Abstract
As a cofactor in numerous enzymatic reactions, magnesium fulfils various intracellular physiological functions. Thus, imbalance in magnesium status—primarily hypomagnesaemia as it is seen more often than hypermagnesaemia—might result in unwanted neuromuscular, cardiac or nervous disorders. Measuring total serum magnesium is a feasible and affordable way to monitor changes in magnesium status, although it does not necessarily reflect total body magnesium content. The following review focuses on the natural occurrence of magnesium and its physiological function. The absorption and excretion of magnesium as well as hypo- and hypermagnesaemia will be addressed.
Keywords: magnesium, physicochemical properties, physiological function, regulation, hypomagnesaemia, hypermagnesaemia
Introduction
Magnesium is the eighth most common element in the crust of the Earth [1, 2] and is mainly tied up within mineral deposits, for example as magnesite (magnesium carbonate [MgCO3]) and dolomite. Dolomite CaMg(CO3)2 is, as the name suggests, abundant in the Dolomite mountain range of the Alps [3]. The most plentiful source of biologically available magnesium, however, is the hydrosphere (i.e. oceans and rivers). In the sea, the concentration of magnesium is ∼55 mmol/L and in the Dead Sea—as an extreme example—the concentration is reported to be 198 mmol/L magnesium [4] and has steadily increased over time.
Magnesium salts dissolve easily in water and are much more soluble than the respective calcium salts. As a result, magnesium is readily available to organisms [5]. Magnesium plays an important role in plants and animals alike [2]. In plants, magnesium is the central ion of chlorophyll [3]. In vertebrates, magnesium is the fourth most abundant cation [5, 6] and is essential, especially within cells, being the second most common intracellular cation after potassium, with both these elements being vital for numerous physiological functions [6–9]. Magnesium is also used widely for technical and medical applications ranging from alloy production, pyrotechnics and fertilizers to health care. Traditionally, magnesium salts are used as antacids or laxatives in the form of magnesium hydroxide [Mg(OH)2], magnesium chloride (MgCl2), magnesium citrate (C6H6O7Mg) or magnesium sulphate (MgSO4).
Chemical characteristics
Magnesium is a Group 2 (alkaline earth) element within the periodic table and has a relative atomic mass of 24.305 Da [7], a specific gravity at 20°C of 1.738 [2, 3], a melting point of 648.8°C [2] and a boiling point of 1090°C [3]. In the dissolved state, magnesium binds hydration water tighter than calcium, potassium and sodium. Thus, the hydrated magnesium cation is hard to dehydrate. Its radius is ∼400 times larger than its dehydrated radius. This difference between the hydrated and the dehydrated state is much more prominent than in sodium (∼25-fold), calcium (∼25-fold) or potassium (4-fold) [5]. Consequently, the ionic radius of dehydrated magnesium is small but biologically relevant [6]. This simple fact explains a lot of magnesium’s peculiarities, including its often antagonistic behaviour to calcium, despite similar chemical reactivity and charge. For instance, it is almost impossible for magnesium to pass through narrow channels in biological membranes that can be readily traversed by calcium because magnesium, unlike calcium, cannot be easily stripped of its hydration shell [10]. Steric constraints for magnesium transporters are also far greater than for any other cation transport system [5]: proteins transporting magnesium are required to recognize the large hydrated cation, strip off its hydration shell and deliver the bare (i.e. dehydrated) ion to the transmembrane transport pathway through the membrane (Figure 1) [5, 11, 12]. There are obvious chemical similarities between calcium and magnesium but in cell biology, major differences often prevail (Table 1).
Fig. 1.
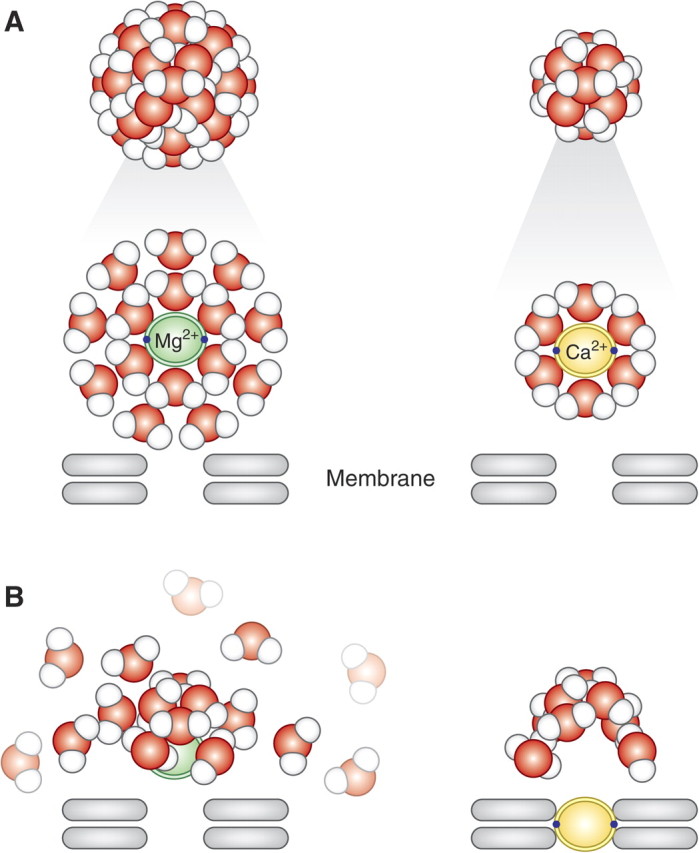
(A and B) Magnesium (top left) is surrounded by two hydration shells, whereas calcium (top right) has just one layer. If elements need to fit into a structure (transporter or membrane ‘pore’), calcium (below right) simply sheds its hydration shell and its dehydrated ion will fit. Magnesium (below left), on the other hand, first has to get rid of two layers, which is highly energy consuming (simplified model).
Table 1.
| Magnesium | Calcium | |
| Chemical aspects | ||
| Name (symbol) | Magnesium (Mg) | Calcium (Ca) |
| Element category | Alkaline earth metal | Alkaline earth metal |
| Abundance | Eighth most abundant element in the crust of the Earth | Fifth most abundant element in the crust of the Earth |
| Atomic number | 12 | 20 |
| Valence | 2 | 2 |
| Crystal structure | Hexagonal | Face-centered cubic |
| Atomic radius | 0.65 Å | 0.94 Å |
| Atomic weight | 24.305 g/mol | 40.08 g/mol |
| Specific gravity | 1.738 (20°C) | 1.55 (20°C) |
| Number of hydration shells | Two layers | One layer |
| Radius after hydration | ∼400 × larger than its dehydrated form | ∼25 × larger than its dehydrated form |
| Isotopes | Magnesium naturally exists in three stable isotopes: | Calcium has five stable isotopes: |
| [24]Mg (most abundant isotope) | [40]Ca (most abundant isotope) | |
| [25]Mg | [42]Ca | |
| [26]Mg | [43]Ca | |
| [28]Mg radioactive, β-decay | [44]Ca | |
| [46]Ca | ||
| Physiological aspects | ||
| Availability in the human body | Normal serum concentration range: 0.65–1.05 mmol/L, divided into three fractions: | Normal serum concentration range: 2.2–2.6 mmol/L, divided into three fractions: |
| Free, ionized (ultrafilterable fraction): 55–70% | Free, ionized (ultrafilterable fraction): 47.5–50% | |
| Protein-bound (non-ultrafilterable): 20–30% | Protein-bound (non-ultrafilterable): 42–46% | |
| Complexed (citrate, bicarbonate, phosphate): 5–15% | Complexed (citrate, bicarbonate, phosphate): 6.0–6.5% | |
| Total body content in adults | ∼24 g | ∼1000 g |
| Function with respect to cell death | Anti-apoptotic | Pro-apoptotic |
| Information attained by serum level | Serum level does not represent total body content | Serum level does not represent total body content |
Physiological role of magnesium in the body
The body of most animals contains ∼0.4 g magnesium/kg [5]. The total magnesium content of the human body is reported to be ∼20 mmol/kg of fat-free tissue. In other words, total magnesium in the average 70 kg adult with 20% (w/w) fat is ∼1000 [7] to 1120 mmol [13] or ∼24 g [14, 15]. These values should be interpreted with caution, however, as analytical methods differ considerably throughout the years. In comparison, the body content of calcium is ∼1000 g (i.e. 42 times greater than the body content of magnesium) [16].
Distribution in the human body
About 99% of total body magnesium is located in bone, muscles and non-muscular soft tissue [17] (see also Table 2). Approximately 50–60% of magnesium resides as surface substituents of the hydroxyapatite mineral component of bone [14, 18]. An illustration of bioapatite is shown in Figure 2. Most of the remaining magnesium is contained in skeletal muscle and soft tissue [14]. The magnesium content of bone decreases with age, and magnesium stored in this way is not completely bioavailable during magnesium deprivation [5]. Nonetheless, bone provides a large exchangeable pool to buffer acute changes in serum magnesium concentration [19]. Overall, one third of skeletal magnesium is exchangeable, serving as a reservoir for maintaining physiological extracellular magnesium levels [19].
Table 2.
Distribution of magnesium in the adult human being, molar mass of magnesium = 24.305 g/mol; Reprinted from [7], with permission from Elsevier
| Tissue | Body weight (kg wet weight) | Concentration (mmol/kg wet weight) | Content (mmol) | % of total body magnesium |
| Serum | 3.0 | 0.85 | 2.6 | 0.3 |
| Red blood cells | 2.0 | 2.5 | 5.0 | 0.5 |
| Soft tissue | 22.7 | 8.5 | 193.0 | 19.3 |
| Muscle | 30.0 | 9.0 | 270.0 | 27.0 |
| Bone | 12.3 | 43.2 | 530.1 | 52.9 |
| Total | 70.0 | 64.05 | 1000.7 | 100.0 |
Fig. 2.
