Abstract
Objectives. We explored the interrelationships among diabetes, hypertension, and missing teeth among underserved racial/ethnic minority elders.
Methods. Self-reported sociodemographic characteristics and information about health and health care were provided by community-dwelling ElderSmile participants, aged 50 years and older, who took part in community-based oral health education and completed a screening questionnaire at senior centers in Manhattan, New York, from 2010 to 2012.
Results. Multivariable models (both binary and ordinal logistic regression) were consistent, in that both older age and Medicaid coverage were important covariates when self-reported diabetes and self-reported hypertension were included, along with an interaction term between self-reported diabetes and self-reported hypertension.
Conclusions. An oral public health approach conceptualized as the intersection of 3 domains—dentistry, medicine, and public health—might prove useful in place-based assessment and delivery of services to underserved older adults. Further, an ordinal logit model that considers levels of missing teeth might allow for more informative and interpretable results than a binary logit model.
The complex interplay among oral health, systemic inflammation, and health outcomes precludes straightforward explanations as to their relationships.1 Nonetheless, there is increasing recognition by oral health professionals of the need to assess their patients for general health conditions that may affect oral health or complicate treatment plans.2 Furthermore, access to quality dental care is an equity issue, because racial/ethnic minorities, underserved populations, and Medicaid beneficiaries (those who are poor or disabled) face substantial barriers that require flexibility and ingenuity to overcome.3
Understanding the developmental processes of dental diseases and their socioeconomic patterns across the life course is crucial in determining optimal times for interventions to better limit the population health burden and reduce socioeconomic inequalities in oral health and health care.4 We believe that social disparities in health and health care are particularly evident in the mouth, even as they are inextricably tied to other systems of the body,5 and that it is never too early or too late in life to intervene to improve health and well-being.6
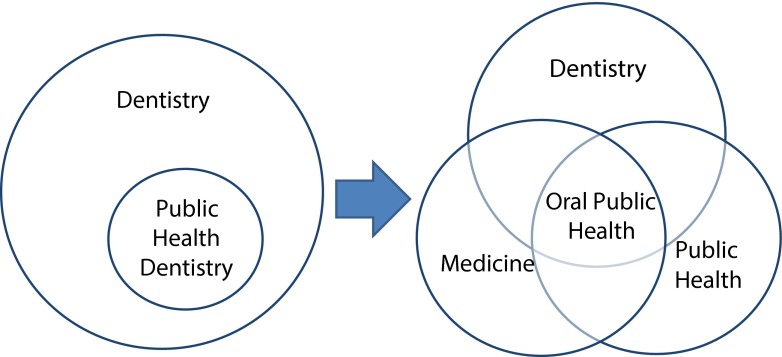
The community-based ElderSmile clinical program of the Columbia University College of Dental Medicine represents an innovative approach to screening and providing treatment to older adults with complex needs, regardless of their ability to pay for services.7 Rather than viewing public health dentistry as a subfield of dentistry in interdisciplinary initiatives such as this one, oral public health is more broadly conceptualized as the intersection of 3 domains: dentistry, medicine, and public health (Figure 1).
FIGURE 1—
The evolution of public health dentistry as a subfield of dentistry, to oral public health as the intersection of 3 broad domains—dentistry, medicine, and public health.
Previous research has sought to identify causal pathways between general and oral health, as well as between poor oral health and mortality.8 For instance, it has been theorized that chronic oral infections caused by periodontal disease and the resultant presence of inflammatory markers may lead to the onset of hypertension and stroke.9,10 Further, a number of recent studies have identified relationships between chronic health conditions, such as diabetes and heart disease, and increased numbers of missing teeth in adults.11–14 Few programs have integrated general and oral health screening and provided follow-up social, medical, and dental services for underserved older adults in community-based settings that are both accessible and affordable.
A notable exception to this rule is the ElderSmile program. In November 2010, the focus of this initiative was expanded to include general health, that is, community-based education and screening for diabetes and hypertension were added to the oral health activities that remain its core functions.15 Importantly, data collection is ongoing, which permits the assessment of relationships between oral and general health, and progress in achieving health equity for its largely racial/ethnic minority, socioeconomically disadvantaged older adult participants over time. Our study had 2 objectives: (1) to examine the relationships between general health conditions (diabetes and hypertension) and missing teeth in the ElderSmile population, and (2) to determine if an ordinal logistic regression model that used 3 response categories for missing teeth (edentulous or 28 missing teeth of a total of 28 teeth, excluding third molars; limited functional capacity or 9–27 missing teeth; and functional dentition or 0–8 missing teeth) provided more information while retaining ease of interpretation compared with a binary logistic regression model that used 2 response categories (edentulous and dentate).
