Abstract
Objectives. We determined the factors that affect naloxone (Narcan) administration in drug overdoses, including the certification level of emergency medical technicians (EMTs).
Methods. In 2012, 42 states contributed all or a portion of their ambulatory data to the National Emergency Medical Services Information System. We used a logistic regression model to measure the association between naloxone administration and emergency medical services certification level, age, gender, geographic location, and patient primary symptom.
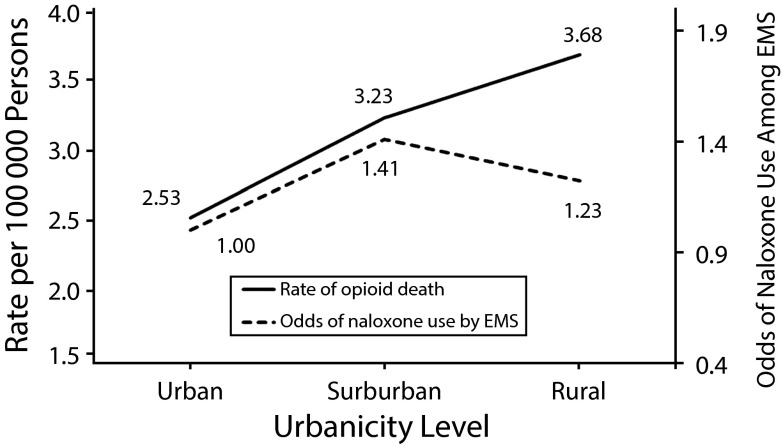
Results. The odds of naloxone administration were much higher among EMT-intermediates than among EMT-basics (adjusted odds ratio [AOR] = 5.4; 95% confidence interval [CI] = 4.5, 6.5). Naloxone use was higher in suburban areas than in urban areas (AOR = 1.41; 95% CI = 1.3, 1.5), followed by rural areas (AOR = 1.23; 95% CI = 1.1, 1.3). Although the odds of naloxone administration were 23% higher in rural areas than in urban areas, the opioid drug overdose rate is 45% higher in rural communities.
Conclusions. Naloxone is less often administered by EMT-basics, who are more common in rural areas. In most states, the scope-of-practice model prohibits naloxone administration by basic EMTs. Reducing this barrier could help prevent drug overdose death.
Drug overdose is a major cause of injury-related death in the United States.1 In 2011, the number of deaths associated with opioid prescription pain relievers was 16 917,2 and an additional 4397 deaths were heroin-related.3 In addition to death, the burden of lost productivity and medical costs associated with opioid-related poisoning is $20.4 billion annually (in 2009 dollars).4 The growing number of overdose deaths suggests that primary prevention efforts need to be strengthened and augmented. In an effort to reduce deaths through any means available, recent attention has focused on the ability of emergency medical services (EMS) providers to save lives at the scene of an opioid drug overdose.
In addition to life support measures to ensure adequate airway support, breathing, and circulation, many EMS providers are equipped with an opioid antagonist medication, naloxone, that can be used to treat respiratory depression in suspected opioid overdose patients. According to 1 study, naloxone is the drug most commonly administered to adolescents in the prehospital setting.5 Prehospital use of this drug is routine,6 serious adverse effects are rare, and it has no abuse potential.7
The drug overdose mortality rate rose 159% in nonmetropolitan rural counties between 1999 and 2004, compared with 54% in metropolitan counties.8 Rural EMS, covering about 20% of the population and 80% of the land mass of the United States,9 are starkly different from urban and suburban EMS. In addition to longer response times,10 major challenges in rural EMS include, but are not limited to, personnel shortages, inadequate advanced training opportunities for EMS response staff, antiquated equipment (e.g., communications equipment), poor public access to EMS, and an absence of regionalized systems of specialized EMS care, such as trauma systems.11
Guidance on EMS administration of pharmaceuticals is contained in the national EMS scope-of-practice model.12 States are free to create their own guidance and protocols; however, most states follow this model. This guidance limits basic life support personnel, including people certified as emergency medical technician–basic (EMT-basic), to assisting patients in taking their own prescribed medications and glucose and aspirin orally. Only advanced life support personnel are permitted to administer naloxone. However, basic life support providers can often be the first responders on the scene in cases of opioid overdose, particularly in rural communities. The availability and dispatch of EMS resources to the scene of an injury or illness is multifactorial and depends on the details of the emergency and anticipated resource requirements, available personnel and equipment, and location of the event.
