Abstract
The science of eliminating health disparities is complex and dependent on demographic data. The Health Information Technology for Economic and Clinical Health Act (HITECH) encourages the adoption of electronic health records and requires basic demographic data collection; however, current data generated are insufficient to address known health disparities in vulnerable populations, including individuals from diverse racial and ethnic backgrounds, with disabilities, and with diverse sexual identities.
We conducted an administrative history of HITECH and identified gaps between the policy objective and required measure. We identified 20 opportunities for change and 5 changes, 2 of which required the collection of less data.
Until health care demographic data collection requirements are consistent with public health requirements, the national goal of eliminating health disparities cannot be realized.
Federal efforts to address racial and ethnic health disparities were initiated by the Heckler Report in 1985.1 Nearly 3 decades later, health disparities persist across racial and ethnic groups and have been estimated to cost $300 billion per year.2 Demographic data, the statistical data of a population, is the foundation for identifying disparities, improving overall quality of health care, improving population health, and measuring progress toward health equity.3 Accurately recording demographic data enables health care providers to identify risk and protective factors for a large number of diseases and conditions and to improve comprehensive care for individual patients.
As understanding of health disparities and contributing risk factors improves, the need for more granular information has increased.3 Racial and ethnic minority populations continue to increase, resulting in cultural and linguistic issues that have an impact on delivery of care and treatment. People with disabilities make up 20% of the adult population and are burdened by preventable disparities in health care compared with their nondisabled peers.4 Lesbian, gay, bisexual, and transgender individuals are becoming increasingly visible in our society and have worse outcomes for a number of medical conditions than their heterosexual and cisgender (individuals identifying as their birth sex) peers.5
In 1997, the Office of Management and Budget (OMB) revised the government-unique race and ethnicity standards to include 5 race and 2 ethnicity categories (Table 1).6 Recognition of the diversity within each OMB race and ethnicity category is critical to eliminating health disparities.3 For example, among Asians in California, rates of colorectal screening varied across racial subgroups, with disparities seen in Chinese, Korean, and Vietnamese individuals compared with Whites, but no disparity seen in other Asian subgroups.7 In this instance, the intervention most effective in reducing the disparity would target Chinese, Korean, and Vietnamese patients, rather than all Asian individuals. For this reason, recent health disparity reports consistently call for the collection of more detailed and consistent information across the health care and public health systems.7–9 Under the Affordable Care Act (ACA), the Department of Health and Human Services developed more granular race and ethnicity standards and added 6 functional questions to assess disability status (Table 1).10
TABLE 1—
Comparison of Race and Ethnicity Collection Standards Adopted by the Office of Management and Budget in 1997 and the Department of Health and Human Services in 2011
| Demographic | Office of Management and Budget6 (Last Revised in 1997) | Department of Health and Human Services10 (Adopted in 2011) |
| Race | Black or African American | Black or African American |
| American Indian or Alaska Native | American Indian or Alaska Native | |
| Asian | Asian Indian | |
| Chinese | ||
| Filipino | ||
| Japanese | ||
| Korean | ||
| Vietnamese | ||
| Other Asian | ||
| Native Hawaiian or other Pacific Islander | Native Hawaiian | |
| Guamanian or Chamorro | ||
| Samoan | ||
| Other Pacific Islander | ||
| White | White | |
| Ethnicity | Non-Hispanic or Latino | Non-Hispanic/Latino/Spanish origin |
| Hispanic or Latino | Mexican | |
| Cuban | ||
| Puerto Rican | ||
| Other Hispanic/Latino/Spanish origin |
THE HITECH ACT
In 2009, Congress passed the Health Information Technology for Economic and Clinical Health Act (HITECH) and invested more than $35 billion to stimulate the adoption and meaningful use of electronic health records (EHRs) by physicians and hospitals.11 One of the primary goals of HITECH was to reduce health disparities.11 As proof of the law’s reach, by 2013, 69% of physicians intended to or were already participating in the Medicare or Medicaid EHR incentive program.12 Physician EHR adoption increased from 25% in 2010 to 40% in 2012 and hospital adoption rates nearly tripled to 44% during the same time period.13
The HITECH programs have evolved through a staged rulemaking process, resulting in a dense, complex, and convoluted administrative history. No comprehensive look at HITECH’s administrative process with regard to demographic data collection currently exists. Therefore, this study provides much-needed documentation of the rulemaking process related to recording demographic data.