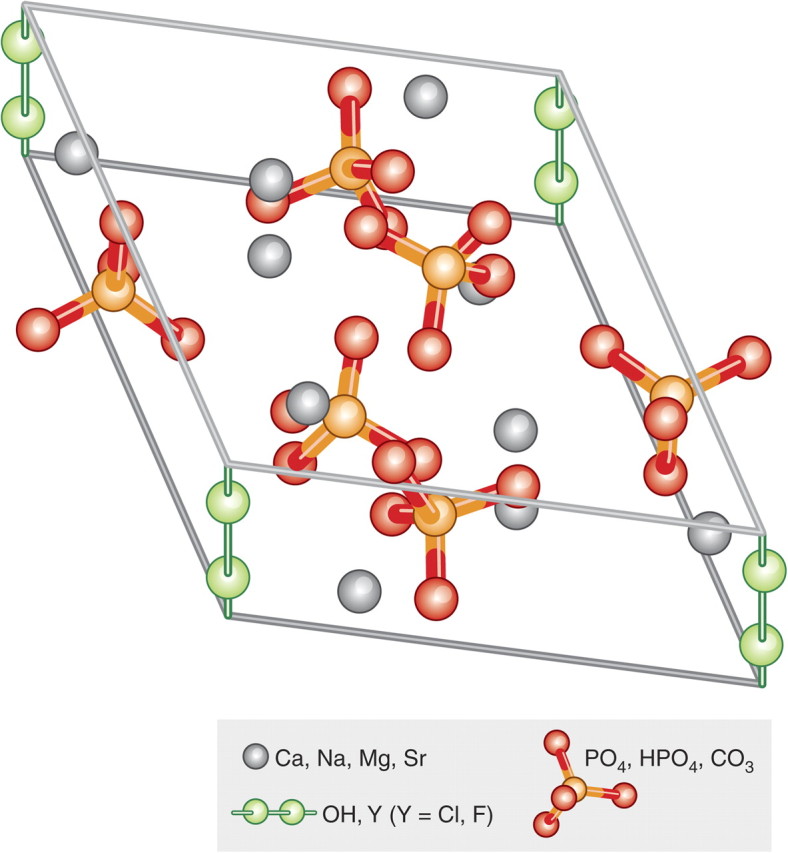
Hydroxyapatite crystal unit. Enamel apatite contains the lowest concentrations of carbonate and magnesium ions, and is rich in fluoride F. Dentin and bone have the highest levels of carbonate and magnesium ions, but have low fluoride content. Fluoride decreases solubility and increases chemical stability, carbonate, chloride and especially magnesium all increase solubility of the otherwise very insoluble mineral. Chemically the mineral comprises a highly substituted carbonated calcium hydroxyapatite (HAP). In the absence of exact compositional analysis the biogenic forms of this mineral are collectively alluded to as “bioapatite”. Ca, calcium; Na, sodium; Mg, magnesium; Sr, strontium; OH, hydroxide; Cl, chloride; F, fluoride; PO4, HPO4, phosphate; CO3, carbonate.
Intracellular magnesium concentrations range from 5 to 20 mmol/L; 1–5% is ionized, the remainder is bound to proteins, negatively charged molecules and adenosine triphosphate (ATP) [18].
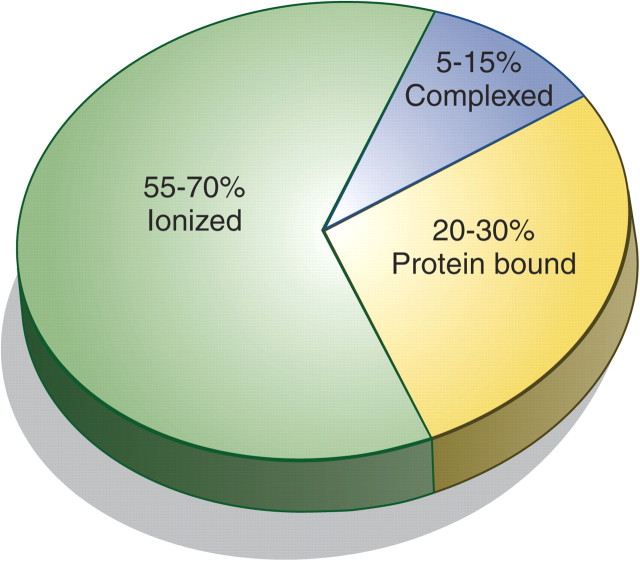
Extracellular magnesium accounts for ∼1% of total body magnesium [14, 18, 20] which is primarily found in serum and red blood cells (RBCs) [5, 7, 21, 22]. Serum magnesium can—just like calcium—be categorized into three fractions. It is either free/ionized, bound to protein or complexed with anions such as phosphate, bicarbonate and citrate or sulphate (Table 1, Figure 3). Of the three fractions in plasma, however, ionized magnesium has the greatest biological activity [5, 7, 21, 22].
Fig. 3.
Total serum magnesium is present in three different states. Because of different measurement methods, results published for each state of serum magnesium vary considerably. Therefore, a range for every state is provided [7, 21, 23–24]. For additional data, please see also Tables 1 and 2 in the article by Cunningham et al. [28] in this supplement.
Magnesium is primarily found within the cell [7] where it acts as a counter ion for the energy-rich ATP and nuclear acids. Magnesium is a cofactor in >300 enzymatic reactions [8, 10]. Magnesium critically stabilizes enzymes, including many ATP-generating reactions [14]. ATP is required universally for glucose utilization, synthesis of fat, proteins, nucleic acids and coenzymes, muscle contraction, methyl group transfer and many other processes, and interference with magnesium metabolism also influences these functions [14]. Thus, one should keep in mind that ATP metabolism, muscle contraction and relaxation, normal neurological function and release of neurotransmitters are all magnesium dependent. It is also important to note that magnesium contributes to the regulation of vascular tone, heart rhythm, platelet-activated thrombosis and bone formation (see review by Cunningham et al. [28] in this supplement) [6, 7, 10, 29, 30]. Some of magnesium’s many functions are listed in Table 3.
Table 3.
Magnesium has numerous functions in the body, for example, serving as a cofactor in enzymatic reactionsa. Reprinted from [8], with permission.
| Enzyme function |
| Enzyme substrate (ATP-Mg, GTP-Mg) |
| Kinases B |
| Hexokinase |
| Creatine kinase |
| Protein kinase |
| ATPases or GTPases |
| Na+ /K+-ATPase |
| Ca2+-ATPase |
| Cyclases |
| Adenylate cyclase |
| Guanylate cyclase |
| Direct enzyme activation |
| Phosphofructokinase |
| Creatine kinase |
| 5-Phosphoribosyl-pyrophosphate synthetase |
| Adenylate cyclase |
| Na+/ K+-ATPase |
| Membrane function |
| Cell adhesion |
| Transmembrane electrolyte flux |
| Calcium antagonist |
| Muscle contraction/relaxation |
| Neurotransmitter release |
| Action potential conduction in nodal tissue |
| Structural function |
| Proteins |
| Polyribosomes |
| Nucleic acids |
| Multiple enzyme complexes |
| Mitochondria |
Magnesium is also necessary for structural function of proteins, nucleic acids or mitochondria. Moreover, it is a natural calcium antagonist [8]. ATP, adenosine triphosphate; GTP, guanosine triphosphate; K, potassium; Mg, magnesium; Na, sodium; Ca, calcium.
In muscle contraction, for example, magnesium stimulates calcium re-uptake by the calcium-activated ATPase of the sarcoplasmic reticulum [14]. Magnesium further modulates insulin signal transduction and cell proliferation and is important for cell adhesion and transmembrane transport including transport of potassium and calcium ions. It also maintains the conformation of nucleic acids and is essential for the structural function of proteins and mitochondria.
It has long been suspected that magnesium may have a role in insulin secretion owing to the altered insulin secretion and sensitivity observed in magnesium-deficient animals [31]. Epidemiological studies have shown a high prevalence of hypomagnesaemia and lower intracellular magnesium concentrations in diabetics. Benefits of magnesium supplementation on the metabolic profile of diabetics have been observed in some, but not all, clinical trials, and so larger prospective studies are needed to determine if dietary magnesium supplementation is associated with beneficial effects in this group [32].
Recent epidemiological studies have suggested that a relatively young gestational age is associated with magnesium deficiency during pregnancy, which not only induces maternal and foetal nutritional problems but also leads to other consequences that might affect the offspring throughout life [33].
There is also evidence that magnesium and calcium compete with one another for the same binding sites on plasma protein molecules [13, 34]. It was shown that magnesium antagonizes calcium-dependent release of acetylcholine at motor endplates [6]. Thus, magnesium may be considered a natural ‘calcium antagonist’. While calcium is a powerful ‘death trigger’ [35], magnesium is not [34]: magnesium inhibits calcium-induced cell death [36]. It is anti-apoptotic in mitochondrial permeability transition and antagonizes calcium-overload-triggered apoptosis. Magnesium is important in health and disease, as will be discussed in more detail in this supplement in the article by Geiger and Wanner [37].
Regulation of magnesium influx and efflux
There is considerable variation in the plasma/tissue exchange of magnesium between various organs of an animal and also between animal species [5]. These observations indicate that various cell types handle magnesium quite differently, which is again different from calcium [10]. Myocardium, kidney parenchyma, fat tissue, skeletal muscle, brain tissue and lymphocytes exchange intracellular and extracellular magnesium at different rates. In mammalian heart, kidney and adipocytes, total intracellular magnesium is able to exchange with plasma magnesium within 3–4 h [38–42]. In man, equilibrium for magnesium among most tissue compartments is reached very slowly, if at all [17]. About 85% of the whole body magnesium, measured as [28]Mg is either non-exchangeable or exchanges very slowly with a roughly estimated biological half-life of ∼1000 h [43].