In adherence to the national scope-of-practice policy guidance, 38 states prohibit EMT-basics from administering parenteral pharmacotherapies.13 In the 12 states that allow EMT-basics to administer naloxone, it is frequently administered intranasally and not by injection. In all states, only advanced life support providers are permitted to initiate intravenous access and administer intravenous medications, including naloxone. In cases of opioid overdose, if EMS providers do not have someone authorized to administer naloxone, the patient may be at a higher risk of death. Recognizing this barrier to naloxone administration, some authors have suggested more widespread use of intranasal naloxone by non–advanced life support providers.13,14 Other researchers have reported that dispatching of EMT-basics results in underuse of naloxone.15
EMS providers operate by following protocols for medical care and administration of medications. These protocols are approved by a local, regional, or state medical director. These clinical protocols direct the actions and interventions of EMS providers on scene and in transport, and they include the collection and use of physiological data (low respiration rate, decreased responsiveness, pupil dilatation, and other signs, including cardiac arrest)16 along with other information (i.e., drug paraphernalia at scene and bystander-provided information) to make a determination of suspected opioid overdose. Although 29 states have established statewide protocols for naloxone administration, only 12 states allow EMT-basic personnel to administer naloxone. In many cases, variability occurs at the regional or local level.17 Standard uniform guidance on naloxone administration does not exist, and published guidance varies across localities and states.
Smaller rural communities have a much higher proportion of EMT-basic personnel.18 Authorizing these EMS personnel to administer naloxone to patients thought to have an opioid overdose will result in fewer deaths. However, the magnitude of this certification barrier to naloxone administration is largely unknown. Whether certification issues among EMS providers have a disproportionate impact on rural areas is also unclear. In addition, major signs or symptoms that contribute to a preliminary diagnosis of overdose by EMS personnel at the injury scene are generally unknown. In this study, we examined the factors that were associated with naloxone administration and that may assist states in reviewing policy on naloxone administration and reduce mortality at the scene of injury in the case of a suspected opioid drug overdose.
METHODS
We examined aggregate data from the National Emergency Medicine Service Information System (NEMSIS), which is funded by the National Highway Traffic Safety Administration. Complete or partial data contributed by 42 states are consolidated to create the NEMSIS data set, which contains demographic data, basic 911 call information, details about the scene of injury or illness, medications administered, and other variables recorded by EMS. The data set is a convenience sample that is not weighted to reflect national estimates. The 2012 NEMSIS data set contained 19.8 million records of EMS events, most prompted by 911 calls.
Identifying Relevant Records
We identified suspected drug cases in the NEMSIS data in which naloxone was administered by means of 2 criteria. We included the record if, first, the dispatch complaint indicated that there was a drug overdose and, second, if the EMS provider recorded the injury cause as a drug overdose. When EMS providers arrive at an injury scene, they use clues about the environment, information about the dispatched call, and patient symptoms to determine whether a drug overdose has occurred.
Cases meeting these criteria tend to be accurately assessed as drug overdoses, and other studies have used this approach.19,20 In this study, we included only EMS events prompted by 911 calls to capture events associated with EMS decision-making and eliminate hospital-to-hospital EMS transports.
Measures Used and Statistical Analysis
The independent variables of the study included demographic (age, gender), clinical (provider’s impression, primary symptom), and EMS informational variables (EMS certification level and urbanicity). We categorized urbanicity into 4 different groups (urban, suburban, rural, and wilderness) on the basis of an urban influence coding system used by the US Department of Agriculture and the Office of Management and Budget. These codes take into account county population size, degree of urbanization, and adjacency to a metropolitan area or areas. This variable was part of the NEMSIS research data set. For a detailed description of code composition, see the National Emergency Services Information System, “National Elapsed Patient Care Times by Urbanicity.”21
To determine overdose mortality within levels of urbanicity, we obtained injury summary data from a published source8 and averaged opioid deaths by level of urbanization. For a measure of urban mortality, we averaged together the rate for large central metropolitan (large central metro) area and large fringe metropolitan (large fringe metro) area. For a measure of suburban mortality, we averaged the rates for medium metropolitan and small metropolitan area. For a measure of rural mortality, we averaged the rates of rural micropolitan and noncore areas. We visually compared these mortality rates with the odds of naloxone administration. All independent variables were categorical. EMS provider level is defined by NEMSIS, using the National Highway Traffic Safety Administration’s National Standard Curriculum, categorized as first responder, EMT-basic, EMT-intermediate, and EMT-paramedic. The EMS agency provided the level of service of the highest credentialed provider for each EMS encounter. The outcome variable for this study was whether the EMS provider administered naloxone.
We analyzed the factors that influenced naloxone administration in suspected drug poisoning events using a standard logistic regression model without stepwise procedures. The results of the logistic regression are presented as adjusted odds ratios (AORs) with 95% confidence intervals (CIs) and P values. We used SAS statistical software version 9.3 for the data analysis.22
RESULTS
We found that of the 19.8 million NEMSIS events, 15 794 779 were prompted by emergency 911 calls. Using our definition of suspected drug overdose events yielded 262 676 EMS events. Thus, approximately 1.7% of all 911 calls requiring EMS services involved a drug overdose. Among these events, naloxone was administered 16 250 times (6.2%). The most common primary symptom that led to naloxone administration was change in responsiveness (n = 9525; 59%).