METHODS
Data were from the ElderSmile clinical program, which at the time of this study (November 2010–June 2012) consisted of 51 prevention centers located at senior centers and other locations where older adults gather in the socioeconomically disadvantaged areas of Harlem and Washington Heights/Inwood communities of northern Manhattan in New York, New York.15 Descriptions of this community-based program, which was targeted to racial/ethnic minority older adults,7,15 reported previously on oral health outcomes for this underserved population,16 including determinants of self-reported oral health.17 Exploratory spatial analyses based upon program intake information that argued for place-based interventions18,19 are available elsewhere.
Study Design and Measures
Our study was cross-sectional in design and restricted to the 556 adults aged 50 years and older at the time of screening who consented to be clinically examined by a dentist and undergo primary care testing for diabetes and hypertension by program staff. Self-reported sociodemographic characteristics and information about health and health care were provided by ElderSmile participants, who took part in community-based oral health and primary care education and completed a screening questionnaire in either English or Spanish, according to their language preferences.
Older adults were enrolled in the ElderSmile program after participating in oral and general health promotion activities and being examined by 1 of the ElderSmile dentists. After the screening dentist reviewed the results of the oral health examination with each patient, patients had the option of being referred to 1 of 3 ElderSmile community-based treatment centers (if there was no dental home) or to their own dentist.16 Program staff conduct chairside glycosylated hemoglobin A1c (HbA1c) and blood pressure (BP) screening (both systolic BP [SBP] and diastolic BP [DBP]) on ElderSmile participants who consented to undergo testing.15 Program staff then made referrals, when indicated, on an individual basis to community-based treatment centers (if there was no medical home) or to patients’ own primary care providers.
Our primary outcome measure of interest was the presence or absence of teeth as determined by an ElderSmile dentist based upon a complete dentition of 28 teeth. Third molars were excluded from the analysis because they are often missing because of reasons other than dental caries or other oral diseases. Edentulism was defined as having no natural permanent teeth in the mouth or 28 missing teeth.20 Because having 20 teeth is considered necessary for functional dentition,21,22 participants with 0 to 8 missing teeth were considered to have functional dentition, and participants with 9 to 27 missing teeth were considered to have limited functional capacity.
Our 2 determinants of primary interest were diabetes and hypertension. These conditions were assessed in 2 ways: by self-report (as yes or no responses to the following questions, “Have you ever been told by a physician that you have diabetes or high blood sugar?” and “Have you ever been told by a physician that you have hypertension or high blood pressure?”) and by chairside measurement of HbA1c (for diabetes) and BP (for hypertension). For ElderSmile participants who were never diagnosed with diabetes, HbA1c values less than 5.7% were considered to be in the normal range, values between 5.7% and 6.4% were considered to be in the prediabetes range, and values of 6.5% or more were considered to be in the diabetes range. For those participants with physician-diagnosed diabetes, HbA1c values of 7.0% or more were considered to be evidence of poor glycemic control.23 For those participants with or without physician-diagnosed hypertension, the cutpoints were as follows: for normal values, SBP less than 120 millimeters of mercury and DBP less than 80 millimeters of mercury; for prehypertension values, SBP of 120 to 139 millimeters of mercury or DBP of 80 to 89 millimeters of mercury; and for high BP values, SBP of 140 millimeters of mercury or greater or DBP of 90 millimeters of mercury or greater.24
The covariates of interest were obtained by self-report and consisted of the following sociodemographic, health, and health care characteristics (along with their attendant categorizations or measurement scales): gender (female, male); race/ethnicity (Hispanic, non-Hispanic White, non-Hispanic Black, other); age (in years); primary language (English, Spanish, other); place of birth (mainland United States, Puerto Rico, Dominican Republic, other); highest level of education completed (primary school, high school, some college or more); tobacco smoking status (never smoked, former smoker, current smoker); health insurance coverage (yes or no), Medicaid coverage (yes or no), and dental insurance coverage (yes or no); time since last visited a medical doctor (< 1 year, 1–3 years, > 3 years), time since last visited a dentist (< 1 year, 1–3 years, > 3 years); and self-rated oral health (excellent, good, fair, poor).
