Abstract
Acute renal infarction is a rare clinical entity most commonly occurring as a result of a thromboembolic event in patients with predisposing risk factors. Its non-specific presentation can lead to delayed or missed diagnosis. However, modern imaging technology has allowed for the diagnosis of renal infarction to be made earlier in its clinical course. Due to its rare nature, treatment guidelines do not exist. We report a case of acute renal infarction identified on computed tomography scan in a patient with no known predisposing factors to thromboembolism that was treated through suction thrombectomy.
Introduction
Acute renal infarction is a rare condition.1,2 Recent advances in diagnostic imaging have increased the detection of renal infarction and several case studies have been published.3–6 The non-specific presentation of acute renal infarction has led to delayed diagnosis, but with the broad availability of high-quality computed tomography (CT) imaging, it is possible to identify cases early and initiate prompt treatment. Given the small numbers of cases described to date, quality evidence regarding treatment is lacking. We describe a case of acute renal infarction and review the clinical characteristics, diagnosis, and treatment options.
Case report
A 57-year-old man presented to the emergency department after waking with sudden left-sided abdominal pain. He denied symptoms beyond left lower quadrant pain and vomiting. His medical history was unremarkable. He was a carpenter and took no medications. Physical examination revealed normal vital signs, left lower quadrant tenderness, and no additional abnormalities. Laboratory investigations revealed mild leukocytosis (white blood count [WBC] 12.1 × 109/L), elevated lactate dehydrogenase (LDH, 271 U/L) and a normal serum creatinine (103 μmol/L). Based on clinical assessment, he was felt to have acute diverticulitis and contrast CT was arranged for confirmation. However, the CT scan revealed multiple left renal infarcts (Fig. 1, part A). Further imaging with renal arteriography showed filling defects in second order vessels to upper and lower poles, as well as distal branches (Fig. 1, part B). Given the lack of published data on the effects of ischemia time in renal infarct to guide treatment, a suction thrombectomy was performed about 12 hours after presentation. The patient was placed on IV heparin and admitted.
Fig. 1.
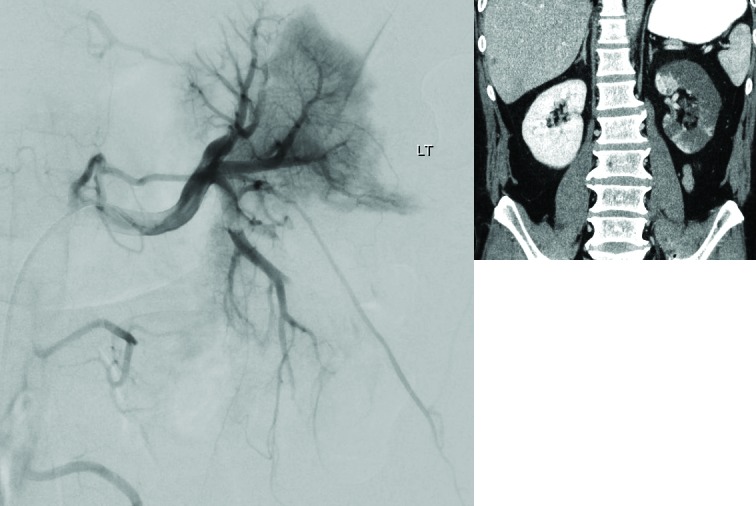
(A) Enhanced computed tomography (CT) scan showing hypoattenuation consistent with infarct throughout left kidney. (B) CT angiography showing prominent proximal thombus in the lower and upper pole second order branches and multiple distal filling defects.
Blood work the following day revealed ongoing leukocytosis (WBC 14.8 × 109/L), LDH of 1295 U/L and a creatinine of 115 μmol/L. Further workup revealed no family history of autoimmune disease, thromboembolism, or coagulopathy. Screening investigations were negative for ischemic heart disease, hypercoagulability, and autoimmune disorders. Echocardiogram revealed normal cardiac function. A CT-angiogram showed a small filling defect in the ascending thoracic aorta but no definite abnormality. There were persistent filling defects in the left renal arterial system and infarcted regions of the left kidney.
The patient’s hospital course was complicated by persistent pain for 3 days post-thrombectomy, attributed to post-embolization syndrome. His pain improved with intravenous steroids. His hospital stay was prolonged by ileus and recurrent abdominal pain resulting from a gastric ulcer. His LDH gradually trended to normal range, while his creatinine stabilized at 85 to 95 μmol/L. He was discharged 19 days after presentation on a 3-month course of warfarin.