In cases in which gender was known, drug poisoning cases were more common among males (46.2%; 52.4% among males and females overall; Table 1). Also, drug poisoning was more common among people aged 0 to 19 years (26.1%) and overwhelmingly occurred in urban areas (82.1%). The most common level of certification among responders was EMT-paramedic (84.7%).
TABLE 1—
Demographic and Injury Characteristics of Suspected Drug Poisoning Cases: National Emergency Medicine Service Information System, United States, 2012
| Characteristic | No. (%) |
| Gender | |
| Female | 110 099 (41.9) |
| Male | 121 288 (46.2) |
| Unknown | 31 289 (11.9) |
| Age, y | |
| 0–19 | 68 479 (26.1) |
| 20–29 | 52 871 (20.1) |
| 30–39 | 40 462 (15.4) |
| 40–49 | 43 276 (16.5) |
| 50–59 | 36 331 (13.8) |
| 60–99 | 21 257 (8.1) |
| Urbanicitya | |
| Urban | 215 606 (82.1) |
| Suburban | 17 941 (6.8) |
| Rural | 21 149 (8.1) |
| Wilderness | 4 738 (1.8) |
| Unknown | 3 242 (1.2) |
| Level of service | |
| EMT–basic | 16 821 (6.4) |
| EMT–intermediate | 4 676 (1.8) |
| EMT–paramedic | 222 545 (84.7) |
| Nurse | 6 221 (2.4) |
| Physician | 3 966 (1.5) |
| Unknown | 8 447 (3.2) |
Note. EMT = emergency medical technician. Totals may not add up to 262 676 because of missing values. Percentages are subject to rounding error.
We categorized urbanicity based on an urban influence coding system used by the US Department of Agriculture and the Office of Management and Budget. These codes take into account county population size, degree of urbanization, and adjacency to a metropolitan area or areas.
We used logistic regression to assess the factors associated with naloxone administration. Our logistic regression model used approximately 83% of the records; the remaining 17% had 1 or more missing values for analysis. The model had a 78.9% concordance rate, indicating that it correctly predicted EMS transport decisions 78.9% of the time. Using the area under the curve c statistic, we found the logistic regression model to be statistically significant (c = 0.797; cutoff = 0.7).23
In examining the odds of naloxone administration within gender, we found that males were less likely to receive naloxone than females (AOR = 0.92; 95% CI = 0.89, 0.95; Table 2). Compared with the 0 to 19 years age group, the odds of naloxone administration were highest for the 20 to 29 years age group (AOR = 2.51; 95% CI = 2.34, 2.71) and lowest for the 60 to 99 years age group (AOR = 1.83; 95% CI = 1.67, 2.01). Using urbanicity as a reference point, the odds of naloxone administration were highest in the suburbs (AOR = 1.41; 95% CI = 1.32, 1.51), followed by rural environments (AOR = 1.23; 95% CI = 1.15, 1.30). The odds of naloxone administration in the wilderness were not significant.
TABLE 2—
Logistic Regression Analysis Factors Associated With Naloxone Administration Among Emergency Medical Services Providers: National Emergency Medical Service Information System, United States, 2012
| Variable | AOR (95% CI) | P |
| Gender | ||
| Female (Ref) | 1.00 | |
| Male | 0.92 (0.89, 0.95) | < .001 |
| Age, y | ||
| 0–19 (Ref) | 1.00 | |
| 20–29 | 2.51 (2.34, 2.71) | < .001 |
| 30–39 | 2.38 (2.21, 2.57) | < .001 |
| 40–49 | 2.01 (1.86, 2.17) | < .001 |
| 50–59 | 1.94 (1.79, 2.10) | < .001 |
| 60–99 | 1.83 (1.67, 2.01) | < .001 |
| Urbanicitya | ||
| Urban (Ref) | 1.00 | |
| Rural | 1.23 (1.15, 1.30) | < .001 |
| Suburban | 1.41 (1.32, 1.51) | < .001 |
| Wilderness | 1.12 (0.99, 1.27) | .07 |
| Primary symptom | ||
| None (Ref) | 1.00 | |
| Bleeding | 0.70 (0.30, 1.38) | .36 |
| Breathing problems | 20.13 (16.93, 24.01) | < .001 |
| Change in responsiveness | 13.70 (11.90, 15.88) | < .001 |
| Choking | 2.18 (0.36, 7.03) | .28 |
| Death | 23.34 (17.86, 30.41) | < .001 |
| Device or equipment problem | <0.001 (—, 7.96) | .97 |
| Diarrhea | <0.001 (—, 1.07) | .92 |
| Drainage or discharge | <0.001 (—, 5.65) | .95 |
| Fever | 5.05 (1.94, 10.82) | < .001 |
| Malaise | 1.95 (1.50, 2.51) | < .001 |
| Mass or lesion | 0.97 (0.06, 4.45) | .98 |
| Mental or psych | 1.59 (1.35, 1.87) | < .001 |
| Nausea or vomiting | 1.05 (0.82, 1.33) | .71 |
