Abstract
Homeless women have disproportionately lower rates of cervical cancer screening and higher rates of cervical cancer. In 2008, only 19% of the homeless women seen by Boston Health Care for the Homeless Program (BHCHP) were screened for cervical cancer. To improve screening, BHCHP implemented a 6-part intervention that incorporates point-of-care service, multidisciplinary screening, improved health maintenance forms, population management, process improvement, and increased provider and patient education. This resulted in a significant increase in cervical cancer screening, from 19% in 2008 to 50% in 2013. When compared with national and local cervical cancer screening trends, BHCHP surpassed improvement rates seen in other vulnerable populations. Simple and innovative interventions proved to be the most effective and practical methods of improving screening.
KEY FINDINGS
▪ The shift from standard practice of scheduled cancer screening appointments to a patient-centric approach using simple initiatives implemented with process improvement techniques to assess efficacy and promote spread resulted in a dramatic improvement in cervical cancer screening rates among homeless women at the Boston Health Care for the Homeless Program.
▪ Use of a 6-step approach for improving cervical cancer screening resulted in a statistically significant and clinically meaningful increase from 19% in 2008 to 50% in 2013 (P < .001).
Cervical cancer is the fourth most common cancer among women in the United States, with 11 818 new cases and 3939 deaths in 2010.1 It is one of the few cancers for which appropriate screening is cost efficient and effective. The average rate of cervical cancer screening for US women between ages 21 and 65 years is 83%2 with a mortality rate of 2.4 deaths per 100 000 women.3 However, homeless women have disproportionately lower rates of screening and higher rates of cervical cancer. Rates of cervical cancer screening among homeless women average 50%,4–6 with mortality rates as high as 7.2 deaths per 100 000 women.7
Homeless women face unique barriers to preventive medical care such as competing priorities of finding daily food and shelter,8 substance use,9 and a high prevalence of physical and sexual trauma.10,11 Previous studies have found that a higher percentage of homeless women do not receive adequate preventive health care12 and have up to a 10 times greater risk of dying than do women in the general population.13 Successful prevention of cervical cancer will depend on innovative, nontraditional methods to reach these vulnerable women.
PROGRAM DESCRIPTION
Boston Health Care for the Homeless Program (BHCHP) is a not-for-profit organization that has been providing health care services to homeless individuals in Boston, Massachusetts, for almost 30 years. The program provides primary and episodic care at 70 community sites and serves more than 12 500 homeless patients a year, 4000 of whom are women. BHCHP has been tracking routine health care quality indicators for more than 10 years and is committed to a patient-centered model of care that brings preventive health services to nontraditional community venues such as street outreach and shelter-based clinics. Despite access to cervical cancer screening, the baseline data for BHCHP women in 2008 showed that only 19% of the eligible women were appropriately screened for cervical cancer. Homeless women face many barriers to screening including competing priorities of daily living, transient living situations, and limited capacity to follow up because of infrequent telephone or mail access.
To improve cervical cancer screening rates, BHCHP designed a systematic approach to incorporate women’s preventive health quality improvement into the existing program. Interventions were based on prevous trials at improving preventive health care, as well as years of clinical experience with this population.
Previous studies showed that up to 38% of homeless women refuse a Papanicolaou test, even when commonly cited obstacles of access and cost are removed.14 Because homeless women face unique barriers to obtaining screenings, we developed a 6-part intervention to improve this quality measure as part of a women’s health initiative. This included expanding the point-of-care screening options, using a multidisciplinary screening strategy, enhancing health maintenance features in the electronic health records, developing process improvement initiatives, creating patient registries for a population management approach, and increasing both provider and patient education.
METHODS
Over a 5-year period, we used this novel approach to engagement and delivery of women’s health services to measure the baseline and interval improvement in women’s health indicators. We collected baseline data on cervical cancer screening rates in 2008 according to the Human Resources and Services Administration criteria for screening. This Uniform Data System is a Human Resources and Services Administration reporting requirement for community health centers and health care for the homeless grantees. The Uniform Data System cervical cancer screening criteria measure the percentage of patients aged 21 to 64 years who have been screened with 1 or more Papanicolaou tests within the last 3 years. To have a point of comparison, we reviewed several existing databases, including the Uniform Data System (Massachusetts and national) and a local urban hospital database.