Magnesium consumption
Humans need to consume magnesium regularly to prevent magnesium deficiency, but as the recommended daily allowance for magnesium varies, it is difficult to define accurately what the exact optimal intake should be. Values of ≥300 mg are usually reported with adjusted dosages for age, sex and nutritional status. The Institute of Medicine recommends 310–360 mg and 400–420 mg for adult women and men, respectively. Other recommendations in the literature suggest a lower daily minimum intake of 350 mg for men and 280–300 mg magnesium for women (355 mg during pregnancy and lactation) [2, 7, 10, 18].
While drinking water accounts for ∼10% of daily magnesium intake [44], chlorophyll (and thus green vegetables) is the major source of magnesium. Nuts, seeds and unprocessed cereals are also rich in magnesium [15]. Legumes, fruit, meat and fish have an intermediate magnesium concentration. Low magnesium concentrations are found in dairy products [7]. It is noteworthy that processed foods have a much lower magnesium content than unrefined grain products [7] and that dietary intake of magnesium in the western world is decreasing owing to the consumption of processed food [45]. With the omnipresence of processed foods, boiling and consumption of de-mineralized soft water, most industrialized countries are deprived of their natural magnesium supply. On the other hand, magnesium supplements are very popular food supplements, especially in the physically active.
Magnesium absorption and excretion
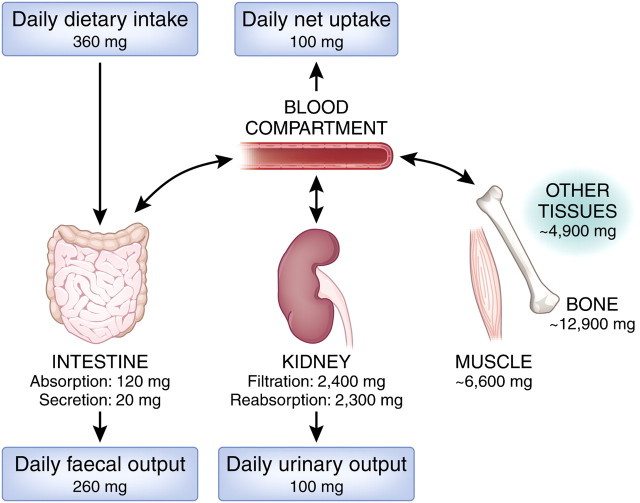
Magnesium homeostasis is maintained by the intestine, the bone and the kidneys. Magnesium—just like calcium—is absorbed in the gut and stored in bone mineral, and excess magnesium is excreted by the kidneys and the faeces (Figure 4). Magnesium is mainly absorbed in the small intestine [21, 15, 46], although some is also taken up via the large intestine [7, 10, 47]. Two transport systems for magnesium in the gut are known (as discussed in the article by de Baaij et al. [48] in this supplement). The majority of magnesium is absorbed in the small intestine by a passive paracellular mechanism, which is driven by an electrochemical gradient and solvent drag. A minor, yet important, regulatory fraction of magnesium is transported via the transcellular transporter transient receptor potential channel melastatin member (TRPM) 6 and TRPM7—members of the long transient receptor potential channel family—which also play an important role in intestinal calcium absorption [21]. Of the total dietary magnesium consumed, only about 24–76% is absorbed in the gut and the rest is eliminated in the faeces [46]. It is noteworthy that intestinal absorption is not directly proportional to magnesium intake but is dependent mainly on magnesium status. The lower the magnesium level, the more of this element is absorbed in the gut, thus relative magnesium absorption is high when intake is low and vice versa. When intestinal magnesium concentration is low, active transcellular transport prevails, primarily in the distal small intestine and the colon (for details, see de Baaij et al. [48] in this supplement).
Fig. 4.
Magnesium balance. Values as indicated based on [7]. The conversion factor from milligrams to millimole is 0.04113.
The kidneys are crucial in magnesium homeostasis [18, 49–51] as serum magnesium concentration is primarily controlled by its excretion in urine [7]. Magnesium excretion follows a circadian rhythm, with maximal excretion occurring at night [15]. Under physiological conditions, ∼2400 mg of magnesium in plasma is filtered by the glomeruli. Of the filtered load, ∼95% is immediately reabsorbed and only 3–5% is excreted in the urine [10, 52], i.e. ∼100 mg. It is noteworthy that magnesium transport differs from that of the most other ions since the major re-absorption site is not the proximal tubule, but the thick ascending limb of the loop of Henle. There, 60–70% of magnesium is reabsorbed, and another small percentage (∼10%) is absorbed in the distal tubules. The kidneys, however, may lower or increase magnesium excretion and re-absorption within a sizeable range: renal excretion of the filtered load may vary from 0.5 to 70%. On one hand, the kidney is able to conserve magnesium during magnesium deprivation by reducing its excretion; on the other hand, magnesium might also be rapidly excreted in cases of excess intake [18]. While reabsorption mainly depends on magnesium levels in plasma, hormones play only a minor role (e.g. parathyroid hormone, anti-diuretic hormone, glucagon, calcitonin), with oestrogen being an exception to this rule.
Magnesium is essential for man and has to be consumed regularly and in sufficient amount to prevent deficiency.
It is a cofactor in more than 300 enzymatic reactions needed for the structural function of proteins, nucleic acids and mitochondria.
Absorption is complex, depending on the individual’s magnesium status, and excretion is controlled primarily by the kidneys.
Assessment of magnesium status
Serum magnesium concentration
To date, three major approaches are available for clinical testing (Table 4). The most common test for the evaluation of magnesium levels and magnesium status in patients is serum magnesium concentration [21, 56], which is valuable in clinical medicine, especially for rapid assessment of acute changes in magnesium status [17]. However, serum magnesium concentration does not correlate with tissue pools, with the exception of interstitial fluid and bone. It also does not reflect total body magnesium levels [17, 57]. Only 1% of total body magnesium is present in extracellular fluids, and only 0.3% of total body magnesium is found in serum, and so serum magnesium concentrations [22] are poor predictors of intracellular/total body magnesium content [7]. This situation is comparable to assessing total body calcium by measuring serum calcium, which, too, does not adequately represent total body content. As with many reference values, laboratory parameters will also vary from laboratory to laboratory resulting in slightly varying ranges for the ‘healthy’ populations evaluated. What is considered the ‘normal level’ might actually be slightly too low, representing a mild magnesium deficit present in the normal population [17].
Table 4.
| Magnesium in: |
| Serum |
| Red blood cellsa |
| Leucocytesb |
| Musclec |
| Metabolic assessment via: |
| Balance studies |
| Isotopic analyses |
| Renal excretion of magnesium |
| Retention of magnesium, following acute administration |
| Free magnesium levels with: |
| Fluorescent probesd |
| Ion-selective electrodese |
| Nuclear magnetic resonance spectroscopyf g |
| Metallochrome dyes |
Red blood cell magnesium concentration does not seem to correlate well with total body magnesium status [53].
Magnesium content of mononuclear cells may be a better predictor of skeletal and cardiac muscle magnesium content [54].
Muscle is an appropriate tissue for the assessment of magnesium status [55] but it is an invasive and expensive procedure requiring special expertise.
Intracellular free magnesium concentration can be determined by using fluorescent probes [10]. Application of fluorescent dyes, however, is limited because the major fluorescent dye for magnesium (mag-fura 2) has a higher affinity for calcium than for magnesium.
Ion-specific microelectrodes can be used to measure the internal free ion concentration of cells and organelles. Major advantages are that readings can be made over long time spans. In contrast to dyes, very little extra ion buffering capacity has to be added to the cells, and direct measurement of the ion flux across the membrane of a cell is possible with every ion passing across the membrane contributing to the result. Nonetheless, ion-selective electrodes for magnesium are not entirely selective for ionized magnesium. A correction is applied based on the ionized calcium concentration [10].
Total magnesium content of a biological sample can be determined by using flame atomic absorption spectroscopy (AAS). However, this technique is destructive and, for optimal accuracy, sample volume has to add up to ∼2 mL with a concentration ranging from 0.1 to 0.4 μmol/L. With this technique, only content, not uptake, can be quantified.
Nuclear magnetic resonance may be used to measure intracellular free magnesium concentration [10].
In addition, there are individuals—in particular those with a subtle chronic magnesium deficiency—whose serum magnesium levels are within the reference range but who still may have a deficit in total body magnesium. And vice versa: some people—though very few—have low serum magnesium levels but a physiological magnesium body content [17]. Moreover, serum magnesium might be higher in vegetarians and vegans than in those with omnivorous diets. The same applies to levels after short periods of maximal exercise as lower serum levels are observed after endurance exercises [58, 59] and also during the third trimester of pregnancy. There is also intra-individual variability [60]. Moreover, measurements are strongly affected by haemolysis (and therefore by a delay in separating blood), and by bilirubin [59].
In healthy individuals, magnesium serum concentration is closely maintained within the physiological range [13, 15, 18]. This reference range is 0.65–1.05 mmol/L for total magnesium concentrations in adult blood serum [61] and 0.55–0.75 mmol/L for ionized magnesium [62]. According to Graham et al. [46], blood plasma concentration in healthy individuals is similar to serum, ranging from 0.7 to 1.0 mmol/L.
Magnesium concentration in RBCs is generally higher than its concentration in serum [46] (i.e. 1.65–2.65 mmol/L) [61]. The magnesium concentration is even higher in ‘young’ RBCs [13], which might be particularly relevant in patients receiving erythropoietin. Thus, when measuring magnesium serum levels, it is important to avoid haemolysis to prevent misinterpretation [17, 22].