| Pain | 0.61 (0.45, 0.81) | < .001 |
| Palpitations | 0.87 (0.34, 1.80) | .73 |
| Rash or itching | <0.001 (—, 0.63) | .88 |
| Swelling | 0.78 (0.13, 2.46) | .72 |
| Transport only | 0.45 (0.21, 0.82) | .02 |
| Unknown | 3.28 (2.84, 3.80) | < .001 |
| Weakness | 1.81 (1.49, 2.21) | < .001 |
| Wound | 0.49 (0.08, 1.55) | .32 |
| Level of service | ||
| EMT–basic (Ref) | 1.00 | |
| EMT–intermediate | 5.45 (4.55, 6.54) | < .001 |
| EMT–paramedic | 5.16 (4.50, 5.95) | < .001 |
| Nurse | 3.57 (2.92, 4.36) | < .001 |
| Physician | 3.16 (2.18, 4.46) | < .001 |
Note. AOR = adjusted odds ratio; CI = confidence interval; EMT = emergency medical technician: OR = odds ratio. Read, n = 262 676; used in model, n = 217 333. Dash indicates confidence interval could not be calculated.
We categorized urbanicity into 4 different groups (urban, suburban, rural, and wilderness) on the basis of an urban influence coding system used by the US Department of Agriculture and the Office of Management and Budget. These codes take into account county population size, degree of urbanization, and adjacency to a metropolitan area or areas.
The classic primary symptoms that prompt naloxone administration—breathing problems, change in responsiveness, and death—resulted in the highest odds of naloxone administration (breathing problems, AOR = 20.13; 95% CI = 16.93, 24.01; change in responsiveness, AOR = 13.70; 95% CI = 11.90, 15.88; death, AOR = 23.34; 95% CI = 17.86, 30.41). Higher odds of naloxone use were also present when the patient exhibited signs of fever, malaise, mental or psychological problems, and weakness (Table 2).
Using EMT-basic as a reference point, the odds of naloxone use were highest for EMT-intermediates (AOR = 5.45; 95% CI = 4.55, 6.54), followed by EMT-paramedics (AOR = 5.16; 95% CI = 4.5, 5.95). For both physicians and nurses, the odds of naloxone administration were more than 3 times those of EMT-basics (physicians, AOR = 3.16; 95% CI = 2.18, 4.46; nurses, AOR = 3.57; 95% CI = 2.92, 4.36; Table 2).
To further demonstrate the burden of drug poisoning and the impact of potential naloxone administration by population density, Figure 1 shows the opioid overdose mortality rate and the odds of naloxone use within the 3 urbanicity categories of urban, suburban, and rural. For comparison purposes, the urban opioid mortality rate is at near parity with the urban use of naloxone (mortality rate = 2.53 per 100 000 people; odds of naloxone use = 1.0). The mortality rate is higher for suburban environments (3.23 per 100 000 persons), and the odds of naloxone use are 1.41 times higher than those for the urban environment. Both mortality rate and odds of naloxone administration increase in suburban environments (28% and 41%, respectively). In the rural environment, the burden is 45% higher (3.68 per 100 000 persons) than in the urban environment (2.53 per 100 000 persons); however, the odds of rural naloxone use increase only 22.5% compared with urban naloxone use. If naloxone was administered at parity with mortality burden across geographic levels, more lives might be saved in rural communities.
FIGURE 1—
Overdose rates and odds of naloxone administration by EMS providers by level of urbanicity: National Emergency Medicine Service Information System, United States, 2012.
Note. EMS = emergency medical services.
DISCUSSION
Recently, an Institute of Medicine panel24 encouraged EMS systems and providers to assume a greater role in public health. Our study confirms that EMT-basic providers do not administer naloxone as often as other EMS providers, likely because of the limitations of the scope-of-practice model for basic life support providers. Rural communities are disproportionately affected by underutilization of naloxone. Because EMS personnel working in rural environments make up 20% of total EMS personnel and cover 80% of the US land mass, resource constraints and certification and scope-of-practice policies may combine to produce a large disparity in naloxone administration in drug overdose treatment in rural communities.