We used the χ2 test to analyze for a statistically significant difference with a significance level of P < .05. We used SAS version 9.3 (SAS Institute, Cary, NC) for data analysis.
RESULTS
Use of the 6-step approach for improving cervical cancer screening resulted in a statistically significant and clinically meaningful increase from 19% in 2008 to 50% in 2013 (P < .001). We completed several subgroup stratified analyses that compared the group from 2008 and 2013 (Table 1). We found that the improvements in cervical cancer screening remained significant across all age groups and races. Behavioral health disorders can sometimes be a barrier to preventive health screening, but we also saw significant improvement in screening rates in women with behavioral health disorders.
TABLE 1—
Boston Health Care for the Homeless Program (BHCHP) Population Papanicolaou Test Rates: Boston, MA, 2008 vs 2013
| 2008, No. (%) |
2013, No. (%) |
||||
| BHCHP Population | Total (n = 2552) | Up-to-Date Pap Test | Total (n = 2882) | Up-to-Date Pap Test | % Increase in Pap Test Rate |
| Age, y | |||||
| 21−29 | 658 (26) | 62 (9) | 719 (25) | 445 (62) | 85** |
| 30−39 | 576 (23) | 102 (18) | 611 (21) | 354 (58) | 69** |
| 40−49 | 722 (28) | 224 (31) | 636 (22) | 372 (58) | 47** |
| 50−59 | 471 (18) | 160 (34) | 734 (25) | 384 (52) | 35** |
| ≥60 | 76 (3) | 19 (25) | 181 (6) | 68 (38) | 34* |
| Patient-reported race | |||||
| Black or African American | 777 (30) | 200 (26) | 944 (33) | 541 (57) | 54** |
| White | 1126 (44) | 268 (24) | 1292 (45) | 712 (55) | 56** |
| Other | 650 (25) | 101 (16) | 646 (22) | 370 (57) | 72** |
| Behavioral health diagnosis prevalence | 1317 (52) | 349 (26) | 1686 (59) | 1040 (62) | 58** |
Note. Pap = Papanicolaou.
*P = .05.
**P < .001.
Boston Health Care for the Homeless Program (BHCHP) 6-Part Cervical Cancer Screening Intervention
| 1. Point-of-care service | 4. Process improvement | |
| Trained nurses and providers to treat every medical encounter as an opportunity for cervical cancer screening. | Standardized Papanicolaou test trays were stocked and stationed in all clinic rooms to improve efficiency. | |
| Urgent and episodic care visits were used to discuss and address cervical cancer screening with patients. | Staff members were encouraged to share best practices and pilot process improvement cycles. | |
| Bilingual appointment reminder slips were placed on patient pillows at shelter sites. | ||
| 2. Multidisciplinary screening | 5. Population management | |
| Behavioral health and primary care services are integrated with a team focus on preventive health care needs. | Teams, sites, and providers distributed transparent quality indicator comparative dashboards. | |
| Nonclinical staff and nurses became part of the inquiry process for cervical cancer screening. | Patient registries were used by staff across sites during team case conferencing, in team huddles, and in direct street and shelter outreach to encourage screening. | |
| Front desk staff at outreach sites assisted patients with preventive care needs assessment surveys. | Front desk staff combined appointment reminder reports and preventive care reports in patient outreach calls. | |
| Cervical cancer screening questions were integrated in core nursing standards. | Teams used huddle reports to conduct previsit preparations for patients with preventive and chronic care needs. | |
| Community support workers and case managers were also incorporated into screening inquiry process. | ||
| 3. Health maintenance form in the electronic health record (EHR) | 6. Provider and patient education | |
| Updated health maintenance form in EHR enhanced visual trigger for providers. | Provider: | |
| Up-to-date measures were in green, and out-of-date measures were in red. | Experts in the field of cervical cancer screening were invited to grand rounds and other teaching events. | |
| Quality measures could be assessed by a multidisciplinary team, including RNs and MAs, during all visits through the EHR. | Providers were offered refresher courses on cervical cancer screening techniques. | |
| Documentation of data in structured fields allowed for efficient aggregation and analysis for data-driven process improvement initiatives. | Patient: | |
| Papanicolaou test day health fairs offered same-day Papanicolaou tests. | ||
| Culturally and linguistically appropriate brochures and posters were created and disseminated by BHCHP’s quality team. | ||
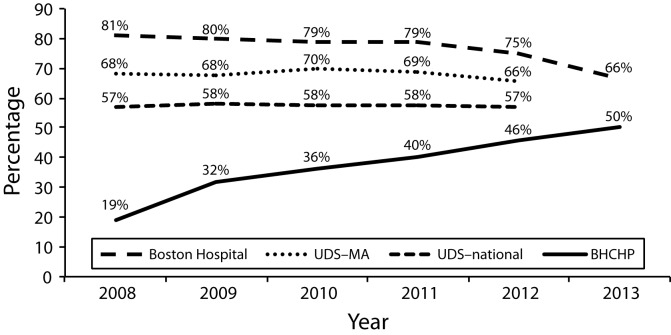
We did find some small statistically significant differences in the 2008 and 2013 population characteristics (data not shown). To help verify that the changes were related to our intervention, comparisons to national and locally available screening rates indicated that the improvement in BHCHP patient screening rates surpassed improvements in other vulnerable population groups (Figure 1).