Discussion
Acute renal infarction involves occlusion of the arterial supply to the kidney and most commonly occurs as the result of thromboembolism.1–9 Incidence in patients presenting to hospital is estimated between 0.004 and 0.007%.3,7 The average age at presentation is in the 6th to 7th decades, with a similar incidence among the sexes.2,3 Bilateral infarcts occur in 2% to 20% of cases.1–9 Renal infarction nearly always occurs in patients with risk factors for thromboembolism, and patients may experience additional embolic sequelae.9 The most common risk factor is atrial fibrillation, present in 25% to 65% of cases.3,5,7 Other risk factors include valvular and ischemic heart disease, cardiomyopathy, known atherosclerotic disease, and prior thromboembolism. Cases have also been described in patients with heritable and acquired hypercoagulability, connective tissue disorders, endocarditis, and trauma.3,8,10
The presentation of acute renal infarction is non-specific. Pain is present in 86% to 100% of cases.3–5 Patients can experience nausea, vomiting, and fever,6,8 and may be hypertensive.2,6,12 Given the vague presentation, renal infarction is often initially misdiagnosed3,4,6 and delayed diagnosis may have prognostic implications.7,8 The most sensitive and specific imaging test for renal infarction is renal artery angiography. This test, however, is invasive and may be avoided in many cases.4,7,12 Other imaging modalities have been employed, with contrast CT used commonly in recent years. CT is non-invasive, widely available and may detect other pathology to account for the presentation.3,7 Acute segmental infarcts appear on contrast CT as wedge-shaped areas of decreased uptake.4,5 Less commonly, a complete renal artery occlusion may result in decreased attenuation throughout the renal parenchyma with a rim of viable tissue, termed the “rim sign,” in the capsule.4,6
With CT-aided diagnosis, earlier administration of treatment is now possible to reduce renal ischemic time. The degree of infarction present will depend on the location and size of obstruction, and the presence of collateralization from lumbar, suprarenal and ureteral arteries.4,10–12 Anticoagulation was previously the mainstay of treatment, however, it may be insufficient to relieve the acute renal ischemia.6,7,10,12 Systemic thrombolysis has been employed with success, but carries significant risk of major bleeding events.10–12 Advances in endovascular techniques have allowed for local administration of thrombolytic agents, which is thought to minimize the risk of adverse systemic bleeding. Most recently, techniques have been employed to mechanically fragment and/or aspirate thromboembolic material from occluded arteries.11,12 These invasive treatments, however, are supported by limited data from case reports and their application is debated. One source of controversy is the time frame within which these techniques should be employed.10–12 Stronger evidence is required to guide treatment options in acute renal infarction, although this is a difficult task given its low incidence.
Prognosis following acute renal infarction is variable, with limited follow-up data available. Renal function, if impaired, commonly returns to baseline within 1 month.9 Mild elevations in creatinine may persist, but it is uncommon for patients to develop clinical kidney disease without preexisting renal impairment. End-stage kidney disease is rare and often complicated by pre-existing comorbidity. Some patients may develop persistent renin-mediated hypertension.5,9,12 A 2012 case series suggested that the most significant source of morbidity and mortality after renal infarction came from underlying disease processes. In particular, patients presenting with embolic renal infarction were likely to incur a subsequent embolic event.9
Conclusion
Acute renal infarction is a rare diagnosis manifesting non-specific signs and symptoms. As a result, it may be misdiagnosed as many mimicking conditions. Although the availability of modern diagnostic imaging has increased rates of detection, the incidence remains relatively low and there is little evidence to guide treatments. We have described a case of acute renal infarction, treated with percutaneous thrombectomy, and used it to discuss the presentation, diagnosis and management options of this condition with the goal of raising awareness to facilitate prompt diagnosis in these patients. Treatment options are varied, and further evidence is needed to evaluate the utility of these options.
Footnotes
Competing interests: The authors declare no competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.Hoxie H, Coggin C. Renal infarction. Arch Intern Med. 1940;65:587–94. doi: 10.1001/archinte.1940.00190090124007. [DOI] [Google Scholar]
- 2.Lessman RK, Johnson SF, Kaufman JJ. Renal artery embolism: Clinical features and long term follow up of 17 cases. Ann Intern Med. 1978;89:477–82. doi: 10.7326/0003-4819-89-4-477. [DOI] [PubMed] [Google Scholar]
- 3.Domanovits H, Paulis M, Nifkardjam M, et al. Acute renal infarction: Clinical characteristics of 17 patients. Medicine. 1999;78:386–94. doi: 10.1097/00005792-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Lumerman J, Hom D, Eiley D, et al. Heightened suspicion and rapid evaluation with CT for early diagnosis of partial renal infarction. J Endourol. 1999;13:209–14. doi: 10.1089/end.1999.13.209. [DOI] [PubMed] [Google Scholar]
- 5.Korzets Z, Plotkin E, Bernheim J, et al. The clinical spectrum of acute renal infarction. Isr Med Assoc J. 2002;4:781–4. [PubMed] [Google Scholar]
- 6.Hazanov N, Somin M, Attali M, et al. Acute renal embolism: Forty-four cases of renal infarction in patients with atrial fibrillation. Medicine. 2004;83:292–9. doi: 10.1097/01.md.0000141097.08000.99. [DOI] [PubMed] [Google Scholar]
- 7.Huang C, Lo H, Huang H, et al. ED presentations of acute renal infarction. Am J Emerg Med. 2007;25:164–9. doi: 10.1016/j.ajem.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Antopolsky M, Simanovsky N, Stalnikowicz R, et al. Renal infarction in the ED: 10-year experience and review of the literature. Am J Emerg Med. 2012;30:1055–60. doi: 10.1016/j.ajem.2011.06.041. [DOI] [PubMed] [Google Scholar]
- 9.Rhee H, Song S, Lee D, et al. The significance of clinical features in the prognosis of acute renal infarction: Single center experience. Clin Exp Nephrol. 2012;16:611–6. doi: 10.1007/s10157-012-0605-7. [DOI] [PubMed] [Google Scholar]
- 10.Kansal S, Feldman M, Cooksey S, et al. Renal artery embolism: A case report and review. J Gen Intern Med. 2008;23:644–7. doi: 10.1007/s11606-007-0489-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenberg J, Steiner M, Marshall J. Acute renal artery thrombosis treated by percutaneous rheolytic thrombectomy. Catheter Cardiovasc Interv. 2002;56:66–8. doi: 10.1002/ccd.10150. [DOI] [PubMed] [Google Scholar]
- 12.Komolafe B, Dishmon D, Sultan W, et al. Successful aspiration and rheolytic thrombectomy of a renal artery infarct and review of the current literature. Can J Cardiol. 2012;28:760.e1–760.e3. doi: 10.1016/j.cjca.2012.06.020. [DOI] [PubMed] [Google Scholar]