In general, surveillance systems that would help inform the health care system of the circumstances surrounding naloxone use are underdeveloped. Incorporating better outcome data into future versions of the NEMSIS data set will allow researchers to better evaluate medical interventions. However, our results also show that EMS personnel are administering naloxone when respiratory depression and central nervous system depression are present. These symptoms are 2 of the triad of classic symptoms and signs of an opioid overdose.25 The odds of naloxone use were strong for change in responsiveness, weakness, and malaise.
Naloxone usage numbers are available on a study-by-study basis. Knowlton et al.26 found that 1.1% of all EMS incidents resulted in naloxone administration. In addition, prior EMS surveillance data have revealed that growth in cases of drug overdose have outpaced the ability of EMS providers to provide naloxone in one rural state.19 EMS protocols vary from mandating naloxone administration for altered mental status, to altered mental status with evidence of drug use, to respiratory depression or arrest after suspected drug use.13 The common standard of emergency medicine practice currently indicates that naloxone only be given if there is respiratory depression or arrest, not for altered mental status.
Naloxone Impact
With respect to overdose cases, EMS providers are in a unique position in the health care system. EMS personnel may treat an opioid overdose case and never take that person to the hospital for additional treatment or care because of the patient’s refusal to go to the emergency department against medical advice. Thus, traditional emergency department surveillance systems will miss many cases of opioid overdose. Naloxone administration by EMS providers, and frequent patient recovery, have also been associated with a large percentage of patients refusing to go to a hospital (18.5%–34%) for additional treatment or observation.27–29 In some cases, patients do not want to go to the emergency department for additional monitoring once they have recovered. Naloxone wears off within 180 minutes, and the opioid-based drug can still be in a person’s system.30 In those cases, additional monitoring can theoretically save lives; however, in studies in San Antonio, Texas, and San Diego, California, involving 1550 overdose refusal of transports, no subsequent deaths were discovered.27,31
In response to increased fatal opioid overdoses, distribution programs that allow family members and friends to administer naloxone have been established. These programs have been successful in saving lives, as evidenced by a recent systematic review,32 and have not been shown to increase overall mortality.33 However, they have come under scrutiny because continued use of naloxone to reverse an opioid overdose does not directly address the drug user’s core addiction problem. The literature has shown limited support for naloxone family distribution programs among EMS professionals.34 However, overall acceptance and use of naloxone by bystanders and family members has occurred at a remarkable pace. In response to the epidemic, state legislatures and professional organizations are taking steps to improve access to naloxone, including providing naloxone to nonprofessional bystanders who may be drug users or the family and friends of people at risk for an opioid overdose. Also, many police departments are now equipping their officers with naloxone. In addition, poison control centers in the United States have recommended naloxone be used by laypersons to reverse opioid overdose, especially when the patient is in respiratory distress,35 and the American Association of Poison Control Centers issued a statement along with the American Academy of Clinical Toxicology and the American College of Medical Toxicology to advocate for the expanded use of naloxone among bystanders.36
As part of the health care process, dispatched EMS personnel routinely use naloxone in efforts to save lives at the scene of injury. However, EMT-basic providers are prohibited from administering naloxone in most states. Among EMS providers, naloxone has traditionally been administered intravenously or intramuscularly, but most evidence has suggested that intranasal naloxone is as effective as intravenous naloxone.37,38 However, some studies have shown that the mean time between naloxone administration and a clinical response was longer for intranasal administration, that its effectiveness may be lower, and that nasal administration required multiple administrations39,40 or follow-up intravenous doses.41 Intramuscular injection of naloxone to opioid overdose patients has shown a high response rate (89%).42 Recently, the US Food and Drug Administration has approved the use of naloxone intramuscular autoinjectors for use by family members.43 However, whether by autoinjector or intranasally, EMT-basic providers in the majority of states are not authorized to administer naloxone.
Rural Burden
On a rate basis, the public health burden for opioid overdose is higher in rural populations. Most EMS personnel in rural areas are volunteers and have received EMT-basic training, which may lead to disparities in access and care between rural and urban populations.44 Although EMT-paramedic service makes intuitive sense in remote areas far from hospitals, it is less likely to be present because of cost and run volume, a phenomenon termed the rural paramedic paradox by the National Association of State EMS Officials.45 Fewer EMT-paramedics and EMT-intermediates are available in rural areas, in which the public health burden for drug overdose is higher, contributing to health care disparity. The national model scope of practice has been adopted by many states as the minimum practice standard for EMS providers. EMT-basics are not able to treat opioid overdose other than through basic airway management. Although EMT-basic service can be adequate for brief periods of time, rural EMS transport is associated with longer transport times, resulting in greater chance of aspiration, hypoxia, and hypercarbia and the potential for increases in excess morbidity and mortality.46–48 Expanded access to naloxone among EMT-basic providers provides an opportunity to address this disparity between the burden of injury and available resources.