Our specific aims were (1) to construct a comprehensive administrative history of HITECH with regard to recording demographic data, (2) to determine the number of opportunities for policy change and policy changes that arose throughout the process, and (3) to identify the reasons for adopting or declining opportunities for policy change with regard to recording demographic data.
The primary purpose of this analysis was to support the collection of enhanced demographic data across various health sectors. It is our intention to unite health care providers, public health practitioners, consumers, EHR vendors, advocates, and policymakers in an effort to develop and adopt robust, forward-thinking policies on the collection of demographic data in EHRs that will lead to the reduction and ultimate elimination of health disparities.
METHODS
We compiled the HITECH administrative history by using the Federal Register’s online advanced search tool. We identified all administrative actions taken between February 17, 2009, and February 28, 2014, by using the search term “HITECH.” We collected and reviewed for relevancy every article with the search term “demographic.” We excluded articles related to privacy and security, health care payment and delivery systems, and specific data collection notices.
We limited our demographic categories of interest to granular race and ethnicity data, preferred language, disability status, sexual orientation, and gender identity. We conducted a targeted search of each relevant document by using the following key terms: disparit*, demographic, race, ethnicity, language, disabilit*, and sexual. Where these terms appeared, we collected the entire section related to the term and additional information necessary for contextual understanding.
We defined and applied variables to the relevant sections of each article. “Baseline” was the statutory minimum or final rule from the previous action. We defined “proposed category” as the categories of demographic data proposed for collection. We defined “final category” as the categories adopted in the final rule. “Standard” was the common terminology used to support each demographic data category. “Opportunity for change” was the explicit consideration by the agency of multiple categories or standards. “Change” was a change in category or standard from the baseline to the final rule (Table 2).
TABLE 2—
Opportunities for Policy Change and Actual Changes in Demographic Data Requirements Through 3 Rounds of Health Information Technology for Economic and Clinical Health Act Administrative Actions
| MU |
SCC |
|||||||||||
| Baseline Demographic Data Category | Proposed Category | Standard | Final Category | Standard | Opportunity for Change | Change | Proposed Category | Standard | Final Category | Standard | Opportunity for Change | Change |
| Round 1a | ||||||||||||
| Race | Race | OMB | Race | OMB | Yes | No | Race | OMB | Race | OMB | Yes | No |
| Ethnicity | Ethnicity | OMB | Ethnicity | OMB | Yes | No | Ethnicity | OMB | Ethnicity | OMB | Yes | No |
| Preferred language | Preferred language | TBD | Preferred language | Deferred to ONC | No | NA | Preferred language | TBD | Preferred language | TBD | No | No |
| Gender | Gender | No mention | Gender | No mention | No | NA | Gender | No mention | Gender | No mention | No | NA |
| Insurance type | No mention | Yes | Yes | Insurance type | No mention | Yes | Yes | |||||
| Other commenter suggestions: Social Security number, birthplace, education, occupation or industry, family history, functional status | No mention | Yes | No | |||||||||
| Totals | 3 | 1 | 4 | 1 | ||||||||
| Round 2b | ||||||||||||
| Race | Race | OMB | Race | OMB | Yes | No | Race | OMB | Race | OMB | Yes | No |
| Ethnicity | Ethnicity | OMB | Ethnicity | OMB | Yes | No | Ethnicity | OMB | Ethnicity | OMB | Yes | No |
| Preferred language | Preferred language | No mention | Preferred language | No mention | No | No | Preferred language | ISO 639-1 | Preferred language | ISO 639-2 constrained by ISO 639-1 | Yes | Yes |