Data Analysis
We computed means, medians, SDs (for normally distributed variables), and interquartile ranges (for non-normally distributed variables) for continuous variables, whereas we computed counts and percentages for categorical variables.22 In addition to descriptive statistics, we conducted the χ2 test for the differences between dentate and edentulous participants for categorical variables.25
We conducted 2 sets of logistic regression models (both bivariable and multivariable): the first was a binary response model with edentulous (yes or no) as the outcome variable; and the second was an ordinal logit model with 3 ordered response categories for number of missing teeth (edentulous or 28 missing teeth, limited functional capacity or 9–27 missing teeth, and functional dentition or 0–8 missing teeth). We included age (in years), Medicaid coverage (yes or no), self-reported diabetes (yes or no), self-reported hypertension (yes or no), and an interaction term between self-reported diabetes and self-reported hypertension in the final multivariable models as important predictors for the number of missing teeth. All analyses were conducted in SAS version 9.1 (SAS Institute, Cary, NC).26
RESULTS
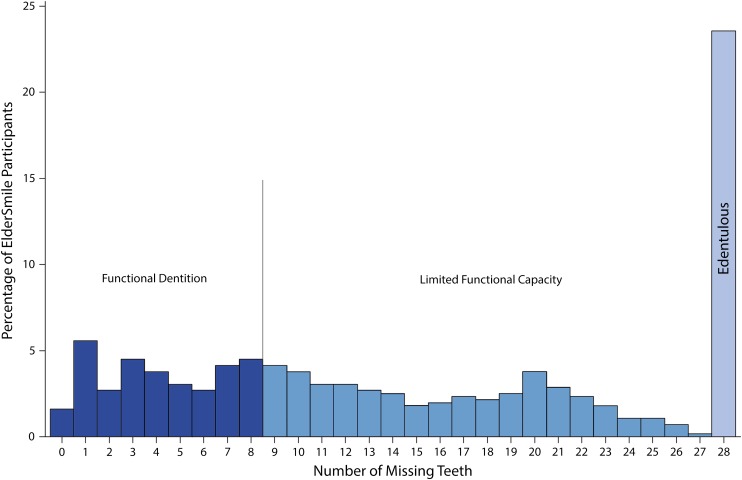
The characteristics of ElderSmile program participants—overall and by dentate status—is available in Table 1. The distribution of the number of missing teeth among ElderSmile program participants is provided in Figure 2; the distribution was not normal. Almost one quarter (23.6%) of the population was edentulous, and less than one third (32.6%) had functional dentition.
TABLE 1—
Sociodemographic, Health, and Health Care Characteristics of Participants by Dentate Status: ElderSmile Program; New York, NY; 2010–2012
| Characteristic | Overall, No.a (%) | Dentate, No.a (%) | Edentulous, No.a (%) | Pb |
| Gender | .98 | |||
| Female | 409 (74.9) | 313 (74.9) | 96 (75.0) | |
| Male | 137 (25.1) | 105 (25.1) | 32 (25.0) | |
| Race/ethnicity | .56 | |||
| Hispanic | 349 (65.7) | 262 (65.3) | 87 (66.9) | |
| Non-Hispanic White | 38 (7.2) | 29 (7.2) | 9 (6.9) | |
| Non-Hispanic Black | 131 (24.7) | 98 (24.4) | 33 (25.4) | |
| Other | 13 (2.4) | 12 (3.0) | 1 (0.8) | |
| Age, y | < .01 | |||
| < 65 | 95 (17.9) | 82 (20.45) | 13 (10.1) | |
| 65–74 | 201 (37.9) | 162 (40.40) | 39 (30.2) | |
| ≥ 75 | 234 (44.2) | 157 (39.15) | 77 (59.7) | |
| Primary language | .21 | |||
| English | 278 (51.8) | 221 (53.9) | 57 (44.9) | |
| Spanish | 244 (45.4) | 178 (43.4) | 66 (52.0) | |
| Other | 15 (2.8) | 11 (2.7) | 4 (3.1) | |
| Place of birth | .41 | |||
| Mainland United States | 188 (35.7) | 146 (36.2) | 42 (34.2) | |
| Puerto Rico | 136 (25.9) | 104 (25.8) | 32 (26.0) | |
| Dominican Republic | 111 (21.1) | 89 (22.1) | 22 (17.9) | |
| Other | 91 (17.3) | 64 (15.9) | 27 (22.0) | |
| Highest education | .05 | |||
| Primary | 219 (48.0) | 167 (46.6) | 52 (53.1) | |
| High school | 130 (28.5) | 98 (27.4) | 32 (32.6) | |
| Some college or more | 107 (23.5) | 93 (26.0) | 14 (14.3) | |
| Smoking status | .09 | |||
| Never smoked | 219 (58.7) | 162 (56.2) | 57 (67.1) | |
| Former smoker | 109 (29.2) | 86 (29.9) | 23 (27.1) | |
| Current smoker | 45 (12.1) | 40 (13.9) | 5 (5.9) | |
| Health insurance | .13 | |||
| Yes | 512 (95.2) | 386 (94.4) | 126 (97.7) | |
| No | 26 (4.8) | 23 (5.6) | 3 (2.3) | |
| Medicaid | < .01 | |||
| Yes | 290 (64.2) | 200 (59.9) | 90 (76.3) | |
| No | 162 (35.8) | 134 (40.1) | 28 (23.7) | |
| Dental insurance | .761 | |||
| Yes | 326 (68.5) | 248 (68.1) | 78 (69.6) | |
| No | 150 (31.5) | 116 (31.9) | 34 (30.4) | |