Limitations
This study has several limitations. First, the data analyzed came from a convenience sample. The NEMSIS data set includes national-standard EMS-related data, but the registry is voluntary. As a result, the data may not be representative of the overall US population. Second, because EMS data do not contain a diagnosis or case, we had to select our sample on the basis of provider impression and dispatch complaint, which may have a higher sensitivity and lower specificity than emergency department data containing diagnosis codes. However, when EMS providers arrive at an injury scene, they use clues about the environment, information about the dispatched call, and patient symptoms to determine whether a drug overdose has occurred. This combined information tends to lead to an accurate assessment in drug overdose cases and is recorded in NEMSIS as the EMS provider’s impression.
Third, inaccuracies in defining population density and years of death data occurred when we graphically overlaid opioid mortality rates onto naloxone administration. The death data were older than the EMS data because of availability. Fourth, given the rapidly expanding access to naloxone, it is possible that family members or others may be administering naloxone, resulting in a diminished need for EMT-basics to administer it.
Conclusions
When drug overdose primary prevention fails, EMS personnel are the health care system’s first responders and are uniquely positioned to treat prescription opioid and heroin overdose cases. In rural communities, the following actions may position EMS responders to save more lives:
Obtaining additional EMS training to obtain the proper certification to administer pharmaceuticals such as naloxone.
Changing the scope of practice to allow EMT-basics to administer intranasal or intramuscular naloxone. This change may save lives and reduce the burden of complications from opioid or heroin overdose, particularly in the rural environment.
Improving EMS surveillance systems and ensuring their full integration into the health care system. Such data can also lead to better determination of the true incidence of opioid overdoses reversed by out-of-hospital naloxone administration. Such improvements may lead to rehabilitative services for and treatment of those addicted to opioids and heroin.
Developing universal and national guidance on naloxone administration.
Acknowledgments
We thank Karen E. Jacobson, BA, NREMT-P, National Emergency Medicine Service Information System (NEMSIS) director, for explaining how NEMSIS data were collected and managed and for her assistance with obtaining the level-of-service provider variable for analysis. Without her assistance, this study would not have been possible. We also thank John J. Seggerson for his literature review and editorial comments.
Human Participant Protection
Institutional review board approval was not required for the analysis of de-identified public data.
References
- 1.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 2.Paulozzi LJ, Mack KA, Hockenberry JM. Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control Centers for Disease Control and Prevention. Vital signs: variation among states in prescribing of opioid pain relievers and benzodiazepines—United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(26):563–568. [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. QuickStats: rates of drug poisoning deaths involving heroin,* by selected age and racial/ethnic groups—United States, 2002 and 2011. MMWR Morb Mortal Wkly Rep. 2014;63(27):595. [Google Scholar]
- 4.Inocencio TJ, Carroll NV, Read EJ, Holdford DA. The economic burden of opioid-related poisoning in the United States. Pain Med. 2013;14(10):1534–1547. doi: 10.1111/pme.12183. [DOI] [PubMed] [Google Scholar]
- 5.Seidel JS. Emergency medical services and the adolescent patient. J Adolesc Health. 1991;12(2):95–100. doi: 10.1016/0197-0070(91)90450-z. [DOI] [PubMed] [Google Scholar]
- 6.Buajordet I, Næss AC, Jacobsen D, Brørs O. Adverse events after naloxone treatment of episodes of suspected acute opioid overdose. Eur J Emerg Med. 2004;11(1):19–23. doi: 10.1097/00063110-200402000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Sporer KA, Firestone J, Isaacs SM. Out-of-hospital treatment of opioid overdoses in an urban setting. Acad Emerg Med. 1996;3(7):660–667. doi: 10.1111/j.1553-2712.1996.tb03487.x. [DOI] [PubMed] [Google Scholar]
- 8.Paulozzi LJ, Xi Y. Recent changes in drug poisoning mortality in the United States by urban–rural status and by drug type. Pharmacoepidemiol Drug Saf. 2008;17(10):997–1005. doi: 10.1002/pds.1626. [DOI] [PubMed] [Google Scholar]