| Gender | Gender | No mention | Sex | No mention | Yes | Yes | Gender | No mention | Sex | No mention | Yes | Yes |
| Disability status | Request for comments | NA | Yes | No | Disability status | Request for comments | NA | Yes | No | |||
| Sexual orientation | Request for comments | NA | Yes | No | ||||||||
| Gender identity | Request for comments | NA | Yes | No | ||||||||
| Other commenter suggestions: Internet access, computer literacy, occupation or industry | No mention | NA | Yes | No | Other commenter suggestions: sexual orientation, gender identity, residency, country of origin, nationality, type of employment, primary place of employment, education level, hobbies | No mention | NA | Yes | No | |||
| Totals | 7 | 1 | 6 | 2 | ||||||||
| Round 3c | ||||||||||||
| Race | Race | OMB | Race | TBD | Yes | TBD | ||||||
| Ethnicity | Ethnicity | OMB | Ethnicity | TBD | Yes | TBD | ||||||
| Preferred language | Preferred language | 3 options | Preferred language | TBD | Yes | TBD | ||||||
| Sex | Sex | No mention | Sex | TBD | Yes | TBD | ||||||
| Disability status | American Community Survey plus English proficiency | TBD | TBD | Yes | TBD | |||||||
| Sexual orientation | HL7 | TBD | TBD | Yes | TBD | |||||||
| Gender identity | HL7 | TBD | TBD | Yes | TBD | |||||||
| Military status | Request for comments | TBD | TBD | Yes | TBD | |||||||
| Occupation or industry | Request for comments | TBD | TBD | Yes | TBD | |||||||
| Race | OMB | Race | TBD | Yes | TBD | |||||||
| Grand totals | 10 | 2 | 10 | 3 | ||||||||
Note. HITECH = Health Information Technology for Economic and Clinical Health Act; HL7 = Health Level Seven International; ISO = International Organization for Standardization; MU = the Meaningful Use program; NA = not applicable; OMB = Office of Management and Budget; ONC = Office of the National Coordinator; SCC = Standards and Certification Criteria program; TBD = to be determined.
MU stage 1; initial SCC; baseline = HITECH.
MU stage 2; 2014 edition SCC; baseline = round 1.
MU stage 3 (The proposed rule was published in the Federal Register on March 30, 2015, and is open for public comment until May 29, 2015; available as a supplement to the online version of this article at http://www.ajph.org).; 2015 voluntary edition SCC; baseline = round 2.
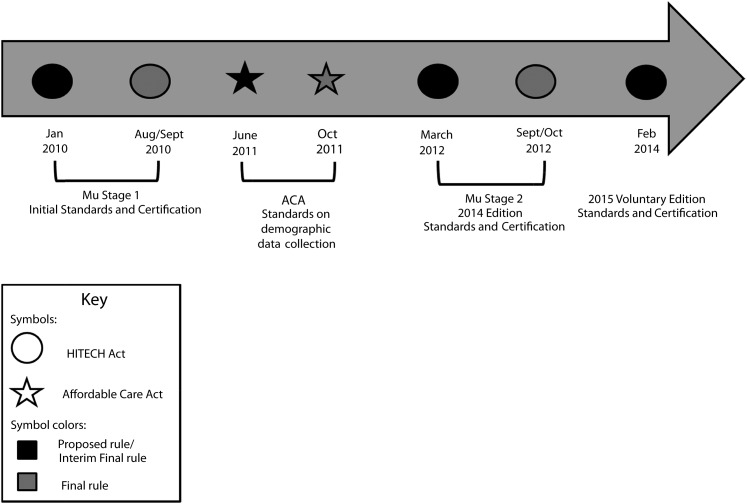
From these findings, we constructed a timeline of every HITECH administrative action relevant to recording demographic data (Figure 1). We included actions taken in accordance with the ACA’s demographic data collection standards to allow for temporal comparison.
FIGURE 1—
Timeline of administrative actions under the Health Information Technology for Economic and Clinical Health Act (HITECH) and the Affordable Care Act (ACA): United States, 2010–2014.
Note. MU = the Meaningful Use program.
RESULTS
The administrative history search of the Federal Register resulted in 136 articles. Once we applied the exclusion criteria, 9 regulatory actions remained relevant. We identified 2 HITECH programs: (1) the Medicare and Medicaid EHR Incentive program (the Meaningful Use program [MU]), administered by the Centers for Medicare and Medicaid Services (CMS) and (2) the Health Information Technology (HIT) Standards and Certification Criteria program (SCC), administered by the Office of the National Coordinator (ONC). Five of the regulatory actions were proposed or interim final rules, 2 for the MU program (stages 1 and 2) and 3 for the SCC program (initial, 2014 edition, and 2015 voluntary edition). Four were final rules, 2 for the MU program and 2 for the SCC program. In total, there were 20 opportunities for policy change. Five changes were made, with 2 of those changes eliminating a category of demographic data, and a number of opportunities remain to be determined. Table 2 shows all opportunities for change and all actual changes.