| Time since last visit to a doctor, y | .52 | |||
| < 1 | 424 (83.8) | 327 (83.8) | 97 (83.6) | |
| 1–3 | 56 (11.1) | 41 (10.5) | 15 (12.9) | |
| > 3 | 26 (5.1) | 22 (5.7) | 4 (3.5) | |
| Time since last visit to a dentist, y | .25 | |||
| < 1 | 244 (50.5) | 194 (52.6) | 50 (43.9) | |
| 1–3 | 138 (28.6) | 100 (27.1) | 38 (33.3) | |
| > 3 | 101 (20.9) | 75 (20.4) | 26 (22.8) | |
| Self-rated oral health | < .01 | |||
| Excellent | 40 (8.5) | 23 (6.3) | 17 (16.0) | |
| Good | 143 (30.4) | 109 (29.9) | 34 (32.1) | |
| Fair | 206 (43.7) | 163 (44.7) | 43 (40.6) | |
| Poor | 82 (17.4) | 70 (19.2) | 12 (11.3) | |
| Self-reported diabetes | .06 | |||
| Yes | 192 (41.3) | 153 (43.7) | 39 (33.9) | |
| No | 273 (58.7) | 197 (56.3) | 76 (66.1) | |
| Self-reported hypertension | .92 | |||
| Yes | 297 (67.5) | 223 (67.4) | 74 (67.9) | |
| No | 143 (32.5) | 108 (32.6) | 35 (32.1) | |
| Total | 556 | 425 | 131 |
Numbers may vary across characteristics because of missing values.
P values correspond to the testing of differences between dentate and edentulous participants using the χ2 test.
FIGURE 2—
Distribution of the number of missing teeth among ElderSmile program participants (third molars excluded): New York, NY; 2010–2012.
Note. The number of missing teeth was categorized according to the level of functionality of the dentition: functional dentition (0-8 missing teeth), limited functional capacity (9-27 missing teeth), and edentulous (28 missing teeth). The sample size was n = 556 participants. The mean number of missing teeth was 15 (median = 14; interquartile range = 18).
Nearly three quarters of the participants were women (74.9%), and approximately two-thirds (65.7%) were Hispanic. Only about one-half (51.8%) identified English as their primary language, and almost as many (45.4%) identified Spanish as their primary language. With regard to meaningful differences between edentulous and dentate program participants, edentulous program participants tended to be older, were less likely to have attended college, were more likely to be covered by Medicaid, and were more likely to consider themselves to have excellent self-rated oral health than their dentate counterparts.
We then examined unadjusted and adjusted binary responses (edentulous, dentate) and ordinal logit models for missing teeth (edentulous, limited functional capacity, and functional dentition), with self-reported diabetes and self-reported hypertension as the predictors of primary interest (see data available as a supplement to the online version of this article at http://www.ajph.org). Consistent with the findings in Table 1, neither self-reported diabetes nor self-reported hypertension alone was an important predictor of edentulism or more missing teeth in any of the models examined. The multivariable models were consistent, in that both older age and Medicaid coverage were important covariates when self-reported diabetes and self-reported hypertension were included, along with an interaction term between self-reported diabetes and self-reported hypertension. As shown in Table 2, the score test for the proportional odds assumption suggested that this assumption was valid (P = 0.55) for the present data, meaning that the levels of missing teeth had a natural ordering; it was apt to use an ordinal logit model for this outcome.26 Because the 95% confidence intervals were, in every instance, tighter around the estimates in the ordinal logit model than in the binary response model, the results for the unadjusted and adjusted ordinal logit models are presented in Table 3 and Table 4, respectively.