- 9.Busko JM. Rural EMS. In: Bass RR, Brice JH, Delbridge TR, Gunderson MR, editors. Emergency Medical Services: Clinical Practice and Systems Oversight. Dubuque, IA: Kendall-Hunt; 2008. pp. 218–228. Medical Oversight of EMS; vol 2. [Google Scholar]
- 10.Gonzalez RP, Cummings GR, Phelan HA, Mulekar MS, Rodning CB. Does increased emergency medical services prehospital time affect patient mortality in rural motor vehicle crashes? A statewide analysis. Am J Surg. 2009;197(1):30–34. doi: 10.1016/j.amjsurg.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 11.US Congress. Rural Emergency Medical Services. Washington, DC: US Government Printing Office; 1989. Office of Technology Assessment. Special Report OTA-H-445. [Google Scholar]
- 12.National Highway Traffic Safety Administration. National EMS scope of practice model. Available at: http://www.nhtsa.gov/people/injury/ems/EMSScope.pdf. Accessed March 17, 2014. [DOI] [PubMed]
- 13.Davis CS, Southwell JK, Niehaus VR, Walley AY, Dailey MW. Emergency medical services naloxone access: a national systematic legal review. Acad Emerg Med. 2014;21(10):1173–1177. doi: 10.1111/acem.12485. [DOI] [PubMed] [Google Scholar]
- 14.Belz D, Lieb J, Rea T, Eisenberg MS. Naloxone use in a tiered-response emergency medical services system. Prehosp Emerg Care. 2006;10(4):468–471. doi: 10.1080/10903120600885134. [DOI] [PubMed] [Google Scholar]
- 15.Curka PA, Pepe PE, Ginger VF, Sherrard RC, Ivy MV, Zachariah BS. Emergency medical services priority dispatch. Ann Emerg Med. 1993;22(11):1688–1695. doi: 10.1016/s0196-0644(05)81307-1. [DOI] [PubMed] [Google Scholar]
- 16.Saybolt MD, Alter SM, Dos Santos F et al. Naloxone in cardiac arrest with suspected opioid overdoses. Resuscitation. 2010;81(1):42–46. doi: 10.1016/j.resuscitation.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 17.Dailey MW, Goldfine C, Tran S. EMS analgesia practices in the US changes in practice over the last 5 years. Acad Emerg Med. 2014;21(5 suppl 1):S74–S75. [Google Scholar]
- 18.Patterson PD, Freeman VA, Moore CG, Slifkin RT. Becoming an Emergency Medical Technician: Urban-Rural Differences in Motivation and Job Satisfaction. Chapel Hill, NC: University of North Carolina; 2007. Working paper no. 89. [Google Scholar]
- 19.Alexander JL, Burton JH, Bradshaw JR, Colin F. Suspected opioid-related emergency medical services encounters in a rural state, 1997–2002. Prehosp Emerg Care. 2004;8(4):427–430. doi: 10.1016/j.prehos.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 20.Weber JM, Tataris KL, Hoffman JD, Aks SE, Mycyk MB. Can nebulized naloxone be used safely and effectively by emergency medical services for suspected opioid overdose? Prehosp Emerg Care. 2012;16(2):289–292. doi: 10.3109/10903127.2011.640763. [DOI] [PubMed] [Google Scholar]
- 21.National Emergency Services Information System. National Elapsed Patient Care Times by Urbanicity. Available at: http://www.nemsis.org/reportingTools/reports/documents/NEMSISReportSpecification-NationalElapsedpatientCareTimesbyUrbanicity.pdf. Accessed February 14, 2014.
- 22. SAS statistical software version 9.3. Cary, NC: SAS Institute Inc.
- 23.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000. [Google Scholar]
- 24.Institute of Medicine. Emergency Medical Services: At the Crossroads. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 25.Boyd J, Randell T, Luurila H, Kuisma M. Serious overdoses involving buprenorphine in Helsinki. Acta Anaesthesiol Scand. 2003;47(8):1031–1033. doi: 10.1034/j.1399-6576.2003.00201.x. [DOI] [PubMed] [Google Scholar]
- 26.Knowlton A, Weir BW, Hazzard F et al. EMS runs for suspected opioid overdose: implications for surveillance and prevention. Prehosp Emerg Care. 2013;17(3):317–329. doi: 10.3109/10903127.2013.792888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wampler DA, Molina DK, McManus J, Laws P, Manifold CA. No deaths associated with patient refusal of transport after naloxone-reversed opioid overdose. Prehosp Emerg Care. 2011;15(3):320–324. doi: 10.3109/10903127.2011.569854. [DOI] [PubMed] [Google Scholar]
- 28.Boyd JJ, Kuisma MJ, Alaspää AO, Vuori E, Repo JV, Randell TT. Recurrent opioid toxicity after pre-hospital care of presumed heroin overdose patients. Acta Anaesthesiol Scand. 2006;50(10):1266–1270. doi: 10.1111/j.1399-6576.2006.01172.x. [DOI] [PubMed] [Google Scholar]
- 29.Vilke GM, Buchanan J, Dunford JV, Chan TC. Are heroin overdose deaths related to patient release after prehospital treatment with naloxone? Prehosp Emerg Care. 1999;3(3):183–186. doi: 10.1080/10903129908958933. [DOI] [PubMed] [Google Scholar]