Round 1
The administrative actions for stage 1 of the MU program and the initial SCC for certified EHRs coincided, with the proposed rules published in the Federal Register on January 13, 2010, and the final rules becoming effective on September 27, 2010, and August 27, 2010, respectively.
Meaningful Use, stage 1.
In the MU proposed rule,14 the recording of demographic data was proposed as a core (required) objective. Within the objective, the proposed categories were race, ethnicity, gender, date of birth, preferred language, and insurance type. The OMB standards were proposed for race and ethnicity. No standards were proposed for preferred language.
From the proposed to the final rule,15 there were 3 opportunities for policy change and 1 change: insurance type was eliminated from the requirements (Table 2). Comments on the complexity of defining insurance type and attributing it to patients in a consistent way merited its elimination as a core measure. Citing the Institute of Medicine report entitled “Race, Ethnicity and Language Data: Standardization for Health Care Quality Improvement,” commenters recommended more granular racial and ethnic standards that roll up to the 5 OMB standards; however, the minimal OMB standards were adopted in the final rule. The agency reasoned that expanding the OMB categories was “beyond the scope of the definition of meaningful use to provide additional definitions for race and ethnicity. . . .”15
Initial set of Standards and Certification Criteria.
The SCC rulemaking was consistent with the MU rulemaking with regard to recording demographic data.16,17 Commenters recommended additional categories of demographic data, including birthplace, education, occupation or industry, and functional status. Because the agency did not address each category separately, all of these recommendations were counted as a single opportunity for policy change. In total, there were 4 opportunities for policy change and 1 change: insurance type was eliminated from the requirements (Table 2). The SCC final rule established the OMB standards for race and ethnicity.
Round 2
The administrative actions for stage 2 of the MU program and the 2014 edition SCC for certified EHRs occurred simultaneously, with the proposed rules published in the Federal Register on March 7, 2012, and the final rules becoming effective on September 4, 2012, and October 4, 2012, respectively.
Meaningful Use, stage 2.
From the proposed to the final rule, there was a total of 7 opportunities for change and 1 actual change (Table 2).18,19 The OMB standards for race were recommended in the proposed rule, and voluntary recording of additional categories was encouraged if they mapped to the 5 OMB categories. The CMS requested comments on the collection of disability status, highlighting the benefits to care coordination from gathering this information in the EHR. The CMS also sought comment on whether sexual orientation and gender identity should be recorded in EHRs.
In the final rule, CMS reported several comments recommending alternative race and ethnicity standards, specifically the Centers for Disease Control and Prevention and the US Census Bureau standards. The agency declined to change but encouraged the voluntary collection of more granular data mapping to the OMB categories. The CMS adopted the term “sex” to replace “gender” on the basis of comments clarifying that “gender” is a social construct and “sex” is a physiological characteristic at birth.
Many commenters supported the addition of disability status, sexual orientation, and gender identity. Yet some comments questioned the clinical significance of recording this information as demographic data. The CMS declined to adopt disability status or sexual orientation and gender identity because of the lack of consensus on definitions, lack of agreed-upon standards, data collection and reporting challenges, and disagreement over where and how to collect this information in an EHR.
Standards and Certification Criteria, 2014 edition.
From the proposed rule to the final rule, there was a total of 6 opportunities for change and 2 actual changes (Table 2).20,21 The ONC proposed to maintain the OMB race and ethnicity categories. The ONC proposed to adopt the International Organization for Standardization’s (ISO’s) language standard ISO 639-1 as the preferred language vocabulary standard as opposed to the more granular ISO 639-2 standard.22 The ONC requested comments about incorporating disability status into demographic data, citing the many benefits of making this change, from improving access, coordinating care across multiple providers, and monitoring disparities between “disabled” and “nondisabled” populations. The ONC did not seek comments on whether sexual orientation and gender identity data should be collected.
The final SCC rule clarified the preferred language standards based on the comments received, and ISO 639-2 constrained by 639-1 was adopted because constraining ISO 639-2 to only the active languages in 639-1 would permit more granularity and is a better approach than in the proposed rule.22 Commenters suggested 3 alternative race and ethnicity standards based on the Institute of Medicine recommendations, the Centers for Disease Control and Prevention vocabulary standards, and those adopted by the Department of Health and Human Services to comply with the ACA, all of which are more granular than the OMB standards. The final rule declined this change, reasoning that the OMB categories are a government-unique standard, are easily understood, and are readily available making them the best standards to support the policy goals. The agency stated that EHR technology must have the capability to map race and ethnicity to the OMB categories if the technology developer chooses to incorporate more granular race and ethnicity categories. Disability status was not adopted for reasons similar to those of CMS. Commenters recommended the incorporation of sexual orientation and gender identity, but the agency declined to make this change.