Although some limitations may apply, serum magnesium concentration is still used as the standard for evaluating magnesium status in patients [21]. It has proven helpful in detecting rapid extracellular changes. In addition, measuring serum magnesium is feasible and inexpensive [As an example: Mg in serum (photometric assessment/AAS)—Germany (Synlab, Augsburg): EBM 32248 (EBM = einheitlicher Bewertungsmaßstab für Ärzte, kassenärztliche Abrechnung; valuation standard) = 1.40 €; GOÄ 3621 1.00 (GOÄ = Gebührenordnung für Ärzte, private; scale of charges for physicians) = 2.33 €; Denmark (GPs laboratory, Copenhagen): 87.50 DDK = 11.66 €; France (Biomnis, Ivry-sur Seine) = 1.89 €] and should become more common in clinical routine.
Twenty-four-hour excretion in urine
Another approach for the assessment of magnesium status is urinary magnesium excretion. This test is cumbersome, especially in the elderly, since it requires at least a reliable and complete 24-h time frame [54]. As a circadian rhythm underlies renal magnesium excretion, it is important to collect a 24-h urine specimen to assess magnesium excretion and absorption accurately. This test is particularly valuable for assessing magnesium wasting by the kidneys owing to medication or patients’ physiological status [7]. The results will provide aetiological information: while a high urinary excretion indicates renal wasting of magnesium, a low value suggests an inadequate intake or absorption [7].
Magnesium retention test—‘loading test’
A further refinement is the magnesium retention test. This ‘loading test’ may serve for identification of patients with hypomagnesaemic and normomagnesaemic magnesium deficiencies. Retention of magnesium following acute oral or parenteral administration is used to assess magnesium absorption, chronic loss and status. Changes in serum magnesium concentration and excretion following an oral magnesium load reflect intestinal magnesium absorption [7, 63]. Magnesium retained during this test is retained in bone. Thus, the lower the bone magnesium content the higher the magnesium retention in this test [64]. The percentage of magnesium retained is increased in cases of magnesium deficiency and is inversely correlated with the concentration of magnesium in bone [65, 66]. This test quantifies the major exchangeable pool of magnesium, providing a more sensitive index of magnesium deficiency than simply measuring serum magnesium concentration. A urinary excretion of >60–70% of the magnesium load suggests that magnesium depletion is unlikely. Standardization of this test, however, is lacking [22].
Isotopic analysis of magnesium
Magnesium exists in three different isotopes: 78.7% occurs as [24]Mg, 10.1% as [25]Mg and 11.2% as [26]Mg [5]. [28]Mg is radioactive and was made available commercially for scientific use in the 1950s to the 1970s. Radioactive tracer elements in ion uptake assays allow the calculation of the initial change in the ion content of the cells. [28]Mg decays by emission of high-energy beta or gamma particles that can be measured using a scintillation counter. However, the radioactive half-life of the most stable radioactive magnesium isotope—[28]Mg—is only 21 h, restricting its use. [26]Mg was used to assess absorption of magnesium from the gastrointestinal tract, presenting nutritional and analytical challenges. Although studies with isotopes of magnesium can provide important information, they are limited to research [7]. Surrogates for magnesium (i.e. Mn2+, Ni2+ and Co2+) have been used [5]. They were used to mimic the properties of magnesium in some enzymatic reactions, and radioactive forms of these elements were successfully employed in cation transport studies. The most common surrogate is Mn2+ that can replace magnesium in the majority of enzymes where ATP-Mg is used as a substrate [5].
Assessment of total serum magnesium concentration is the most practicable and inexpensive approach for the detection of acute changes in magnesium status.
However, one should bear in mind that serum magnesium concentration does not reflect the patient's magnesium status accurately as it does not correlate well with total magnesium body content.
Pathophysiology
Hypomagnesaemia
The definition of magnesium deficiency seems simpler than it is, primarily because accurate clinical tests for the assessment of magnesium status are still lacking. Evaluation of serum magnesium concentration and collection of a 24-h urine specimen for magnesium excretion are at present the most important laboratory tests for the diagnosis of hypomagnesaemia. The next step would be to perform a magnesium retention test [7].
In the literature, patients with serum magnesium concentrations ≤0.61 mmol/L (1.5 mg/dL) [67–69] and ≤0.75 mmol/L, respectively, were considered hypomagnesaemic [70, 71].
Hypomagnesaemia is common in hospitalized patients, with a prevalence ranging from 9 to 65% [67, 69–72]. A particularly high incidence of hypomagnesaemia is observed in intensive care units. Furthermore, a significant association has been reported between hypomagnesaemia and esophageal surgery [70]. In these severely ill patients, nutritional magnesium intake was probably insufficient. Certain drugs have been associated with magnesium wasting (although the relationship between these factors remains unclear), putting the afflicted patients at an increased risk for acute hypomagnesaemia. Such medications include aminoglycosides, cisplatin, digoxin, furosemide, amphotericin B and cyclosporine A [67, 70] (Table 5). Moreover, it was observed that in patients with severe hypomagnesaemia, mortality rates increase [67, 70]. Therefore, assessment of magnesium status is advised, particularly in those who are critically ill. When hypomagnesaemia is detected, one should address—if identifiable—the underlying pathology to reverse the depleted status [73].
Table 5.
Settings in which symptomatic hypomagnesaemia might occur
| Decreased dietary intake: |
| Malnutrition |
| Parenteral infusions without magnesium |
| Gastrointestinal malabsorption and loss [6]: |
| Severe or prolonged chronic diarrhoea [6–8] |
| Increased renal loss [6]: |
| Congenital or acquired tubular defects (see de Baaij et al. [48] in this supplement) |
| Drug induced: |
| Loop diureticsa [7, 74] |
| Aminoglycosides [7, 8, 70, 75] |
| Amphotericin B [8, 76] |
| Cyclosporine [8, 77] and tacrolimus [78] |
| Cisplatin [8, 79] |
| Cetuximab [80] |
| Omeprazole [81] |
| Pentamidine [8, 82] |
| Foscarnet [83] |
| Endocrine causes: |
| Primary and secondary hyperaldosteronism [8, 84] |
| Hungry bone syndrome, e.g. after surgery of primary hyperparathyroidismb [7, 8] |
| Syndrome of inappropriate anti-diuretic hormone hypersecretion |
| Diabetes mellitus [6, 8] |
| Other causes:Stress |
| Chronic alcoholismc [7, 8] |
| Excessive lactation, heat, prolonged exercise [6] |
| Severe burns [6, 85] |
| Cardiopulmonary bypass surgery [86] |
| Iatrogenic [6] |
Loop diuretics such as furosemide, torasemide, ethacrynic acid, bumethanide and piretanide cause an increased urinary excretion [74]. Thiazide diuretics, acting on the early distal tubule, might lead to magnesium loss only in the long run [87]. In contrast, potassium-sparing diuretics, such as triamterene and amiloride acting on the late distal tubule, contribute to magnesium conservation by the kidneys. Osmotic agents such as mannitol or glucose hamper tubular re-absorption and augment magnesium excretion [7, 52].
Hypomagnesaemia—due to deposition of magnesium in the calcium- and magnesium-depleted bone—occurs in one third of the patients after surgical correction of primary hyperparathyroidism [7].
It was observed that chronic alcohol consumption goes along with a significant increase of urinary magnesium excretion and a reduced muscle magnesium content. Thus, empiric use of magnesium replacement therapy was suggested as part of the therapeutic alcohol withdrawal syndrome regimen [7].
Hypomagnesaemia has been linked to poor condition (malignant tumours, cirrhosis or cerebrovascular disease) [70] and a number of other ailments. Magnesium deficiencies might stem from reduced intake caused by poor nutrition or parenteral infusions lacking magnesium, from reduced absorption and increased gastrointestinal loss, such as in chronic diarrhoea, malabsorption or bowel resection/bypass [6–8]. Deficiencies might also be triggered by increased magnesium excretion in some medical conditions such as diabetes mellitus, renal tubular disorders, hypercalcaemia, hyperthyroidism or aldosteronism or in the course of excessive lactation or use of diuretics (Table 5). Compartmental redistribution of magnesium in illnesses such as acute pancreatitis might be another cause of acute hypomagnesaemia [7]. In addition, several inherited forms of renal hypomagnesaemia exist [88]. These genetic changes led to the detection of various transporters (see de Baaij et al. [48] in this supplement, for further details).
Chronic hypomagnesaemia
Diagnosis of chronic hypomagnesaemia is difficult as there may be only a slightly negative magnesium balance over time. There is equilibrium among certain tissue pools, and serum concentration is balanced by magnesium from bone. Thus, there are individuals with a serum magnesium concentration within the reference interval who have a total body deficit for magnesium. Magnesium levels in serum and 24-h urine samples may be normal, and so parenteral administration of magnesium with assessment of retention should be considered if in doubt [7]. Chronic latent magnesium deficiency has been linked to atherosclerosis, myocardial infarction, hypertension (see also Geiger and Wanner [37] in this supplement.), malignant tumours, kidney stones, alteration in blood lipids, premenstrual syndrome and psychiatric disorders.
Clinical signs of hypomagnesaemia
Clinical signs of hypo- and hypermagnesaemia overlap often and are rather non-specific. Manifestations of hypomagnasaemia might include tremor, agitation, muscle fasciculation, depression, cardiac arrhythmia and hypokalaemia [6, 10, 67] (Table 6). Early signs of magnesium deficiency include loss of appetite, nausea, vomiting, fatigue and weakness [67]. As magnesium deficiency worsens, numbness, tingling, muscle contractions, cramps, seizures, sudden changes in behaviour caused by excessive electrical activity in the brain, personality changes [67], abnormal heart beat and coronary spasms might occur. Severe hypomagnesaemia is usually accompanied by other imbalances of electrolytes such as low levels of calcium and potassium in the blood (for mechanisms, see de Baaij et al. [48] in this supplement). However, even in patients with severe hypomagnesaemia, clinical signs associated with magnesium deficiency may be absent [7]. In addition, there seems to be a greater likelihood of clinical symptoms with a rapid decrease in serum magnesium concentration compared with a more gradual change. Therefore, physicians should not wait for clinical signs to occur before checking serum magnesium levels [7].