TABLE 2—
Response Profile for Number of Missing Teeth of a Total 28 Teeth, Excluding Third Molars: ElderSmile Program; New York, NY; 2010–2012
| Ordered Value | Missing Teeth | No.a (%b) |
| 3 = edentulous | 28 | 131 (23.6) |
| 2 = limited functional capacity | 9–27 | 244 (43.9) |
| 1 = functional dentition | 0–8 | 181 (32.6) |
Note. Total number of respondents = 556. The score test for the proportional odds assumption suggests that this assumption is valid (P = .55) for the current data, χ2 = 3.9910; df = 5; Pr > χ2 = 0.5507.
Numbers may vary across models because of missing values for included characteristics.
Percent does not sum to 100% because of rounding.
TABLE 3—
Unadjusted Odds Ratios and 95% Confidence Intervals for Univariable Ordinal Logit Models for Associations Among Sociodemographic, Health Insurance, and Health Characteristics and Number of Missing Teeth, Using 3 Response Categories: ElderSmile Program; New York, NY; 2010–2012
| Characteristic | OR (95% CI) |
| Age (≥ 5 y) | 1.29 (1.18, 1.41) |
| Medicaid (yes vs no) | 2.09 (1.45, 3.01) |
| Diabetes (yes vs no) | 0.90 (0.64, 1.27) |
| Hypertension (yes vs no) | 1.23 (0.85, 1.78) |
Note. CI = confidence interval; OR = odds ratio.
TABLE 4—
Adjusted Odds Ratios and 95% Confidence Intervals for Multivariable Ordinal Logit Models for Associations Among Sociodemographic, Health Insurance, and Health Characteristics and Number of Missing Teeth, Using 3 Response Categories, and Including an Interaction Term for Diabetes and Hypertension: ElderSmile Program; New York, NY; 2010–2012
| Characteristic | AOR (95% CI) |
| Age (≥ 5 y) | 1.43 (1.26, 1.62) |
| Medicaid (yes vs no) | 2.22 (1.43, 3.43) |
| Diabetes (yes vs no at hypertension = no) | 0.20 (0.08, 0.48) |
| Diabetes (yes vs no at hypertension = yes) | 1.52 (0.92, 2.51) |
| Hypertension (yes vs no at diabetes = no) | 0.40 (0.23, 0.71) |
| Hypertension (yes vs no at diabetes = yes) | 3.20 (1.35, 7.11) |
Note. AOR = adjusted odds ratio; CI = confidence interval. As used in the formula below, γj is defined as the probability that the response category ≤ j, where j = 1, 2, 3:
log γj/1 – γj = Age + Medicaid + Diabetes + Hypertension + Diabetes * Hypertension.
To better understand the findings of effect modification between self-reported diabetes and self-reported hypertension, we examined the distributions of missing teeth in 4 groups of ElderSmile program participants (see data available as a supplement to the online version of this article at http://www.ajph.org), as defined by their self-reported diabetes (yes or no) and self-reported hypertension status (yes or no). Again, none of these distributions was normal. The lowest median for missing teeth (i.e., median = 11) was observed in participants whose self-reported diabetes status was yes, and whose self-reported hypertension status was no, even though there were few participants in this group (n = 36). In this group, there were fewer edentulous participants than in the other 3 groups. The highest median for missing teeth (median = 17) was observed in participants whose self-reported diabetes status was no, and whose self-reported hypertension status was no, but the interquartile range (IQR = 23) was relatively large, indicating more spread in this distribution than for the group whose self-reported diabetes status was yes and self-reported hypertension status was yes (median = 16; IQR = 18). These nuances regarding the distributions were better captured in an ordinal logistic regression model that used 3 response categories for missing teeth (edentulous or 28 missing teeth of a total of 28 teeth, excluding third molars; limited functional capacity or 9–27 missing teeth; and functional dentition or 0–8 missing teeth) compared with a binary logistic regression model that used 2 response categories (edentulous and dentate), while retaining ease of interpretation.