Round 3
On February 26, 2014, the ONC released a notice of proposed rulemaking for the voluntary 2015 edition EHR certification criteria (2015 SCC), which lacked a CMS Meaningful Use program counterpart.23 The proposed rule anticipated a MU stage 3 proposal in the fall (available as a supplement to the online version of this article at http://www.ajph.org).
The proposed rule identified challenges based on the previous action (SCC 2014 edition final rule) adopting preferred language standards. Since the final rule’s publication, ONC published a list of frequently asked questions to clarify the standards and acknowledged that the approach taken in the final rule failed to support current languages, including sign language and Hmong.24 Because of this oversight, the 2015 SCC proposed rule sought comment on 3 options: full adoption of ISO 639-2 codes, adoption of ISO 639-3 codes, or adoption of standards included in “Tags for identifying languages, September 2009,” a memo describing current best practices for language identification.22 (ISO 639-1 consists of 2-letter codes representing most of the major languages of the world. ISO 639-2 consists of 3-letter codes representing more languages than ISO 639-1. ISO 639-3 consists of 3-letter codes and is the most comprehensive of the ISO series, including living, extinct, and ancient languages.)
Following the proposed rule, the ONC sought comments on changes to the SCC in anticipation of the 2017 edition. Up for consideration were the recording of disability status, sexual orientation, gender identity, military status, and industry or occupation. Comments were sought on the appropriateness of these categories and ways to include them in current demographic data requirements. The rule proposed 6 functional questions currently included in the American Community Survey with the addition of a question about English proficiency, seeking comment on whether the questions were appropriate or if better alternatives exist and how to capture this information in an EHR. Sexual orientation and gender identity standards were proposed on the basis of the recent IOM report, “Collecting sexual orientation and gender identity data in electronic health records: workshop summary.” Comments on the collection of military service history and occupation and industry were requested. The comment period for this proposed rule closed on April 28, 2014.
DISCUSSION
There is a gap between the criteria and standards supporting the MU measure recording demographic data and the policy objective of reducing health disparities. Medical practices are driven by the MU criteria and, without requirements for more informative data, providers are not encouraged through the policy to identify pertinent demographics that lead to proper clinical diagnosis and improved outcomes. Evidence-based measures that better support the policy objective exist and are included in public health programs and surveys (Table 3).
TABLE 3—
Policy Gaps Between Demographic Data Requirements Proposed and Adopted in the Meaningful Use Program and Those Used in Public Health Surveys
| Demographic Data Category | Possible Evidence-Based Standards (Explicitly Acknowledged in Final Rules) | No. of Categories | Proposed in MU | Adopted in MU | Used in Public Health Surveys |
| Race | OMB | 5 | X | X | X |
| DHHS | 14a | X | X | ||
| CDC | > 500a | X | X | ||
| IOM | Locally relevant choicesa | X | NA | ||
| Ethnicity | OMB | 2 | X | X | X |
| DHHS | 5a | X | X | ||
| CDC | > 30a | X | X | ||
| IOM | Locally relevant choices | X | NA | ||
| Preferred language | ISO 639-1 | > 200 | X | Xb | X |
| ISO 639-2 | > 500 | X | Xb | X | |
| ISO 639-3 | Approximately 6000 | X | X | ||
| Tags for Identifying Languages, September 2009 | Develops unique identifiers for languages included in ISO 639 registry | X | NA | NA | |
| Sex | 2 | X | X | X | |
| Disability or functional status | American Community Survey | 6 | X | X | |
| Sexual orientation | HL7 | 8 | X | X | |
| Gender identity | HL7 | 8 | X |
Note. CDC = Centers for Disease Control and Prevention; DHHS = Department of Health and Human Services; HL7 = Health Level Seven International; IOM = Institute of Medicine; ISO = International Organization for Standardization; MU = the Meaningful Use program; NA = not applicable; OMB = Office of Management and Budget.
All subcategories roll up to OMB categories.
ISO 639-2 alpha-3 codes limited to those that also have a corresponding alpha-2 code in ISO 639-1.
