing Breast Cancer Disparities in Latinas; P50CA148596-01, PI: David R. Williams, Lung Cancer Disparities Center: Jointly Addressing Race and Socioeconomic Status; P50HL105187-01, PI: Lisa A. Cooper, Johns Hopkins Center for Eliminating Cardiovascular Health Disparities; P50HL105185-01, PI: Katheine L. Tucker, Boston Puerto Rican Health Study - CVD Risk Factors; P50CA105632-06, PI: Electra D. Paskett, Reducing Cervical Cancer in Appalachia; P50HL105189-01, PI: Lynda H. Powell, Rush Center for Urban Health Equity; P50HL105188-01, PI: Alexander N. Ortega, Family and Neighborhood Interventions to Reduce Heart Disease Risk in East L.A; P50CA106743-06, PI: Richard Warnecke, UIC Center for Population Health and Health Disparities; P50HL105184-01, PI: Alice S. Ammerman, Center for Reduced CVD Disparities: Genes, Clinics, and Communities; P50CA148110-01, PI: Dedra S. Buchwald, Center for Native Population Health Disparities.
We would also like to acknowledge the other members of Centers for Population Health and Health Disparities (CPHHD) Training and Career Development Workgroup: Andrea Krinke, MPH, University of Washington CPHHD, Seattle; Emily Kontos, ScD, and Linnea Benson-Whelan, BS, Harvard T. H. Chan School of Public Health CPHHD, Boston, MA; Gloria Sorensen, PhD, MPH, Harvard T. H. Chan School of Public Health; Johanna Lampe, PhD, Fred Hutchinson Cancer Research Center CPHHD, Seattle; John Griffith, PhD, and Lindsay Mancini, BS, Northeastern University CPHHD, Boston; Joy Mays, Johns Hopkins University School of Medicine CPHHD, Baltimore, MD; Katrina Donahue, MD, MPH, University of North Carolina CPHHD, Chapel Hill; Luis Falcon, PhD, University of Massachusetts CPHHD, Lowell; Marian Fitzgibbon, PhD, University of Illinois CPHHD, Chicago; Toyin Sokari, MPH, The Ohio State University CPHHD, Columbus.
Human Participant Protection
Institutional review board approval was not required for the CPHHD training program activities because human participant research was not conducted on our program's trainees.
References
- 1.Voelker R. Decades of work to reduce disparities in health care produce limited success. JAMA. 2008;299(12):1411–1413. doi: 10.1001/jama.299.12.1411. [DOI] [PubMed] [Google Scholar]
- 2.The Centers for Population Health and Health Disparities. NIH Announces the Funding of The Centers for Population Health and Health Disparities. 2010. Available at: http://cancercontrol.cancer.gov/populationhealthcenters/cphhd/index.html. Accessed November 22, 2014.
- 3.Cooper LA, Ortega AN, Ammerman AS et al. Calling for a bold new vision of health disparities intervention research. Am J Public Health. 2015;105(suppl 3):S374–S376. doi: 10.2105/AJPH.2014.302386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Golden SH, Brown A, Cauley JA et al. Health disparities in endocrine disorders: biological, clinical, and nonclinical factors—an Endocrine Society scientific statement. J Clin Endocrinol Metab. 2012;97(9):E1579–E1639. doi: 10.1210/jc.2012-2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warnecke RB, Oh A, Breen N et al. Approaching health disparities from a population perspective: the National Institutes of Health Centers for Population Health and Health Disparities. Am J Public Health. 2008;98(9):1608–1615. doi: 10.2105/AJPH.2006.102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Estape E, de Laurido LES, Shaheen M et al. A multiinstitutional, multidisciplinary model for developing and teaching translational research in health disparities. Clin Transl Sci. 2011;4(6):434–438. doi: 10.1111/j.1752-8062.2011.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diez-Roux AV, Nieto FJ, Caulfield L, Tyroler HA, Watson RL, Szklo M. Neighbourhood differences in diet: the Atherosclerosis Risk in Communities (ARIC) Study. J Epidemiol Community Health. 1999;53(1):55–63. doi: 10.1136/jech.53.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vargas Bustamante A, Fang H, Garza J et al. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigr Minor Health. 2012;14(1):146–155. doi: 10.1007/s10903-010-9406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson B, Vilchis H, Moran C, Copeland W, Holte S, Duggan C. Increasing cervical cancer screening in the United States-Mexico Border Region. J Rural Health. 2014;30(2):196–205. doi: 10.1111/jrh.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holmes JH, Lehman A, Hade E et al. Challenges for multilevel health disparities research in a transdisciplinary environment. Am J Prev Med. 2008;35(2, suppl):S182–S192. doi: 10.1016/j.amepre.2008.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Plascak JJ, Llanos AA, Pennell ML, Weier RC, Paskett ED. Neighborhood factors associated with time to resolution following an abnormal breast or cervical cancer screening test. Cancer Epidemiol Biomarkers Prev. 2014;23:2819. doi: 10.1158/1055-9965.EPI-14-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Committee on Public Health Priorities to Reduce and Control Hypertension in the US Population. A Population-Based Policy and Systems Change Approach to Prevent and Control Hypertension. Available at: http://www.nap.edu/openbook.php?record_id=12819. Accessed November 20, 2014.