FIGURE 1—
Boston Hospital, Uniform Data System (UDS) Massachusetts, UDS National, and Boston Health Care for the Homeless Program (BHCHP) cervical cancer screening trend data: 2008–2013.
Note. Percentage of eligible women who received 1 or more Papanicolaou tests in the past 3 years. Eligible women are those between 21 and 69 years of age seen for a medical visit in the past year. Exclusion criteria include women who have had a hysterectomy.
DISCUSSION
This 6-step approach to improving cervical cancer screening for homeless women was effective in improving screening rates for homeless women in Boston. Gaps in care were closed, and significant improvements in cervical cancer screening were reported with all subgroups of the study population. The importance of an integrated behavioral health and primary care model was also highlighted with the improvement extending to women with behavioral health diagnoses. Furthermore, our data showed that screening rate improvements in our group were considerably higher than those reported among similar groups of women at a local, state, and national level.
Lessons Learned From the Field
| Competing priorities |
| The biggest challenge has been prioritizing a patient’s agenda while addressing preventive care in every visit. Urgent competing priorities, including access to food, shelter, and safety, can overshadow preventive care. Including community support workers and case managers in the screening inquiry process has helped ease the burden for the clinical team. |
| Documentation practices |
| Standardizing documentation has been crucial to quality reporting through our electronic medical record. This has allowed us to monitor and report our progress sitewide and programwide. |
| Simple and creative interventions |
| Encouraging staff members to think of simple and creative interventions and providing venues to share best practices has been successful in reaching patients. |
| Having open access clinics for preventive health care is important. |
| Accomplishing follow-up |
| Patients should be informed of open access clinic hours, allowing options of when and where to receive their results. |
| Access to medical records should be provided via shared electronic health record across sites |
| A network approach should be implemented for contacting a patient by intentional redundancy |
| Trauma-informed care |
| Incorporating trauma-informed care to cervical cancer screening is key to building a comfortable, safe environment for the patient. |
| Such care included engaging in open conversations about a patient’s history, explaining the examination procedure, and addressing behavioral health needs. |
| Involve all stakeholders |
| Clinical and nonclinical staff must be educated about quality metrics and connecting them to the mission of the program. |
| The culture of process improvement must be infused throughout the program. |
| Multiple clinic staff should ask about and document screenings electronically. |
| Staff should collaborate with patients’ behavioral health care providers. |
| The strength of existing staff and patient trusting relationships can be used to educate staff and patients. |
Our study was potentially limited in that the observed improvement in our screening rates could be explained by factors other than our intervention, including changes in our population’s characteristics. However, population changes over the 5-year period were minor, and significant improvement occurred in all subgroups. Furthermore, comparable groups did not have similar improvements. We therefore believe that the observed improvement was likely related to our intervention.