The inconsistent demographic data collection standards between the HITECH programs and the ACA programs may exacerbate health disparities and are problematic for both research and practice. Practice is hindered because public health is collecting information that, in the case of disability status, sexual orientation, and gender identity, has limited clinical comparison, and with regard to race and ethnicity, is more informative than the data being collected in EHRs. Research using public health survey data will provide specific information that cannot be adapted to the clinical level because of insufficient data collection in EHRs. The ONC and CMS recognize the importance of comparable data between EHRs and public health, yet this study shows the agencies have declined nearly every opportunity to align the Department of Health and Human Services data adopted in the ACA with the MU and SCC programs.16
Although ONC and CMS have declined to require expanded demographic data collection, the agencies encourage providers to voluntarily collect additional demographic data as is appropriate for their practice.16 This suggestion is merely an illusion of flexibility and expanded data collection efforts as most EHR vendors are solely focused on building systems compliant with the SCC criteria. (Andy Slavitt, chief executive officer, OptumInsight, stated to the Subcommittee on Healthcare and Technology Subcommittee on Small Business “[N]ew product development is focused on satisfying those regulatory hurdles, rather than on simple innovations that improve productivity.”25) Therefore, health care providers who wish to collect more information must expand their budgets and payment structures to develop the functionality and infrastructure within their individual EHR system or build the capacity in their own information technology departments. This is particularly challenging for health care providers that serve minority and underserved communities who are less likely to have the financial means to build this capacity. Until expanded demographic data categories are included in the SCC program requirements, vendors lack incentives to build the capacity within their EHRs.
It is difficult to gauge the likelihood for policy change in the MU and SCC programs, but the 2015 voluntary SCC proposed rule may provide some insight into future rulemakings. It is thus far the most aggressive proposal with regard to adding categories of demographic data; however, it proposed to maintain the minimally informative OMB standards for race and ethnicity. The evolution of the preferred language standards is a promising precedent, although the challenges experienced with adopting a single standard may deter future aggressive policies.
Limitations
The methodology used in this study was time-consuming, but it comprehensively collected all administrative actions taken within the timeframe of interest. This study did not look at the HITECH legislative history or the recommendations of the subagency HIT Policy Committee or the HIT Standards Committee, which would provide even more insight into the policymaking process.
These methods do not include uses of demographic data in EHRs beyond the MU core objective of “record demographics.” Other MU objectives utilize similar information. For example, functional status was adopted in MU stage 2 as a requirement for the care summary document. However, limiting these data to the care summary document maintains the long-held view of disability as merely a medical condition and precludes analysis of preventable health disparities that have an impact on people with disabilities.
Conclusions
The use of EHRs to identify and reduce health disparities is promising, but limited by the type of demographic data that is currently collected. To recognize HITECH’s policy priority of reducing health disparities, more granular race and ethnicity data, disability status, and sexual orientation and gender identity must be collected in EHRs. The only way to ensure the consistent and comprehensive collection of this information is to incorporate expanded requirements into the MU and SCC programs. Public health leaders have a responsibility to encourage health care providers, EHR vendors, and policymakers to adopt and effectively implement evidence-based policies and practices necessary to help document and eliminate health disparities.
Acknowledgments
The project described was supported by the National Institute on Minority Health and Health Disparities grant U54MD008173, a component of the National Institutes of Health.
Note. The article’s contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute on Minority Health and Health Disparities or the National Institutes of Health.
Human Participant Protection
No protocol approval was necessary because all data were obtained from publicly available secondary sources.
References
- 1.Washington, DC: US Department of Health and Human Services; 1985. Report of the Secretary’s Task Force on Black and Minority Health, vol. 1. [Google Scholar]
- 2.LaVeist T, Gaskin D, Richard P. The Economic Burden of Health Inequalities in the United States. Washington, DC: Joint Center for Political and Economic Studies; 2009. [Google Scholar]
- 3.Institute of Medicine. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: National Academy Press; 2009. [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality. 2013 National Health Care Disparities Report. 2014. Pub. no. 14-0006. Available at: http://www.ahrq.gov/research/findings/nhqrdr/nhdr13/2013nhdr.pdf. Accessed June 26, 2014. [Google Scholar]
- 5.Agency for Healthcare Research and Quality. 2011 National Health Care Disparities Report. 2012. Pub. no. 12-0006. Available at: http://www.ahrq.gov/research/findings/nhqrdr/nhdr11/nhdr11.pdf. Accessed June 26, 2014. [Google Scholar]
- 6. Office of Management and Budget: revisions to the standards for the classification of federal data on race and ethnicity, 62 Federal Register 36873 (notice October 30, 1997).