Table 6.
Clinical and laboratory manifestations of hypomagnesaemia. Reprinted from [7], with permission from Elsevier
| Neuromuscular | Cardiac | Central nervous system | Metabolic |
| Weakness | Arrhythmias | Depression | Hypokalaemia |
| Tremor | ECG changes | Agitation | Hypocalcaemia |
| Muscle fasciculation | Psychosis | ||
| Positive Chvostek's signb | Nystagmus | ||
| Positive Trousseau’s signc | Seizures | ||
| Dysphagia |
ECG, electrocardiogram.
Sign of tetany, an abnormal reaction (i.e. facial twitching) seen as a reaction to the tapping of the facial nerve.
Characteristic spasm of muscles of the hand and forearm seen following occlusion of the brachial artery.
Hypermagnesaemia
As the kidneys play a crucial role in magnesium homeostasis, in advanced chronic kidney disease, the compensatory mechanisms start to become inadequate and hypermagnesaemia may develop (see Cunningham et al [28] in this supplement). Symptomatic hypermagnesaemia may be caused by excessive oral administration of magnesium salts or magnesium-containing drugs such as some laxatives [89] and antacids [14], particularly when used in combination in the elderly and when renal function declines [8, 67, 90–94]. In addition, hypermagnesaemia may be iatrogenic, when magnesium sulphate is given as an infusion for the treatment of seizure prophylaxis in eclampsia [67, 95] or erroneously in high doses for magnesium supplementation [96, 97].
Prevalence of—mostly undiagnosed—hypermagnesaemia in hospitalized patients is reported, varying from 5.7% [98] to 7.9% [67] and 9.3% [69]. In intensive care patients, the prevalence of total hypermagnesaemia was reported as being 13.5%, whereas ionized hypermagnesaemia was 23.6% [99]. These studies did not specify whether hypermagnesaemia in hospitalized patients was a pathological consequence of severe disease, or if it was iatrogenic, perhaps reflecting excessive magnesium supplementation in intensive care.
Case reports exist of pre-term babies with extreme hypermagnesaemia—magnesium levels of 17.5 mmol/L [100] and 21.5 and 22.5 mmol/L [97]—which, in one case, was the result of a malfunctioning total parenteral nutrition mixing device. All three infants survived. There are other reports about affected neonates whose mothers had gestational toxicosis and who had been treated with magnesium sulphate because of eclamptic convulsion [7]. Excessive magnesium ingestion and intoxication was also reported in association with drowning in the Dead Sea. The average serum magnesium concentration in 48 adults who ‘nearly drowned’ in the Dead Sea was 3.16 mmol/L, with one patient recorded at 13.57 mmol/L [101–103].
Clinical signs of hypermagnesaemia
Serum magnesium concentrations, as reported in the literature, vary widely among patients with similar signs and symptoms. In the beginning, no immediate clinical signs may be present and hypermagnesaemia might stay undetected for sometime [67]. For example, increased magnesium concentrations (>1.07 mmol/L) were found in sera from 7.9% of 6252 patients, but no description of symptoms was noted in 80% of clinical charts, also not in patients with values >1.6 mmol/L (0.8%) [67]. Moderately elevated serum magnesium levels may be associated with hypotension, cutaneous flushing, nausea and vomiting, but these symptoms mostly occur only upon infusion of magnesium sulphate. At higher concentrations, magnesium might lead to neuromuscular dysfunction, ranging from drowsiness to respiratory depression, hypotonia, areflexia and coma in severe cases. Cardiac effects of hypermagnesaemia may include bradycardia; uncharacteristic electrocardiogram findings such as prolonged PR, QRS and QT intervals, complete heart block, atrial fibrillation and asystole. However, these findings are neither diagnostic nor specific for this metabolic abnormality [100] (Table 7).
Table 7.
Clinical manifestations of hypermagnaesemiaa
| Serum Mg (mmol/L) | Symptoms |
|||
| Neurological | Circulatory–respiratory–gastrointestinal | ECG | Comments | |
| 2.1–2.4 | Paralytic ileus [110] | Bradycardia [111] | Both single case reports, one Patient suffering from chronic renal insufficiency (creatinine clearance 13 ml/min) [111], iatrogenic [111] | |
| 2.5–4.0 | Deep tendon reflexes depressed [107, 108, 109], muscle weakness, slurred speech, lethargy [91] | Hypotension, nausea, flushing, decreased uterine tone upon magnesium infusion [109]; gastrointestinal paralysis [110] | Tachycardia, T-wave abnormalities; prolonged QT-time [91] | Target level for treatment of eclampsia is 2.5-4.0 mmol/L. [22, 108, 109, 112, 113]. However, serum Mg values are measured infrequently. Even in patients treated with MgSO4, decisions are based on clinical signs such as depressed deep-tendon reflexes [27]. Case reports [91, 110], renal insufficiency [110] |
| 3.7–4.9 | Confusion [114], loss of deep tendon reflexes [109], neuromuscular blockade, quadriparesis [115] | Hypotension [114] | Single case reports [114, 115], renal failure, PD treatment [115], review [109] | |
| 5.0–6.95 | Lethargy [94, 116], slurred speech, profound muscle weakness [90] | Hypotension [94, 116], increased respiratory rateb [94, 109]; respiratory arrest [95] | Atrial fibrillation [94]; QT prolongation [92, 116] sinus tachycardia, 1st degree AV-block, bradycardia [92] | Single case reports [92, 95, 116], case reports and reviews [90, 94], review [109] |
| Up to ≤7.65 and 7.3 | Paralysis of the limbs [117] | No respiratory arrest, slight decrease of blood pressure [117] | Sinus arrhythmia, slight alterations in ventricular action (T-wave, ST, R abnormalities, prolonged PR interval) [117] | Clinical investigation in two individuals in an experimental setting during magnesium sulphate infusion [117] |
| >8.9–10.65 | ‘Coma’ [118, 119], pseudocomatose state, central brain-stem herniation syndrome, non-fatal neuromuscular blockade | Profound hypotension, cardiopulmonary non-fatal arrest [118, 120], cardiovascular collapse at 25 mg/dL (10.3 mmol) [109] | Prolonged QT interval, bradycardia [120] | Case reports [118–121], review [109] |
| Up to 13. 5 [102]; 16.9 [122]; 17.8 [100]; 21.5 and 22.5 [97] | Respiratory depression, apnoea [97, 100], cardiopulmonary arrest [122] | Non-fatal refractory bradycardia [97] | Case reports, newborns [97, 100], case report, child [122], description of Dead Sea poisoning in 48 patients with different degrees of intoxication, the most dangerous combination occurred when serum calcium concentration was also high [102] | |
The table demonstrates a certain difficulty to link clinically distinct symptoms to specific serum magnesium levels. However, neurological symptoms, such as depression/loss of deep tendon reflexes, unequivocally occur at serum levels greater than 3.7 to 4.0 mmol/L.
Symptom also used for monitoring purposes in eclampsia [109]
AV, atrio-ventricular; Mg, magnesium; MgSO4, magnesium sulphate; PD, peritoneal dialysis.
Absence of deep tendon reflexes might help diagnose excess magnesium levels [7]. Deep tendon reflexes may be diminished at serum magnesium concentrations >2.5 mmol/L and will vanish when levels exceed 5 mmol/L. At these levels, severe muscle weakness has also been observed [21] (Table 7).
Treatment of hypo- and hypermagnesaemia
In cases of mild hypomagnesaemia in otherwise healthy individuals, oral magnesium administration is used successfully [68]. Acute and chronic oral magnesium supplementation has been described as well tolerated with a good safety profile [104, 105]. Intravenous administration of magnesium, mostly as magnesium sulphate, should be used when an immediate correction is mandatory as in patients with ventricular arrhythmia and severe hypomagnesaemia [106].
Treatment of patients with symptomatic hypermagnesaemia includes discontinuation of magnesium administration, use of supportive therapy and administration of calcium gluconate [6, 107]. Treatment of severe, symptomatic hypermagnesaemia may require haemodialysis [7].
Mild hypo- and hypermagnesaemia are quite common, especially in hospitalized patients, and may not be associated with clinical symptoms.
Severe hypo- and hypermagnesaemia show partially overlapping symptoms, making diagnosis difficult without assessment of serum magnesium concentration.
Conclusions
The chemistry of magnesium is unique among cations of biological relevance. Magnesium is essential for man and is required in relatively large amounts. Magnesium is a cofactor in >300 enzymatic reactions and thus it is essential for many crucial physiological functions, such as heart rhythm, vascular tone, nerve function and muscle contraction and relaxation. Magnesium is also needed for bone formation and can also be referred to as a natural ‘calcium antagonist’. However, hypomagnesaemia is rather common, in particular, in hospitalized patients. Moreover, as the intake of refined foods increases—as appears to be the case in developed countries—magnesium deficiency will most likely evolve into a more common disorder. Nonetheless, total serum magnesium is rarely measured in clinical practice. Despite some limitations, the assessment of serum magnesium concentration is inexpensive and easy to employ and provides important information about magnesium status in patients.
Acknowledgments
Ronald J. Elin, Department of Pathology and Laboratory Medicine, School of Medicine, University of Louisville, Louisville, KY USA, thoroughly investigated the basics of magnesium and published numerous scientific papers on this topic. As basic knowledge comes from these publications, we often quoted his work. In addition, the authors thank Martina Sintzel, Zürich, Switzerland and Yvette C. Zwick, Munich, Germany for providing writing and editorial assistance and Richard Clark, Dunchurch, UK for his comments on the final manuscript, all on behalf of Fresenius Medical Care Deutschland GmbH. Fresenius also made an unrestricted educational grant to meet the cost of preparing this article. These declarations are in line with the European Medical Writers’ Association guidelines.