DISCUSSION
With regard to the first objective of our study, that is, examining the relationships between general health conditions (diabetes and hypertension) and missing teeth in the ElderSmile population, our results depended in part upon whether self-reported or chairside measurements for diabetes and hypertension were used. When we examined HbA1c and BP values (both DBP and SBP) and missing teeth, we found no relationships. This was perhaps best explained by the fact that sizable proportions of ElderSmile participants had self-reported diabetes (41.3%) or self-reported hypertension (67.5%) (Table 1). Earlier findings from this population included (1) among ElderSmile participants with no previous diagnosis by a physician of diabetes or hypertension, 7.8% and 42.2% had HbA1c levels in the diabetes range and prediabetes range, and 24.6% and 37.7% had BP readings in the hypertension range and prehypertension range, respectively15; and (2) among ElderSmile participants with a previous diagnosis by a physician of diabetes or hypertension, 38.3% had HbA1c levels in the out-of-control range, and 37.8% and 39.8% had BP levels in the hypertension range and prehypertension range, respectively.15 (Note, however, that the BP guidelines for hypertensive adults in the general population aged 60 years and older were recently raised to a treatment goal of SBP < 150 mm Hg and DBP < 90 mm Hg.27)
By contrast, we did find effect modification for self-reported diabetes and self-reported hypertension with regard to the level of missing teeth in the ElderSmile population. That is, the relationship between self-reported hypertension and missing teeth depended upon whether the participant also had self-reported diabetes. This was especially evident in Table 4, in which the adjusted odds ratio for having both self-reported hypertension and self-reported diabetes in the ordinal logit model for level of missing teeth was 3.20 (95% confidence interval = 1.35, 7.11), whereas neither self-reported diabetes nor self-reported hypertension alone was an important determinant of the level of missing teeth (Table 3).
In other words, in a population of underserved racial/ethnic minority older adults, their access to and quality of medical and dental care and preventive resources (e.g., nutrition and physical activity) helped to determine the diagnosis and treatment of primary care sensitive conditions (e.g., diabetes and hypertension) and oral health outcomes (e.g., missing teeth). Thus, it is important to embrace an oral public health approach (Figure 1) to ensure that all 3 domains are considered in the community-based care of older adults, namely, dentistry (lifetime accumulation of numbers of missing teeth), medicine (timely screening and ongoing care of primary care sensitive conditions), and public health (community-based amenities such as health screenings at senior centers and support for access to neighborhood follow-up treatment services for identified concerns).
With regard to the second objective of our study, an ordinal logistic regression model that used 3 response categories for missing teeth (edentulous or 28 missing teeth of a total of 28 teeth, excluding third molars; limited functional capacity or 9–27 missing teeth; and functional dentition or 0–8 missing teeth) provided more information while retaining ease of interpretation compared with a binary logistic regression model that used 2 response categories (edentulous and dentate). A recent report that analyzed data from the US National Health and Nutrition Examination Survey to understand the association between diabetes and tooth loss used a binary logistic regression model to examine edentulism (as per this study), but then used a linear regression model to examine the number of missing teeth among dentate participants only.20 By contrast, the ordinal logistic regression model we used allowed for consideration of the entire study population in 1 model (both edentulous and dentate participants), while taking into account the non-normal distribution of missing teeth among ElderSmile participants.
Strengths and Limitations
The strengths of our study were that it was part of the larger ElderSmile program at the Columbia University College of Dental Medicine. This context permitted the leveraging of resources in the form of faculty and students to assist in dental screenings and health promotion activities, and better ensured high participation rates for the involved community partners, because of the ongoing relationships between the college and the administrators and staff at the involved senior centers.
Our study limitations were that the assessments reported were restricted by the field nature of the study. Furthermore, older adults who were home-bound or institutionalized were not included in the study. Finally, because of logistical constraints, not all older adults who might have otherwise been willing to be screened for HbA1c were accommodated when the primary care activities were initially implemented.
Future Needs
Advances in public health, medicine, and dentistry have led to increased life spans for populations worldwide, but also to greater inequities between those with and without means. As people age, chronic noncommunicable diseases become more prevalent,14,28 and numbers of missing teeth may begin to accumulate, absent quality dental care.13 In a summary way, the number of missing teeth in one’s mouth reflects that person’s economic and health history over the life course,29 because higher numbers of missing teeth are related to socioeconomic position, health behaviors, and intelligence.8,30,31 Loss of teeth may lead to pain and difficulty chewing, decreased consumption of fruits and vegetables, lower intake of key nutrients, and ultimately, unintentional weight loss,32 or in some cases, weight gain and obesity.33
Using US national data for older adults, Griffin et al.21 found racial/ethnic and income disparities in untreated dental disease and oral health–related quality of life. On the basis of these findings, they argued that public health priorities ought to include better integrating oral health into medical care, implementing community programs to promote healthy behaviors and improve access to preventive services, developing a comprehensive strategy to address the oral health needs of the homebound and long-term care residents, and assessing the feasibility of ensuring a safety net that covers preventive and basic restorative services to eliminate pain and infection. Because of the potential for screening and referral of urban racial/ethnic minority adults in community-based settings, ElderSmile might prove to be a place-based model for improving access to care, especially if policies to support the integration of public health, medical, and dental services (Figure 1) are realized.