- 7.Agency for Healthcare Research and Quality. 2012 National Health Care Disparities Report. 2013. Pub no. 13-0003. Available at: http://www.ahrq.gov/research/findings/nhqrdr/nhdr12/2012nhdr.pdf. Accessed June 26, 2014. [Google Scholar]
- 8.Joint Center for Political and Economic Studies. Patient Protection and Affordable Care Act of 2010: advancing health equity for racially and ethnically diverse populations. 2010. Available at: http://csmh.umaryland.edu/Toolbar/Toolbardocs/reformdiversepopulations.pdf. Accessed June 26, 2014.
- 9. Reducing health care disparities: collection and use of race, ethnicity and language data. Chicago, IL: Health Research and Educational Trust; 2013. Available at: http://www.hpoe.org. Accessed June 26, 2014.
- 10.Department of Health and Human Services. Implementation guidance on data collection standards for race, ethnicity, sex, primary language, and disability status. 2011. Available at: http://aspe.hhs.gov/datacncl/standards/aca/4302/index.pdf. Accessed June 26, 2014.
- 11. American Recovery and Reinvestment Act, Pub L No. 111-5.
- 12.Hsiao C-J, Hing E. Hyattsville, MD: National Center for Health Statistics; 2014. Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001–2013. NCHS data brief, no 143. [PubMed] [Google Scholar]
- 13.DesRoches CM, Charles D, Furukawa MF, Joshi MS, Kralovec P, Mostashari F. Adoption of electronic health records grows rapidly, but fewer than half of US hospitals had at least a basic system in 2012. Health Aff (Millwood) 2013;32(8):1478–1485. doi: 10.1377/hlthaff.2013.0308. [DOI] [PubMed] [Google Scholar]
- 14. Medicare and Medicaid Programs: electronic health record incentive program, 75 Federal Register 1844 (proposed January 13, 2010). [PubMed]
- 15. Medicare and Medicaid Programs: electronic health record incentive program, 75 Federal Register 44314 at 44341 (July 28, 2010; codified at 42 CFR 412, 413, 422, et al.). [PubMed]
- 16. Health information technology: initial set of standards, implementation specifications, and certification criteria for electronic health record technology, 75 Federal Register 2014 (proposed January 13, 2010). [PubMed]
- 17. Health information technology: initial set of standards, implementation specifications, and certification criteria for electronic health record technology, 75 Federal Register 44590 (July 28, 2010; codified at 45 CFR part 170). [PubMed]
- 18. Medicare and Medicaid Programs: electronic health record incentive program—stage 2, 77 Federal Register 13698 (proposed March 7, 2012). [PubMed]
- 19. Medicare and Medicaid Programs: electronic health record incentive program—stage 2, 77 Federal Register 53968 (September 4, 2012; codified at 42 CFR 412, 413, 422, et al.). [PubMed]
- 20. Health information technology: standards, implementation specifications, and certification criteria for electronic health record technology, 2014 edition; revisions to the permanent certification program for health information technology, 77 Federal Register 13832 (proposed March 7, 2012). [PubMed]
- 21. Health information technology: standards, implementation specifications, and certification criteria for electronic health record technology, 2014 edition; revisions to the permanent certification program for health information technology, 77 Federal Register 54163 (September 4, 2012; codified at 45 CFR part 170). [PubMed]
- 22.International Organization for Standardization. Language codes—ISO 639. Available at: http://www.iso.org/iso/home/standards/language_codes.htm. Accessed June 26, 2014.
- 23. Voluntary 2015 edition electronic health record (EHR) certification criteria; interoperability updates and regulatory improvements, 79 Federal Register 10880 (proposed February 26, 2014).
- 24. HealthIT.gov Web site. ONC Regulations FAQs. Available at: http://www.healthit.gov/policy-researchers-implementers/onc-regulations-faqs. Accessed January 15, 2015.
- 25. Statement of Andy Slavitt, chief executive officer, OptumInsight to the Subcommittee on Healthcare and Technology Subcommittee on Small Business, June 2, 2011. Available at: http://smbiz.house.gov/UploadedFiles/Slavitt_Testimony.pdf. Accessed June 26, 2014.