- 13.Jones RG, Trivedi AN, Ayanian JZ. Factors influencing the effectiveness of interventions to reduce racial and ethnic disparities in health care. Soc Sci Med. 2010;70(3):337–341. doi: 10.1016/j.socscimed.2009.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adams AS, Uratsu C, Dyer W et al. Health system factors and antihypertensive adherence in a racially and ethnically diverse cohort of new users. JAMA Intern Med. 2013;173(1):54–61. doi: 10.1001/2013.jamainternmed.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Marco M, Kearney W, Smith T, Jones C, Kearney-Powell A, Ammerman A. Growing partners: building a community–academic partnership to address health disparities in rural North Carolina. Prog Community Health Partnersh. 2014;8(2):181–186. doi: 10.1353/cpr.2014.0021. [DOI] [PubMed] [Google Scholar]
- 16.Gehlert S, Coleman R. Using community-based participatory research to ameliorate cancer disparities. Health Soc Work. 2010;35(4):302–309. doi: 10.1093/hsw/35.4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jean-Jacques M, Persell SD, Thompson JA, Hasnain-Wynia R, Baker DW. Changes in disparities following the implementation of a health information technology-supported quality improvement initiative. J Gen Intern Med. 2012;27(1):71–77. doi: 10.1007/s11606-011-1842-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cooper LA, Marsteller JA, Noronha GJ et al. A multi-level system quality improvement intervention to reduce racial disparities in hypertension care and control: study protocol. Implement Sci. 2013;8:60. doi: 10.1186/1748-5908-8-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ephraim PL, Hill-Briggs F, Roter DL et al. Improving urban African Americans’ blood pressure control through multi-level interventions in the Achieving Blood Pressure Control Together (ACT) study: a randomized clinical trial. Contemp Clin Trials. 2014;38(2):370–382. doi: 10.1016/j.cct.2014.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krieger N. Epidemiology and social sciences: towards a critical reengagement in the 21st century. Epidemiol Rev. 2000;22(1):155–163. doi: 10.1093/oxfordjournals.epirev.a018014. [DOI] [PubMed] [Google Scholar]
- 21.Berkman LF, Kawachi I. Social Epidemiology. Oxford, UK: Oxford University Press; 2000. [Google Scholar]
- 22.Boardman JD, Saint Onge JM, Rogers RG, Denney JT. Race differentials in obesity: the impact of place. J Health Soc Behav. 2005;46(3):229–243. doi: 10.1177/002214650504600302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corral I, Landrine H, Hao Y, Zhao L, Mellerson JL, Cooper DL. Residential segregation, health behavior and overweight/obesity among a national sample of African American adults. J Health Psychol. 2012;17(3):371–378. doi: 10.1177/1359105311417191. [DOI] [PubMed] [Google Scholar]
- 24.Robert SA, Reither EN. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Soc Sci Med. 2004;59(12):2421–2434. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 25.Lopez RP. Neighborhood risk factors for obesity. Obesity (Silver Spring) 2007;15(8):2111–2119. doi: 10.1038/oby.2007.251. [DOI] [PubMed] [Google Scholar]
- 26.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Fruit and vegetable access differs by community racial composition and socioeconomic position in Detroit, Michigan. Ethn Dis. 2006;16(1):275–280. [PubMed] [Google Scholar]
- 27.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Institute of Medicine Report. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 28.Chin MH, Goldmann D. Meaningful disparities reduction through research and translation programs. JAMA. 2011;305(4):404–405. doi: 10.1001/jama.2011.26. [DOI] [PubMed] [Google Scholar]
- 29.Ferré CD, Jones L, Norris KC, Rowley DL. The Healthy African American Families (HAAF) project: from community-based participatory research to community-partnered participatory research. Ethn Dis. 2010;20(1 suppl 2) S2-1–8. [PMC free article] [PubMed] [Google Scholar]
- 30.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 31.US Library of Medicine. Dissemination and Implementation Science. 2013. Available at: http://www.nlm.nih.gov/hsrinfo/implementation_science.html. Accessed November 20, 2014.
- 32.Flynn SJ, Ameling JM, Hill-Briggs F et al. Facilitators and barriers to hypertension self-management in urban African Americans: perspectives of patients and family members. Patient Prefer Adherence. 2013;7:741–749. doi: 10.2147/PPA.S46517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mobula LM, Okoye MT, Boulware LE, Carson KA, Marsteller JA, Cooper LA. Cultural competence and perceptions of community health workers’ effectiveness for reducing health care disparities. J Prim Care Community Health. 2015;6(1):10–15. doi: 10.1177/2150131914540917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hussain T. Provider perspectives on essential functions for care management in the collaborative treatment of hypertension: the P.A.R.T.N.E.R. framework. J Gen Intern Med. 2014 doi: 10.1007/s11606-014-3130-4. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cunningham BA, Marsteller JA, Romano MJ et al. Perceptions of health system orientation: quality, patient centeredness, and cultural competency. Med Care Res Rev. 2014;71(6):559–579. doi: 10.1177/1077558714557891. [DOI] [PubMed] [Google Scholar]
- 36.Golden SH, Purnell T, Halbert JP et al. A community-engaged cardiovascular health disparities research training curriculum: implementation and preliminary outcomes. Acad Med. 2014;89(10):1348–1356. doi: 10.1097/ACM.0000000000000426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bleich SN, Bennett WL, Gudzune KA, Cooper LA. Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring) 2012;20(5):999–1005. doi: 10.1038/oby.2011.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Danesh D, Paskett ED, Ferketich AK. Disparities in receipt of advice to quit smoking from health care providers: 2010 National Health Interview Survey. Prev Chronic Dis. 2014;11:E131. doi: 10.5888/pcd11.140053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nelms E, Wang L, Pennell M et al. Trust in physicians among rural Medicaid-enrolled smokers. J Rural Health. 2014;30(2):214–220. doi: 10.1111/jrh.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]