Acknowledgments
The authors were supported in the research, analysis, and writing of this article by the National Institute for Dental and Craniofacial Research and the Office of Behavioral and Social Sciences Research of the National Institutes of Health (grant R21DE021187, titled “Leveraging Opportunities to Improve Oral Health in Older Adults,” and grant R01DE023072, titled “Integrating Social and Systems Science Approaches to Promote Oral Health Equity”). The Fan Fox and Leslie R. Samuels Foundation and The Legacy Foundation provided major funding for the diabetes and hypertension educational and screening components of the ElderSmile program.
Human Participant Protection
All appropriate Columbia University, New York University, and University at Buffalo institutional review board and Health Insurance Portability and Accountability Act safeguards were followed.
References
- 1.Joshipura KJ, Ritchie C. Can the relation between tooth loss and chronic disease be explained by socio-economic status? Eur J Epidemiol. 2005;20(3):203–204. doi: 10.1007/s10654-005-1232-3. [DOI] [PubMed] [Google Scholar]
- 2.Lamster IB, Kunzel C, Lalla E. Diabetes mellitus and oral health care: time for the next step. J Am Dent Assoc. 2012;143(3):208–210. doi: 10.14219/jada.archive.2012.0131. [DOI] [PubMed] [Google Scholar]
- 3. Institute of Medicine of the National Academies. Improving Access to Oral Health Care for Vulnerable and Underserved Populations. 2011. Available at: http://www.iom.edu/Reports/2011/Improving-Access-to-Oral-Health-Care-for-Vulnerable-and-Underserved-Populations.aspx. Accessed January 3, 2014.
- 4.Lamster IB, Northridge ME, editors. Improving Oral Health for the Elderly: An Interdisciplinary Approach. New York, NY: Springer; 2008. [Google Scholar]
- 5.Lamster IB. Oral health care services for older adults: a looming crisis. Am J Public Health. 2004;94(5):699–702. doi: 10.2105/ajph.94.5.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Northridge ME, Lamster IB. A lifecourse approach to preventing and treating oral disease. Soz Praventivmed. 2004;49(5):299–300. doi: 10.1007/s00038-004-4040-8. [DOI] [PubMed] [Google Scholar]
- 7.Marshall S, Northridge ME, De La Cruz LD, Vaughan RD, O’Neil-Dunne J, Lamster IB. ElderSmile: a comprehensive approach to improving oral health for seniors. Am J Public Health. 2009;99(4):595–599. doi: 10.2105/AJPH.2008.149211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sabbah W, Mortensen LH, Sheiham A, Batty GD. Oral health as a risk factor for mortality in middle-aged men: the role of socioeconomic position and health behaviours. J Epidemiol Community Health. 2013;67(5):392–397. doi: 10.1136/jech-2012-201340. [DOI] [PubMed] [Google Scholar]
- 9.Desvarieux M, Demmer RT, Rundek T et al. Relationship between periodontal disease, tooth loss, and carotid artery plaque: the Oral Infections and Vascular Disease Epidemiology Study (INVEST) Stroke. 2003;34(9):2120–2125. doi: 10.1161/01.STR.0000085086.50957.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choe H, Kim YH, Park JW, Kim SY, Lee SY, Jee SH. Tooth loss, hypertension and risk for stroke in a Korean population. Atherosclerosis. 2009;203(2):550–556. doi: 10.1016/j.atherosclerosis.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 11.Okoro CA, Balluz LS, Eke PI et al. Tooth loss and heart disease: findings from the Behavioral Risk Factor Surveillance System. Am J Prev Med. 2005;29(5, suppl 1):50–56. doi: 10.1016/j.amepre.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 12.Kaur G, Holtfreter B, Rathmann W et al. Association between type 1 and type 2 diabetes with periodontal disease and tooth loss. J Clin Periodontol. 2009;36(9):765–774. doi: 10.1111/j.1600-051X.2009.01445.x. [DOI] [PubMed] [Google Scholar]
- 13.Patel MH, Kumar JV, Moss ME. Diabetes and tooth loss: an analysis of data from the National Health and Nutrition Examination Survey, 2003–2004. J Am Dent Assoc. 2013;144(5):478–485. doi: 10.14219/jada.archive.2013.0149. [DOI] [PubMed] [Google Scholar]