Conflict of interest statement. W.J.-D. has received speakers' honoraria from Amgen, Genzyme, Fresenius and Köhler-Chemie. M.K. has received speaker's and/or consultancy honoraria from Amgen, Abbott, Fresenius, Genzyme, Medice and Shire and research support from Abbott and Amgen.
References
- 1.Cotton FA, Wilkinson G. Weilheim, Germany: Chemie GmbH; 1967. Anorganische Chemie. [Google Scholar]
- 2.Weast RC. Handbook of Chemistry and Physics. Boca Raton, FL: CRC Press; 1987. [Google Scholar]
- 3.Hollemann AF, Wiberg E. Lehrbuch der anorganischen Chemie. Berlin, Germany: De Gruyter; 1964. [Google Scholar]
- 4.Bodaker I, Sharon I, Suzuki MT, et al. Comparative community genomics in the Dead Sea: an increasingly extreme environment. ISME J. 2010;4:399–407. doi: 10.1038/ismej.2009.141. [DOI] [PubMed] [Google Scholar]
- 5.Maguire ME, Cowan JA. Magnesium chemistry and biochemistry. Biometals. 2002;15:203–210. doi: 10.1023/a:1016058229972. [DOI] [PubMed] [Google Scholar]
- 6.Wacker W. Magnesium and Man. Cambridge, MA: Havard University Press; 1980. pp. 1–184. [Google Scholar]
- 7.Elin RJ. Magnesium metabolism in health and disease. Dis Mon. 1988;34:161–218. doi: 10.1016/0011-5029(88)90013-2. [DOI] [PubMed] [Google Scholar]
- 8.Swaminathan R. Magnesium metabolism and its disorders. Clin Biochem Rev. 2003;24:47–66. [PMC free article] [PubMed] [Google Scholar]
- 9.Feillet-Coudray C, Coudray C, Gueux E, et al. A new in vitro blood load test using a magnesium stable isotope for assessment of magnesium status. J Nutr. 2003;133:1220–1223. doi: 10.1093/jn/133.4.1220. [DOI] [PubMed] [Google Scholar]
- 10.Saris NE, Mervaala E, Karppanen H, et al. An update on physiological, clinical and analytical aspects. Clin Chim Acta. 2000;294:1–26. doi: 10.1016/s0009-8981(99)00258-2. [DOI] [PubMed] [Google Scholar]
- 11.Grubbs RD, Maguire ME. Magnesium as a regulatory cation: criteria and evaluation. Magnesium. 1987;6:113–127. [PubMed] [Google Scholar]
- 12.Maguire ME. Magnesium: a regulated and regulatory cation. Met Ions Biol Syst. 1990;26:135–153. [Google Scholar]
- 13.Walser M. Magnesium metabolism. Ergeb Physiol. 1967;59:185–296. doi: 10.1007/BF02269144. [DOI] [PubMed] [Google Scholar]
- 14.Aikawa JK. Magnesium: Its Biological Significance. Boca Raton, FL: CRC Press; 1981. [Google Scholar]
- 15.Fox C, Ramsoomair D, Carter C. Magnesium: its proven and potential clinical significance. South Med J. 2001;94:1195–1201. [PubMed] [Google Scholar]
- 16.Lewellen TK, Nelp WB, Murano R, et al. Absolute measurement of total-body calcium by the Ar-37 method-preliminary results: concise communication. J Nucl Med. 1977;18:929–932. [PubMed] [Google Scholar]
- 17.Elin RJ. Assessment of magnesium status for diagnosis and therapy. Magnes Res. 2010;23:194–198. doi: 10.1684/mrh.2010.0213. [DOI] [PubMed] [Google Scholar]
- 18.Rude R. Magnesium disorders. In: Kokko J, Tannen R (eds) Fluids and electrolytes. Philadelphia, PA: W.B. Saunders Company, 1996, pp. 421–445. [Google Scholar]
- 19.Alfrey AC, Miller NL. Bone magnesium pools in uremia. J Clin Invest. 1973;52:3019–3027. doi: 10.1172/JCI107500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kroll MH, Elin RJ. Relationships between magnesium and protein concentrations in serum. Clin Chem. 1985;31:244–246. [PubMed] [Google Scholar]
- 21.Touyz RM. Magnesium in clinical medicine. Front Biosci. 2004;9:1278–1293. doi: 10.2741/1316. [DOI] [PubMed] [Google Scholar]
- 22.Fawcett WJ, Haxby EJ, Male DA. Magnesium: physiology and pharmacology. Br J Anaesth. 1999;83:302–320. doi: 10.1093/bja/83.2.302. [DOI] [PubMed] [Google Scholar]
- 23.Speich M, Bousquet B, Nicolas G. Reference values for ionized, complexed, and protein-bound plasma magnesium in men and women. Clin Chem. 1981;27:246–248. [PubMed] [Google Scholar]
- 24.Walser M. Ion association. VI. Interactions between calcium, magnesium, inorganic phosphate, citrate and protein in normal human plasma. J Clin Invest. 1961;40:723–730. doi: 10.1172/JCI104306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Navarro-Gonzalez JF, Mora-Fernandez C, Garcia-Perez J. Clinical implications of disordered magnesium homeostasis in chronic renal failure and dialysis. Semin Dial. 2009;22:37–44. doi: 10.1111/j.1525-139X.2008.00530.x. [DOI] [PubMed] [Google Scholar]
- 26.Wills MR, Lewin MR. Plasma calcium fractions and the protein-binding of calcium in normal subjects and in patients with hypercalcaemia and hypocalcaemia. J Clin Pathol. 1971;24:856–866. doi: 10.1136/jcp.24.9.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Keller H. Klinisch-chemische Labordiagnostik für die Praxis. Stuttgart, Germany: Georg Thieme; 1991. p. 222. [Google Scholar]
- 28.Cunningham J, Rodríguez JM, Messa P. Magnesium in chronic kidney disease stages 3 and 4, and in dialysis patients. Clin Kidney J. 2012;5(Suppl 1):i39–i51. doi: 10.1093/ndtplus/sfr166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shechter M, Merz CN, Paul-Labrador M, et al. Oral magnesium supplementation inhibits platelet-dependent thrombosis in patients with coronary artery disease. Am J Cardiol. 1999;84:152–156. doi: 10.1016/s0002-9149(99)00225-8. [DOI] [PubMed] [Google Scholar]
- 30.Altura BM, Altura BT. New perspectives on the role of magnesium in the pathophysiology of the cardiovascular system. I. Clinical aspects. Magnesium. 1985;4:226–244. [PubMed] [Google Scholar]
- 31.Reis MA, Reyes FG, Saad MJ, et al. Magnesium deficiency modulates the insulin signaling pathway in liver but not muscle of rats. J Nutr. 2000;130:133–138. doi: 10.1093/jn/130.2.133. [DOI] [PubMed] [Google Scholar]
- 32.Barbagallo M, Dominguez LJ. Magnesium metabolism in type 2 diabetes mellitus, metabolic syndrome and insulin resistance. Arch Biochem Biophys. 2007;458:40–47. doi: 10.1016/j.abb.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 33.Takaya J, Kaneko K. Small for gestational age and magnesium in cord blood platelets: intrauterine magnesium deficiency may induce metabolic syndrome in later life. J Pregnancy. 2011;2011:270474. doi: 10.1155/2011/270474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hunter DR, Haworth RA, Southard JH. Relationship between configuration, function, and permeability in calcium-treated mitochondria. J Biol Chem. 1976;251:5069–5077. [PubMed] [Google Scholar]
- 35.Orrenius S, Zhivotovsky B, Nicotera P. Regulation of cell death: the calcium-apoptosis link. Nat Rev Mol Cell Biol. 2003;4:552–565. doi: 10.1038/nrm1150. [DOI] [PubMed] [Google Scholar]
- 36.Reynolds JL, Joannides AJ, Skepper JN, et al. Human vascular smooth muscle cells undergo vesicle-mediated calcification in response to changes in extracellular calcium and phosphate concentrations: a potential mechanism for accelerated vascular calcification in ESRD. J Am Soc Nephrol. 2004;15:2857–2867. doi: 10.1097/01.ASN.0000141960.01035.28. [DOI] [PubMed] [Google Scholar]
- 37.Geiger H, Wanner C. Magnesium in disease. Clin Kidney J. 2012;5(Suppl 1):i25–i38. doi: 10.1093/ndtplus/sfr165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elliott DA, Rizack MA. Epinephrine and adrenocorticotropic hormone-stimulated magnesium accumulation in adipocytes and their plasma membranes. J Biol Chem. 1974;249:3985–3990. [PubMed] [Google Scholar]
- 39.Page E, Polimeni PI. Magnesium exchange in rat ventricle. J Physiol. 1972;224:121–139. doi: 10.1113/jphysiol.1972.sp009884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Polimeni PI, Page E. Magnesium in heart muscle. Circ Res. 1973;33:367–374. doi: 10.1161/01.res.33.4.367. [DOI] [PubMed] [Google Scholar]
- 41.Rogers T, Mahan P. Exchange of radioactive magnesium in the rat. Proc Soc Exp Biol Med. 1959;100:235–239. doi: 10.3181/00379727-100-24584. [DOI] [PubMed] [Google Scholar]
- 42.Rogers T. Distribution of Magnesium in the Rat. Radioisotopes in Animal Nutrition and Physiology. Vienna, Austria: International Atomic Energy Commission; 1965. pp. 285–282. [Google Scholar]