- 30.Rubin P, Blaschke TF, Guilleminault C. Effect of naloxone, a specific opioid inhibitor, on blood pressure fall during sleep. Circulation. 1981;63(1):117–121. doi: 10.1161/01.cir.63.1.117. [DOI] [PubMed] [Google Scholar]
- 31.Vilke GM, Sloane C, Smith AM, Chan TC. Assessment for deaths in out-of-hospital heroin overdose patients treated with naloxone who refuse transport. Acad Emerg Med. 2003;10(8):893–896. doi: 10.1111/j.1553-2712.2003.tb00636.x. [DOI] [PubMed] [Google Scholar]
- 32.Clark AK, Wilder CM, Winstanley EL. A systematic review of community opioid overdose prevention and naloxone distribution programs. J Addict Med. 2014;8(3):153–163. doi: 10.1097/ADM.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 33.Walley AY, Xuan Z, Hackman HH et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346 doi: 10.1136/bmj.f174. f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tobin KE, Gaasch WR, Clarke MC, MacKenzie E, Latkin CA. Attitudes of emergency medical service providers toward naloxone distribution programs. J Urban Health. 2005;82(2):296–302. doi: 10.1093/jurban/jti052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kroll D. More attention to preventing opioid-overdose deaths with naloxone. Forbes. February 10, 2014. Available at: http://www.forbes.com/sites/davidkroll/2014/02/10/more-attention-to-preventing-opioid-overdose-deaths-with-naloxone. Accessed August 15, 2014.
- 36. American Association of Poison Control Centers publishes joint position statement on expanding access to naloxone [press release]. Alexandria, VA: American Association of Poison Control Centers; October 7, 2014.
- 37.Doe-Simkins M, Walley AY, Epstein A, Moyer P. Saved by the nose: bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health. 2009;99(5):788–791. doi: 10.2105/AJPH.2008.146647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ashton H, Hassan Z. Intranasal naloxone in suspected opioid overdose. Emerg Med J. 2006;23(3):221–223. doi: 10.1136/emj.2005.034322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Robertson TM, Hendey GW, Stroh G, Shalit M. Intranasal naloxone is a viable alternative to intravenous naloxone for prehospital narcotic overdose. Prehosp Emerg Care. 2009;13(4):512–515. doi: 10.1080/10903120903144866. [DOI] [PubMed] [Google Scholar]
- 40.Merlin MA, Saybolt M, Kapitanyan R et al. Intranasal naloxone delivery is an alternative to intravenous naloxone for opioid overdoses. Am J Emerg Med. 2010;28(3):296–303. doi: 10.1016/j.ajem.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 41.Barton ED, Colwell CB, Wolfe T et al. Efficacy of intranasal naloxone as a needleless alternative for treatment of opioid overdose in the prehospital setting. J Emerg Med. 2005;29(3):265–271. doi: 10.1016/j.jemermed.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 42.Enteen L, Bauer J, McLean R et al. Overdose prevention and naloxone prescription for opioid users in San Francisco. J Urban Health. 2010;87(6):931–941. doi: 10.1007/s11524-010-9495-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.FDA approves new hand-held auto-injector to reverse opioid overdose [press release] Silver Spring, MD: US Food and Drug Administration; April 3, 2014. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm391465.htm. Accessed May 29, 2014.
- 44.Chng CL, Collins J, Eaddy S. A comparison of rural and urban emergency medical system (EMS) personnel: a Texas study. Prehosp Disaster Med. 2001;16(3):159–165. doi: 10.1017/s1049023x00025917. [DOI] [PubMed] [Google Scholar]
- 45.Joint Committee on Rural Emergency Care. Improving Access to EMS and Health Care in Rural Communities: A Strategic Plan. Falls Church, VA: National Association of State EMS Officials; 2010. [Google Scholar]
- 46.Elling R, Politis J. An evaluation of emergency medical technicians’ ability to use manual ventilation devices. Ann Emerg Med. 1983;12(12):765. doi: 10.1016/s0196-0644(83)80254-6. [DOI] [PubMed] [Google Scholar]
- 47.Cummins RO, Austin D, Graves JR, Litwin PE, Pierce J. Ventilation skills of emergency medical technicians: a teaching challenge for emergency medicine. Ann Emerg Med. 1986;15(10):1187–1192. doi: 10.1016/s0196-0644(86)80863-0. [DOI] [PubMed] [Google Scholar]
- 48.Jesudian MC, Harrison RR, Keenan RL, Maull KI. Bag-valve-mask ventilation; two rescuers are better than one: preliminary report. Crit Care Med. 1985;13(2):122–123. doi: 10.1097/00003246-198502000-00015. [DOI] [PubMed] [Google Scholar]