The shift from standard practice of scheduled cancer screening appointments to a patient-centric approach using simple initiatives implemented with process improvement techniques to assess efficacy and promote spread resulted in a dramatic improvement in cervical cancer screening rates among homeless women at BHCHP. With many states undergoing Medicaid expansion under the Affordable Care Act, more vulnerable populations will have access to health insurance. However, our findings indicated that service access alone does not ensure use. Most homeless women in Boston had health insurance in 2008, but the cervical cancer screening rate was only 19%. Effective screening had to be tailored to address the unique stressors that homeless women face. This included offering screening at times when women could prioritize their medical care, culturally competent education on the importance of screening, and a multidisciplinary approach. Other vulnerable populations will need similar innovative approaches to improve cancer screening rates and eliminate disparities. Fortunately, the interventions that worked the best were simple process improvement enhancements and teamwork. The tenets of our process can be used by others to incorporate quality improvement into practice for other vulnerable populations.
Acknowledgments
The authors wish to acknowledge Robin E. Clark, PhD, at the University of Massachusetts Medical School for his insight and expertise.
Human Participant Protection
The Boston University Medical Center institutional review board has reviewed and approved this study as exempt.
References
- 1.US Cancer Statistics Working Group. United States Cancer Statistics: 1999–2011 Incidence and Mortality Web-Based Report. Atlanta, GA: Centers for Disease Control and Prevention and National Cancer Institute; 2014. [Google Scholar]
- 2.Cancer Prevention & Early Detection Facts & Figures 2013. Atlanta, GA: American Cancer Society; 2013. [Google Scholar]
- 3.Chasan R, Manrow R. Cervical cancer. National Institutes of Health Fact Sheet. 2010. Available at: http://report.nih.gov/nihfactsheets/viewfactsheet.aspx?csid=76. Accessed September 9, 2014.
- 4.Chau S, Chin M, Chang J et al. Cancer risk behaviors and screening rates among homeless adults in Los Angeles County. Cancer Epidemiol Biomarkers Prev. 2002;11:431–438. [PubMed] [Google Scholar]
- 5.Long HL, Tulsky JP, Chambers DB et al. Cancer screening in homeless women: attitudes and behaviors. J Health Care Poor Underserved. 1998;9:276–292. doi: 10.1353/hpu.2010.0070. [DOI] [PubMed] [Google Scholar]
- 6.Diamant AL, Brook RH, Fink A, Gelberge L. Use of preventive services in a population of very low-income women. J Health Care Poor Underserved. 2002;13:151–163. doi: 10.1353/hpu.2010.0552. [DOI] [PubMed] [Google Scholar]
- 7.Hogenmiller JR, Atwood JR, Lindsey AM, Johnson DR, Hertzog M, Scott JC. Self-efficacy scale for Pap smear screening participation in sheltered women. Nurs Res. 2007;56(6):369–377. doi: 10.1097/01.NNR.0000299848.21935.8d. [DOI] [PubMed] [Google Scholar]
- 8.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–220. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bassuk EL, Weinreb LF, Buckner JC, Browne A, Salomon A, Bassuk SS. The characteristics and needs of sheltered homeless and low-income housed mothers. JAMA. 1996;276(8):640–646. [PubMed] [Google Scholar]
- 10.Wenzel SL, Leake BD, Gelberg L. Health of homeless women with recent experience of rape. J Gen Intern Med. 2000;15(4):265–268. doi: 10.1111/j.1525-1497.2000.04269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wenzel SL, Koegel P, Gelberg L. Antecedents of physical and sexual victimization among homeless women: a comparison to homeless men. Am J Community Psychol. 2000;28(3):367–390. doi: 10.1023/A:1005157405618. [DOI] [PubMed] [Google Scholar]
- 12.Lewis JH, Andersen RM, Gelberg L. Health care for homeless women. J Gen Intern Med. 2003;18(11):921–928. doi: 10.1046/j.1525-1497.2003.20909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheung AM, Hwang SW. Risk of death among homeless women: a cohort study and review of the literature. CMAJ. 2004;170(8):1243–1247. doi: 10.1503/cmaj.1031167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bharel M, Casey C, Wittenberg E. Disparities in cancer screening: acceptance of Pap smears among homeless women. J Womens Health (Larchmt) 2009;18(12):2011–2016. doi: 10.1089/jwh.2008.1111. [DOI] [PubMed] [Google Scholar]