- 43.Avioli LV, Berman M. Mg28 kinetics in man. J Appl Physiol. 1966;21:1688–1694. doi: 10.1152/jappl.1966.21.6.1688. [DOI] [PubMed] [Google Scholar]
- 44.Marx A, Neutra RR. Magnesium in drinking water and ischemic heart disease. Epidemiol Rev. 1997;19:258–272. doi: 10.1093/oxfordjournals.epirev.a017957. [DOI] [PubMed] [Google Scholar]
- 45.Ford ES, Mokdad AH. Dietary magnesium intake in a national sample of US adults. J Nutr. 2003;133:2879–2882. doi: 10.1093/jn/133.9.2879. [DOI] [PubMed] [Google Scholar]
- 46.Graham L, Caesar J, Burgen A. Gastrointestinal absorption and excretion of Mg28 in man. Metabolism. 1960;9:646–659. [PubMed] [Google Scholar]
- 47.Kayne LH, Lee DB. Intestinal magnesium absorption. Miner Electrolyte Metab. 1993;19:210–217. [PubMed] [Google Scholar]
- 48.de Baaij JHF, Hoenderop JGJ, Bindels RJM. Regulation of magnesium balance: lessons learned from human genetic disease. Clin Kidney J. 2012;5(Suppl 1):i15–i24. doi: 10.1093/ndtplus/sfr164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dirks JH. The kidney and magnesium regulation. Kidney Int. 1983;23:771–777. doi: 10.1038/ki.1983.93. [DOI] [PubMed] [Google Scholar]
- 50.Quamme GA, Dirks JH. The physiology of renal magnesium handling. Ren Physiol. 1986;9:257–269. doi: 10.1159/000173090. [DOI] [PubMed] [Google Scholar]
- 51.Barnes BA, Cope O, Harrison T. Magnesium conservation in the human being on a low magnesium diet. J Clin Invest. 1958;37:430–440. doi: 10.1172/JCI103623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Massry SG, Seelig MS. Hypomagnesemia and hypermagnesemia. Clin Nephrol. 1977;7:147–153. [PubMed] [Google Scholar]
- 53.Elin RJ, Hosseini JM, Gill JR., Jr Erythrocyte and mononuclear blood cell magnesium concentrations are normal in hypomagnesemic patients with chronic renal magnesium wasting. J Am Coll Nutr. 1994;13:463–466. doi: 10.1080/07315724.1994.10718435. [DOI] [PubMed] [Google Scholar]
- 54.Martin BJ, Lyon TD, Walker W, et al. Mononuclear blood cell magnesium in older subjects: evaluation of its use in clinical practice. Ann Clin Biochem. 1993;30 doi: 10.1177/000456329303000104. (Pt 1): 23–27. [DOI] [PubMed] [Google Scholar]
- 55.Moller JB, Klaaborg KE, Alstrup P, et al. Magnesium content of the human heart. Scand J Thorac Cardiovasc Surg. 1991;25:155–158. doi: 10.3109/14017439109098102. [DOI] [PubMed] [Google Scholar]
- 56.Huijgen HJ, Sanders R, van Olden RW, et al. Intracellular and extracellular blood magnesium fractions in hemodialysis patients; is the ionized fraction a measure of magnesium excess? Clin Chem. 1998;44:639–648. [PubMed] [Google Scholar]
- 57.Spiegel DM. Magnesium in chronic kidney disease: unanswered questions. Blood Purif. 2011;31:172–176. doi: 10.1159/000321837. [DOI] [PubMed] [Google Scholar]
- 58.Bardicef M, Bardicef O, Sorokin Y, et al. Extracellular and intracellular magnesium depletion in pregnancy and gestational diabetes. Am J Obstet Gynecol. 1995;172:1009–1013. doi: 10.1016/0002-9378(95)90035-7. [DOI] [PubMed] [Google Scholar]
- 59.Young DS. Effects of Preanalytical Variables on Clinical Laboratory Tests. Washington, DC: AACC Press; 1997. [Google Scholar]
- 60.Gonzalez-Revalderia J, Garcia-Bermejo S, Menchen-Herreros A, et al. Biological variation of Zn, Cu, and Mg in serum of healthy subjects. Clin Chem. 1990;36:2140–2141. [PubMed] [Google Scholar]
- 61.Tietz NW. Clinical Guide to Laboratory Tests. Philadelphia, PA: WB Saunders; 1990. [Google Scholar]
- 62.Maj-Zurawska M. Clinical findings on human blood with the KONE ISE for Mg2+ . Scand J Clin Lab Invest Suppl. 1994;217:69–76. [PubMed] [Google Scholar]
- 63.Nicar MJ, Pak CY. Oral magnesium load test for the assessment of intestinal magnesium absorption. Application in control subjects, absorptive hypercalciuria, primary hyperparathyroidism, and hypoparathyroidism. Miner Electrolyte Metab. 1982;8:44–51. [PubMed] [Google Scholar]
- 64.Cohen L, Laor A. Correlation between bone magnesium concentration and magnesium retention in the intravenous magnesium load test. Magnes Res. 1990;3:271–274. [PubMed] [Google Scholar]
- 65.Rude RK. Magnesium metabolism and deficiency. Endocrinol Metab Clin North Am. 1993;22:377–395. [PubMed] [Google Scholar]
- 66.Nadler JL, Rude RK. Disorders of magnesium metabolism. Endocrinol Metab Clin North Am. 1995;24:623–641. [PubMed] [Google Scholar]
- 67.Hashizume N, Mori M. An analysis of hypermagnesemia and hypomagnesemia. Jpn J Med. 1990;29:368–372. doi: 10.2169/internalmedicine1962.29.368. [DOI] [PubMed] [Google Scholar]
- 68.Guerrero-Romero F, Tamez-Perez HE, Gonzalez-Gonzalez G, et al. Oral magnesium supplementation improves insulin sensitivity in non-diabetic subjects with insulin resistance. A double-blind placebo-controlled randomized trial. Diabetes Metab. 2004;30:253–258. doi: 10.1016/s1262-3636(07)70116-7. [DOI] [PubMed] [Google Scholar]
- 69.Wong ET, Rude RK, Singer FR, et al. A high prevalence of hypomagnesemia and hypermagnesemia in hospitalized patients. Am J Clin Pathol. 1983;79:348–352. doi: 10.1093/ajcp/79.3.348. [DOI] [PubMed] [Google Scholar]
- 70.Chernow B, Bamberger S, Stoiko M, et al. Hypomagnesemia in patients in postoperative intensive care. Chest. 1989;95:391–397. doi: 10.1378/chest.95.2.391. [DOI] [PubMed] [Google Scholar]
- 71.Whang R, Ryder KW. Frequency of hypomagnesemia and hypermagnesemia. Requested vs routine. JAMA. 1990;263:3063–3064. [PubMed] [Google Scholar]
- 72.Ryzen E, Wagers PW, Singer FR, et al. Magnesium deficiency in a medical ICU population. Crit Care Med. 1985;13:19–21. doi: 10.1097/00003246-198501000-00006. [DOI] [PubMed] [Google Scholar]
- 73.Bernstein L. Improving Magnesium Absorption and Bioavailibility. Geriatric Times; 2002. 3. [Google Scholar]
- 74.Ryan MP. Diuretics and potassium/magnesium depletion. Directions for treatment. Am J Med. 1987;82:38–47. doi: 10.1016/0002-9343(87)90131-8. [DOI] [PubMed] [Google Scholar]
- 75.Elliott C, Newman N, Madan A. Gentamicin effects on urinary electrolyte excretion in healthy subjects. Clin Pharmacol Ther. 2000;67:16–21. doi: 10.1067/mcp.2000.103864. [DOI] [PubMed] [Google Scholar]
- 76.Wazny LD, Brophy DF. Amiloride for the prevention of amphotericin B-induced hypokalemia and hypomagnesemia. Ann Pharmacother. 2000;34:94–97. doi: 10.1345/aph.19127. [DOI] [PubMed] [Google Scholar]
- 77.June CH, Thompson CB, Kennedy MS, et al. Correlation of hypomagnesemia with the onset of cyclosporine-associated hypertension in marrow transplant patients. Transplantation. 1986;41:47–51. doi: 10.1097/00007890-198601000-00009. [DOI] [PubMed] [Google Scholar]
- 78.Lote CJ, Thewles A, Wood JA, et al. The hypomagnesaemic action of FK506: urinary excretion of magnesium and calcium and the role of parathyroid hormone. Clin Sci (Lond) 2000;99:285–292. [PubMed] [Google Scholar]
- 79.Lajer H, Daugaard G. Cisplatin and hypomagnesemia. Cancer Treat Rev. 1999;25:47–58. doi: 10.1053/ctrv.1999.0097. [DOI] [PubMed] [Google Scholar]
- 80.Tejpar S, Piessevaux H, Claes K, et al. Magnesium wasting associated with epidermal-growth-factor receptor-targeting antibodies in colorectal cancer: a prospective study. Lancet Oncol. 2007;8:387–394. doi: 10.1016/S1470-2045(07)70108-0. [DOI] [PubMed] [Google Scholar]
- 81.Broeren MA, Geerdink EA, Vader HL, et al. Hypomagnesemia induced by several proton-pump inhibitors. Ann Intern Med. 2009;151:755–756. doi: 10.7326/0003-4819-151-10-200911170-00016. [DOI] [PubMed] [Google Scholar]
- 82.Otsuka M, Kanamori H, Sasaki S, et al. Torsades de pointes complicating pentamidine therapy of Pneumocystis carinii pneumonia in acute myelogenous leukemia. Intern Med. 1997;36:705–708. doi: 10.2169/internalmedicine.36.705. [DOI] [PubMed] [Google Scholar]