- 14.Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis. 2013;10:E65. doi: 10.5888/pcd10.120203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marshall SE, Cheng B, Northridge ME, Kunzel C, Huang C, Lamster IB. Integrating oral and general health screening at senior centers for minority elders. Am J Public Health. 2013;103(6):1022–1025. doi: 10.2105/AJPH.2013.301259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Northridge ME, Ue FV, Borrell LN et al. Tooth loss and dental caries in community-dwelling older adults in northern Manhattan. Gerodontology. 2012;29(2):e464–e473. doi: 10.1111/j.1741-2358.2011.00502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Northridge ME, Chakraborty B, Kunzel C, Metcalf S, Marshall S, Lamster IB. What contributes to self-rated oral health among community-dwelling older adults? Findings from the ElderSmile program. J Public Health Dent. 2012;72(3):235–245. doi: 10.1111/j.1752-7325.2012.00313.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Widener MJ, Metcalf SS, Northridge ME, Chakraborty B, Marshall SE, Lamster IB. Exploring the role of peer density in the self-reported oral health outcomes of older adults: a kernel density based approach. Health Place. 2012;18(4):782–788. doi: 10.1016/j.healthplace.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Widener MJ, Northridge ME, Chakraborty B et al. Spatial patterns of diabetes and hypertension in older adults: exploratory findings based upon screening data from the ElderSmile program. Am J Prev Med. 2014;46(6):643–648. doi: 10.1016/j.amepre.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dye BA, Tan S, Smith V et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007;248:1–92. [PubMed] [Google Scholar]
- 21.Griffin SO, Jones JA, Brunson D, Griffin PM, Bailey WD. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health. 2012;102(3):411–418. doi: 10.2105/AJPH.2011.300362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. Recent Advances in Oral Health. WHO Technical Report Series No. 826. Geneva, Switzerland: World Health Organization; 1992. pp. 16–17. [PubMed] [Google Scholar]
- 23. US National Library of Medicine. Medline Plus. HbA1c. Available at: http://www.nlm.nih.gov/medlineplus/ency/article/003640.htm. Accessed December 17, 2013.
- 24. US National Heart, Lung and Blood Institute. What is high blood pressure? Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/hbp. Accessed December 17, 2013.
- 25.Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and Proportions. 3rd ed. Hoboken, NJ: John Wiley & Sons; 2003. [Google Scholar]
- 26.SAS Institute, Inc. SAS/STAT 9.1 User’s Guide. Cary, NC: SAS Institute, Inc.; 2004. [Google Scholar]
- 27.James PA, Oparil S, Carter BL et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 28.Metcalf SS, Northridge ME, Lamster IB. A systems perspective for dental health in older adults. Am J Public Health. 2011;101(10):1820–1823. doi: 10.2105/AJPH.2011.300321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holm-Pedersen P, Schultz-Larsen K, Christiansen N, Avlund K. Tooth loss and subsequent disability and mortality in old age. J Am Geriatr Soc. 2008;56(3):429–435. doi: 10.1111/j.1532-5415.2007.01602.x. [DOI] [PubMed] [Google Scholar]
- 30.Starr JM, Hall R. Predictors and correlates of edentulism in healthy older people. Curr Opin Clin Nutr Metab Care. 2010;13(1):19–23. doi: 10.1097/MCO.0b013e328333aa37. [DOI] [PubMed] [Google Scholar]
- 31.Vos T, Flaxman AD, Naghavi M et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sheiham A, Steele JG, Marcenes W et al. The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res. 2001;80(2):408–413. doi: 10.1177/00220345010800020201. [DOI] [PubMed] [Google Scholar]
- 33.de Oliveira Bernardo C, Boing AF. de Assis Guedes de Vasconcelos FA, Peres KG, Peres MA. Association between tooth loss and obesity in Brazilian adults: a population-based study. Rev Saude Publica. 2012;46(5):834–842. doi: 10.1590/s0034-89102012000500010. [DOI] [PubMed] [Google Scholar]