- 83.Huycke MM, Naguib MT, Stroemmel MM, et al. A double-blind placebo-controlled crossover trial of intravenous magnesium sulfate for foscarnet-induced ionized hypocalcemia and hypomagnesemia in patients with AIDS and cytomegalovirus infection. Antimicrob Agents Chemother. 2000;44:2143–2148. doi: 10.1128/aac.44.8.2143-2148.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.al-Ghamdi SM, Cameron EC, Sutton RA. Magnesium deficiency: pathophysiologic and clinical overview. Am J Kidney Dis. 1994;24:737–752. doi: 10.1016/s0272-6386(12)80667-6. [DOI] [PubMed] [Google Scholar]
- 85.Klein GL, Herndon DN. Magnesium deficit in major burns: role in hypoparathyroidism and end-organ parathyroid hormone resistance. Magnes Res. 1998;11:103–109. [PubMed] [Google Scholar]
- 86.Aglio LS, Stanford GG, Maddi R, et al. Hypomagnesemia is common following cardiac surgery. J Cardiothorac Vasc Anesth. 1991;5:201–208. doi: 10.1016/1053-0770(91)90274-w. [DOI] [PubMed] [Google Scholar]
- 87.Kuller L, Farrier N, Caggiula A, et al. Relationship of diuretic therapy and serum magnesium levels among participants in the Multiple Risk Factor Intervention Trial. Am J Epidemiol. 1985;122:1045–1059. doi: 10.1093/oxfordjournals.aje.a114186. [DOI] [PubMed] [Google Scholar]
- 88.Knoers NV. Inherited forms of renal hypomagnesemia: an update. Pediatr Nephrol. 2009;24:697–705. doi: 10.1007/s00467-008-0968-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Xing JH, Soffer EE. Adverse effects of laxatives. Dis Colon Rectum. 2001;44:1201–1209. doi: 10.1007/BF02234645. [DOI] [PubMed] [Google Scholar]
- 90.Fung MC, Weintraub M, Bowen DL. Hypermagnesemia. Elderly over-the-counter drug users at risk. Arch Fam Med. 1995;4:718–723. doi: 10.1001/archfami.4.8.718. [DOI] [PubMed] [Google Scholar]
- 91.Clark BA, Brown RS. Unsuspected morbid hypermagnesemia in elderly patients. Am J Nephrol. 1992;12:336–343. doi: 10.1159/000168469. [DOI] [PubMed] [Google Scholar]
- 92.Kontani M, Hara A, Ohta S, et al. Hypermagnesemia induced by massive cathartic ingestion in an elderly woman without pre-existing renal dysfunction. Intern Med. 2005;44:448–452. doi: 10.2169/internalmedicine.44.448. [DOI] [PubMed] [Google Scholar]
- 93.Mordes JP, Wacker WE. Excess magnesium. Pharmacol Rev. 1978;29:273–300. [PubMed] [Google Scholar]
- 94.Onishi S, Yoshino S. Cathartic-induced fatal hypermagnesemia in the elderly. Intern Med. 2006;45:207–210. doi: 10.2169/internalmedicine.45.1482. [DOI] [PubMed] [Google Scholar]
- 95.Cao Z, Bideau R, Valdes R, Jr, et al. Acute hypermagnesemia and respiratory arrest following infusion of MgSO4 for tocolysis. Clin Chim Acta. 1999;285:191–193. doi: 10.1016/s0009-8981(99)00110-2. [DOI] [PubMed] [Google Scholar]
- 96.Vissers RJ, Purssell R. Iatrogenic magnesium overdose: two case reports. J Emerg Med. 1996;14:187–191. doi: 10.1016/0736-4679(95)02115-9. [DOI] [PubMed] [Google Scholar]
- 97.Ali A, Walentik C, Mantych GJ, et al. Iatrogenic acute hypermagnesemia after total parenteral nutrition infusion mimicking septic shock syndrome: two case reports. Pediatrics. 2003;112:e70–e72. doi: 10.1542/peds.112.1.e70. [DOI] [PubMed] [Google Scholar]
- 98.Whang R, Whang DD. Update: mechanisms by which magnesium modulates intracellular potassium. J Am Coll Nutr. 1990;9:84–85. doi: 10.1080/07315724.1990.10720354. [DOI] [PubMed] [Google Scholar]
- 99.Escuela MP, Guerra M, Anon JM, et al. Total and ionized serum magnesium in critically ill patients. Intensive Care Med. 2005;31:151–156. doi: 10.1007/s00134-004-2508-x. [DOI] [PubMed] [Google Scholar]
- 100.Huey CG, Chan KM, Wong ET, et al. Los Angeles County-University of Southern California Medical Center clinical pathology case conference: extreme hypermagnesemia in a neonate. Clin Chem. 1995;41:615–618. [PubMed] [Google Scholar]
- 101.Oren S, Rapoport J, Zlotnik M, et al. Extreme hypermagnesemia due to ingestion of Dead Sea water. Nephron. 1987;47:199–201. doi: 10.1159/000184491. [DOI] [PubMed] [Google Scholar]
- 102.Porath A, Mosseri M, Harman I, et al. Dead Sea water poisoning. Ann Emerg Med. 1989;18:187–191. doi: 10.1016/s0196-0644(89)80112-x. [DOI] [PubMed] [Google Scholar]
- 103.Topf JM, Murray PT. Hypomagnesemia and hypermagnesemia. Rev Endocr Metab Disord. 2003;4:195–206. doi: 10.1023/a:1022950321817. [DOI] [PubMed] [Google Scholar]
- 104.Mathers TW, Beckstrand RL. Oral magnesium supplementation in adults with coronary heart disease or coronary heart disease risk. J Am Acad Nurse Pract. 2009;21:651–657. doi: 10.1111/j.1745-7599.2009.00460.x. [DOI] [PubMed] [Google Scholar]
- 105.Fuentes JC, Salmon AA, Silver MA. Acute and chronic oral magnesium supplementation: effects on endothelial function, exercise capacity, and quality of life in patients with symptomatic heart failure. Congest Heart Fail. 2006;12:9–13. doi: 10.1111/j.1527-5299.2006.04692.x. [DOI] [PubMed] [Google Scholar]
- 106.Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e385–e484. doi: 10.1161/CIRCULATIONAHA.106.178233. [DOI] [PubMed] [Google Scholar]
- 107.Krendel DA. Hypermagnesemia and neuromuscular transmission. Semin Neurol. 1990;10:42–45. doi: 10.1055/s-2008-1041252. [DOI] [PubMed] [Google Scholar]
- 108.Pritchard JA. The use of magnesium sulfate in preeclampsia-eclampsia. J Reprod Med. 1979;23:107–114. [PubMed] [Google Scholar]
- 109.Turner JA. Diagnosis and management of pre-eclampsia: an update. Int J Womens Health. 2010;2:327–337. doi: 10.2147/IJWH.S8550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Golzarian J, Scott HW, Jr, Richards WO. Hypermagnesemia-induced paralytic ileus. Dig Dis Sci. 1994;39:1138–1142. doi: 10.1007/BF02087570. [DOI] [PubMed] [Google Scholar]
- 111.Berns AS, Kollmeyer KR. Magnesium-induced bradycardia. Ann Intern Med. 1976;85:760–761. doi: 10.7326/0003-4819-85-6-760. [DOI] [PubMed] [Google Scholar]
- 112.Yoshida A, Itoh Y, Nagaya K, et al. Prolonged relaxant effects of vecuronium in patients with deliberate hypermagnesemia: time for caution in cesarean section. J Anesth. 2006;20:33–35. doi: 10.1007/s00540-005-0354-9. [DOI] [PubMed] [Google Scholar]
- 113.ANZCA Guidelines. Management of pre-clampsia and eclampsia. 2011 http://www.anzca.edu.au/fellows/sig/obstetric-anaesthesia-sig/obstetric-anaesthesia-scientific-evidence/management-of-pre-eclampsia-and-eclampsia.html. [Google Scholar]
- 114.McLaughlin SA, McKinney PE. Antacid-induced hypermagnesemia in a patient with normal renal function and bowel obstruction. Ann Pharmacother. 1998;32:312–315. doi: 10.1345/aph.17284. [DOI] [PubMed] [Google Scholar]
- 115.Jung GJ, Gil HW, Yang JO, et al. Severe hypermagnesemia causing quadriparesis in a CAPD patient. Perit Dial Int. 2008;28:206. [PubMed] [Google Scholar]
- 116.Kutsal E, Aydemir C, Eldes N, et al. Severe hypermagnesemia as a result of excessive cathartic ingestion in a child without renal failure. Pediatr Emerg Care. 2007;23:570–572. doi: 10.1097/PEC.0b013e31812eef1c. [DOI] [PubMed] [Google Scholar]
- 117.Somjen G, Hilmy M, Stephen CR. Failure to anesthetize human subjects by intravenous administration of magnesium sulfate. J Pharmacol Exp Ther. 1966;154:652–659. [PubMed] [Google Scholar]
- 118.Qureshi T, Melonakos TK. Acute hypermagnesemia after laxative use. Ann Emerg Med. 1996;28:552–555. doi: 10.1016/s0196-0644(96)70120-8. [DOI] [PubMed] [Google Scholar]
- 119.Gerard SK, Hernandez C, Khayam-Bashi H. Extreme hypermagnesemia caused by an overdose of magnesium-containing cathartics. Ann Emerg Med. 1988;17:728–731. doi: 10.1016/s0196-0644(88)80624-3. [DOI] [PubMed] [Google Scholar]
- 120.Smilkstein MJ, Smolinske SC, Kulig KW, et al. Severe hypermagnesemia due to multiple-dose cathartic therapy. West J Med. 1988;148:208–211. [PMC free article] [PubMed] [Google Scholar]
- 121.Rizzo MA, Fisher M, Lock JP. Hypermagnesemic pseudocoma. Arch Intern Med. 1993;153:1130–1132. [PubMed] [Google Scholar]
- 122.Tofil NM, Benner KW, Winkler MK. Fatal hypermagnesemia caused by an Epsom salt enema: a case illustration. South Med J. 2005;98:253–256. doi: 10.1097/01.SMJ.0000145307.80421.4B. [DOI] [PubMed] [Google Scholar]